- 1Health Policy Research Group, Department of Pharmacology and Therapeutics, College of Medicine, University of Nigeria, Enugu, Nigeria
- 2Department of Health Administration and Management, Faculty of Health Science and Technology, College of Medicine, University of Nigeria, Enugu, Nigeria
Background: Getting evidence from Health Policy and Systems Research (HPSR) into policy and practice for effective control of neglected tropical diseases (NTDs) is essential for providing better service delivery because evidence-informed decision-making improves the effectiveness of a health system and health outcomes. The paper provides new knowledge on the policy-/decision-makers’ level of knowledge, capacity to use, and how evidence from HPSR has been used in decision-making for the control of endemic tropical diseases (ETDs), especially the NTDs and malaria in Nigeria.
Methods: A cross-sectional qualitative study of decision-makers was undertaken in Anambra and Enugu states, southeast Nigeria. Data was collected through in-depth interviews (n=22) of purposively selected decision-makers to assess how HPSR evidence is translated into policy and practice for controlling ETDs. The respondents were selected based on their job description, roles, and involvement in the control of ETDs. Data were analyzed using the thematic content approach.
Results: There is a considerable level of knowledge on HPSR and its relationship with evidence-informed policy- and decision-making towards control of ETDs and health system strengthening. Organizational capacity to use HPSR evidence in decision-making was found to be weak due to various reasons such as no embedded structure for translating research evidence to policy and practice, lack of decision-making autonomy by individuals, and politically driven decisions. Few respondents have either ever used or are currently using HPRS evidence for developing/reviewing and implementing strategies for ETDs programs. Majority of the respondents reported that their main source of evidence was routine data from health information management system, which they found useful due to its representativeness and completeness. Main enabler for using HPSR evidence for decision-making is existing collaborations between researchers and policy-/decision-makers.
Conclusion: There is a high level of awareness about evidence from HPSR and the usefulness of such evidence in decision-making. However, this awareness does not translate to optimal use of evidence for decision-making due to weak organizational capacity and other constraints. There is the need to invest in capacity-building activities to develop a critical mass of users of evidence (policy-/decision-makers) to facilitate enhanced uptake of high-quality evidence into policy decisions for better control of ETDs.
Introduction
Globally, there is increasing interest and recognition among countries, including low- and middle-income countries (LMICs), on the value of using research evidence for effective health policy-making in providing quality health services and management (1, 2). Linking evidence from research in disease control is essential in providing policy-makers and implementers (users of evidence) with empirical evidence on better service delivery which will ultimately lead to improved health outcomes (3, 4). Studies have shown that evidence-informed decision making (EIDM) improves the effectiveness of a health system (5, 6). Thus, the relevancy and role of research evidence in promoting efficient, effective, and equitable service delivery particularly in LMIC with diverse healthcare needs cannot be overemphasized (7, 8).
In many resource-poor countries, evidence-based decisions are needed for more effective control of endemic tropical diseases (ETDs) such as neglected tropical diseases (NTDs) and also malaria. This is pertinent when viewed from the finding that NTDs constitute a significant annual health burden (among the top 10 leading causes of long-term disability and premature deaths) resulting in losses in health, social progress, and economic productivity (4) necessitating the call for global efforts to eliminate NTDs by 2030 (9).
There are over one billion people with at least an NTD (including more than 500 million children) and 500,000 deaths yearly (9). In Africa, 34 countries are endemic to lymphatic filariasis, with Nigeria bearing the highest burden of the disease, with a risk population of 80 to 120 million people (10, 11). Nigeria also contributes the highest burden of 29 million cases of schistosomiasis among sub-Saharan African (SSA) countries (12), as well as the highest number (38 million) of hookworm infestation, Ascaris (55 million), and trichuria (34 million) in the region (11–13).
Malaria is also highly endemic in SSA, with the greatest burden of malaria in the world found in Nigeria (12). Malaria cases accounted for an estimated 229 million cases in 87 malaria-endemic countries of which twenty-nine (29) countries contributed 95% of malaria cases globally. The World Health Organization (WHO) African Region, accounted for about 94% of cases with an estimated 215 million cases in 2019 with Nigeria accounting for the highest proportion of the cases (27%) (14). Among 31 countries that accounted for 95% of malaria death, African countries alone contributed 51% of global death. Also, approximately 95% of malaria deaths were reported in 31 countries. Nigeria (23%) accounted for about 51% of all malaria deaths globally in 2019 (14). Despite this, malaria remains the leading cause of morbidity and mortality in Nigeria (15).
Nigeria, like many sub-Saharan African (SSA) countries did not meet Millennium Development Goal (MDG) targets on endemic diseases due to numerous health systems challenges, limiting ETDs control efforts (16). This poor performance could be linked to low levels of use of evidence in the control of the diseases.
However, an issue with use of evidence-based decision-making is the ability of the policy-makers/decision-makers to have the capacity to interpret and use the evidence from research for decision-making in the control of the diseases. Hence, it has been shown that the knowledge of users of evidence (policy-makers/decision-makers), skills, and the importance attached to research and users of evidence-researcher interaction influence their level of use of research evidence (17–19). Another important factor in evidence-to-policy-and-practice process is capacity limitations to knowledge translation (KT) (19–21).
Hence, inadequate capacity for knowledge translation among users of evidence, especially from Health Policy and Systems Research (HPSR), limits their use of such evidence (22). Capacity, defined as the ability to execute tasks in a sustainable approach, is a multifaceted concept that involves different interrelated elements (including staff expertise and structures) at the individual, organizational, and wider health systems levels (23).
Capacity to undertake HPSR, defined as the “production of new knowledge to improve how societies organize themselves to achieve collective health goals” (24, 25), is crucial for overall health systems strengthening and attaining its objectives such as improved health outcomes (26). HPSR aims to produce scientifically reliable evidence that helps in informing the numerous and diverse decisions that must be made by ministers of health, policy-makers, implementers, etc., on how to plan and manage different health systems components towards achieving the desired changes (24).
In developing countries, the capacity to undertake and use HPRS evidence has generally been suboptimal (25), underscoring the need for capacity strengthening (27). Evidence from HPSR for decision-making goes beyond published in peer-reviewed journals, but also includes reports from program evaluation, routine service data particularly those generated via the Health Management Information System (HMIS), and other experiments/systematically generated knowledge outputs such as policy brief (24).
Getting evidence from HPSR into policy and practice for effective control of NTDs is essential for providing better service delivery because evidence-informed decision-making improves effectiveness of a health system and health outcomes. Given the context-sensitive nature of HPSR, it was important to assess the level of knowledge and capacity to use evidence from HPSR in decision-making for controlling NTDs in Nigeria.
Hence, this paper provides new knowledge on the policy-makers’/decision-makers’ level of knowledge, capacity to use, and how evidence from HPSR has been used in decision-making for the control of ETDs, especially the NTDs and malaria in Southeast Nigeria. It also highlights contextual issues and enablers influencing getting evidence from HPSR into policy and practice for more effective control of NTDs and malaria.
Methods
Study Area and Design
The study was undertaken in Anambra and Enugu States that are located in the southeastern part of Nigeria. In 2018, the estimated population of Anambra state is 4.5 million while that of Enugu state is 3.3 million. The annual growth rate for both states is 2.8% (28). Structurally, the states’ health systems are organized in three tiers: primary healthcare, secondary healthcare facilities, and the tertiary healthcare. The State Ministry of Health (SMOH) manages and coordinates primary and secondary healthcare services in the States. The States have co-endemicity of several NTDs including onchocerciasis, schistosomiasis, and soil-transmitted helminthiasis (29). The recent Nigeria survey in 2018 shows high prevalence of malaria in Anambra and Enugu State, respectively (30).
The study adopted a qualitative cross-sectional design to assess users of evidences (policy-makers and program managers/implementers) knowledge, capacity, and use of HPSR evidence in decision-making or implementation of programs for the control of ETDs in Anambra and Enugu States, Southeast Nigeria.
Study Participants and Sampling
The study respondents comprised of top- and mid-level users of evidence drawn from SMOH and State Primary Health Care Development Agency (SPHCDA), which is agency of the SMOH. The respondents were purposively selected based on their various roles and current involvement in endemic disease control. They included policy-makers: Commissioners of health, Permanent Secretaries of the SMOH, Executive Secretaries of SPHCDA; Divisional heads/Directors of the Department of Public Health/disease control, Planning Research and Statistics, Pharmaceutical services and Medical services; Hospital Administrator of States Health Management Boards; Program Implementer: Program Managers of States Malaria Control and Elimination Program (SMEP) and Neglected Tropical Diseases (NTDs) control programme and; data managers: Health Management and Information System (HMIS) Officers, planning officers, and data analysts/statistician. These respondents are saddled with day-to-day management, implementation of programs and decision-making targeted towards the control of ETDs in the States.
Data Collection
An in-depth interview (IDI) guide developed by the study team was used to collect information from the above-listed respondents. Prior to commencement of actual data collection, the guide was reviewed by experts in HPSR for construct validity. The validated instrument was then pretested on similar respondents in Ebonyi State (a neighboring state also located in southeast Nigeria) fortnight to the actual data collection. Thereafter, the tool was duly revised and modified following feedback from the pretest exercise, which was then used for the actual data collection.
The IDI guide elicited information on knowledge of HPSR and its relationship to evidence-informed decision-/policy-making for the control of ETDs; individual and institutional capacity to use research evidence; use and roles research evidences play in endemic diseases control; procedures in place in the organization(s) for evidence-informed decision-making; current sources and methods of getting research evidence for programming or planning. The guide also explored contextual factors enabling and/or constraining use HPSR evidence in planning and implementing programs. The same guide was used to collect information from the both study States.
Interview appointments were sought from the respondents by either personal visits, phone text message, or voice calls by the trained study team. Interviews were conducted in pairs (an interviewer and a note-taker) by trained and experienced qualitative researchers as in their various offices as convenient for the respondents. Each interview was conducted in English and lasted about 50–60 min, audiotaped, and transcribed verbatim. Permission to audio record interview was sought and obtained from each respondent. Notes taken during the interviews were built into the transcripts. Data collection and analysis was done between July and September 2016. The findings were then presented during the validation meeting shortly after the data collection in November 2016, in which the stakeholders and respondents participated and with the objective of verifying the accuracy and trustworthiness of the results, and positive feedback was obtained
Data Analysis
Thematic manual content analysis approach was used for the data analysis. This involved extensive reading and proofreading of the transcripts to get familiar with the concepts, coding the data manually based on pregenerated codes from the study objectives and the IDI guide, consolidating emerging themes under common themes, and interpretation (31). The final themes and subthemes generated (Figure 1) were then applied to the entire transcripts.
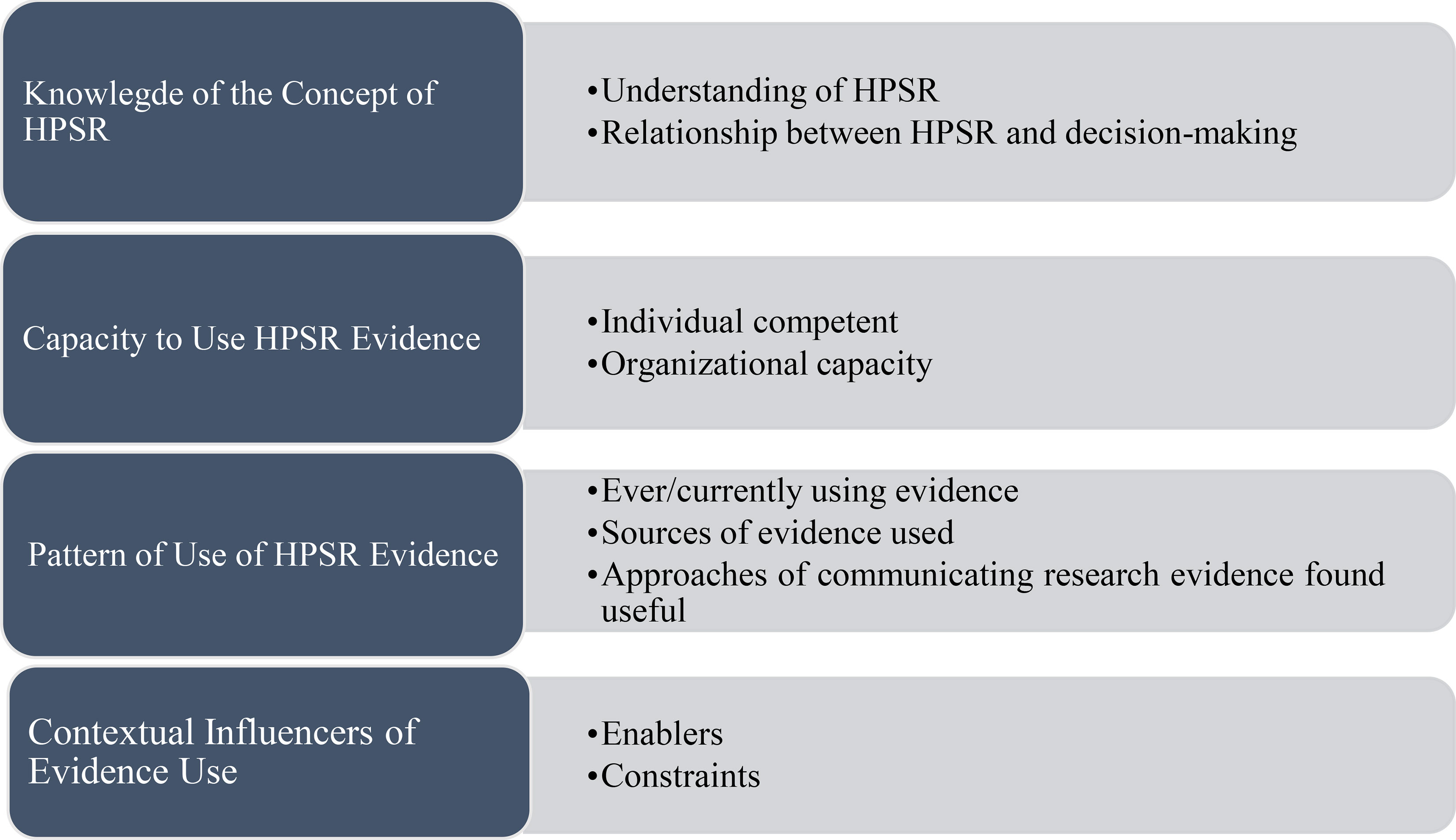
Figure 1 Coding framework for knowledge and use of HPSR evidence among users of evidence for the control of endemic diseases.
Results
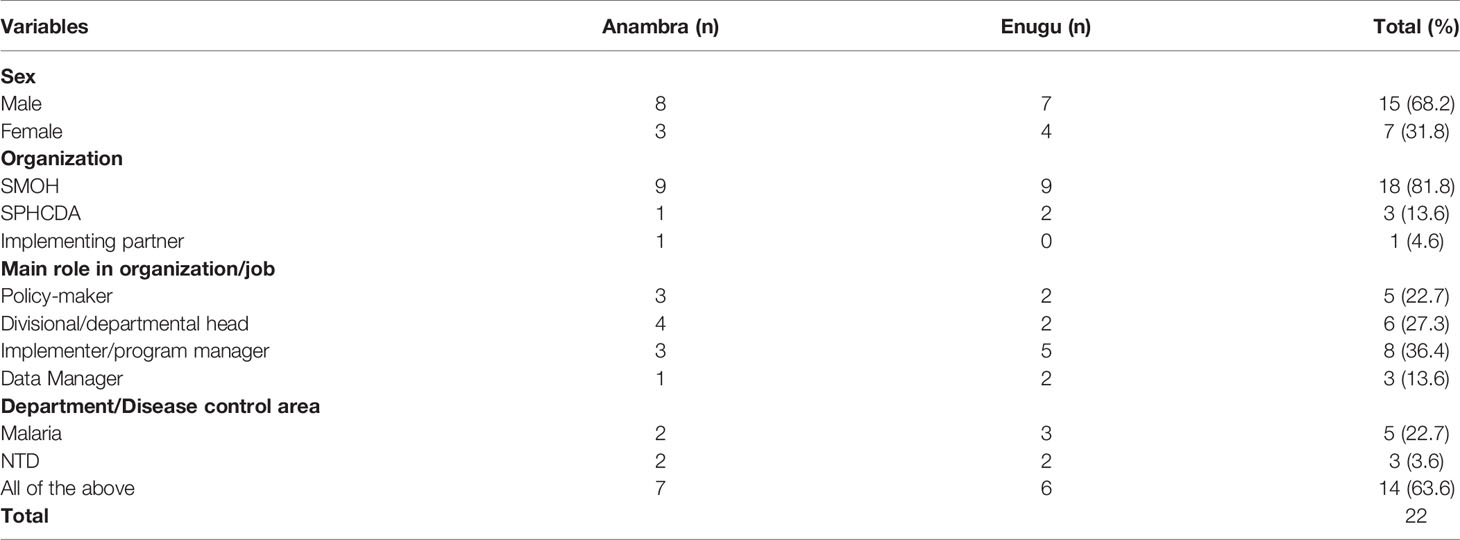
A total of twenty-two (22) interviews were conducted in both States. Table 1 highlights the background information of the respondents. The results are presented according to the key themes that were explored as described in the data analysis section (Figure 1). A total of 15 (68.2%) respondents were males, while 7 (31.8%) were females. Majority of the respondents 18 (81.8%) were from SMOH. With respect to the main role in their various organizations, 22.7% were policy-makers, 27.3% divisional heads, and 36.4% program implementers. Most of the respondents, 14 (63.6%), were currently coordinating/making decisions for malaria and NTD diseases control as at the time of the study in their states.
Knowledge of HPSR and Its Relationship With Evidence-Informed Decision-Making in ETDs Control
Understanding of HPSR
The respondents’ opinions and responses about their understanding of HPSR varied greatly from descriptive definition to sparse knowledge. A common response was that HPSR is aimed at improving service delivery towards ETDs and the health system at large. Respondents expressed their understanding of health policy and systems research to include: (i) evaluation of policies to identify gaps and how to bridge the gaps. “HPSR is to review and see some of the policies in health by the government at both federal and state; to see how we have been making use of them, to identify gaps and source for refined ways of bridging the gaps so that it will continue to improve and the system will continue to improve” (EU1); (ii) in-depth study of organizational directions; (iii) a platform that enables interaction of different stakeholders in the development and implementation of policies; and (iv) the process of generating and sharing information. “You have different actors that interact to produce policy and its implementation. So it [HPSR] is like a multi-disciplinary platform, where people come together to generate information including data and all that to improve on the situation” (EU2).
HPSR was also perceived to have to do with the process of gathering and synthesizing recommendations made from several multidiscipline research findings and using these recommendations to bring about positive change in patterns of practice or policy. This process of change would then involve multiple and relevant stakeholders.
“HPSR is the overall framework that guides the roll out of plans and programs to implement health care delivery. And the system research will be things like operational research that will be ongoing, as ways and means of improving the system” (AU05).
“My understanding, maybe as the name is, health policy and system researches; I think it has to do with the generality of health of the nation and everything that goes into it. How is it done? Finding what is happening, what we wish to do, and also finding out what should be done. And first of all, you have to find out what is there, what we need to do, research into possible solutions, alternatives, best practices, and things that will work, generally in our climate, everything. It has to do with everything!” (AU04).
Other respondents expressed their understanding of HPSR to mean the use of data output at the facility level to plan further programs: “Well, my own understanding is based on findings of what is happening in our health facilities. For us to know where we will focus more, we will focus our intervention. But before you commence any intervention, you must know the situation, I mean the situation report before you think about any intervention” (AU01).
Relationship Between HPSR and EIDM
Concerning HPRS relationship with EIDM, a respondent stated that “although in the Nigerian, policies are made just to catch up with what is going on and are not being actively followed or used” (EU6). There was a general understanding that decisions and policies should be guided by evidence from research and other evidence sources such as utilization data. According to them, evidence is necessary for forecasting and future planning. In the words of a respondent, “evidence will make you know the direction you are going in terms of implementation” (EU4). Hence, the purpose of HPSR is to use evidence from research to guide decisions for health systems improvement and policy change. This forms the basis of the relationship between HPSR and EIDM. “HPSR is a way of using the product of your research to effect policy change for the health system” (AU3).
Some respondents mentioned the consequences of making decisions that are not evidence-informed to include inequitable allocation of resources, inefficiencies, and poor health outcomes.
Capacity to Use HPSR Evidence
Individual Competence
The individual competence for HPSR among users of evidence were perceived to be quite poor, given their different roles and levels of experience. However, most respondents stated they had not been involved in HPSR or any form of research in the past so had either produced, communicated, or used other forms of evidence in decision-making. Nevertheless, most respondents had never used research evidence for decision-making; they felt that given their experience of using other forms of evidence, they would be able to use HPSR evidence if they had to.
Organizational Capacity
Majority of the respondents stated that they have poor capacity for HPSR within their various organization. Some of their views were that (i) capacity to use research evidence for decisions does not exist or is inadequate, “For now, I don’t think we have such capacity to carry out such” (AU4); (ii) capacity exists in silos not as a group, “Everybody is doing at his own individual capacity, but not for the state ministry of health” (EU1); (iii) most policy-decisions are political rather than evidence-based; (iv) use of research evidence in decision-making is not a culture of the SMOH, “It is not a practice. We are still learning these new concept” (EU5), “…we use projection in planning our programs” (AU9); (v) people receive training on how to use data for planning but, “The capacity they have received to make organizational decision based on evidence have been short of expectation” (EU2). It was reported that the directorate for planning, research, and statistics at the SMOH, which is responsible for collating and analyzing data and making it available for planning and policy-making towards better control of endemic diseases, has not been able to have been in moribund state. In the word of a respondent, “Some of us that are in the DPRS don’t know what it [research evidence] is even all about” (AU4), thus “the department may not be working optimally” (AU5). More so, there was consensus that notwithstanding of the existence of the directorate, there is no policy, strategy, or guideline for ensuring that research evidence is used for decision-making. Hence, there is no functional structure in place at the SMOH to ensure that research evidence is used for decision- and policy-making.
However, some respondents reported they had a functional organizational structure for EIDM and had this to say:
“We have an M&E unit and district health information system database—HMIS. We collect data from the facilities and from the government and these are fed back into the design of the endemic diseases control programme/activities. It is like a cycle. The information comes, it gets straight back into the system and it continues.” (EU7).
“From the data elements that we can also advice the government and we also brief them on the ways forward in any of these programs depending on the information we have gathered.” (EU4).
Pattern of Use of HPSR Evidence for Decision-/Policy-Making
Ever or Currently Using HPSR Evidence
Most of the respondents were of the opinion that evidence informs decisions made in their units, departments, and the State Ministry of Health as a whole for i) developing policy and strategies; ii) implementing various programs; iii) reviewing programs; and iv) budgeting. According to program manager, a “recent evidence from individual research and the state NTDs report will be used in planning further programme … there is one we conducted last month on Filariasis. Then another one conducted on Schistosomiasis, we are using the evidence to plan our upcoming program, those ones have not been implemented … once the Carter Centre [Donor Agency on NTDs] takes decision on it, it will be implemented” (AU09). Other instances where evidence had been used for decision-making although not directly related to ETDs were also reported. In the words of a director:
“The federal government gave us the result of a nation-wide survey, the finding says that the HIV prevalence of our state is 9.7%, which tells us that we are in a danger, that’s why we stand on that result in making our yearly budgeting…. That is why we push more money in HIV prevention and treatment.” (AU01).
Another respondent reported that their department’s decision to register and train traditional birth attendants for safer provision of maternity (particularly delivery) services was based on a research outcome. According to her:
“In our public health facilities, we always have a lot of women attending antenatal clinic but during delivery, only few of them deliver in public facilities. So we started asking ourselves, where did they go? From the research we got from the women who attends antenatal care, we discovered that most of the time, they go to the TBAs [for delivery] for various reasons. That was the reason we started training the TBAs in our state.” (EU8).
However, some respondents stated that research evidence does not play a significant (or any) role in decision-making for the control of malaria and NTDs in the SMOH. “For now, I don’t think there is a role that research plays. Most at times we use projection in determining these interventions” (EU4). It was noted that personal and political interests greatly influence decisions made and may actually be the first consideration in deciding on what gets into the period (operational or strategic) plans of the ministry/agency. A policy-maker stated that “what we normally put in our annual plan is based on the priorities and policy thrust of the present administration. So we consider that first, the policy thrust, and the desire of the present administration” (EU4).
Sources of HPSR Evidence
HMIS data generated from health facilities on service delivery appears to be the main source of evidence for decision-making towards ETDs control. Most respondents stated that they have found this to be extremely useful because it is representative, exhaustive, and collected regularly.
Other sources include i) community/large surveys reports such as DHS; ii) program reports; iii) journal articles including form professional groups, online articles and; iv) reports from implementing partners and donor agencies. Survey reports have been used in the past to determine what quantity of materials, drugs, or commodities to supply to facilities for control of malaria and other NTDs. Journals have been found useful because “it helps us to know the best practice” (EU5).
According to some respondents, program reports are found to be useful for the following reasons: (i) coherence of information; (ii) relevance of recommendations; (iii) regularity, “our monthly reports come every month” (EU6); (iv) adequacy of content; (v) simplicity of the report. “The program report I get every month is more like conversations of different program areas, issues, and challenges” (EU6); (vi) verifiable source of data/information and; (vii) affords opportunity for comparison with other States.
However, some respondents stated that the least preferred are the publications and technical reports due to perceived lack of time to read and a poor reading culture of users of evidence, “…because, in our society, people don’t tend to be good…., they are not good at reading. So, if you put things in books, they may not read it…” (AU02).
Approaches of Communicating Research Evidence Most Useful for Decision-Making
There was a general view that there is no particular method of communicating research evidence that fits decision-making all the time. Instead, a number of factors such as purpose of information, target audience and availability of resources, time and skills influence the choice of methods used in the past. These factors also determine which method is most appropriate to use. “I wouldn’t say there is one particular method that you should do, because it depends on the people, it depends to a large extent on your target population and you’re the objectives of the program” (EU7). Table 2 summarizes most commonly used strategy of communicating research evidence found useful for decision-making towards endemic disease control.
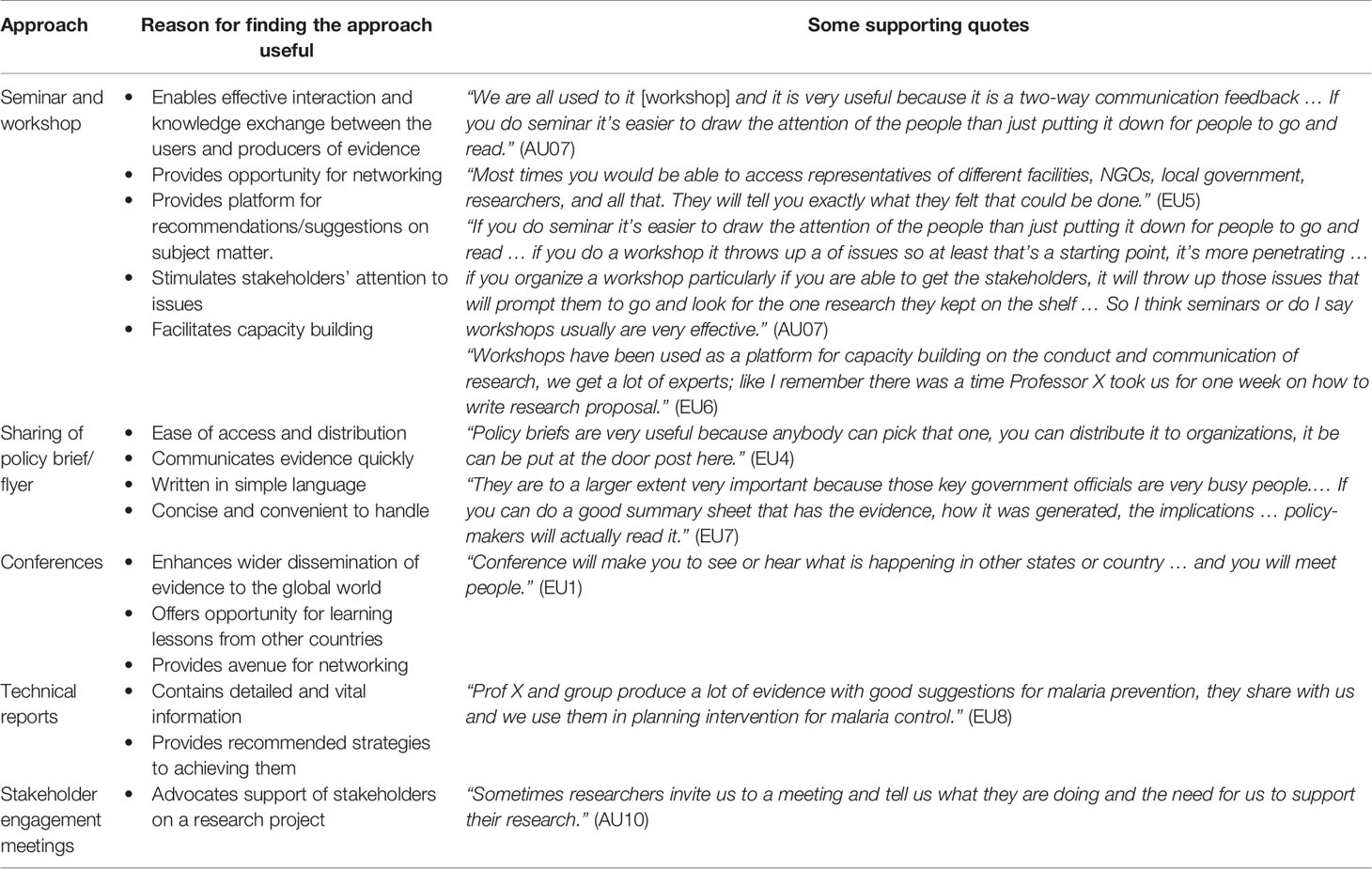
Table 2 Approaches for communicating research evidence for decision-making towards endemic disease control.
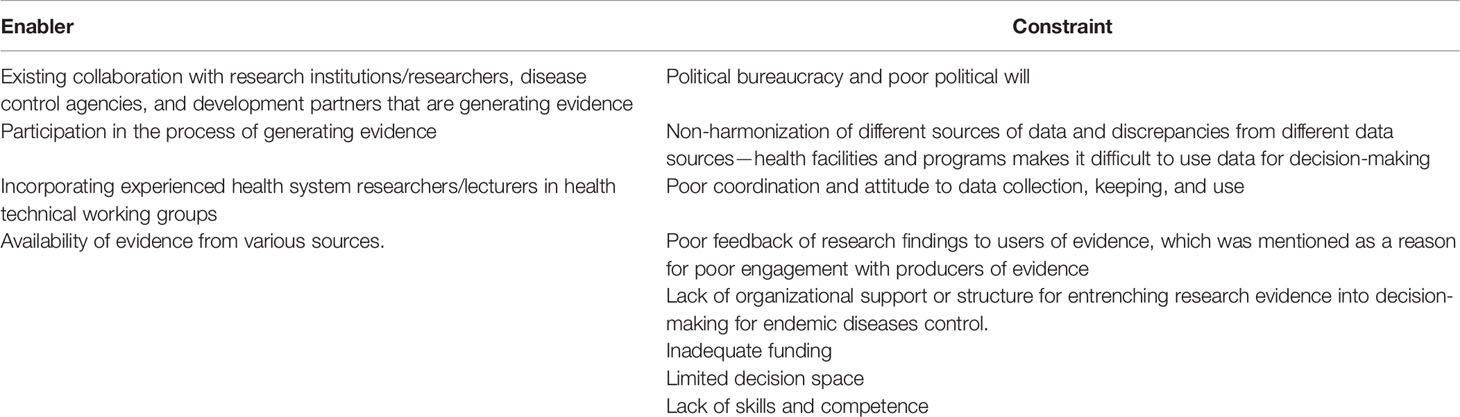
Contextual Influences on Evidence Use for Decision-Making
Enablers
Factors that have enabled respondents in using research evidence for decision-making or influencing policy for the control of endemic diseases include (i) existing collaboration with research institutions/researchers, disease control agencies, and development partners that are generating evidence; “We have good relationship with research institutions and with so many other bodies, even other development partners who also generate their own evidence. For instance, SPARC. They work with the government and generate a lot of information, we get them from them” (EU7); (ii) participation in the process of generating evidence, “When you have findings from the process you have undertaken, it makes it easier for you. You feel happy when you have employed yourself in generating that output” (EU5); (iv) incorporating experienced health system researchers/lecturers in health technical working groups for endemic diseases program/policy and; (v) availability of adequacy of evidence from various sources.
Constraints to EIDM
A major constraint to evidence-informed decision-making for endemic disease control that was identified is political bureaucracy, which causes delays in research uptake. More so, it appears that, contextually, research and use of research evidence has not received much support as there is a lack of political will, in that the ruling class prefers to fund projects with tangible outcomes like structures and buildings in order to get further support from their electorate.
“In Nigeria, and most developing countries, they [politicians] always believe in visible capital projects. …They want to see structures in order to win elections and all that … So in political era and political situation, you see them spend money on buildings and unnecessary health centres, and hospitals … the most important thing for them is that they are building so that their electorate will see them and vote them again. Now, when it comes out to intellectual property like experts meetings, workshops, etc., and real health programme planning that are nor physical structures, they won’t fund them.” (AU13/AP05).
Another constraint is non-harmonization of different sources of data and discrepancies from different data sources—health facilities and programs—making it difficult to synthesize and use data for decision-making.
“The problem we are facing is the harmonization. Because, the partners will come with their own, the federal government will come with their own, and we also align our own with the federal government. The partners, the state and federal government have their way of collecting data, and then you have discrepancies.” (EU4).
Other constraints to evidence use in decision-making include (i) lack of skills and competence to analyze and use data; (ii) inadequate funding is a major challenge to collation and synthesizing of data from health facilities; (iii) poor coordination of data collection, and storage, “…you can go to the facility or even SMOH and ask for evidence of epidemic we had one year ago, and you will be surprised that they do not have it” (AU11); (iv) no or little feedback of research findings to users of evidence, which was mentioned as a reason for poor engagement with producers of evidence.
“Well most of the time the university community/researchers … come for one research or the other but they will not come back to tell you what they got or their findings; they will just finish from the field and go back to their school.” (EU10).
(v) lack of organizational support or structure for entrenching research evidence into decision-making for endemic diseases control and; (vi) limited decision space. The summary of contextual factors influencing use of HPSR evidence in endemic disease control is presented in Table 3.
“Most of the decisions are taken by the ministry/agency, so you are not autonomous, you follow them because he who pays the piper dictates the tune…” (AU09).
“Basically, programs and policies are already packaged and then sent [either from donors, State or Federal government] for us to implement.” (EU9).
Discussion
The high knowledge of HPSR and its relationship with EDIM among the respondents in this study could be attributed to previous collaboration or engagement including seminars, workshops, and conferences organized by health systems researchers/academic communities where users of evidence were exposed to the concept of HPSR. Although, the results of our sample may not be generalizable to Nigeria, since we collected data from just two states out of 36 states in Nigeria, the knowledge that was provided is transferable to similar contexts.
The finding of poor capacity to use evidence from research for decision-making process among policy-/decision-makers due to various contextual barriers implies that it is important for policy-/decision-makers to understand the gravity of not using evidence in decision-making. This capacity could be developed with continuous and sustainable capacity building on HPSR and advocacy to policy-/decision-makers on the positive value of EIDM for more effective control of NTDs and addressing other health system challenges. A previous study had highlighted several solutions including the institutionalization of sustainable capacity building to poor individual and organizational capacity to use research evidence in programs and policy geared towards ETDs control (5, 32–34). It has been shown that capacity building of policy-/decision-makers can improve both individual and organizational competency for HPSR towards more effective control of endemic diseases (35, 36).
The finding that although many of the policy/decision-makers were knowledgeable that research evidence should inform policy decisions but only a few reported they are currently using/have ever used in the past for developing policy/strategy and implementation or reviewing programs shows that high knowledge or awareness of HPSR does not translate to policy and practice. Our finding is in line with other studies that reported limited use of evidence in decision-making (18, 37), and in contrast with another study that found knowledge to translate to evidence use (4).
In line with our findings, other studies had reported that one important reason for the lack of adequate commitment to the evidence-to-policy process in the Nigerian health system is the policy-maker’s poor capacity of accessing, synthesizing, and utilizing existing research evidence (2, 38). Certainly, without sufficient capacity in knowledge translation and HPSR, users of evidence will not have the capacity of accessing and synthesizing information for EIDM, and the potential for shared learning will be misplaced. The results on institutional barriers to optimal use of evidence in decision-making toward ETDs are in concordance with other studies (32–34, 37, 39, 40).
Our study shows that there are clear channels for gathering evidence that could be used for decision-making, with the main and preferred source of receiving research evidence to be from the routine Health Management Information System (HMIS). The preference for HMIS among users of evidence is not a surprise because the platform is hosted in the SMOH. Hence, the policy-makers/decision-makers are familiar with the information and it is also readily available to them.
A major strength of this study is that it explored the views of actors who are involved either directly and/or indirectly with the planning and/or implementation of the ETDs and NTDs control programs. These actors are needed for getting research evidence into policy and practice. Also, the application of the qualitative method allows in-depth exploration and understanding of the subject matter.
The study has some limitations. First, it was a relatively small study sample size of 22 in both states, which may have provided limited insights with respect to the study findings. However, our reliability and trust of the study is the fact that we specifically sampled targeted key state implementers and policy-makers involved in disease control programs and decision-making/implementation while excluding those who were not involved in disease control programs, which contributed to the limited sample number. More so, the results of our sample may not be generalizable to Nigeria, since we collected data from only two out of 36 states in Nigeria. However, principles highlighted in this study may be transferable to similar settings.
In conclusion, the paper shows that there is a high level of awareness about evidence from HPSR and the usefulness of such evidence in decision-making. However, this awareness does not translate to optimal use of evidence from HPSR for decision-making in the control of ETDs due to weak organizational capacity and other institutional constraints. Our findings suggest that there is the need to invest in sustainable and continuous capacity-building activities to develop a critical mass of users of evidence (policy-/decision-makers) in HPSR as well as setting up of institutional structure and processes to facilitate enhanced uptake of high-quality evidence into policy decisions for better control of ETDs.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Health Research and Ethics Committee, University of Nigeria Teaching Hospital, Enugu. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
OO conceptualized the study. UE and OO collected and analyzed the data. UE drafted the first manuscript. Both authors read, revised, and approved the manuscript before submission. All authors contributed to the article and approved the submitted version.
Funding
The study received financial support from the UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (WHO/TDR) (Reference 2015/B40427).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Authors are grateful to the Ministries of Health in Enugu and Anambra states for granting approval to conduct this study. We also thank the researchers that participated in the data collection and analysis.
References
1. World Health Organization (WHO). Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes. WHO’s Framework for Action. Geneva: WHO (2007).
2. Uneke CJ, Ezeoha AE, Ndukwe CD, Oyibo PG, Onwe F, Igbinedion EB, et al. Individual and Organisational Capacity for Evidence Use in Policy Making in Nigeria: An Exploratory Study of the Perceptions of Nigeria Health Policy Makers. Evid Policy (2011) 7(3):251–76(26). doi: 10.1332/174426411x591744
3. Global Health Council. Getting Research Into Policy and Practice (GRIPP). Available at: http://www.globalhealth.org/view_top.php3?id=186 (Accessed 12 April 2021).
4. Chu KM, Jayaraman S, Kyamanywa P, Ntakiyiruta G. Building Research Capacity in Africa: Equity and Global Health Collaborations. PLoS Med (2014) 11(3):e1001612. doi: 10.1371/journal.pmed.1001612
5. Campbell DM, Redman S, Jorm L, Cooke M, Zwi AB, Rychetnik L. Increasing the Use of Evidence in Health Policy: Practice and Views of Policymakers and Researchers. Aust New Z Health Policy (2009) 6:21. doi: 10.1186/1743-8462-6-21
6. Dobrow MJ, Goel V, Upshur REG. Evidence-Based Health Policy: Context and Utilization“. Soc Sci Med (2004) 58:207–17. doi: 10.1016/S0277-9536(03)00166-7
7. Golub RM, Fontanarosa PB. Comparative Effectiveness Research Relative Successes. JAMA (2012) 307(15):1543–645. doi: 10.4172/2471-268X.1000132
8. Herrick LM, Locke GR, Zinsmeister AR, Talley NJ. Challenges and Lessons Learned in Conducting Comparative-Effectiveness Trials. Am J Gastroenterol (2012) 107:644–9. doi: 10.1038/ajg.2011.475
9. Word Health Organization (WHO). Available at: https://www.who.int/news/item/28-01-2021-who-issues-new-10-year-plan-to-end-suffering-from-neglected-tropical-diseases.
10. Okorie PN, Ademowo GO, Saka Y, Davies E, Okoronkwo C, Bockarie MJ, et al. Lymphatic Filariasis in Nigeria; Micro-Stratification Overlap Mapping (MOM) as a Prerequisite for Cost-Effective Resource Utilization in Control and Surveillance. PLoS Negl Trop Dis (2013) 7(9):e2416. doi: 10.1371/journal.pntd.0002416
11. Hotez PJ, Asojo OA, Adesina AM. Nigeria: ‘‘Ground Zero’’ for the High Prevalence Neglected Tropical Diseases. PLoS Negl Trop Dis (2012) 6:e1600. doi: 10.1371/journal.pntd.0001600
12. Adenowo AF, Oyinloye BE, Ogunyinka BI, Kappo AP. Impact of Human Schistosomiasis in Sub-Saharan Africa. Braz J Infect Dis (2015) 19(2):196–205. doi: 10.1016/j.bjid.2014.11.004
13. Federal Ministry of Health. Nigeria Master Plan for Neglected Tropical Disease (NTDs) 2013–2017 Vol. 142. . Abuja: Federal Ministry of Health (2013).
14. WHO. World Malaria Report 2020: 20 Years of Global Progress and Challenges. Geneva: World Health Organization (2020). Licence: CC BY-NC-SA 3.0 IGO.
15. National Malaria Elimination Programme (NMEP), National Population Commission (NPopC), National Bureau of Statistics (NBS), ICF International. Nigeria Malaria Indicator Survey 2015. Abuja, Nigeria, and Rockville, Maryland, USA: NMEP, NPopC, and ICF International (2016).
16. National Population Commission (NPC) [Nigeria], ICF. Nigeria Demographic and Health Survey - 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF (2019). Available at: https://dhsprogram.com/pubs/pdf/FR293/FR293.pdf.
17. Zardo P, Collie A. Predicting Research Use in a Public Health Policy Environment: Results of a Logistic Regression Analysis. Implement Sci (2014) 9:142. doi: 10.1186/s13012-014-0142-8
18. Oliver K, Innvaer S, Lorenc T, Woodman J, Thomas J. A Systematic Review of Barriers to and Facilitators of the Use of Evidence by Policymakers. BMC Health Serv Res (2014) 14:2. doi: 10.1186/1472-6963-14-2
19. Ouimet M, Bédard P-O, Turgeon J, Lavis JN, Gélineau F, Gagnon F, et al. Correlates of Consulting Research Evidence Among Policy Analysts in Government Ministries: A Cross-Sectional Survey. Evid Policy J Res Debate Pract (2010) 6:433–60. doi: 10.1332/174426410X535846
20. Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in Knowledge Translation: Time for a Map? J Contin Educ Health Prof (2006) 26(1):13–24. doi: 10.1002/chp.47
21. World Health Organization. Implementation Research Toolkit−Workbook. World Health Organization on Behalf of the Special Programme for Research and Training in Tropical Diseases. Geneva, Switzerland: World Health Organization (2014).
22. Humphries S, Stafinski T, Mumtaz Z, Menon D. Barriers and Facilitators to Evidence-Use in Program Management: A Systematic Review of the Literature. BMC Health Serv Res (2014) 14:171. doi: 10.1186/1472-6963-14-171
23. Green A, Bennett S eds. “Sound Choices: Enhancing Capacity for Evidence-Informed Health Policy”. In: AHPSR Biennual Review. Geneva: WHO, Alliance for Health Policy and Systems Research.
24. Alliance for Health Policy and Systems Research. What is HPSR? (2007). Available at: http://www.who.int/alliance-hpsr/about/hpsr/en/index.html (Accessed on 12 March 2021).
25. WHO. Changing Mindsets - Strategy on Health Policy and Systems Research. Geneva: World Health Organization (2012).
26. Gilson L ed. Health Policy and Systems Research. A Methodology Reader. Geneva, Switzerland: Alliance for Health Policy and Systems Research, World Health Organization (2012).
27. Sheikh K, Gilson L, Agyepong IA, Hanson K, Ssengooba F, Bennett S. Building the Field of Health Policy and Systems Research: Framing the Questions. PLoS Med (2011) 8(8):e1001073. doi: 10.1371/journal.pmed.1001073
28. National Bureau of Statistics (NBS). Social Statistics in Nigeria. Abuja, Nigeria: Federal Republic of Nigeria (2019).
29. National Population Commission (NPC) [Nigeria] and ICF. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF (2019).
30. Federal Ministry of Health (FMOH). Nigeria Master Plan for Neglected Tropical Diseases (NTDs) 2013-2017. Abuja, Nigeria: FMOH (2012).
31. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the Framework Method for the Analysis of Qualitative Data in Multidisciplinary Health Research. BMC Med Res Method (2013) 13:117. doi: 10.1186/1471-2288-13-117
32. Ezenwaka U, Mbachu C, Etiaba E, Uzochukwu B, Onwujekwe O. Integrating Evidence From Research Into Decision-Making for Controlling Endemic Tropical Diseases in South East Nigeria: Perceptions of Producers and Users of Evidence on Barriers and Solutions Health Research Policy and Systems. Health Res Policy Syst (2020) 18(4):1–10. doi: 10.1186/s12961-019-0518-y
33. Sibbald S, Tetroe J, Graham I. Research Funder Required Research Partnerships: A Qualitative Inquiry. Implement Sci (2014) 9(1):176. doi: 10.1186/s13012-014-0176-y
34. Dwan KM, Mcinnes P, Mazumdar S. Measuring the Success of Facilitated Engagement Between Knowledge Producers and Users: A Validated Scale. Evid Policy J Res Debate Pract (2015) 11(2):239–52. doi: 10.1332/174426414X14165029835102
35. Onwujekwe O, Etiaba E, Mbachu C, Arize I, Nwankwor C, Ezenwaka U, et al. Does Improving the Skills of Researchers and Decision Makers in Health Policy and Systems Research Lead to Enhanced Evidence-Based Decision Making in Nigeria?—A Short Term Evaluation. PLoS One (2020) 15(9):e0238365. doi: 10.1371/journal.pone.023836
36. Onwujekwe O, Mbachu C, Etiaba E, Ezumah N, Ezenwaka U, Arize I, et al. Impact of Capacity Building Interventions on Individual and Organizational Competency for HPSR in Endemic Disease Control in Nigeria: A Qualitative Study. Implement Sci (2020) 15:22. doi: 10.1186/s13012-020-00987-z
37. Onwujekwe O, Etiaba E, Mbachu C, Ezenwaka U, Chikezie I, Arize I, et al. Building the Capacity of Users and Producers of Evidence in Health Policy and Systems Research for Better Better Control of Endemic Diseases in Nigeria: A Situational Analysis. Global Health (2019) 15(69):1–11. doi: 10.1186/s12992-019-0530-6
38. Uneke CJ, Ezeoha AE, Ndukwe CD, Oyibo PG, Onwe F, Ogbonna A. Assessment of Organizational Capacity for Evidence Based Health Systems Operations in Nigeria. Soc Work Public Health (2013) 28(2):97–108. doi: 10.1080/19371918.2011.555639
39. Shroff1 ZC, Javadi D, Gilson L, Kang R and Ghaffar A. Institutional Capacity to Generate and Use Evidence in LMICs: Current State and Opportunities for HPSR. Health Res Policy Syst (2017) 15:94. doi: 10.1186/s12961-017-0261-1
Keywords: evidence-based policy, health policy and systems research, HPSR, neglected tropical diseases, NTDs, getting research into policy and practice, GRIPP
Citation: Ezenwaka U and Onwujekwe O (2021) Getting Evidence From Health Policy and Systems Research Into Policy and Practice for Controlling Endemic Tropical Diseases in Nigeria: Assessing Knowledge, Capacity, and Use. Front. Trop. Dis 2:735990. doi: 10.3389/fitd.2021.735990
Received: 04 July 2021; Accepted: 06 September 2021;
Published: 24 September 2021.
Edited by:
Yodi Mahendradhata, Gadjah Mada University, IndonesiaReviewed by:
Prakash Ghimire, Tribhuvan University, NepalJianhai Yin, National Institute of Parasitic Diseases, China
Copyright © 2021 Ezenwaka and Onwujekwe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Uchenna Ezenwaka, ZXplbndha2F1Y2hlQHlhaG9vLmNvbQ==
 Uchenna Ezenwaka
Uchenna Ezenwaka Obinna Onwujekwe
Obinna Onwujekwe