Abstract
Background:
Using the CHA2DS2-VASc score to recognize the risk of stroke in patients with atrial fibrillation has been well-established. However, few studies have assessed whether the CHA2DS2-VASc score has a similar predictive value in recurrence after myocardial infarction (MI).
Methods:
We conducted a retrospective observational cohort study of adult inpatients with MI. The CHA2DS2-VASc and modified CHA2DS2-VASc (MCHA2DS2-VASc) scores of all patients were calculated. The associations of both scores with recurrent MI were analyzed.
Results:
A total of 6,700 patients with MI (60.0 ± 11.1 years, 77.2% men) were enrolled, and 759 (11.3%) presented a definite recurrence during hospitalization. After multivariable adjustment by logistic regression in patients with MI, the CHA2DS2-VASc and MCHA2DS2-VASc scores were independently associated with recurrence. The MCHA2DS2-VASc score showed a better predictive value for risk of recurrence than that of CHA2DS2-VASc in overall [area under the receiver operating characteristic curve (AUC) 0.757 vs. 0.676] or male patients (AUC 0.759 vs. 0.708). MCHA2DS2-VASc was superior to CHA2DS2-VASc for identifying “truly high-risk” patients with MI, regardless of overall patients or sex-specific subgroups. The two scores had a similar focus on the identification of “low-risk” patients in overall or women, but not in men.
Conclusion:
The CHA2DS2-VASc and MCHA2DS2-VASc scores for predicting recurrence are validated in patients with MI. However, MCHA2DS2-VASc could be more helpful to secondary prevention than CHA2DS2-VASc after MI, especially in men. The superiority of MCHA2DS2-VASc compared with CHA2DS2-VASc in women is just more discriminatory for “truly high-risk” patients.
Introduction
In recent years, morbidity and mortality from coronary heart disease (CHD) have been declining in most developed countries but rising in other low-and middle-income countries. Globally, death and disability rates from CHD in patients presenting with myocardial infarction (MI) remain high when the quality of medical and health services is improved remarkably (1). Patients with recurrent MI often have a poor prognosis, largely due to a reduction in cardiac pump activity and malignant arrhythmias, and even trigger sudden cardiac death (2, 3). Better management via risk stratification is imperative for short- and long-term secondary prevention of MI. A number of clinically applicable cardiovascular risk-stratification schemes have been proven as efficient tools for risk stratification and therapeutic decision-making, such as Thrombolysis in Myocardial Infarction (TIMI) risk score, which is based on nine clinical characteristics (4).
Major international atrial fibrillation (AF) guidelines recommend estimating stroke risk in patients with AF based on the CHA2DS2-VASc score, which summarizes common stroke risk factors. CHA2DS2-VASc score performs just modestly in predicting high-risk patients, and its advantage is better at identifying “truly low-risk” patients with AF who develop stroke and thromboembolism (5).
Many clinical stroke risk factors (e.g., obstructive sleep apnea, left atrium dilatation, and renal impairment) (6–8) as well as some biomarkers (e.g., troponin, natriuretic peptides, and von Willebrand factor) (9, 10) are closely related to the stroke risk, but they do not improve the predictive value of CHA2DS2-VASc score. Moreover, patients with MI seem to be at increased risk for recurrent major adverse cardiovascular events (MACEs), owing to their clinical characteristics, comorbidities, and biomarkers, such as elderly (especially older women) (11), diabetes mellitus (DM), heart failure (HF), renal dysfunction (12), and interleukin-1beta (13). Coincidentally, there are some concordant factors between stroke and recurrent MI, which are two different disorders. Therefore, this study was conducted to evaluate whether the CHA2DS2-VASc score could assess the risk of recurrence in patients with MI, presented overall and stratified by sex.
Materials and methods
Study population
A retrospective observational cohort of 6,700 adult inpatients in the First Affiliated Hospital of Nanjing Medical University, Affiliated Hospital of Xuzhou Medical University, and Xuzhou Central Hospital between January 2019 and December 2021 was evaluated. This study was conducted on inpatients with types 1–3 MI but not types 4–5 procedure-related MI, which occurred more than 28 days at enrollment (2). The history of MI was ascertained based on self-reporting or medical records. Patients with recurrent MI were enrolled who underwent acute myocardial infarction (AMI) during hospitalization. All patients had an MI attack for the first time during enrollment. Subjects with recurrent MI diagnosed prior to the enrollment were excluded. In addition, the study excluded patients who had congenital cardiovascular diseases, idiopathic cardiomyopathy, rheumatic mitral stenosis, mechanical or bioprosthetic heart valve, or mitral valve repair, malignant tumor, liver or kidney failure, major bleeding, and immune diseases. This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2022-SR-062) under a waiver of informed consent, in accordance with ethical guidelines set up by the World Medical Association (The Declaration of Helsinki).
Data collection
Investigators collected epidemiological, demographic, clinical, and outcome data from electronic medical records, such as each patient’s age, sex, and history of hypertension, DM, HF, thromboembolism, dyslipidemia, and AF. All information was recorded on a computerized database using a standardized electronic data collection form, which serves as the data source of this study.
Definitions and outcome measures
Each patient’s CHA2DS2-VASc score ranging from 0 to 9 was calculated [patients were given 1 point for HF, hypertension, age 65–74 years, DM, vascular disease, and female sex and 2 points for age ≥ 75 years and prior stroke/transient ischemic attack (TIA)/embolus] using baseline characteristics. Modified CHA2DS2-VASc (MCHA2DS2-VASc) to give 1 point for age ≥ 75 years, DM, and dyslipidemia, 2 points for prior stroke/TIA/embolus and male sex, 3 points for hypertension, and 5 points for HF, ranged from 0 to 15. The optimal cutoff point of CHA2DS2-VASc was 3 and MCHA2DS2-VASc was 8 for predicting the incidence of recurrent MI, which was determined by receiver operating characteristic (ROC) curve, area under the curve (AUC) analysis, and Youden index. Patients were subsequently categorized into the low-risk group (0–2) and high-risk group (3–9) according to the CHA2DS2-VASc and low-risk group (0–7) and high-risk group (8–15) according to the MCHA2DS2-VASc.
The primary outcome of this study was the occurrence of AMI in hospitals. The definition of AMI based on the Fourth Universal Definition of Myocardial Infarction (2018) is as follows: a clinical (or pathological) event in the setting of evidence of acute myocardial ischemia (ischemic symptoms, ischemic electrocardiographic changes, coronary artery intervention, new wall motion abnormalities, or fixed defect on radionuclide scanning) in which there is the presence of acute myocardial cell death detected by abnormal cardiac biomarkers (14).
Statistical analysis
Baseline characteristics of patients were described using means and standard deviations (SDs) for normally distributed continuous data and numbers and percentages for categorical data. These characteristics were compared using Student’s t-tests, chi-square tests, or Kruskal–Wallis tests, as appropriate. The correlations between CHA2DS2-VASc and recurrence rate and MCHA2DS2-VASc and recurrence rate were evaluated using the test of Spearman’s rank-correlation coefficient. To identify the independent predictors of in-hospital recurrent MI, a multivariate logistic regression model was performed using the following variables: age, sex, hypertension, DM, HF, thromboembolism, dyslipidemia, and AF. The results of logistic regression analysis were reported as an odds ratio (OR) with a 95% confidence interval (CI). The predictive value of CHA2DS2-VASc and MCHA2DS2-VASc with regard to recurrence was assessed using AUC in the presentation of the ROC curve. The AUC used to quantify the discriminatory capacity of the two scores for recurrence is defined as excellent (0.9–1), good (0.8–0.89), fair (0.7–0.79), poor (0.6–0.69), or fail/no discriminatory capacity (0.5–0.59) (15). Statistical significance was accepted for two-sided p-values < 0.05. The statistical analyses were performed using SPSS version 22.0.
Results
Baseline characteristics
In this study, 1,530 (22.8%) women and 5,170 (77.2%) men were included (Table 1). A total of 759 (11.3%) patients experienced a recurrent MI. Age at entry ranged from 21 to 94 years (mean age 60 years). Patients with recurrent MI were older and had higher CHA2DS2-VASc and MCHA2DS2-VASc scores than those without such disorders. In the two groups, most recurrent patients were male (81.6 vs. 76.6%). Compared with the patients without recurrence, recurrent patients were more likely to have the comorbidities of hypertension, DM, HF, thromboembolism, dyslipidemia, and AF. Most recurrent patients were ≥65 years of age, whereas those aged ≤ 64 years were responsible for the majority of patients without recurrence.
TABLE 1
| Total (n = 6,700) | Recurrence | P-value | ||
| No (n = 5,941) | Yes (n = 759) | |||
| Age at baseline, mean (SD), years | 60.0 (11.1) | 59.7 (11.0) | 62.9 (11.8) | < 0.001 |
| Components of the CHA2DS2-VASc score, n (%) | ||||
| Age group, years | < 0.001 | |||
| ≤64 | 4216 (62.9) | 3824 (64.4) | 392 (51.6) | |
| 65–74 | 1811 (27.0) | 1576 (26.5) | 235 (31.0) | |
| ≥75 | 673 (10.0) | 541 (9.1) | 132 (17.4) | |
| Female | 1530 (22.8) | 1390 (23.4) | 140 (18.4) | 0.002 |
| Hypertension | 2964 (44.2) | 2442 (68.8) | 522 (41.1) | < 0.001 |
| Diabetes mellitus | 1904 (28.4) | 1596 (26.9) | 308 (40.6) | < 0.001 |
| Heart failure | 4060 (60.6) | 3397 (57.2) | 663 (87.4) | < 0.001 |
| NYHA class | < 0.001 | |||
| I | 1420 (21.2) | 1115 (18.8) | 305 (40.2) | |
| II | 1719 (25.7) | 1493 (25.1) | 226 (29.8) | |
| III | 640 (9.6) | 562 (9.5) | 78 (10.3) | |
| IV | 281 (4.2) | 227 (3.8) | 54 (7.1) | |
| Thromboembolism | 520 (7.8) | 400 (6.7) | 120 (15.8) | < 0.001 |
| Stroke/transient ischemic attack | 458 (6.8) | 349 (5.9) | 109 (14.4) | < 0.001 |
| Comorbidities, n (%) | ||||
| Dyslipidemia | 2845 (42.5) | 2489 (41.9) | 356 (46.9) | 0.009 |
| Atrial fibrillation | 341 (5.1) | 283 (4.8) | 58 (7.6) | 0.001 |
| CHA2DS2-VASc score, mean (SD) | 3.2 (1.6) | 3.1 (1.5) | 4.1 (1.7) | < 0.001 |
| MCHA2DS2-VASc score, mean (SD) | 6.9 (3.2) | 6.5 (3.1) | 9.4 (2.7) | < 0.001 |
Baseline characteristics of myocardial infarction patients with or without recurrence.
NYHA, New York Heart Association; SD, standard deviation.
Patient characteristics and recurrent myocardial infarction
The independent predictors of recurrence analyzed by logistic regression are reported in Tables 2, 3. After multivariable adjustment, older age, male sex, hypertension, DM, HF, thromboembolism, dyslipidemia, and CHA2DS2-VASc and MCHA2DS2-VASc scores were strongly independently associated with recurrent MI. Contrary to the male sex, the female sex as a stroke-related factor in AF was not considered to be an independent recurrent MI risk factor by multivariable analysis.
TABLE 2
| Coefficient | S.E. | Wald | OR | 95% CI | P-value | |
| Age | 0.011 | 0.004 | 7.343 | 1.011 | 1.003–1.018 | 0.007 |
| Male | 0.803 | 0.106 | 57.243 | 2.232 | 1.813–2.749 | < 0.001 |
| Hypertension | 1.173 | 0.091 | 167.915 | 3.231 | 2.706–3.859 | < 0.001 |
| Diabetes mellitus | 0.290 | 0.086 | 11.530 | 1.337 | 1.131–1.581 | 0.001 |
| Heart failure | 1.603 | 0.114 | 196.516 | 4.968 | 3.970–6.216 | < 0.001 |
| Thromboembolism | 0.589 | 0.121 | 23.639 | 1.802 | 1.421–2.285 | < 0.001 |
| Dyslipidemia | 0.243 | 0.083 | 8.699 | 1.276 | 1.085–1.500 | 0.003 |
Multivariate regression analysis investigating independent predictors of recurrent myocardial infarction.
The adjusted model was adjusted for age, sex, hypertension, diabetes mellitus, heart failure, thromboembolism, dyslipidemia, and atrial fibrillation.
CI, confidence interval; OR, odds ratio; SE, standard error.
TABLE 3
| Coefficient | S.E. | Wald | OR | 95% CI | P-value | |
| CHA2DS2-VASc score | ||||||
| Model 1 | 0.388 | 0.023 | 278.743 | 1.473 | 1.408–1.542 | <0.001 |
| Model 2 | 0.624 | 0.033 | 352.294 | 1.867 | 1.749–1.993 | <0.001 |
| Model 3 | 0.258 | 0.035 | 54.048 | 1.295 | 1.209–1.387 | <0.001 |
| MCHA2DS2-VASc score | ||||||
| Model 1 | 0.342 | 0.016 | 476.346 | 1.408 | 1.365–1.452 | <0.001 |
| Model 2 | 0.335 | 0.016 | 421.329 | 1.398 | 1.354–1.443 | <0.001 |
| Model 3 | 0.342 | 0.016 | 476.346 | 1.408 | 1.365–1.452 | <0.001 |
CHA2DS2-VASc and MCHA2DS2-VASc scores in predicting recurrence following myocardial infarction.
Model 1: unadjusted. Model 2: adjusted for age and sex. Model 3: adjusted for age, sex, hypertension, diabetes mellitus, heart failure, thromboembolism, dyslipidemia, and atrial fibrillation. CI, confidence interval; OR, odds ratio; SE, standard error.
Relationship between CHA2DS2-VASc, MCHA2DS2-VASc, and recurrent myocardial infarction
The frequency distribution of the CHA2DS2-VASc and MCHA2DS2-VASc scores, and the incidence of recurrent MI across the CHA2DS2-VASc and MCHA2DS2-VASc scores in the study cohort, stratified by sex, are shown in Figure 1. The overall incidence of recurrent MI increased from 2.0 to 33.3% when the CHA2DS2-VASc score increased from 1 to 9 (Figure 1A). In addition, patients confer an overall increased risk of recurrent MI from 1.4 to 61.5%, while the MCHA2DS2-VASc score increased from 0 to 15 (Figure 1B). The positive correlations between CHA2DS2-VASc and recurrence rate and MCHA2DS2-VASc and recurrence rate were observed, and the Spearman correlation coefficients were 0.198 (p < 0.001) and 0.283 (p < 0.001) separately. Further analyses revealed that the risk for recurrent MI incidence positively correlated with the CHA2DS2-VASc (Spearman correlation coefficient for men = 0.241 and women = 0.235) and MCHA2DS2-VASc (Spearman correlation coefficient for men = 0.294 and women = 0.237) among both women and men.
FIGURE 1
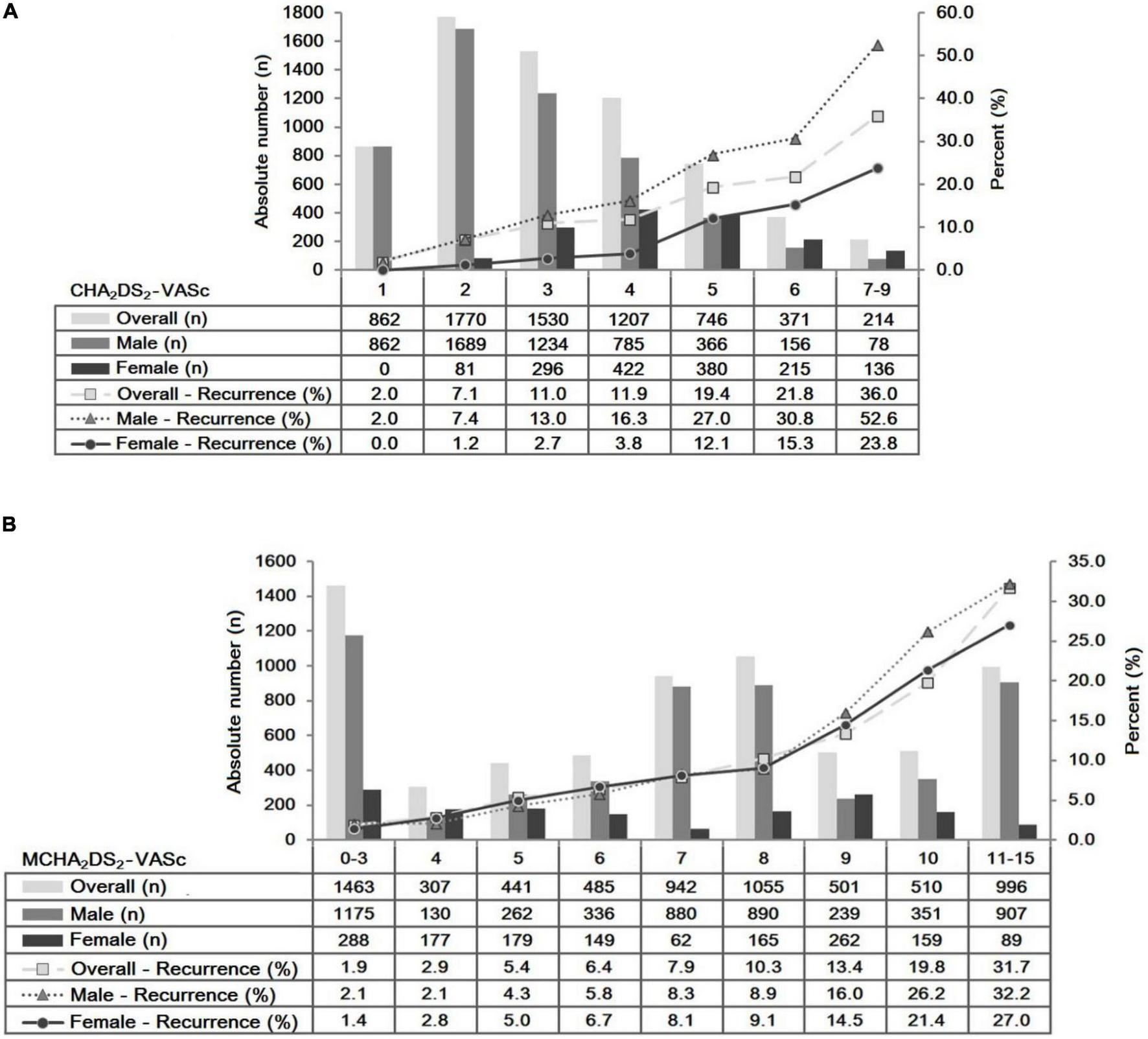
Frequency distribution and incidence of recurrent myocardial infarction for congestive heart failure, hypertension, age 65–74 years, diabetes mellitus, vascular disease, female sex, age ≥ 75 years, and prior stroke/transient ischemic attack/embolus [CHA2DS2-VASc (A)] and age ≥ 75 years, diabetes mellitus, dyslipidemia, prior stroke/transient ischemic attack/embolus, hypertension, male sex, and congestive heart failure [MCHA2DS2-VASc (B)] scores’ strata, presented overall, male sex, and female sex.
Receiver operating characteristic curves for CHA2DS2-VASc and MCHA2DS2-VASc in predicting recurrent myocardial infarction
The ROC curves of CHA2DS2-VASc and MCHA2DS2-VASc scores were analyzed (Figure 2 and Table 4). The predictive value of MCHA2DS2-VASc for recurrence was fair, being 0.757 (0.739–0.774) with a cutoff value of 8, but CHA2DS2-VASc had just a poor effect on prediction, with the AUC of 0.676 (0.657–0.696) and a cutoff value of 3 (Figure 2A). Thus, for the secondary prevention of MI, MCHA2DS2-VASc was recommended to take into consideration the recurrence risk assessment because it significantly improved the predictive value compared with the CHA2DS2-VASc (Z = 6.02, p < 0.001).
FIGURE 2
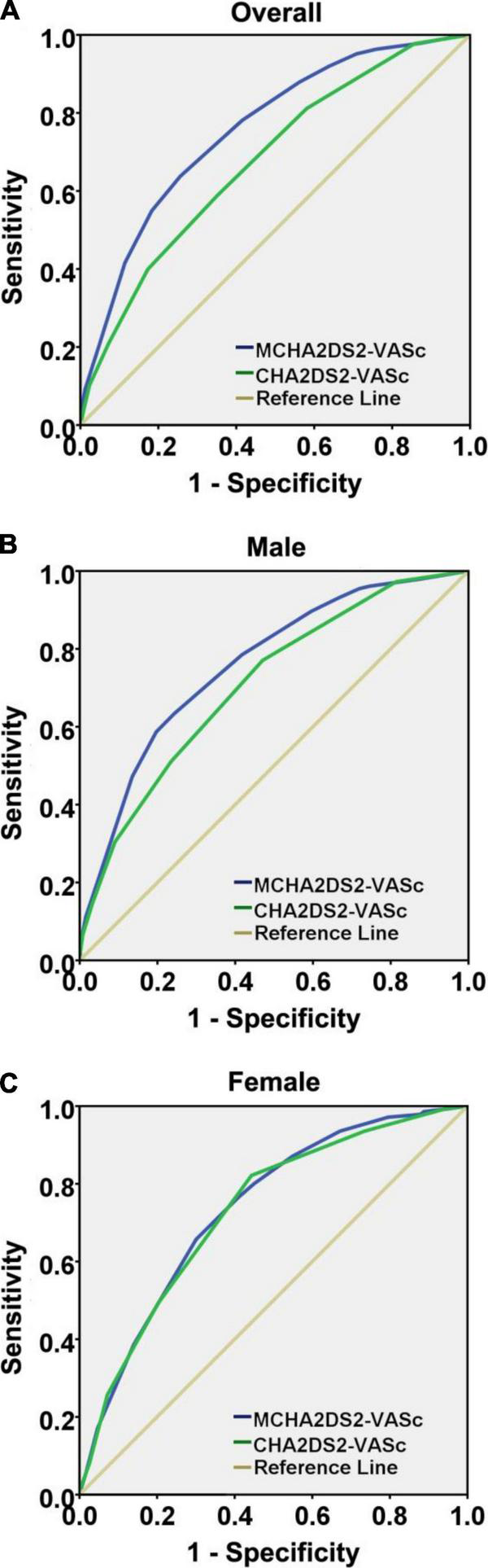
Receiver operating characteristic curve analysis comparing CHA2DS2-VASc and MCHA2DS2-VASc scores’ ability to predict recurrent myocardial infarction, presented overall (A), male sex (B), and female sex (C).
TABLE 4
| AUC | S.E. | P-value | 95% CI | Sensitivity (%) | Specificity (%) | Cut off point | |
| CHA2DS2-VASc | |||||||
| Overall | 0.676 | 0.010 | <0.001 | 0.657–0.696 | 58.9 | 64.8 | 3 |
| Male | 0.708 | 0.011 | <0.001 | 0.687–0.730 | 77.1 | 52.9 | 2 |
| Female | 0.730 | 0.021 | <0.001 | 0.688–0.771 | 82.1 | 55.7 | 4 |
| MCHA2DS2-VASc | |||||||
| Overall | 0.757 | 0.009 | <0.001 | 0.739–0.774 | 63.8 | 74.4 | 8 |
| Male | 0.759 | 0.010 | <0.001 | 0.739–0.779 | 63.3 | 75.7 | 8 |
| Female | 0.736 | 0.020 | <0.001 | 0.696–0.776 | 65.7 | 69.9 | 8 |
Predictive ability, sensitivity, and specificity of CHA2DS2-VASc and MCHA2DS2-VASc scores for recurrent myocardial infarction development, presented overall, and stratified by sex.
AUC, area under the ROC curve; CI, confidence interval; SE, standard error.
The AUCs of CHA2DS2-VASc and MCHA2DS2-VASc scores in predicting recurrent MI in male patients were 0.708 (0.687–0.730) and 0.759 (0.739–0.779), respectively. Both the two scores had a fair predictive value for recurrence, but the two predictors showed significant differences in risk assessment (Z = 3.43, p < 0.001) (Figure 2B). However, the superiority of the MCHA2DS2-VASc score among women yielded inconsistent findings. The AUCs of CHA2DS2-VASc and MCHA2DS2-VASc scores were 0.730 (0.688–0.771) and 0.736 (0.696–0.776), respectively. The predictive abilities of the two scores were both fair, and there was no significant difference between them (Z = 0.21, p = 0.836) (Figure 2C).
CHA2DS2-VASc, MCHA2DS2-VASc, and recurrent myocardial infarction risk stratification
Recurrent MI risk differentiation among patients presented overall and stratified by sex was classified as low risk and high risk, based on CHA2DS2-VASc and MCHA2DS2-VASc scores (Table 5). The overall patients classified as low-risk using CHA2DS2-VASc (score < 3) or MCHA2DS2-VASc (score < 8) had similarly low recurrence rates (5.4 vs. 4.6%). There was also no evidence of a statistical difference in the recurrence rates among those in women (MCHA2DS2-VASc < 8 vs. CHA2DS2-VASc < 4) identified as low risk. High-risk MCHA2DS2-VASc associated with a higher incidence of recurrent MI as compared with high-risk CHA2DS2-VASc was found in overall (19.4 vs. 15.1%), male (20.4 vs. 14.0%), and female (15.9 vs. 11.4%) patients.
TABLE 5
| Case (n) | Recurrence rate (%) | P-value | |
| Overall | |||
| Low-risk | 0.116 | ||
| CHA2DS2-VASc<3 | 2,632 | 143 (5.4) | |
| MCHA2DS2-VASc < 8 | 3,638 | 166 (4.6) | |
| High-risk | < 0.001 | ||
| CHA2DS2-VASc ≥ 3 | 4,068 | 616 (15.1) | |
| MCHA2DS2-VASc ≥ 8 | 3,062 | 593 (19.4) | |
| Male | |||
| Low-risk | < 0.001 | ||
| CHA2DS2-VASc < 2 | 862 | 17 (2.0) | |
| MCHA2DS2-VASc < 8 | 2,783 | 133 (4.8) | |
| High-risk | < 0.001 | ||
| CHA2DS2-VASc ≥ 2 | 4,308 | 602 (14.0) | |
| MCHA2DS2-VASc ≥ 8 | 2,387 | 486 (20.4) | |
| Female | |||
| Low-risk | 0.189 | ||
| CHA2DS2-VASc < 4 | 377 | 9 (2.4) | |
| MCHA2DS2-VASc < 8 | 855 | 33 (3.9) | |
| High-risk | 0.006 | ||
| CHA2DS2-VASc ≥ 4 | 1,153 | 131 (11.4) | |
| MCHA2DS2-VASc ≥ 8 | 675 | 107 (15.9) | |
Comparison of CHA2DS2-VASc and MCHA2DS2-VASc scores for incidence of recurrent myocardial infarction, presented overall, and stratified by sex.
Discussion
This study, based on a large cohort of patients with MI admitted with a duration longer than 28 days, has the following three main findings: (i) MCHA2DS2-VASc score is a fair predictor of recurrent MI, but only poor predictive accuracy of CHA2DS2-VASc score is available, (ii) MCHA2DS2-VASc score is significantly superior to CHA2DS2-VASc score in predicting male patients who develop recurrent MI, although the predictive value of the two scores is fair in both men and women, and (iii) MCHA2DS2-VASc score is better at identifying high-risk patients and is as good as CHA2DS2-VASc score in identifying patients at low-risk of recurrence among overall and female patients.
It has been reported that the CHA2DS2-VASc score is useful to predict many different diseases. In patients with CAD and sinus rhythm, CHA2DS2-VASc exhibited moderate accuracy in predicting the risk of stroke or TIA in the period following an episode of worsening HF and reduced ejection (15). In acute coronary syndrome patients treated with aspirin and clopidogrel following PCI, CHA2DS2-VASc (AUC = 0.59) was able to predict platelet reactivity (16). Gunduz et al. found the predictive value of CHA2DS2-VASc (AUC = 0.89) for mortality, intensive care unit (ICU) hospitalization, and length of stay in the ICU among COVID-19 patients (17). Similarly, another study also reported that CHA2DS2-VASc (AUC = 0.794) was significantly associated with all-cause mortality in COVID-19 patients (18).
A large number of people do not survive their first MI event, and if they do survive, their rate of adverse cardiovascular events, hospitalization, and mortality is greater than for the non-MI population. A risk stratification tool must be considered for each patient with MI in order to identify patients at high risk for disease progression. Notably, we found that many of the risk factors for incident MI recurrence were also risk factors for AF-related complications. Thus, we developed and tested the CHA2DS2-VASc score to predict the risk for recurrence after MI.
A total of 6,700 patients with MI were included in our analysis. Baseline characteristics showed significant differences between patients with or without recurrence, such as older age, female sex, hypertension, DM, HF, thromboembolism, dyslipidemia, and AF. Moreover, patients with recurrence had higher CHA2DS2-VASc scores. A positive linear relationship in both sexes of elevated CHA2DS2-VASc with recurrent events was found. After adjustment for baseline risk, higher CHA2DS2-VASc was independently associated with higher recurrent event rates. Every 1-SD increase in CHA2DS2-VASc was associated with a 29.5% increased risk. The AUC of CHA2DS2-VASc in predicting recurrence was 0.676 in overall, 0.708 in men, and 0.730 in women.
Despite being a predictor of recurrent MI, the CHA2DS2-VASc score has just poor accuracy. Thus, we analyzed risk factors for recurrence to improve model prediction. Our data indicated that older age, male sex, hypertension, DM, HF, thromboembolism, and dyslipidemia were independently significantly associated with a higher risk of recurrence. These risk factors were summarized in the clinical risk factor-based MCHA2DS2-VASc score. There was a positive linear relationship between MCHA2DS2-VASc and recurrence rate. Our observation of associations in both crude and comorbidity-adjusted analyses suggested that MCHA2DS2-VASc acted independently of other risk factors for recurrent events. Every 1-SD increase in MCHA2DS2-VASc was associated with a 40.8% increased risk. MCHA2DS2-VASc was able to predict recurrence with an AUC of 0.757. It was noteworthy that MCHA2DS2-VASc was possibly better than CHA2DS2-VASc in identifying patients with MI with a risk of recurrence.
Heart failure is a common complication in patients with AMI, ranging from 15 to 35% of cases. Patients with HF exist in a hypercoagulable state and are at increased risk for thromboembolic events, even when in sinus rhythm (19). The presence of symptoms of HF and/or left ventricular systolic dysfunction identifies a population of MI survivors at high risk for death, reinfarction, and worsening HF (20). Reduced left ventricular ejection fraction still remains the most powerful independent predictor of sudden arrhythmic death in patients with MI. Current direct evidence noted that prior MI in heart failure with preserved ejection fraction was associated with a 31-fold higher risk of cardiovascular death in the first 30 days and persistently elevated rates of HF hospitalization (21). In view of the above published clinical trials and our findings, it seems robust to give 5 points for HF as a component of the MCHA2DS2-VASc score.
Other risk factors involved in the MCHA2DS2-VASc score, such as older age, DM, and dyslipidemia, are established as risk factors for CHD reported in many studies. The number of aging patients with CHD is associated with increased morbidity and mortality but also medical treatment, stent placement, and coronary artery bypass graft (22). In the EMPA-REG OUTCOME trial, empagliflozin reduced the risk of MACEs in patients with DM and atherosclerotic cardiovascular disease (23). In addition to placing older adults at increased risk for CHD, dyslipidemia may cause a rapid aggravation of the long-term prognosis, such as frequent premature death, multiple ischemic recurrences, and multivessel disease, in younger adults who develop CHD early in life (24). Familial hypercholesterolemia also increased mortality and increased risk of recurrent AMI after the first AMI event (25). Thus, the US and European guidelines recommend for high-risk patients, such as those with a recent MI, to aggressively lower low-density lipoprotein cholesterol levels (26). From the above mentioned, therefore, we have every reason to believe that the same risk factors should be paid more attention to control in both primary and secondary prevention of CHD.
Patients with AF with a CHA2DS2-VASc score of 1 or more for men and 2 or more for women are likely to benefit from antithrombotic therapy. However, the female sex is an age-dependent stroke risk modifier rather than a risk factor per se (27). In our study, logistic regression analysis confirmed that the male sex was an independent risk factor for MI recurrence but not the female sex; therefore, 2 points were assigned to the male sex instead of the female sex in the MCHA2DS2-VASc score. One observational study indicates that rates of recurrent MI, recurrent CHD events, and mortality in the first year after MI were higher among men than women (28). However, another study found that women experienced a large excess risk of recurrence after MI, independently of clinical characteristics (29).
Possible reasons for sex differences in the predictive value of MCHA2DS2-VASc score for recurrent events include the complexities of the interactions of risk factors and the effects of certain risk factors stratified by sex are incompletely captured by available data. In addition, the number of male patients with MI in our study was significantly larger than that of women. In addition, low-risk factors often result in a low hospitalization rate. We confirmed that the value of MCHA2DS2-VASc would be more discriminatory for “truly low-risk” female patients with a rising population.
Limitations
Some limitations should be considered in our study. First, given the retrospective nature of our study, data are likely to have a certain extent of bias. Hospitalization for patients with MI with mild symptoms and few cardiovascular risk factors is much lower. Thus, the incidence of recurrent MI might be overestimated. Our analysis was conducted with the patients consecutively recruited from three large medical centers, which could partly reduce this selection bias. We also acknowledge that our data were based on electronic medical records from Hospital Information System that are not created for research purposes. However, since the system is routinely used in clinical practice, the data are sufficiently accurate, complete, and full for this study purpose. The degrees of underreporting and misdiagnosis rate for risk factors in hospital registers are often low, which leads to the data with high validity. In addition, the in-hospital duration and observation periods are not fully described, quantified, and compared. However, since the analysis was the occurrence of in-hospital AMI, which occurred less than 28 days, the results of our study were irrelevant to these missing data. Our retrospective results should be confirmed by prospective cohort studies. Second, recurrent MI risk is a continuum. The MCHA2DS2-VASc score has a fair predictive value of artificially categorizing patients with MI into low and high-risk strata, only with a greater focus on the identification of “high-risk” patients. To improve identifying “truly low-risk” patients, it is necessary to be more inclusive of common recurrence risk factors as part of the MCHA2DS2-VASc score. Third, our analyses were based on data from inpatients with MI, and the results may not be entirely generalizable to other settings where comorbidity is less prevalent. It seems to increase the relative risk estimates in the analysis of provoked MI recurrence. Similarly, since our study is limited to Chinese individuals, it may be difficult to extrapolate our findings to other populations. Fourth, given that the MCHA2DS2-VASc score should be applicable to most patients with MI for most of the time and situations in everyday clinical practice, our study did not cover treatment and laboratory data. Therefore, it is not possible to exclude the effects of the paucity of data on the risk of recurrence.
Conclusion
CHA2DS2-VASc and MCHA2DS2-VASc scores are both validated in recurrent MI prediction. However, MCHA2DS2-VASc has a better predictive value than CHA2DS2-VASc in overall and male patients with MI and, importantly, should be considered as being a similar predictive value to CHA2DS2-VASc in female patients. MCHA2DS2-VASc shifts toward a greater focus on the identification of high-risk patients with MI, and as good as CHA2DS2-VASc focus on identifying low-risk patients in women. The next step is to expand data collection for risk factors that are unique to and more common in women than men and to improve cardiovascular prevention models for women.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
XL conceived and designed the study and supervised all the work. HP collected the data, planned the analyses, and drafted the manuscript. XZ and IC performed all calculations and interpreted the data. HZ and YZ designed the case report forms. SL supervised the statistical analyses. All authors contributed intellectually to the manuscript, reviewed drafts, and accepted the final draft.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81730106 to XL), the National High Technology Research and Development Program of China (2017YFC1700505 to XL), the Natural Science Foundation of Jiangsu Province (BK20190158 to HP), the Xuzhou Municipal Bureau of Science and Technology (KC19026 to HP), and the Six Talent Peaks Project in Jiangsu Province (WSN270 to HP).
Acknowledgments
We thank Zhenkun Zong (Affiliated Hospital of Xuzhou Medical University, Xuzhou, Jiangsu, China) for the technical assistance on partial data collection and database management.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
JoshiPHde LemosJA. Diagnosis and management of stable angina: a review.JAMA. (2021) 325:1765–78. 10.1001/jama.2021.1527
2.
Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology.2019 Chinese Society of Cardiology (CSC) guidelines for the diagnosis and management of patients with ST – segment elevation myocardial infarction.Chin J Cardiol. (2019) 47:766–83. 10.3760/cma.j.issn.0253-3758.2019.10.003
3.
WaksJWBuxtonAE. Risk stratification for sudden cardiac death after myocardial infarction.Annu Rev Med. (2018) 69:147–64. 10.1146/annurev-med-041316-090046
4.
GrinbergTBentalTHammerYAssaliAVaknin-AssaHKornowskiRet alTemporal trends of the management and outcome of patients with myocardial infarction according to the risk for recurrent cardiovascular events.Am J Med. (2020) 133:839.e–47.e. 10.1016/j.amjmed.2019.12.027
5.
HindricksGPotparaTDagresNArbeloEBaxJJBlomström-LundqvistCet al2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC.Eur Heart J. (2021) 42:373–498. 10.1093/eurheartj/ehaa612
6.
GoudisCDaiosSKorantzopoulosPLiuT. Should we incorporate obstructive sleep apnea in CHA2DS2-VASc score?Sleep Breath. (2021) 25:2099–101. 10.1007/s11325-021-02305-3
7.
ZhangYYuanYQ. Value of left atrial diameter with CHA2DS2-VASc score in predicting left atrial/left atrial appendage thrombosis in non-valvular atrial fibrillation.Arq Bras Cardiol. (2021) 116:325–31. 10.36660/abc.20190492
8.
PremužićVStevanovićRRadićPSalvettiMLovrić-BenčićMJelakovićAet alChronic kidney disease and cardiovascular mortality in patients with atrial fibrillation: European Society of Hypertension project – ESH A Fib.Medicine. (2021) 100:e23975. 10.1097/MD.0000000000023975
9.
FuYLiKGaoYWangLChenMYangX. A novel risk score for predicting left atrial and left atrial appendage thrombogenic milieu in patients with non-valvular atrial fibrillation.Thromb Res. (2020) 192:161–6. 10.1016/j.thromres.2020.05.010
10.
ZhangFYangXCJiaXWTangXHWangZWangZQ. Von Willebrand factor and ADAMTS13 plasma in older patients with high CHA2DS2-VASc score with and without atrial fibrillation.Eur Rev Med Pharmacol Sci. (2017) 21:4907–12.
11.
LeonardiSBuenoHAhrensIHassagerCBonnefoyELettinoM. Optimised care of elderly patients with acute coronary syndrome.Eur Heart J Acute Cardiovasc Care. (2018) 7:287–95. 10.1177/2048872618761621
12.
ShoreSJonesPGMaddoxTMBradleySMStolkerJMArnoldSVet alLongitudinal persistence with secondary prevention therapies relative to patient risk after myocardial infarction.Heart. (2015) 101:800–7. 10.1136/heartjnl-2014-306754
13.
SilvainJKerneisMZeitouniMLattucaBGalierSBrugierDet alInterleukin-1beta and risk of premature death in patients with myocardial infarction.J Am Coll Cardiol. (2020) 76:1763–73. 10.1016/j.jacc.2020.08.026
14.
ThygesenKAlpertJSJaffeASChaitmanBRBaxJJMorrowDAet alFourth universal definition of myocardial infarction (2018).J Am Coll Cardiol. (2018) 72:2231–64. 10.1016/j.jacc.2018.08.1038
15.
MehraMRVaduganathanMFuMFerreiraJPAnkerSDClelandJGFet alA comprehensive analysis of the effects of rivaroxaban on stroke or transient ischaemic attack in patients with heart failure, coronary artery disease, and sinus rhythm: the COMMANDER HF trial.Eur Heart J. (2019) 40:3593–602. 10.1093/eurheartj/ehz427
16.
AsherEAbu-MuchABragazziNLYounisAYounisAMasalhaEet alCHADS2 and CHA2DS2-VASc scores as predictors of platelet reactivity in acute coronary syndrome.J Cardiol. (2021) 77:375–9. 10.1016/j.jjcc.2020.09.010
17.
GunduzRYildizBSOzdemirIHCetinNOzenMBBakirEOet alCHA2DS2-VASc score and modified CHA2DS2-VASc score can predict mortality and intensive care unit hospitalization in COVID-19 patients.J Thromb Thrombolysis. (2021) 52:914–24. 10.1007/s11239-021-02427-1
18.
Caro-CodónJLipGYHReyJRIniestaAMRosilloSOCastrejon-CastrejonSet alPrediction of thromboembolic events and mortality by the CHADS2 and the CHA2DS2-VASc in COVID-19.Europace. (2021) 23:937–47. 10.1093/europace/euab015
19.
LinAYDinatoloEMetraMSbolliMDasseniNButlerJet alThromboembolism in heart failure patients in sinus rhythm: epidemiology, pathophysiology, clinical trials, and future direction.JACC Heart Fail. (2021) 9:243–53. 10.1016/j.jchf.2021.01.009
20.
De LucaL. Established and emerging pharmacological therapies for post-myocardial infarction patients with heart failure: a review of the evidence.Cardiovasc Drugs Ther. (2020) 34:723–35. 10.1007/s10557-020-07027-4
21.
CunninghamJWVaduganathanMClaggettBLJohnJEDesaiASLewisEFet alMyocardial infarction in heart failure with preserved ejection fraction: pooled analysis of 3 clinical trials.JACC Heart Fail. (2020) 8:618–26. 10.1016/j.jchf.2020.02.007
22.
SmitMCoetzeeARLochnerA. The pathophysiology of myocardial ischemia and perioperative myocardial infarction.J Cardiothorac Vasc Anesth. (2020) 34:2501–12. 10.1053/j.jvca.2019.10.005
23.
McGuireDKZinmanBInzucchiSEWannerCFitchettDAnkerSDet alEffects of empagliflozin on first and recurrent clinical events in patients with type 2 diabetes and atherosclerotic cardiovascular disease: a secondary analysis of the EMPA-REG OUTCOME trial.Lancet Diabetes Endocrinol. (2020) 8:949–59. 10.1016/S2213-8587(20)30344-2
24.
ZeitouniMNannaMGSunJLChiswellKPetersonEDNavarAM. Performance of guideline recommendations for prevention of myocardial infarction in young adults.J Am Coll Cardiol. (2020) 76:653–64. 10.1016/j.jacc.2020.06.030
25.
SvendsenKKroghHWIglandJTellGSMundalLJHolvenKBet al2.5-fold increased risk of recurrent acute myocardial infarction with familial hypercholesterolemia.Atherosclerosis. (2021) 319:28–34. 10.1016/j.atherosclerosis.2020.12.019
26.
GencerBMachFMurphySADe FerrariGMHuberKLewisBSet alEfficacy of evolocumab on cardiovascular outcomes in patients with recent myocardial infarction: a prespecified secondary analysis from the FOURIER trial.JAMA Cardiol. (2020) 5:952–7. 10.1001/jamacardio.2020.0882
27.
WuVCWuMAboyansVChangSHChenSWChenMCet alFemale sex as a risk factor for ischaemic stroke varies with age in patients with atrial fibrillation.Heart. (2020) 106:534–40. 10.1136/heartjnl-2019-315065
28.
PetersSAEColantonioLDDaiYZhaoHBittnerVFarkouhMEet alTrends in recurrent coronary heart disease after myocardial infarction among US women and men between 2008 and 2017.Circulation. (2021) 143:650–60. 10.1161/CIRCULATIONAHA.120.047065
29.
AslehRManemannSMWestonSABielinskiSJChamberlainAMJiangRet alSex differences in outcomes after myocardial infarction in the community.Am J Med. (2021) 134:114–21. 10.1016/j.amjmed.2020.05.040
Summary
Keywords
CHA2DS2-VASc, myocardial infarction, recurrence, sex differences, risk stratification
Citation
Pang H, Zhu X, Cheang I, Zhang H, Zhou Y, Liao S and Li X (2022) CHA2DS2-VASc score for in-hospital recurrence risk stratification in patients with myocardial infarction. Front. Cardiovasc. Med. 9:925932. doi: 10.3389/fcvm.2022.925932
Received
22 April 2022
Accepted
07 November 2022
Published
01 December 2022
Volume
9 - 2022
Edited by
Hamidreza Goodarzynejad, University Health Network, Canada
Reviewed by
Marco Matteo Ciccone, University of Bari Aldo Moro, Italy; Deyong Long, Beijing Anzhen Hospital, Capital Medical University, China
Updates
Copyright
© 2022 Pang, Zhu, Cheang, Zhang, Zhou, Liao and Li.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shengen Liao, shengenliao@163.comXinli Li, xinli3267@njmu.edu.cn
†These authors have contributed equally to this work
This article was submitted to Sex and Gender in Cardiovascular Medicine, a section of the journal Frontiers in Cardiovascular Medicine
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.