- 1Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University and Shandong Provincial Qianfoshan Hospital, Jinan, China
- 2Department of Radiology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 3Department of Traditional Chinese Medicine, Shandong College of Traditional Chinese Medicine, Yantai, China
- 4Department of Cardiology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
Background: In 2019, there was a global outbreak of new coronary pneumonia. Studies have found that the severity of patients with new coronary pneumonia may be related to their comorbidities. This article discusses the impact of thyroid disease on the severity of new coronary pneumonia through a meta-analysis and provides new treatment ideas for the later treatment and recovery of new coronary pneumonia.
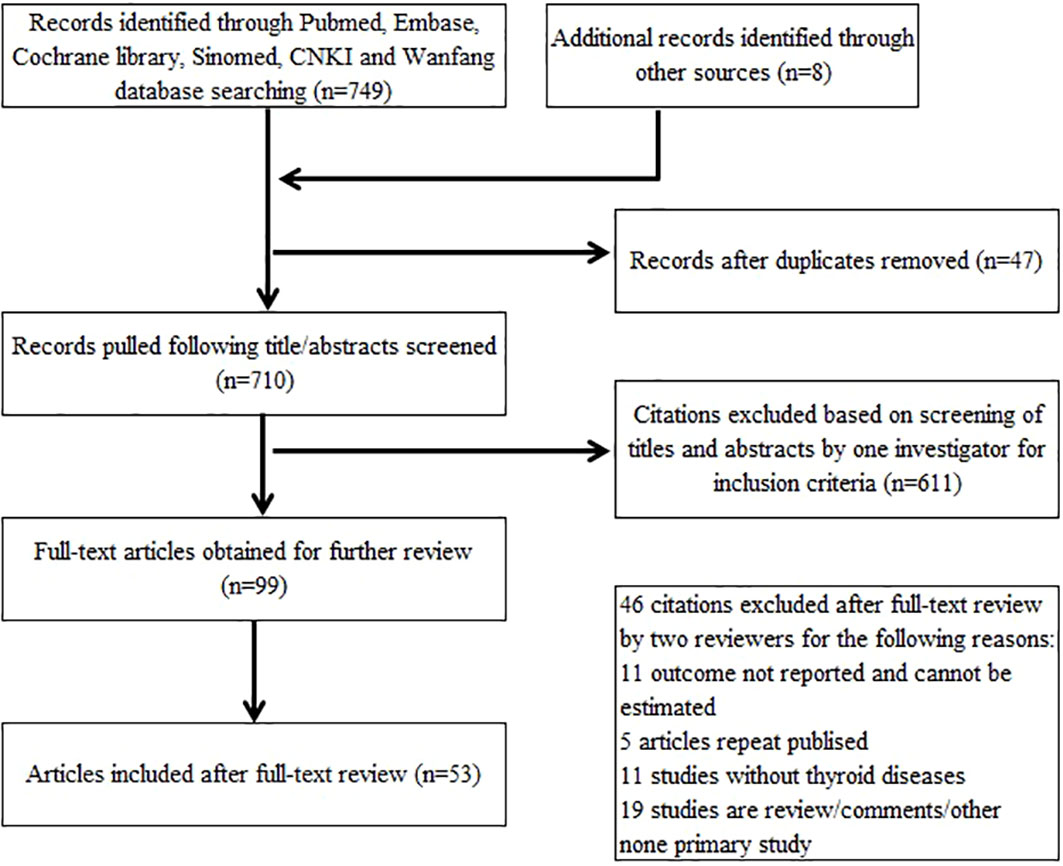
Methods: Databases including PubMed, Embase, Cochrane Library, SINOMED, China national knowledge infrastructure (CNKI), and Wanfang for coronavirus disease 2019 (COVID-19) infection and thyroid diseases were searched. Reference lists of all eligible articles and related previous review articles were handsearched. Fifty-three articles were included to conduct the meta-analysis.
Results: Fifty-three articles with 12,022 COVID-19 infection patients were included in this meta-analysis. The proportion of patients with thyroid diseases in all COVID-19 infection patients fluctuates between 0% and 88.46%. Of the 53 included studies, 22 studies reported the severity of COVID-19 infection and grouped. The fixed-effects model was used to merge odds ratio (OR) values, and the pooled effect size in favor of non-severe patients is 2.62 (95% CI = 1.96–3.49, P < 0.0001), which means that patients with severe COVID-19 infection are more likely to have thyroid diseases. The analysis subgrouped into Asia and Europe shows that patients with COVID-19 severe infection in Asia are 3.77 times more likely to have thyroid diseases than non-severe patients (fixed-effects model: OR = 3.77, 95% CI = 2.66–5.35, P < 0.00001). No significant statistical heterogeneity was found by the heterogeneity analysis (chi-square = 19.85, P = 0.34, I2 = 9%). Severe COVID-19 infection patients are more likely to be complicated by hypothyroidism and low T3 syndrome. The pooled ORs with fixed-effects model are 3.72 (95% CI = 1.62–8.58, P = 0.002) and 5.86 (95% CI = 2.79–12.33, P < 0.00001), respectively.
Conclusion: COVID-19 infection patients with thyroid diseases are very common, and severe patients are more likely to have thyroid diseases. Asian COVID-19 infection, hypothyroidism patients, and patients with low T3 syndrome are more likely to progress to severe condition.
Systematic Review Registration: https://inplasy.com, identifier INPLASY202190079.
Introduction
Coronavirus is an enveloped single-stranded positive-stranded RNA virus of the Coronavirus family. The new 2019 novel coronavirus (2019-nCoV) is currently the seventh known coronavirus that can infect humans (1) and usually causes mild to moderate infection of the respiratory tract (1).
It has been found that patients infected with 2019-nCoV, especially those with severe disease, have high levels of immune factors such as interleukin-1B (IL-1B) and interferon gamma (IFNγ) in their blood, suggesting that cytokine concentrations are associated with the severity of the disease (2).
Evidence to date shows that having chronic diseases increases the risk of serious illnesses from coronavirus disease 2019 (COVID-19) (3). Coronaviruses are known to have direct effects on several endocrine glands, including the thyroid. In patients infected with SARS-CoV, a coronavirus related to SARS-CoV-2, autopsy revealed damage to thyroid follicles and parafollicular cells (4). Abnormalities in thyroid function have also been found to be associated with the severity of respiratory disease. Several different types of thyroid dysfunction caused by COVID-19 disease have been identified, including mild to moderate non-thyroidal disease syndrome (NTIS), severe NTIS, and subclinical hypothyroidism. All three different types of thyroid dysfunction are associated with the severity of COVID-19 prognosis (5). In one study of 61 survivors of severe acute respiratory syndrome (SARS), conducted 3 months after recovery, four (6.6%) were diagnosed to be primary hypothyroidism (6), and thyroid lesions were found in autopsies of patients who died of SARS (4). It has also been found that changes in thyroid function are often seen during the acute phase of COVID-19 (7). However, there are differences in the prevalence of thyroid disease in COVID-19 patients, which have not been comprehensively studied. Also, whether thyroid disease is associated with the severity of COVID-19 remains controversial. In addition, whether the type of thyroid disease or regional differences in patients are associated with the severity of COVID-19 remains unclear.
In this study, we performed a meta-analysis of the association between thyroid diseases and new coronary pneumonia and analyzed whether thyroid diseases were related to the severity of COVID-19. We also aimed to provide new ideas for the prognosis of new coronary pneumonia, especially the rehabilitation treatment of new coronary patients with thyroid disease.
Materials and methods
This meta-analysis was conducted under the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and it was also registered on the International Platform of Registered Systematic Review and Meta-analysis Protocols (registration number: INPLASY202190079; DOI number: 10.37766/inplasy2021.9.0079).
Searching progress
PubMed, Embase, Cochrane Library, SINOMED, CNKI, and Wanfang were searched for studies of thyroid diseases in patients with COVID-19 infection. The literature search for this meta-analysis was restricted to published results. Databases were searched from the earliest data to 15 April 2022 with the following search terms: (“coronavirus disease 2019” OR “COVID-19”) AND (“thyroid diseases” OR “hyperthyroidism” OR “hypothyroidism” OR “thyroid function”). Reference lists of all eligible articles and related previous review articles were handsearched. Eligible studies met the following criteria: 1) published in English or Chinese language; 2) study assessed the association between COVID-19 infection and thyroid diseases (population: patients with COVID-19 infection; exposure factor: thyroid diseases; outcome: the incidence of thyroid diseases in patients with COVID-19 infection); 3) study was designed as the cohort study or case series; 4) study reported at least one result including but not limited to the number of cases, prevalence, etc.
Study selection and data extraction
Studies were independently screened by two reviewers, and disagreements were resolved by consensus. From the eligible studies, the following data were extracted: countries and regions of inclusion of patients, study type, total number of COVID-19 infection patients, type of thyroid diseases, and number of patients with thyroid diseases.
Methodological quality assessment
Among these 53 studies, 51 studies are retrospective cohort studies and the remaining two are case series. Newcastle–Ottawa Scale (NOS) was used to assess the methodological quality. The score of 9 is highest for NOS and shows the highest quality. Two authors scored these items independently.
Statistical analysis
The main outcome was the number of patients with thyroid diseases in patients with COVID-19 infection. The number of patients with thyroid diseases in patients with severe disease of COVID-19 infection was also collected. Fixed-effects model was performed by computing odds ratios (ORs) and 95% CI for dichotomous variables. The I2 was calculated as an index of heterogeneity between studies. The analyses were performed by Review Manager 5.3 (Cochrane Collaboration, United Kingdom, http://www.cochrane.org).
Results
Search results and characteristics of included studies
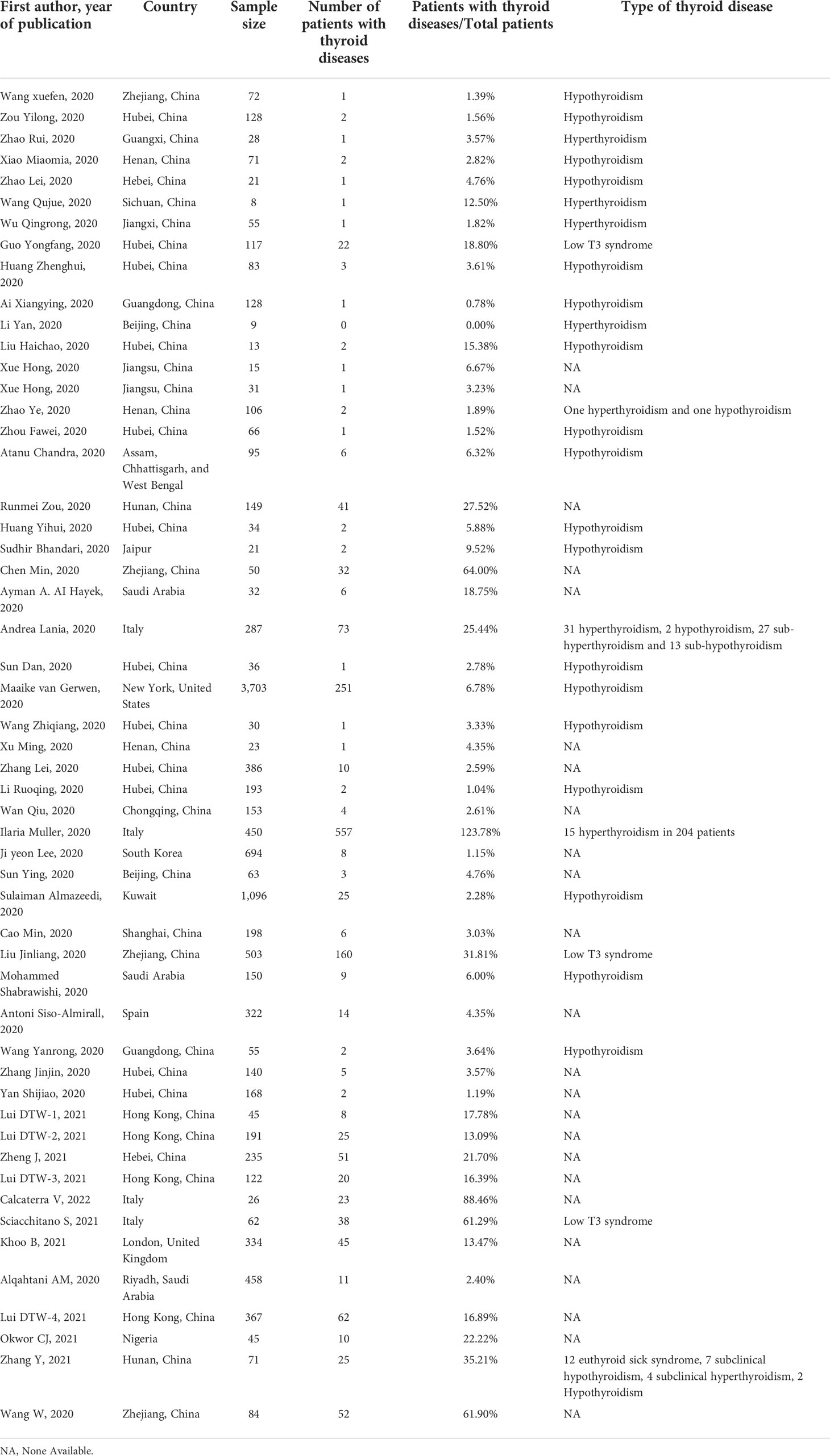
Our research yielded 702 articles of potentially relevant studies. Eight additional articles from the reference lists of eligible articles were also included. After screening the abstract, 99 were selected for full-text review. In total, 53 articles (3, 5, 7–57) were included in this meta-analysis. Searching progress is shown in Figure 1. Of the included 53 studies, 38 studies’ data are collected from Chinese COVID-19 infection patients. Italy has four articles and Saudi Arabia has three articles included. Jaipur; United States; South Korea; Kuwait; Spain; Assam, Chhattisgarh, and West Bengal; United Kingdom; and Nigeria have one article each. In total, there are 12,022 COVID-19 infection patients in all the included studies; sample size ranges from 8 to 3,707. Of these, 1,135 patients had thyroid diseases and the number was between 0 and 251. Overall, the proportion of patients with thyroid diseases in all COVID-19 infection patients fluctuates between 0% and 88.46%. Twenty-one studies reported hypothyroidism, seven studies reported hyperthyroidism, three studies reported low T3 syndrome, and the remaining 24 studies did not show the type of thyroid diseases. The detailed characteristics of the included studies are summarized in Table 1.
Quality assessment of included studies
The quality of these included studies was assessed by NOS, and it was found that all of these cohort studies and case series studies get a high-quality assessment (higher than 5 scores).
Association of the severity of COVID-19 infection with thyroid diseases
Of the 53 included studies, 22 studies reported the severity of COVID-19 infection and grouped. Fixed-effects model was used to merge OR values, and the pooled effect size in favor of non-severe patients is 2.62 (95% CI = 1.96–3.49, P < 0.0001), meaning patients with severe COVID-19 infection are more likely to have thyroid diseases. Due to the different types of thyroid diseases and different countries, there exists heterogeneity (heterogeneity test, chi-square = 38.24, P = 0.01, I2 = 45%) (Figure 2). Figures 3, 4 show the subgroup analysis results according to the different countries and types of thyroid diseases in patients with COVID-19 infection. Italy, Spain, and United Kingdom belong to Europe; the remaining countries including China, South Korea, Kuwait, and Saudi Arabia belong to Asia. The analysis subgrouped into Asia and Europe shows that patients with COVID-19 severe infection in Asia are 3.77 times more likely to have thyroid diseases than non-severe patients (fixed-effects model: OR = 3.77, 95% CI = 2.66–5.35, P < 0.00001). No significant statistical heterogeneity was found by the heterogeneity analysis (chi-square = 19.85, P = 0.34, I2 = 9%). Pooled data from three studies conducted in Europe (Italy, Spain, and United Kingdom) did not show the relationship (fixed-effects model: OR = 1.17, 95% CI = 0.68–1.99, P = 0.57) (Figure 3). Subgroup analysis was further conducted by types of thyroid diseases, and the results are shown in Figure 4. Severe COVID-19 infection patients are more likely to be complicated by hypothyroidism and low T3 syndrome. The pooled OR with fixed-effects model in the subgroup of hypothyroidism is 3.72 (95% CI = 1.62–8.58, P = 0.002). No statistical heterogeneity was found by the heterogeneity analysis (chi-square = 3.10, P = 0.54, I2 = 0%). Two studies analyzed the relationship of low T3 syndrome and the severity of COVID-19, and the pooled OR with fixed-effects model is 5.86 (95% CI = 2.79–12.33, P < 0.00001) without any heterogeneity (chi-square = 0.39, P = 0.53, I2 = 0%). In conclusion, COVID-19 infection patients with thyroid diseases are very common, and severe patients are more likely to have thyroid diseases. Asian COVID-19 infection, hypothyroidism patients, and patients with low T3 syndrome are more likely to progress to severe conditions.
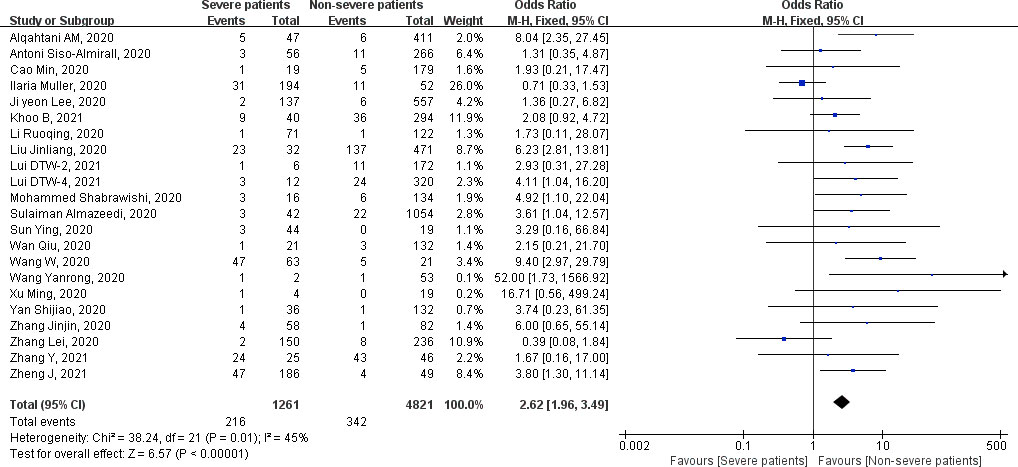
Figure 2 Forest plot of the association of the severity of coronavirus disease 2019 (COVID-19) infection with thyroid diseases.
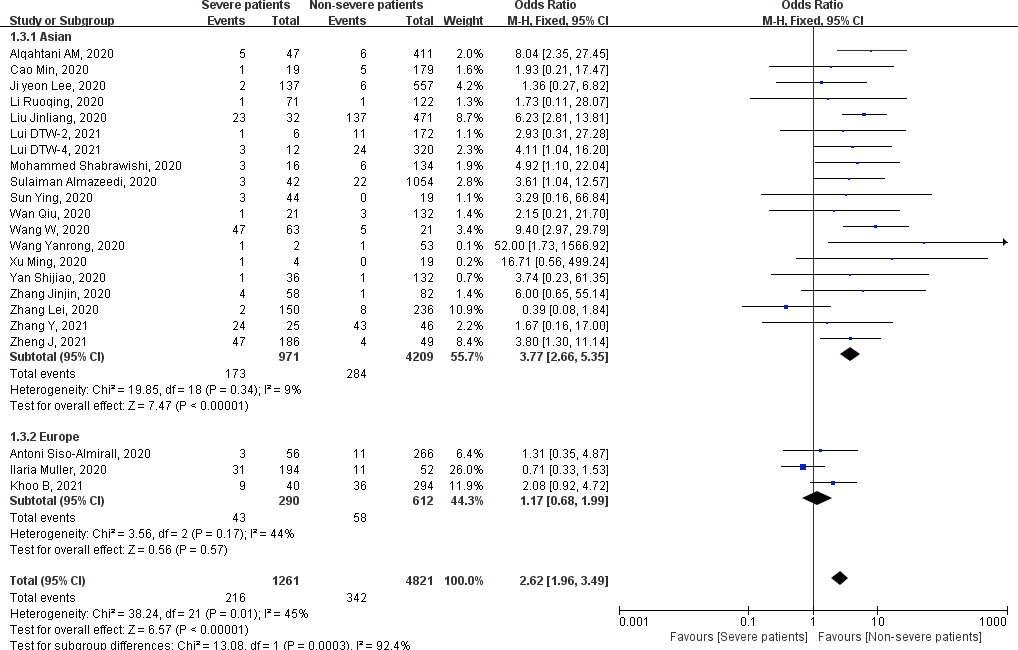
Figure 3 Forest plot of the association of the severity of coronavirus disease 2019 (COVID-19) infection with thyroid diseases in Asia and Europe.
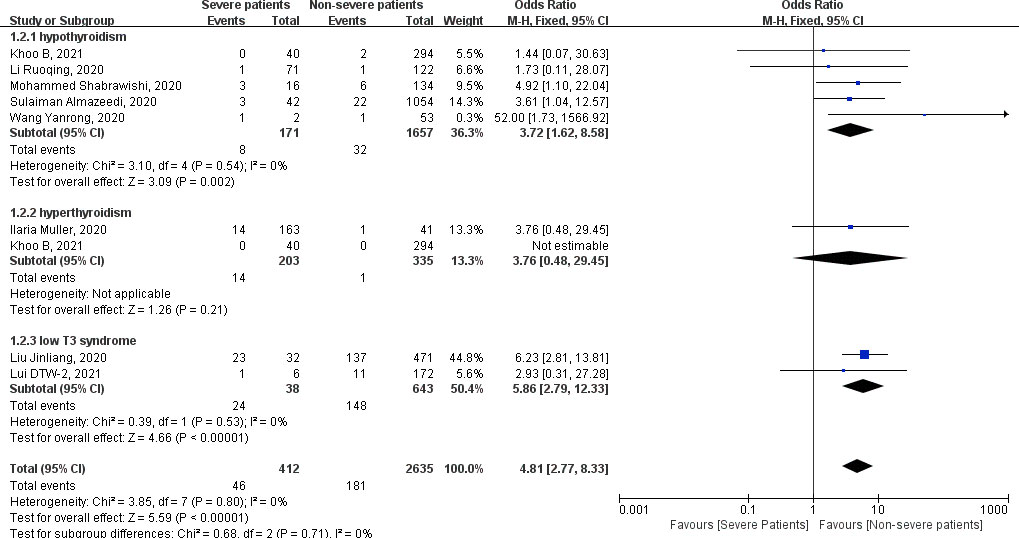
Figure 4 Forest plot of the association of the severity of coronavirus disease 2019 (COVID-19) infection with hypothyroidism, hyperthyroidism, and low T3 syndrome.
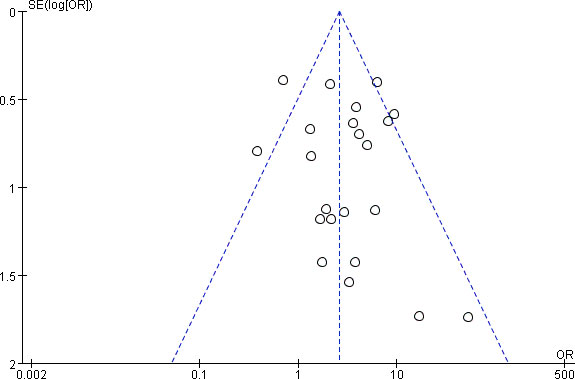
Publication Bias
Funnel plot was done to show the publication bias, and Figure 5 shows a symmetrical funnel plot that indicated that no obvious publication bias existed. Moreover, the Begg’s test and Egger’s test were furtherly done. The P value of the Begg’s test was 0.866, and 0.434 in the Egger’s test, which means that the funnel plot is symmetric and there is no publication bias in the 22 studies selected for this meta-analysis.
Discussion
Studies have found that patients infected with 2019-nCoV have different degrees of disease, and patients with chronic diseases may increase the risk of serious diseases. In our meta-analysis, patients with severe COVID-19 infection were found to be more likely to develop hypothyroidism and low T3 syndrome (58). This is consistent with previous studies. Studies have found that patients with lower thyroid stimulating hormone (TSH) have higher rates of fever (49) and patients with thyroid dysfunction have a poorer prognosis, and our study also found that patients with COVID-19 in Asia with hypothyroidism and low T3 syndrome were more likely to progress to severe infection.
Why does COVID-19 affect the thyroid? COVID-19 was found to affect thyroid tissue and function (59), and three different possible mechanisms have been proposed (60). The first one suggests that high expression of angiotensin converting enzyme 2 (ACE2) and transmembrane serine protease 2 (TMPRSS2) in the thyroid may contribute to SARS-CoV-2 entry. The second possible explanation is that systemic immune activation in response to SARS-CoV-2 infection may lead to thyroid damage. A third hypothesis is that the direct cytotoxic effects of the virus at the pituitary level and the indirect effects through activation of pro-inflammatory cytokine production create a “cytokine storm” that in turn induces NTIS, leading to selective transient pituitary dysregulation (61), which affects thyroid function. This is the most widely recognized reason for the mechanism.
In addition, our study found that Asian patients with COVID-19 who had hypothyroidism and low T3 syndrome were more likely to develop severe infection. So, why are patients with hypothyroidism and low T3 syndrome with neo-coronary pneumonia more likely to develop severe disease?
The invasion of COVID-19 into the body leads to an increase in IL-6, and it has been found that a decrease in free T3 concentration is associated with an increase in IL-6 (13). In addition, thyroid hormones are important in the regulation of innate immune responses (13). Therefore, excessive or insufficient levels of thyroid hormones observed in thyroid disorders would lead to an imbalance in the innate immune response. It is believed that the innate immune response is the front line of the defense system in COVID-19 infections and that a disturbed innate immune response is significantly associated with severe COVID-19 infections (62). Therefore, patients with thyroid disease may have an innate immune system disorder due to abnormal thyroid hormone levels, making patients with neo-coronary pneumonia with combined thyroid disease more likely to have exacerbations. It has been clinically shown that the clinical manifestations of patients with low T3 syndrome and severe neo-coronary pneumonia are closely correlated with various laboratory indices, which may be important indicators affecting the prognosis of patients with severe neo-coronary pneumonia. Patients with low T3 syndrome have a significantly impaired immune system, as evidenced by a significant decline in lymphocytes, which may be a key factor in the death of patients with neointimal pneumonia (8).
In conclusion, it is very common for COVID-19-infected patients to have concomitant thyroid disease, and severe COVID-19 patients are more likely to develop thyroid disease. Asian COVID-19-infected patients, patients with hypothyroidism, and patients with low T3 syndrome are more likely to develop severe disease. Whereas in the present study, the same results were not found in the European population probably due to the fact that the majority of the literature included in this paper was from Asian countries and fewer studies were from European countries, which could lead to potential bias, although no significant statistical heterogeneity was found in the heterogeneity analysis (chi-square = 19.85, P = 0.34, I2 = 9%). We suggest that thyroid disease may affect the immune system, leading to a weakened ability to defend against neo-coronavirus and more likely to lead to exacerbation of the disease, but neo-coronavirus infection may also affect thyroid function by affecting immune factors, thus making this effect more pronounced. Controlling or maintaining normal thyroid function may have a positive effect on the treatment and recovery from neo-coronavirus pneumonia, and care should also be taken to maintain thyroid hormone levels during the treatment of patients with neo-coronavirus pneumonia.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
YT and JZ wrote the manuscript, TW is responsible for data processing, HW is responsible for the figure drawing, JY and SW were responsible for the literature search. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Projects of medical and health technology development program in Shandong province (grant number 2016WS0499), Shandong Provincial Natural Science Foundation of China Grants (grant number ZR2019PH025). They support the study design; the data collection, analysis and interpretation of data; the writing of the report; and the decision to submit the article for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Corman VM, Lienau J, Witzenrath M. Coronaviren als ursache respiratorischer infektionen. Der Internist (2019) 60(11):1136–45. doi: 10.1007/s00108-019-00671-5
2. Huang C, Wang Y, Li X, Ren L, Cao B. Clinical features of patients infected with 2019 novel coronavirus in wuhan, china. Lancet (2020) 395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5
3. Almazrou S. Clinical characteristics and outcomes among covid-19 hospitalized patients with chronic conditions: a retrospective single-center study. J Multidiscip Healthc (2020) 13:1089–1097. doi: 10.2147/JMDH.S273918
4. Wei L, Sun S, Xu CH, Zhang J, Xu J, Zhu H, et al. Pathology of the thyroid in severe acute respiratory syndrome. Hum Pathol (2007) 38:95–102. doi: 10.1016/j.humpath.2006.06.011
5. Zheng J, Cui Z, Shi N, Tian S, Chen T, Zhong X, et al. Suppression of the hypothalamic-pituitary-thyroid axis is associated with the severity of prognosis in hospitalized patients with covid-19. BMC Endocrine Disord (2021) 21(1):228–237. doi: 10.1186/s12902-021-00896-2
6. Leow KS, Kwek SK, Ng WK, Ong KC, Kaw JL, Lee SU. Hypocortisolism in survivors of severe acute respiratory syndrome (sars). Clin Endocrinol (2010) 63(2):197–202. doi: 10.1111/j.1365-2265.2005.02325.x
7. Sciacchitano S, Vitis CD, D'Ascanio M, Giovagnoli S, Mancini R. Gene signature and immune cell profiling by high-dimensional, single-cell analysis in covid-19 patients, presenting low t3 syndrome and coexistent hematological malignancies. J Trans Med (2021) 19(1):139. doi: 10.1186/s12967-021-02805-6
8. Ai X, Yao C, Fu X, Lin L, Xie M, Tan X. Analysis of clinical characteristics and early warning indicators of 128 patients with 2019-n cov infection in guangzhou area. Lingnan J Emergency Med (2020) 25(1):7–9,13. doi: 10.3969/j.issn.1671-301X.2020.01.003
9. Guo Y, Liu W, Li K, Wang S, Liang K, Zhang J. Imact of low T3 syndrome on the prognosis of patieients with sevwere coronavirus disease. J Precis Med (2020) 35(5):453–7. doi: 10.13362/j.jpmed.202005017
10. Huang Z, Xu S, Chen J, Wei Q, Lin L, Ye X, et al. Predictive value of laboratory tests on severity of newly hospitalized patients with COVID-19. Chin J Lab Med (2021) 43(10):973–7. doi: 10.3760/cma.j.cn114452-20200304-00174
11. Li R, Tao J, Yao X, Yang F, Peng P, Tang J, et al. Multi−Center clinical research of risk factors associated with severe and critical patients with coronavirus disease. China Pharm (2020) 29(9):15–8. doi: 10.3969/j.issn.1006−49312020.09.004
12. Li Y, Xu S, Du T, Xu J, Li Y, Yu X, et al. Clinical features of novel coronavirus infection patients and a feasible screening procedur. Chin J Emerg Med (2020) 29(3):336–40. doi: 10.3760/cma.j.issn.1671-0282.2020.03.007
13. Liu H, Li L, Mao C, Xu R, Zhang F, Hu Z, et al. Analyses of the clinical features of 13 corona virus disease 2019 non-survivors. Med J Chin PLA (2020) 445(5):481–5. doi: 10.11855/j.issn.0577-7402.2020.05.03
14. Wan Q, Shhi A, He T, Tang L. Clincal features of 153 patients with COVID 19 in chongqing municipality. Chin J Clin Infect Dis (2020) 13(1):16–20. doi: 10.3760/cma.j.issn.16742397.2020.01.004
15. Wang X, Zhou Z, Yang H, Tian F, Wang C, Cui G, et al. Extrapulmonary organ damage and clinical significance in patients with coronavirus disease 2019. Zhejiang Med (2020) 42(5):485–96. doi: 10.12056/j.issn.1006-2785.2020.42.5.2020-603
16. Wang Q, Li Q, Xu L, Qu J. Clinical features of eight patients with novel corona virus disease 2019 in meishan, sichuan province. Chin J Antibiot (2020) 1–6. doi: 10.13461/j.cnki.cja.007020
17. Wu Q, Song X, Gong X, Liu Q, Liu J, Liu H. Clinical analysis of 55 patients with COVID-19. Jiangsu Med J (2020) 46(6):546–50. doi: 10.19460/cnki.0253-3685.2020.06.002
18. Xiao M, Hou M, Liu X, Li Z, Zhao Q. Clinical characteristics of 71 patients with coronavirus disease 2019. J Cent South Univ (Med Sci) (2020) 7):790–6. doi: 10.11817/j.issn.1672-7347.2020.200187
19. Xu M, Li M, Zhan W, Han T, Liu L, Zhang G, et al. Clinical analysis of 23 patients with coronavirus disease 2019 in xinyang city of henan province. Chin Crit Care Med (2020) 32(2):1–6. doi: 10.3760/cma.j.issn.2095-4352.2020.02.000
20. Xue H, Ming F, Li M, Zhang X, Wang J, Shao J. Clinical characteristics of patients with clustering novel coronavirus pneumonia in nantong. Chin J Clin Med (2020) 27(3):373–7. doi: 10.12025/j.issn.1008-6358.2020.20200422
21. Xue H, Ming F, Tian L, Xu J, Qian H, Han X. Analysis of the clinical characteristics of the first and second generation patients with new coronavirus infection. Med J Commun (2020) 34(2):107–9. doi: 10.19767/j.cnki.32-1412.2020.02.001
22. Zhang L, Jiang W, Zheng Y, Yan Z, Wu B, Li D, et al. Risk factors for disease severity of COVID⁃19. J Pract Med (2020) 36(14):1866–70.
23. Zhao L, Xue J, Wang Y, Dai E, Xu Z, Li Y, et al. The clinical feature and imaging analysis of patients with new coronavirus infection in shijiazhuang. Tianjin Med J (2020) 48(7):588–91. doi: 10.11958/20200360
24. Zhao R, Liang Y, Lin Y, Lu N, Li Q, Li Y, et al. Clinical characteristics of 28 patients with novel coronavirus pneumonia. Chin J Infect Dis (2020) 38(2):90–3. doi: 10.3760/cma.j.issn.10006680.2020.02.007
25. Zhao Ye, Zhong S, Li F, Liu G, Wang X, Liu Z. Digestive tract symptoms in patients with new type of coronary pneumonia in xinyang district, henan province analysis of clinical characteristics and risk factors. Chin J Dig (2020) 40(3):171–5. doi: 10.3760/cma.j.issn.02541432.2020.03.007
26. Zhou F, Zheng C, Wang Z, Yin N, Peng X, Li D. Clinical characteristics of 66 patients with novel coronavirus (2019-nCoV) –infected pneumonia (NCIP) in enshi, hubei. Chin J Emerg Med (2020) 29(04):488–93. doi: 10.3760/cma.j.issn.1671-0282.2020022.001
27. Zou Y, Yu Y, Liu Y, He C, Xu B, Fan C, et al. Relation between disease severity and clinical features in COVID-19 patients. Guangxi Med J (2020) 42(13):1707–12. doi: 10.11675/j.issn.0253-4304.2020.13.21
28. Chandra A, Chakraborty U, Banik B, Bandopadhyay S, Pandey P. Clinical characteristics of hospitalized patients with 2019 novel coronavirus infection in tertiary care centres of three states of india. J Indian Med Assoc (2020) 118(5):31–3. doi: 10.4269/ajtmh.20-1096
29. Zou R, Wu C, Zhang S, Wang G, Zhong Y. Euthyroid sick syndrome in patients with covid-19. Front Endocrinol (2020) 11:566439. doi: 10.3389/fendo.2020.566439
30. Huang Y, Tu M, Wang S, Chen S, Zhou W, Chen D, et al. Clinical characteristics of laboratory confirmed positive cases of sars-cov-2 infection in wuhan, china: a retrospective single center analysis. Travel Med Infect Dis (2020) 36:101606. doi: 10.1016/j.tmaid.2020.101606
31. Bhandari S, Bhargava A, Sharma S, Keshwani P, Banerjee S. Clinical profile of covid-19 infected patients admitted in a tertiary care hospital in north india. J Assoc Phys India (2020) 68(5):13–7.
32. Chen M, Zhou W, Xu W. Thyroid function analysis in 50 patients with covid-19: a retrospective study. Thyroid (2020) 1:8–11. doi: 10.1089/thy.2020.0363
33. Lania A, Sandri MT, Cellini M, Mirani M, Mazziotti G. Thyrotoxicosis in patients with covid-19: the thyrcov study. Eur J Endocrinol (2020) 183(4):381–7. doi: 10.1530/EJE-20-0335
34. Sun D, Chen X, Li H, Lu X, Xiao H, Zhang F, et al. SARS-CoV-2 infection in infants under 1 year of age in wuhan city, China. World J Pediatr (2020) 16(3):260–6. doi: 10.1007/s12519-020-00368-y
35. Wang Z, Wang Z, Xiong G. Clinical characteristics and laboratory results of pregnant women with covid-19 in wuhan, china. Int J Gynecol Obstet (2020) 150(3):312–7. doi: 10.1002/ijgo.13265
36. Muller I, Cannavaro D, Dazzi D, Covelli D, Montavani G, Muscatello A, et al. Sars-cov-2-related atypical thyroiditis. sciencedirect (2020) 8(9):739–41. doi: 10.1016/S2213-8587(20)30266-7
37. Lee JY, Hong SW, Hyun M, Park JS, Lee JH, Suh YS, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in daegu, south korea. Int J Infect Dis (2020) 98:462–6. doi: 10.1016/j.ijid.2020.07.017
38. Sun Y, Dong Y, Wang L, Xie H, Wang FS. Characteristics and prognostic factors of disease severity in patients with covid-19: the beijing experience. J Autoimmun (2020) 112:102473. doi: 10.1016/j.jaut.2020.102473
39. Almazeedi S, Al-Youha S, Jamal MH, Al-Haddad M, Al-Muhaini A, Al-Ghimlas F, et al. Characteristics, risk factors and outcomes among the first consecutive 1096 patients diagnosed with COVID-19 in Kuwait. EClinicalMedicine (2020) 4(24):100448. doi: 10.1016/j.eclinm.2020.100448
40. Cao M, Zhang D, Wang Y, Lu Y, Zhu X, Li Y, et al. Clinical features of patients infected with the 2019 novel coronavirus (COVID-19) in shanghai, China. medRxiv (2020) 6:2020.03.04.20030395. doi: 10.1101/2020.03.04.20030395 (preprint)
41. Liu J, Wu X, Lu F, Zhao L, Shi L, Xu F. Low t3 syndrome is a strong predictor of poor outcomes in patients with community-acquired pneumonia. Sci Rep (2016) 6(1):22271. doi: 10.1038/srep22271
42. Shabrawishi M, Al-Gethamy MM, Naser AY, Ghazawi MA, Alwafi H. Clinical, radiological and therapeutic characteristics of patients with covid-19 in saudi arabia. PLoS One (2020) 15(8):e0237130. doi: 10.1371/journal.pone.0237130
43. Wang Y, Liu Y, Liu L, Wang X, Luo N, Li L, et al. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in shenzhen, China. J Infect Dis (2020) 221(11):1770–4. doi: 10.1093/infdis/jiaa119
44. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with sars-cov-2 in wuhan, china. Allergy (2020) 75(7):1730–41. doi: 10.1111/all.14238
45. Guan W-J, Ni Z-Y, Hu Yu, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in hainan, China. N Engl J Med (2020) 382(18):1708–20. doi: 10.1056/NEJMoa2002032
46. Al Hayek AA, Robert AA, Alotaibi ZK, Al Dawish M. Clinical characteristics of hospitalized and home isolated covid-19 patients with type 1 diabetes. Diabetes Metab Syndrome: Clin Res Rev (2020) 14(6):1841–5. doi: 10.1016/j.dsx.2020.09.013
47. Sisó-Almirall A, Kostov B, Mas-Heredia M, Vilanova-Rotllan S, Benavent-Reu J. Prognostic factors in spanish covid-19 patients: a case series from barcelona. PLoS One (2020) 15(8):e0237960. doi: 10.1371/journal.pone.0237960
48. Gerwen MV, Alsen M, Little C, Barlow J, Genden E. Outcomes of patients with hypothyroidism and covid-19: a retrospective cohort study. Front Endocrinol (2020) 11:565. doi: 10.3389/fendo.2020.00565
49. Lui DTW, Fung MMH, Chiu KWH, Lee CH, Chow WS, Lee ACH, et al. Higher sars-cov-2 viral loads correlated with smaller thyroid volumes on ultrasound among male covid-19 survivors. Endocrine (2021) 74(2):205–14. doi: 10.1007/s12020-021-02855-2
50. Lui TW, Chi HL, Chow WS, Yu CW, Hung I. Thyroid dysfunction in relation to immune profile, disease status and outcome in 191 patients with covid-19. J Clin Endocrinol Metab (2020) 106(2):e926–35. doi: 10.1210/clinem/dgaa813
51. Lui D, Ho LC, Sun CW, Lee A, Raymond TA, Fong C, et al. Insights from prospective follow-up of thyroid function and autoimmunity among covid-19 survivors. J Endocrine Soc (Supplement_1) (2021) 36(3):582–9. doi: 10.3803/EnM.2021.983
52. Calcaterra V, Biganzoli G, Dilillo D, Mannarino S, Fiori L, Pelizzo G, et al. Non-thyroidal illness syndrome and sars-cov-2-associated multisystem inflammatory syndrome in children. J Endocrinol Invest (2021) 45(1):199–208. doi: 10.1007/s40618-021-01647-9
53. Bernard K, Tan T, Clarke SA, Mills EG, Bijal P, Manish M, et al. Thyroid function before, during and after covid-19. J Clin Endocrinol Metab (2020) 106(2):e803–11. doi: 10.1210/clinem/dgaa830
54. Alqahtani AM, Almazrou SH, Almalki ZS, Alanazi AS. Assessing the severity of illness in patients with coronavirus disease in saudi arabia: a retrospective descriptive cross-sectional study. Front Public Health (2020) 8:593256. doi: 10.3389/fpubh.2020.593256
55. Lui DTW, Lee CH, Chow WS, Lee ACH, Tam AR, Fong CHY, et al. Role of non-thyroidal illness syndrome in predicting adverse outcomes in covid-19 patients predominantly of mild to moderate severity. Clin Endocrinol (2021) 95(3):469–77. doi: 10.1111/cen.14476
56. Okwor CJ, Meka IA, Akinwande KS, Edem VF, Okwor VC. Assessment of thyroid function of newly diagnosed SARS-CoV-2 infected patients in Nigeria. Pan Afr Med J (2021) 2(40):9. doi: 10.11604/pamj.2021.40.9.26358
57. Zhang Y, Lin F, Tu W, Zhang J, Pan P. Thyroid dysfunction may be associated with poor outcomes in patients with covid-19. Mol Cell Endocrinol (2021) 521:111097. doi: 10.1016/j.mce.2020
58. Wang W, Su X, Ding Y, Fan W, Teng L. Thyroid function abnormalities in covid-19 patients. Front Endocrinol (2021) 11 623792. doi: 10.3389/fendo.623792
59. Chen T, Wu D, Chen H, Yan W, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ (2020) 368:m1091. doi: 10.1136/bmj.m1091
60. Chen M, Zhou W, Xu W. Thyroid function analysis in 50 patients with COVID-19: a retrospective study. Thyroid (2021) 31:8–11. doi: 10.1089/thy.2020.0363
61. Chen W, Tian Y, Li Z, Zhu J, Wei T, Lei J. Potential interaction between SARS-CoV-2 and thyroid: A review. Endocrinology (2021) 162(3):bqab004. doi: 10.1210/endocr/bqab004
Keywords: thyroid diseases, hypothyroidism, coronavirus disease 2019, COVID-19, meta-analysis
Citation: Tian Y, Zhao J, Wang T, Wang H, Yao J, Wang S and Mou Y (2022) Thyroid diseases are associated with coronavirus disease 2019 infection. Front. Endocrinol. 13:952049. doi: 10.3389/fendo.2022.952049
Received: 24 May 2022; Accepted: 10 August 2022;
Published: 02 September 2022.
Edited by:
Akira Sugawara, Tohoku University, JapanReviewed by:
Pietro Locantore, Catholic University of the Sacred Heart, ItalyMonica Marazuela, Autonomous University of Madrid, Spain
Copyright © 2022 Tian, Zhao, Wang, Wang, Yao, Wang and Mou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yaru Mou, bW91eWFydTE5ODNAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Yutian Tian
Yutian Tian Junyu Zhao
Junyu Zhao Tingting Wang
Tingting Wang Haipeng Wang
Haipeng Wang Jinming Yao
Jinming Yao Song Wang
Song Wang Yaru Mou
Yaru Mou