- 1Nutrition, Metabolism and Genomics Group, Division of Human Nutrition and Health, Wageningen University and Research, Wageningen, Netherlands
- 2Zvitambo Institute for Maternal and Child Health Research, Harare, Zimbabwe
- 3Blizard Institute, Queen Mary University of London, London, United Kingdom
- 4The Childhood Acute Illness & Nutrition (CHAIN) Network, Nairobi, Kenya
- 5Kenya Medical Research Institute (KEMRI) - Wellcome Trust Research Programme, Nairobi, Kenya
- 6Tropical Gastroenterology and Nutrition Group, University of Zambia, Lusaka, Zambia
- 7Nuffield Department of Medicine, Centre for Tropical Medicine & Global Health, University of Oxford, Oxford, United Kingdom
A Commentary on mechanisms of kwashiorkor-associated immune suppression: Insights from human, mouse, and pig studies. By Michael H, Amimo JO, Rajashekara G, Saif LJ and Vlasova AN (2022). Front. Immunol. 13:826268. doi:
https://doi.org/10.3389/fimmu.2022.826268
Introduction
Derangement in functional immunity is a characteristic of children with severe malnutrition (SM). Deaths among children with SM are principally from infections, and understanding their pathophysiology to develop effective treatment strategies is essential to improving outcomes. Several reviews have discussed the state of knowledge of SM immunology (1–3). However, differences in immune function between kwashiorkor and wasting have not been adequately documented.
We were delighted to see a review of kwashiorkor-associated immune suppression, as there are very few reports that have studied kwashiorkor-specific immunological changes, especially in clinical settings. However, we believe that the review of Michael et al. (4) on kwashiorkor-associated immune function contains several oversimplifications and extrapolations of results given the recognized heterogeneity and power limitations of existing immunological assessments in SM (5). We believe that clarity in reporting results from clinical studies (also highlighted by literature reviews cited by Michael et al.) and in how they compare to experimental models is essential to add value to the wider field of malnutrition-related immunology. Therefore, while we applaud the authors for their work, we are concerned about several aspects of their recent review for reasons we discussed in this commentary.
Discussion
Firstly, the idea that reduced protein intake leads to hypoalbuminemia, which decreases oncotic pressur leading to edema in kwashiorkor, is widely believed, but this is an oversimplification which is not supported by strong evidence. In a recent study, we found that hypoalbuminemia is associated but alone was insufficient to explain edema in kwashiorkor (6). Other factors apart from hypoalbuminemia and low protein intake must develop kwashiorkor (7), such as extracellular matrix (ECM) degradation and lymphatic damage (6). Moreover, it was previously shown that edema in children with kwashiorkor resolved even when they were treated with a protein-deficient diet (8), and despite a small increase in serum albumin concentration among children whose oedema resolved or improved, serum albumin concentrations remained far below clinically recognized norms in children (6, 9). It is important to emphasize that oversimplification of kwashiorkor etiology (presented in the review text and Figure 2 but unsupported by empirical evidence) can result in ineffective treatment strategies.
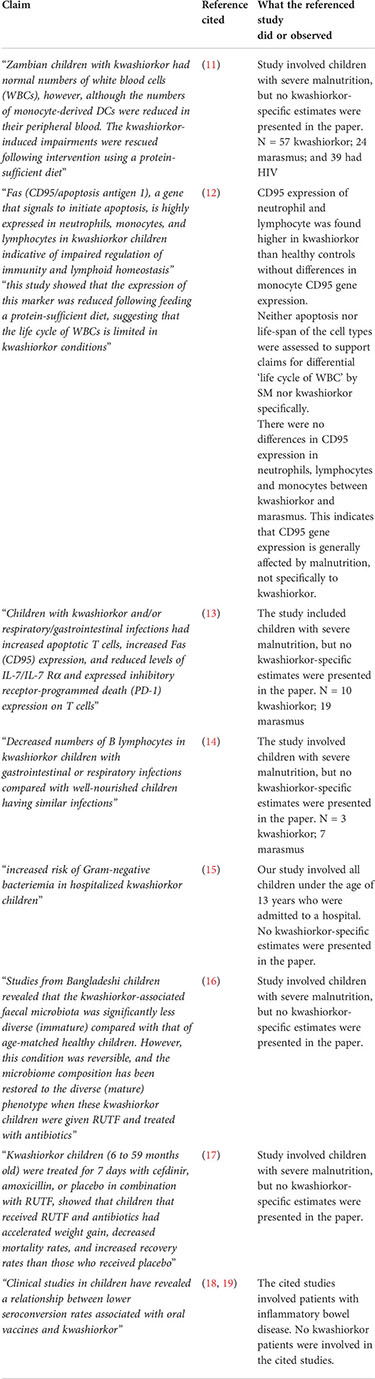
Secondly, some of the immune function effects stated in the review are not borne out by the cited references. It is tempting to suggest that kwashiorkor is characterized by a “profound impaired immune function,” as the authors claim. For instance, diseases with heightened inflammation are associated with ECM degradation, and the degradation of the ECM is linked to immune function (10). However, the papers cited did not study kwashiorkor specifically. For instance, the paper by Hughes et al. (11) involved both wasting and kwashiorkor. Half of these children also had HIV, and most likely had other infections, which resulted in their hospital admission. The analysis by Hughes et al. was controlled for edema; thus, no kwashiorkor-specific estimates were presented in the paper. The table given below lists statements about kwashiorkor-associated immunological characteristics in the review by Michael et al. that are not supported by the cited references.
Evaluation of claims regarding kwashiorkor-associated immunological changes.
The review also contains a section about micronutrient deficiencies specific to kwashiorkor. However, none of the micronutrient literature presented is specific to kwashiorkor, much less to wasting. Furthermore, the review highlighted the impact of kwashiorkor on infection and vaccination in the gnotobiotic piglet model, which may not be translational to human kwashiorkor, as discussed below. More clinical evidence in humans is needed.
The authors use the evidence they gathered in this review to justify gnotobiotic pigs as better models of kwashiorkor than mouse models because the pig models replicate the immune function found in human kwashiorkor better than mice. However, as above, there is no strong evidence for kwashiorkor-specific immune changes. Unlike in animal models, the clinical heterogeneity inherent to SM renders many existing studies underpowered or unable to distinguish from acute infection to draw conclusions on immune function in human SM per se, let alone in kwashiorkor specifically. We agree that pig models may offer a valuable opportunity for immunological studies (2), but disagree that there is sufficient evidence to use immunological effects to validate these models.
Finally, we agree with the authors that the mouse models of kwashiorkor, which have attracted the most citations, lack face validity (2). Most importantly, the mouse model proposed by Smith et al. (20) did not develop edema, which is pathognomonic of kwashiorkor. In contrast, the pig model of the authors developed generalized edema, which is more indicative of kwashiorkor. Upon reviewing the pig model development, we noticed that the phenotype appeared when nursing piglets were fed with Parmalat (bovine whole milk containing 3.3% protein, 3.3% fat, and 5% carbohydrates) mixed with sterile water (50:50 v/v), resulting in 50% less protein (21). Control pigs were fed 100% Parmalat. This model raises two questions. First, the malnourished pigs received 50% less of all constituent macronutrients rather than reduced protein alone, making it difficult to conclude that the phenotype observed is solely due to protein deficiency. Second, kwashiorkor in children peaks at around 2 years of age, often after weaning. The neonatal gnotobiotic pigs were fed a diet deficient in macronutrients before 4 days of age. Thus, these porcine models may have different intestinal development than children with kwashiorkor, and the cause of the edema may relate to immature intestinal development or other causes. Other non-kwashiorkor pathologies in children with edema have been described by Golden (7).
In summary, the review highlighted interesting immune features in children with severe malnutrition but did not specifically describe the immune function in kwashiorkor. Hence, the reported similarities between the immune function of children with kwashiorkor and gnotobiotic pig models cannot be used to establish the face validity of the porcine model. Kwashiorkor-specific studies on immune function are still lacking, providing an opportunity for further translational research. Rather than viewing experimental models as the “only alternative to clinical studies,” we regard insights from clinical and translational immunology studies as essential to achieve the goal of the authors of carefully selecting appropriate, evidence-based mechanistic and pre-clinical models that can support therapeutic interventions for SM.
Author Contributions
GBG wrote the initial draft. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
CDB is supported by the joint Wellcome Trust and Royal Society Grant (206225/Z/17/Z). JPS (220566/Z/20/Z), JMN (222967/Z/21/Z), and RCR (206455/Z/17/Z) are supported by the Wellcome Trust. JAB is supported by MRC/DFID/Wellcome Trust Joint Global Health Trials scheme (MR/M007367/1) and the Bill and Melinda Gates Foundation (OPP1131320).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bourke CD, Berkley JA, Prendergast AJ. Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol (2016) 37:386–98. doi: 10.1016/j.it.2016.04.003
2. Bourke CD, Jones KDJ, Prendergast AJ. Current understanding of innate immune cell dysfunction in childhood undernutrition. Front Immunol (2019) 10:1728. doi: 10.3389/fimmu.2019.01728
3. Rytter MJH, Kolte L, Briend A, Friis H, Christensen VB. The immune system in children with malnutrition–a systematic review. PLoS One (2014) 9:e105017. doi: 10.1371/journal.pone.0105017
4. Michael H, Amimo JO, Rajashekara G, Saif LJ, Vlasova AN. Mechanisms of kwashiorkor-associated immune suppression: Insights from human, mouse, and pig studies. Front Immunol (2022) 13:826268. doi: 10.3389/fimmu.2022.826268
5. Ibrahim MK, Zambruni M, Melby CL, Melby PC. Impact of childhood malnutrition on host defense and infection. Clin Microbiol Rev (2017) 30:919–71. doi: 10.1128/CMR.00119-16
6. Gonzales GB, Njunge JM, Gichuki BM, Wen B, Ngari M, Potani I, et al. The role of albumin and the extracellular matrix on the pathophysiology of oedema formation in severe malnutrition. eBioMedicine (2022) 79:103991. doi: 10.1016/j.ebiom.2022.103991
7. Golden MH. Nutritional and other types of oedema, albumin, complex carbohydrates and the interstitium - a response to Malcolm coulthard's hypothesis: Oedema in kwashiorkor is caused by hypo-albuminaemia. Paediatrics Int Child Health (2015) 35:90–109. doi: 10.1179/2046905515Y.0000000010
8. Golden MN. Protein deficiency, energy deficiency and the oedema of malnutrition. Lancet (1982) 319:1261–5. doi: 10.1016/S0140-6736(82)92839-2
9. Golden MN, Golden B, Jackson A. Albumin and nutritional oedema. Lancet (1980) 315:114–6. doi: 10.1016/S0140-6736(80)90603-0
10. Tomlin H, Piccinini AM. A complex interplay between the extracellular matrix and the innate immune response to microbial pathogens. Immunology (2018) 155:186–201. doi: 10.1111/imm.12972
11. Hughes SM, Amadi B, Mwiya M, Nkamba H, Tomkins A, Goldblatt D. Dendritic cell anergy results from endotoxemia in severe malnutrition. J Immunol (2009) 183:2818–26. doi: 10.4049/jimmunol.0803518
12. Nassar MF, El-Batrawy SR, Nagy NM. CD95 expression in white blood cells of malnourished infants during hospitalization and catch-up growth. East Mediterr Health J (2009) 15:574–83. doi: 10.26719/2009.15.3.574
13. Badr G, Sayed D, Alhazza IM, Elsayh KI, Ahmed EA, Alwasel SH. T Lymphocytes from malnourished infants are short-lived and dysfunctional cells. Immunobiology (2011) 216:309–15. doi: 10.1016/j.imbio.2010.07.007
14. Nájera O, González C, Toledo G, López L, Ortiz R. Flow cytometry study of lymphocyte subsets in malnourished and well-nourished children with bacterial infections. Clin Diagn Lab Immunol (2004) 11:577–80. doi: 10.1128/CDLI.11.3.577-580.2004
15. Berkley JA, Lowe BS, Mwangi I, Williams T, Bauni E, Mwarumba S, et al. Bacteremia among children admitted to a rural hospital in Kenya. N Engl J Med (2005) 352:39–47. doi: 10.1056/NEJMoa040275
16. Subramanian S, Huq S, Yatsunenko T, Haque R, Mahfuz M, Alam MA, et al. Persistent gut microbiota immaturity in malnourished Bangladeshi children. Nature (2014) 510:417. doi: 10.1038/nature13421
17. Trehan I, Goldbach HS, LaGrone LN, Meuli GJ, Wang RJ, Maleta KM, et al. Antibiotics as part of the management of severe acute malnutrition. N Engl J Med (2013) 368:(5):425–35. doi: 10.1056/NEJMoa1202851
18. Hamilton AL, Kamm MA, Ng SC, Morrison M. Proteus Spp. as putative gastrointestinal pathogens. Clin Microbiol Rev (2018) 31(3):e00085–17. doi: 10.1128/CMR.00085-17
19. Presley LL, Ye J, Li X, Leblanc J, Zhang Z, Ruegger PM, et al. Host-microbe relationships in inflammatory bowel disease detected by bacterial and metaproteomic analysis of the mucosal-luminal interface. Inflamm Bowel Dis (2012) 18:409–17. doi: 10.1002/ibd.21793
20. Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J, et al. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science (2013) 339:548–54. doi: 10.1126/science.1229000
Keywords: kwashiorkor, immune, severe malnutrition, marasmus, edematous malnutrition
Citation: Gonzales GB, Bourke CD, Sturgeon JP, Njunge JM, Robertson RC, Kelly PM and Berkley JA (2022) Commentary: Mechanisms of kwashiorkor-associated immune suppression: Insights from human, mouse, and pig studies. Front. Immunol. 13:959465. doi: 10.3389/fimmu.2022.959465
Received: 01 June 2022; Accepted: 27 June 2022;
Published: 25 July 2022.
Edited by:
Harry D. Dawson, Department of Agriculture, United StatesReviewed by:
Stephanie N. Langel, Duke University, United StatesCopyright © 2022 Gonzales, Bourke, Sturgeon, Njunge, Robertson, Kelly and Berkley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gerard Bryan Gonzales, YnJ5YW4uZ29uemFsZXNAd3VyLm5s
 Gerard Bryan Gonzales
Gerard Bryan Gonzales Claire D. Bourke
Claire D. Bourke Jonathan P. Sturgeon
Jonathan P. Sturgeon James M. Njunge4,5
James M. Njunge4,5 Ruairi C. Robertson
Ruairi C. Robertson Paul M. Kelly
Paul M. Kelly James A. Berkley
James A. Berkley