- 1Department of Emergency Medicine, University of Colorado School of Medicine, Aurora, CO, United States
- 2Department of Neurology, University of Colorado School of Medicine, Aurora, CO, United States
- 3Department of Health Systems, Management, and Policy, Colorado School of Public Health, Aurora, CO, United States
- 4Department of Emergency Medicine, Yale School of Medicine, New Haven, CT, United States
Introduction: Prehospital stroke care can influence in-hospital stroke care, including facilitating earlier diagnosis and treatment. This study sought to determine the association between prehospital IV access and time to computed tomography (CT), intravenous (IV) thrombolytic administration, and endovascular therapy in patients with stroke.
Methods: This was a multi-institutional, multi-agency retrospective analysis of patients who were identified as having stroke-like presentations by emergency medical services (EMS) and had a final clinical diagnosis of stroke or transient ischemic attack (TIA) from January 1, 2020, to December 31, 2022. Data were analyzed using descriptive statistics and multivariable linear regressions controlling for receiving hospital stroke certification level, sex, age, initial NIHSS score, hospital prenotification of suspected stroke, and EMS-documented blood glucose level, stroke scale, and last known well (LKW) time.
Results: Of the 3,109 patients in the study, 91.2% (n = 2,834) arrived with IV access obtained from EMS. Patients who arrived with IV access had a median door-to-CT time of 10 min [interquartile range (IQR) 7–16 min] compared to those without IV access who had a median door-to-CT time of 12 min (IQR 8–21 min; p < 0.05). After adjusting for covariates, arrival without IV access increased the door-to-CT time by 26% [ratio estimate 1.26, 95% confidence interval (CI), 1.14–1.39] compared to those with IV access. Similarly, after controlling for covariates, lack of prehospital IV access was associated with increased time to intravenous thrombolysis (IVT; ratio estimate 1.17, 95% CI, 1.01–1.36), but not with time to endovascular thrombectomy (EVT; ratio estimate 1.05, 95% CI, 0.82–1.33) compared to those with prehospital IV access.
Conclusion: EMS insertion of an IV prior to hospital arrival was associated with shorter time to imaging and shorter time to intravenous thrombolysis but was not associated with a difference in time to endovascular thrombectomy.
Introduction
Worldwide, stroke is the second-leading cause of death, with the number of annual deaths increasing by 43% over the last 20 years (1). A high-functioning stroke system can significantly reduce the morbidity and mortality of patients with stroke. However, when it comes to recognition and intervention, time is of the essence. For every minute in delay to treatment, a patient loses approximately 1.9 million neurons, and for each hour that passes without treatment, the neuronal loss equates to roughly 3.6 years of normal aging (2).
Intravenous thrombolysis (IVT) efficacy is time dependent, and reductions in time to IVT administration [door-to-needle (DTN) time] both improve clinical outcomes and decrease mortality (3–5). Computed tomography (CT) or other advanced imaging is essential in making the decision of whether to treat with either IVT or endovascular thrombectomy (EVT). Decreased door-to-CT (DTCT) time is associated with decreased DTN time and represents an important target for improving in-hospital stroke care (6).
Most patients with an acute stroke arrive at the emergency department via emergency medical services (EMS) transport (7, 8). Patients who arrive via EMS receive faster evaluation, imaging, and treatment compared to patients who arrive via private vehicle, which has made prehospital stroke recognition, evaluation, and management a major focus of improving outcomes (9, 10). EMS providers can accurately diagnose stroke in the prehospital setting using validated stroke scales (11–13). Prehospital identification of patients with acute stroke is associated with improved in-hospital care, including shorter times to CT and therapy (14). Interventions associated with decreased DTCT and DTN times include EMS-to-hospital prenotification of suspected stroke, obtaining a last known well (LKW) time, and documenting a blood glucose level (15–21).
The American Heart Association (AHA) updated its prehospital stroke care guidelines in 2019 and identified eight recommendations for optimal care (22). Full compliance with these guidelines is poor, ranging from only 0.39% of encounters in a nationwide dataset to 5.1% in smaller local datasets, likely due in part to transport-related time constraints in the prehospital setting (21). While the updated AHA guidelines do not mention intravenous (IV) access in the prehospital environment, the previous 2013 AHA guidelines recommend establishment of IV access per local protocol but note that prehospital interventions should not delay rapid transport to the receiving hospital (23). Other guidelines give a level C recommendation to obtaining IV access during transport, acknowledging the utility of this intervention while noting that it should not delay transport (24). These guidelines identify a reasonable concern regarding prehospital IV access—obtaining IV access could delay rapid transport to the hospital, including extending the on-scene time (time from EMS arrival to the patient until initiation of transport to the hospital).
The impact of prehospital IV access on time to imaging and intervention in patients with acute stroke is unknown. This study sought to determine the association between prehospital IV access and time to CT, IVT, and EVT in patients with suspected stroke. The hypothesis was that IV access could facilitate more rapid in-hospital care and that there would be no significant differences in on-scene or transport times.
Methods
Population
This was a multi-institutional, multi-agency retrospective analysis of adult (aged 18 years or older) patients who were identified as having a suspected stroke by EMS clinicians in the field and had a final diagnosis of hemorrhagic or ischemic stroke or transient ischemic attack (TIA) that were included in the IMPACT (Innovative Measures for Prehospital Advancement in Cerebrovascular Treatment) collaboration between January 1, 2020, and December 31, 2022. Patient encounters were included if: (1) EMS primary or secondary impression was stroke, cerebral vascular accident (CVA), or TIA or if an EMS clinician activated a “stroke alert,” and (2) the final in-hospital diagnosis was CVA (ischemic or hemorrhagic) or TIA (Figure 1). Spontaneous subarachnoid hemorrhages, but not those due to trauma, were included as a hemorrhagic stroke. TIA diagnosis was based on the treating physician's clinical judgement. EMS impressions were based on prehospital provider clinical assessment and use of validated prehospital stroke scales. There was variation between and within agencies as to the preferred stroke scale, which included the Cincinnati Prehospital Stroke Scale (CPSS), Face Arm Speech Time (FAST), Balance Eyes-Face Arm Speech Time (BE-FAST), and the Miami Emergency Neurologic Deficit Exam (MEND), as well as stroke severity or large vessel occlusion scales, such as the Field Assessment Stroke Triage for Emergency Destination (FAST-ED), Los Angeles Motor Scale (LAMS), and Vision, Aphasia, Neglect (VAN) tools. IMPACT includes EMS agencies (both private and fire-based) and hospitals [academic and community hospitals that were a mix of comprehensive stroke centers (CSC), primary stroke centers (PSC), acute stroke ready hospitals (ASRH), and those that were not a recognized stroke center] from across Colorado or on the border with Colorado. EMS agencies transport patients based on local protocols, which recommend transport to “the closest appropriate facility.” It is not the current practice of any agency within IMPACT to bypass hospitals capable of basic stroke care to transport to higher designations, such as CSCs.
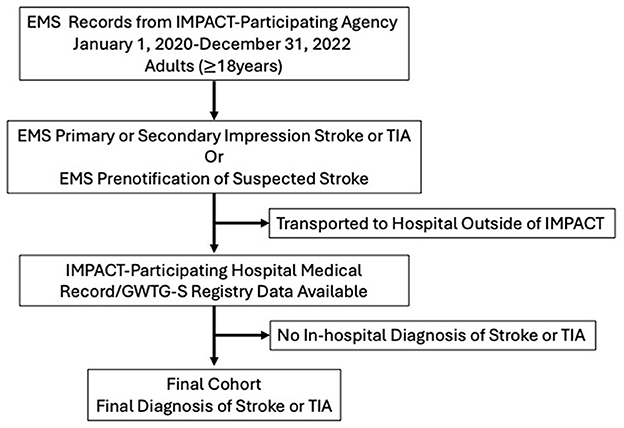
Figure 1. Flow chart for identification of EMS encounters meeting full inclusion/exclusion criteria.
Data abstraction
Data were extracted by a group of highly trained abstractors. Before completing data extraction for this study, each individual had to complete training and practice chart extractions (minimum of 30 practice charts) to demonstrate 90% accuracy for all variables extracted. EMS agency variables and data for hospitals that were not recognized as stroke centers were extracted using standardized case report forms created in REDCap, a HIPAA-compliant program. Additional in-hospital data were extracted from local Get with the Guidelines Stroke (GWTG-S) registries for any hospital that was a recognized stroke center. The variables from the local GWTG-S registry case report included age, sex, race (White, Black or African American, other, or unable to determine/missing), ethnicity (Hispanic or non-Hispanic), past medical history, DTCT time, DTN time, time to endovascular thrombectomy (DTG), and National Institutes of Health Stroke Scale (NIHSS) score. Missing data from within the GWTG-S registry were manually extracted from the electronic health record when possible. The terms door-to-endovascular thrombectomy and door-to-groin (DTG) are used interchangeably in this manuscript. Door-to-thrombectomy is a broader term that can include door-to-groin puncture, door-to-device, door-to-first pass, or door-to-recanalization. Door-to-groin was the preferred variable; however, when this was missing, the door-to-first pass or door-to-device were used. Prehospital variables included age, sex, race, ethnicity, computer-aided dispatch times, primary and secondary impressions, vital signs, exam findings, and interventions performed prior to hospital arrival (including those items in the AHA guidelines and IV access). IV access was categorized as a binary variable (present or absent) for analysis. Because of incomplete and inconsistent documentation of unsuccessful prehospital IV access attempts, these data were not collected for analysis. AHA recommendations for prehospital stroke care include: (1) documentation of a stroke scale, (2) prenotification of receiving hospital when a stroke scale is positive, (3) blood glucose measurement, (4) 12-lead electrocardiogram, (5) supplemental oxygen for hypoxia (pulse oximetry < 94%), (6) documentation of LKW time, (7) less than 2 min from dispatch to being enroute, and (8) less than 15 min on scene (14, 22–24). Any acute intervention was defined as a patient receiving IVT and/or EVT.
Data analysis
Descriptive statistics characterized the cohort, reporting the number and proportion for categorical variables and mean, standard deviation, and median with interquartile range (IQR) for continuous variables. In cases where continuous variables were skewed or not normally distributed, we also reported the geometric mean with 95% confidence intervals (CI). For time-to variables, any time of 0 min was transformed to 0.5 min to allow for appropriate analysis and to account for the reasonable assumption that there would be a minimum of 30 s between the time a patient entered the emergency department and arrived at CT, even when a patient went straight to CT. Times were log transformed prior to analysis. Univariate analysis of those transported with or without IV therapy used chi-square or an ANOVA-type test on the log-transformed data to identify differences. Multivariable regression models, with random effects for hospital, were used to test the association between prehospital IV access and DTCT, DTN, or DTG times while controlling for stroke certification of the receiving hospital (CSC, PSC, ASRH, or not stroke certified), sex, age, initial NIHSS, documentation of a stroke scale, documentation of a blood glucose level, documentation of LKW, and completion of EMS prenotification. The model for DTG did not include stroke certification level as EVT could only be performed at a CSC. Analyses were performed on an available case basis. All analyses were performed using SAS 9.4 software.
Results
Demographics and patient characteristics
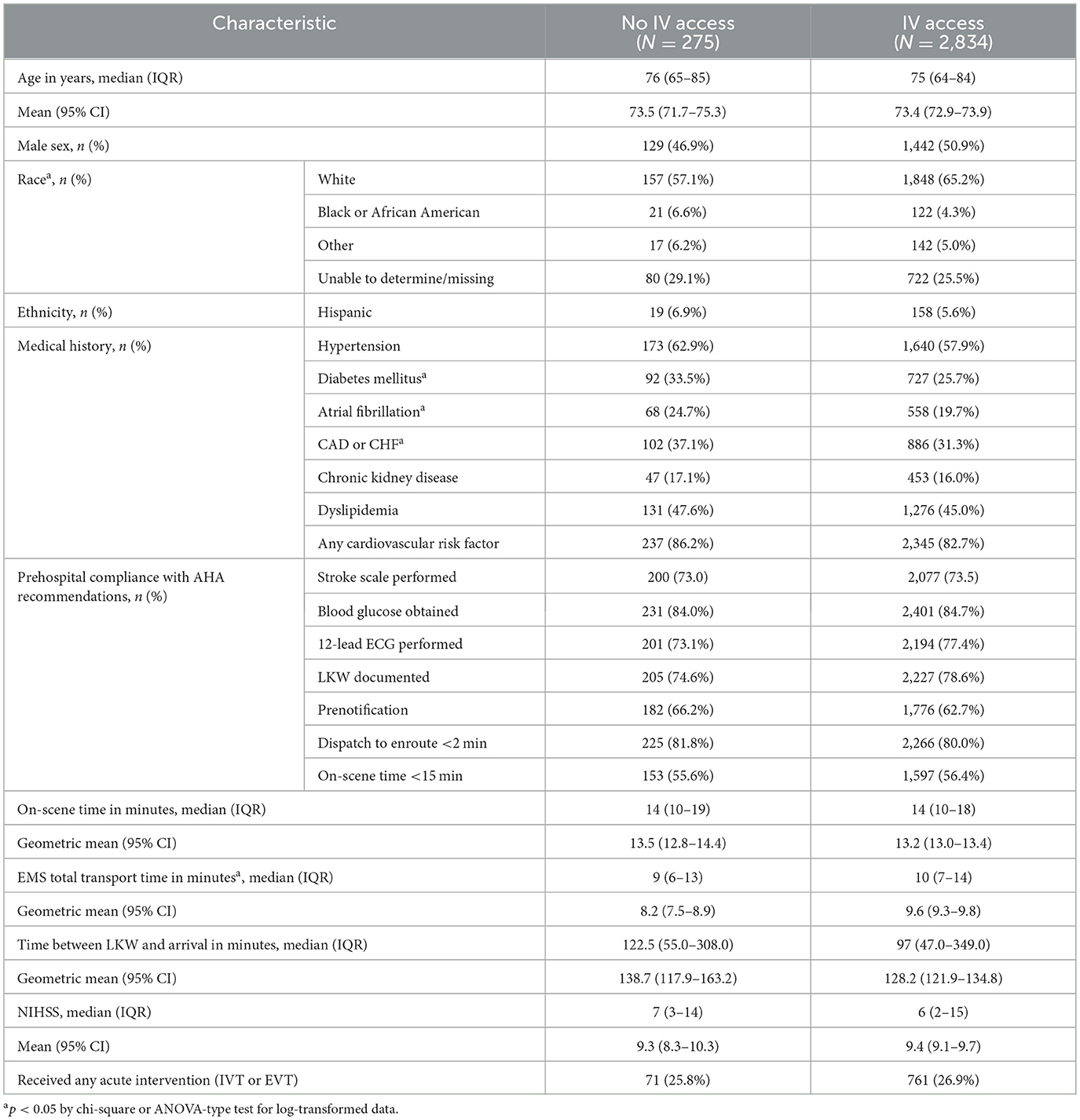
Within the study period, 3,109 patients were identified as meeting the inclusion criteria within the IMPACT network. IV access was obtained in 2,834 (91.2%) of patients. There was no difference in those with or without prehospital IV access in terms of sex, age, ethnicity, presence of any cardiovascular risk factor, or initial NIHSS score (Table 1). The overall study group was 49.5% female, with a median age of 75 years (IQR 64–84 years) and 5.7% Hispanic. There was a higher proportion of White patients among those with prehospital IV access (65.2%, n = 1,848) compared to those without prehospital IV access (57.1%, n = 157; p < 0.01). Of the patients who had an IV placed by an EMS clinician, 40.0% (n = 1,133) arrived with two or more points of IV access. There was no difference in on-scene time between those with IV access obtained by EMS (median 14 min, IQR 10–19 min) compared to those without prehospital IV access (median 14 min, IQR 10–19 min; p = 0.44), but the total transport time among those in whom IV access was obtained was longer than those in whom IV access was not obtained (with IV: median 10 min, IQR 7–14 min; without IV: median 9 min, IQR 6–13 min, p < 0.05).
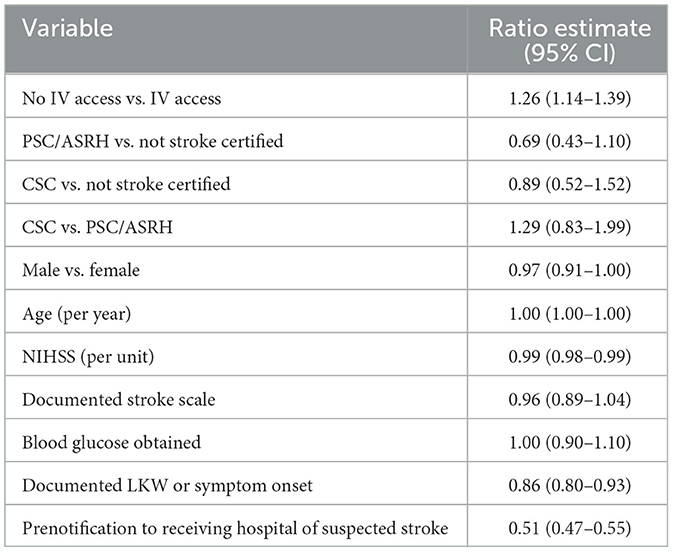
Prehospital IV access was associated with reduced door-to-CT times
Patients who arrived with prehospital IV access had a median DTCT time of 10 min (IQR 7–16 min; geometric mean 11.1 min, 95% CI, 10.7–11.6 min), whereas patients who arrived without prehospital IV access had a median DTCT time of 12 min (IQR 8–21 min; geometric mean 13.9 min, 95% CI, 12.5–15.6 min, p < 0.05). DTCT time was missing in 8% (n = 22) of encounters without prehospital IV access and 7.5% (n = 213) of encounters with prehospital IV access. These were excluded from the multivariable modeling. After controlling for variables determined a priori to impact DTCT time (stroke center certification level, sex, age, NIHSS score at admission, prehospital blood glucose level, documentation of LKW time, and prenotification to the receiving facility of suspected stroke), the lack of prehospital IV access was associated with a 26% increase in DTCT times compared to those who had IV access from the prehospital setting (ratio estimate 1.26, 95% CI, 1.14–1.39; Table 2). The adjusted geometric mean DTCT time among those without prehospital IV access was 15.9 min (95% CI, 12.8–19.7 min) while it was only 12.6 min (95% CI, 10.3–15.4 min) among those with prehospital IV access.
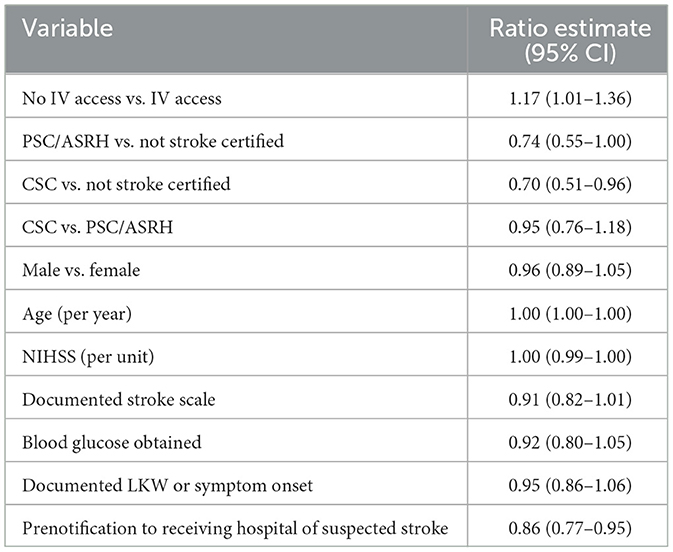
Prehospital IV access was associated with reduced door-to-intravenous thrombolytic times
Overall, 17.6% (n = 547) of all patients received IVT, of whom 92.7% (n = 507) arrived with prehospital IV access and 7.3% (n = 40) arrived without prehospital IV access. The median DTN in patients with prehospital IV access was 36 min (IQR 26–49 min; geometric mean 37.1 min, 95% CI, 35.5–38.8 min), which was similar to the median DTN time in patients without prehospital IV access (median 40 min, IQR 32–53 min; geometric mean 41.0 min, 95% CI, 36.0–46.7 min, p > 0.05). After controlling for variables determined a priori to impact DTN time (stroke center certification level, sex, age, NIHSS, prehospital blood glucose level, documentation of LKW time, and prenotification to the receiving facility of suspected stroke), arrival without prehospital IV access was associated with a 17% increase in DTN time compared to arrival with prehospital IV access (ratio estimate 1.17, 95% CI, 1.01–1.36; Table 3). The adjusted DTN geometric mean was 45.7 min (95% CI, 40.1–51.9 min) among those with prehospital IV access and 53.4 min (95% CI, 44.2–64.4 min) among those without prehospital IV access.
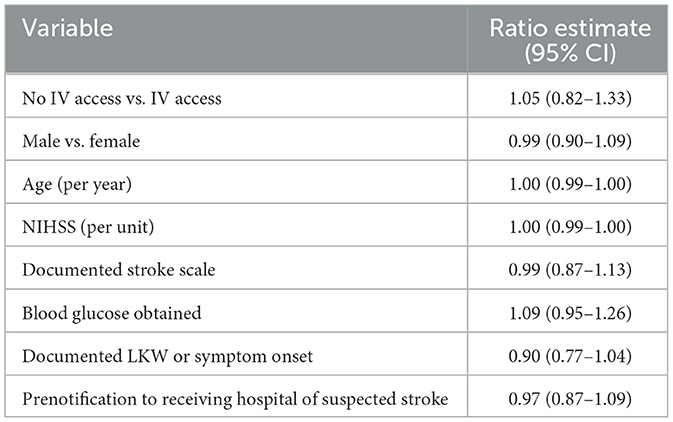
Prehospital IV access was not associated with reduced door-to-endovascular therapy times
Only 5.3% (n = 165) of all patients received EVT. Of these, 90.9% (n = 150) of patients arrived from the field with IV access and only 9.1% (n = 15) of patients arrived from the field without IV access. The DTG time of patients with prehospital IV access (median 91 min, IQR 79–115 min; geometric mean 94.2 min, 95% CI, 89.2–99.5 min) was similar to the DTG time of patients without prehospital IV access (median 92 min, IQR 80–137 min; geometric mean 102.1 min, 95% CI, 80.8–129.2 min, p > 0.05). Even after adjusting for sex, age, NIHSS score, EMS-documented stroke scale, and LKW, EMS-measured blood glucose level, and hospital prenotification of suspected stroke, prehospital IV access was not associated with DTG times (ratio estimate 1.05, 95% CI, 0.82–1.33; Table 4). The adjusted geometric mean DTG time was similar in both those with and without prehospital IV access (with IV: 102.6 min, 95% CI, 78.7–133.7 min; without IV: 107.2 min, 95% CI, 78.7–146.2 min).
Discussion
In this analysis, the presence of prehospital IV access was associated with decreased time to CT and time to IVT but not with change in time to EVT. On average, we observed an approximate time saving of 3 min in door-to-CT times (12.6 vs. 15.9 min) for patients with IV access obtained in the prehospital setting compared to those arriving without an IV. This time saving increased to almost 8 min when looking at time to thrombolytic administration (45.7 vs. 53.4 min). While not found to be statistically significant in this study's dataset, a similar time saving was noted in the time to EVT of approximately 5 min (102.6 vs. 107.2 min).
It is important to note that institutional protocols vary with regard to the necessity of IV access prior to CT imaging in patients with suspected stroke. While the priority imaging is a non-contrast CT head, vascular access is critical for vascular imaging to assess for large vessel occlusions and the need for EVT, and for the administration of medications, including antihypertensives and thrombolytics. For this reason, it is the expectation at facilities in our network that patients have IV access prior to CT imaging. However, in select cases where obtaining IV access appears to significantly delay imaging (at the discretion of providers), IV access may be temporarily forgone, and the treating team may prioritize non-contrasted imaging prior to IV access. In these cases, our results could be less applicable.
It is known that on-scene time accounts for nearly half of the total alarm-to-door time (time from dispatch to arrival at the hospital) for EMS calls (25). While transport time is difficult to influence, prehospital stroke management should continue to minimize on-scene time, a task some systems are approaching with scene time limits (26). In the study presented here, there were no differences in the on-scene time between patients arriving with or without prehospital IV access, but transport times were longer in encounters where prehospital IV access was obtained. While this study was not designed to evaluate causality, it is unlikely that obtaining IV access results in longer transport times. Rather, we suspect longer transport times allow for a greater likelihood of being able to obtain IV access in the prehospital setting. Additionally, EMS clinicians need to be cognizant of the fact that time saved in hospital by having an IV in place upon arrival could easily be negated by lengthened on-scene times. This highlights the importance of using the fixed transport time to perform the most high-yield interventions, as long as no immediate life threats are identified on scene that require intervention.
When we consider the time required to obtain and secure IV access, especially in time-sensitive, high-pressure situations, 3–8 min of time saved between emergency department arrival and either CT or IVT is potentially clinically significant. This study was not designed to evaluate the clinical implications of this degree of time savings in terms of patient outcomes. However, every minute faster to IVT results in an additional day of disability-free life and every minute faster to EVT means an additional week of functional independence (27–29). Therefore, these data support the idea that minutes do count, and time really is brain.
Hospitals continue to streamline their processes for rapid evaluation and management of patients with suspected stroke. This includes interventions, such as prehospital stroke alerts, patients being transported directly to CT from the ambulance bay, and pharmacists standing by with thrombolytics at the ready. Prehospital IV access can also aid in these processes and can now be added to the shortlist of prehospital interventions with meaningful impacts on time to imaging and acute interventions (i.e., hospital prenotification of suspected stroke, obtaining a blood glucose level, and documenting a LKW) (15–21).
In the era of electronic patient care reports, prehospital providers are tasked with performing and documenting a myriad interventions on all patient transports. Furthermore, it is nearly impossible to recognize all potential stroke patients and perform all the AHA recommendations for prehospital stroke care, especially considering the average time from patient contact to hospital arrival is less than 25 min. To ensure high-quality care in these time-limited conditions, emphasizing IV access in addition to other critical elements of stroke care may be challenging. Feedback systems represent one method of increasing compliance with the recommendations for prehospital stroke care. Hospital feedback to EMS clinicians caring for patients with confirmed ischemic strokes improved compliance with state protocols, including prehospital IV access—IV access obtained by EMS clinicians increased from 76.1 to 84.9% of encounters after the implementation of a focused feedback program (30). Beyond EMS clinician feedback, EMS medical directors will need to support prehospital providers in prioritizing tasks and provide the rationale behind these priorities. Together, this can help streamline acute stroke care and, perhaps, ultimately improve patient outcomes.
Limitations
There were several limitations of this retrospective study. While groups arriving with and without IV access were quite comparable, we did note that patients arriving with IV access were more likely to be White than those arriving without IV access. While this study was not structured to speculate as to the causality of this, it highlights an important racial difference and may demonstrate bias within the prehospital system. Further studies are needed to investigate the systemic drivers of this disparity. Another limitation is the inconsistent documentation of patients' home medications, including anticoagulation, which is an especially pertinent piece of information when weighing risk of thrombotic and hemorrhagic events, as well as eligibility for intervention on hospital arrival. Additionally, EMS records did not consistently report the IV size or location. Not all forms of IV access can be used for advanced imaging, such as CT-perfusion scans. While evaluation of the association between door-to times and arrival with a form of IV access that can be used for both advanced imaging and administration of thrombolytics is ideal, this study was limited to binary evaluation based only on the presence or absence of any form of prehospital IV access. Additionally, differences in hospital CT protocols regarding the size and location of an IV that is acceptable for contrasted CT head and neck imaging also make identifying an “optimal” IV placement challenging.
Additionally, thrombolytic administration can be delayed due to the need for acute control of hypertension. Our dataset did not include data about patients requiring IV antihypertensives, which could modify our results, though the directionality of this possible effect modification is unclear. While this would cause a delay in thrombolytic administration, the presence of prehospital IV access could allow for more expeditious delivery of antihypertensives and could thus potentiate the results of our study. There were also low outcomes of interest in the cohorts receiving IVT or EVT, as compared to the overall cohort, thereby limiting the ability to detect a small but significant association between prehospital IV access and time to EVT. Despite these limitations, this study provides insight into the association between prehospital IV access and patient care and outcomes in acute stroke.
Conclusions
This study demonstrates an association between prehospital IV access and a shorter time to both CT imaging and IVT administration. However, obtaining prehospital IV access was not associated with a shorter time to EVT. Given the time savings implied by these findings for time to imaging and IVT, future work with medical directors and prehospital systems should explore ways to prioritize IV access during transport for patients with suspected stroke without extending the total time between arrival at the patient and transfer of care to the emergency department.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, in de-identified form and upon reasonable request; the data are not publicly available.
Ethics statement
The studies involving humans were approved by the Colorado Multi-Institutional Review Board (COMIRB#23-1035). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
GS: Conceptualization, Data curation, Visualization, Writing – original draft, Writing-review and editing. CW: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DN: Data curation, Project administration, Supervision, Writing – review & editing. IE: Data curation, Writing – review & editing. ML-V: Data curation, Writing – review & editing. BT: Data curation, Writing – review & editing. JD: Data curation, Writing – review & editing. SS: Formal analysis, Methodology, validation, Writing – review & editing. AF: Project administration, Supervision, Writing – review & editing. ML: Project administration, Supervision, Writing – review & editing. EM: Data curation, Investigation, Writing – review & editing. LD: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. University of Colorado IMPACT Research Fund (Anonymous Donor). The use of REDCap was supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535.
Acknowledgments
This work was presented at the National Association of EMS Physicians Annual Meeting on January 10th, 2025, in San Diego, California. We would like to thank all members of the IMPACT research collaboration who contributed data from and provided care to the patients included in this study.
Conflict of interest
LD reports grant money to Yale University School of Medicine to conduct research conceived and sponsored by TETMedical, Inc. CW reports serving as a consultant for Analog Devices, Inc., a company involved in the development of healthcare technology. This relationship is outside of the submitted work.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/femer.2025.1692565/full#supplementary-material
References
1. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
2. Saver JL. Time is brain—quantified. Stroke. (2006) 37:263–6. doi: 10.1161/01.STR.0000196957.55928.ab
3. Fonarow GC, Smith EE, Saver JL, Reeves MJ, Hernandez AF, Peterson ED, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. (2011) 123:750–8. doi: 10.1161/CIRCULATIONAHA.110.974675
4. Saver JL, Fonarow GC, Smith EE, Reeves MJ, Grau-Sepulveda MV, Pan W, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. (2013) 309:2480. doi: 10.1001/jama.2013.6959
5. Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. (2012) 379:2364–72. doi: 10.1016/S0140-6736(12)60738-7
6. Sadeghi-Hokmabadi E, Taheraghdam A, Hashemilar M, Rikhtegar R, Mehrvar K, Rasi Marzaki Y, et al. Simple in-hospital interventions to reduce door-to-CT time in acute stroke. Int J Vascu Med. (2016) 2016:1656212. doi: 10.1155/2016/1656212
7. Adeoye O, Lindsell C, Broderick J, Jauch E, Khoury J, Moomaw CJ, et al. Emergency medical services use by stroke patients: a population-based study. Am J Emerg Med. (2009) 27:141–5. doi: 10.1016/j.ajem.2008.02.004
8. Asaithambi G, Tong X, Lakshminarayan K, Coleman King SM, George MG, Odom EC. Emergency medical services utilization for acute stroke care: analysis of the Paul Coverdell National Acute Stroke Program, 2014–2019. Prehosp Emerg Care. (2022) 26:326–32. doi: 10.1080/10903127.2021.1877856
9. Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, et al. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get With the Guidelines-Stroke. Circulation. (2013) 6:262–9. doi: 10.1161/CIRCOUTCOMES.113.000089
10. Patel MD, Rose KM, O'Brien EC, Rosamond WD. Pre-hospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina stroke care collaborative. Stroke. (2011) 42:2263–8. doi: 10.1161/STROKEAHA.110.605857
11. Zhelev Z, Walker G, Henschke N, Fridhandler J, Yip S. Prehospital stroke scales as screening tools for early identification of stroke and transient ischemic attack. Cochrane Database Syst Rev. (2019) 4:CD011427. doi: 10.1002/14651858.CD011427.pub2
12. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Stroke. (2000) 31:71–6. doi: 10.1161/01.STR.31.1.71
13. Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati prehospital stroke scale: reproducibility and validity. Ann Emerg Med. (1999) 33:373–8. doi: 10.1016/S0196-0644(99)70299-4
14. Zachrison KS, Nielsen VM, de la Ossa NP, Madsen TE, Cash RE, Crowe RP, et al. Prehospital stroke care part 1: emergency medical services and the stroke systems of care. Stroke. (2023) 54:1138–47. doi: 10.1161/STROKEAHA.122.039586
15. Bae H-J, Kim D-H, Yoo N-T, Choi JH, Hwang Y, Cha JK. Prehospital notification from the emergency medical service reduces the transfer and intra-hospital processing times for acute stroke patients. J Clin Neurol. (2010) 6:138–42. doi: 10.3988/jcn.2010.6.3.138
16. Kim SK, Lee SY, Bae HJ, Lee YS, Kim JM, Moon HS, et al. Pre-hospital notification reduced the door-to-needle time for IV t-PA in acute ischaemic stroke. Eur J Neurol. (2009) 16:1331–5. doi: 10.1111/j.1468-1331.2009.02762.x
17. Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. (2012) 5:514–22. doi: 10.1161/CIRCOUTCOMES.112.965210
18. Nielsen VM, DeJoie-Stanton C, Song G, Christie A, Guo J, Zachrison KS. The association between presentation by EMS and EMS prenotification with receipt of intravenous tissue-type plasminogen activator in a state implementing stroke systems of care. Prehosp Emerg Care. (2020) 24:319–25. doi: 10.1080/10903127.2019.1662862
19. Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehosp Emerg Care. (2008) 12:426–31. doi: 10.1080/10903120802290828
20. McKinney JS, Mylavarapu K, Lane J, Roberts V, Ohman-Strickland P, Merlin MA. Hospital prenotification of stroke patients by emergency medical services improves stroke time targets. J Stroke Cerebrovasc Dis. (2013) 22:113–8. doi: 10.1016/j.jstrokecerebrovasdis.2011.06.018
21. Dylla L, Rice JD, Poisson SN, Tozer Fink KR, Zlupko G, Madsen TE, et al. Analysis of stroke care among 2019–2020 National Emergency Medical Services Information System encounters. J Stroke Cerebrovasc Dis. (2022) 31:106278. doi: 10.1016/j.jstrokecerebrovasdis.2021.106278
22. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
23. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2013) 44:870–947. doi: 10.1161/STR.0b013e318284056a
24. Glober NK, Sporer KA, Guluma KZ, Serra JP, Barger JB, Brown JF, et al. Acute stroke: current evidence-based recommendations for prehospital care. West J Emerg Med. (2016) 17:104–28. doi: 10.5811/westjem.2015.12.28995
25. Simonsen SA, Andresen M, Michelsen L, Viereck S, Lippert FK, Iversen HK. Evaluation of pre-hospital transport time of stroke patients to thrombolytic treatment. Scand J Trauma Resusc Emerg Med. (2014) 22:65. doi: 10.1186/s13049-014-0065-z
26. Patel MD, Brice JH, Moss C, Suchindran CM, Evenson KR, Rose KM, et al. An evaluation of emergency medical services stroke protocols and scene times. Prehosp Emerg Care. (2014) 18:15–21. doi: 10.3109/10903127.2013.825354
27. Kunz WG, Hunink MG, Almekhlafi MA, Menon BK, Saver JL, Dippel DWJ, et al. Public health and cost consequences of time delays to thrombectomy for acute ischemic stroke. Neurology. (2020) 95:e2465–75. doi: 10.1212/WNL.0000000000010867
28. Meretoja A, Keshtkaran M, Saver JL, Tatlisumak T, Parsons MW, Kaste M, et al. Stroke thrombolysis: save a minute, save a day. Stroke. (2014) 45:1053–8. doi: 10.1161/STROKEAHA.113.002910
29. Meretoja A, Keshtkaran M, Tatlisumak T, Donnan GA, Churilov L. Endovascular therapy for ischemic stroke: save a minute—save a week. Neurology. (2017) 88:2123–7. doi: 10.1212/WNL.0000000000003981
Keywords: prehospital, emergency medical services, stroke, cerebrovascular accident, intravenous access, TIA, thrombolysis, thrombectomy
Citation: Sowitz G, D. Wham C, Nicke D, Espinoza I, Lensink-Vasan M, Thrower B, Duenas J, Sillau S, Farcas A, Leppert M, Molina Kuna E and Dylla L (2025) Prehospital intravenous access is associated with decreased door-to-computed tomography and door-to-intravenous thrombolysis time, but not door-to-endovascular therapy time. Front. Disaster Emerg. Med. 3:1692565. doi: 10.3389/femer.2025.1692565
Received: 25 August 2025; Accepted: 31 October 2025;
Published: 26 November 2025.
Edited by:
David Häske, University of Tübingen, GermanyReviewed by:
Bernardo Liberato, Emory University, United StatesDaian Popa, University of Medicine and Pharmacy “Victor Babes” Timisoara, Romania
Copyright © 2025 Sowitz, D. Wham, Nicke, Espinoza, Lensink-Vasan, Thrower, Duenas, Sillau, Farcas, Leppert, Molina Kuna and Dylla. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Layne Dylla, TGF5bmUuRHlsbGFAeWFsZS5lZHU=
†ORCID: Geoffrey Sowitz orcid.org/0000-0002-7393-7369
Courtney D. Wham orcid.org/0009-0003-0359-5118
Daria Nicke orcid.org/0009-0008-1320-3962
Ian Espinoza orcid.org/0009-0006-1758-7401
Stefan Sillau orcid.org/0000-0002-8691-3139
Andra Farcas orcid.org/0000-0002-7229-447X
Michelle Leppert orcid.org/0000-0002-0679-7634
Elizabeth Molina Kuna orcid.org/0000-0001-9548-9141
Layne Dylla orcid.org/0000-0002-5664-779X
†These authors have contributed equally to this work
 Geoffrey Sowitz
Geoffrey Sowitz Courtney D. Wham
Courtney D. Wham Daria Nicke1‡
Daria Nicke1‡ Stefan Sillau
Stefan Sillau Layne Dylla
Layne Dylla