- 1Student Research Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Department of Microbiology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Department of Medicine, Division of Pulmonary, Critical Care, Sleep and Allergy, University of Miami, Coral Gables, FL, United States
Introduction: Diabetes mellitus (DM) is one of the most common comorbidities among patients with coronavirus disease 2019 (COVID-19) which may exacerbate complications of this new viral infection. Metformin is an anti-hyperglycemic agent with host-directed immune-modulatory effects, which relieve exaggerated inflammation and reduce lung tissue damage. The current systematic review aimed to summarize the available evidence on the potential mechanism of action and the efficacy of metformin in COVID-19 patients with DM.
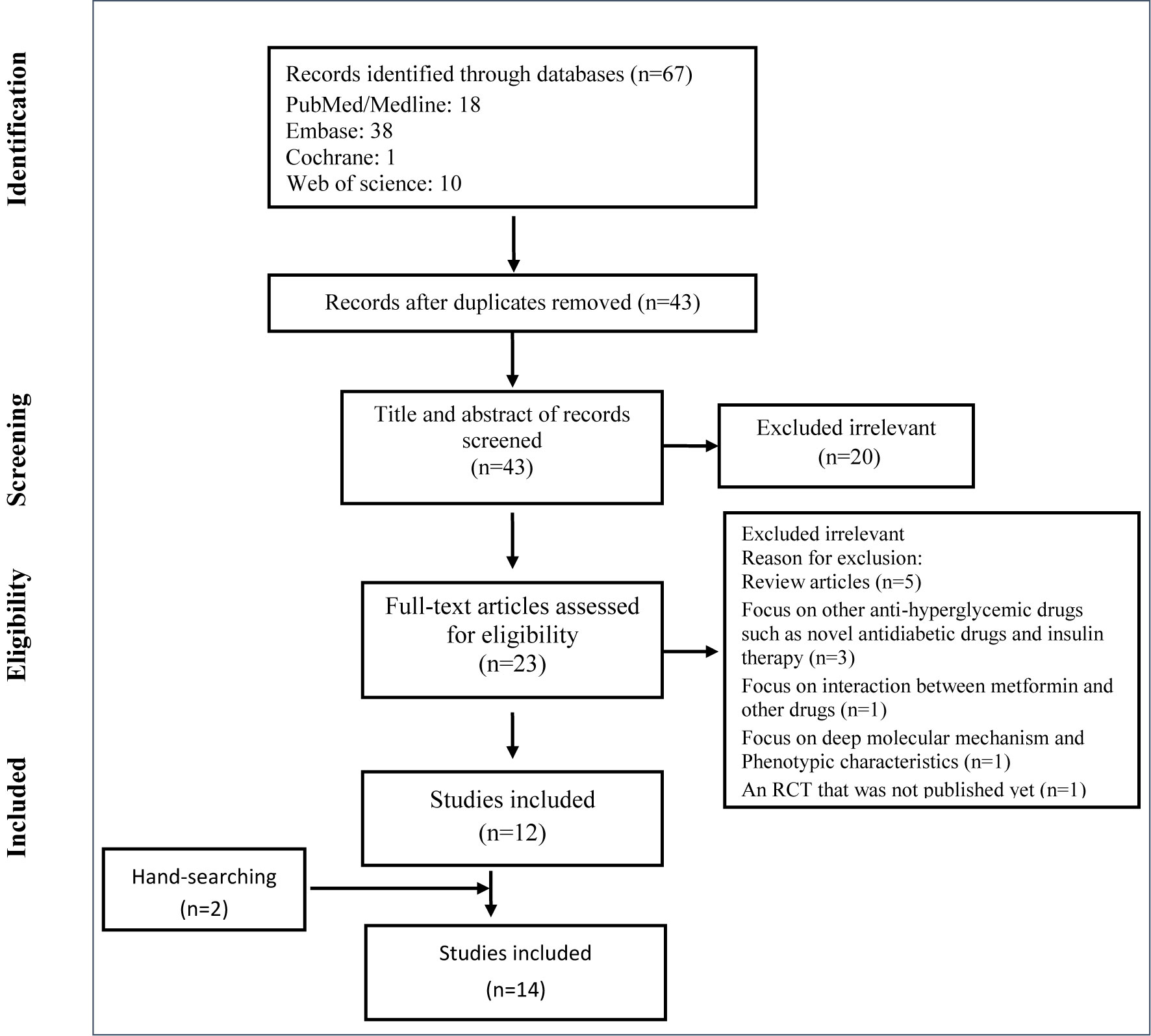
Methods: A systematic search was carried out in PubMed/Medline, EMBASE, the Cochrane Controlled Register of Trials (CENTRAL), and Web of Science up to July 30, 2020. The following keywords were used: “COVID-19”, “SARS-CoV-2”, “2019-nCoV”, “metformin”, and “antidiabetic drug”.
Results: Fourteen studies were included in our systematic review. Three of them were observational with 6,659 participants. Decreasing insulin resistance, reduction of some inflammatory cytokines like IL-6 and TNF-α, modulation of angiotensin-converting enzyme 2 (ACE2) receptor, and improving neutrophil to lymphocyte ratio are some of the potential mechanisms of metformin in COVID-19 patients with DM. Nine out of fourteen articles revealed the positive effect of metformin on the prognosis of COVID-19 in diabetic or even non-diabetic patients. Moreover, different studies have shown that metformin is more effective in women than men.
Conclusions: The use of metformin may lead to improve the clinical outcomes of patients with mild to moderate SARS-CoV-2, especially in diabetic women. Further observational studies should be conducted to clarify the effects of metformin as a part of the treatment strategy of COVID-19.
Introduction
In late December 2019, a cluster of patients with pneumonia was referred to hospitals in Wuhan city, Hubei province, China (1). Further clinical investigations showed that a novel coronavirus called Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) caused the disease, COVID-19 (2). Rapidly, COVID-19 affected almost all countries and territories worldwide, so that the World Health Organization (WHO) declared it as a pandemic on March 11, 2020 (3). As of late February 2021, more than 112 million prevalent numbers and above 2.5 million deaths were due to affecting by SARS-CoV-2 (4). Some pharmacologic therapeutic approaches like chloroquine, lopinavir/ritonavir, favipiravir, and tocilizumab have been used in clinical practice without any proven effect (5), while some drugs such as remdesivir have shown some effects on reducing time to recovery (6). Seniors, patients with preexisting diseases including hypertension, diabetes, coronary heart disease, and chronic obstructive pulmonary disease are at a higher risk of morbidity and mortality of COVID-19 (7).
Based on findings of a study on diabetic patients compared to controls, inflammatory responses and levels of inflammation-related biomarkers are higher among patients with diabetes mellitus (DM), which suggests considering DM as a major risk factor in the progression and prognosis of SARS-CoV-2 (8). DM is one of the most common comorbidities among COVID-19 patients, which leads to the intensive care unit (ICU) admission in 14%-32% of cases (9). Different potential mechanisms were mentioned for severity and increased risk of COVID-19 in patients with DM, including upregulation of angiotensin-converting-enzyme-2 (ACE2) expression (10), increased interleukin-6 (IL-6) expression (11), and decreasing CD4-positive T-cells in diabetic patients with Mediterranean Eastern respiratory syndrome coronavirus (MERS-CoV) (12) that may have the similar mechanism with COVID-19.
Metformin is a well-known antidiabetic drug, which showed immunomodulatory effects by phosphorylation of adenosine monophosphate (AMP)-activated protein kinase in animal models (13). A large-scale observational study showed that metformin reduced the mortality of chronic lower respiratory diseases significantly compared to the overall population (14).
This systematic review aimed to determine the potential efficacy of metformin in COVID-19 and the underlying mechanism of action in patients with preexisting DM.
Methods
This systematic review was according to the “Preferred Reporting Items for Systematic Reviews and Meta-analyses” (PRISMA) statement (15).
Search Strategy
A systematic search was carried out in the literature from the following bibliographical databases: PubMed/Medline, EMBASE, the Cochrane Controlled Register of Trials (CENTRAL), and Web of Science up to July 30, 2020. The following search terms were used: “COVID-19”, “SARS-CoV-2”, “2019-nCoV”, “metformin”, and “antidiabetic drug”. Lists of references of selected articles and relevant review articles were hand-searched to identify further studies. There were no restrictions on publication date and type of article but only studies written in English were selected.
Study Selection
All potentially English relevant articles were screened in two stages for eligibility. In the first stage, two reviewers independently reviewed titles and abstracts and chose those fitting selection criteria for full-text evaluation. Discrepancies were discussed with a third reviewer. In the second stage of assessment with full-text evaluation, all types of studies except reviews that discussed the effect of metformin in different stages of the COVID-19 and represented its mechanism were considered by the same authors. Disagreements and technical uncertainties were discussed and resolved between review authors.
Data Extraction
The following variables were extracted from all included studies: first author, year of publication, type of study, country/ies where the study was conducted, viral entrance pathway of SARS-CoV-2, mechanism of action of metformin against COVID-19, other effective drugs with the role of them, Possibility of using metformin in COVID-19 treatment and target society. In three analytic studies the extracted data included: study population (number of cases with metformin and number of controls without metformin), mean age (both in metformin and no-metformin group), COVID-19 diagnosis technique (clinical and confirmed diagnosis), and the effect of metformin on outcomes (effect on the duration of hospitalization, the effect on in-hospital death, and effect on poor prognosis). Two authors independently extracted the data from the selected studies. The data was jointly reconciled, and disagreements were discussed and resolved between review authors.
Results
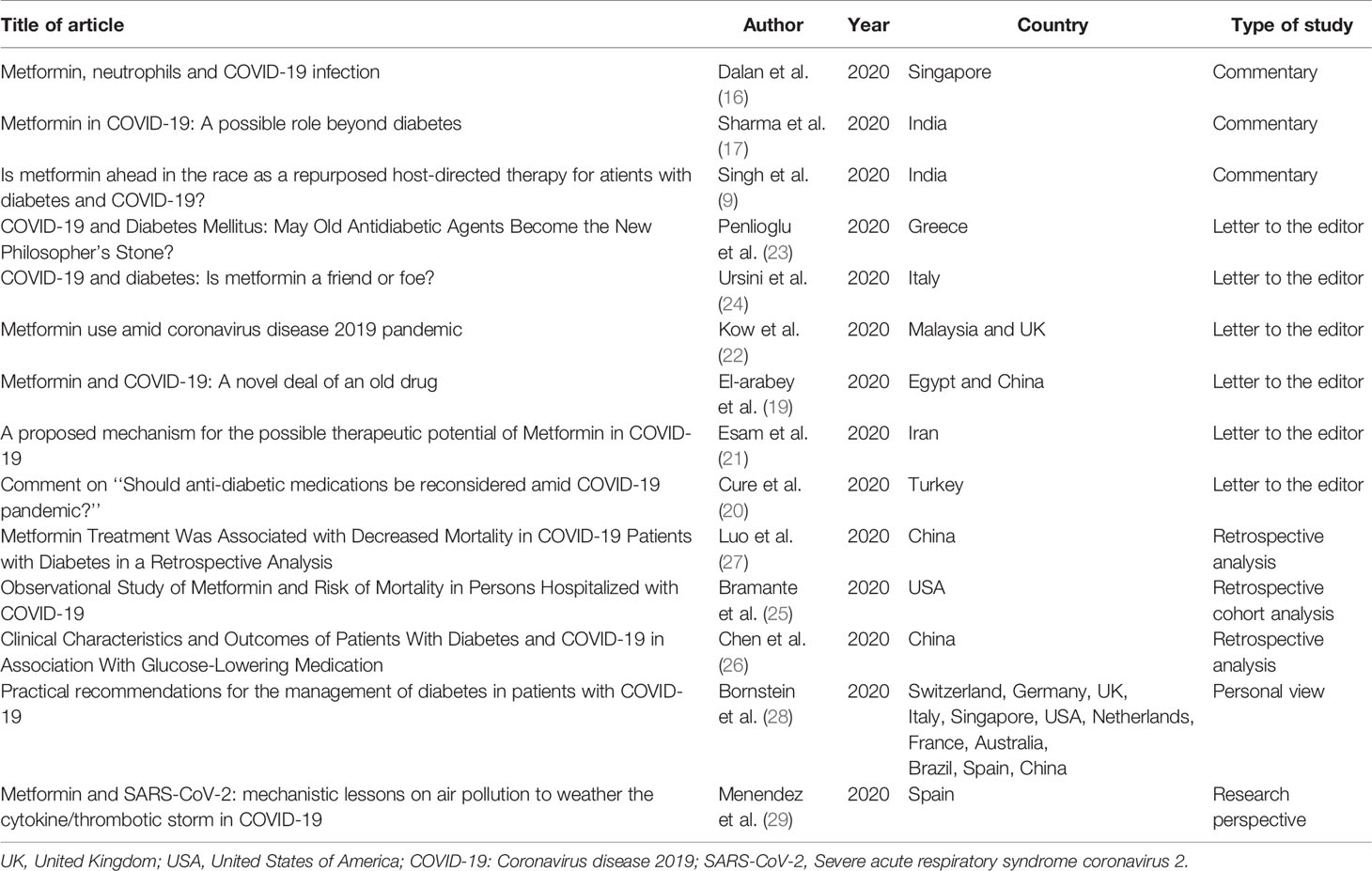
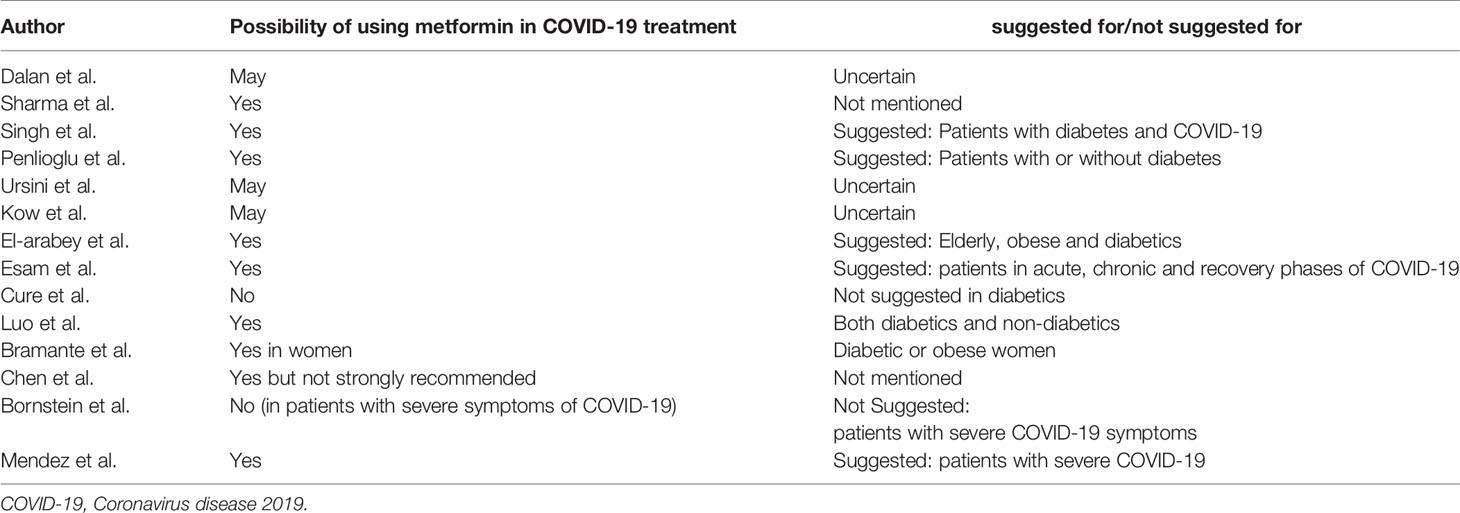
The selection process of articles is shown in Figure 1. Fourteen articles were included and classified into the followings: three commentaries (16–18), six letters to the editor (19–24), three observational studies (25–27), one personal view (28), and one research prospective study (29) (Table 1). Two of the three observational studies were conducted in China and one in the USA. The total population of the observational articles was 6,659. History of exposure, clinical symptoms, imaging findings, and laboratory assessments was included in clinical diagnosis. Also, PCR or immunoglobulin (Ig)-M and IgG tests were used to confirm the diagnosis (Tables 1 and 2).
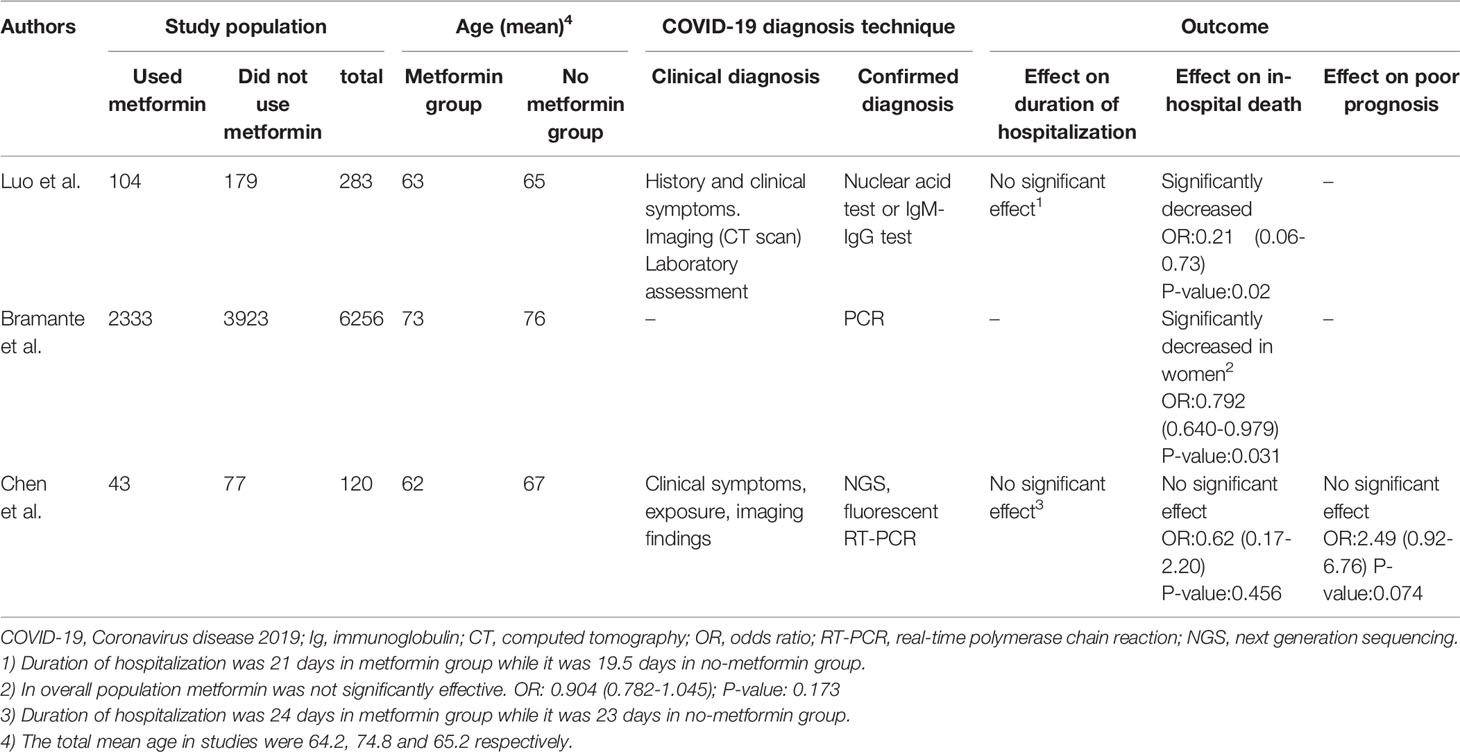
Table 2 Detailed characteristics and statistical information of three retrospective analytical studies.
Possibility of Using Metformin in COVID-19 Treatment
Nine out of fourteen articles showed the efficacy of metformin on COVID-19 that not only can be continued in diabetic patients as an anti-hyperglycemic drug but also may be offered in non-diabetics as a part of treatment protocol (17–19, 21, 23, 25–27, 29). Three articles did not provide a definitive opinion on the use of metformin for therapeutic purposes (16, 22, 24), and two articles reported that metformin should not be used in patients with SARS-CoV-2 infection (20, 28) (Table 3). Among these articles, Bramante et al. (25) by designing a retrospective cohort analysis study noticed that metformin has sex-specific effects and is useful for diabetic or obese women. Chen et al. (26) reported the positive effect of metformin in the course of the disease, whereas this effect was not statistically significant. On the contrary, Bornstein et al. (28) reported that metformin should not be used in patients with severe symptoms of COVID-19, but it is not contraindicated in patients with mild or moderate symptoms.
Effect of Metformin on Clinical Outcomes
Duration of hospitalization, in-hospital death, and poor prognosis (progression to severe or critical illness) was discussed as major outcomes in three retrospective analytical studies. Luo et al. (27) and Chen et al. (26) did not report any significant effect of metformin on the duration of hospitalization. Furthermore, according to Luo et al. study (27), there was no significant relationship between metformin and poor prognosis. For in-hospital death, Luo et al. (27) represented a significant decrease in the metformin group and Bramante et al. (25) reported this significant effect only in women. On the other hand, the article by Chen et al. (26) did not represent any significant relationship between the administration of metformin and in-hospital mortality reduction. More details on the three mentioned studies are available in Table 2.
Potential Mechanisms of Metformin and Other Drugs Against SARS-CoV-2
The suggested mechanisms of action for metformin within the fourteen included papers can be classified into some major categories. First, El-Arabey et al. (19) and Kow et al. (22) mentioned that weight reduction might have moderate protective effects against SARS-CoV-2, especially in the elderly. Second, adenosine monophosphate-activated protein kinase (AMPK) pathways that can affect the expression of ACE2, the receptor for SARS-CoV-2, is another pathway that can be modulated by metformin (17, 23–25). The articles by Penlioglou et al. (23), Sharma et al. (17), and Bramante et al. (25) mentioned protective roles of metformin by different mechanisms such as a reduction in insulin resistance (23), improving ACE2 stability (17), balancing renin-angiotensin-aldosterone system (17), modulation of ACE2 receptor (25), and controlling blood glucose levels (25). However, Ursini et al. (24) suggested that overexpression of ACE2 as a result of the AMPK pathway can put diabetic patients at higher risk of affecting by SARS-CoV-2. Third, high production of lactate and lactic acidosis due to metformin might be another potential mechanism for the high rate of infection in patients using metformin (20, 22, 28). Fourth, anti-inflammatory effects of metformin can protect patients administrating metformin from SARS-CoV-2 in different ways like inhibition of cytokine storms (18, 27, 29), inhibition of IL-6 crisis (18), and modulation of gut microbiota composition (18). Fifth, reduction of neutrophil count and improving neutrophil to lymphocyte ratio is another mechanism of metformin against COVID-19 in patients with preexisting diabetes mellitus (16, 25). In addition to these main mechanisms, metformin can play roles in protecting from or predisposing diabetic patients to SARS-CoV-2 infection in other various pathways, including reduction of vitamin B12 and immunosuppression (22), inhibition of PI3K/AKT/mTOR pathway (17), reducing thrombosis formation (25), prevention of lung damage and fibrosis (21, 27), interruption of the endocytic cycle due to decreasing acidity of endosomes and lysosomes (21), and reduction of some inflammatory cytokines like IL-6 (18, 25, 26) and TNF-α (25). Table 4 shows the mechanisms of metformin and other drugs on SARS-CoV-2 infection in diabetic patients.
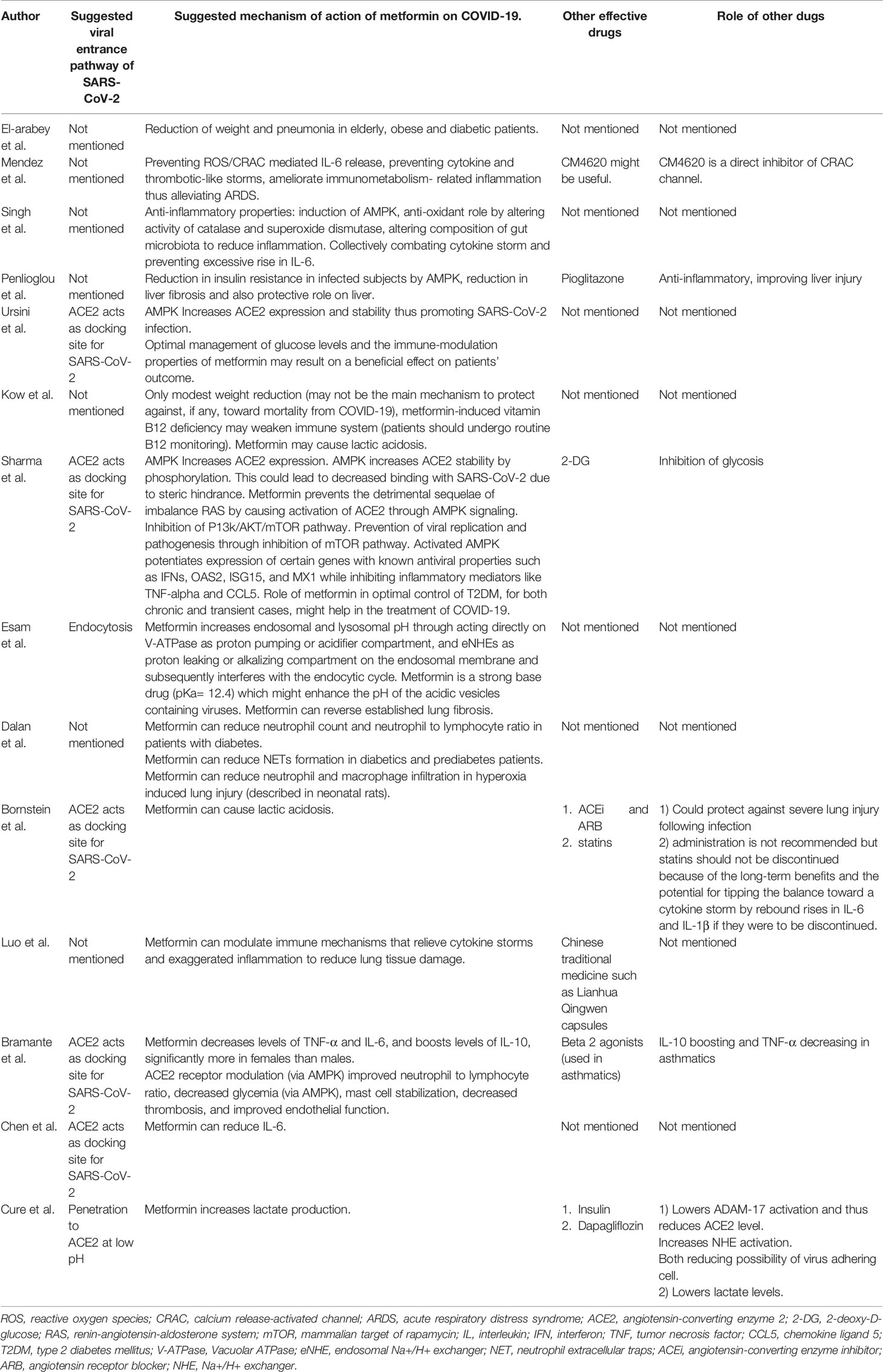
Table 4 Suggested potential mechanisms of action of metformin and other drugs on Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2).
Discussion
In the present work, most of the evaluated studies have shown that the use of metformin in the treatment regimen of diabetic and non-diabetic patients with COVID-19 is beneficial. Only two studies found that metformin should not be used in severe forms of the COVID-19, however, they did not prohibit its use in moderate to mild cases of infection.
COVID-19 is associated with poor prognosis and increased mortality rate in patients with DM. Also, diabetes management in patients suffering from COVID-19 is a great clinical challenge. Most of the studies evaluated in the current systematic review point to the beneficial effect of metformin in the treatment of COVID-19 patients with diabetes. Metformin as an agent of host-directed therapy can modulate immune mechanisms and therefore might prevent progression to acute respiratory distress syndrome (ARDS). Since there are some metabolic similarities between COVID-19 and DM such as hyperglycemia, oxidative stress, and pro-inflammatory cytokines, it is not unreasonable to expect that metformin with effects such as decreasing the levels of inflammatory cytokines IL-6 and TNF-alpha as well as increasing IL-10, an anti-inflammatory cytokine can play a beneficial role in reducing the complications of COVID-19 in patients with DM (30). Metformin induces the formation of M2 macrophages and T-regulatory as well as CD8 memory T cells which in turn minimize the inflammatory reactions (31). However, some studies have suggested not using this medication in the COVID-19 treatment protocol. In fact, in patients suffering from heart failure, respiratory distress, sepsis or renal impairment use of metformin should be stopped due to the risk of lactic acidosis (28). Of course, it should be noted that the risk of acidosis following the use of metformin is not very high, however, it should be considered, especially in hospitalized patients. Another issue to be considered is that metformin reduces intestinal absorption of vitamin B12 and lowers serum vitamin B12 concentrations in some metformin-treated patients. Due to the role of vitamin B12 in regulating the immune system its deficiency may negatively affect the cellular immune responses and thereafter facilitates infection from COVID-19 (32, 33). So, routine monitoring of vitamin B12 is suggested in metformin-treated patients.
Ursini et al. speculated that metformin synergistically with ACEi or ARBs may theoretically result in increasing ACE2 availability in the respiratory tract thus promoting Coivid-19 (24).
Nevertheless, it has been shown that poorly controlled blood glucose levels make patients prone to experience more complications or in-hospital death due to COVID-19. In other words, hospitalized patients with COVID-19 and diabetes had a longer length of stay in the hospital than patients without diabetes (34). Metformin by enhancing the activity of existing insulin and reducing hepatic glucose production exerts its glucose-lowering effect. That’s why it does not generally cause hypoglycemia in patients with or without diabetes (27). However, since the effects of host-directed therapy agents such as metformin on the virus itself are limited, we do not expect a reduction in the hospitalization period and the time it takes for the patient to be free of the virus (27). Luo et al. (27) and Chen et al. (26) findings are consistent with this theory. However, it has been proposed that metformin may have an inhibitory effect on the virus, by increasing insulin sensitivity (35).
The next issue is the more effective effects of metformin in women compared to men (25, 36). Also, metformin causes a greater reduction in TNF-α and IL-6 in women (36–38). The article by Mackey et al. suggests that this might be due to a higher secretion of TNF-α from mast cells in response to inflammation in women (39). Moreover, Klein et al. claim that sex hormones and epigenetic changes of the Y chromosome may be responsible for the sex-specific effects of metformin (40). Also, Li et al. proposed that although metformin increases the expression of ACE2 in both sexes equally, the subsequent inflammatory response can be different between men and women, which can also have a relation to the sex-specific benefits of metformin (41). Last, of all, metformin can increase the levels of IL-10, an anti-inflammatory cytokine, in women more than men (42, 43). According to the above, it is proven that Metformin is more beneficial in women with DM and COVID-19 compared to similar men.
The beneficial effects of metformin to reduce the duration of hospitalization, in-hospital death and poor prognosis are controversial. Since the studies performed in these cases are limited, evidence may not be sufficient to confirm or deny the adequacy of metformin in reducing these complications in patients with diabetes suffering from COVID-19.
The current study has been limited with a lack of clinical trials and the number of cohort studies. So we couldn’t design a meta-analysis study. Furthermore, only the efficacy of metformin is discussed in our study, and the effects, mechanisms, complications, and interactions of other diabetic and non-diabetic drugs that may use in combination therapy in diabetic patients have not been studied.
Conclusions
According to the current knowledge, it can be concluded that the use of metformin can have beneficial effects on COVID-19, especially in diabetic patients, while more studies such as retrospective analysis of COVID-19 diabetic cohorts are suggested to be conducted. These beneficial effects of metformin should be considered, especially among female patients. On the other side, in the case of hospitalized patients with severe symptoms of COVID-19 and underlying diseases, the possibility of adverse effects of metformin like lactate acidosis should be taken into account.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Author Contributions
MZ, MJN, MM: designed the study. MZ, SAN, MMZ: performed the search, study selection, and data synthesis. MJN, MZ, BH, SAN, MMZ: wrote the first draft of the manuscript. MJN, MM: revised the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study is related to the project NO 1399/62228 From Student Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran. We also appreciate the “Student Research Committee” and “Research & Technology Chancellor” in Shahid Beheshti University of Medical Sciences for their financial support of this study.
References
1. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med (2020) 382(13):1199–207. doi: 10.1056/NEJMoa2001316
2. Park SE. Epidemiology, virology, and clinical features of severe acute respiratory syndrome -coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin Exp Pediatr (2020) 63(4):119–24. doi: 10.3345/cep.2020.00493
3. (WHO) WHO. WHO Director-General"s opening remarks at the media briefing on COVID-19 - 11 March 2020. (2020). Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
4. (WHO) WHO. Coronavirus disease (COVID-2019) situation reports. (2020). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/.
5. Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA (2020) 323(18):1824–36. doi: 10.1001/jama.2020.6019
6. Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med (2020) 383(19):1813–26. doi: 10.1056/NEJMoa2007764
7. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (2020) 395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3
8. Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes/Metabol Res Rev (2020), e3319. doi: 10.1002/dmrr.3319
9. Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr (2020) 14(4):303–10. doi: 10.1016/j.dsx.2020.04.004
10. Rao S, Lau A, So HC. Exploring Diseases/Traits and Blood Proteins Causally Related to Expression of ACE2, the Putative Receptor of SARS-CoV-2: A Mendelian Randomization Analysis Highlights Tentative Relevance of Diabetes-Related Traits. Diabetes Care (2020) 43(7):1416–26. doi: 10.2337/dc20-0643
11. Maddaloni E, Buzzetti R. Covid-19 and diabetes mellitus: unveiling the interaction of two pandemics. Diabetes/Metabol Res Rev (2020), e33213321–e33213321. doi: 10.1002/dmrr.3321
12. Kulcsar KA, Coleman CM, Beck SE, Frieman MB. Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection. JCI Insight (2019) 4:(20). doi: 10.1172/jci.insight.131774
13. Kajiwara C, Kusaka Y, Kimura S, Yamaguchi T, Nanjo Y, Ishii Y, et al. Metformin Mediates Protection against Legionella Pneumonia through Activation of AMPK and Mitochondrial Reactive Oxygen Species. J Immunol (Baltimore Md 1950) (2018) 200(2):623–31. doi: 10.4049/jimmunol.1700474
14. Mendy A, Gopal R, Alcorn JF, Forno E. Reduced mortality from lower respiratory tract disease in adult diabetic patients treated with metformin. Respirology (2019) 24(7):646–51. doi: 10.1111/resp.13486
15. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097
16. Dalan R. Metformin, neutrophils and COVID-19 infection. Diabetes Res Clin Pract (2020) 164:108230. doi: 10.1016/j.diabres.2020.108230
17. Sharma S, Ray A, Sadasivam B. Metformin in COVID-19: A possible role beyond diabetes. Diabetes Res Clin Pract (2020) 164:108183. doi: 10.1016/j.diabres.2020.108183
18. Singh AK, Singh R. Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19? Diabetes Res Clin Pract (2020) 165:108268. doi: 10.1016/j.diabres.2020.108268
19. EL‐Arabey AA, Abdalla M. Metformin and COVID-19: A novel deal of an Old Drug. J Med Virol (2020) 92:2293–4. doi: 10.1002/jmv.25958
20. Cure E, Cumhur Cure M. Comment on “Should anti-diabetic medications be reconsidered amid COVID-19 pandemic?” Diabetes Res Clin Pract (2020) 164:108184. doi: 10.1016/j.diabres.2020.108184
21. Esam Z. A proposed mechanism for the possible therapeutic potential of Metformin in COVID-19. Diabetes Res Clin Pract (2020) 167:108282. doi: 10.1016/j.diabres.2020.108282
22. Kow CS, Hasan SS. Metformin use amid coronavirus disease 2019 pandemic. J Med Virol (2020) 92:2401–2. doi: 10.1002/jmv.26090
23. Penlioglou T, Papachristou S, Papanas N. COVID-19 and Diabetes Mellitus: May Old Anti-diabetic Agents Become the New Philosopher’s Stone? Diabetes Ther Res Treat Educ Diabetes Related Disord (2020) 11(6):1–3. doi: 10.1007/s13300-020-00830-0
24. Ursini F, Ciaffi J, Landini MP, Meliconi R. COVID-19 and diabetes: Is metformin a friend or foe? Diabetes Res Clin Pract (2020) 164:108167. doi: 10.1016/j.diabres.2020.108167
25. Bramante C, Ingraham N, Murray T, Marmor S, Hoversten S, Gronski J, et al. Observational Study of Metformin and Risk of Mortality in Patients Hospitalized with Covid-19. MedRxiv Prepr Server Health Sci (2020). doi: 10.1101/2020.06.19.20135095
26. Chen Y, Yang D, Cheng B, Chen J, Peng A, Yang C, et al. Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication. Diabetes Care (2020) 43(7):1399. doi: 10.2337/dc20-0660
27. Luo P, Qiu L, Liu Y, Liu XL, Zheng JL, Xue HY, et al. Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis. Am J Trop Med Hygiene (2020) 103(1):69–72. doi: 10.4269/ajtmh.20-0375
28. Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol (2020) 8(6):546–50. doi: 10.1016/S2213-8587(20)30152-2
29. Menendez JA. Metformin and SARS-CoV-2: mechanistic lessons on air pollution to weather the cytokine/thrombotic storm in COVID-19. Aging (2020) 12(10):8760–5. doi: 10.18632/aging.103347
30. Zumla A, Hui DS, Azhar EI, Memish ZA, Maeurer M. Reducing mortality from 2019-nCoV: host-directed therapies should be an option. Lancet (2020) 395(10224):e35–6. doi: 10.1016/S0140-6736(20)30305-6
31. Schuiveling M, Vazirpanah N, Radstake T, Zimmermann M, Broen JCA. Metformin, A New Era for an Old Drug in the Treatment of Immune Mediated Disease? Curr Drug Targets (2018) 19(8):945–59. doi: 10.2174/1389450118666170613081730
32. de Jager J, Kooy A, Lehert P, Wulffele MG, van der Kolk J, Bets D, et al. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ (2010) 340:c2181. doi: 10.1136/bmj.c2181
33. Tamura J, Kubota K, Murakami H, Sawamura M, Matsushima T, Tamura T, et al. Immunomodulation by vitamin B12: augmentation of CD8+ T lymphocytes and natural killer (NK) cell activity in vitamin B12-deficient patients by methyl-B12 treatment. Clin Exp Immunol (1999) 116(1):28–32. doi: 10.1046/j.1365-2249.1999.00870.x
34. Al-Salameh A, Lanoix JP, Bennis Y, Andrejak C, Brochot E, Deschasse G, et al. Characteristics and outcomes of COVID-19 in hospitalized patients with and without diabetes. Diabetes Metab Res Rev (2020), e3388. doi: 10.1002/dmrr.3388
35. Chen Y, Gu F, Guan JL. Metformin Might Inhibit Virus through Increasing Insulin Sensitivity. Chin Med J (Engl) (2018) 131(3):376–7. doi: 10.4103/0366-6999.223856
36. Park JW, Lee JH, Park YH, Park SJ, Cheon JH, Kim WH, et al. Sex-dependent difference in the effect of metformin on colorectal cancer-specific mortality of diabetic colorectal cancer patients. World J Gastroenterol (2017) 23(28):5196–205. doi: 10.3748/wjg.v23.i28.5196
37. Kelly B, Tannahill GM, Murphy MP, O’Neill LAJ. Metformin Inhibits the Production of Reactive Oxygen Species from NADH:Ubiquinone Oxidoreductase to Limit Induction of Interleukin-1β (IL-1β) and Boosts Interleukin-10 (IL-10) in Lipopolysaccharide (LPS)-activated Macrophages. J Biol Chem (2015) 290(33):20348–59. doi: 10.1074/jbc.M115.662114
38. Matsiukevich D, Piraino G, Lahni P, Hake PW, Wolfe V, O’Connor M, et al. Metformin ameliorates gender-and age-dependent hemodynamic instability and myocardial injury in murine hemorrhagic shock. Biochim Biophys Acta (BBA) Mol Basis Dis (2017) 1863(10, Part B):2680–91. doi: 10.1016/j.bbadis.2017.05.027
39. Mackey E, Ayyadurai S, Pohl CS, D’ Costa S, Li Y, Moeser AJ. Sexual dimorphism in the mast cell transcriptome and the pathophysiological responses to immunological and psychological stress. Biol Sex Differ (2016) 7:60–0. doi: 10.1186/s13293-016-0113-7
40. Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol (2016) 16(10):626–38. doi: 10.1038/nri.2016.90
41. Li M-Y, Li L, Zhang Y, Wang X-S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty (2020) 9(1):45. doi: 10.1186/s40249-020-00662-x
42. Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med (2020) 383(25):2451–60. doi: 10.1056/NEJMcp2009575
Keywords: metformin, diabetes mellitus, SARS-CoV-2, COVID-19, 2019-nCoV, systematic review
Citation: Zangiabadian M, Nejadghaderi SA, Zahmatkesh MM, Hajikhani B, Mirsaeidi M and Nasiri MJ (2021) The Efficacy and Potential Mechanisms of Metformin in the Treatment of COVID-19 in the Diabetics: A Systematic Review. Front. Endocrinol. 12:645194. doi: 10.3389/fendo.2021.645194
Received: 23 December 2020; Accepted: 03 March 2021;
Published: 19 March 2021.
Edited by:
Reza Beigverdi, Tehran University of Medical Sciences, IranReviewed by:
Mukunthan Murthi, John H. Stroger, Jr. Hospital of Cook County, United StatesKayo Henrique Fernandes E. Magalhaes Santos, Jackson Memorial Hospital, United States
Copyright © 2021 Zangiabadian, Nejadghaderi, Zahmatkesh, Hajikhani, Mirsaeidi and Nasiri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammad Javad Nasiri, bWoubmFzaXJpQGhvdG1haWwuY29t; Mehdi Mirsaeidi, TXNtMjQ5QG1lZC5taWFtaS5lZHU=
 Moein Zangiabadian
Moein Zangiabadian Seyed Aria Nejadghaderi
Seyed Aria Nejadghaderi Mohammad Mahdi Zahmatkesh
Mohammad Mahdi Zahmatkesh Bahareh Hajikhani
Bahareh Hajikhani Mehdi Mirsaeidi
Mehdi Mirsaeidi Mohammad Javad Nasiri
Mohammad Javad Nasiri