- 1Department of Nutrition and Dietetics with Clinic of Metabolic Diseases and Gastroenterology, Institute of Food and Nutrition, Warsaw, Poland
- 2Department of Neonatology, Mazovian Brodnowski Hospital, Warsaw, Poland
- 3Clinic of Obstetrics, Gynecology and Oncology, 2nd Faculty of Medicine, Medical University of Warsaw, Warsaw, Poland
Introduction: Vitamin D deficiency in pregnant women may result in reduced neonatal development due to the fact that systemic vitamin D status during fetal life depends on maternal concentrations. Some authors reported significant differences in neonatal anthropometric measurements depending on maternal vitamin D concentrations.
Objective: The aim of this study is to evaluate the relationship between maternal and cord blood concentrations of vitamin D and neonatal anthropometric measurements at birth.
Materials and methods: This study included 94 pregnant women, at term, who delivered at the Department of Obstetrics, Women’s Diseases and Gynecological Oncology, Medical University of Warsaw. Total serum 25(OH)D concentration was measured in mother–child pairs, and newborn anthropometric data were collected. A multiple regression analysis was used for statistical analysis.
Results: No relationship between maternal and neonatal cord blood vitamin D concentrations vs. neonatal weight, length, head, and chest circumference at birth was found (p > 0.05). Severe vitamin D deficiency (<10 ng/ml) was detected in 10.6%, deficiency (10–20 ng/ml) in 39.4%, insufficiency (20–30 ng/ml) in 39.4%, and optimal vitamin D concentration (>30 ng/ml) only in 10.6% of the pregnant women. Cord blood vitamin D deficiency (<20 ng/ml) was found in 28.7% of the neonates.
Conclusion: No differences between neonatal anthropometric measurements of infants born to mothers with normal and deficient vitamin D concentrations were found.
Introduction
Vitamin D is responsible for a number of important functions in the fetus, and vitamin D blood saturation in the neonate is directly dependent on maternal levels. Vitamin D insufficiency in the mother results in neonatal insufficiency (1, 2), which may negatively affect the anthropometric parameters in the neonate, skeletal calcium score, the immune system, and increase the risk for asthma and type 1 diabetes in later life (3–5).
Currently, the recommended intake of vitamin D and its optimal concentration in the body are the source of much heated debate among medical researchers (6, 7). The American Academy of Pediatrics recommends that serum concentration of 25(OH)D in maternal blood be more than 32 ng/ml (8). In light of various reports, the general consensus is that it should exceed 30 ng/ml (9, 10). However, some experts are of the opinion that maternal levels of at least >20 ng/ml will ensure adequate vitamin D concentration in the neonate (11), while latest publications suggest that 25(OH)D concentration should be at least 40 ng/ml (2). With 30 ng/ml as the threshold value for adequate concentration, vitamin D insufficiency or deficiency is a common occurrence, affecting as many as 99–100% of pregnant women in Turkey (12, 13), 85% in India (14), 69–95% in Central Europe (15–17), 52–85% in Southern Europe (18, 19), 74% in the United States (20), and 63% in China (21). The contemporary lower reference range for cord blood vitamin D level is 20 ng/ml (1, 22). However, as in the case of maternal levels, there is no consensus regarding the optimal concentrations (23–26). The literature reports unanimously agree that cord blood serum concentration of vitamin D is directly correlated with maternal levels. Regardless, cord levels may be higher (24, 27–29), equal to (12, 14, 19), and lower than maternal venous vitamin D concentration (30, 31). Neonates born to mothers with adequate vitamin D concentrations during pregnancy are supplied until 8 weeks of life (2, 32). The contemporary literature questions whether the dose of vitamin D routinely administered to all newborns in the first weeks after birth should depend on the maternal concentrations and infant weight (3, 23).
The aim of this study is to evaluate the relationship between maternal and cord blood vitamin D concentrations and the anthropometric parameters of the newborn (weight, length, and head and chest circumference) as well as the Apgar score.
Materials and Methods
Study Design
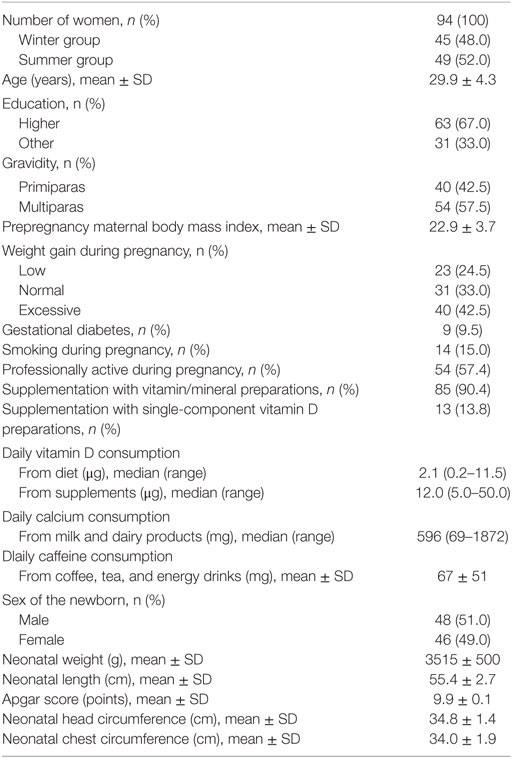
The cross-sectional study was conducted among 100 pregnant women at the Department of Obstetrics, Gynecology and Oncology, Medical University of Warsaw. The study included women who delivered during two extreme seasons as far as exposure to sun is concerned (winter–summer) to investigate the widest range of vitamin D concentrations in the body. The winter group comprised women who delivered between December 2014 and February 2015, whereas the summer group included women who delivered between July and August 2015. This study included women who presented at the hospital on weekdays in the morning. The exclusion criteria were as follows: non-Polish nationality, multiple gestation, advanced stage of labor, chronic maternal diseases before pregnancy, and threatened course of labor. Informed written consent was obtained. Maternal blood was drawn after admission to the delivery ward (at the same time when blood was drawn for diagnostic purposes), and cord blood was drawn at delivery. Samples were immediately delivered to the hospital laboratory. Only term deliveries (94 patients: 45 from the winter group and 49 from the summer group) were included into the analysis. The Ethics Committee of the Institute of Food and Nutrition approved of the study (Code 10/162/KB/2014). Maternal and neonatal characteristics are presented in Table 1.
Laboratory Analysis and Data Collection
Total 25(OH)D [25(OH)D2 and 25(OH)D3] concentrations were measured in the blood using immunological tests (LIAISON® 25 OH Vitamin D TOTAL Assay; DiaSorin). The lower detection threshold for vitamin D is 4.0 ng/ml. The intraassay and interassay CV were <8% and <11%, respectively. Neonatal data (sex, weight, length, Apgar score at 5 min, and head and chest circumference) were obtained from the hospital medical records. The anthropometric measurements were taken by the midwives immediately upon delivery. Weight was measured using a physician beam scale. The remaining measurements were taken with the use of a tape measure. The total neonatal length was measured from the vertex of the head to the soles (with the feet kept vertical at 90°). The occipital–frontal head circumference (tape was placed on the maximum protrusion of the occipital and supraorbital ridges) and the chest circumference (tape was placed horizontally on the sternum and lower tip of the shoulder blade) were measured. A Food Frequency Questionnaire, validated at the Institute of Food and Nutrition, was used to assess vitamin D, calcium, and caffeine consumption during the entire course of pregnancy. To precisely evaluate portion size, direct interviewing (face-to-face) and the “Photo Album of Meals and Products” were used for data collection. The questionnaire also included data on supplementation, patient lifestyle, and weight gain. As advised by the American Institute of Medicine, the recommended weight gain for pregnant women is 12.5–18 kg for underweight, 11.5–16 kg for normal weight, 7.0–11.5 kg for overweight, and 5–9 for obese women (33). These values were also used in our study. Lower or higher weight gain was considered as insufficient or excessive. The nutritional status was estimated using the body mass index (BMI). The content of vitamin D in vitamin/mineral supplements for pregnant women, as well as single-component vitamin D preparations, was estimated based on our earlier analysis (34). As many as 75% of the multicomponent supplements for pregnant women, which are available in Poland, contain a small amount of vitamin D (5–10 µg). Only single-component preparations contain larger amount of vitamin D (mean, 25 µg). The following criteria of maternal serum 25(OH)D concentrations were used: recommended level, >30 ng/ml; insufficiency, 20–30 ng/ml; deficiency, 10–20 ng/ml; and severe deficiency, <10 ng/ml (9, 27). As for cord blood, in accordance with the current recommendations of some experts, the concentration of ≥20 ng/ml was treated as the recommended level, whereas <12 ng/ml signified severe deficiency (1, 22).
Statistical Analysis
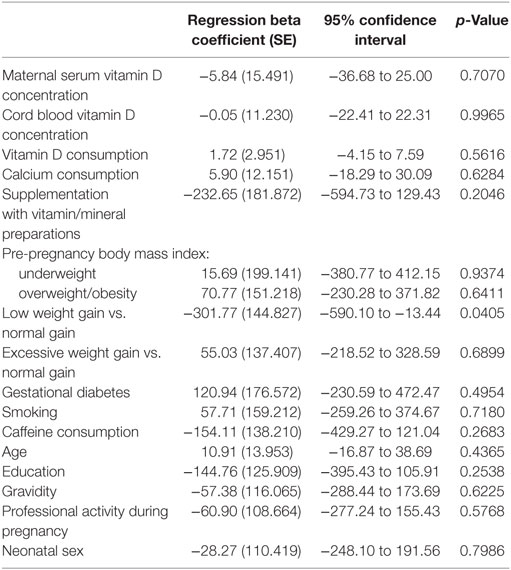
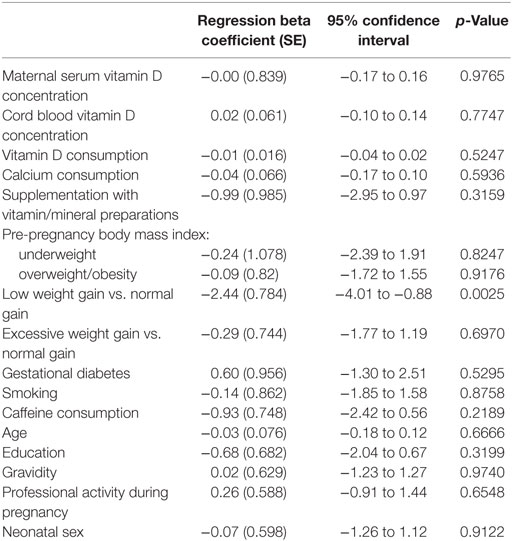
A multiple regression analysis was used to investigate a possible relationship between selected baseline characteristics (serum vitamin D concentration, vitamin D and calcium consumption, gravidity, maternal age and education, prepregnancy BMI, weight gain during pregnancy, smoking, caffeine consumption, use of dietary supplements, professional activity during pregnancy, gestational diabetes, and sex of the neonate) and neonatal weight, length, and head and chest circumference. p < 0.05 was considered as statistically significant.
Results
Overall, severe vitamin D deficiency (<10 ng/ml) was detected in 10 (10.6%), deficiency (10–20 ng/ml) in 37 (39.4%), insufficiency (>20–30 ng/ml) in 37 (39.4%), and optimal vitamin D concentration (>30 ng/ml) only in 10 (10.6%) pregnant women. The neonates had higher levels of vitamin D than the mothers (mean, 27.0 ± 11.1 ng/ml vs. 19.5 ± 7.8 ng/ml). As a consequence, vitamin D deficiency (<20 ng/ml) and severe deficiency (<12 ng/ml) were found in 27 (28.7%) and 9 (9.6%) cases, respectively.
No relationship between maternal and cord blood vitamin D concentrations and neonatal anthropometric measurements at birth (weight, length, and head and chest circumference) was found (p > 0.05). Due to the fact that mean Apgar score was close to the optimal values (9.9 points), that parameter was not included in the statistical analysis. Neontal somatic development was good in all neonates. No statistically significant differences were found between neonatal anthropometric parameters in the winter and summer groups although vitamin D concentrations were higher in the summer compared to the winter group [mean, 22.2 ± 6.5 ng/ml vs. 16.3 ± 8.0 ng/ml (p = 0.0003) for the mothers and 31.3 ± 9.4 ng/ml vs. 22.0 ± 11.0 ng/ml (p = 0.0001) for the neonates]. Weight gain during pregnancy was the only factor that proved to be associated with neonatal body weight and length. Children born to mothers whose weight gain in pregnancy was lower than the recommendations were 302 g lighter (p = 0.0405) and 2.4 cm shorter (p = 0.0025), compared to infants born to mothers with normal weight gain (Tables 2 and 3).
Discussion
In our study, we found no association between vitamin D status and the somatic development of the newborns. Despite the fact that maternal vitamin D levels were diverse (minimum, 4 ng/ml; maximum, 37.7 ng/ml), no relationship between any of the investigated anthropometric parameters and maternal values was found. Also, regardless of the fact that predelivery maternal concentrations of vitamin D were too low in approximately 90% of the women, the overall condition of the neonates was good, even in cases classified as “severely deficient in vitamin D” (<10 ng/ml in maternal and <12 ng/ml in cord blood). Lack of a relationship between maternal vitamin D concentrations and neonatal measurements in Poland was reported by Skowrońska-Jóźwiak et al., although their study focused on insufficiently low vitamin D concentrations, which were confirmed in almost 69% of mothers of term infants (16). As for data from other countries, Rodriguez et al. and Eggemoen et al. found no connection between neonatal anthropometric parameters and maternal vitamin D levels, even despite the fact that vitamin D deficiency (<20 ng/ml) was detected in 19.7% and 51% of the women, respectively (18, 35). Loudyi et al. reported no association between maternal vitamin D status and neonatal weight at birth among the investigated women (vitamin D concentration ≤20 ng/ml in 90% of the cases) (36). Shakiba and Iranmanesh and Josefson et al. found no relationship between cord vitamin D concentration and neonatal weight and length (25, 31), while Dalgård et al. reported the same lack of relationship for neonatal weight and head circumference (37).
Nevertheless, some authors have postulated the existence of such a relationship and reported significant differences in neonatal size depending on vitamin D concentrations. An Indian study has demonstrated lower weight (by 480 g), length (by 9.5 cm), and head and chest circumference (by 4.5 and 4.8 cm, respectively) in neonates born to mothers with vitamin D deficiency compared to the recommended levels (14). Nobles et al. found a smaller difference (by 176 g) in the weight of infants born to mothers with vitamin D deficiency in the United States (20). As for cord blood, yet another study reported decreased neonatal length (by 0.5 cm) in a group of children with very low vitamin D concentrations (<4.8 ng/ml) compared to the recommended levels (37). Interesting results were reported by Lykkedegn et al., who demonstrated a U-shaped association between neonatal weight at birth and cord blood vitamin D concentrations. A significant weight gain was observed after the concentration values exceed 24 ng/ml (38).
In light of the conflicting data from individual studies, meta-analyses seem to be the most valuable sources of information. A meta-analysis of observational studies has indicated that lowered maternal vitamin D concentration (<15 ng/ml) results in lower neonatal weight at birth (by 131 g), but has no impact on the length and head circumference (6). Another meta-analysis has concluded that maternal vitamin D concentration of <20 ng/ml increases the risk for small-for-gestational age infant (39).
The conclusions on the effects of vitamin D supplementation during pregnancy are also conflicting. A meta-analysis of randomized clinical trials has found that vitamin D supplementation during pregnancy increases neonatal weight and length but does not affect the course of pregnancy. However, these authors emphasize the need for further studies to obtain more conclusive results (40). Harvey et al., in a systematic review, claimed that the available literature reports are not sufficient to confirm the existence of a relation between vitamin D concentration and neonatal condition at birth, or even to recommend obligatory vitamin D supplementation in pregnant women (7).
The results of our study did not reveal deteriorated neonatal condition at birth among children born to mothers with low vitamin D levels compared to optimal concentrations. Nevertheless, several limitations might have biased the final results, especially the fact that the analysis of vitamin D level was a single test and was conducted on the day of the delivery, which does not signify that the concentration was typical for the entire course of pregnancy or at least its significant part. The second limitation of our study was a relatively small sample size, which was the result of the number of deliveries at the Clinic and the nature of the study, i.e., the winter–summer group, so caution is advised when formulating final conclusions.
Conclusion
Our study did not demonstrate a relationship between the anthropometric features of the neonates and maternal and cord blood vitamin D levels. In the absence of differences in neonatal condition between infants born to mothers with vitamin D deficiency and with adequate levels, it seems safe to conclude that the currently recommended vitamin D levels in pregnant women (>30 ng/ml) do not need to be reached to ensure proper fetal growth. Regardless, vitamin D performs various essential functions in the human body, some of which remain to be fully elucidated, so its concentration during pregnancy should not only be perceived through neonatal anthropometric measurements but also be perceived through long-term development and health condition of the children.
Ethics Statement
This study was carried out in accordance with the recommendations of the Ethics Committee of the Institute of Food and Nutrition approved of the study (Code 10/162/KB/2014) with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Ethics Committee of the Institute of Food and Nutrition.
Author Contributions
RW conceived the idea for the study. RW, MJ, and WS contributed to the design of the research. RW, MK-N, MT, MB, and MS-S collected the data. RW and MK-N analyzed the data and wrote the paper. All authors edited and approved the final version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer JK and handling editor declared their shared affiliation.
Acknowledgments
The authors wish to express their sincere gratitude to the management and personnel of Zakład Diagnostyki Laboratoryjnej, Mazowiecki Szpital Bródnowski, in Warsaw, for their invaluable help and assistance.
References
1. Kiely M, O’Donovan SM, Kenny LC, Hourihane JO, Irvine AD, Murray DM. Vitamin D metabolite concentrations in umbilical cord blood serum and associations with clinical characteristics in large prospective mother-infant cohort in Ireland. J Steroid Biochem Mol Biol (2017) 167:162–8. doi:10.1016/j.jsbmb.2016.12.006
2. Hollis BW, Wagner CL. New insights into the vitamin D requirements during pregnancy. Bone Res (2017) 5:17030. doi:10.1038/boneres.2017.30
3. Marshall I, Mehta R, Petrova A. Vitamin D in the maternal-fetal-neonatal interface: clinical implications and requirements for supplementation. J Matern Fetal Neonatal Med (2013) 26:633–8. doi:10.3109/14767058.2012.746306
4. Kaushal M, Magon N. Vitamin D in pregnancy: a metabolic outlook. Indian J Endocrinol Metab (2013) 17:76–82. doi:10.4103/2230-8210.107862
5. Thorne-Lyman A, Fawzi W. Vitamin D during pregnancy and maternal, neonatal and infant health outcomes: a systematic review and meta-analysis. Pediatr Perinat Epidemiol (2012) 26:75–90. doi:10.1111/j.1365-3016.2012.01284.x
6. Aghajafari F, Nagulesapillai T, Ronksley PE, Tough SC, O’Beirne M, Rabi DM. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. BMJ (2013) 346:f1169. doi:10.1136/bmj.f1169
7. Harvey NC, Holroyd C, Ntani G, Javaid K, Cooper P, Moon R, et al. Vitamin D supplementation in pregnancy: a systematic review. Health Technol Assess (2014) 45:1–190. doi:10.3310/hta18450
8. Wagner CL, Greer FR, American Academy of Pediatrics Section on Breastfeeding, American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics (2008) 122:1142–52. doi:10.1542/peds.2008-1862
9. Płudowski P, Karczmarewicz E, Bayer M, Carter G, Chlebna-Sokół D, Czech-Kowalska J, et al. Practical guidelines for the supplementation of vitamin D and the treatment of deficits in Central Europe – recommended vitamin D intakes in the general population and groups at risk of vitamin D deficiency. Endokrynol Pol (2013) 64:319–27. doi:10.5603/EP.2013.0012
10. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab (2011) 96:1911–30. doi:10.1210/jc.2011-0385
11. Streym VS, Moller KU, Rejnmark L, Heickendorff L, Mosekilde L, Vestergaard P. Maternal and infant vitamin D status during the first 9 months of infant life – a cohort study. Eur J Clin Nutr (2013) 67:1022–8. doi:10.1038/ejcn.2013.152
12. Halicioglu O, Aksit S, Koc F, Sezin A, Akman SA, Albudak E, et al. Vitamin D deficiency in pregnant woman and their neonates in spring time in western Turkey. Paediatr Perinat Epidemiol (2012) 26:53–60. doi:10.1111/j.1365-3016.2011.01238.x
13. Kılıcaslan AÖ, Kutlu R, Kilinc I, Ozberk DI. The effects of vitamin D supplementation during pregnancy and maternal vitamin D levels on neonatal vitamin D levels and birth parameters. J Matern Fetal Neonatal Med (2017) 25:1–8. doi:10.1080/14767058.2017.1326897
14. Sathish P, Raveendran S, Padma R, Balakrishnan D, Muthusami M. Correlation between maternal and neonatal blood vitamin D levels and its effect on the newborn anthropometry. Int J Reprod Contracept Obstet Gynecol (2016) 5:2983–8. doi:10.18203/2320-1770.ijrcog20162821
15. Gellert S, Ströhle A, Bitterlich N, Hahn A. Higher prevalence of vitamin D deficiency in German pregnant women compared to non-pregnant women. Arch Gynecol Obstet (2017) 296:43–51. doi:10.1007/s00404-017-4398-5
16. Skowrońska-Jóźwiak E, Lebiedzińska K, Smyczyńska J, Lewandowski KC, Głowacka E, Lewiński A. Effects of maternal vitamin D status on pregnancy outcomes, health of pregnant women and their offspring. Neuroendocrinol Lett (2014) 35:367–72.
17. Domaracki P, Sadlecki P, Odrowąż-Sypniewska G, Dzikowska E, Walentowicz P, Siodmiak J, et al. Serum 25(OH) vitamin D levels in Polish women during pregnancies complicated by hypertensive disorders and gestational diabetes. Int J Mol Sci (2016) 17:1574. doi:10.3390/ijms17101574
18. Rodriguez A, García-Esteban R, Basterretxea M, Lertxundi A, Rodríguez-Bernal C, Iñiguez C, et al. Associations of maternal circulating 25-hydroxyvitamin D3 concentration with pregnancy and birth outcomes. BJOG (2015) 122:1695–704. doi:10.1111/1471-0528.13074
19. Karras SN, Shah I, Petroczi A, Goulis DG, Bili H, Papadopoulou F, et al. An observational study reveals that neonatal vitamin D is primarily determined by maternal contributions: implications of a new assay on the roles of vitamin D forms. Nutr J (2013) 12:77. doi:10.1186/1475-2891-12-77
20. Nobles CJ, Markenson G, Chasan-Taber L. Early pregnancy vitamin D status and risk for adverse maternal and infant outcomes in a bi-ethnic cohort: the Behaviors Affecting Baby and You (B.A.B.Y.) study. Br J Nutr (2015) 114:2116–28. doi:10.1017/S0007114515003980
21. Wang C, Gao JS, Yu SL, Qiu L, Zeng L, Wang DH. Correlation between neonatal vitamin D level and maternal vitamin D level. Zhongguo Dang Dai Er Ke Za Zhi (2016) 18:20–3.
22. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press (2011).
23. Płudowski P, Socha P, Karczmarewicz E, Zagórecka E, Łukaszkiewicz J, Stolarczyk A, et al. Vitamin D supplementation and status in infants: a prospective cohort observational study. J Pediatr Gastroenterol Nutr (2011) 53:93–9. doi:10.1097/MPG.0b013e318216920f
24. Jacquemyn Y, Ajaji M, Karepouan N. Vitamin D levels in maternal serum and umbilical cord blood in a multi-ethnic population in Antwerp, Belgium. Facts Views Vis Obgyn (2013) 5:3–5.
25. Shakiba M, Iranmanesh MR. Vitamin D requirement in pregnancy to prevent deficiency in neonates: a randomized trial. Singapore Med J (2013) 54:285–8. doi:10.11622/smedj.2013110
26. Czech-Kowalska J, Gruszfeld D, Jaworski M, Bulsiewicz D, Latka-Grot J, Pleskaczyńska A, et al. Determinants of postpartum vitamin D status in the Caucasian mother-offspring pairs at a latitude of 52°N: a cross-sectional study. Ann Nutr Metab (2015) 67:33–41. doi:10.1159/000437099
27. Dovnik A, Mujezinović F, Treiber M, Pečovnik Balon B, Gorenjak M, Maver U, et al. Seasonal variations of vitamin D concentrations in pregnant women and neonates in Slovenia. Eur J Obstet Gynecol Reprod Biol (2014) 181:6–9. doi:10.1016/j.ejogrb.2014.07.019
28. Nicolaidou P, Hatzistamatiou Z, Papadopoulou A, Kaleyias J, Floropoulou E, Lagona E, et al. Low vitamin D status in mother-newborn pairs in Greece. Calcif Tissue Int (2006) 78:337–42. doi:10.1007/s00223-006-0007-5
29. Cadario F, Savastio S, Pozzi E, Capelli A, Dondi E, Gatto M, et al. Vitamin D status in cord blood and newborns: ethnic differences. Ital J Pediatr (2013) 39:1–12. doi:10.1186/1824-7288-39-35
30. Godang K, Frøslie KF, Henriksen T, Qvigstad E, Bollerslev J. Seasonal variation in maternal and umbilical cord 25(OH) vitamin D and their associations with neonatal adiposity. Eur J Endocrinol (2014) 170:609–17. doi:10.1530/EJE-13-0842
31. Josefson JL, Reisetter A, Scholtens DM, Price HE, Metzger BE, Langman CB, et al. Maternal BMI associations with maternal and cord blood vitamin D levels in a North American subset of hyperglycemia and adverse pregnancy outcome (HAPO) study participants. PLoS One (2016) 11(3):e0150221. doi:10.1371/journal.pone.0150221
32. Henderson A. Vitamin D and the breastfed infant. J Obstet Gynecol Neonatal Nurs (2005) 34:367–72. doi:10.1177/0884217505276157
33. Institute of Medicine. Weight Gain during Pregnancy: Reexamining the Guidelines. Washington, DC: The National Academies Press (2009).
34. Wierzejska R. Dose of the vitamin D in prenatal supplements and the current prevention its deficiency at mothers and newborns. Gin Pol Med Proj (2015) 37:49–53.
35. Eggemoen ÅR, Jenum AK, Mdala I, Knutsen KV, Lagerløv P, Sletner L. Vitamin D levels during pregnancy and associations with birth weight and body composition of the newborn: a longitudinal multiethnic population-based study. Br J Nutr (2017) 117:985–93. doi:10.1017/S000711451700068X
36. Loudyi FM, Kassouati J, Kabiri M, Chahid N, Kharbach A, Aguenaou H, et al. Vitamin D status in Moroccan pregnant women and newborns: reports of 102 cases. Pan Afr Med J (2016) 24:170. doi:10.11604/pamj.2016.24.170.4782
37. Dalgård C, Petersen MS, Steuerwald U, Weihe P, Grandjean P. Umbilical cord serum 25-hydroxyvitamin D concentrations and relations to birthweight, head circumference and infant length at age 14 days. Paediatr Perinat Epidemiol (2016) 30:238–45. doi:10.1111/ppe.12288
38. Lykkedegn S, Beck-Nielsen SS, Sorensen GL, Andersen LB, Fruekilde PBN, Nielsen J, et al. Vitamin D supplementation, cord 25-hydroxyvitamin D and birth weight: findings from the Odense Child Cohort. Clin Nutr (2017) 36:1621–7. doi:10.1016/j.clnu.2016.10.008
39. Wei SQ, Qi HP, Luo ZC, Fraser WD. Maternal vitamin D status and pregnancy outcomes: a systematic review and meta-analysis. J Matern Fetal Neonatal Med (2013) 26:889–99. doi:10.3109/14767058.2013.765849
40. Pérez-López FR, Pasupuleti V, Mezones-Holguin E, Benites-Zapata VA, Thota P, Deshpande A, et al. Effect of vitamin D supplementation during pregnancy on maternal and neonatal outcomes: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril (2015) 103:1278–88. doi:10.1016/j.fertnstert.2015.02.019
Keywords: vitamin D, blood, pregnancy, newborn, health
Citation: Wierzejska R, Jarosz M, Klemińska-Nowak M, Tomaszewska M, Sawicki W, Bachanek M and Siuba-Strzelińska M (2018) Maternal and Cord Blood Vitamin D Status and Anthropometric Measurements in Term Newborns at Birth. Front. Endocrinol. 9:9. doi: 10.3389/fendo.2018.00009
Received: 13 November 2017; Accepted: 08 January 2018;
Published: 25 January 2018
Edited by:
Pawel Pludowski, Children’s Memorial Health Institute, PolandReviewed by:
Spyridon N. Karras, Papageorgiou General Hospital, GreeceJustyna Czech-Kowalska, Children’s Memorial Health Institute, Poland
Copyright: © 2018 Wierzejska, Jarosz, Klemińska-Nowak, Tomaszewska, Sawicki, Bachanek and Siuba-Strzelińska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Regina Wierzejska, cndpZXJ6ZWpza2FAaXp6Lndhdy5wbA==
 Regina Wierzejska
Regina Wierzejska Mirosław Jarosz1
Mirosław Jarosz1 Magdalena Siuba-Strzelińska
Magdalena Siuba-Strzelińska