- 1Duke Global Health Institute, Duke University, Durham, NC, United States
- 2Division of Infectious Diseases and International Health, Duke University School of Medicine, Durham, NC, United States
- 3Global Health Research Center, Duke-Kunshan University, Kunshan, China
- 4Emerging Infectious Diseases Program, Duke-NUS Medical School, Singapore, Singapore
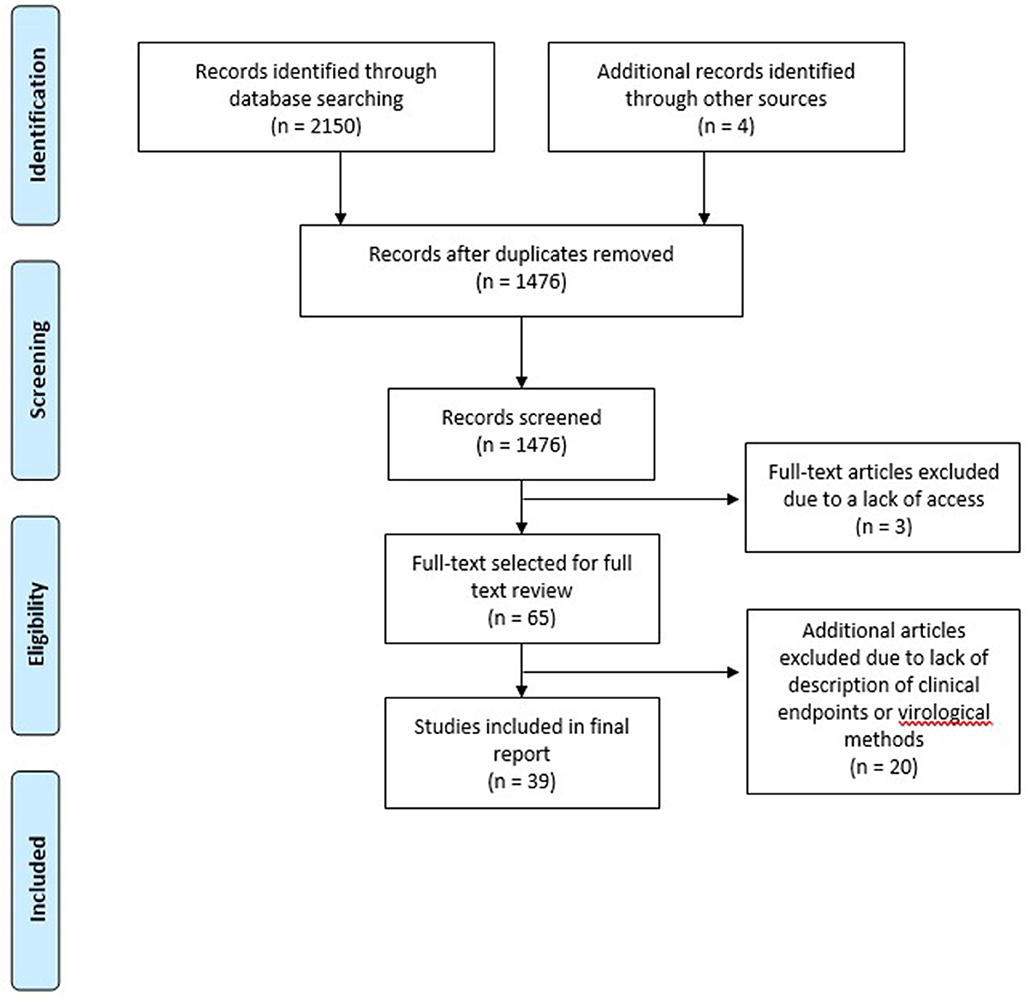
Due to their overall immunocompromised state, lung transplant recipients (LTRs) are at increased risk for the development of viral respiratory infections compared to the general population. Such respiratory infections often lead to poor transplant outcomes. We performed a systematic review of the last 30 years of medical literature to summarize the impact of specific respiratory viruses on LTRs. After screening 2,150 articles for potential inclusion, 39 manuscripts were chosen for final review. We found evidence for an association of respiratory viruses including respiratory syncytial virus (RSV), parainfluenza virus, and influenza viruses with increased morbidity following transplant. Through the literature search, we also documented associations of RSV and adenovirus infections with increased mortality among LTRs. We posit that the medical literature supports aggressive surveillance for respiratory viruses among this population.
Introduction
Lung transplant recipients (LTRs) are susceptible to a multitude of respiratory tract infections. Viral pathogens of particular relevance in LTRs include influenza A and B viruses, respiratory syncytial virus (RSV), parainfluenza virus (PIV), human metapneumovirus (HMpV), rhinovirus, coronavirus (CoV), picornavirus (PcV), and adenovirus (1–3). While these viruses may result in asymptomatic colonization or self-limited upper respiratory tract infection, there is greater potential for severe infection among LTRs. The severity of infection is contributed to by the marked immunocompromised state of LTRs alongside impaired respiratory mucociliary clearance in the first months after surgery and the unique scenario of the allograft being directly exposed to the outside environment. Respiratory viral infections have been associated with significant morbidity and mortality in LTRs (2–4), and increasingly, associations have been proposed between respiratory viruses and acute allograft rejection (AR) (5), chronic lung allograft dysfunction (CLAD) including bronchiolitis obliterans syndrome (BOS) (2, 6) and/or decreased survival (4). In an effort to more fully examine the relationship between respiratory viruses and adverse outcomes among lung transplant recipients, we conducted this systematic review. We sought to focus upon the associations of respiratory viruses with (1) AR, (2) CLAD (including BOS), and (3) mortality post-lung transplant.
Methods
We conducted a literature search, similar to that conducted by Vu et al. in 2010 (7) and identified 23 papers since the previous review. We searched the MEDLINE database from 1 January 1985 to 30 December 2018 using the following key words: “lung transplant recipients or immunocompromised hosts,” and “influenza, PIV, RSV, HMpV, CoV, bocavirus, AdV, and respiratory viruses,” respectively. Selection criteria for papers were as described in Vu et al. (7). Briefly, selected articles included original peer-reviewed papers reporting at minimum three lung transplant cases with a description of virus detection methods, as well as a description of clinical endpoints.
Results
Search Results
A total of 2,150 articles were identified by our search strategy After duplicates were removed, a total of 1,476 articles were screened for inclusion (Figure 1). Titles, abstracts, and keywords of all English articles were independently reviewed by two authors. Articles that did not describe viral detection methods or clinical endpoints were not considered for full text review. Following the screening of abstracts, 65 articles were selected for full text review. To determine final articles for inclusion, full text review was conducted independently by three authors. In addition to the 65 articles selected for inclusion, an additional four articles were identified from the reviewed articles as potentially significant and these were also reviewed in full. Among these 69 articles, 30 articles were excluded because the virologic detection methods or clinical endpoints were not well-described, resulting in a total of 39 articles being included in this review (Table 1).
Respiratory Viruses and Acute Allograft Rejection
Among the viruses evaluated, RSV was most prevalent and was documented in 9 (23%) of the 39 studies (see Table 1). In a prospective study of community-acquired respiratory viral infections in LTRs, RSV infection occurred in eight (23%) of 35 LTRs and was associated with a high rate of AR (88%) in comparison to other respiratory viruses [HMpV, n = 4 (25%); PIV, n = 11 (55%); influenza A/B, n = 9 (56%); rhinovirus, n = 2 (0)] (32). Furthermore, in a retrospective review of 10 LTRs with lower respiratory tract infections with RSV, Uckay et al. found that four patients (40%) had ≥3 AR episodes following laboratory confirmed RSV infection (31). Five other studies also noted single cases of RSV-associated AR in their patient populations (6, 17, 28, 34, 37).
Following RSV, influenza A and B were the respiratory viruses most commonly associated with lung transplant rejection, with seven studies (18%) reporting an association (Table 1). In a retrospective cohort evaluation of LTRs admitted with respiratory viral infections, Vilchez et al. (15) found some degree of AR in 9/15 (64%) of patients diagnosed with influenza respiratory infections (15). Hopkins et al. described a group of nine subjects with influenza that experienced 1.22 episodes of acute rejection on average, compared to 1.33 episodes of acute rejection in a group of nine subjects without influenza infections (23), suggesting that the risk for infection with influenza may not be exacerbated by lung transplant procedures.
PIVs were also identified as an important cause of morbidity, including AR, among lung transplant recipients. In a prospective study of respiratory virus associated morbidity in LTRs, 6/11 (55%) of PIV-infected subjects experienced AR though this was based primarily upon clinical as opposed to histopathologic diagnosis (32). In another prospective study, PIV was detected in 20 lung transplant recipients with histopathologic evidence of AR in 2 (50%) of the four patients undergoing transbronchial biopsy (41). Vilchez et al. documented PIV infection in 24 LTRs (PIV-1 n = 7; PIV-2 n = 2; PIV-3 n = 15) with histopathologic evidence of AR documented in 18 (82%) of the 22 undergoing evaluation (14).
While the data reviewed above supports a possible association between respiratory viruses and AR, there are noted limitations including derivation from retrospective, single center studies with variable definitions of AR and durations of follow-up. Further, conflicting data exists in the literature regarding the association of respiratory viruses with AR in LTRs; for example, Sayah et al. found that LTRs who experienced community acquired respiratory virus infections were not significantly more likely to experience AR than LTRs without infection (37). The relationships of AR and respiratory viruses was assessed in a study examining biopsies from 77 transplant patients, in which Soccal et al. found no association for subjects with AR and respiratory infection (44). Though these authors did not connect specific respiratory viruses with cases of AR, they postulated that respiratory viruses in general may aggravate existing lung impairments and slow recovery, but do not advance AR on their own (44).
Respiratory Viruses and CLAD/BOS
Similar to the data presented for respiratory viruses and AR, CLAD has been most commonly associated with RSV, influenza viruses, and PIV. In studies examining RSV infected patients, up to 25% of patients experienced CLAD (32), and among patients who received treatment for RSV, many did not develop CLAD (4). Hopkins et al. noted previous BOS in six RSV-infected subjects and documented the new onset or progression of BOS in five RSV-infected subjects (23). Additionally, Uckay et al. found that seven of 10 lung transplant recipients developed new or increased BOS after RSV infection (31); while similarly in a prospective study conducted by Li et al., three RSV-positive LTRs demonstrated BOS at the time of RSV infection, and two others developed new or progressive BOS within 6 months of RSV infection (35).
The pattern of influenza infection in LTRs is seasonally related to the strains of influenza virus that are prevalent. In LTRs infected with influenza A virus, studies have noted that up to 40% of patients were diagnosed with BOS (3, 16) and during the 2009 pandemic H1N1 influenza outbreak, nearly 50% of Australian LTRs developed BOS (33). In LTRs with severe CLAD, such as BOS grade 3, patients with influenza A were unable to successfully regain baseline lung functionality (16).
In contrast to the dual infection pattern (infection before and after surgery) seen with RSV infection, among LTRs, the available evidence indicates that PIV infections most often occurred after transplant surgery. Khalifah et al. conducted a retrospective review of medical records from a large medical university and found that four (57%) out of seven subjects with PIV infection experienced CLAD (4). Similarly, two other studies found that ~45% of PIV-infected patients developed CLAD (2, 32). In a 2001 epidemiological study of PIV infections among LTRs with BOS, three of the four PIV serotypes 1 (n = 2), 2 (n = 1), and 3 (n = 4) were implicated (14). PIV infections and associated CLAD have been demonstrated to have year-round incidence (13, 45), indicating the need for continued surveillance among lung transplant recipients.
There is some evidence that respiratory viruses are predictors of the development of CLAD in LTRs. (4, 12). Palmer et al. documented BOS in 50% of lung transplant recipients who survived respiratory viruses (13), indicating that competing risks may be confounding the true relationship of respiratory viruses and CLAD in LTRs Respiratory viruses may be directly impairing the recovery of lung function in LTRs with CLAD (16), contributing to overall morbidity in LTRs.
Respiratory Viruses and Mortality
Mortality directly associated with respiratory viruses is difficult to determine in medically complex LTRs. However, the viruses identified by this review as most commonly associated with mortality or patient survival were RSV and AdV. In particular, RSV was associated with 33% of all LTR infections in a pediatric population; however, these infections were not associated with mortality or CLAD (42). Similarly for AdV, AdV—associated mortality has been documented in up to 50% of LTRs with ADV pneumonia (12). Despite this, Liu et al. found AdV infection did not statistically predict mortality (42). In consideration of high mortality rates in LTRs, it is not always clear if death is related to the respiratory infection or other complications of transplant surgery, or infection with other viruses (9, 13, 25). Complications related to surgical procedure, concomitant viruses, secondary infections with bacterial and fungal pathogens, etc. also play a role in lung transplant patient survival. However, studies have directly attributed patient mortality to incidence of respiratory viral infections (33, 41), indicating that respiratory viruses may play a role in lung transplant recipient mortality.
Discussion
In this review, we found considerable evidence that respiratory viruses are associated with adverse outcomes in LTRs. Similar to Vu et al., which also examined the causal link between respiratory virus infection and adverse outcomes in LTRs, we found that the virus most often linked to these outcomes was respiratory syncytial virus (RSV). In the studies where RSV was reported, it was noted that most cases occurred during the winter months when RSV is most prevalent (17).
In the detection of PIVs, which were reported in association with adverse outcomes in eight (21%) of 38 included studies, cases were reported throughout the year; indicating a need for continual respiratory virus surveillance for LTRs (13, 14, 42). Additionally, in studies that linked the detection of respiratory viruses, such as influenza or AdV, to AR it has been postulated that respiratory infections may initiate other risk factors for rejection (4).
This systematic review had a number of limitations. First, as we limited the online review to studies published between 1985 and 2018, the review may have missed some early reports of respiratory virus association with lung transplant surgery. Second, through our search strategy we focused upon studies that contained both a description of virus detection methods, as well as a description of clinical endpoints and we may have missed some important case studies or reports of infection without descriptions comparable to the other studies included in this review. There is also the possibility of false pathology across the studies reviewed and although our study criteria attempted to limit this issue, it is possible our team missed discrepancies between studies. While our review suggests that respiratory virus infection is likely associated with adverse outcomes among LTRs, there is a need for continued evaluation of this relationship to determine what outcomes are most often associated with specific respiratory viruses.
Our findings convey an important message: the detection of respiratory viruses or the development of a clinical respiratory virus infection among LTRs is often associated with adverse outcomes. Hence, we suggest that intensive, year-round surveillance for respiratory viruses among LTRs is warranted due to the severity and frequency of these adverse outcomes. As multiplex molecular respiratory pathogen assays continue to improve and next generation sequencing becomes more widely available and less expensive, researchers, and clinicians may wish to employ these techniques to support respiratory virus detection and treatment.
Conclusions
Based on our review of 30 years of medical reports we have summarized compelling evidence that a relationship between respiratory viral infections and adverse lung transplant outcomes exists. From this examination, RSV has the greatest impact on LTRs. Additionally, influenza A viruses and PIVs are a major cause of morbidity and mortality among LTRs. Hence, we argue that these observations support intensive, year-round surveillance for respiratory viruses among LTRs.
Author Contributions
EB, JZ, and JC conducted the literature review and wrote the manuscript. GG conceived of the idea of the review and helped revise the manuscript to add important scientific content. All authors reviewed the final version of the manuscript and agreed to its submission.
Funding
This report was funded in part by Duke University discretionary funding (Gray PI).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Kellie Soafer, formerly of Duke University, for her support in the initial review of abstracts. We thank Professor Jennifer H. Saullo, MD of Duke University for her early review of this manuscript.
References
1. Kroger AT, Atkinson WL, Marcuse EK, Pickering LK Advisory Committee on Immunization Practices Centers for Disease C Prevention. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. (2006) 55:1–48.
2. Gottlieb J, Schulz TF, Welte T, Fuehner T, Dierich M, Simon AR, et al. Community-acquired respiratory viral infections in lung transplant recipients: a single season cohort study. Transplantation. (2009) 87:1530–7. doi: 10.1097/TP.0b013e3181a4857d
4. Khalifah AP, Hachem RR, Chakinala MM, Schechtman KB, Patterson GA, Schuster DP, et al. Respiratory viral infections are a distinct risk for bronchiolitis obliterans syndrome and death. Am J Respir Crit Care Med. (2004) 170:181–7. doi: 10.1164/rccm.200310-1359OC
5. Kumar D, Husain S, Chen MH, Moussa G, Himsworth D, Manuel O, et al. A prospective molecular surveillance study evaluating the clinical impact of community-acquired respiratory viruses in lung transplant recipients. Transplantation. (2010) 89:1028–33. doi: 10.1097/TP.0b013e3181d05a71
6. Kumar D, Erdman D, Keshavjee S, Peret T, Tellier R, Hadjiliadis D, et al. Clinical impact of community-acquired respiratory viruses on bronchiolitis obliterans after lung transplant. Am J Transplant. (2005) 5:2031–6. doi: 10.1111/j.1600-6143.2005.00971.x
7. Vu DL, Bridevaux PO, Aubert JD, Soccal PM, Kaiser L. Respiratory viruses in lung transplant recipients: a critical review and pooled analysis of clinical studies. Am J Transplant. (2011) 11:1071–8. doi: 10.1111/j.1600-6143.2011.03490.x
8. Kramer MR, Marshall SE, Starnes VA, Gamberg P, Amitai Z, Theodore J. Infectious complications in heart-lung transplantation. Analysis of 200 episodes. Arch Intern Med. (1993) 153:2010–6. doi: 10.1001/archinte.1993.00410170090009
9. Apalsch AM, Green M, Ledesma-Medina J, Nour B, Wald ER. Parainfluenza and influenza virus infections in pediatric organ transplant recipients. Clin Infect Dis. (1995) 20:394–9. doi: 10.1093/clinids/20.2.394
10. Ohori NP, Michaels MG, Jaffe R, Williams P, Yousem SA. Adenovirus pneumonia in lung transplant recipients. Hum Pathol. (1995) 26:1073–9. doi: 10.1016/0046-8177(95)90268-6
11. Riise GC, Kjellstrom C, Ryd W, Schersten H, Nilsson F, Martensson G, et al. Inflammatory cells and activation markers in BAL during acute rejection and infection in lung transplant recipients: a prospective, longitudinal study. Eur Resp J. (1997) 10:1742–6. doi: 10.1183/09031936.97.10081742
12. Bridges ND, Spray TL, Collins MH, Bowles NE, Towbin JA. Adenovirus infection in the lung results in graft failure after lung transplantation. J Thorac Cardiovasc Surg. (1998) 116:617–23. doi: 10.1016/S0022-5223(98)70168-0
13. Palmer SM Jr, Henshaw NG, Howell DN, Miller SE, Davis RD, Tapson VF. Community respiratory viral infection in adult lung transplant recipients. Chest. (1998) 113:944–50. doi: 10.1378/chest.113.4.944
14. Vilchez RA, McCurry K, Dauber J, Iacono A, Keenan R, Zeevi A, et al. The epidemiology of parainfluenza virus infection in lung transplant recipients. Clin Infect Dis. (2001) 33:2004–8. doi: 10.1086/324348
15. Vilchez R, McCurry K, Dauber J, Iacono A, Keenan R, Griffith B, et al. Influenza and parainfluenza respiratory viral infection requiring admission in adult lung transplant recipients. Transplantation. (2002) 73:1075–8. doi: 10.1097/00007890-200204150-00010
16. Hopkins PM, Plit ML, Carter IW, Chhajed PN, Malouf MA, Glanville AR. Indirect fluorescent antibody testing of nasopharyngeal swabs for influenza diagnosis in lung transplant recipients. J Heart Lung Transplant. (2003) 22:161–8. doi: 10.1016/S1053-2498(02)00467-9
17. McCurdy LH, Milstone A, Dummer S. Clinical features and outcomes of paramyxoviral infection in lung transplant recipients treated with ribavirin. J Heart Lung Transplant. (2003) 22:745–53. doi: 10.1016/S1053-2498(02)00569-7
18. Larcher C, Geltner C, Fischer H, Nachbaur D, Muller LC, Huemer HP. Human metapneumovirus infection in lung transplant recipients: clinical presentation and epidemiology. J Heart Lung Transplant. (2005) 24:1891–901. doi: 10.1016/j.healun.2005.02.014
19. Sumino KC, Agapov E, Pierce RA, Trulock EP, Pfeifer JD, Ritter JH, et al. Detection of severe human metapneumovirus infection by real-time polymerase chain reaction and histopathological assessment. J Infect Dis. (2005) 192:1052–60. doi: 10.1086/432728
20. Humar A, Doucette K, Kumar D, Pang XL, Lien D, Jackson K, et al. Assessment of adenovirus infection in adult lung transplant recipients using molecular surveillance. J Heart Lung Transplant. (2006) 25:1441–6. doi: 10.1016/j.healun.2006.09.015
21. Kaiser L, Aubert JD, Pache JC, Deffernez C, Rochat T, Garbino J, et al. Chronic rhinoviral infection in lung transplant recipients. Am J Resp Crit Care. (2006) 174:1392–9. doi: 10.1164/rccm.200604-489OC
22. Dare R, Sanghavi S, Bullotta A, Keightley M-C, George KS, Wadowsky RM, et al. Diagnosis of human metapneumovirus infection in immunosuppressed lung transplant recipients and children evaluated for pertussis. J Clin Microbiol. (2007) 45:548–52. doi: 10.1128/JCM.01621-06
23. Hopkins P, McNeil K, Kermeen F, Musk M, McQueen E, Mackay I, et al. Human metapneumovirus in lung transplant recipients and comparison to respiratory syncytial virus. Am J Respir Crit Care Med. (2008) 178:876–81. doi: 10.1164/rccm.200711-1657OC
24. Ison MG, Sharma A, Shepard JAO, Wain JC, Ginns LC. Outcome of influenza infection managed with oseltamivir in lung transplant recipients. J Heart Lung Transplant. (2008) 27:282–8. doi: 10.1016/j.healun.2007.11.575
25. Costa C, Terlizzi ME, Solidoro P, Libertucci D, Bergallo M, Cavallo R. Detection of parvovirus B19 in the lower respiratory tract. J Clin Virol. (2009) 46:150–3. doi: 10.1016/j.jcv.2009.06.026
26. Engelmann I, Welte T, Fuhner T, Simon AR, Mattner F, Hoy L, et al. Detection of epstein-barr virus DNA in peripheral blood is associated with the development of bronchiolitis obliterans syndrome after lung transplantation. J Clin Virol. (2009) 45:47–53. doi: 10.1016/j.jcv.2009.02.005
27. Gerna G, Piralla A, Rovida F, Rognoni V, Marchi A, Locatelli F, et al. Correlation of rhinovirus load in the respiratory tract and clinical symptoms in hospitalized immunocompetent and immunocompromised patients. J Med Virol. (2009) 81:1498–507. doi: 10.1002/jmv.21548
28. Pelaez A, Lyon GM, Force SD, Ramirez AM, Neujahr DC, Foster M, et al. Efficacy of oral ribavirin in lung transplant patients with respiratory syncytial virus lower respiratory tract infection. J Heart Lung Transplant. (2009) 28:67–71. doi: 10.1016/j.healun.2008.10.008
29. Bergallo M, Costa C, Terlizzi ME, Astegiano S, Curtoni A, Solidoro P, et al. Quantitative detection of the new polyomaviruses KI, WU and Merkel cell virus in transbronchial biopsies from lung transplant recipients. J Clin Pathol. (2010) 63:722–5. doi: 10.1136/jcp.2010.077966
30. Liu V, Dhillon GS, Weill D. A multi-drug regimen for respiratory syncytial virus and parainfluenza virus infections in adult lung and heart-lung transplant recipients. Transplant Infect Dis. (2010) 12:38–44. doi: 10.1111/j.1399-3062.2009.00453.x
31. Uckay I, Gasche-Soccal PM, Kaiser L, Stern R, Mazza-Stalder J, Aubert J-D, et al. Low incidence of severe respiratory syncytial virus infections in lung transplant recipients despite the absence of specific therapy. J Heart Lung Transplant. (2010) 29:299–305. doi: 10.1016/j.healun.2009.08.012
32. Weinberg A, Lyu DM, Li S, Marquesen J, Zamora MR. Incidence and morbidity of human metapneumovirus and other community-acquired respiratory viruses in lung transplant recipients. Transplant Infect Dis. (2010) 12:330–5. doi: 10.1111/j.1399-3062.2010.00509.x
33. Ng BJH, Glanville AR, Snell G, Musk M, Holmes M, Chambers DC, et al. The impact of pandemic influenza A H1N1 2009 on Australian lung transplant recipients. Am J Transplant. (2011) 11:568–74. doi: 10.1111/j.1600-6143.2010.03422.x
34. Ariza-Heredia EJ, Fishman JE, Cleary T, Smith L, Razonable RR, Abbo L. Clinical and radiological features of respiratory syncytial virus in solid organ transplant recipients: a single-center experience. Transpl Infect Dis. (2012) 14:64–71. doi: 10.1111/j.1399-3062.2011.00673.x
35. Li L, Avery R, Budev M, Mossad S, Danziger-Isakov L. Oral versus inhaled ribavirin therapy for respiratory syncytial virus infection after lung transplantation. J Heart Lung Transplant. (2012) 31:839–44. doi: 10.1016/j.healun.2012.04.002
36. Lo MS, Lee GM, Gunawardane N, Burchett SK, Lachenauer CS, Lehmann LE. The impact of RSV, adenovirus, influenza, and parainfluenza infection in pediatric patients receiving stem cell transplant, solid organ transplant, or cancer chemotherapy. Pediatr Transplant. (2013) 17:133–43. doi: 10.1111/petr.12022
37. Sayah DM, Koff JL, Leard LE, Hays SR, Golden JA, Singer JP. Rhinovirus and other respiratory viruses exert different effects on lung allograft function that are not mediated through acute rejection. Clin Transplant. (2013) 27:E64–71. doi: 10.1111/ctr.12054
38. Bridevaux P-O, Aubert JD, Soccal PM, Mazza-Stalder J, Berutto C, Rochat T, et al. Incidence and outcomes of respiratory viral infections in lung transplant recipients: a prospective study. Thorax. (2014) 69:32–8. doi: 10.1136/thoraxjnl-2013-203581
39. Schuurmans MM, Isenring BD, Jungo C, Boeni J, Mueller NJ, Kohler M, et al. Clinical features and outcomes of influenza infections in lung transplant recipients: a single-season cohort study. Transplant Infect Dis. (2014) 16:430–9. doi: 10.1111/tid.12228
40. Tabarelli W, Bonatti H, Tabarelli D, Eller M, Muller L, Ruttmann E, et al. Long term complications following 54 consecutive lung transplants. J Thorac Dis. (2016) 8:1234–44. doi: 10.21037/jtd.2016.05.03
41. Peghin M, Hirsch HH, Len O, Codina G, Berastegui C, Saez B, et al. Epidemiology and immediate indirect effects of respiratory viruses in lung transplant recipients: a 5-year prospective study. Am J Transplant. (2017) 17:1304–12. doi: 10.1111/ajt.14042
42. Liu M, Mallory GB, Schecter MG, Worley S, Arrigain S, Robertson J, et al. Long-term impact of respiratory viral infection after pediatric lung transplantation. Pediatr Transplant. (2010) 14:431–6. doi: 10.1111/j.1399-3046.2010.01296.x
43. Matar LD, McAdams HP, Palmer SM, Howell DN, Henshaw NG, Davis RD, et al. Respiratory viral infections in lung transplant recipients: radiologic findings with clinical correlation. Radiology. (1999) 213:735–42. doi: 10.1148/radiology.213.3.r99dc25735
44. Soccal PM, Aubert JD, Bridevaux PO, Garbino J, Thomas Y, Rochat T, et al. Upper and lower respiratory tract viral infections and acute graft rejection in lung transplant recipients. Clin Infect Dis. (2010) 51:163–70. doi: 10.1086/653529
Keywords: lung transplant, adult, respiratory virus, infection, acute rejection
Citation: Bailey ES, Zemke JN, Choi JY and Gray GC (2019) A Mini-Review of Adverse Lung Transplant Outcomes Associated With Respiratory Viruses. Front. Immunol. 10:2861. doi: 10.3389/fimmu.2019.02861
Received: 10 September 2019; Accepted: 21 November 2019;
Published: 19 December 2019.
Edited by:
Soldevila Gloria, National Autonomous University of Mexico, MexicoReviewed by:
John-David Aubert, Lausanne University Hospital (CHUV), SwitzerlandSolidoro Paolo, AOU Città della Salute e della Scienza di Torino SC Pneumologia U, Italy
Copyright © 2019 Bailey, Zemke, Choi and Gray. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emily S. Bailey, ZW1pbHkuYmFpbGV5QHR0dWhzYy5lZHU=
†Present address: Emily S. Bailey, Julia Jones Matthews Department of Public Health, Graduate School of Biomedical Sciences, Texas Tech University Health Sciences Center, Abilene, TX, United States
 Emily S. Bailey
Emily S. Bailey Juliana N. Zemke1,2
Juliana N. Zemke1,2 Jessica Y. Choi
Jessica Y. Choi Gregory C. Gray
Gregory C. Gray