- 1Department of Cardiothoracic Surgery, The First Affliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 2Department of Thoracic and Cardiovascular Surgery, The First People’s Hospital of Nanning, The Fifth Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 3Department of Orthopedic Surgery, The First People’s Hospital of Nanning, The Fifth Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 4Department of Pharmacy, The People’s Hospital of Guangxi Zhuang Autonomous Region & Guangxi Academy of Medical Sciences, Nanning, Guangxi, China
Background: Non-rheumatic valvular heart disease (NRVHD), driven by aging populations and epidemiological transitions, has become the dominant form of valvular heart disease globally, yet its burden trends and demographic disparities remain undercharacterized. This study quantifies the global and Chinese burden of NRVHD from 1990 to 2021, analyzing age-sex disparities and temporal trends.
Methods: Using data from the Global Burden of Disease (GBD) 2021 Study. First, the number of incidence, prevalence, deaths, and disability-adjusted life years (DALYs) cases, along with their corresponding age-standardized rates (ASRs), were reported globally and in China, stratified by different sub-types in 2021. These sub-types included sex and age groups. Second, to explore the temporal trend of the disease burden, data from 1990 to 2021 were analyzed both globally and by sub-types. The estimated annual percentage change (EAPC) value was calculated using a linear regression model.
Results: In 2021, NRVHD caused 2,206,928 global incidence cases (ASR: 25.0/100,000) and 28.4 million prevalence cases (ASR: 335.3/100,000), with 181,078 deaths (ASR: 2.31/100,000) and 3.24 million DALYs (ASR: 39.7/100,000). China accounted for 292,215 incidence cases (ASR: 12.8/100,000) and 3.28 million prevalence cases (ASR: 156.2/100,000), demonstrating lower deaths cases (ASDR: 0.13 vs. global 2.31/100,000) but accelerated burden growth. From 1990 to 2021, global incidence rose 129%, while China's surged 220%. Age-standardized deaths rate declined globally and in China, contrasting with rising prevalence. Males bore higher burdens globally and in China, with elderly populations disproportionately affected.
Conclusion: NRVHD burden has escalated globally, characterized by rising morbidity amid declining mortality, a paradox amplified in China. While therapeutic advances and hypertension control contributed to mortality reductions, persistent sex-age disparities and rural-urban inequities demand targeted strategies. China's rapid epidemiological transition underscores the urgency of integrating primary prevention, equitable technology access, and enhanced surveillance to address aging-related valvulopathies.
1 Introduction
Valvular heart disease (VHD) remains a significant contributor to global cardiovascular morbidity and mortality, with non-rheumatic valvular heart disease (NRVHD) emerging as an increasingly critical public health concern in the context of aging populations and epidemiological transitions. While rheumatic heart disease (RHD) has historically dominated VHD burden in low-income regions, NRVHD, encompassing degenerative, congenital, ischemic, and other non-infectious etiologies, now accounts for over 65% of global VHD cases, particularly in high- and middle-income countries (1). This shift parallels demographic aging, as degenerative aortic valve disease prevalence rises exponentially after age 65 (2), and increased survival from cardiovascular comorbidities like hypertension and coronary artery disease (3).
The Global Burden of Disease (GBD) Study 2021 provides critical insights into this evolving landscape, building upon previous analyses that identified VHD as responsible for 12.6 million prevalent cases and 262,000 deaths globally in 2017 (4). However, prior GBD reports have not systematically differentiated NRVHD from RHD in national-level assessments, potentially obscuring distinct risk factor profiles and intervention needs. This gap is particularly relevant for China, where rapid population aging [projected 26% population ≥60 years by 2030 (5)] coincides with dramatic declines in RHD prevalence from 1.19/1000 in 1990 to 0.32/1000 in 2019 (6), while degenerative VHD hospitalizations increased 4.8-fold between 2003−2016 (7).
Recent studies highlight the growing NRVHD burden in China, with aortic stenosis prevalence tripling among adults ≥75 years from 2001−2015 (8), and mitral regurgitation affecting 19.3% of community-dwelling elderly (9). Yet these regional analyses lack integration with global trends and standardized disability metrics. The GBD framework enables comparative assessment through disability-adjusted life years (DALYs), which capture both premature mortality and functional impairment, critical for diseases like NRVHD where interventions often prioritize quality-of-life preservation over survival (10).
This study leverages GBD 2021 data to: (1) Quantify NRVHD burden globally and in China from 1990−2021; (2) Analyze age-sex disparities. Our findings aim to inform health policies addressing the dual challenges of aging-related cardiovascular disease and persistent health disparities in VHD management.
2 Methods
2.1 Data sources
Epidemiological data were extracted from the GBD 2021 database, which aggregates input sources across 204 countries and territories. Key data references included:
Systematic reviews and population-based studies: A comprehensive literature search (1990–2021) was performed across PubMed, EMBASE, China National Knowledge Infrastructure (CNKI), and regional databases to identify studies reporting NRVHD incidence, prevalence, and mortality. Studies were included if they provided echocardiographically confirmed diagnoses based on international guidelines (≥moderate aortic stenosis defined by peak velocity ≥3 m/s) (11).
Vital registration systems: Death certificates and hospital records coded with ICD-10 classifications (I05–I08, I34–I38) were obtained from national health agencies, including the Chinese Center for Disease Control and Prevention (CDC) and WHO Mortality Database. NRVHD cases were defined as ICD-10 I34–I38, excluding rheumatic heart disease (I05–I08).
Disease registries: Subnational data for China were supplemented by the China Cardiovascular Association (CCA) Valve Disease Registry (2015–2020), covering 31 provinces with 28,543 NRVHD cases (12).
2.2 Data processing and modeling
Case definitions aligned with GBD 2021 cause hierarchies, excluding post-rheumatic cases (GBD cause code 294). The DisMod-MR 2.1 Bayesian meta-regression tool was employed to synthesize heterogeneous data, adjusting for covariates including: Echocardiography access, Ambient particulate matter pollution (PM2.5) exposure, and Comorbidity index (aggregating hypertension, diabetes, and coronary artery disease). Covariate selection adhered to the GBD 2021 hierarchy (13). Age-standardized rates (ASRs) were calculated using the GBD 2021 global reference population, with uncertainty intervals (UIs) derived from 1,000 posterior draws of the model.
2.3 Statistical analysis
First, the description of the disease burden was carried out. In 2021, the number of incidence, prevalence, deaths, and DALYs of NRVHD, along with their corresponding age-standardized rates (ASRs), were reported globally and in China, stratified by different sub-types. These sub-types included sex and age groups.
Second, to explore the temporal trend of the disease burden, data from 1990 to 2021 were analyzed both globally and by sub-types. “The estimated annual percentage change (EAPC) value was calculated by fitting a log-linear regression model to the ASRs” (Equations 1, 2) (45). Specifically, the model was defined as:
where α is the intercept and β represents the slope coefficient. The EAPC was then derived as:
Statistical significance was determined when the P-value was less than 0.05. All statistical analyses, including database construction, collation, and analysis, were performed using the R (version 4.0.2) software.
3 Results
3.1 Global and national burden of NRVHD in 2021
In 2021, NRVHD accounted for substantial global disease burden. Globally, there were 2,206,928 incidence cases (95% UI: 2,048,267–2,375,325), corresponding to an age-standardized incidence rate (ASIR) of 25.0 per 100,000 population (95% UI: 23.17–26.92). The prevalence reached 28,389,034 cases (95% UI: 26,323,458–30,585,670), with an age-standardized prevalence rate (ASPR) of 335.29 per 100,000 (95% UI: 311.34–361.05). NRVHD-related deaths totaled 181,078 (95% UI: 155,364–195,717), yielding an age-standardized death rate (ASDR) of 2.31 per 100,000 (95% UI: 1.96–2.50). The DALYs burden stood at 3,238,185 (95% UI: 2,934,104–3,594,474), with an age-standardized DALYs rate (ASDAR) of 39.72 per 100,000 (95% UI: 35.79–44.14) (Tables 1–4).
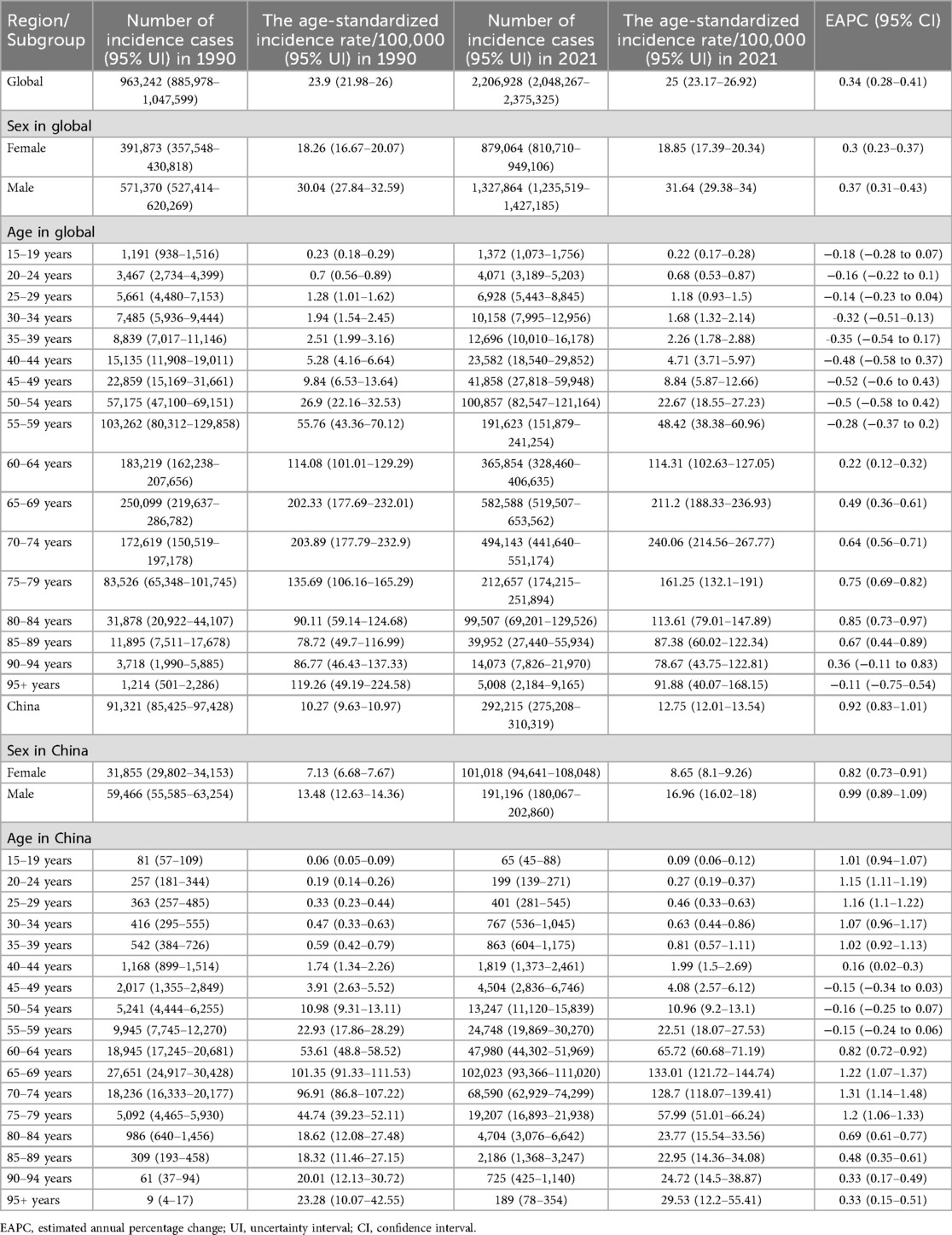
Table 1. The number of incidence cases and the age-standardized incidence rate attributable to non-rheumatic valvular heart disease globally and in China in 1990 and 2021, and its trends from 1990 to 2021 globally.
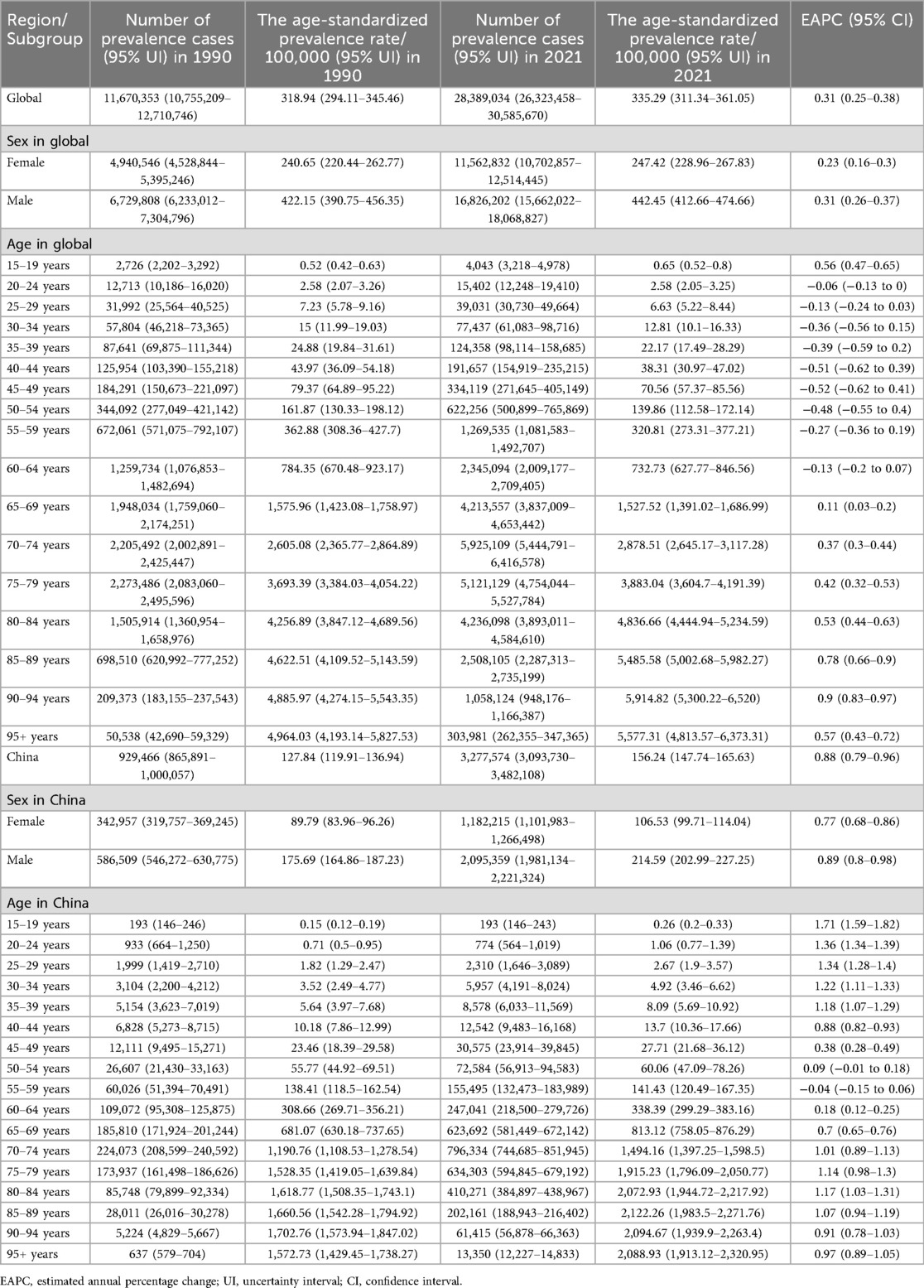
Table 2. The number of prevalence cases and the age-standardized prevalence rate attributable to non-rheumatic valvular heart disease globally and in China in 1990 and 2021, and its trends from 1990 to 2021 globally.
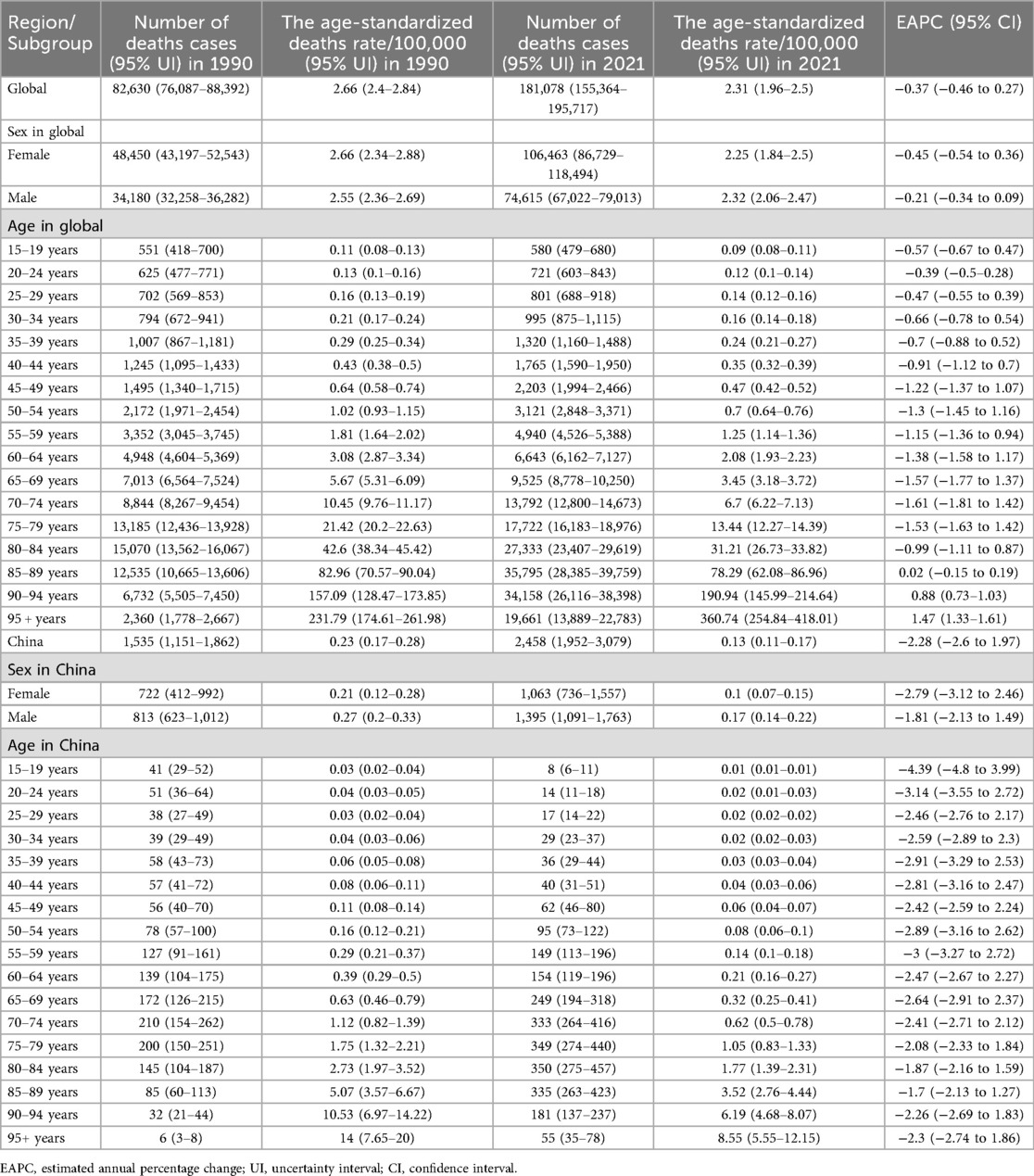
Table 3. The number of deaths cases and the age-standardized deaths rate attributable to non-rheumatic valvular heart disease globally and in China in 1990 and 2021, and its trends from 1990 to 2021 globally.
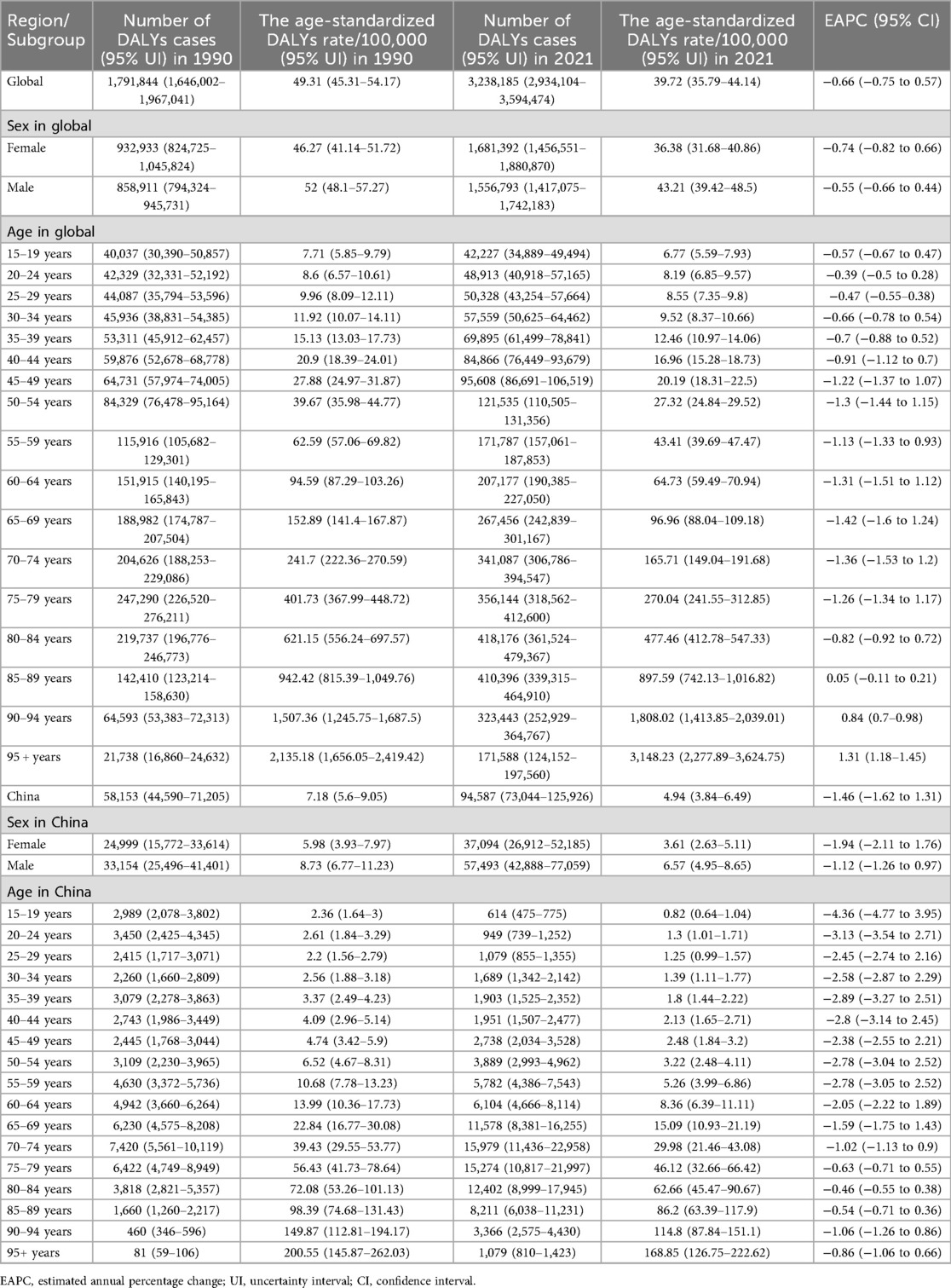
Table 4. The number of DALYs cases and the age-standardized DALYs rate attributable to non-rheumatic valvular heart disease globally and in China in 1990 and 2021, and its trends from 1990 to 2021 globally.
China exhibited distinct epidemiological patterns. In 2021, incidence cases numbered 292,215 (95% UI: 275,208–310,319), with an ASIR of 12.75 per 100,000 (95% UI: 12.01–13.54). Prevalence cases totaled 3,277,574 (95% UI: 3,093,730–3,482,108), corresponding to an ASPR of 156.24 per 100,000 (95% UI: 147.74–165.63). Deaths (2,458; 95% UI: 1,952–3,079) and DALYs (94,587; 95% UI: 73,044–125,926) were markedly lower than global averages, with ASDR and ASDAR at 0.13 (95% UI: 0.11–0.17) and 4.94 (95% UI: 3.84–6.49) per 100,000, respectively (Tables 1–4).
Globally, males exhibited higher burden metrics than females for incidence, prevalence, deaths, DALYs cases and the corresponding ASRs, except for ASDR and ASDAR. In contrast, Chinese males consistently surpassed females across all indicators (Figures 1, 2 and Tables 1–4).
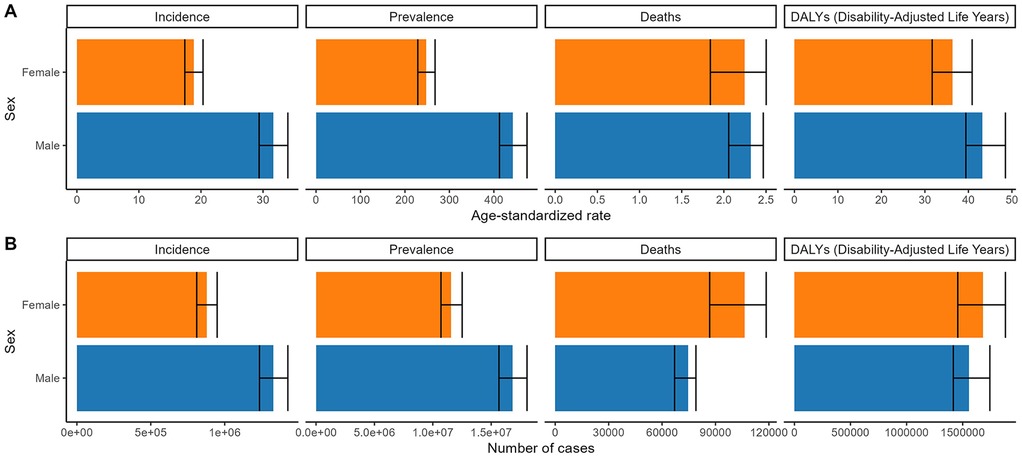
Figure 1. Numbers and age-standardized rates of non-rheumatic valvular heart disease related incidence, prevalence, deaths, and DALYs for both sex in 2021 globally. (A) Age-standardized rate. (B) Number of cases.
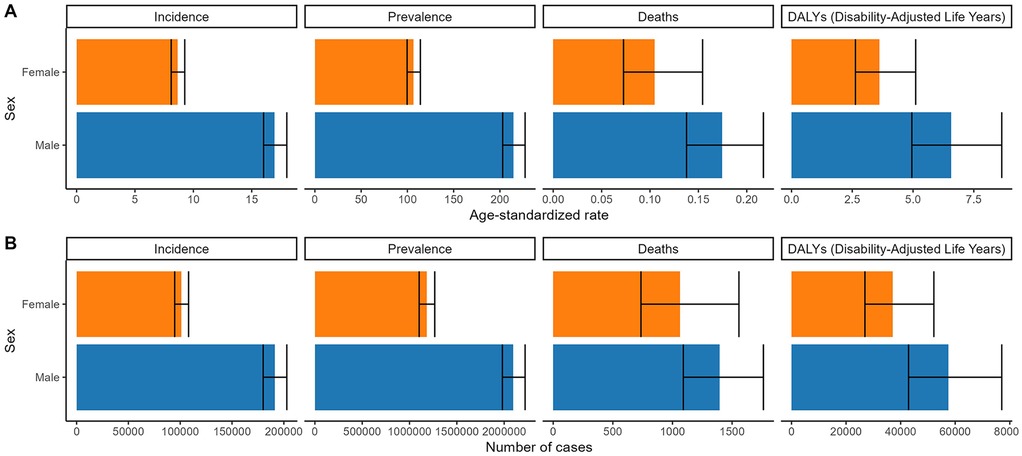
Figure 2. Numbers and age-standardized rates of non-rheumatic valvular heart disease related incidence, prevalence, deaths, and DALYs for both sex in 2021 in China. (A) Age-standardized rate. (B) Number of cases.
The distribution of incidence, prevalence, deaths, and DALYs across age groups globally and in China in 2021 is presented in Figures 3, 4. The number of incidence, prevalence, deaths, and DALYs cases initially increased with age, reaching a peak and then declining globally and in China. The ASDR and ASDAR continuously increased with age. However, ASIR demonstrated a bimodal age distribution: an initial rise in young adulthood, a mid-life decline, and a secondary peak after age 95 (Figures 3, 4 and Tables 1–4).
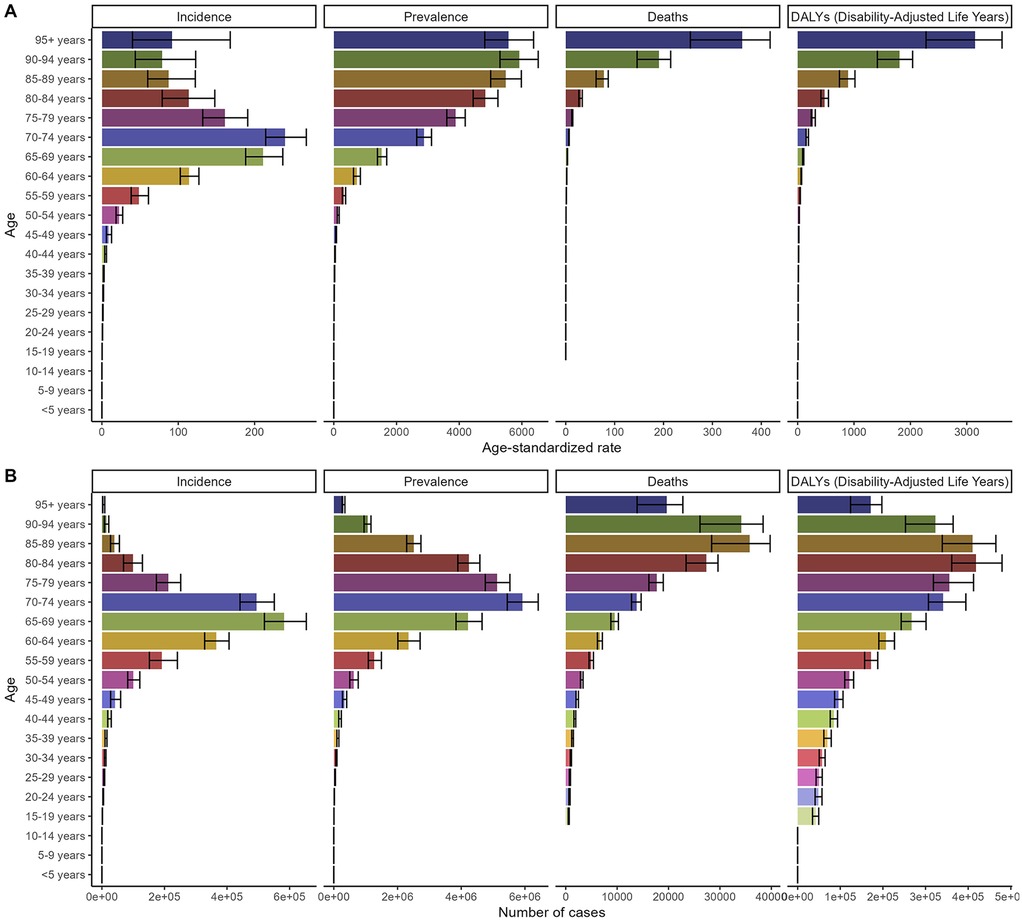
Figure 3. Numbers and age-standardized rates of non-rheumatic valvular heart disease related incidence, prevalence, deaths, and DALYs for different age groups in 2021 globally. (A) Age-standardized rate. (B) Number of cases.
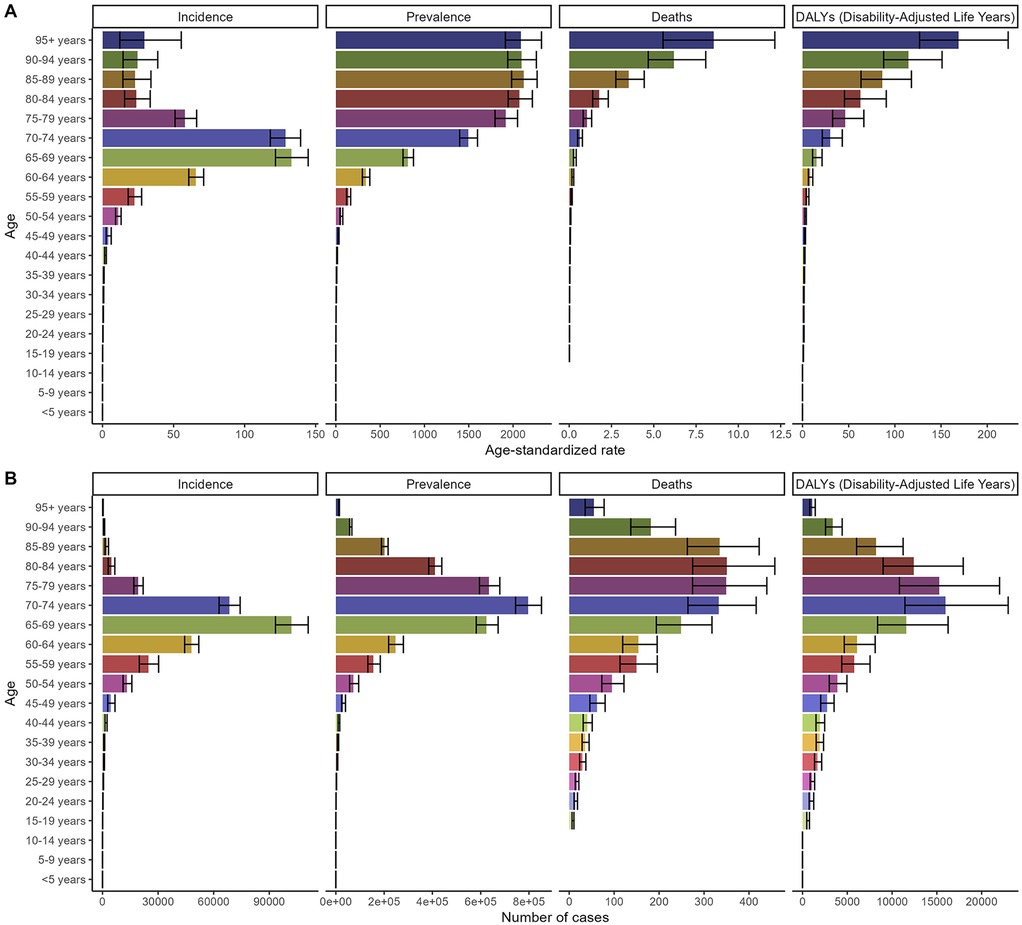
Figure 4. Numbers and age-standardized rates of non-rheumatic valvular heart disease related incidence, prevalence, deaths, and DALYs for different age groups in 2021 in China. (A) Age-standardized rate. (B) Number of cases.
3.2 Temporal trends in disease burden: 1990–2021
Between 1990 and 2021, NRVHD burden escalated globally. incidence cases increased by 129.1% (963,242–2,206,928), while prevalence nearly tripled (6,729,808 to 28,389,034). Deaths and DALYs rose by 119.2% (82,630–181,078) and 80.8% (1,791,844–3,238,185), respectively. Age-standardized rates revealed divergent trends: ASIR increased from 23.9 to 25.0 per 100,000 (+4.6%), and ASPR rose from 422.15 to 442.45 per 100,000 (+4.8%). Conversely, ASDR and ASDAR declined by 13.2% (2.66–2.31) and 19.5% (49.31–39.72), respectively (Figures 5, 6 and Tables 1–4).
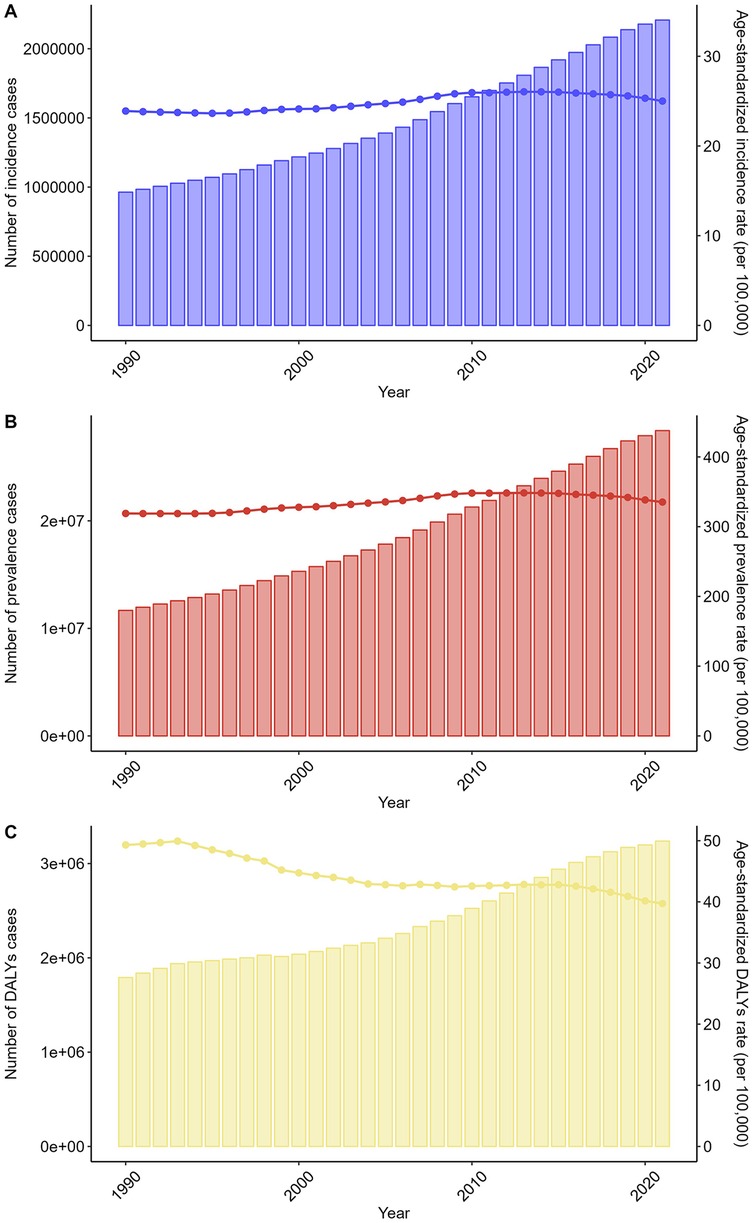
Figure 5. Trends in the numbers and age-standardized rates of non-rheumatic valvular heart disease-related incidence, prevalence, and DALYs globally from 1990 to 2021. (A) Number of incidence cases. (B) Number of prevalence cases. (C) Number of DALYs cases.
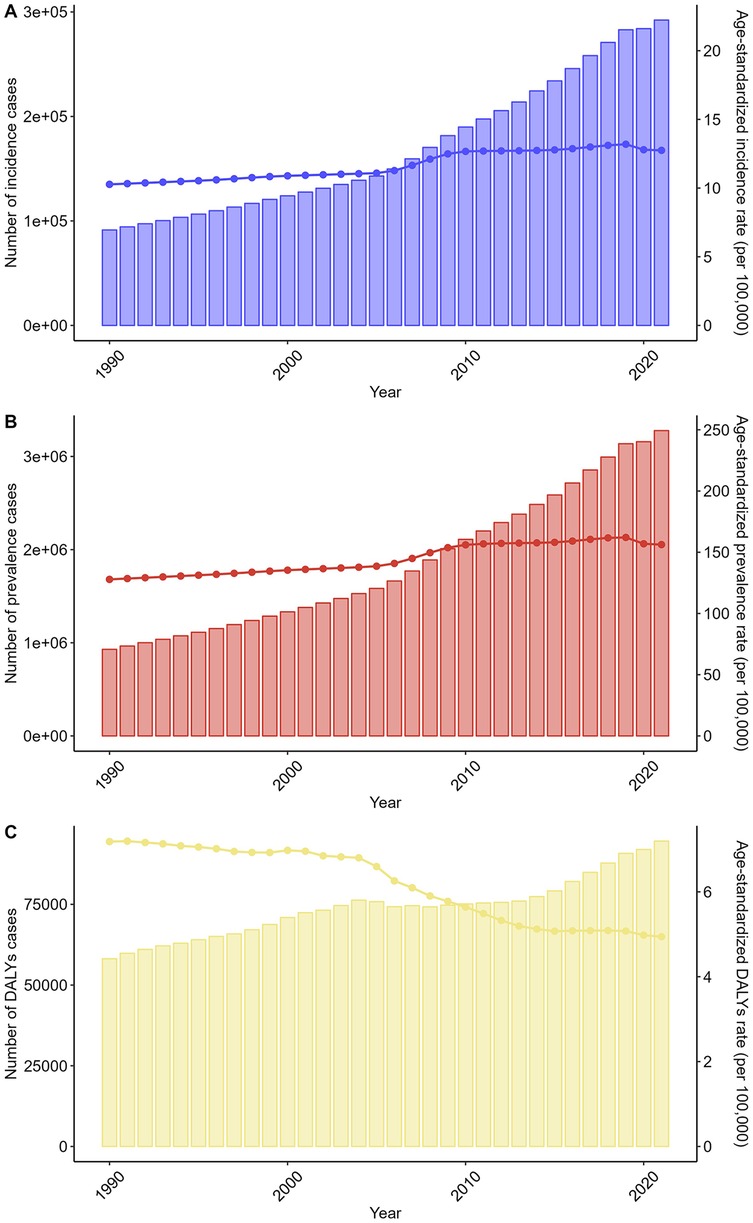
Figure 6. Trends in the numbers and age-standardized rates of non-rheumatic valvular heart disease-related incidence, prevalence, and DALYs in China from 1990 to 2021. (A) Number of incidence cases. (B) Number of prevalence cases. (C) Number of DALYs cases.
China mirrored global patterns but with amplified growth. incidence cases surged by 220.1% (91,321–292,215), and prevalence increased 3.5-fold (929,466–3,277,574). Deaths and DALYs rose by 60.1% (1,535–2,458) and 62.6% (58,153–94,587). Age-standardized metrics showed similar divergence: ASIR increased from 10.27 to 12.75 per 100,000 (+24.1%), and ASPR rose from 127.84 to 156.24 per 100,000 (+22.2%). ASDR and ASDAR declined by 43.5% (0.23–0.13) and 31.2% (7.18 to 4.94), respectively (Figures 5, 6 and Tables 1–4).
Sex-stratified analyses confirmed parallel trends in males and females globally and in China (Supplementary Figures S1, S2 and Tables 1–4). Additionally, the trends were also consistent across all age groups globally and in China (Supplementary Figures S3 and S4 and Tables 1–4).
4 Discussion
This systematic analysis of GBD 2021 data reveals three critical epidemiological transitions in NRVHD: (1) a global escalation in incidence and prevalence contrasting with declining mortality rates, (2) accelerated burden growth in China surpassing global averages, and (3) persistent sex-age disparities shaped by demographic and healthcare inequities. These findings align with, yet crucially extend, prior research on VHD epidemiology, while exposing unique challenges for health systems navigating aging populations and evolving disease profiles.
The observed 129.1% global increase in NRVHD incidence (1990–2021) mirrors population aging trajectories, particularly in high-income countries where degenerative aortic stenosis prevalence triples with each decade beyond age 65 (14). Our ASPR increase (+4.8%) corroborates Coffey et al.'s projection that non-rheumatic etiologies now account for >70% of VHD cases in aging societies (15). Moreover, diagnostic drift must be considered: increased echocardiography access in LMICs [5-fold since 2000 (20)] amplified detection of subclinical cases, partially explaining the incidence-prevalence-mortality divergence. However, the concurrent 13.2% ASDR decline challenges historical assumptions about NRVHD's intractability. Therapeutic advances contributed significantly, particularly in China where TAVI expansion [100 to 6,500 procedures/year, 2012–2021 (28)] contributed to the ASDR decline.
Advancements in minimally invasive interventions, notably transcatheter aortic valve implantation (TAVI), have expanded treatment eligibility. Since its 2002 introduction, TAVI utilization has grown exponentially, with 150,000 annual procedures globally by 2021 (16). This technological shift reduced perioperative mortality from 8.2% (surgical AVR) to 2.9% (TAVI) in high-risk patients (17), partially explaining mortality declines despite rising case numbers.
Second, improved cardiovascular risk factor management has altered disease progression. The 19.5% global ASDAR reduction aligns with studies showing statins and antihypertensives slow calcific aortic stenosis progression by 18%–34% (18). In China, aggressive hypertension control (prevalence reduced from 21.7% to 15.3% in 1990–2021) (19) may have contributed to its steeper 31.2% ASDAR decline.
Third, diagnostic ascertainment bias cannot be discounted. Echocardiography availability increased 5-fold in low/middle-income countries (LMICs) since 2000 (20), potentially inflating incidence counts through detection of subclinical cases. This “diagnostic creep” may artificially amplify morbidity-mortality divergence, a phenomenon previously documented in chronic kidney disease epidemiology (21).
China's 220.1% NRVHD incidence surge, triple the global rate, epitomizes the collision between rapid aging and incomplete healthcare modernization. Three factors dominate:
1. Demographic Pressures: China's ≥65 population ballooned from 5.6% (1990) to 13.5% (2021) (22), directly fueling degenerative valve disease. Our estimated ASPR of 156.24/100,000 aligns with Wu et al.'s national survey finding aortic stenosis prevalence tripling among those ≥75 years (2001–2015) (23).
2. Epidemiological Transition: As China controlled rheumatic fever (RHD prevalence dropped 73% since 1990) (24), NRVHD emerged as the dominant valvulopathy. Hospitalization data shows degenerative VHD surpassing RHD as the leading valve surgery indication since 2010 (25).
3. Healthcare Access Gaps: Despite progress, echocardiography penetration remains uneven, 85% in urban vs. 32% in rural China (26). This underdiagnosis paradoxically suggests our estimates may understate true burden, particularly in western provinces.
However, China's mortality decline (−43.5% ASDR) outpaces global trends, likely reflecting concentrated investment in tertiary cardiac care. Between 2015 and 2021, China increased cardiac surgery centers from 564 to 1,122 (27), with TAVI procedures growing from 100 (2012) to 6,500 annually (28). Yet this progress remains fragile: rural mortality rates are 3.1-fold higher than urban areas for valve diseases (29), exposing persistent equity challenges.
Our findings reinforce, but complicate, established narratives about VHD disparities. Globally, males’ higher incidence/prevalence aligns with known sex-specific risk profiles: aortic stenosis progression is 40% faster in males (30), while hypertension, a key mitral regurgitation driver, affects 31% of men vs. 26% of women globally (31). However, the absence of sex differences in ASDR/ASDAR contradicts studies suggesting worse post-intervention survival in women (32). This paradox may reflect:
1. Treatment Bias: Women are 23% less likely to undergo valve surgery at advanced ages (33), potentially excluding high-risk females from mortality statistics.
2. Competing Risks: Longer female life expectancy increases non-cardiac mortality, diluting NRVHD-specific death rates.
In China, males’ across-the-board burden dominance likely intertwines biological and cultural factors. Smoking rates are 48.4% in men vs. 2.0% in women (34), exacerbating aortic calcification. Simultaneously, patriarchal norms may prioritize male healthcare access, a phenomenon observed in cancer screening disparities (35).
Age distribution patterns reveal another layer of complexity. The bimodal ASIR peak, rising in young adulthood (congenital/residual RHD), dipping mid-life, then surging post-70 (degenerative), mirrors pathophysiological transitions documented in European registries (36). Age distribution patterns further revealed clinical imperatives: bimodal ASIR peaks (young adulthood and senescence) underscore the need for early-life congenital/residual RHD screening and age-targeted degenerative disease surveillance. The steep elderly incidence spike suggests delayed diagnosis: median time from symptom onset to surgery remains 5.2 years vs. 1.8 years in the U.S (37).
These findings necessitate tiered policy responses:
Global Priorities:
1. Enhanced Surveillance: Current ICD coding often conflates valve etiologies (38). WHO should mandate distinct NRVHD/RHD reporting to guide resource allocation.
2. TAVI Cost-Reduction: With 80% of LMICs lacking TAVI access (39), device cost-innovation (China's Venus Valve priced at 12,000 vs.12,000 vs.32,000 Western equivalents) (40) is critical.
China-Specific Strategies:
1. Primary Prevention: Integrate valve screening into national hypertension/diabetes programs, a model piloted in Guangdong reduced severe VHD by 18% (41).
2. Regional Resource Balancing: Expand “mobile echo units” to rural areas, replicating Sichuan Province's 37% case-detection increase (42).
3. Sex-Sensitive Care: Address implicit bias in treatment referrals through clinician training programs.
While leveraging GBD's standardized methodology, several limitations warrant consideration:
1. Etiological Overlap: GBD's reliance on hospital data may undercount “secondary” NRVHD (mitral regurgitation from ischemic cardiomyopathy) (43).
2. Treatment Effect Lag: Mortality declines from recent TAVI adoption may be underestimated in 2021 data.
3. Chinese Subtypes: Lack of provincial-level etiology data (bicuspid aortic valve prevalence varies from 0.5% in Guangxi to 1.2% in Shandong) (44) limits localized interventions.
Future research should prioritize etiology-specific burden mapping and cost-effectiveness analyses of novel interventions across diverse healthcare settings.
This study has several methodological constraints. First, reliance on modeled GBD estimates rather than primary population-based registries may mask subnational heterogeneities, particularly given the absence of provincial-level data for China. Consequently, localized burden patterns (e.g., rural-urban gradients) remain incompletely characterized. Second, aggregation of non-rheumatic valvular heart disease without etiological stratification (e.g., aortic stenosis vs. mitral regurgitation) limits mechanistic insights and precludes lesion-specific interventions. Third, potential misclassification of secondary valvular lesions—notably ischemic mitral regurgitation—may occur in administrative coding systems, affecting burden accuracy. Finally, while mortality declines were statistically robust globally, wider UIs in under-surveilled regions indicate reduced precision in subnational estimates due to sparse data. These limitations underscore the need for enhanced clinical registries to validate model outputs and capture etiological spectra.
5 Conclusion
This systematic analysis of GBD 2021 data highlights the dual challenge of rising NRVHD morbidity and declining mortality globally and in China, driven by population aging and epidemiological transition. Between 1990 and 2021, global NRVHD incidence surged by 129%, with China experiencing a 220% increase, reflecting accelerated demographic shifts. While age-standardized mortality rates declined by 13.2% globally and 43.5% in China, attributable to advances in transcatheter interventions and cardiovascular risk management, persisting sex disparities (male predominance) and geographic inequities (rural China's mortality tripling urban rates) underscore unmet needs. China's rapid burden escalation, juxtaposed with fragmented healthcare access, calls for prioritized primary prevention (hypertension control), equitable diffusion of cost-effective technologies (domestically produced TAVI valves), and strengthened surveillance systems to address aging-related valvulopathies. These findings mandate integrated strategies balancing therapeutic innovation with preventive equity to mitigate NRVHD's growing societal impact.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
WC: Conceptualization, Writing – original draft. JW: Investigation, Writing – review & editing. XZ: Software, Writing – original draft. YL: Data curation, Writing – original draft. BZ: Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The work was financially supported by the National Natural Science Foundation of China (8236020468).
Acknowledgments
We would like to thank all the professionals who contributed to the discussion and elaboration of this minireview.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1641448/full#supplementary-material
References
1. Coffey S, Roberts-Thomson R, Brown A, Carapetis J, Chen M, Enriquez-Sarano M, et al. Global epidemiology of valvular heart disease. Nat Rev Cardiol. (2021) 18(12):853–64. doi: 10.1038/s41569-021-00570-z
2. Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. The tromsø study. Heart. (2013) 99(6):396–400. doi: 10.1136/heartjnl-2012-302265
3. Lindman BR, Bonow RO, Otto CM. Current management of calcific aortic stenosis. Circ Res. (2013) 113(2):223–37. doi: 10.1161/CIRCRESAHA.111.300084
4. Collaborators GCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392(10159):1736–88. doi: 10.1016/S0140-6736(18)32203-7
5. Wang YJ, Li ZX, Gu HQ, Zhai Y, Zhou Q, Jiang Y, et al. China stroke statistics: an update on the 2019 report from the national center for healthcare quality management in neurological diseases, China national clinical research center for neurological diseases, the Chinese stroke association, national center for chronic and non-communicable disease control and prevention, Chinese center for disease control and prevention and institute for global neuroscience and stroke collaborations. Stroke Vasc Neurol. (2022) 7(5):415–50. doi: 10.1136/svn-2021-001374
6. Ou Z, Yu D, Liang Y, Wu J, He H, Li Y, et al. Global burden of rheumatic heart disease: trends from 1990 to 2019. Arthritis Res Ther. (2022) 24(1):138. doi: 10.1186/s13075-022-02829-3
7. Ma Q, Li R, Wang L, Yin P, Wang Y, Yan C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the global burden of disease study 2019. Lancet Public Health. (2021) 6(12):e897–906. doi: 10.1016/S2468-2667(21)00228-0
8. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. (2020) 382(13):1199–207. doi: 10.1056/NEJMoa2001316
9. Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health (CPH) study): a national cross-sectional study. Lancet. (2018) 391(10131):1706–17. doi: 10.1016/S0140-6736(18)30841-9
10. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2021;77(4):e25–e197. doi: 10.1016/j.jacc.2020.11.018
11. Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. (2022) 43(7):561–632. doi: 10.1093/eurheartj/ehab395
12. Liu Y, Zhang C, Wang Q, Wu K, Sun Z, Tang Z, et al. Temporal trends in the disease burden of colorectal cancer with its risk factors at the global and national level from 1990 to 2019, and projections until 2044. Clin Epidemiol. (2023) 15:55–71. doi: 10.2147/CLEP.S388323
13. Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. (2016) 388(10062):e19–23. doi: 10.1016/S0140-6736(16)30388-9
14. Eveborn GW, Schirmer H, Lunde P, Heggelund G, Hansen JB, Rasmussen K. Assessment of risk factors for developing incident aortic stenosis: the tromsø study. Eur J Epidemiol. (2014) 29(8):567–75. doi: 10.1007/s10654-014-9936-x
15. Santangelo G, Bursi F, Faggiano A, Moscardelli S, Simeoli PS, Guazzi M, et al. The global burden of valvular heart disease: from clinical epidemiology to management. J Clin Med. (2023) 12(6):2178. doi: 10.3390/jcm12062178
16. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. (2021) 143(5):e35–71. doi: 10.1161/CIR.0000000000000932
17. Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. (2016) 374(17):1609–20. doi: 10.1056/NEJMoa1514616
18. Cowell SJ, Newby DE, Prescott RJ, Bloomfield P, Reid J, Northridge DB, et al. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med. (2005) 352(23):2389–97. doi: 10.1056/NEJMoa043876
19. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE million persons project). Lancet. (2017) 390(10112):2549–58. doi: 10.1016/S0140-6736(17)32478-9
20. Marijon E, Mocumbi A, Narayanan K, Jouven X, Celermajer DS. Persisting burden and challenges of rheumatic heart disease. Eur Heart J. (2021) 42(34):3338–48. doi: 10.1093/eurheartj/ehab407
21. Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. (2015) 88(5):950–7. doi: 10.1038/ki.2015.230
22. Xie J, Lu C. Is there a casual relation between air pollution and dementia? Environ Sci Pollut Res Int. (2023) 30(9):23248–62. doi: 10.1007/s11356-022-23226-y
23. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5
24. Shi L, Bao C, Wen Y, Liu X, You G. Analysis and comparison of the trends in burden of rheumatic heart disease in China and worldwide from 1990 to 2019. BMC Cardiovasc Disord. (2023) 23(1):517. doi: 10.1186/s12872-023-03552-w
25. Zhang H, Wang H, Shen X, Jia X, Yu S, Qiu X, et al. The landscape of regulatory genes in brain-wide neuronal phenotypes of a vertebrate brain. Elife. (2021) 10:e68224. doi: 10.7554/eLife.68224
26. Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet. (2019) 394(10196):407–18. doi: 10.1016/S0140-6736(19)31147-X
27. The Writing Committee of the Report on Cardiovascular Health and Diseases in China, Hu SS. Report on cardiovascular health and diseases in China 2021: an updated summary. J Geriatr Cardiol. (2023) 20(6):399–430. doi: 10.26599/1671-5411.2023.06.001
28. Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, et al. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. (2020) 181(4):894–904.e9. doi: 10.1016/j.cell.2020.03.045
29. Zhang M, Shi Y, Shi O, Zhao Z, Zhang X, Li C, et al. Geographical variations in cardiovascular health in China: a nationwide population-based survey of 74,726 adults. Lancet Reg Health West Pac. (2020) 3:100033. doi: 10.1016/j.lanwpc.2020.100033
30. Aggarwal SR, Clavel MA, Messika-Zeitoun D, Cueff C, Malouf J, Araoz PA, et al. Sex differences in aortic valve calcification measured by multidetector computed tomography in aortic stenosis. Circ Cardiovasc Imaging. (2013) 6(1):40–7. doi: 10.1161/CIRCIMAGING.112.980052
31. (NCD-RisC). NRFC. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398(10304):957–80. doi: 10.1016/S0140-6736(21)01330-1
32. Chandrasekhar J, Dangas G, Yu J, Vemulapalli S, Suchindran S, Vora AN, et al. Sex-based differences in outcomes with transcatheter aortic valve therapy: TVT registry from 2011 to 2014. J Am Coll Cardiol. (2016) 68(25):2733–44. doi: 10.1016/j.jacc.2016.10.041
33. Chaker Z, Badhwar V, Alqahtani F, Aljohani S, Zack CJ, Holmes DR, et al. Sex differences in the utilization and outcomes of surgical aortic valve replacement for severe aortic stenosis. J Am Heart Assoc. (2017) 6(9):e006370. doi: 10.1161/JAHA.117.006370
34. Chan KH, Xiao D, Zhou M, Peto R, Chen Z. Tobacco control in China. Lancet Public Health. (2023) 8(12):e1006–e15. doi: 10.1016/S2468-2667(23)00242-6
35. Cao M, Li H, Sun D, He S, Yu Y, Li J, et al. Cancer screening in China: the current status, challenges, and suggestions. Cancer Lett. (2021) 506:120–7. doi: 10.1016/j.canlet.2021.02.017
36. Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: the euro heart survey on valvular heart disease. Eur Heart J. (2003) 24(13):1231–43. doi: 10.1016/S0195-668X(03)00201-X
37. Yang Y, Wang Z, Chen Z, Wang X, Zhang L, Li S, et al. Current status and etiology of valvular heart disease in China: a population-based survey. BMC Cardiovasc Disord. (2021) 21(1):339. doi: 10.1186/s12872-021-02154-8
38. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010
39. Vervoort D, Swain JD, Pezzella AT, Kpodonu J. Cardiac surgery in low- and middle-income countries: a state-of-the-art review. Ann Thorac Surg. (2021) 111(4):1394–400. doi: 10.1016/j.athoracsur.2020.05.181
40. Hensey M, Murdoch DJ, Sathananthan J, Alenezi A, Sathananthan G, Moss R, et al. First-in-human experience of a new-generation transfemoral transcatheter aortic valve for the treatment of severe aortic regurgitation: the J-valve transfemoral system. EuroIntervention. (2019) 14(15):e1553–e5. doi: 10.4244/EIJ-D-18-00935
41. Zhang X, Gu X, Xu Y, Wang X, Weng F, Wen Y, et al. Prevalence and clustering of modifiable cardiovascular disease risk factors among elderly adults in Yuexiu district, Guangzhou city, China: a cross sectional study. BMC Cardiovasc Disord. (2025) 25(1):237. doi: 10.1186/s12872-025-04676-x
42. Li X, Shi Y, Zhao D, Jin K, Zhu J, Wang Y. Unmet needs for rehabilitation service of middle-aged and older adult residents in Chengdu, Sichuan, China: a cross-sectional study. Sci Rep. (2023) 13(1):11989. doi: 10.1038/s41598-023-38960-7
43. Chen QF, Shi S, Wang YF, Shi J, Liu C, Xu T, et al. Global, regional, and national burden of valvular heart disease, 1990 to 2021. J Am Heart Assoc. (2024) 13(24):e037991. doi: 10.1161/JAHA.124.037991
44. Yang LT, Michelena HI, Maleszewski JJ, Schaff HV, Pellikka PA. Contemporary etiologies, mechanisms, and surgical approaches in pure native aortic regurgitation. Mayo Clin Proc. (2019) 94(7):1158–70. doi: 10.1016/j.mayocp.2018.11.034
Keywords: valvular heart disease, global, China, disease burden, GBD
Citation: Chen W, Wei J, Zheng X, Lan Y and Zheng B (2025) Burden of non-rheumatic valvular heart disease globally and in China from 1990 to 2021: a systematic analysis for the global burden of disease study 2021. Front. Cardiovasc. Med. 12:1641448. doi: 10.3389/fcvm.2025.1641448
Received: 5 August 2025; Accepted: 24 October 2025;
Published: 20 November 2025.
Edited by:
Abdul-Aziz Seidu, James Cook University, AustraliaReviewed by:
Xue Wu, University of California, San Francisco, United StatesYizhe Song, Washington University in St. Louis, United States
Mengting Li, University of Florida, United States
Copyright: © 2025 Chen, Wei, Zheng, Lan and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baoshi Zheng, emhlbmdiczI1QHZpcC5zaW5hLmNvbQ==; Yanni Lan, MjM3OTExNjIzQHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Wen Chen1,2,†
Wen Chen1,2,† Jiyong Wei
Jiyong Wei Yanni Lan
Yanni Lan