- 1Department of Dermatology, Rambam Health Care Campus, Haifa, Israel
- 2Department of Dermatology, Center for Blistering Diseases, Tufts University School of Medicine, Boston, MA, United States
The many clinical aspects of anti-p200 pemphigoid are not well-characterized. We aimed to analyze and correlate known existing data on the epidemiological, clinical, histological, and immunological features of anti-p200 pemphigoid. We performed a review using Medline, Embase, and Web of Science databases (1900–2018). Case reports and series of patients were included. A total of 68 eligible studies that comprised 113 anti-p200 pemphigoid patients were included in the qualitative analysis, where there was a mean age of onset of 65.5 years. All patients presented with bullae/vesicles, and 54.3% had urticarial plaques. A similarity to bullous pemphigoid was reported in 66.1% of cases, but palmoplantar (51.4%), cephalic (40.3%), and mucosal (38.5%) involvement, besides frequent development of scars/milia (15.7%), were reported. Autoantibodies against recombinant laminin γ1 were detected in the sera of 73.1% of patients. Psoriasis was present in 28.3% of anti-p200 pemphigoid patients, particularly among Japanese patients (56.4%). The incidence of pustular psoriasis in this subgroup, was significantly greater than in the normal population. In conclusion, the diagnosis of anti-p200 pemphigoid may be suspected when a subepidermal autoimmune blistering disease develops in a younger age group, along with significant acral and cephalic distribution and mucosal involvement.
Introduction
Anti-p200 pemphigoid is a rare subepidermal autoimmune bullous disease (AIBD) initially described in 1996 (1, 2). This novel disease, presumed to be a subset of pemphigoid, was characterized by autoantibodies targeting a 200-kDa protein localized within the lower lamina lucida of the basement membrane zone (BMZ). Their sera bound to the dermal side of salt-split skin by indirect immunofluorescence (IIF) microscopy (3). Subsequent studies demonstrated that sera from 90% of anti-p200 pemphigoid patients recognized laminin γ1, which C-terminus was identified as an immunodominant region and utilized for immunoblotting and ELISA for diagnosis (4, 5). In outstanding research by German and Japanese investigators, using human foreskin and various mouse strains, the investigators clearly demonstrated that autoantibodies in anti-p200 pemphigoid sera are pathogenic, but their pathogenicity is not entirely mediated by autoantibodies against laminin γ1. The specific or precise role for laminin γ1 in pathogenesis requires further study, as ex vivo and in vivo studies did not show evidence of a direct pathogenic role of anti-laminin γ1 antibodies, leaving the true molecular identity of the pathogenic 200 kDa autoantigen yet to be fully characterized (6, 7). To elaborate, in two different mouse animal models for anti-laminin γ1 pemphigoid, although murine IgG of the recombinant laminin γ1 C-terminus bound to the epidermal basement membrane zone in the passive transfer model, no obvious blister formation was seen (7). In an earlier ex vivo model of autoantibody-mediated leukocyte-dependent neutrophil activation, human and rabbit IgG from the C-terminus of laminin γ1 failed to attract neutrophils at the dermal-epidermal-junction and to induce dermal-epidermal separation (6).
The clinical presentation of anti-p200 is polymorphic and may mimic bullous pemphigoid (BP), mucous membrane pemphigoid (MMP), and other subepidermal AIBD (8). However, data on its morphological features and the clinical course are limited, primarily because of the small number of reported cases and the lack of a large cohort of patients studied in detail with long-term follow-up.
We did not focus on therapy because it was considered beyond the scope of this analysis due to lack of uniformity, cohesive information, defined protocol, and outcome data. The aim of the current study was to perform a review of the available epidemiological, clinical, histological, and immunopathological data and the major comorbidities in patients with anti-p200 pemphigoid. The purpose was to help clinicians recognize this newly described clinical entity. This could result in early therapy and better prognosis.
Materials and Methods
Data Collection
The literature review was conducted using Ovid-Medline (1946–present), Embase (1947–present), and Web of Science (1900–present) to identify eligible articles. Publications until August 9th 2018, were searched. The search strategies are detailed in Supplementary Table 1.
Selection of Articles
All publications reporting on one or multiple cases of anti-p200 pemphigoid were included. All cases were defined by the authors of the respective publications as anti-p200 pemphigoid based on the following three mandatory criteria: (i) clinical profile suggestive of subepidermal AIBD; (ii) reactivity to the 200 kDa protein or to the recombinant C-terminus of laminin γ1 by immunoblot analysis; and (iii) exclusion of other subepidermal AIBDs. Additionally, at least one of the following two minor criteria was required to establish the diagnosis of anti-p200 pemphigoid: (i) subepidermal cleft on histology; (ii) and direct immunofluorescence (DIF), demonstrating linear deposition of IgG and/or C3. Publications lacking these criteria were excluded.
Data Extraction
The following information was obtained when authors provided it: age at onset, sex, ethnicity, morphological features of the mucocutaneous manifestation and their anatomic distribution, histopathology, immunopathology, comorbidities, and triggering factors (if known). All statistical analysis was performed using SPSS software, version 23 (SPSS, Chicago, IL, USA).
Results
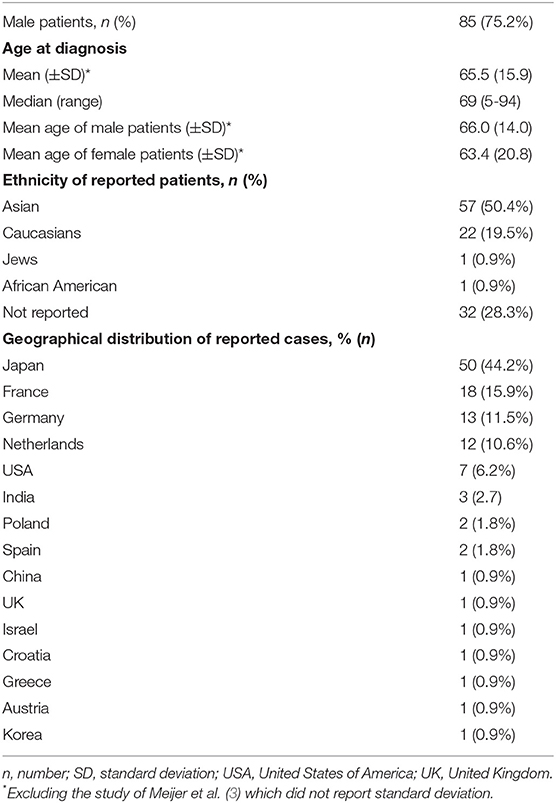
After a full-text review, 68 articles fulfilled the inclusion criteria, thereby providing 113 patients from 15 different countries that were included in the qualitative synthesis. Between 1996 and 2018, 50 cases (44.2%) were reported from Japan (Table 1).
Clinical Characteristics
The mean age at onset was 65.5 years (range 5–94) (9, 10). The majority of the patients were males (n = 85; 75.2%) and of Asian ancestry (n = 57, 50.4%; Table 1).
The clinical presentation was described as resembling other subepidermal AIBD and inflammatory dermatoses by authors in 68 (60.2%) patients. The leading similar condition was BP (n = 45; 66.2%), followed by linear IgA bullous dermatosis (LABD; n = 5; 7.4%) (9, 11–14), epidermolysis bullosa acquisita (EBA; n = 3; 4.4%) (15–17), dermatitis herpetiformis (DH; n = 3; 4.4%) (18–20), mucous membrane pemphigoid (n = 3; 4.4%) (21–23), and others (Table 2). In the remaining 45 patients, a similarity to a distinct clinical entity was not mentioned.
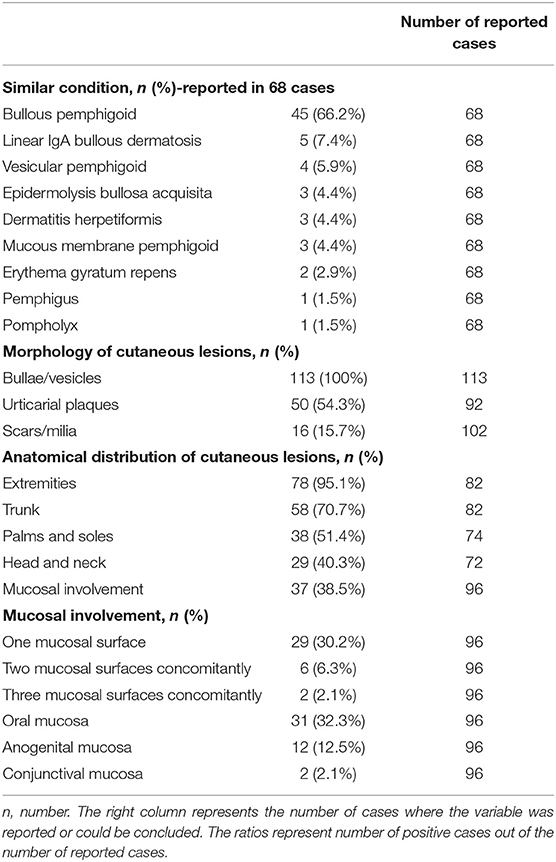
Table 2. Clinical and morphological characteristics of the reported patients with anti-p200 pemphigoid.
All patients presented with bullae and/or vesicles, 54.3% (50/92) had urticarial plaques, 15.7% (16/102) had scars and/or milia (Table 2).
The distribution of cutaneous lesions was reported in 72 patients. The extremities were the most frequently involved (95.1%), the trunk in 70.7%, and palmoplantar and cephalic involvement in 51.4 and 40.3% of patients, respectively. Generalized involvement was reported in 41.5% of patients. Mucosal involvement was reported in 38.5% of patients, with the oral mucosa (32.3%) being the most frequently involved. None of the patients had exclusively mucosal diseases (Table 2). Of great interest, the prevalence of mucosal involvement among Japanese patients (22.5%) was significantly lower when compared to the remaining patients (48.2%; P < 0.001).
Histological Characteristics
Histology data was available on 100 (88.5%) patients. A subepidermal blistering was observed in all patients, along with mild to dense inflammatory infiltrates in the upper dermis composed of neutrophils and eosinophils in 41 (41.0%) and 15 (15.0%) patients, respectively. A mixed infiltrate of neutrophils and eosinophils was seen in 40 (40.0%) of patients. In two patients, an exclusively lymphocytic infiltrate was observed (24, 25); papillary microabscesses were observed in 11 (11.0%) patients, a predominantly neutrophilic infiltrate in 10 patients (2, 14, 18–20, 26–29) and a mixed infiltrate in one patient (3). Eosinophilic spongiosis was observed in two patients (3, 27) and ruptured secondary milia with inflammatory granulomatous in one patient (16).
Immunopathological Characteristics
DIF microscopy of perilesional skin was reported in 98 (88.1%) patients. Deposition of IgG and C3 was observed in 77 (78.6%), whereas the simultaneous deposition of IgG, IgA, and C3 was observed in 10 (10.2%) patients (3, 9, 12, 14, 20, 30). Deposition of IgG or C3 alone was observed in two (2.0%) (16, 31) and four (4.1%) patients (22, 32–34), respectively. N-serration deposition pattern from a BMZ immunoreactant was shown in 11 of 13 (84.6%) patients, whereas this pattern was undetermined in the remaining two (15.4%) patients (3, 35, 36) (Table 3).
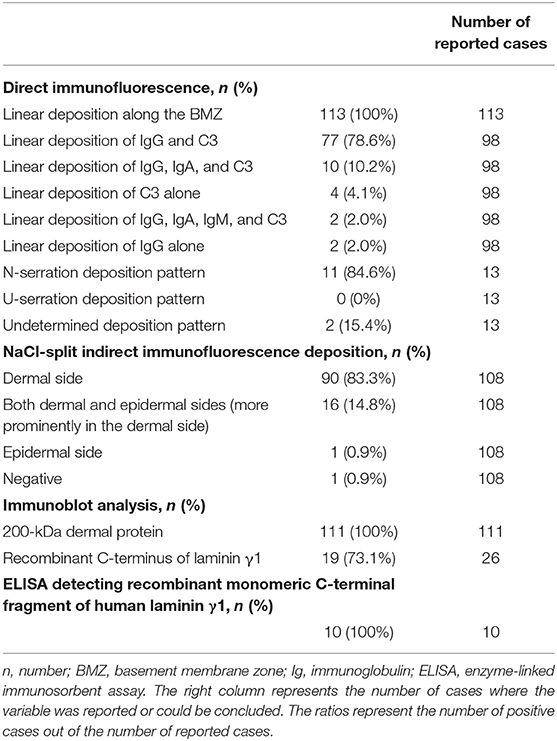
Table 3. Immunopathological and immunological characteristics of the reported patients with anti-p200 pemphigoid.
On salt-split skin, binding to the dermal side of the split was reported in 90 patients (83.3%) and binding to both the dermal and epidermal sides in 16 patients (14.8%) (Table 3). Immunoblot analysis demonstrated reactivity to the 200 kDa protein in all 111 patients tested using human dermal extract (n = 108), epidermal extracts (n = 11) (10, 37) and keratinocytes extracts (n = 2) (32). Sera of several patients were tested on multiple extracts, and 10 of the 11 patients reacting to the epidermal extract were also seropositive on dermal extracts (10). In the remaining two patients, immunoblotting showed reactivity only to the recombinant C-terminus of laminin γ1 (38, 39). Of significant interest is that the sera of patients who were positive for antibodies when tested using immunoblot analysis with the recombinant C-terminus of laminin γ1 was positive in 17 of 24, with a 70.8% sensitivity (3, 9, 31, 38–43). Sera of 10 patients was tested by ELISA bound to a recombinant monomeric C-terminal fragment of human laminin γ1 (10, 44, 45) (Table 3).
Autoantibodies targeting other antigens were detected in 20 (17.7%). Autoantibodies against BP-180 alone, BP-230 alone and both BP-180 and BP-230 were identified in two (1.8%) (19, 46), four (3.5%) (2, 36, 47), and three (2.7%) patients (10, 48), respectively. Antibodies to Type-VII collagen were found in three (2.7%) patients (15, 16, 49), whereas autoantibodies against different subunits of laminin 332 were detected in 7 (6.2%) patients (21, 22, 34, 44, 50–52).
Associated Comorbidities
An association with psoriasis was reported in 32 patients (28.3%). Psoriasis preceded the diagnosis of anti-p200 pemphigoid in all patients by a mean of 15.1 ± 10.4 years (median, 18 years; range, 0.1–30 years). Four (12.5%) patients had developed bullous disease with pustular psoriasis simultaneously (33, 35, 53, 54). The onset of anti-p200 pemphigoid was associated with erythrodermic psoriasis in one (3.1%) patient (55). The remaining patients (84.4%) had psoriasis vulgaris. Of interest, 28 (87.5%) patients with psoriasis were Japanese, whereas the remaining four (12.5%) were Europeans (10, 27, 56, 57).
Taken together, the prevalence of psoriasis in anti-p200 pemphigoid Japanese patients was 56.0% (95% CI, 42.3–68.8%) as compared to only 6.4% (95% CI, 2.5–15.2%) among non-Japanese patients (P < 0.001). There was a slightly higher frequency of males among anti-p200 pemphigoid patients with psoriasis compared to those without psoriasis (87.5 vs. 70.4%; P = 0.058). The age of presentation was comparable in the two subgroups (data not shown).
Concomitant malignancies were reported in three female patients. One had metastatic clear cell carcinoma of the ovary (21), one had uterine adenocarcinoma (58), and the other had metastatic esophageal adenocarcinoma (38). Other comorbidities reported included: end-stage kidney disease due to IgA nephropathy and glomerulonephritis (n = 2) (22, 34), ulcerative colitis (n = 1) (50), esophagitis (n = 1) (15), polyarteritis nodosa (n = 1) (59), and autosomal recessive congenital ichthyosis (n = 1) (36). Unproven trigger factors included scabies (n = 2) (60, 61) and use of penicillin (n = 1) (62).
Discussion
This review highlights the multiple aspects of a recently described interesting subset of pemphigoid. Based on the current information, its main focus is the clinical features. Many of the unique characteristics and associations could be important to cutaneous biology and the pathogenesis of autoimmunity. A heterogeneous clinical profile that mimicked BP was present in the majority of patients, accompanied by a high prevalence of cephalic, palmoplantar and mucosal involvement. Autoantibodies against the recombinant C-terminus of laminin γ1 were detected by immunoblotting in 73.1% of patients. The prevalence of coexistent psoriasis was significantly higher than in the general population. Interestingly, the presence of psoriasis was very significantly higher in Japanese than non-Japanese patients (56.0 vs. 6.4%, respectively).
Palmoplantar lesions and mucosal involvement in BP has been reported in up to 20% of patients (63–65), and these regions were affected in 51.4 and 38.5% of patients with anti-p200 pemphigoid, respectively. Interestingly, scars and milia were reported in 3.4% of patients with BP (63) but in 15.7% of patients with anti-p200 pemphigoid. In the clinical criteria suggested by Vaillant et al. (66), which yield a positive predictive value of 95% for a clinical diagnosis of BP, it is the absence of each of the three aforementioned features that has been identified as an independent predictive criterion for the diagnosis of BP.
The age at onset of patients with anti-p200 pemphigoid (65.5 years) is younger than many with BP, where it commonly occurs in those older than 70 (67–69). An overwhelming preponderance of males (75.2%) were reported with anti-p200 pemphigoid, which contrasts with the female-to-male ratio ranges between 1.04 and 5.1 in different cohorts of BP (69).
In 2009, Dainichi et al. (4) found that 90% of sera tested from anti-p200 pemphigoid patients reacted to the C-terminus of recombinant laminin γ1, using an immunoblot assay. This observation has been confirmed by Groth et al. (5). This analysis demonstrates that sera from 73.1% of the patients reported reacting to the C-terminus of recombinant laminin γ1 protein using the immunoblotting assay. With respect to the ELISA using a monomeric C-terminal fragment of human laminin, the sensitivity was estimated at 68.6% (5).
The incidence of anti-p200 pemphigoid is considerably low amongst AIBD (70). In a cohort of 145 Japanese patients with various AIBDs, anti-p200 pemphigoid was the second most prevalent AIBD (37.2%). The prevalence of psoriasis among non-Japanese anti-p200 pemphigoid patients (6.4%) was greater than its incidence in the general population of the world (71, 72). The pathomechanism of this ethnic association is yet to be established (70). Pustular psoriasis was present in 12.5% of p-200 pemphigoid patients. This incidence is significantly higher than the 1.3% reported in a cohort of 104,669 patients with different variants of psoriasis (P < 0.001) (73). This observation confirmed an earlier Japanese study which reported that 53.8% of patients with pustular psoriasis and AIBD had anti-p200 pemphigoid (70). The molecular basis for this rare and unique combination of clinical entities has not been clearly defined and warrants attention. Senescence was suggested to alter the distribution and amount of proteins in the BMZ, thus increasing its antigenicity and raising the risk of the development of an autoimmune response against its components (74). Since the cell cycle and turnover of the epidermal keratinocytes are extremely accelerated in psoriasis, it was recently assumed that the extracellular matrix in psoriatic skin may simulate the senescent extracellular matrix and contribute to the development of BP and other AIBDs that were found to be associated with psoriasis (75).
Our current knowledge of anti-p-200 pemphigoid brings into focus several important and interesting issues. Traditionally, pemphigoid is divided into BP and mucous membrane pemphigoid. It is possible that because anti-p200 pemphigoid has certain features of both conditions, it could be the bridge or missing link between them. Some anti-p200 pemphigoid also has features of other AIBD, since their sera contain autoantibodies associated with them. It would be interesting to speculate whether this was due to epitope spreading (76). Patients with systemic lupus erythematosus have multiple pathogenic autoantibodies per patient (77), including multiple phenotypes and symptomatologies.
An additional unsolved question is whether anti-p-200 pemphigoid is truly rare or whether it is rather underdiagnosed worldwide. In the US, tests for detecting autoantibodies to laminin γ1 are commercially unavailable, though they are available in Germany and Japan. Moreover, investigators in those countries, whose laboratories are equipped to perform these assays, provide them to their colleagues. The majority of patients are thus reported from Japan and Europe. Unless there are very specific unidentified reasons, there are generally no reasons to believe that it cannot not be as prevalent in other countries. Unless more patients are studied, serologically characterized and followed up for several years, this challenging variant of pemphigoid will remain less well-studied and understood. This would be tragic, because it could help advance our knowledge.
The main limitations of this review are that it was based on case reports and small case series and that it is retrospective. Some of the variables were not provided by some authors. Data on treatment were scarce, limited and not comprehensive. Limited follow-up did not provide a clear clinical course or an overview of the impact of treatment on clinical course. The universal lack of the ELISAs makes it impossible to assess its global presence. Since psoriasis is present universally, its relationship could not be accurately assessed.
In conclusion, this new subset provides, to clinicians and scientists alike, a unique opportunity to study several new frontiers of cutaneous biology, inflammation, immunology, scar formation and disease pathogenesis. The location of laminin γ1 provides the opportunity to study interactions amongst other BMZ proteins. An association with psoriasis provides a playground to study what influences neutrophils to cause different pathologies and clinical profiles. The presence of scarring in mucosal tissues of some patients and not in others could provide important leads into what thrusts patients into one direction or the other. This opportunity, provided by nature, should not be missed but utilized to the advantage of our patients and the progress of our specialty.
Author Contributions
AA and KK contributed to the concept, content, and writing of the manuscript.
Funding
This study was supported in part by an unrestricted educational grant from the Dysimmune Diseases Foundation, Panama City, FL, USA.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2019.02466/full#supplementary-material
References
1. Zillikens D, Kawahara Y, Ishiko A, Shimizu H, Mayer J, Rank CV, et al. A novel subepidermal blistering disease with autoantibodies to a 200-kDa antigen of the basement membrane zone. J Invest Dermatol. (1996) 106:1333–8. doi: 10.1111/1523-1747.ep12349283
2. Chen KR, Shimizu S, Miyakawa S, Ishiko A, Shimizu H, Hashimoto T. Coexistence of psoriasis and an unusual IgG-mediated subepidermal bullous dermatosis: identification of a novel 200-kDa lower lamina lucida target antigen. Br J Dermatol. (1996) 134:340–6. doi: 10.1111/j.1365-2133.1996.tb07625.x
3. Meijer JM, Diercks GFH, Schmidt E, Pas HH, Jonkman MF. Laboratory diagnosis and clinical profile of anti-p200 pemphigoid. JAMA Dermatol. (2016) 152:897–904. doi: 10.1001/jamadermatol.2016.1099
4. Dainichi T, Kurono S, Ohyama B, Ishii N, Sanzen N, Hayashi M, et al. Anti-laminin gamma-1 pemphigoid. Proc Natl Acad Sci USA. (2009) 106:2800–5. doi: 10.1073/pnas.0809230106
5. Groth S, Recke A, Vafia K, Ludwig RJ, Hashimoto T, Zillikens D, et al. Development of a simple enzyme-linked immunosorbent assay for the detection of autoantibodies in anti-p200 pemphigoid. Br J Dermatol. (2011) 164:76–82. doi: 10.1111/j.1365-2133.2010.10056.x
6. Vafia K, Groth S, Beckmann T, Hirose M, Dworschak J, Recke A, et al. Pathogenicity of autoantibodies in anti-p200 pemphigoid. PLoS ONE. (2012) 7:e41769. doi: 10.1371/journal.pone.0041769
7. Koga H, Ishii N, Dainichi T, Tsuruta D, Hamada T, Ohata C, et al. An attempt to develop mouse model for anti-laminin gamma 1 pemphigoid. J Dermatol Sci. (2013) 70:108–15. doi: 10.1016/j.jdermsci.2013.01.001
8. Goletz S, Hashimoto T, Zillikens D, Schmidt E. Anti-p200 pemphigoid. J Am Acad Dermatol. (2014) 71:185–91. doi: 10.1016/j.jaad.2014.02.036
9. Patsatsi A, Meltzanidou P, Katafigiotis S, Sotiriadis D, Schmidt E, Lambropoulos A. Chronic bullous disease of childhood with IgG reactivity to p200 antigen. Int J Dermatol. (2017) 56:773–5. doi: 10.1111/ijd.13616
10. Commin MH, Schmidt E, Duvert-Lehembre S, Lasek A, Morice C, Estival JL, et al. Clinical and immunological features and outcome of anti-p200 pemphigoid. Br J Dermatol. (2016) 175:776–81. doi: 10.1111/bjd.14629
11. Myers DJ, Unwala RD, Xia L, Groth S, Zillikens D, Stratman EJ. Generalized annular bullous eruption–quiz case. Anti-laminin gamma1 pemphigoid with a linear IgA bullous dermatosis-like presentation. Arch Dermatol. (2011) 147:109–14. doi: 10.1001/archdermatol.2010.404-a
12. Kawahara Y, Matsuo Y, Hashimoto T, Nishikawa T. A case of unique subepidermal blistering disease with autoantibodies against a novel dermal 200-kD antigen. Dermatology. (1998) 196:213–6. doi: 10.1159/000017901
13. Goto-Ohguchi Y, Nishie W, Akiyama M, Tateishi Y, Aoyagi S, Tsuji-Abe Y, et al. A severe and refractory case of anti-p200 pemphigoid resulting in multiple skin ulcers and scar formation. Dermatology. (2009) 218:265–71. doi: 10.1159/000182268
14. Watanabe M, Tsunoda T, Tagami H. A subepidermal blistering dermatosis associated with coexistent IgG and IgA anti-dermal basement membrane zone antibodies; demonstration of IgG antibodies reactive against a 200-kDa dermal antigen. Eur J Dermatol. (2002) 12:603–6.
15. Yamada T, Suzuki M, Koike Y, Kida K, Murata S, Ishii N, et al. A case of epidermolysis bullosa acquisita with autoantibody to anti-p200 pemphigoid antigen and exfoliative esophagitis. Dermatology. (2006) 212:381–4. doi: 10.1159/000092292
16. Pastar Z, Rados J, Lipozencic J, Dobric I, Marinovic B, Ishii N, et al. Case of concurrent epidermolysis bullosa acquisita and anti-p200 pemphigoid - How to treat it? Int J Dermatol. (2007) 46:295–8. doi: 10.1111/j.1365-4632.2006.02969.x
17. Umemoto N, Demitsu T, Toda S, Noguchi T, Suzuki SI, Kakurai M, et al. A case of anti-p200 pemphigoid clinically mimicking inflammatory epidermolysis bullosa acquisita [1]. Br J Dermatol. (2003) 148:1058–60. doi: 10.1046/j.1365-2133.2003.05312.x
18. Wozniak K, Hashimoto T, Fukuda S, Ohyama B, Ishii N, Koga H, et al. IgA anti-p200 pemphigoid. Arch Dermatol. (2011) 147:1306–10. doi: 10.1001/archdermatol.2011.303
19. Salmhofer W, Kawahara Y, Soyer HP, Kerl H, Nishikawa T, Hashimoto T. A subepidermal blistering disease with histopathological features of dermatitis herpetiformis and immunofluorescence characteristics of bullous pemphigoid: a novel subepidermal blistering disease or a variant of bullous pemphigoid? Br J Dermatol. (1997) 137:599–604. doi: 10.1111/j.1365-2133.1997.tb03794.x
20. Yasuda H, Tomita Y, Shibaki A, Hashimoto T. Two cases of subepidermal blistering disease with anti-p200 or 180-kd bullous pemphigoid antigen associated with psoriasis. Dermatology. (2004) 209:149–55. doi: 10.1159/000079602
21. Mitsuya J, Hara H, Ito K, Ishii N, Hashimoto T, Terui T. Metastatic ovarian carcinoma-associated subepidermal blistering disease with autoantibodies to both the p200 dermal antigen and the γ2 subunit of laminin 5 showing unusual clinical features. Br J Dermatol. (2008) 158:1354–7. doi: 10.1111/j.1365-2133.2008.08483.x
22. Mitate E, Kawano S, Nakao Y, Goto Y, Kobayashi I, Onozawa K, et al. Concurrence of autoantibodies to both laminin γ1 and γ2 subunits in a patient with kidney rejection response. Acta Derm Venereol. (2013) 93:114–5. doi: 10.2340/00015555-1395
23. Zhiliang L, Xiaodong Z, Peiying J, Suying F, Baoxi W. A case of refractory antilaminin γ1 pemphigoid successfully treated with dexamethasone and mycophenolate mofetil. Int J Dermatol. (2015) 54:e194–6. doi: 10.1111/ijd.12763
24. Waki Y, Kamiya K, Komine M, Maekawa T, Murata S, Ishii N, et al. A case of anti-laminin gamma1 (p200) pemphigoid with psoriasis vulgaris successfully treated with apremilast. Eur J Dermatol. (2018) 28:413–4. doi: 10.1684/ejd.2018.3280
25. Majima Y, Yagi H, Tateishi C, Groth S, Schmidt E, Zillikens D, et al. A successful treatment with ustekinumab in a case of antilaminin-gamma1 pemphigoid associated with psoriasis. Br J Dermatol. (2013) 168:1367–9. doi: 10.1111/bjd.12163
26. Mascaro JMJ, Zillikens D, Giudice GJ, Caux F, Fleming MG, Katz HM, et al. A subepidermal bullous eruption associated with IgG autoantibodies to a 200 kd dermal antigen: the first case report from the United States. J Am Acad Dermatol. (2000) 42:309–15. doi: 10.1016/S0190-9622(00)90101-4
27. García-Díez I, Martínez-Escala ME, Ishii N, Hashimoto T, Mascaró Galy JM, Pujol RM, et al. Usefulness of a simple immunohistochemical staining technique to differentiate anti-p200 pemphigoid from other autoimmune blistering diseases: a report of 2 cases. Actas Dermosifiliogr. (2016) 108:e1–5. doi: 10.1016/j.adengl.2016.11.018
28. Rose C, Weyers W, Denisjuk N, Hillen U, Zillikens D, Shimanovich I. Histopathology of anti-p200 pemphigoid. Am J Dermatopathol. (2007) 29:119–24. doi: 10.1097/DAD.0b013e31803326e6
29. Egan CA, Yee C, Zillikens D, Yancey KB. Anti-p200 pemphigoid: diagnosis and treatment of a case presenting as an inflammatory subepidermal blistering disease. J Am Acad Dermatol. (2002) 46:786–9. doi: 10.1067/mjd.2002.120923
30. Kingsbery MY, Grossman ME, Nguyen H. Consider antilaminin gamma-1 pemphigoid when faced with conflicting histopathology and immunofluorescence results. J Am Acad Dermatol. (2013) 68:e60–1. doi: 10.1016/j.jaad.2012.08.038
31. Iikawa M, Muroi E, Ishii Y, Mochid AK, Setoyama M, Kurokawa M, et al. A case of anti-laminin gamma; 1 pemphigoid with cutaneous polyarteritis nodosa. Nishi Nihon Hifuka. (2013) 75:7–10. doi: 10.2336/nishinihonhifu.75.7
32. Hofmann SC, Voith U, Sasaki TS, Trueeb RM, Nischt RN, Bruckner-Tuderman L. Evidence for synthesis of p200, the autoantigen in anti-p200 pemphigoid, by keratinocytes and fibroblasts. J Invest Dermatol. (2007) 127:S73. doi: 10.1038/sj.jid.5700952
33. Miyakura T, Yamamoto T, Tashiro A, Okubo Y, Oyama B, Ishii N, et al. Anti-p200 pemphigoid associated with annular pustular psoriasis. Eur J Dermatology. (2008) 18:481–2. doi: 10.1684/ejd.2008.0465
34. Kamata M, Fujita H, Hamanaka T, Takahashi K, Koga H, Hashimoto T, et al. Anti-laminin gamma1 pemphigoid accompanied by autoantibodies to laminin alpha3 and gamma2 subunits of laminin-332. JAMA Dermatol. (2013) 149:1437–9. doi: 10.1001/jamadermatol.2013.5358
35. Igarashi M, Tsunemi Y, Koga H, Hashimoto T, Tateishi C, Tsuruta D, et al. Anti-laminin gamma1 pemphigoid associated with pustular psoriasis. Eur J Dermatol. (2014) 24:629–30. doi: 10.1684/ejd.2014.2419
36. Ohzone A, Numata S, Hamada T, Fukuda S, Teye K, Shirakashi Y, et al. Anti-laminin-gamma 1 pemphigoid developed in a case of autosomal recessive congenital ichthyosis. Acta Derm Venereol. (2015) 95:93–4. doi: 10.2340/00015555-1875
37. Munsch C, Prey S, Joly P, Meyer N, Lamant L, Livideanu C, et al. [Anti-p200 pemphigoid: a spectacular response to dapsone]. Ann Dermatol Venereol. (2011) 138:739–42. doi: 10.1016/j.annder.2011.05.024
38. Goetze S, Dumke A-K, Zillikens D, Hipler UC, Elsner P. Anti-p200/laminin gamma1 pemphigoid associated with metastatic oesophageal cancer. J Eur Acad Dermatol Venereol. (2017) 31:e219–21. doi: 10.1111/jdv.13983
39. Tatsumi M, Kamei R, Nakai D, Mabuchi E, Ikegami E, Fukuda S, et al. Complicated case of anti-laminin gamma-1 pemphigoid in psoriasis. Ski Res. (2012) 11:75–81. doi: 10.11340/skinresearch.11.1_75
40. McCarty M, Zillikens D, Fivenson D. Anti-p200 pemphigoid (anti-laminin-gamma1 pemphigoid) demonstrating pathergy. Int J Women Dermatol. (2015) 1:173–4. doi: 10.1016/j.ijwd.2015.09.002
41. Alloo A, Strazzula L, Rothschild B, Hawryluk E, Levine D, Hoang MP, et al. Refractory antilaminin γ1 pemphigoid successfully treated with intravenous immunoglobulin and mycophenolate mofetil. J Eur Acad Dermatology Venereol. (2014) 28:1401–3. doi: 10.1111/jdv.12352
42. Goyal N, Rao R, Shenoi S, Pai S, Kumar P, Bhogal B, et al. Epidermolysis bullosa acquisita and anti-p200 pemphigoid as major subepidermal autoimmune bullous diseases diagnosed by floor binding on indirect immunofluorescence microscopy using human salt-split skin. Indian J Dermatol Venereol Leprol. (2017) 83:550–5. doi: 10.4103/ijdvl.IJDVL_678_16
43. Geller S, Gat A, Zeeli T, Schmidt E, Ishii N, Hashimoto T, et al. A refractory, cutaneous, subepidermal bullous disease. Clin Exp Dermatol. (2016) 41:573–5. doi: 10.1111/ced.12823
44. Monshi B, Groth S, Richter L, Schmidt E, Zillikens D, Rappersberger K. A long-term study of a patient with anti-p200 pemphigoid: correlation of autoantibody levels with disease activity and an example of epitope spreading. Br J Dermatol. (2012) 167:1179–83. doi: 10.1111/j.1365-2133.2012.11076.x
45. Ishida S, Takahashi K, Kanaoka M, Okawa T, Tateishi C, Yasukochi A, et al. Case of subepidermal autoimmune bullous disease with psoriasis vulgaris reacting to both BP180 C-terminal domain and laminin gamma-1. J Dermatol. (2015) 42:391–3. doi: 10.1111/1346-8138.12801
46. Ansai S-I, Hashizume S, Kawana S, Tateishi C, Koga H, Hashimoto T. Case of anti-laminin gamma-1 pemphigoid with antibody against C-terminal domain of BP180 in a patient with psoriasis vulgaris. J Dermatol. (2014) 41:1031–3. doi: 10.1111/1346-8138.12625
47. Kawahara Y, Zillikens D, Yancey KB, Marinkovich MP, Nie Z, Hashimoto T, et al. Subepidermal blistering disease with autoantibodies against a novel dermal 200-kDa antigen. J Dermatol Sci. (2000) 23:93–102. doi: 10.1016/S0923-1811(99)00093-6
48. Imanishi A, Tateishi C, Imanishi H, Sowa-Osako J, Koga H, Tsuruta D, et al. Pemphigoid with antibodies to laminin gamma 1, BP180 and BP230, associated with psoriasis vulgaris: Successful disease control with cyclosporin. J Dermatol. (2015) 42:394–7. doi: 10.1111/1346-8138.12798
49. Furukawa H, Miura T, Takahashi M, Nakamura K, Kaneko F, Ishii F, et al. A case of anti-p200 pemphigoid with autoantibodies against both a novel 200-kD dermal antigen and the 290-kD epidermolysis bullosa acquisita antigen. Dermatology. (2004) 209:145–8. doi: 10.1159/000079601
50. Akasaka E, Nakano H, Korekawa A, Fukui T, Kaneko T, Koga H, et al. Anti-laminin γ1 pemphigoid associated with ulcerative colitis and psoriasis vulgaris showing autoantibodies to laminin γ1, type XVII collagen and laminin-332. Eur J Dermatol. (2015) 25:198–9. doi: 10.1684/ejd.2014.2499
51. Shimanovich I, Petersen EE, Weyers W, Sitaru C, Zillikens D. Subepidermal blistering disease with autoantibodies to both the p200 autoantigen and the alpha3 chain of laminin 5. (2005) 52:S90–2. doi: 10.1016/j.jaad.2004.07.036
52. Li X, Qian H, Ishii N, Yamaya M, Fukuda H, Mukai H, et al. A case of concurrent antilaminin gamma 1 pemphigoid and antilaminin-332-type mucous membrane pemphigoid. Br J Dermatol. (2014) 171:1257–9. doi: 10.1111/bjd.13107
53. Fujimura Y, Natsuga K, Hamade Y, Nomura Y, Kaku Y, Muramatsu R, et al. Anti-laminin-gamma 1 pemphigoid with generalized pustular psoriasis and psoriasis vulgaris. Acta Derm Venereol. (2016) 96:120–1. doi: 10.2340/00015555-2168
54. Saeki H, Hayashi N, Komine M, Soma Y, Shimada S, Watanabe K, et al. A case of generalized pustular psoriasis followed by bullous disease: an atypical case of bullous pemphigoid or a novel bullous disease? Br J Dermatol. (1996) 134:152–5. doi: 10.1046/j.1365-2133.1996.d01-758.x
55. Kaminaka C, Kanazawa N, Furukawa F, Hashimoto T. Case of anti-laminin-γ1 pemphigoid associated with psoriatic erythroderma. J Dermatol. (2010) 37:272–5. doi: 10.1111/j.1346-8138.2009.00790.x
56. Morris SD, Mallipeddi R, Oyama N, Gratian MJ, Harman KE, Bhogal BS, et al. Psoriasis bullosa acquisita. Clin Exp Dermatol. (2002) 27:665–9. doi: 10.1046/j.1365-2230.2002.01100.x
57. Gawaz A, Metzler G, Hertl M, Hashimoto T, Schaller M. Treatment of anti-laminin γ1 pemphigoid with mycophenolate mofetil. J Dtsch Dermatol Ges. (2015) 13:696–7. doi: 10.1111/ddg.12564
58. Hayashi M, Okamura K, Ujiie H, Iwata H, Suzuki T. Case of anti-p200 pemphigoid accompanying uterine malignancy. J Dermatol. (2018) 45:e341–2. doi: 10.1111/1346-8138.14473
59. Mai Y, Nishie W, Izumi K, Toyonaga E, Ikawa H, Mori T, et al. Detection of major epitopes for autoantibodies in dipeptidyl peptidase IV inhibitors-associated bullous pemphigoid. J Invest Dermatol. (2018) 138:S53. doi: 10.1016/j.jid.2018.03.319
60. Iijima S, Okazaki Y, Watanabe S, Tsuruta D, Tateishi C, Ishii N, et al. Case of concurrence of anti-laminin gamma-1 pemphigoid and scabies. J Dermatol. (2015) 42:1024–6. doi: 10.1111/1346-8138.13020
61. Ogata M, Misago N, Inoue T, Hirashima N, Narisawa Y, Ishii N, et al. A case of anti-p200 pemphigoid-discussion of association with scabies. Nishi Nihon Hifuka. (2006) 68:375–9. doi: 10.2336/nishinihonhifu.68.375
62. Wozniak K, Kowalewski C, Hashimoto T, Ishii N, Glinska-Wielochowska M, Schwartz RA. Penicillin-induced anti-p200 pemphigoid: an unusual morphology. Acta Derm Venereol. (2006) 86:443–6. doi: 10.2340/00015555-0117
63. Della Torre R, Combescure C, Cortés B, Marazza G, Beltraminelli H, Naldi L, et al. Clinical presentation and diagnostic delay in bullous pemphigoid: a prospective nationwide cohort. Br J Dermatol. (2012) 167:1111–7. doi: 10.1111/j.1365-2133.2012.11108.x
64. Clapé A, Muller C, Gatouillat G, Le Jan S, Barbe C, Pham B-N, et al. Mucosal involvement in bullous pemphigoid is mostly associated with disease severity and to absence of anti-BP230 autoantibody. Front Immunol. (2018) 9:479. doi: 10.3389/fimmu.2018.00479
65. Di Zenzo G, Thoma-Uszynski S, Fontao L, Calabresi V, Hofmann SC, Hellmark T, et al. Multicenter prospective study of the humoral autoimmune response in bullous pemphigoid. Clin Immunol. (2008) 128:415–26. doi: 10.1016/j.clim.2008.04.012
66. Vaillant L, Bernard P, Joly P, Prost C, Labeille B, Bedane C, et al. Evaluation of clinical criteria for diagnosis of bullous pemphigoid. French Bullous Study Group. Arch Dermatol. (1998) 134:1075–80. doi: 10.1001/archderm.134.9.1075
67. Joly P, Baricault S, Sparsa A, Bernard P, Bédane C, Duvert-Lehembre S, et al. Incidence and mortality of bullous pemphigoid in France. J Invest Dermatol. (2012) 132:1998–2004. doi: 10.1038/jid.2012.35
68. Kridin K, Bergman R. Ethnic variations in the epidemiology of bullous pemphigoid in Israel. Int J Dermatol. (2017) 57:34–9. doi: 10.1111/ijd.13813
69. Kridin K. Subepidermal autoimmune bullous diseases: overview, epidemiology, and associations. Immunol Res. (2018) 66:6–17. doi: 10.1007/s12026-017-8975-2
70. Ohata C, Ishii N, Koga H, Fukuda S, Tateishi C, Tsuruta D, et al. Coexistence of autoimmune bullous diseases (AIBDs) and psoriasis: a series of 145 cases. J Am Acad Dermatol. (2015) 73:50–5. doi: 10.1016/j.jaad.2015.03.016
71. Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. (2017) 31:205–12. doi: 10.1111/jdv.13854
72. Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. (2012) 133:377–85. doi: 10.1038/jid.2012.339
73. Takahashi H, Nakamura K, Kaneko F, Nakagawa H, Iizuka H. Analysis of psoriasis patients registered with the Japanese Society for Psoriasis Research from 2002-2008. J Dermatol. (2011) 38:1125–9. doi: 10.1111/j.1346-8138.2010.01145.x
74. Watanabe M, Natsuga K, Nishie W, Kobayashi Y, Donati G, Suzuki S, et al. Type XVII collagen coordinates proliferation in the interfollicular epidermis. Elife. (2017) 6:e26635. doi: 10.7554/eLife.26635
75. Dainichi T, Kabashima K. Interaction of psoriasis and bullous diseases. Front Med. (2018) 5:222. doi: 10.3389/fmed.2018.00222
76. Chan LS, Vanderlugt CJ, Hashimoto T, Nishikawa T, Zone JJ, Black MM, et al. Epitope spreading: lessons from autoimmune skin diseases. J Invest Dermatol. (1998) 110:103–9. doi: 10.1046/j.1523-1747.1998.00107.x
Keywords: anti-p200 pemphigoid, anti-laminin gamma-1 pemphigoid, IIF of salt-split skin, immunoblotting, ELISA, BMZ autoantibodies, mucosal disease, psoriasis
Citation: Kridin K and Ahmed AR (2019) Anti-p200 Pemphigoid: A Systematic Review. Front. Immunol. 10:2466. doi: 10.3389/fimmu.2019.02466
Received: 08 August 2019; Accepted: 03 October 2019;
Published: 22 October 2019.
Edited by:
Ralf J. Ludwig, Universität zu Lübeck, GermanyReviewed by:
Takashi Hashimoto, Osaka City University, JapanHiroshi Koga, Kurume University School of Medicine, Japan
Copyright © 2019 Kridin and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: A. Razzaque Ahmed, YXJhaG1lZG1kQG1zbi5jb20=
 Khalaf Kridin
Khalaf Kridin A. Razzaque Ahmed
A. Razzaque Ahmed