- Department of Thyroid Surgery, West China Hospital, Sichuan University, Chengdu, China
Background: Thyroidectomy for massive goiters is challenging because of the increased risk of tracheomalacia, combined sternotomy, postoperative morbidity, and mortality, whereas studies investigating the clinicopathologic characteristics, postoperative morbidities, and surgical outcomes of massive goiters are limited.
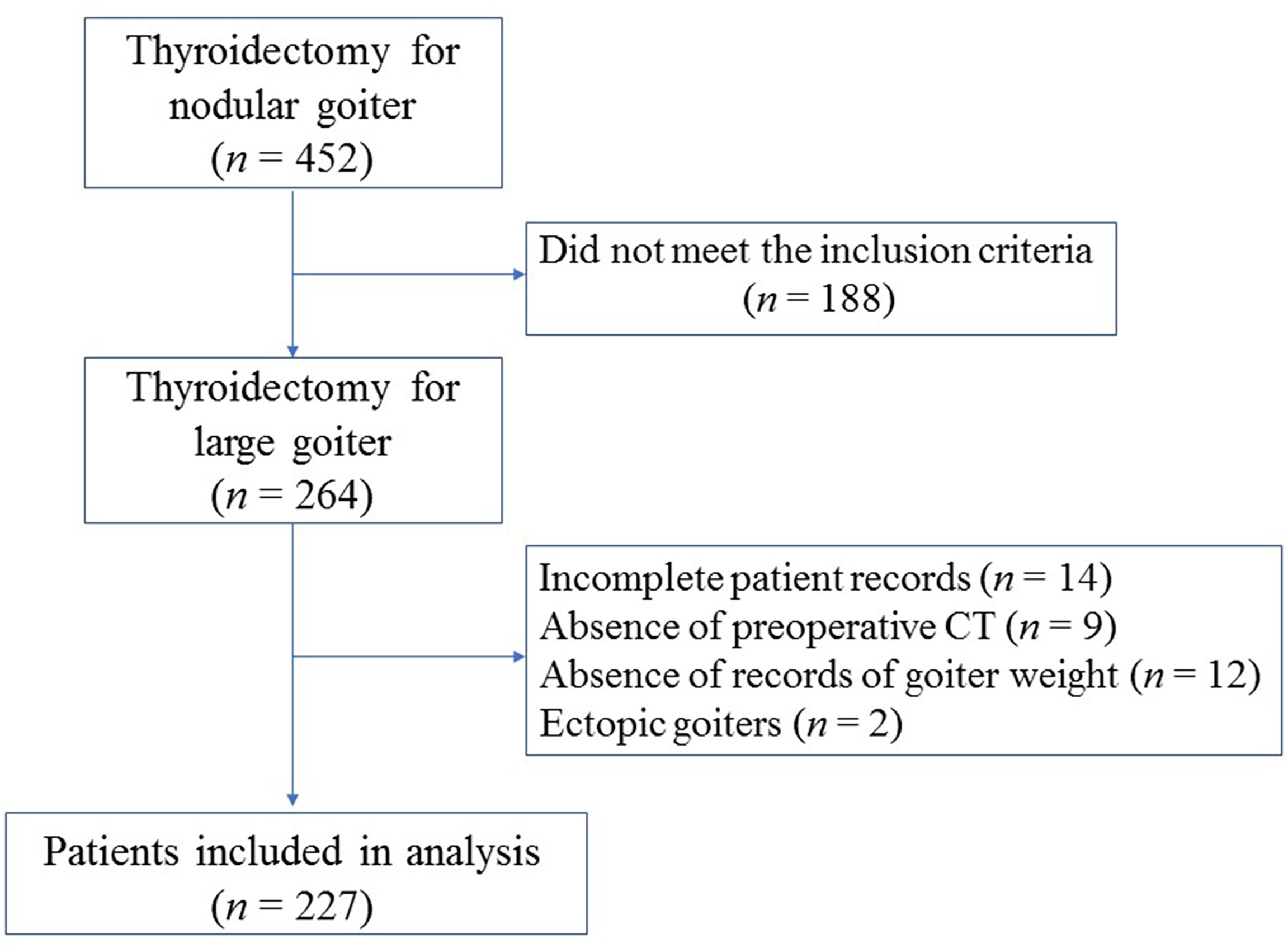
Methods: Patients with goiters undergoing thyroid surgery between 2009 and 2019 were retrospectively reviewed. A total of 227 patients were enrolled and divided into massive goiter group and large goiter group according to the weight of the goiter. Clinicopathologic characteristics, postoperative morbidities, and surgical outcomes were compared between the two groups.
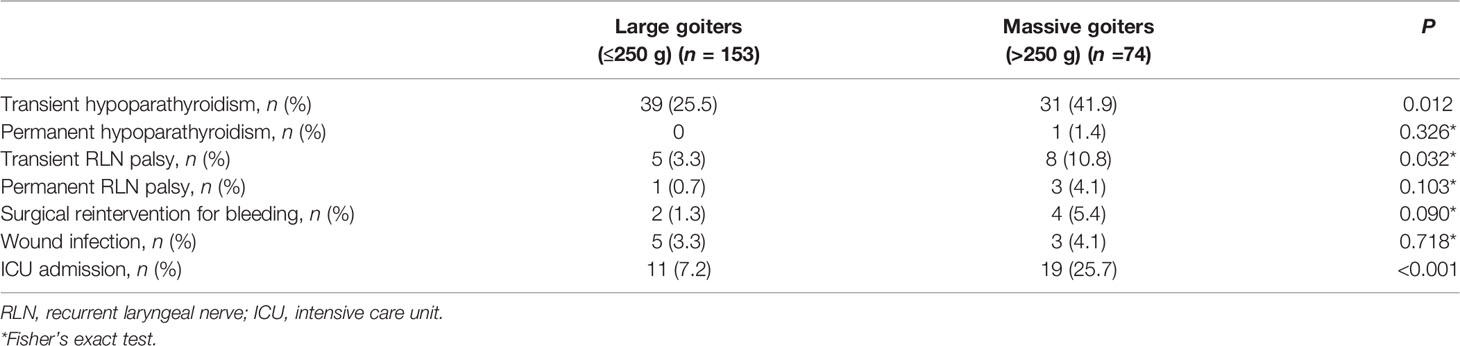
Results: Seventy-four patients (32.6%) had a goiter weighing more than 250 g and 153 patients (67.4%) were categorized in the large goiter group. Compared to large goiter patients, massive goiter patients had higher rates of retrosternal extension (82.4% vs. 30.7%), combined sternotomy (12.2% vs. 1.3%), intensive care unit admission (25.7% vs. 7.2%), transient hypoparathyroidism (41.9% vs. 25.5%), and transient recurrent laryngeal nerve palsy (10.8% vs. 3.3%) as well as prolonged length of hospital stay (P < 0.05).
Conclusions: Massive goiter patients were at increased risk of combined sternotomy, intensive care unit admission, postoperative morbidities as well as prolonged length of hospital stay after thyroidectomy compared to large goiter patients, but most of them can be treated through a cervical approach with a favorable outcome.
Introduction
Multinodular goiter (MNG) is a common thyroid disorder, which is estimated to affect about 1.5 billion people worldwide (1, 2). Iodine deficiency is considered to be the most common cause of goiter in iodine-deficient areas, and the incidence of nodular goiter has declined with the popularization and implementation of iodized salt intake in the last decades (3, 4). However, the prevalence of nodular goiter, in iodine repletion countries, is reported in a range from 13% to 45% (5). Most nodular goiters are generally asymptomatic and slow growing, while surgical intervention should be considered for patients with compressive symptoms, disfigurement, or suspected malignancy. The severity of compressive symptoms depends on the size and location of the goiter, which may worsen owing to the rapid growth or hemorrhage. In a recent study (6), shortness of breath was noted in 40% of patients with large cervical goiter (>100 g) and 52% with substernal goiter.
Surgical intervention is the most effective treatment for massive goiters that offers a definitive effect on alleviation of compressive symptoms. However, patients with massive goiters pose airway and surgical challenges due to the airway deformity and distorted neck anatomy. In addition, retrosternal extension, with a reported incidence of 12%~46%, is another challenge to surgeons because of the risk of an extra-thoracic approach (7, 8). Therefore, it is important to conduct a detailed preoperative evaluation as well as peri-operative management in patients with massive goiters. Although there have been many studies focusing on large goiters (>100 g), there are few studies targeting massive goiters.
The aim of this study was to investigate the clinicopathologic characteristics, postoperative morbidities, and surgical outcomes of patients with massive goiters.
Materials and Methods
Study Design
We conducted a retrospective study of patients who underwent thyroidectomy as treatment for goiter in West China Hospital, Sichuan University from September 2009 to December 2019. Clinical and pathological data were retrieved from electronic medical record system from the Computer Information Resource Center of West China Hospital. Demographic and clinicopathologic variables, including age, gender, compressive symptoms, retrosternal extension, surgical procedures, postoperative morbidities, length of hospital stay, concurrent thyroid malignancy, and surgical outcomes, were analyzed and compared between the large goiter group and the massive goiter group. Patients with incomplete record, in absence of preoperative CT record, or in absence of goiter weight record as well as an ectopic goiter were excluded. This study was designed according to the STROBE criteria and was approved by the Institutional Review Board of West China Hospital, Sichuan University.
Peri-Operative Management
All patients underwent a preoperative thyroid function test including thyroid stimulating hormone, free triiodothyronine, free thyroxine, thyroglobulin, and antibodies against thyroperoxidase and thyroglobulin as well as serum parathyroid hormone (PTH). Patients with hyperthyroidism in the study were treated with methimazole (10-30 mg/day; Merck KGaA, Darmstadt, Germany) to achieve a euthyroid state prior to surgery. Both ultrasonography (US) and cervicothoracic CT scan were performed in all patients to assess the size, location, and adjacent structures of the goiter. A fiberoptic laryngoscopy was performed preoperatively to assess vocal cord mobility. Post-operative laryngoscopy was selectively performed in patients with voice change. Fine-needle aspiration cytology (FNAC) was selectively performed in patients with suspected malignancy based on preoperative US findings. Moreover, an esophageal or tracheal endoscopy was performed in patients with suspected malignancy or significant symptoms of dysphagia and dyspnea.
Serum calcium and PTH levels were routinely assessed for all patients on the first day after surgery. Intravenous and oral calcium supplementations with 1,25-dihydroxyvitamin D3 (1.8~2.4 g/day; Caltrate, Wyeth, New Jersey, USA) were prescribed if the patient exhibited symptoms of hypocalcemia. The dosage of these medications was gradually tapered off with the normalization of serum calcium and PTH levels.
Definitions
Although there is no uniform definition of a large goiter, several studies defined a large goiter as the gross weight of more than 100 g (6, 7). Therefore, a large goiter was also defined as a goiter with a gross weight > 100 g, and a massive goiter was defined as a goiter with a gross weight >250 g in the present study. Similarly, a substernal goiter was defined as a goiter extending below the plane of the thoracic inlet on computed tomography (CT) scan in the supine position.
Hypoparathyroidism was defined as a serum PTH level lower than 1.6 pmol/L with a concurrent serum calcium level <2.0 mmol/L. Permanent hypoparathyroidism was defined as postoperative hypocalcemia for more than 6 months. Vocal cord palsy was diagnosed if vocal cord immobility was confirmed by laryngoscopy. Permanent recurrent laryngeal nerve (RLN) palsy was defined as persistent vocal cord palsy for more than 12 months postoperatively.
Statistical Analysis
Normally or nonnormally distributed continuous variables were described as mean ± standard deviation (SD) or median, respectively. Comparisons between two groups were conducted using Pearson’s chi-square test or Fisher’s exact test for categorical variables, whereas continuous variables were compared using Student’s t-test or Mann-Whitney U test. Statistically significant was accepted when P < 0.05. All statistical analyses were performed using SPSS Statistics software version 21.0 (IBM Inc., Chicago, IL, USA).
Results
Patient Characteristics
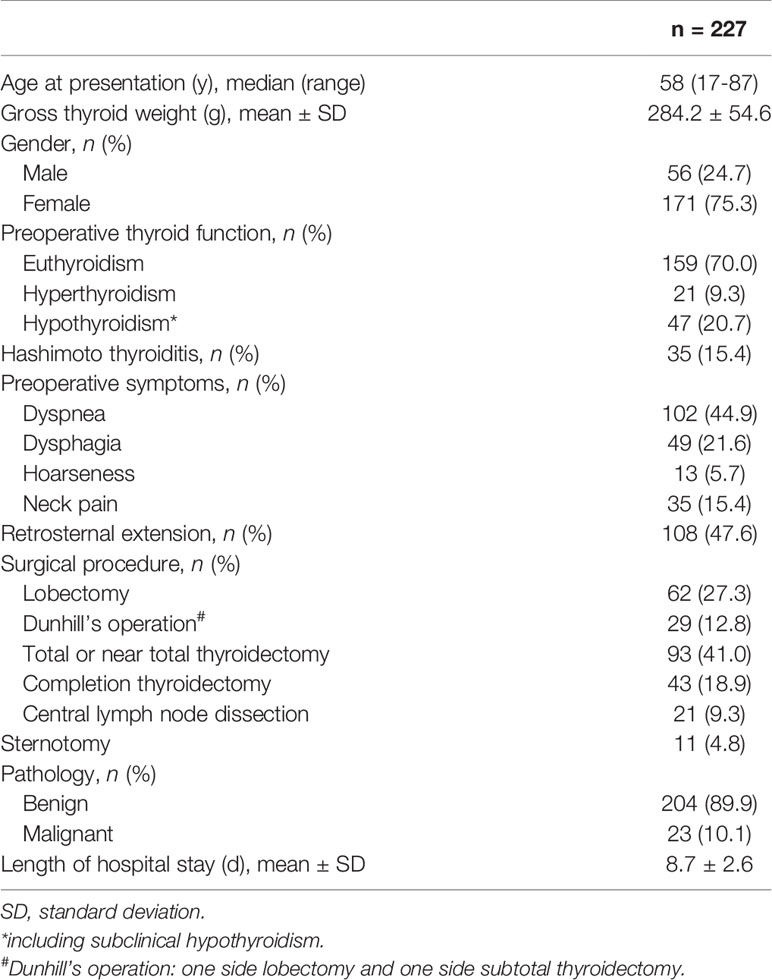
From September 2009 to December 2019, a total of 452 thyroidectomies were performed for nodular goiters in our department. Finally, a total of 227 patients who met the criteria were included (Figure 1). Patient demographics and characteristics are summarized in Table 1. There were 171 females and 56 males, with a median age of 58 years (range, 17-87 years). The most common compressive symptom was dyspnea (44.9%), followed by dysphagia (21.6%). Of these, 159 patients (70.0%) had a normal thyroid function, while 21 patients (9.3%) exhibited hyperthyroidism and 47 (20.7%) exhibited hypothyroidism. Total thyroidectomy or near total thyroidectomy was performed in 93 patients (41.0%), lobectomy in 62 patients (27.3%), Dunhill’s operation in 29 patients (12.8%), and 43 patients (18.9%) underwent completion thyroidectomy. In addition, concurrent central lymph node dissection (level VI) was performed in 21 patients (9.3%).
Retrosternal extension was observed in 108 patients (47.6%). Based on careful review of CT images, the inferior limit of goiter extended over the aortic arch in 9 patients (4.0%) and to the tracheal bifurcation in 2 patients (0.8%). Malignancy was identified in 23 patients (10.1%) and the type of malignancies included papillary microcarcinoma (n = 13), papillary carcinoma (n = 8), and follicular papillary carcinoma (n = 2). Among them, 16 cases were diagnosed by FNAC, while other 7 cases with negative FNAC results were confirmed by intraoperative frozen section examination or by paraffin pathological diagnosis.
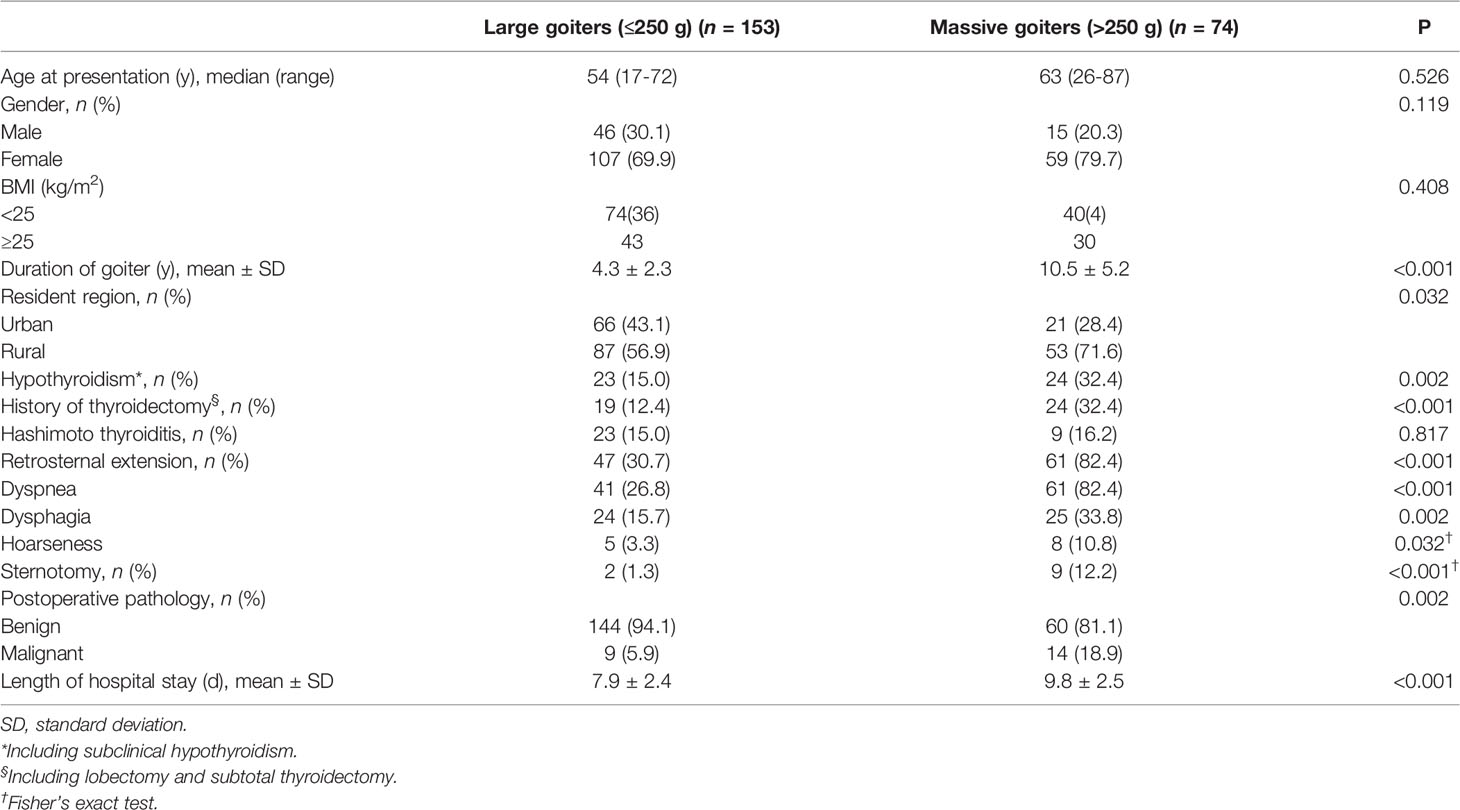
The mean ± SD weight of goiter was 284.2 ± 54.6 g. One hundred and fifty-three patients (67.4%) were categorized in the large goiter group and 74 patients (32.6%) had a goiter weight >250 g. As shown in Table 2, massive goiter patients were more frequently from rural areas (P = 0.032) with a longer duration course of goiter (P < 0.001) compared to large goiter patients. The rates of compressive symptoms (P < 0.05) and retrosternal extension (P < 0.001) were significantly higher in the massive goiter group. Moreover, patients with massive goiters more frequently had a previous thyroidectomy (P < 0.001) with significantly higher rates of hypothyroidism (P = 0.002), combined sternotomy (P < 0.001), and prolonged length of hospital stay (P < 0.001).
Primary Outcomes
Postoperative outcomes are shown in Table 3. One case of permanent hypoparathyroidism was recorded in the massive goiter group. There was a higher incidence of transient hypoparathyroidism in the massive goiter group compared to the large goiter group (41.9% vs. 25.5%, P = 0.012). Moreover, there was an increased risk of transient RLN palsy in the massive group (P = 0.032). No statistical differences were observed in permanent RLN palsy and permanent hypoparathyroidism between the two groups. Additionally, massive goiter patients had a significantly higher rate of intensive care unit (ICU) admission (P < 0.001). None of the patients in both groups required tracheostomy, while 5 massive goiter patients (6.7%) required prolonged intubation to prevent tracheomalacia, all of which were successfully extubated a few days later. Despite the higher rate of concurrent malignancy in the massive group, neither the patients in the large group nor in the massive group suffered recurrent disease with a mean follow-up time of 6.7 months (range, 3–18 months) and 14.2 months (range, 9–24 months), respectively.
Discussion
Goiter is defined as an enlargement of the thyroid gland that usually presents as a swelling in the front of the neck, which can be further classified as endemic or non-endemic, diffuse or nodular, and toxic or nontoxic (9). Most goiters are asymptomatic and do not require surgical intervention, while surgery is recommended in patients with compressive symptoms, suspected malignancy, drug-resistant hyperthyroidism, or retrosternal extension (10–12). Patients with large goiters frequently present with shortness of breath, dysphagia, and voice change; however, the most common symptom is nonspecific. In our study, the most common symptom was dyspnea, and patients in the massive goiter group had a much higher rate of compressive symptoms (for example, dyspnea, dysphagia, and hoarseness). Compressive symptoms may be directly related to goiter size, while goiter size is correlated with growth time: the longer the growth time, the larger the size. Consistent with the data of Agarwal et al. (13), we found that the duration course of goiter in the massive goiter group was longer than that in the large goiter group. These results, in a word, justify that a massive goiter potentially results from an untreated goiter with further progression for a long time.
Goiter can affect the thyroid gland diffusely or only involve one lobe. Although performing total thyroidectomy or lobectomy remains controversial, lobectomy may be an appropriate procedure for goiters which are isolated to one lobe. However, in a prospective study with a mean follow-up time of 14.5 years, Beatriz et al. (14) found that about 15% of patients (394/2,675) with MNG required completion thyroidectomy for recurrence. In this study, 43 patients (18.9%) underwent completion thyroidectomy; however, we could not conclude that the patients had recurrence of MNG because it is difficult to evaluate whether residual goiter remained after the initial surgery. Moreover, whether nodular disease involves the contralateral lobe is difficult to assess. Interestingly, we found that a higher proportion of patients with massive goiter had a previous thyroidectomy. In general, the residual thyroid tissue after lobectomy can secrete sufficient thyroid hormone to maintain daily metabolism, while thyroxine will be insufficient if the remnant of thyroid tissue is small or involved in diseases, such as Hashimoto thyroiditis or nodular goiter. Low-level of thyroid hormone stimulates the synthesis and secretion of TSH; the latter one plays an important role in the development of nodular thyroid hyperplasia (15, 16). As shown in the present study, the patients with massive goiter were found to have a higher rate of hypothyroidism, which suggests that close surveillance of thyroid function and appropriate supplementation of thyroxine may play an important role in preventing goiter progression.
Retrosternal extension, namely substernal goiter, is frequently associated with a large goiter. Although numerous definitions have been proposed and compared, there is no consensus on the definition of substernal goiter. In the literature, the reported incidence of substernal goiter varies from 12% to 46% due to the use of different criteria (7, 8). In the present study, 108 patients (47.6%) were confirmed with retrosternal extension, and all of them located in the anterior mediastinum. Moreover, we identified that the rate of retrosternal extension in the massive group was higher than that in the large group, which is consistent with a previous report (12). Most substernal goiters can be managed through a cervical approach; sternotomy should be taken into consideration if the extension is beyond the level of the aortic arch, in combination with malignancy, or in the presence of a posterior mediastinal goiter, ectopic goiter, or recurrent goiter (17–19). Only 11 patients (4.8%) in the study required a combined sternotomy, and all the patients who underwent a combined sternotomy had a goiter extending below the level of the aortic arch. Similar to the report by Sancho et al. (20), in which a goiter weight of over 250 g is an independent predictor of an increased need for additional sternotomy, suggesting that a much higher rate of sternotomy would be performed in patients with massive goiters. Cervical and thoracic CT scans play a valuable role in evaluating the depth and extent of substernal goiter and its relationship with surrounding structures, which is helpful in planning the surgical strategy and anesthesia intubation.
Total thyroidectomy for massive goiter is challenging, which is associated with a significantly higher risk of RLN and parathyroid damage (21, 22). Our data showed that the rate of RLN injury was 11.2%, which was comparable between the two groups. Lin et al. (23) reported that the incidence of right-sided RLN injury was more common than that of left-sided RLN injury. However, no such difference was noted between right-sided and left-sided RLN injuries in this study. In our experience, adequate exposure is crucial in ensuring safe thyroidectomy and preventing the potential risk of RLN injury. Recently, continuous intraoperative nerve monitoring has been reported as a useful and effective modality in identifying and preserving the integrity of the nerve, which effectively lower the incidence of postoperative vocal cord palsy (24). Postoperative hypoparathyroidism is not uncommon in large goiters due to an increased risk of inadvertent dissection or devascularization of parathyroid glands. The incidence of transient hypoparathyroidism was significantly higher in the massive goiter group, whereas the rate of permanent hypoparathyroidism was similar between the two groups. This may have resulted from the reason that patients undergoing lobectomy, Dunhill’s procedure, and completion thyroidectomy were also enrolled in the present study.
The incidence of malignancy in MNG has been reported to vary from 4% to 17% (25). In our study, the overall incidence of malignancy was 10.1% (23/227), and it was 18.9% (14/74) in the massive goiter group, which was significantly higher than that in the large goiter group. Whether there is an increased risk of malignancy in large goiter remains controversial; however, malignancy implies an increased risk of RLN and parathyroid injury due to the necessity of lymph node dissection. Although the relationship between goiter size and malignancy has not been clearly determined, it has been reported that malignancy was significantly higher in intrathoracic goiter (26, 27). On the basis of the study, a detailed preoperative US evaluation with FNAC is indispensable for massive goiters, even though the diagnostic accuracy of malignancy was relatively low in our study (69.6%). This can be attributed to the limitations of sonographic detection of surrounding structures, the deep location of the tumor, and/or tumor size <1.0 cm. In our experience, intraoperative frozen section examination provides a supplementary modality for the diagnosis of malignant nodules.
Some limitations should be noted in our study. First, retrospective analysis in general is subject to informational biases: data accuracy is closely dependent on the registration/codification process. Second, the present study was conducted in a single institution with a limited sample size. Finally, the rate of retrosternal extension was not accurately assessed and compared because there is no uniform definition of a retrosternal goiter. However, in our opinion, we prefer to define a substernal goiter that extending below the plane of the thoracic inlet on the basis of that researchers in different facilities and circumstances can easily and uniformly use this anatomic definition.
Conclusions
Massive goiter (>250 g) patients were at higher risk of combined sternotomy, ICU admission, postoperative morbidities as well as prolonged length of hospital stay after thyroidectomy compared to large goiter patients. Although massive goiters were associated with an increased rate of retrosternal extension, most of them can be removed through a cervical approach. The overall surgical outcomes for massive goiters may potential less favorable than for large goiters, whereas most massive goiters can be safely excised with minimal morbidity with an experienced surgeon and a dedicated planning.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The study was approved by the Institutional Review Board of West China Hospital, Sichuan University. Written informed consent to participate in this study was provided by the patients or their legal guardian.
Author Contributions
QC, data collection, analysis, drafting of manuscript, interpretation of data, final approval, and accountability for all aspects of the work. AS, data collection, interpretation of data, and final approval. XZ, interpretation of data, analysis, and final approval. FL and RG, data collection, analysis, and final approval. JZ, interpretation of data, critical review, revising, and final approval. ZL, interpretation of data, critical review, and final approval. TW, study design, interpretation of data, critical review, revising, final approval, and accountability for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Moalem J, Suh I, Duh QY. Treatment and Prevention of Recurrence of Multinodular Goiter: An Evidence-Based Review of the Literature. World J Surg (2008) 32(7):1301–12. doi: 10.1007/s00268-008-9477-0
2. Simó R, Nixon IJ, Vander Poorten V, Quer M, Shaha AR, Sanabria A, et al. Surgical Management of Intrathoracic Goitres. Eur Arch Otorhinolaryngol (2019) 276(2):305–14. doi: 10.1007/s00405-018-5213-z
3. Phitayakorn R, Super DM, McHenry CR. An Investigation of Epidemiologic Factors Associated With Large Nodular Goiter. J Surg Res (2006) 133(1):16–21. doi: 10.1016/j.jss.2006.02.044
4. Fiore E, Tonacchera M, Vitti P. Influence of Iodization Programmes on the Epidemiology of Nodular Goitre. Best Pract Res Clin Endocrinol Metab (2014) 28(4):577–88. doi: 10.1016/j.beem.2014.04.002
5. Carlé A, Krejbjerg A, Laurberg P. Epidemiology of Nodular Goitre. Influence of Iodine Intake. Best Pract Res Clin Endocrinol Metab (2014) 28(4):465–79. doi: 10.1016/j.beem.2014.01.001
6. Nankee L, Chen H, Schneider DF, Sippel RS, Elfenbein DM. Substernal Goiter: When Is a Sternotomy Required? J Surg Res (2015) 199(1):121–5. doi: 10.1016/j.jss.2015.04.045
7. Ríos A, Rodríguez JM, Balsalobre MD, Tebar FJ, Parrilla P. The Value of Various Definitions of Intrathoracic Goiter for Predicting Intra-Operative and Postoperative Complications. Surgery (2010) 147(2):233–8. doi: 10.1016/j.surg.2009.06.018
8. Wong WK, Shetty S, Morton RP, McIvor NP, Zheng T. Management of Retrosternal Goiter: Retrospective Study of 72 Patients at Two Secondary Care Centers. Auris Nasus Larynx (2019) 46(1):129–34. doi: 10.1016/j.anl.2018.06.012
9. Patel KN, Yip L, Lubitz CC, Grubbs EG, Miller BS, Shen W, et al. The American Association of Endocrine Surgeons Guidelines for the Definitive Surgical Management of Thyroid Disease in Adults. Ann Surg (2020) 271(3):e21–93. doi: 10.1097/SLA.0000000000003580
10. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association Management Guidelines for Patients With Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid (2009) 19(11):1167–214. doi: 10.1089/thy.2009.0110
11. White ML, Doherty GM, Gauger PG. Evidence-Based Surgical Management of Substernal Goiter. World J Surg (2008) 32(7):1285–300. doi: 10.1007/s00268-008-9466-3
12. Chen AY, Bernet VJ, Carty SE, Davies TF, Ganly I, Inabnet WB 3rd, et al. American Thyroid Association Statement on Optimal Surgical Management of Goiter. Thyroid (2014) 24(2):181–9. doi: 10.1089/thy.2013.0291
13. Agarwal A, Agarwal S, Tewari P, Gupta S, Chand G, Mishra A, et al. Clinicopathological Profile, Airway Management, and Outcome in Huge Multinodular Goiters: An Institutional Experience From an Endemic Goiter Region. World J Surg (2012) 36(4):755–60. doi: 10.1007/s00268-012-1447-x
14. de Rienzo-Madero B, Sabra JP, Gand E, Donatini G, Kraimps JL. Unilateral Benign Multinodular Versus Solitary Goiter: Long-Term Contralateral Reoperation Rates After Lobectomy. Surgery (2019) 165(1):75–9. doi: 10.1016/j.surg.2018.04.074
15. Hegedüs L, Bonnema SJ, Bennedbaek FN. Management of Simple Nodular Goiter: Current Status and Future Perspectives. Endocr Rev (2003) 24(1):102–32. doi: 10.1210/er.2002-0016
16. Dauksiene D, Petkeviciene J, Klumbiene J, Verkauskiene R, Vainikonyte-Kristapone J, Seibokaite A, et al. Factors Associated With the Prevalence of Thyroid Nodules and Goiter in Middle-Aged Euthyroid Subjects. Int J Endocrinol (2017) 2017:8401518. doi: 10.1155/2017/8401518
17. Machado NO, Grant CS, Sharma AK, al Sabti HA, Kolidyan SV. Large Posterior Mediastinal Retrosternal Goiter Managed by a Transcervical and Lateral Thoracotomy Approach. Gen Thorac Cardiovasc Surg (2011) 59(7):507–11. doi: 10.1007/s11748-010-0712-x
18. de Perrot M, Fadel E, Mercier O, Farhamand P, Fabre D, Mussot S, et al. Surgical Management of Mediastinal Goiters: When Is a Sternotomy Required? Thorac Cardiovasc Surg (2007) 55(1):39–43. doi: 10.1055/s-2006-924440
19. Cichoń S, Anielski R, Konturek A, Baczyński M, Cichoń W, Orlicki P. Surgical Management of Mediastinal Goiter: Risk Factors for Sternotomy. Langenbecks Arch Surg (2008) 393(5):751–7. doi: 10.1007/s00423-008-0338-y
20. Sancho JJ, Kraimps JL, Sanchez-Blanco JM, Larrad A, Rodríguez JM, Gil P, et al. Increased Mortality and Morbidity Associated With Thyroidectomy for Intrathoracic Goiters Reaching the Carina Tracheae. Arch Surg (2006) 141(1):82–5. doi: 10.1001/archsurg.141.1.82
21. Ozbas S, Kocak S, Aydintug S, Cakmak A, Demirkiran MA, Wishart GC. Comparison of the Complications of Subtotal, Near Total and Total Thyroidectomy in the Surgical Management of Multinodular Goitre. Endocr J (2005) 52(2):199–205. doi: 10.1507/endocrj.52.199
22. Barczyński M, Konturek A, Hubalewska-Dydejczyk A, Gołkowski F, Cichoń S, Nowak W. Five-Year Follow-Up of a Randomized Clinical Trial of Total Thyroidectomy Versus Dunhill Operation Versus Bilateral Subtotal Thyroidectomy for Multinodular Nontoxic Goiter. World J Surg (2010) 34(6):1203–13. doi: 10.1007/s00268-010-0491-7
23. Lin YS, Wu HY, Lee CW, Hsu CC, Chao TC, Yu MC. Surgical Management of Substernal Goitres at a Tertiary Referral Centre: A Retrospective Cohort Study of 2,104 Patients. Int J Surg (2016) 27:46–52. doi: 10.1016/j.ijsu.2016.01.032
24. Staubitz JI, Watzka F, Poplawski A, Riss P, Clerici T, Bergenfelz A, et al. Effect of Intraoperative Nerve Monitoring on Postoperative Vocal Cord Palsy Rates After Thyroidectomy: European Multicentre Registry-Based Study. BJS Open (2020) 4(5):821–9. doi: 10.1002/bjs5.50310
25. Knobel M. Etiopathology, Clinical Features, and Treatment of Diffuse and Multinodular Nontoxic Goiters. J Endocrinol Invest (2016) 39(4):357–73. doi: 10.1007/s40618-015-0391-7
26. Moten AS, Thibault DP, Willis AW, Willis AI. Demographics, Disparities, and Outcomes in Substernal Goiters in the United States. Am J Surg (2016) 211(4):703–9. doi: 10.1016/j.amjsurg.2015.11.022
Keywords: multinodular goiter, thyroidectomy, retrosternal extension, massive goiter, sternotomy
Citation: Chen Q, Su A, Zou X, Liu F, Gong R, Zhu J, Li Z and Wei T (2022) Clinicopathologic Characteristics and Outcomes of Massive Multinodular Goiter: A Retrospective Cohort Study. Front. Endocrinol. 13:850235. doi: 10.3389/fendo.2022.850235
Received: 07 January 2022; Accepted: 24 February 2022;
Published: 24 May 2022.
Edited by:
Catherine Fiona Sinclair, Icahn School of Medicine at Mount Sinai, United StatesReviewed by:
Erivelto Martinho Volpi, Centro de referencia no ensino do diagnóstico por imagem (CETRUS), BrazilSerena Ippolito, PO Ospedale del Mare, Italy
Copyright © 2022 Chen, Su, Zou, Liu, Gong, Zhu, Li and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Wei, c3VyZ2VvbndlaXRhb0AxNjMuY29t
 Qiang Chen
Qiang Chen Anping Su
Anping Su Zhihui Li
Zhihui Li