- 1Department of Internal Medicine, East Carolina University, Greenville, NC, United States
- 2Department of Internal Medicine, United Health Services Hospital, Johnson City, NY, United States
- 3Department of Internal Medicine, T.J. Samson Community Hospital, Glasgow, KY, United States
- 4Department of Cardiology, Hamad Medical Corporation, Doha, Qatar
- 5Department of Medicine, Kingston Public Hospital, Kingston, Jamaica
- 6Libyan Biotechnology Research Center, Tripoli, Libya
- 7Department of Internal Medicine, St Luke’s Hospital, Cedar Rapids, IA, United States
- 8Department of Medicine, Bukovinian State Medical University, Chernivtsi, Ukraine
- 9Department of Medicine, University of Zenica Faculty of Medicine, Zenica, Bosnia and Herzegovina
- 10Department of Medicine, Government Medical College and Hospital, Jammu, India
- 11Department of Medicine, Rawalpindi Medical University, Rawalpindi, Pakistan
- 12Department of Cardiology, King Edward Medical University, Lahore, Pakistan
- 13Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, United States
- 14National Heart & Lung Institute, Imperial College London, London, United Kingdom
- 15Department of Cardiology, Royal Brompton Hospital, London, United Kingdom
- 16Department of Cardiovascular Disease, University of Alabama at Birmingham, Birmingham, AL, United States
- 17Department of Cardiology, Mercy One Siouxland Heart and Vascular Center, Sioux City, IA, United States
- 18UHS Heart & Vascular Institute, United Health Services Hospital, Johnson City, NY, United States
Background: It is uncertain whether a liberal red blood cell (RBC) transfusion strategy is superior to a restrictive approach in patients with acute coronary syndrome (ACS) and anemia.
Methods: We searched MEDLINE, Embase, the Cochrane Library, and ClinicalTrials.gov from inception to April 2024 for randomized controlled trials (RCTs) comparing liberal and restrictive transfusion strategies in ACS patients with concurrent anemia.
Results: Five RCTs (4,510 patients) were included in this meta-analysis. There was no significant difference between the liberal and restrictive RBC transfusion strategy groups in the risk of major adverse cardiovascular events (MACE) (RR 0.91, 95% CI: 0.68–1.21; I2 = 63%) and all-cause mortality (RR 0.85, 95% CI: 0.72, 1.00; I2 = 0%). A liberal transfusion strategy reduced the risk of myocardial infarction (MI) (RR 0.80, 95% CI: 0.66, 0.98; I2 = 0%). There were no significant differences between the two strategies in the risk of revascularization, heart failure, stroke, cardiac mortality, acute kidney injury or failure, and pneumonia, bacteremia, or infection. Liberal transfusion increased the risk of acute lung injury (RR 8.97, 95% CI: 1.65, 48.65; I2 = 0%).
Conclusions: Our meta-analysis demonstrated that a liberal RBC transfusion strategy reduced the risk of MI and increased the risk of acute lung injury but did not affect other clinical outcomes compared to a restrictive approach in patients with mainly acute MI and anemia. New large-scale multicenter RCTs are required to confirm or refute our findings and provide more reliable results.
Systematic Review Registration: PROSPERO (CRD42024506844).
Introduction
The prevalence of anemia in patients with acute coronary syndromes (ACS) is reported to be 28% and is independently associated with a 50% increased risk of mortality in both men and women (1). Patients with ACS and anemia are older than those without anemia, have a higher prevalence of comorbidities, and are less likely to receive reperfusion therapy with either thrombolysis or primary percutaneous intervention (2).
In particular, anemia is an overlooked comorbidity in patients undergoing acute myocardial infarction (AMI), with 15%–43% having concomitant anemia in varying stages (3). Fundamentally, anemia results in diminished carrying capacity of oxygen in the blood, further compounding a preexisting supply/demand mismatch in cardiac tissue due to decreased coronary perfusion. Anemia has also been implicated in blunting the cytokine-mediated immune response generated by AMI, thereby limiting vascular healing capacity and thus worsening prognosis beyond the acute phase (4). Standardized treatment for AMI, such as heparin in the immediate period and antiplatelet agents that may be continued long-term, often potentiate the severity of anemia. Consequently, anemia has been associated with increased mortality in patients with AMI (3).
Augmenting the supply of oxygen delivered to infarcted tissue is the principle behind blood transfusion as therapy in individuals with ACS and anemia. However, transfusions are not necessarily benign interventions. Transfusion reactions, circulatory overload, acute lung injury, and infections, among others, are well-documented side effects of blood transfusions (5). Achieving the optimal balance between providing adequate oxygenation to compromised tissue and limiting the costs of transfusions has been a longstanding subject of debate.
There have been multiple attempts to compare outcomes between restrictive transfusion and liberal approaches. Historically, a liberal approach [hemoglobin (Hb) goal >10 g/dl] was favored. However, in 2014, the American Heart Association (AHA) and the American College of Cardiology (ACC) adopted guidelines against transfusing patients beyond Hb >8 g/dl in hemodynamically stable patients with AMI (6). Soon afterward, the American Association of Blood Banks (AABB) weighed in, citing no recommendation for or against a restrictive approach (7, 8). As per the 2023 European Society of Cardiology (ESC) guidelines for the management of ACS, no recommendation as to the optimal transfusion strategy can be made at present (9).
A previous meta-analysis by Abdelazeem et al. on transfusion strategies in patients with ACS and anemia, which included 821 patients, showed that a restrictive blood transfusion strategy was not associated with reduced all-cause mortality, recurrent MI, and heart failure exacerbation compared to a liberal strategy (10). The largest randomized controlled trial (RCT) on this topic to date has recently been published, including 3,500 adult patients (11). Therefore, we conducted this meta-analysis to integrate data from newer studies and compare the restrictive vs. liberal red blood cell (RBC) transfusion strategies in ACS patients with greater certainty and statistical power.
Methods
The protocol of this review was registered with PROSPERO (CRD42024506844). The guidelines presented in the Cochrane Handbook for Systematic Reviews of Intervention (12) and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (13) were followed for conducting this meta-analysis.
Data sources and searches
We conducted electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (via Ovid), Embase (via Ovid), and ClinicalTrials.gov from inception to April 2024, with no language restrictions, using terms related to “acute coronary syndrome,” “myocardial infarction,” and “blood transfusion.” The detailed search strategies for each database are provided in Supplementary Table S1. Additionally, we reviewed reference lists of included studies and relevant systematic reviews and performed forward citation searching using Web of Science to identify further eligible articles.
Eligibility criteria
We included studies that fulfilled the following PICOS criteria: (1) population: patients diagnosed with ACS and concurrent anemia; (2) intervention: a liberal RBC transfusion strategy; (3) comparator: a restrictive transfusion strategy; (4) outcomes: including any outcome of interest as defined below; and (5) study type: RCTs. ACS was defined as ST-segment elevation MI (STEMI), non-STEMI (NSTEMI), or unstable angina. Anemia was defined as a Hb level <10 g/dl or hematocrit ≤30%. We excluded case reports, single-arm studies, reviews, and animal studies.
Study selection and data extraction
All literature retrieved from our searches was imported into Mendeley Desktop 1.19.8, and duplicates were removed. The remaining records were then uploaded to Rayyan, where two reviewers independently screened the titles and abstracts, followed by full-text screening. Any disagreements between the reviewers were resolved through discussion.
Two reviewers independently extracted data into a structured Excel spreadsheet, capturing study characteristics, participant characteristics, intervention and comparator details, and outcome data. In case of missing data, we planned to contact the study authors to ask for additional information; however, no such instance arose.
Outcomes
The primary outcomes were major adverse cardiovascular events (MACE) defined as the composite of death, myocardial infarction (MI), and revascularization or congestive heart failure, and all-cause mortality. The secondary outcomes included the risk of MI, revascularization, heart failure, stroke, cardiac mortality, acute lung injury, acute kidney injury or failure, and the incidence of pneumonia, bacteremia, or infection.
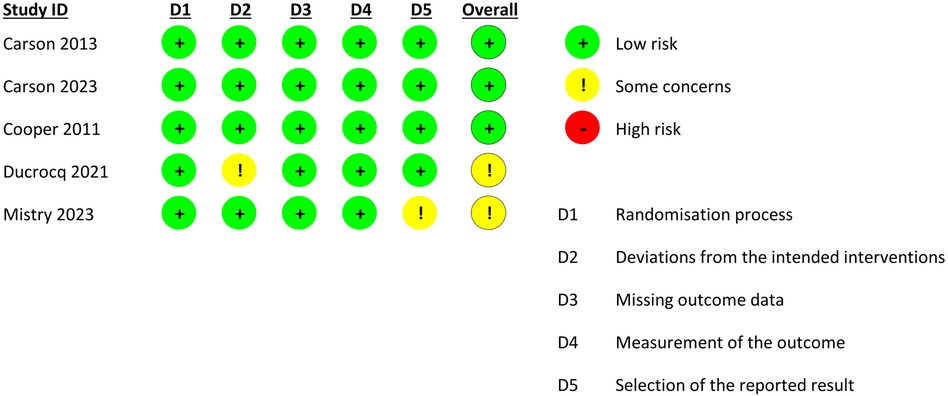
Quality and certainty of evidence assessment
The risk of bias assessment was conducted using the revised Cochrane “Risk of Bias” tool (RoB 2.0) for RCTs (14). The results were presented as a figure.
The quality of evidence for our primary outcomes was graded as very low, low, moderate, or high using the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) assessment tool. GRADE rates the quality of evidence based on the risk of bias, imprecision, inconsistency, and indirectness (15).
Data analysis
Meta-analyses were conducted using Review Manager (RevMan) 5.4, employing a random-effects model with the DerSimonian-Laird variance estimator. The risk ratio (RR) was used as the effect measure. Heterogeneity was assessed using χ² test and I² statistic. We interpreted I2 values according to the guidance presented in the Cochrane Handbook for Systematic Reviews of Interventions (12). We conducted a sensitivity analysis on primary outcomes by excluding the trial by Carson et al. (16) because it was the only study that included patients with unstable angina. We also conducted sensitivity analyses by only including trials with a 30-day follow-up and trials comparing thresholds of Hb <10 g/dl and Hb <8 g/dl. Publication bias could not be assessed as there were less than 10 studies in the review.
Results
Study selection and characteristics
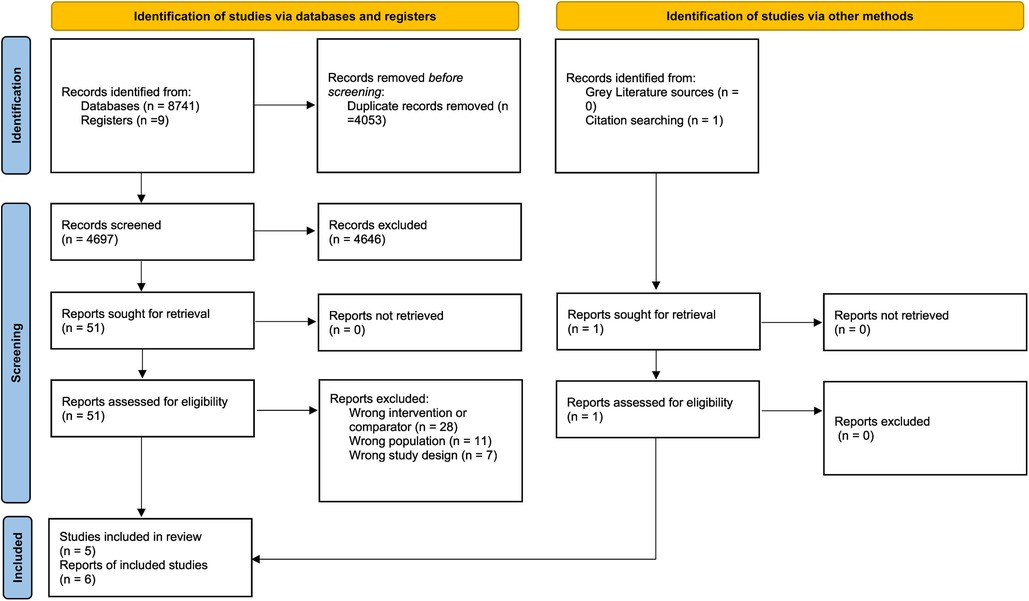
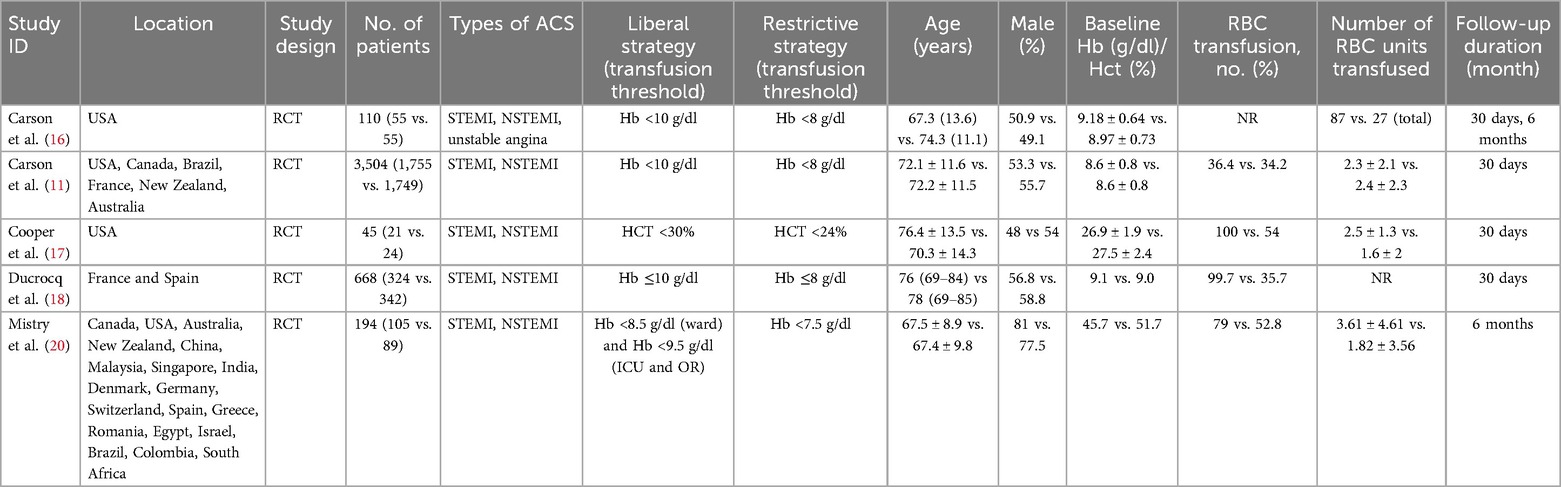
We included a total of six reports from five RCTs in our meta-analysis (11, 16–20). The PRISMA flowchart depicts the detailed screening process (Figure 1). Table 1 illustrates the detailed characteristics of the studies. Most studies included STEMI and NSTEMI patients. The studies took place in a diverse range of countries. The follow-up period ranged from 30 days to 6 months.
Risk of bias in included studies
Three of the five included RCTs had a low risk of bias (Figure 2) (11, 16, 17). One trial had some concerns of bias in the deviations from the intended interventions domain (18), and one reported some concerns of bias in the selection of the reported results (20).
Results of the meta-analysis
Primary outcomes
Major adverse cardiovascular events (MACE)
No statistically significant difference was found between the liberal RBC transfusion and restrictive RBC transfusion groups regarding MACE (RR 0.91, 95% CI: 0.68–1.21; Figure 3). A substantial level of heterogeneity was reported among the studies for this outcome (I2 = 63%). The certainty of evidence was rated as moderate due to concerns about inconsistency (Supplementary Table S2). The results of the sensitivity analysis by the exclusion of Carson et al. (16) were similar to the primary analysis. Analyzing studies with a 30-day follow-up only also yielded similar results. However, only including studies comparing thresholds of Hb <10 g/dl and Hb <8 g/dl tilted the results in favor of the liberal strategy but remained nonsignificant (RR 0.86, 95% CI: 0.73–1.02; I2 = 26%).
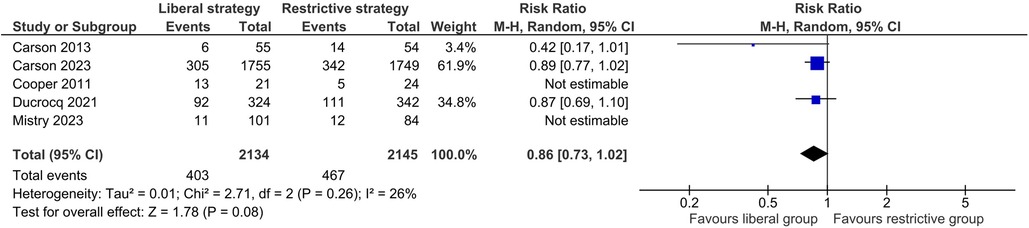
Figure 3. Effect of a liberal versus restrictive transfusion strategy on major adverse cardiovascular events.
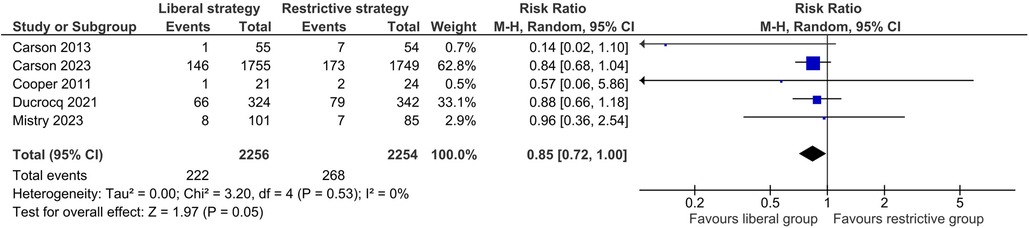
All-cause mortality
There was no significant difference between the two transfusion strategies in the risk of all-cause mortality (RR 0.85, 95% CI: 0.72–1.00; I2 = 0%, Figure 4). The certainty of evidence was rated as moderate due to concerns about imprecision (Supplementary Table S2). The sensitivity analyses did not change the results substantially.
Secondary outcomes
A liberal RBC transfusion strategy reduced the incidence of MI (RR 0.80, 95% CI: 0.66–0.98; I2 = 0%; Supplementary Figure S1). There were no significant differences between the two groups in the risk of revascularization (RR 0.93, 95% CI: 0.63–1.38; I2 = 0%; Supplementary Figure S2), heart failure (RR 1.08, 95% CI: 0.62–1.89; I2 = 44%; Supplementary Figure S3), stroke (RR 0.90, 95% CI: 0.55–1.48; I2 = 0%; Supplementary Figure S4), and cardiac mortality (RR 0.95, 95% CI: 0.33–2.75; I2 = 88%; Supplementary Figure S5). Liberal blood transfusion increased the risk of acute lung injury (RR 8.97, 95% CI: 1.65–48.65; I2 = 0%; Supplementary Figure S6). The rates of acute kidney injury or failure (RR 0.95, 95% CI: 0.76–1.18; I2 = 18%; Supplementary Figure S7) and pneumonia, bacteremia, or infection (RR 1.15, 95% CI: 0.23–5.80; I2 = 50%; Supplementary Figure S8) were similar between the two transfusion strategies.
Discussion
Our meta-analysis demonstrated that a liberal RBC transfusion strategy and a restrictive one in patients with mainly AMI did not differ in terms of the risk of MACE and all-cause mortality. Moreover, the two transfusion strategies did not differ in terms of the risk of revascularization, heart failure, stroke, cardiac mortality, acute kidney injury or failure, pneumonia, bacteremia, or infection. However, liberal blood transfusion reduced the risk of MI and increased the risk of acute lung injury.
As highlighted in our meta-analysis, the absence of difference in mortality between both transfusion groups aligns with findings from previous studies (21–23). A recent meta-analysis of RCTs by Abdelazeem et al. reported similar all-cause mortality, recurrent MI, revascularization, and heart failure exacerbation between the two groups; however, the included RCTs had a limited number of patients, with the cumulative sample size of the meta-analysis being only 821 patients (10). Our study included the MINT trial, the most recent RCT with the largest sample size (N = 3,500) to date, and hence, our analyses accumulate greater statistical power and provide more reliable results (11).
The two largest trials on this topic were incorporated into our study: the MINT and REALITY trials. REALITY was a non-inferiority trial; the study was underpowered regarding superiority (18). The non-inferiority of the restrictive transfusion observed at 30 days was not found at one year: the restrictive strategy was associated with more frequent MACE than the liberal strategy at one year. However, these findings are the results of a post hoc analysis and should be considered exploratory (19).
A study conducted by Wang et al. showed no difference in risk for MI between the two transfusion strategies (24). Their study is in agreement with previous studies that suggest that the liberal strategy is associated with more harm than benefit (25–27). However, in our study, liberal transfusion led to a reduction in the risk of MI. Patients with acute myocardial ischemia are subject to bleeding and acute anemia, especially when they are using anti-platelet medications or therapeutic anticoagulants, and transfusion might be warranted to enhance oxygen delivery and mitigate bleeding risks (28–30). Furthermore, it is to be noted that we found a trend toward reduced all-cause mortality with a liberal transfusion strategy. While these findings favor liberal RBC transfusion, the clinical benefit is uncertain. In addition, the increased risk of acute lung injury seen in our analyses needs to be considered, although the extremely wide 95% CIs suggest that it might be a spurious finding. Moreover, existing literature has shown that RBC transfusion is associated with acute kidney injury (31); however, our analysis did not corroborate this. Insufficient RCTs compound the controversy surrounding these findings to provide conclusive evidence. Large prospective trials are needed in the future to assess the outcomes of both strategies.
One final aspect to consider when choosing the liberal transfusion strategy is the cost burden and the financial implication, especially in the USA, a country where transfusion shortage is a concern (32). The REALITY trial compared the incremental cost-effectiveness ratio at 30 days and the 1-year quality-adjusted life year (QALY) between both strategies, and results suggest that the restrictive option is more cost-effective than liberal transfusion (33). Transfusion remains a costly treatment, and blood transfusions come with an increased risk of transfusion reactions and use of medical resources (18). Thus, this should be taken into account when making any recommendations.
This review had several limitations. Many of the RCTs included were open-label trials and carried a risk of performance bias, as blinding patients and healthcare providers was not possible. Also, some RCTs, such as the MINT trial, lacked central adjudication for many of the included outcomes. Furthermore, there was some variation in the length of follow-up and the transfusion thresholds between the studies, which could have led to heterogeneity in our results. Additionally, as this is a study-level analysis, and we did not have access to individual patient data, we were unable to investigate further subgroups of interest, such as STEMI vs. NSTEMI patients. Finally, we could not assess publication bias as our meta-analysis included less than 10 studies.
Conclusion
Our meta-analysis showed no statistically significant difference in the risk of MACE and all-cause mortality between the liberal and restrictive transfusion groups in patients with ACS, mainly AMI. Among secondary outcomes, there was a lower risk of MI and an elevated incidence of acute lung injury in the liberal transfusion group. There was no statistically significant difference between the two transfusion groups in the risk of heart failure, stroke, cardiac mortality, acute kidney injury or failure, pneumonia, bacteremia or infection, and the need for revascularization. Further, large-scale RCTs are required to establish which of these two transfusion strategies is better.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
SH: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. WU: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. KG: Investigation, Methodology, Writing – original draft, Writing – review & editing. JS: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. SM: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. NA: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. AM: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. TD: Formal analysis, Writing – original draft, Writing – review & editing. SC: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. SN: Investigation, Methodology, Writing – original draft, Writing – review & editing. MR: Writing – original draft, Writing – review & editing. HC: Formal analysis, Supervision, Writing – original draft, Writing – review & editing. AA: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. RA: Methodology, Supervision, Writing – original draft, Writing – review & editing. AS: Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. MS: Formal analysis, Supervision, Writing – original draft, Writing – review & editing. NB: Supervision, Writing – original draft, Writing – review & editing. AY: Supervision, Writing – original draft, Writing – review & editing. KP: Methodology, Writing – original draft, Writing – review & editing. AR: Methodology, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1457400/full#supplementary-material
References
1. Mamas MA, Kwok CS, Kontopantelis E, Fryer AA, Buchan I, Bachmann MO, et al. Relationship between anemia and mortality outcomes in a national acute coronary syndrome cohort: insights from the UK myocardial ischemia national audit project registry. J Am Heart Assoc. (2016) 5:e003348. doi: 10.1161/JAHA.116.003348
2. Huynh R, Hyun K, D’Souza M, Kangaharan N, Shetty PC, Mariani J, et al. Outcomes of anemic patients presenting with acute coronary syndrome: an analysis of the cooperative national registry of acute coronary care, guideline adherence and clinical events. Clin Cardiol. (2019) 42:791–6. doi: 10.1002/clc.23219
3. Sabatine MS, Morrow DA, Giugliano RP, Burton PBJ, Murphy SA, McCabe CH, et al. Association of hemoglobin levels with clinical outcomes in acute coronary syndromes. Circulation. (2005) 111:2042–9. doi: 10.1161/01.cir.0000162477.70955.5f
4. Stucchi M, Cantoni S, Piccinelli E, Savonitto S, Morici N. Anemia and acute coronary syndrome: current perspectives. Vasc Health Risk Manag. (2018) 14:109–18. doi: 10.2147/VHRM.S140951
5. Lotterman S, Sharma S. Blood transfusion. In: StatPearls. Treasure Island, FL: StatPearls Publishing (2024).
6. Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes. J Am Coll Cardiol. (2014) 64:e139–228. doi: 10.1016/j.jacc.2014.09.017
7. Sherwood MW, Rao SV. Acute coronary syndromes: blood transfusion in patients with acute MI and anaemia. Nat Rev Cardiol. (2013) 10:186–7. doi: 10.1038/nrcardio.2013.14
8. Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, et al. Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med. (2012) 157:49–58. doi: 10.7326/0003-4819-157-1-201206190-00429
9. Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes: developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. (2023) 44:3720–826. doi: 10.1093/eurheartj/ehad191
10. Abdelazeem B, Malik B, Kandah E, Banour S, Rafae A, Kunadi A, et al. Restrictive versus liberal blood transfusion strategy in patients with acute myocardial infarction: a meta-analysis of randomized clinical trials. J. Community Hosp Intern Med Perspect. (2022) 12:40–7. doi: 10.55729/2000-9666.1051
11. Carson JL, Brooks MM, Hébert PC, Goodman SG, Bertolet M, Glynn SA, et al. Restrictive or liberal transfusion strategy in myocardial infarction and anemia. N Engl J Med. (2023) 389:2446–56. doi: 10.1056/NEJMoa2307983
12. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed Hoboken, New Jersey: Wiley Blackwell (2019). ISBN 978-1-119-53662-8.
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71–n71. doi: 10.1136/bmj.n71
14. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898–l4898. doi: 10.1136/bmj.l4898
15. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J. (2008) 336:924. doi: 10.1136/bmj.39489.470347.AD
16. Carson JL, Brooks MM, Abbott JD, Chaitman B, Kelsey SF, Triulzi DJ, et al. Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease. Am Heart J. (2013) 165:964–971.e1. doi: 10.1016/j.ahj.2013.03.001
17. Cooper HA, Rao SV, Greenberg MD, Rumsey MP, McKenzie M, Alcorn KW, et al. Conservative versus liberal red cell transfusion in acute myocardial infarction (the CRIT randomized pilot study). Am J Cardiol. (2011) 108:1108–11. doi: 10.1016/j.amjcard.2011.06.014
18. Ducrocq G, Gonzalez-Juanatey JR, Puymirat E, Lemesle G, Cachanado M, Durand-Zaleski I, et al. Effect of a restrictive vs liberal blood transfusion strategy on Major cardiovascular events among patients with acute myocardial infarction and anemia: the REALITY randomized clinical trial. JAMA. (2021) 325:552–60. doi: 10.1001/jama.2021.0135
19. Gonzalez-Juanatey JR, Lemesle G, Puymirat E, Ducrocq G, Cachanado M, Arnaiz JA, et al. One-year major cardiovascular events after restrictive versus liberal blood transfusion strategy in patients with acute myocardial infarction and anemia: the REALITY randomized trial. Circulation. (2022) 145:486–8. doi: 10.1161/CIRCULATIONAHA.121.057909
20. Mistry N, Hare GMT, Shehata N, Belley-Cote E, Papa F, Kramer RS, et al. Transfusion thresholds for acute coronary syndromes-insights from the TRICS-III randomized controlled trial, systematic review, and meta-analysis. J Am Heart Assoc. (2023) 12:e028497. doi: 10.1161/JAHA.122.028497
21. Goel S, Hooda A, Greenstein S, Park WJ, Gidwani U, Sharma S. 100.19 restrictive versus liberal blood transfusion in patients with myocardial infarction and Anemia: a meta-analysis of randomized clinical trials. JACC Cardiovasc Interv. (2024) 17:S6–S6. doi: 10.1016/j.jcin.2024.01.085
22. Kou R, Park JJ, Li A, Laureano M, Crowther M. Restrictive versus liberal transfusion for anemic patients with acute myocardial infarction: systematic review and meta-analysis. Health Sci Rev. (2022) 5:100059. doi: 10.1016/j.hsr.2022.100059
23. Sukhon F, Jabri A, Al-Abdouh A, Alameh A, Alhuneafat L, Jebaje ZA, et al. Liberal versus conservative transfusion strategy for patients with acute myocardial infarction and anemia: a systematic review and meta-analysis. Curr Probl Cardiol. (2024) 49:102247. doi: 10.1016/j.cpcardiol.2023.102247
24. Wang Y, Shi X, Wen M, Chen Y, Zhang Q. Restrictive versus liberal blood transfusion in patients with coronary artery disease: a meta-analysis. Curr Med Res Opin. (2017) 33:761–8. doi: 10.1080/03007995.2017.1280010
25. Ergelen M, Uyarel H, Altay S, Ayhan E, Isik T, Bacaksiz A, et al. Prognostic impact of red blood cell transfusion in patients undergoing primary angioplasty for ST elevation myocardial infarction. Coron Artery Dis. (2012) 23:517. doi: 10.1097/MCA.0b013e328359614c
26. Silvain J, Abtan J, Kerneis M, Martin R, Finzi J, Vignalou J-B, et al. Impact of red blood cell transfusion on platelet aggregation and inflammatory response in anemic coronary and noncoronary patients: the TRANSFUSION-2 study (impact of transfusion of red blood cell on platelet activation and aggregation studied with flow cytometry use and light transmission aggregometry). J Am Coll Cardiol. (2014) 63:1289–96. doi: 10.1016/j.jacc.2013.11.029
27. Chatterjee S, Wetterslev J, Sharma A, Lichstein E, Mukherjee D. Association of blood transfusion with increased mortality in myocardial infarction: a meta-analysis and diversity-adjusted study sequential analysis. JAMA Intern Med. (2013) 173:132–9. doi: 10.1001/2013.jamainternmed.1001
28. Carson JL, Stanworth SJ, Dennis JA, Trivella M, Roubinian N, Fergusson DA, et al. Transfusion thresholds for guiding red blood cell transfusion. Cochrane Database Syst. Rev. (2021) 12(12):CD002042. doi: 10.1002/14651858.CD002042.pub5
29. Carson JL, Guyatt G, Heddle NM, Grossman BJ, Cohn CS, Fung MK, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. (2016) 316:2025–35. doi: 10.1001/jama.2016.9185
30. Roubinian NH, Carson JL. Acute myocardial infarction and blood transfusion: lessons learned from animal models and clinical studies. Blood Transfus. (2023) 21:185–8. doi: 10.2450/BloodTransfus.427
31. Zimarino M, Barbanti M, Dangas GD, Testa L, Capodanno D, Stefanini GG, et al. Early adverse impact of transfusion after transcatheter aortic valve replacement. Circ Cardiovasc Interv. (2020) 13:e009026. doi: 10.1161/CIRCINTERVENTIONS.120.009026
32. Jones JM, Sapiano MRP, Mowla S, Bota D, Berger JJ, Basavaraju SV. Has the trend of declining blood transfusions in the United States ended? Findings of the 2019 national blood collection and utilization survey. Transfusion. (2021) 61:S1–S10. doi: 10.1111/trf.16449
33. Durand-Zaleski I, Ducrocq G, Mimouni M, Frenkiel J, Avendano-Solá C, Gonzalez-Juanatey JR, et al. Economic evaluation of restrictive vs. liberal transfusion strategy following acute myocardial infarction (REALITY): trial-based cost-effectiveness and cost-utility analyses. Eur Heart J Qual Care Clin Outcomes. (2023) 9:194–202. doi: 10.1093/ehjqcco/qcac029
Keywords: ACS, transfusion, restrictive transfusion, liberal transfusion, acute coronary syndrome
Citation: Hidri S, Ur Rehman W, Gardezi K, Shah JZ, Masetti SVS, Almansouri NE, Maan A, Dave T, Catic S, Nagoke SS, Rehman MEU, Cheema HA, Ahmad A, Ahmed R, Selma AB, Sabouni MA, Braiteh N, Yarkoni A, Patel K and Rehman AU (2025) Liberal versus restrictive red blood cell transfusion strategy in acute coronary syndrome and anemia: an updated systematic review and meta-analysis. Front. Cardiovasc. Med. 12:1457400. doi: 10.3389/fcvm.2025.1457400
Received: 2 August 2024; Accepted: 7 April 2025;
Published: 24 April 2025.
Edited by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyReviewed by:
Zixu Zhao, Capital Medical University, ChinaLuca Scorpiglione, Asl Lanciano Vasto Chieti, Italy
Copyright: © 2025 Hidri, Ur Rehman, Gardezi, Shah, Masetti, Almansouri, Maan, Dave, Catic, Nagoke, Rehman, Cheema, Ahmad, Ahmed, Selma, Sabouni, Braiteh, Yarkoni, Patel and Rehman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wajeeh Ur Rehman, d2FqZWVoLnJlaG1hbjlAZ21haWwuY29t; Mohammad Ebad Ur Rehman, ZWJhZHJlaG1hbi5yZWhtYW5AZ21haWwuY29t; Huzaifa Ahmad Cheema, aHV6YWlmYWFobWFkY2hlZW1hQGdtYWlsLmNvbQ==
 Sinda Hidri
Sinda Hidri Wajeeh Ur Rehman
Wajeeh Ur Rehman Karam Gardezi3
Karam Gardezi3 Sai Venkata Siddhartha Masetti
Sai Venkata Siddhartha Masetti Naiela E. Almansouri
Naiela E. Almansouri Tirth Dave
Tirth Dave Sumeja Catic
Sumeja Catic Simranjeet Singh Nagoke
Simranjeet Singh Nagoke Mohammad Ebad Ur Rehman
Mohammad Ebad Ur Rehman Huzaifa Ahmad Cheema
Huzaifa Ahmad Cheema Raheel Ahmed
Raheel Ahmed