- 1College of Medicine and Health Sciences (CMHS), University of Rwanda, Kigali, Rwanda
- 2Department of Obstetrics and Gynecology, Kigali University Teaching Hospital, Kigali, Rwanda
- 3Planning, Monitoring and Health Financing Department, Ministry of Health, Kigali, Rwanda
- 4Chronic Diseases Initiative for Africa (CDIA), University of Cape Town, Cape Town, South Africa
- 5Non-Communicable Disease Division, Rwanda Biomedical Centre, Kigali, Rwanda
- 6Pettenkofer School of Public Health, Munich, Germany
- 7Institute for Medical Information Processing, Biometry and Epidemiology, Maximilian University of Munich, Munich, Germany
- 8Centre for Evidence-based Health Care, Division of Epidemiology and Biostatistics, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
- 9Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- 10Internal Medicine Department, Kigali University Teaching Hospital, Kigali, Rwanda
Background: Collaborative approaches to generating knowledge between knowledge users (KUs) and researchers as a means of enhancing evidence-informed decision making have been gaining ground over the last few years. The principal study targeted rural and urban communities within the catchment areas of Cyanika health centre (Burera district, Northern Province) and Kacyiru health centre (Gasabo district, in City of Kigali), respectively to understand perceptions and preferences of communication with respect to cardiovascular disease (CVD) risk in Rwanda. This paper describes the integration of citizen science within an integrated knowledge translation (IKT) approach for this study.
Methods: The citizen science approach included deliberate, selective and targeted engagement of KUs at various steps throughout the study. It incorporated national and district levels stakeholders, primary health care stakeholders, local community leaders and influencers, and local community members (selected and trained to be termed citizen scientists) in the process of implementation. Data for this paper included minutes, reports and notes from meetings and workshops which were perused to report the immediate outcomes and challenges of citizen science within an IKT approach for a study such as described for Rwanda.
Results: As a result of a deliberate IKT strategy, key national stakeholders attended and contributed to all phases of citizen science implementation. Project-based and relationship-based immediate outcomes were documented. In line with local community health issues reported by the citizen scientists, the local community stakeholders pledged home grown solutions. These included enhancement of compliance to implement the “kitchen garden per household” policy, teaching local residents on preparation of healthy diet from locally available food items, organizing collective physical activity, fighting against locally made substandard beverages and teaching local residents on CVD (risk factors). As an indicator of the probable uptake of research evidence, district officials appreciated citizen scientists’ work and decided to consider presented results in their next fiscal year action plan.
Conclusion: Citizen science proved to be an important strategy for research co-production in Rwanda. While this strategy falls within the remit of a larger IKT approach it focuses on the role and ownership of research by local community residents. This study demonstrated that to improve the relevance and impact of research in local community a deliberate IKT approach that incorporates citizen science can be invaluable.
Introduction
Collaborative approaches to generating knowledge between knowledge users (KUs) and researchers as a means of enhancing evidence-informed decision making have been gaining ground over the last few years (1). The generation of knowledge that responds to the needs of health systems’ knowledge users requires context sensitive approaches (1). Otherwise, health sector policy and strategic development plans advance inappropriate or irrelevant action if they do not take into account participatory approaches to identify and solve community public health issues.
Citizen science – also at times referred to as community-led or community-based participatory research (CBPR) (2) - is one such participatory approach and has previously been described as the general public engagement in scientific research activities when citizens actively contribute to science either with their intellectual effort or surrounding knowledge or with their tools and resources (3). It can inform local policy makers about residents’ perceptions and views, and provide access to lay knowledge (3). This helps to formulate policies and design interventions relevant to the local context. This is in line with Horowitz C et al. who argue that communities can be armed to advocate for what they need, combining arguments based on evidence and ethics: doing what works and doing what is right (4). Citizen science is critically perceived by some scholars as a process of producing scientific knowledge in which non-scientific or non-professional actors — whether individuals or groups — actively and intentionally participate (5). Other researchers proved citizen science to be helpful when there is a need to develop tailored interventions and they considered it as an expression of democratic values (3).
The co-production of knowledge through an ongoing relationship between researchers and research users is intended to be mutually beneficial, and this is what called an integrated knowledge translation (IKT) approach (6, 7). Research projects incorporating an IKT approach aim to create context-sensitive research, that is relevant and accessible to decision-makers, thus supporting decision making and improving the health of populations (6, 7). KUs include stakeholders involved in policy-making and practice as well as the end recipients, such as communities (individuals or group of individuals), that are influenced by the intervention (2). Thus, it is rational and worthy to embed citizen science within the IKT in case there is need to tailor knowledge for use within specific contexts and support the development of evidence-based decisions. Integrating citizen science within an IKT approach could be in the response to the call from Jull J et al. to consider both CBPR/citizen science and IKT approaches and processes when designing and conducting a collaborative research that has co-creation of knowledge as the aim (1).
In that regard, the Collaboration for Evidence Based Healthcare and Public Health in Africa (CEBHA+) project in Rwanda considered integrating citizen science within a broader study that aimed to understand urban and rural community residents’ perceptions and preferences of communication with respect to cardiovascular disease (CVD) risk. This approach was implemented in three out of five CEBHA+ sites (Ethiopia, Malawi and Rwanda) and the study protocol integrating the citizen science implementation was published elsewhere (8). Further details about the CEBHA+ project are described elsewhere as well (9, 10). Essentially, in Rwanda, research activities of the CEBHA+ project have been implemented through the following four research tasks (RTs):
▪ Research task one (RT1): Evidence-informed policies and practices on screening approaches for hypertension and diabetes, and those at high risk of cardiovascular disease in sub-Saharan Africa.
▪ Research task two (RT2): Evidence-informed policies and practices on integrated models of healthcare delivery for hypertension and diabetes in sub-Saharan Africa.
▪ Research task three (RT3): Evidence-informed policies and practices on population level interventions to prevent hypertension and diabetes in sub-Saharan Africa.
▪ Research task four (RT4): Finding the evidence for improved implementation of road traffic injury prevention interventions.
In addition to the aforementioned four research tasks (RTs), the project has another major activity which deals with capacity building through 1) long term courses at PhD and masters levels, and 2) short courses in various research areas. Building infrastructure is also one of the components of this project (source: Full proposal of the research networks for health innovation in Sub-Saharan Africa, unpublished). Citizen science was implemented within the RT1.
In order to increase the likelihood of results uptake in Rwanda, citizen science was embedded within an IKT approach. IKT constitutes one of the key components of the CEBHA+ project, ultimately aiming to foster the uptake of results from the research studies conducted under this project (9). Practically, the IKT approach focuses on the engagement of KUs throughout the research process to co-produce research directly relevant to policy and practice change (9, 11).
Previous studies have reported that IKT is an emerging approach in research and reported a knowledge gap on the description of how an IKT is implemented (11–13). Particularly, a scoping review conducted by Logan et al. on IKT with public health policy makers recommended other researchers who apply an IKT approach to capture and report the detailed IKT activities, including steps, involved stakeholders, leaders of each activity, and how often activities take place in a view to allow a nuanced typology of different IKT models to emerge (13).
To the best of our knowledge, no other study conducted in the context of Rwanda used citizen science embedded in IKT to explore public health issues. Thus, this paper aimed to describe the citizen science implementation within the IKT approach and report its immediate outcomes within a study that sought to explore rural and urban residents’ perception and preference of communication strategies towards CVD risk in Rwanda. Ultimately, this paper provided insights to those with an interest in combining citizen science and IKT approaches in a community-led partnered research project.
Methods
Study Sites and Overall Approach
The embedding of citizen science within an IKT approach was nested within the second phase of a research study evaluating the performance of a non-laboratory CVD risk score, perception of CVD risk, and implementation of a population-based CVD risk screening and referral in Rwanda. The protocol of the qualitative study on CVD risk perception, under which citizen science was implemented, was published elsewhere (8). The protocol describes in detail how the citizen science approach was planned to explore the rural and urban residents’ perception and preference of communication strategies towards CVD risk in Rwanda, Ethiopia and Malawi. In Rwanda, the protocol was slightly changed by embedding citizen science within IKT approach. The initial protocol of citizen science implementation was designed in the way research team should engage with local community leaders and primary health care (PHC) stakeholders before implementing the study. In contrast to the initial protocol, in Rwanda the implementation of citizen science started by engaging with stakeholders at ministry of health (MoH) level during the study design (writing the protocol) stage before engaging local community leaders and primary health care (PHC) stakeholders. Afterwards, researchers and KUs co-implemented all phases of citizen science approach by which local community residents were selected and trained to volunteer in the implementation of the study, particularly during the stages of data collection and analysis, and dissemination of the findings. That’s how the citizen science was embedded within the IKT strategy.
The citizen science approach, in the present study, was implemented with deliberate engagement of KUs at different steps of study implementation. However, types of KUs engaged in each step of citizen science implementation depended on the intended objective. The citizen science approach primarily targeted beneficiaries of informed policies and practices. The latter were the residents from rural and urban communities purposively selected in the catchment areas of Cyanika health centre (Burera district, Northern province) and Kacyiru health centre (Gasabo district, City of Kigali), respectively, in Rwanda.
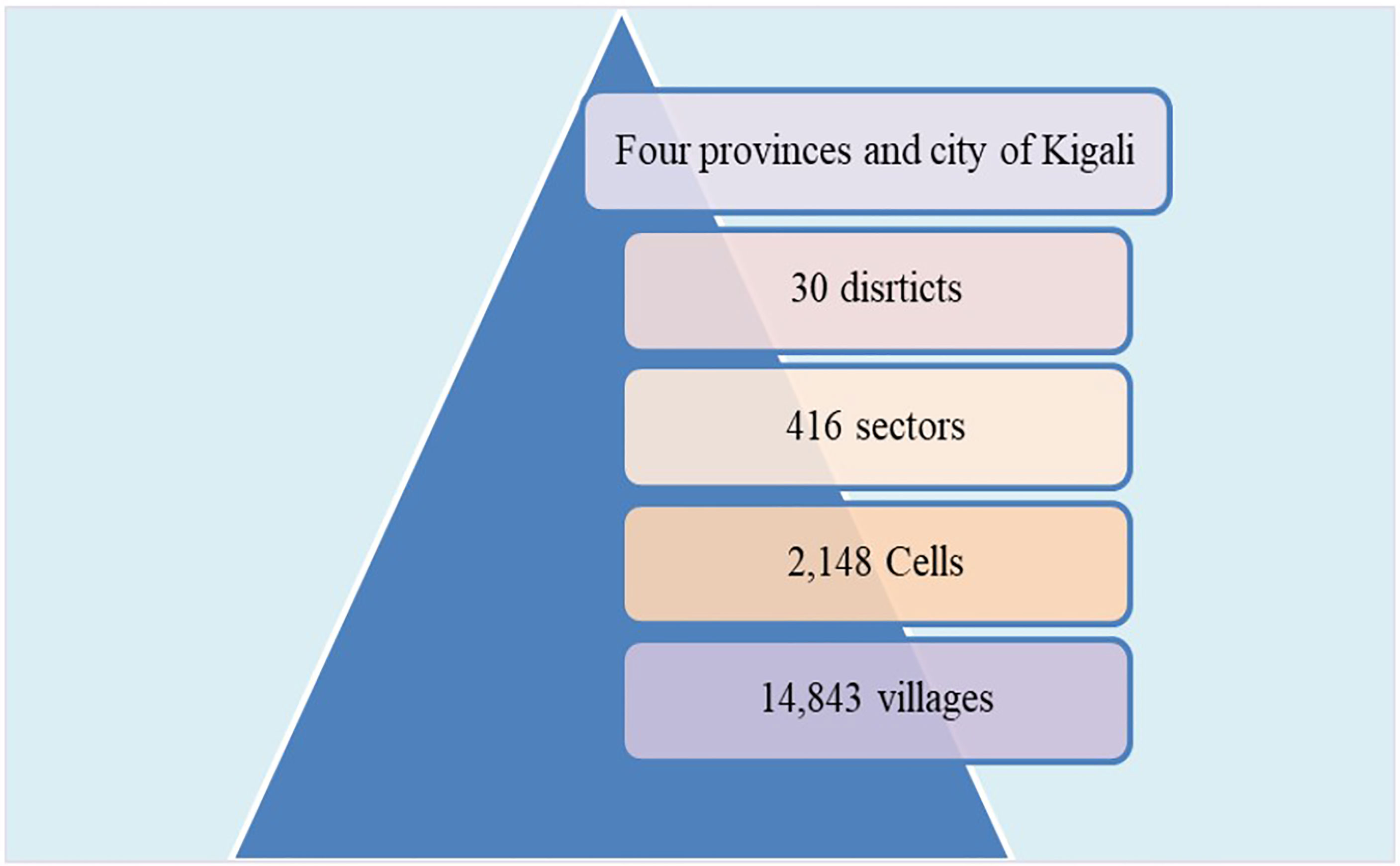
In line with the protocol of the CEBHA+ IKT approach (9), we involved decision-makers in positions that allow them to make system-level, organizational or technical decisions that affect the general health of communities or populations. We therefore engaged, at national level, staff from the Planning, Monitoring and Evaluation, and Financing Directorate General at the Rwanda MoH and staff from non-communicable diseases (NCDs) Division, CVD unit at the Rwanda Biomedical Center (RBC) which is the policy implementing agency of the Rwanda MoH. At the district level, we engaged with district health unit staff as well as staff from health centers at primary health care facilities. We also engaged with coordinators of community health workers (CHWs) at the cell level (the basic politico-administrative unit composed by villages in Rwanda). The politico-administrative units and their respective numbers in Rwanda, as described by The Ministry of Local Government (MINALOC) (14), are illustrated in the Figure 1.
Political leaders at district, sector, cell and village levels were key actors for us to engage with in order to ensure a conducive environment for the citizen science aspect of the study and ultimately to foster the uptake and advocacy of the study findings.
Data Sources and Analysis
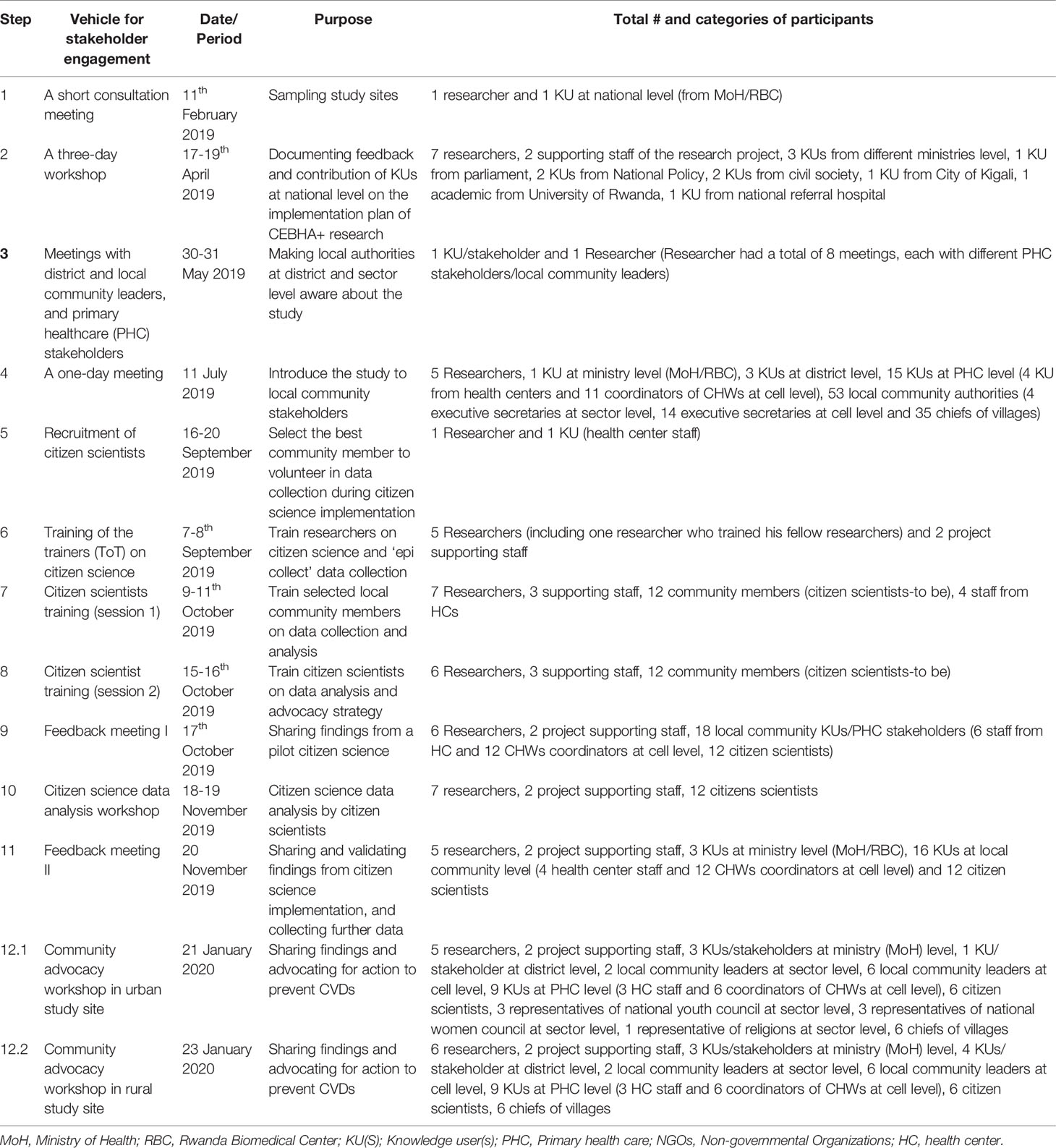
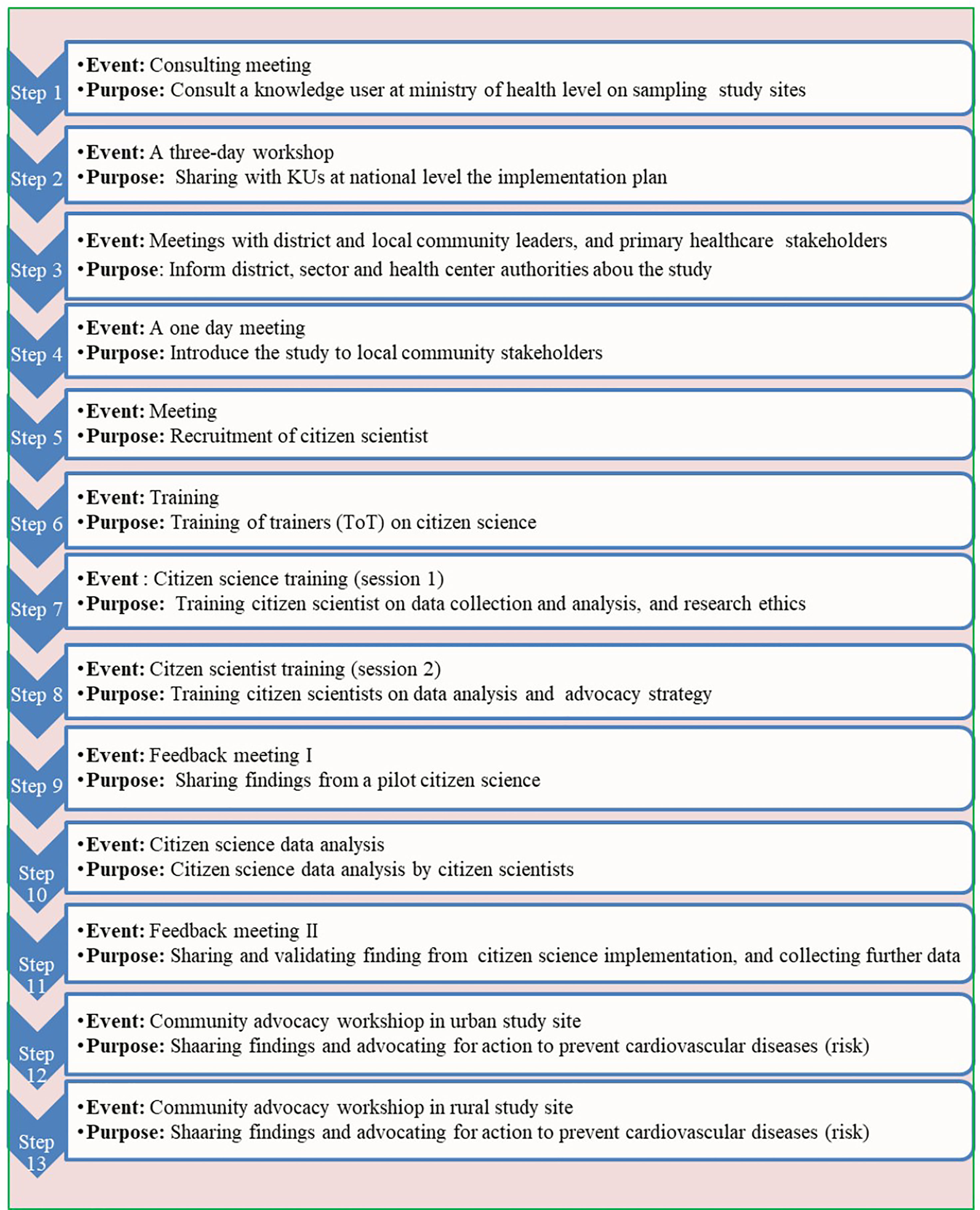
Data for this paper included minutes, reports and notes from meetings and workshops as described in the Table 1 and visualized in the Figure 2. The documents were perused to report the immediate outcomes as well as any challenges encountered during each step during citizen science implementation.
Ethical Considerations
The study was approved by the Institutional Review Board of the Rwanda Ministry of Health (MoH), known as the Rwanda National Ethics Committee (RNEC) (No.256/RNEC/2019). Citizen scientists were trained to research ethics before being deployed to their local communities to collect data from their fellow community members. Community members interviewed by citizen scientist provided written consent before interview.
Results
The presentation of the results focuses only on the components of citizen science implementation that most closely link to policymakers and advocacy. In this study, all citizen science implementation steps were conducted in collaboration with KUs at MoH level. In order to embed citizen science within IKT approach, researchers first of all engaged with KUs at MoH level, then they (researchers and KUs) collaboratively co-implemented all steps of citizen science in line with the protocol (8). The steps employed during the citizen science approach were planned in a deliberate IKT strategy and are presented in chronological order of their implementation (Table 1 and Figure 1). Each step of citizen science implementation is described in terms of dates, purpose of the step, number and categories of participants (Table 1). This paper reported the immediate outcomes of the citizen science implementation with an IKT approach. Any IKT-related challenges encountered during the implementation of citizen science approach were reported as well.
Step 1: A Short Consultation Meeting With Stakeholders at the National Level
This consultation meeting was preceded by a meeting engaging different stakeholders in relation to the CEBHA+ project in general, which was held on 8th February 2019. At this preceding meeting, all stakeholders at national level who attended were introduced to the CEBHA+ project (its goal, objectives, scopes and different research tasks). During the meeting, researchers arranged follow-up meetings with key stakeholder in charge of the CVD unit at RBC/MoH level in order to speak more in depth about the overall research under which citizen science was implemented. In this context, one researcher subsequently had a consultation meeting with one stakeholder in CVD unit at MoH/RBC level for consultation on the overall implementation of qualitative phase. This consultation meeting resulted in, on one hand, a program based outcome as the CEBHA+ research staff, together with a member of the RBC/MoH agreed on study sites and the criteria of community members who should be potential citizen scientists. On the other hand, the meeting resulted in relationship based outcomes as the member of the MoH expressed an interest to be part of the research team and committed to contribute to the protocol development and implementation.
Step 2: A Three-Day Workshop to Share the Study Protocol With KUs at National Level
This workshop was prepared in the context of sharing the implementation plans of all research activities, under different research tasks of the CEBHA+ project, with KUs/stakeholders at national level. In the context of the IKT strategy, most of stakeholders of this workshop could be considered as brokers as majority of them held technical positions in their respective institutions, and were therefore advisors to policy makers. This workshop was organized at the CEBHA+ project level, not at the level RT1 that implemented citizen science. It is in this regard that the protocol of the study, under which citizen science nested, was presented to the KUs (Table 1). The immediate outcomes of this workshop were program-based and included the in-kind contributions like facilitating data accessibility, committing technical inputs (data collection and analysis, and manuscripts writing) and promising advocacy to policy makers.
Step 3: Meetings With District and Local Community Leaders, and Primary Health Care Stakeholders (KUs at Local/Community Level)
In order to inform PHC workers and local community leaders about the CEBHA+ project, in particular the RT 1 study project under which citizen science approach was implemented, the research team organized eight individual meetings with different stakeholders at local community level (see Table 1). The aim of these meetings was to explain the study objectives and its implementation plan to local administrative (district, and sector) leaders and PHC stakeholders and to prepare a one-day meeting to introduce the study to a wide range of community leaders and PHC stakeholders. The outcomes of these one-on-one meetings were that conducive environment of data collection was created and ensured as local (district and sector level) authorities and PHC stakeholders accepted to engage their subordinates and/or local community residents into the study.
Step 4: A One-Day Meeting to Introduce the Study to Local Community Leaders and PHC Stakeholders
This meeting served the research team to introduce the study to meeting participants (Table 1), explained the citizen science approach and pre-selected candidates from the local community to volunteer in citizen science (CS) implementation (i.e. citizen scientists-to-be).This meeting was co-facilitated by five researchers and one KU from MoH/RBC. The latter has played an active role in the CS implementation as he contributed in the protocol writing and co-presented the protocol to the ethics committee for ethical clearance. In this meeting, he co-facilitated the meeting by making the presentation on the burden of CVDs and other NCDs in Rwanda. Moreover, he also assisted in providing some clarifications of some aspects of the study protocol implementation when the meeting participants expressed a need for this. The immediate outcomes of this meeting included (i) commitment from leaders of villages to sensitize local community residents about the study, (ii) leaders of villages and CHWs coordinators helped to pre-select/identify potential citizen scientists, and (iii) commitment from local community leaders (executive secretaries at sector and cell levels, and leaders of villages) to collaborate with researchers during the implementation of the study.
Step 5: Recruitment of Citizen Scientists
In each study site, one researcher and one KU at PHC level (one staff from health center) worked together to recruit community members and request them to voluntarily participated into the study as citizen scientists-to be. During the step 4, described earlier, four to six community members were proposed per one village out of six villages sampled in this study per each study site. During the recruitment, one of the two candidates that were eventually selected at each village was considered as a primary contact and the second as a backup in case the first was unavailable at the time of training. The immediate outcome was the shared ownership between researchers and PHC stakeholders on the subsequent steps of CS implementation.
Step 6: Training of the Trainers (ToT) on Citizen Science
Four project researchers were trained by one of researchers (JKO) with previous experience and training in conducting citizen science approaches.
Step 7: Citizen Scientists Training (Session 1)
Seven researchers (SR, BMC, SN, JPN, GU, JKO and JBN) collaboratively trained 12 community members on collecting data (audio narratives and pictures) with the Epicollect5 Mobile app (http://five.epicollect.net), analyzing data using pre-designed template, and on research ethics. Staff from two HCs sampled from this study attended the training. After the training, citizen scientists conducted a pilot test of citizen science by going back to their respective villages to collect data from two of their fellow community members. As an immediate outcome of this step, the training objectives were met, and health center staff got an understanding on citizen science implementation and committed to co-coordinate and co-supervise the data collection phase as assigned.
Step 8: Citizen Scientists Training (Session 2)
After the pilot data collection (as mentioned in the step 7) was completed, a second session was organized to help citizen scientists to practice data analysis using their previously collected data. CEBHA+ researchers oversaw citizen scientists during data analysis but did not interfere with analysis. To ensure quality of the data analysis, citizen scientists from each study site were split into two groups, and they were tasked to analyze the same data collected in their local community. Once two groups completed data analysis, they met to agree each other on their data analysis outputs and they consulted project researchers for any discrepancies. At the end of this training, the ability of community members to analyze qualitative data (narratives and photos) was reassured.
Step 9: Feedback Meeting One
After the analysis of pilot data, in the presence of the research team and national stakeholders, the citizen scientists presented findings to PHC stakeholders (Table 1) for results validation and further opportunities for data collection. The immediate outcomes included the validation of findings, particularly the ones related to local community perception and preferred communication strategies towards CVD risk.
Step 10: Citizen Science Data Analysis Workshop
After the pilot study, citizen scientists proceeded to collect qualitative data (pictures and audio narratives), using Epicollect5 Mobile app, from their fellow community members. Once this phase was completed, a two-day workshop for data analysis followed. Meeting outcomes: Attendees identified some health issues exposing their community to CVD (risk) which could be solved by community members themselves or KUs at local community level within their means, like initiating physical activity at community level, constructing kitchen garden among others.
Step 11: Feedback Meeting Two
Immediately after the citizen science data analysis workshop, the second feedback meeting was organized for citizen scientists to present the study findings to the PHC stakeholders (KUs at community level) for validation. The meeting also presented an opportunity for further data collection. Thus, the meeting was also an opportunity of knowledge co-creation between researchers, PHC stakeholders and local community members. The first immediate outcome was PHC stakeholders at the community level committing to solve some local community health issues which they felt they were able to address: this included fighting against locally made substandard beverages and those from neighboring countries, increasing kitchen gardens, teaching local residents about CVD (risk). The second immediate outcome is that PHC stakeholders helped identify relevant community opinion leaders and political leaders to be invited in the community advocacy workshop (CAW).
Step 12: Community Advocacy Workshops
Two separate one-day community advocacy workshops (CAWs) were conducted with the aim to share the findings from citizen science implementation with local community (district, sector and cell levels) authorities and PHC stakeholders at both the rural and urban study site. At each site, one citizen scientist selected by his/her fellow citizen scientists presented the findings and advocated for pertinent action. The CAWs were opportunities for health advocacy campaigns and called upon local community authorities to take action to solve health issues – particularly those that require either community social and behavior change or enforcement of laws at community level and do not have any financial implications. Other forms of advocacy and appeal (such as issue briefs for key decision makers) have been planned by the CEBHA+ team to be developed and disseminated in the later stages of the CEBHA+ project implementation.
Step 12.1. Community Advocacy Workshop in Urban Study Site
Table 1 displays categories of stakeholders who attended the CAW in urban study site. There were several immediate outcomes: District officials requested researchers to assist in designing strategies to solve health issues like the issue of lack of knowledge on CVDs as identified by citizen scientists. Local authorities expressed a need to share with CHWs the findings from the citizen science so that they could help in sensitizing local community to fight against CVD (risk). In addition to this, citizen scientists committed to work with villages leaders to initiate some healthy practices such as organizing physical activity at village level, sensitizing their fellow community members on preparation of healthy diet from locally available food items and sensitizing them to contribute on the repairing sewage system.
Step 12.2. Community Advocacy Workshop in Rural Study Site
This CAW in the rural study site was organized and facilitated in the same way as in urban study site and list of CAW participants is provided in the Table 1. The immediate outcomes included local community leaders committed to initiate some CVD prevention interventions (such as physical activities) and citizen scientists committed to keep on collaborating with local authorities and PHC stakeholders to sensitize the community to adopt healthy practices preventing CVD (risk). Some participants committed to actions to solve health issues included fighting against locally made substandard beverages and those from neighboring countries, increasing kitchen gardens, teaching local residents on CVD (risk factors).
Main Challenges of the Citizen Science Implemented Within an IKT Approach
The implementation of the citizen science approach consisted of 13 steps (table 1). Most of the time researchers and KUs at MoH level collaboratively planned all events (meetings/workshops) and agreed each other on the date and the venue. However, due to competing priorities, KUs at MoH/RBC were not able to participate in four out of 12 events (steps/phases) they were invited to participate in. At the urban study site, some local authorities promised to attend CAW but they were not able to attend with apologies of having being invited in unforeseen and unpredicted events, and they delegated one of their staff at district level to represent them.
Due to the COVID-19 pandemic, researchers were not able to organise follow up meetings or evaluate the long term outcomes of the citizen science implemented within IKT approach.
Discussion
This paper aimed to describe the steps and the immediate outcomes of the citizen science approach that was embedded within the IKT approach of the CEBHA+ project in Rwanda. The citizen science approach was linked to a study that aimed to explore the rural and urban dwellers’ perceptions and preferences of communication strategies towards CVD risk in Rwanda. Its results will be published in a separate paper. A range of KUs involved in the implementation of the citizen science included policy makers at high/national level (i.e. ministerial and district levels), health care providers (health center level), CHWs, security organs (national police), local community leaders and other local community opinion leaders. The representatives of social groups (women, youth) and faith-based organizations were involved as community opinion leaders. Overall, partnership between CEBHA+ researchers, KUs (at high/national level and district level), PHC stakeholders and local community leaders was encouraging and positive relationships were forged and fostered through both CBPR/citizen science and IKT approaches.
The implementation of citizen science embedded within IKT resulted in immediate outcomes which can be characterized into two categories. The first category can be termed ‘relationship-based immediate outcomes’ which were expressed when KUs at RBC/MoH level accepted to collaborate with CEBHA+ researchers on the research design and its implementation. The relationship-based immediate outcomes were also recorded when HC accepted to co-supervise or coordinate citizen science data collection and they contributed in the recruitment of citizen scientists selected from their catchment area. The approach therefore represents an opportunity for local health facilities to study a given health issue in the community. The second category was termed as ‘project-based immediate outcomes’ and included active participation of KUs and citizen scientists. The implementation of this citizen science and IKT approach faced some challenges like infrequent attendance and absenteeism of KUs in some research activities because of competing priorities.
IKT approach was applied by involving decision makers or KUs at PHC level (CHWs and health centers staff), district health unit staff and MoH/RBC level. This conforms to the way Nguyen et al. described KUs, in the IKT lens, as health care providers along health care services delivery system to administrators to ministers of health (15). The implementation of citizen science started by first of all engaging with KUs, this was the act of embedding citizen science approach within IKT approach, and could be conceptualized as ‘the embeddedness’ of the two above collaborative research approaches. The benefit of engaging with KUs before starting citizen science implementation aimed to enhance the potential for evidence uptake. This strategy is consistent with recommendations in the literature (16). Citizen science embedded within an IKT approach helped facilitate macro and micro-level knowledge partnership between researchers and KUs (i.e practitioners, policy makers and local community members). This complies with the global burgeoning principle that research should go beyond the focus on the ‘know-do-gap’ (17), by pushing evidence across and investing in partnership to co-produce knowledge.
The successful and continuous partnerships between researchers and KUs undoubtedly were a result of the in-person contacts, through meetings and workshops. This is in line with a previous study that reported that the in-person contact is an influential factor determining the involvement of KUs in research process and their use of research evidence (12). The meetings and workshops (i.e. presentations, trainings) were the common forms of interactions between researchers, KUs and local community leaders (12). The momentum of the continuing partnerships of the researchers and KUs was fundamentally sustained by the existing core principle of the CEBHA+ project to use IKT strategies in order to foster the uptake of research findings (9). Furthermore, budget for stakeholder engagement activities was taken into considerations in the project design phase. One of the CEBHA+ sites, South Africa, stable and supportive funding was recognized among constructs favouring the implementation of IKT processes and strategies (18). This also underpins how allocating financial resources is paramount for applying IKT approach in research process (11). Funds dedicated to IKT activities were also reported among the enablers for IKT approach (12, 19–21). This implies that budget allocation should include IKT activities during the collaborative research design phase. Commitment of KUs to be part of the team of investigators and contribute to the implementation of the study was reported as an immediate outcome in the present study, and was also reported in a scoping review conducted by Logan et al. on IKT with public health policy makers (22). The positive impact on relationship between KUs and researchers during research coproduction was already opinioned by other researchers (23).
In the present study, local community members represented by citizen scientists were involved in data collection and analysis, and dissemination of the results through CAWs. However, for a standard CBPR/citizen science, Jull et al. suggested to involve community members in every stage of the research process from issue identification to writing and dissemination through framing research questions, research design, data collection and analysis (1). The stages of issue identification and crafting of research questions were completed by researchers themselves without involvement of community members by referring to the existing literature. In contrast to the results of the study conducted by Gagliardi et al. who reported that KUs are most often involved in conceptualizing research and disseminating or implementing the findings (12), in our study key KUs were involved in all steps of the study, however sometimes KUs were not able to attend some meetings or workshops because of competing priorities. This infrequent attendance of KUs in IKT activities and events (meetings or workshops) were reported by other studies (11, 12). Other researchers reported the difficulties to reconcile the stakeholder agendas while implementing a collaborative researchers (23).
During the process of applying citizen science and IKT approaches together, citizen scientists committed to work with PHC stakeholders and local community leaders to solve issues which they felt could be addressed by local communities. In the rural area, committed actions included fighting against locally made substandard beverages and those from neighboring countries, increasing kitchen gardens, teaching local residents about CVD (risk). At the urban study site, committed actions included organizing physical activity at village level, sensitizing fellow community members on preparation of healthy diet from locally available food items and sensitizing them to contribute on the repairing sewage system. This is in agreement with Leon et al. who found that communities can be trained to advocate for what they need, to do what works and what is relevant (24). It is also in line with another study which reported that benefits of citizen science included community development, empowerment, and changes of attitudes, values and norms, action to solve issues and engagement in policy making (1, 15). This community involvement in research can also empower users of health services (i.e. citizens) the capacity to influence change and improvement in issues that affect most people lives (25). Having local community members suggesting solutions to solve their own problems in the present study proved the relevance of citizen engagement, IKT and local evidence-informed solutions, thereby responding to the existing dearth of evidence relevant to African health systems contexts as claimed by some scholars (26, 27).
Limitations and Strengths
Due to Covid-19 impact, researchers were not able to evaluate the impact of using citizen science and IKT approaches. This evaluation would have targeted the long term outcomes related to co-created solutions/commitments to prevent CVD (risk factors) as pledged by citizen scientists and local community local leaders during the feedback sessions and CAWs. However, this paper reported the immediate outcomes in detail and provided a thorough description how KUs and community members were involved throughout the research trajectory. The steps to apply citizen science embedded within IKT approach, as used in this study, might be adapted in other contexts for research projects aiming to foster the uptake of research evidence for KUs and the involvement of community members in solving the issues putting them at health risk.
Even though, due to Covid-19 containment measures we were not able to evaluate the impact of the implementation of citizen science embedded within IKT approach, immediate results indicated that this approach would be impactful. This was proved during different meetings and workshops when citizen scientists presented findings to PHC stakeholders, local community leaders and community opinion leaders who agreed what presented by citizen scientists and appreciated their work. In addition to this, citizen scientists themselves and local community leaders committed to solve health issues they felt they were in their control, with local community means. Therefore, the citizen science approach embedded within an IKT is recommended to research projects intending to collaborate with knowledge users with a view to explore lay knowledge on diseases (like NCDs) or any other health issues for which local community residents could collaborate with KUs and local community leaders to solve them. The combinations of two knowledge co-creation approaches (citizen science and IKT) are recommended in the context of low-and middle-income countries where NCDs are emerging as an additional burden to existing burden of communicable diseases and most of the populations do not have knowledge on most NCDs. This recommendation is in line with other researchers who proved difficult to align themselves with a single collaborative research approach and suggested to combine approaches or some of their respective elements (15).
Conclusion
Knowledge co-creation approaches are emerging in health care and public health systems. To the best of our knowledge, citizen science/CBPR and IKT approaches were used simultaneously in Rwanda for the very first time during our study exploring rural and urban community residents perceptions and preferred communication strategies towards CVD (risk) in Rwanda. Thus, other researchers may adapt the steps of implementing CBPR and IKT approaches, as described, in similar research projects. Citizen science proved to be an important strategy for research co-production in Rwanda. While this strategy falls within the remit of a larger IKT approach it focuses on the role and ownership of research by local community residents. This study demonstrated that to improve the relevance and impact of research in local community a deliberate IKT approach that incorporates citizen science can be invaluable. However, further studies are needed to provide insights on the impact or long term outcomes resulting from the implementation of citizen science embedded within an IKT approach.
Data Availability Statement
The data for this paper included minutes, reports and notes from meetings and workshops held during the processes of implementation. These reports are available from the corresponding author (JBN at amVhbmJlcmNobWFuc25peWliaXppQHlhaG9vLmZy), and the project coordinator / co-author (SN at bnRhd3VzZWxlbWFuQG51cnNwaC5vcmc=) on reasonable request.
Ethics Statement
The studies involving human participants were reviewed and approved by Rwanda National Ethics Committee. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JBN was the lead author, contributed to the study conceptualization and methodology, coordinated the research implementation, contributed to the devise of the conceptual ideas for the current manuscript and drafted the initial manuscript. SN, SR, DT, and EN contributed to the study conceptualization and methodology, contributed to the coordination of the research implementation and to the devise of the conceptual ideas for the current manuscript and revised it for scientific insight. JPN contributed to the coordination of the research implementation and to the devise of the conceptual ideas for the current manuscript and revised it for scientific insight. GU and AN contributed to the coordination of the research implementation and revised the manuscript for scientific insight. NJ contributed to conceptualizing the manuscript and revised it for scientific insight, and served as senior advisor on the conceptualization of the manuscript, the drafting as well as the finalization of the manuscript. KO contributed to the study conceptualization, methodology, research implementation and revised the manuscript for scientific insight. NL contributed to the study conceptualization, methodology and revised the manuscript for scientific insight. CB contributed to the study conceptualization, methodology, research implementation, initial manuscript drafting and provided insight in the revised manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the German Federal Ministry of Education and Research (BMBF) as part of the Research Networks for Health Innovations in sub-Saharan Africa Funding Initiative through Collaboration for Evidence-based Healthcare and Public Health in Africa (CEBHA+) project (Number: 66.3010.7-002.09).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are thankful to the staff from Kacyiru and Cyanika HCs for their contribution in the recruitment of citizen scientists and the coordination of data collection. We would like to also express our gratitude to local community members, from Kacyiru and Cyanika HCs, who volunteered to contribute in this study. We also expressed our gratitude to Mr. Theoneste Seminali for his ICT support during the research implementation. Last but not least, we thank Ms. Nadine Mukahirwa for her contribution in organizing the logistics of the events held during the research implementation.
References
1. Jull J, Giles A, Graham ID. Community-Based Participatory Research and Integrated Knowledge Translation: Advancing the Co-Creation of Knowledge. Implement Sci (2017) 12(1):1–9. doi: 10.1186/s13012-017-0696-3
2. Springer MV, Skolarus LE. Community-Based Participatory Research: Partnering With Communities. Int Sect Early Career Train (2019) 50(3):E48–50. doi: 10.1161/STROKEAHA.118.024241
3. Den Broeder L, Devilee J, Van Oers H, Schuit AJ, Wagemakers A. Citizen Science for Public Health. Health Promot Int (2018) 33(3):505–14. doi: 10.1093/heapro/daw086
4. Horowitz CR, Robinson M, Seifer S. Community-Based Participatory Research From the Margin to the Mainstream are Researchers Prepared? Circulation (2009) 119:2633–42. doi: 10.1161/CIRCULATIONAHA.107.729863
6. Kothari A, Wathen CN. A Critical Second Look at Integrated Knowledge Translation. Health Policy (New York) (2013) 109(2):187–91. doi: 10.1016/j.healthpol.2012.11.004
7. Kothari A, McCutcheon C, Graham ID. Defining Integrated Knowledge Translation and Moving Forward: A Response to Recent Commentaries. Int J Heal Policy Manag (2017) 6(5):299–300. doi: 10.15171/ijhpm.2017.15
8. Okop KJ, Murphy K, Lambert EV, Kedir K, Getachew H, Howe R, et al. Community-Driven Citizen Science Approach to Explore Cardiovascular Disease Risk Perception, and Develop Prevention Advocacy Strategies in Sub-Saharan Africa: A Programme Protocol. Res Involv Engagem (2021) 7(1):1–14. doi: 10.1186/s40900-020-00246-x
9. Pfadenhauer LM, Grath T, Delobelle P, Jessani N, Meerpohl JJ, Rohwer A, et al. Mixed Method Evaluation of the CEBHA+ Integrated Knowledge Translation Approach: A Protocol. Heal Res Policy Syst (2021) 19(1):1–12. doi: 10.1186/s12961-020-00675-w
10. Rehfuess EA, Durão S, Kyamanywa P, Meerpohl JJ, Young T, Rohwer A. An Approach for Setting Evidence-Based and Stakeholder-Informed Research Priorities in Low- and Middle-Income Countries. Policy Pract (2016) 94(4):297–305. doi: 10.2471/BLT.15.162966
11. McIsaac JLD, Penney TL, Storey KE, Sigfridson L, Cunningham J, Kuhle S, et al. Integrated Knowledge Translation in Population Health Intervention Research: A Case Study of Implementation and Outcomes From a School-Based Project. Heal Res Policy Syst (2018) 16(1):1–10. doi: 10.1186/s12961-018-0351-8
12. Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated Knowledge Translation (IKT) in Health Care: A Scoping Review. Implement Sci (2016) 11(1):1–12. doi: 10.1186/s13012-016-0399-1
13. Gagliardi AR, Dobrow MJ. Identifying the Conditions Needed for Integrated Knowledge Translation (IKT) in Health Care Organizations: Qualitative Interviews With Researchers and Research Users. BMC Health Serv Res (2016) 16(1):1–9. doi: 10.1186/s12913-016-1533-0
14. MINALOC. The Local Government System in Rwanda Country Profile 2017–18 (2018). Available at: http://www.clgf.org.uk/default/assets/File/Country_profiles/Rwanda.pdf. 2018.
15. Nguyen T, Graham ID, Mrklas KJ, Bowen S, Cargo M, Estabrooks CA, et al. How Does Integrated Knowledge Translation (IKT) Compare to Other Collaborative Research Approaches to Generating and Translating Knowledge? Learning from experts in the field. Heal Res Policy Syst (2020) 18(1):1–20. doi: 10.1186/s12961-020-0539-6
16. Glegg SMN, Jenkins E, Kothari A. How the Study of Networks Informs Knowledge Translation and Implementation: A Scoping Review. Implement Sci (2019) 14(1):1–27. doi: 10.1186/s13012-019-0879-1
17. Greenhalgh T, Sietsewieringa S. Is it Time to Drop the “Knowledge Translation” Metaphor? A Critical Literature Review. J R Soc Med (2011) 104(12):501–9. doi: 10.1258/jrsm.2011.110285
18. Jessani NS, Rohwer A, Schmidt BM, Delobelle P. Integrated Knowledge Translation to Advance Noncommunicable Disease Policy and Practice in South Africa: Application of the Exploration, Preparation, Implementation, and Sustainment (EPIS) Framework. Heal Res Policy Syst (2021) 19(1):1–15. doi: 10.1186/s12961-021-00733-x
19. Berman J, Mitambo C, Matanje-Mwagomba B, Khan S, Kachimanga C, Wroe E, et al. Building a Knowledge Translation Platform in Malawi to Support Evidence-Informed Health Policy. Heal Res Policy Syst (2015) 13(1):1–5. doi: 10.1186/s12961-015-0061-4
20. Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A Systematic Review of Barriers to and Facilitators of the Use of Evidence by Policymakers. BMC Health Serv Res (2014) 14:2. doi: 10.1186/1472-6963-14-2
21. Oliver K, Kothari A, Mays N. The Dark Side of Coproduction: Do the Costs Outweigh the Benefits for Health Research? Heal Res Policy Syst (2019) 17(1):1–10. doi: 10.1186/s12961-019-0432-3
22. Leon AC, Davis LL, Kraemer HC. The Role and Interpretation of Pilot Studies in Clinical Research. J Psychiatr Res (2011) 45(5):626–9. doi: 10.1016/j.jpsychires.2010.10.008
23. Beckett K, Farr M, Kothari A, Wye L, Le May A. Embracing Complexity and Uncertainty to Create Impact: Exploring the Processes and Transformative Potential of Co-Produced Research Through Development of a Social Impact Model. Heal Res Policy Syst (2018) 16(1):1–18. doi: 10.1186/s12961-018-0375-0
24. Logan ML, Bishop A CJ. Integrated Knowledge Translation With Public Health Policy Makers : A Scoping Review. Healthc Policy (2019) 14(3):55–77. doi: 10.12927/hcpol.2019.25792
25. Helen Hayes SB, INVOLVE MT. Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research. INVOLVE, Eastleigh [Internet]. Natl Institute Health Res (2012).
26. Edwards A, Zweigenthal V, Olivier J. Evidence Map of Knowledge Translation Strategies, Outcomes, Facilitators and Barriers in African Health Systems. Heal Res Policy Syst (2019) 17(1):1–14. doi: 10.1186/s12961-019-0419-0
Keywords: citizen science, integrated knowledge translation, knowledge users, cardiovascular disease, Rwanda
Citation: Niyibizi JB, Nganabashaka JP, Ntawuyirushintege S, Tumusiime D, Umwali G, Rulisa S, Nyandwi A, Okop KJ, Ntaganda E, Sell K, Levitt N, Jessani NS and Bavuma CM (2021) Using Citizen Science Within an Integrated Knowledge Translation (IKT) Approach to Explore Cardiovascular Disease Risk Perception in Rwanda. Front. Trop. Dis 2:752357. doi: 10.3389/fitd.2021.752357
Received: 02 August 2021; Accepted: 27 September 2021;
Published: 13 October 2021.
Edited by:
Yodi Mahendradhata, Gadjah Mada University, IndonesiaReviewed by:
I Wayan Gede Artawan Eka Putra, Udayana University, IndonesiaPaulina Carmona-Mora, University of California, Davis, United States
Copyright © 2021 Niyibizi, Nganabashaka, Ntawuyirushintege, Tumusiime, Umwali, Rulisa, Nyandwi, Okop, Ntaganda, Sell, Levitt, Jessani and Bavuma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jean Berchmans Niyibizi, amVhbmJlcmNobWFuc25peWliaXppQHlhaG9vLmZy
†These authors share senior authorship
 Jean Berchmans Niyibizi
Jean Berchmans Niyibizi Jean Pierre Nganabashaka
Jean Pierre Nganabashaka Seleman Ntawuyirushintege1
Seleman Ntawuyirushintege1 David Tumusiime
David Tumusiime Ghislaine Umwali
Ghislaine Umwali Stephen Rulisa
Stephen Rulisa Alypio Nyandwi
Alypio Nyandwi Kufre Joseph Okop
Kufre Joseph Okop Naomi Levitt
Naomi Levitt Nasreen S. Jessani
Nasreen S. Jessani