- 1The Second School of Clinical Medicine, Southern Medical University, Guangzhou, China
- 2Department of Pediatric Cardiac Surgery, The Seventh Medical Center of the PLA General Hospital, Beijing, China
- 3Department of Radiology, The Seventh Medical Center of the PLA General Hospital, Beijing, China
Right aortic arch with isolation of left brachiocephalic artery is a rare congenital aortic arch anomaly. Herein, we reported a case of this rare anomaly with ventricular septal defect in a 9-month-old infant. We successfully reconstructed the islolated left brachiocephalic artery and repaired the ventricular septal defect in one stage.
Introduction
Right aortic arch (RAA) with isolation of the left brachiocephalic artery (ILBA) is a very rare congenital anomaly. This anomaly is defined as the left brachiocephalic artery (LBA) loses its attachment to the aorta and is connected with the pulmonary artery(PA) via a ductus arteriosus(DA) (1–3). Reconstructing continuity between the LBA and the aortic arch can be difficult when the two vessels are far apart. In this report, we used a pedicle flap of ascending aorta as the posterior wall and a bovine pericardial patch as the anterior wall to establish the continuity between the LBA and the arotic arch.
Case report
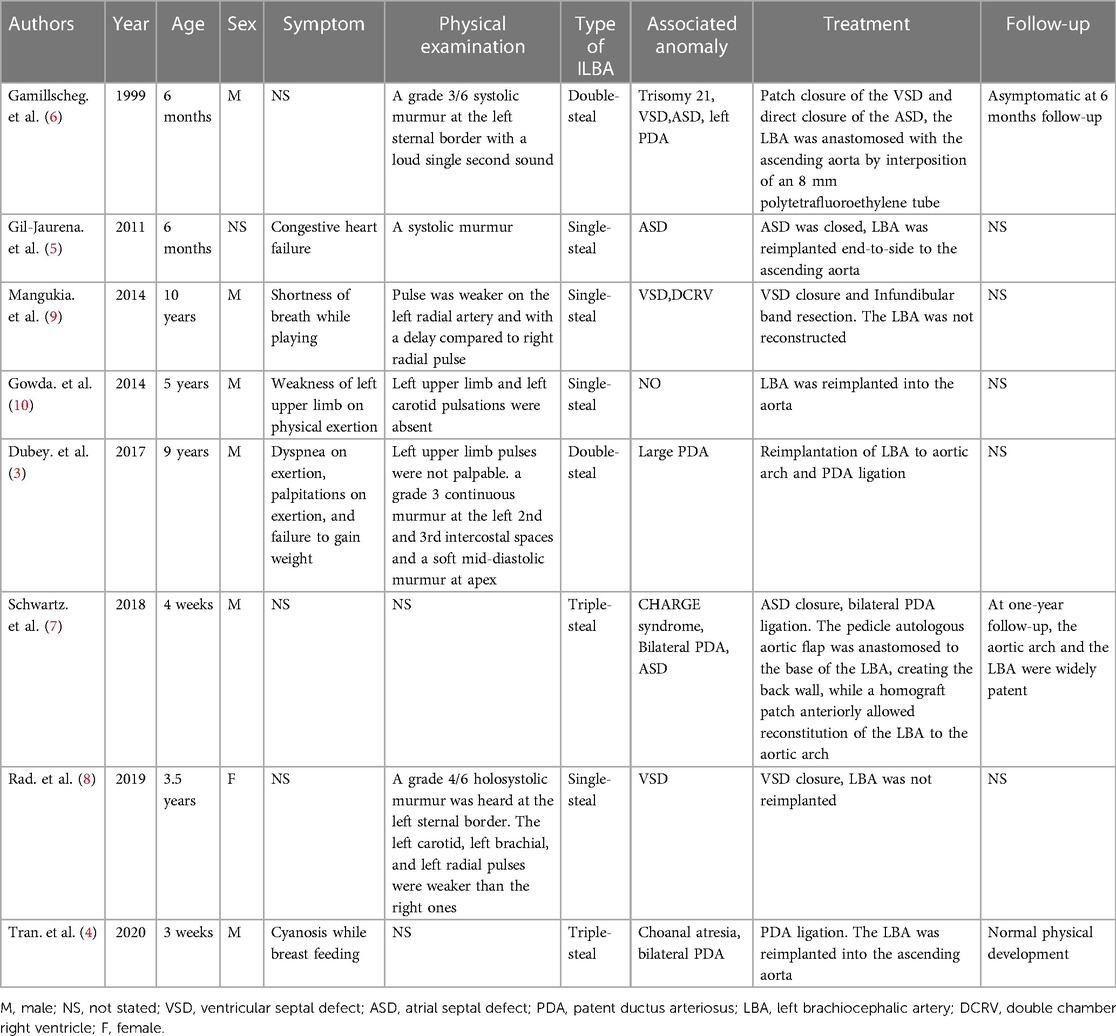
A 9-month-old male infant was referred to our hospital due to recurrent respiratory tract infection. The patient was 7.5 kilogram and had normal growth and development. Clinical examination findings included a precordial grade 3/6 systolic murmur, left radial artery and left carotid artery pulses were not palpable. Both upper limbs were the same size. Echocardiography showed a 6 mm perimembranous ventricular septal defect (VSD) and the right aortic arch, with no LBA arising from the aortic arch. The computed tomographic angiography showed the right aortic arch and its only two branches, the right common carotid artery and the right subclavian artery. To identify the branch of the aortic arch, we performed cardiac catheterization for the patient. The aortic angiogram demonstrated a right aortic arch with only two arch branches. The first branch was the right common carotid artery followed by the right subclavian artery. The LBA have no connection with the aortic arch and was delayed filled by retrograde flow from the cerebral circulation (Figure 1). Considering the long-term development of the cerebral and the left upper extremity, we decided to perform VSD repair and reconstruct the LBA in one stage.
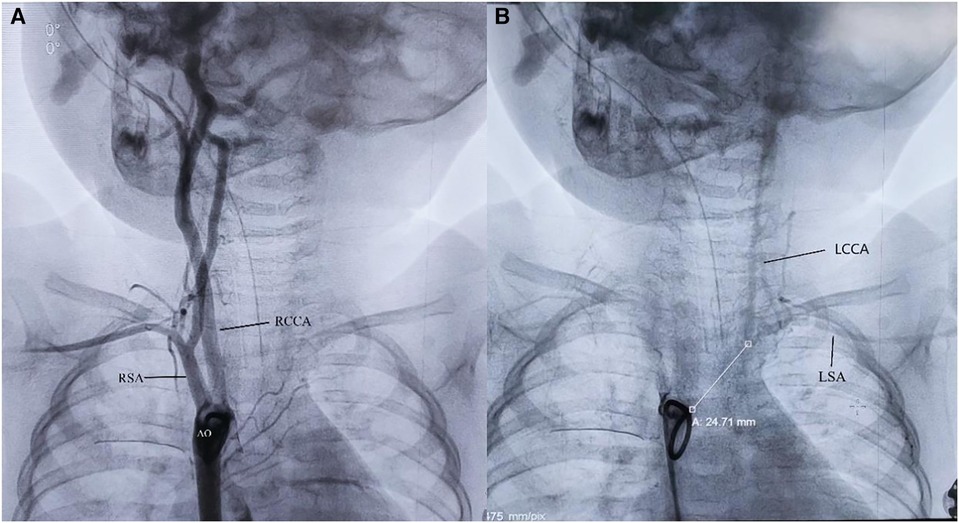
Figure 1. (A) The aortic angiogram demonstrated a right aortic arch with only two arch branches. (B) The LBA have no connection with the aortic arch and was delayed filled by retrograde flow from the cerebral circulation. AO, aorta; RCCA, right common carotid artery; RSA, right subclavian artery; LCCA, left common carotid artery; LSA, left subclavian artery; white line: The distance between the LBA and AO is 24.71 millimeters.
A median sternotomy was performed. During the operation, we found that the LBA was connected to the main pulmonary artery via the left ligamentum arteriosum (Figure 2). The LBA and its branches, as well as the ascending aorta were extensively mobilized. Cardiopulmonary bypass was established by bicaval cannulation and aortic cannulation. The aortic cannula was placed near the right common carotid artery origin. The VSD was repaired with a bovine pericardial patch via a right atriotomy. The left ligamentum arteriosum was divided. After the residual ductal tissues on the side of the LBA were removed, there was a significant distance between the isolated LBA and the aortic arch. A pedicle flap was created in the anteriolateral wall of the ascending aorta. The aortic flap was turned upward and anastomosed with the posterior wall of the LBA, and a bovine pericardial patch was used as the anterior wall to connect the aortic arch with the LBA (Figures 2, 3). Postoperatively, the patient had good left radial artery pulse, and computed tomographic angiography showed that the reconstructed LBA was patent (Figure 4). During the 6 months follow-up, the patient was asymptomatic and had normal development.
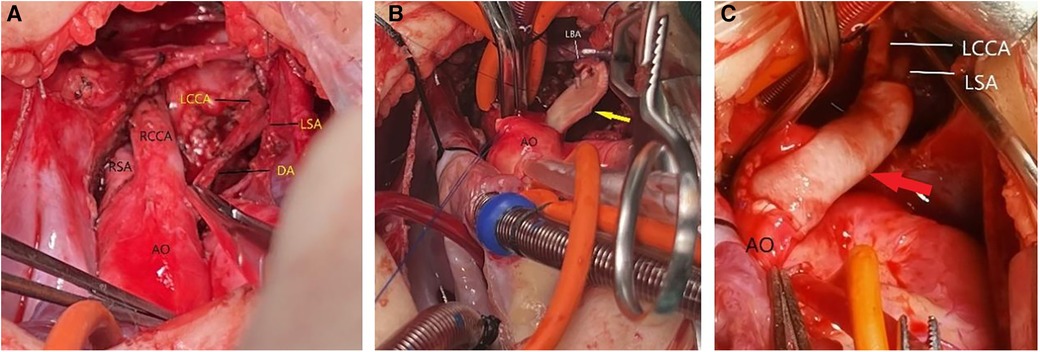
Figure 2. (A) The LBA was connected to the main pulmonary artery via the left ligamentum arteriosum. (B) A pedicle flap was created in the anteriolateral wall of the ascending aorta. The aortic flap was turned upward and anastomosed with the posterior wall of the LBA. (C) A bovine pericardial patch was used as the anterior wall to connect the aortic arch with the LBA. AO, aorta; RCCA, right common carotid artery; RSA, right subclavian artery; LCCA, left common carotid artery; LSA, left subclavian artery; DA, ductus arteriosus; LBA, left brachiocephalic artery. yellow arrow: a pedicle flap of the ascending aorta. red arrow: a bovine pericardial patch.
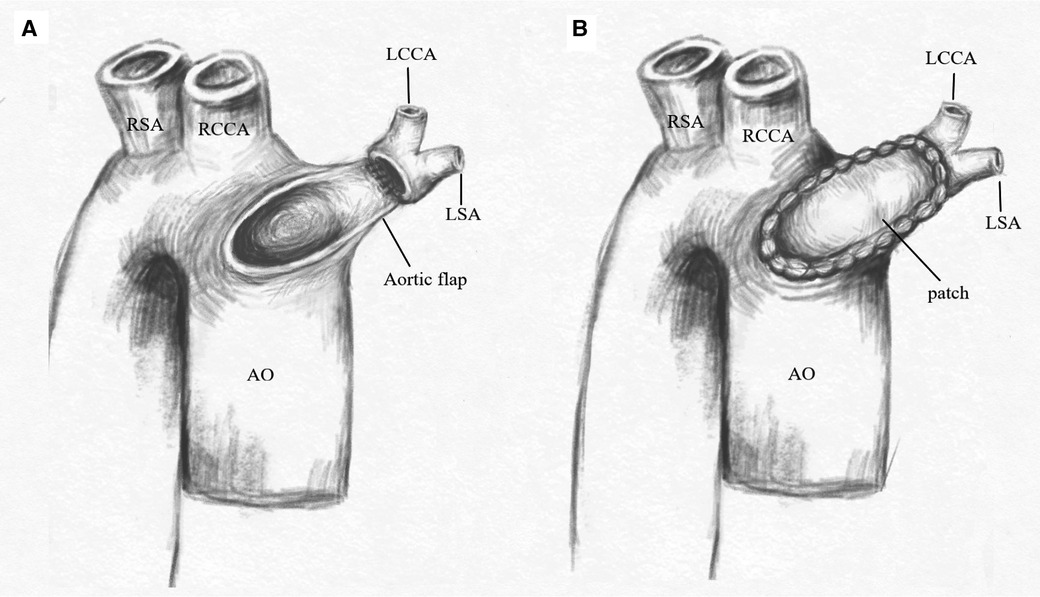
Figure 3. (A) A pedicle flap was created in the anteriolateral wall of the ascending aorta. The aortic flap was turned upward and anastomosed with the posterior wall of the LBA. (B) A bovine pericardial patch was used as the anterior wall to connect the aortic arch with the LBA. AO, aorta; RCCA, right common carotid artery; RSA, right subclavian artery; LCCA, left common carotid artery; LSA, left subclavian artery.
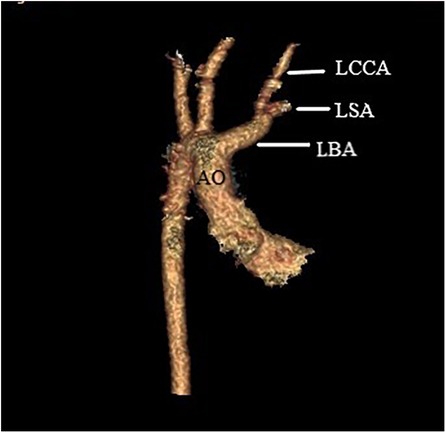
Figure 4. Postoperative computed tomographic angiography showed that the reconstructed LBA was patent. AO, aorta; LCCA, left common carotid artery; LSA, left subclavian artery; LBA, left brachiocephalic artery.
Discussion
Right aortic arch (RAA) with ILBA is a rare anatomic variation of aortic arch anomaly, in which the LBA loses its attachment to the aorta and abnormally connect with the PA via a ductus arteriosus. To date, most reports of this anomaly were case reports, and most cases were associated with intracardiac malformations (3–9) (Table 1). The clinical presentation, management, and prognosis of the patients with ILBA depend on anatomical characteristics and whether it is associated with other malformations. Rad (8) and colleagues proposed a novel anatomic-clinical-prognostic classification of ILBA, classifying it into three types: single-steal type with single source of steal from LBA through the left subclavian artery and with no connection to PA, double-steal type with double sources of steal from LBA through left subclavian artery and patent ductus arteriosus (PDA), triple-steal type with triple sources of steal from LBA through left subclavian artery and bilateral PDAs. According to the above classification, our case belonged to the single-steal type. In our case, the absence of pulse in the left radial artery and left carotid artery, with the presence of a right aortic arch with two arch branches led us to suspect this anomaly, and aorta angiography confirmed the diagnosis.
The ILBA could induce subclavian artery steal phenomenon, which decrease perfusion of the cerebral and left upper extremity and affects the development of these organs. If combined with PDA, it can also lead to pulmonary artery steal and cause congestive heart failure. Therefore, we suggested that the continuity between the LBA and the aorta should be reconstructed for this anomaly, which is very important to preserve normal perfusion of the cerebral and left upper extremity and maintain organs development. Various surgical techniques for reconstructed the continuity between the LBA and the aorta had been reported in previous literature, such as direct anastomosis of IBA and aorta (4, 5, 10), using a synthetic tube to connect the LBA and the aorta (6). In our patient, there was a significant distance between the isolated LBA and the aortic arch, two vessles were unable to be anastomosed directly. However, we also did not consider using synthetic tube because it has no growth potential and could stenosis in the long term. Schwartz (7) and colleagues described a case of this anomaly using an autologous pedicle flap of ascending aorta as well as a homograft patch as the roof to recreate continuity between the aorta and left innominate artery. We drawed on this technique to reconstructed the continuity between the LBA and the aorta, and achieved satisfactory outcome. The long-term patency of the LBA needed further follow-up.
Conclusion
Right aortic arch with isolation of left brachiocephalic artery is a rare congenital aortic arch anomaly. Absent or weak pulse of the left radial artery combined with right aortic arch and two arch branches is the clue to the diagnosis of the ILBA. Reconstructing the continuity between the LBA and the aorta is beneficial to the development of children. The technique we described in this report provides a surgical strategy for patients with two vessels far apart.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board of The Seventh Medical Center of the PLA General Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
GW: Conceptualization, Writing – original draft, Writing – review & editing. JW: Writing – review & editing. HZ: Investigation, Writing – review & editing. HW: Investigation, Writing – review & editing. QM: Data curation, Writing – review & editing. LS: Investigation, Writing – review & editing. GZ: Funding acquisition, Resources, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was supported by the Military Family Planning Special Research Project (20JSZ15).
Acknowledgment
The authors appreciate the excellent illustration work by JW.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1381222/full#supplementary-material
References
1. Levine S, Serfas LS, Rusinko A. Right aortic arch with subclavian steal syndrome (atresia of left common carotid and left subclavian arteries). Am J Surg. (1966) 111:632–7. doi: 10.1016/0002-9610(66)90030-4
2. Crump WD, Dische MR, Anthony CL. Right aortic arch, isolated left common carotid and left subclavian arteries, and subclavian steal syndrome: a variant of polysplenia syndrome. Hum Pathol. (1981) 12:936–8. doi: 10.1016/S0046-8177(81)80200-6
3. Dubey G, Gupta SK, Kothari SS. Isolated left brachiocephalic artery with the right aortic arch: a rare differential of large patent ductus arteriosus. Ann Pediatr Cardiol. (2017) 10:78–81. doi: 10.4103/0974-2069.197067
4. Tran VQ, Nguyen TLT, Nguyen MT, Luong CM, Dinh DM, Vuong AD. A case of right ductus and left innominate artery from the pulmonary trunk. Asian Cardiovasc Thorac Ann. (2020) 28(1):45–7. doi: 10.1177/0218492319865425
5. Gil-Jaurena JM, Ferreiros M, Zabala I, Cuenca V. Right aortic arch with isolation of the left innominate artery arising from the pulmonary artery and atrial septal defect. Ann Thorac Surg. (2011) 91:303. doi: 10.1016/j.athoracsur.2010.06.015
6. Gamillscheg A, Stein JI, Beitzke A. Ventricular and atrial septal defects, and right aortic arch associated with isolation of the left innominate artery from the aorta. Heart. (2000) 83:99–100. doi: 10.1136/heart.83.1.99
7. Schwartz MC, Pourmoghadam K, O’Brien M, Fleishman CE, DeCampli W. Surgical palliation of right aortic arch with an isolated innominate artery from the left ductcs arteriosus. World J Pediatr Congenital Heart Surg. (2018) 9(1):98–100. doi: 10.1177/2150135117737688
8. Rad EM, Pouraliakbar HR. Isolation of left brachiocephalic artery revisited: a 52-year literature review and introduction of a novel anatomic-clinical-prognostic classification. Ann Pediatr Cardiol. (2019) 12:117–29. doi: 10.4103/apc.APC_74_18
9. Mangukia C, Sethi S, Agarwal S, Mishra S, Satsangi DK. Right aortic arch with isolation of the left innominate artery in a case of double chamber right ventricle and ventricular septal defect. Ann Pediatr Cardiol. (2014) 7:148–51. doi: 10.4103/0974-2069.132500
Keywords: isolation of left brachiocephalic artery, right aortic arch, aortic arch anomaly, congenital heart defect, subclavian steal syndrome
Citation: Wang G, Wang J, Zhang H, Wang H, Meng Q, Song L and Zhou G (2024) Case Report: Right aortic arch with isolation of left brachiocephalic artery and ventricular septal defect. Front. Cardiovasc. Med. 11:1381222. doi: 10.3389/fcvm.2024.1381222
Received: 5 February 2024; Accepted: 5 April 2024;
Published: 22 April 2024.
Edited by:
Jaspal Dua, Liverpool Heart and Chest Hospital NHS Trust, United KingdomReviewed by:
Maruti Haranal, U N Mehta Institute of Cardiology and Research, India Omar R. J. Tamimi, King Fahd Medical City, Saudi Arabia© 2024 Wang, Wang, Zhang, Wang, Meng, Song and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gengxu Zhou emhvdWd4ODQwMEAxMjYuY29t
 Gang Wang
Gang Wang Jieqiong Wang2
Jieqiong Wang2