- 1Department of Epidemology, Hawassa University, Hawassa, Ethiopia
- 2Department of Anesthesia, Arsi University, Asella, Ethiopia
Background: The malaria control strategy has shown an improvement in providing services and allocating resources to enhance malaria elimination. The world malaria report indicated that there was a marked increment of insecticide treated net (ITNs) utilization among pregnant women. However, in Ethiopia, the number of households with possession and utilization of ITNs is still far behind the WHO recommendations. Hence, this study was aimed to measure the magnitude of ITN utilization and to identify factors associated with its utilization among pregnant women from April 4, 2021 to April 15, 2021 in Sodo Zuria Woreda, in Wolaita Zone, Southern Ethiopia.
Methods: A community based cross-sectional study was employed. Data were collected using interviewer administered pretested, structured questionnaires. Simple random sampling method was used to select 459 pregnant women. Data were entered into Epi Info version 7 and then exported to statistical package for the social sciences for further analysis. We used time period for data collection of current study. Binary’s logistic regression was used to determine factors affecting insecticides treated net (ITN) utilization. Adjusted Odd Ratios (OR) with 95% CI was used to measures the strengths of associations.
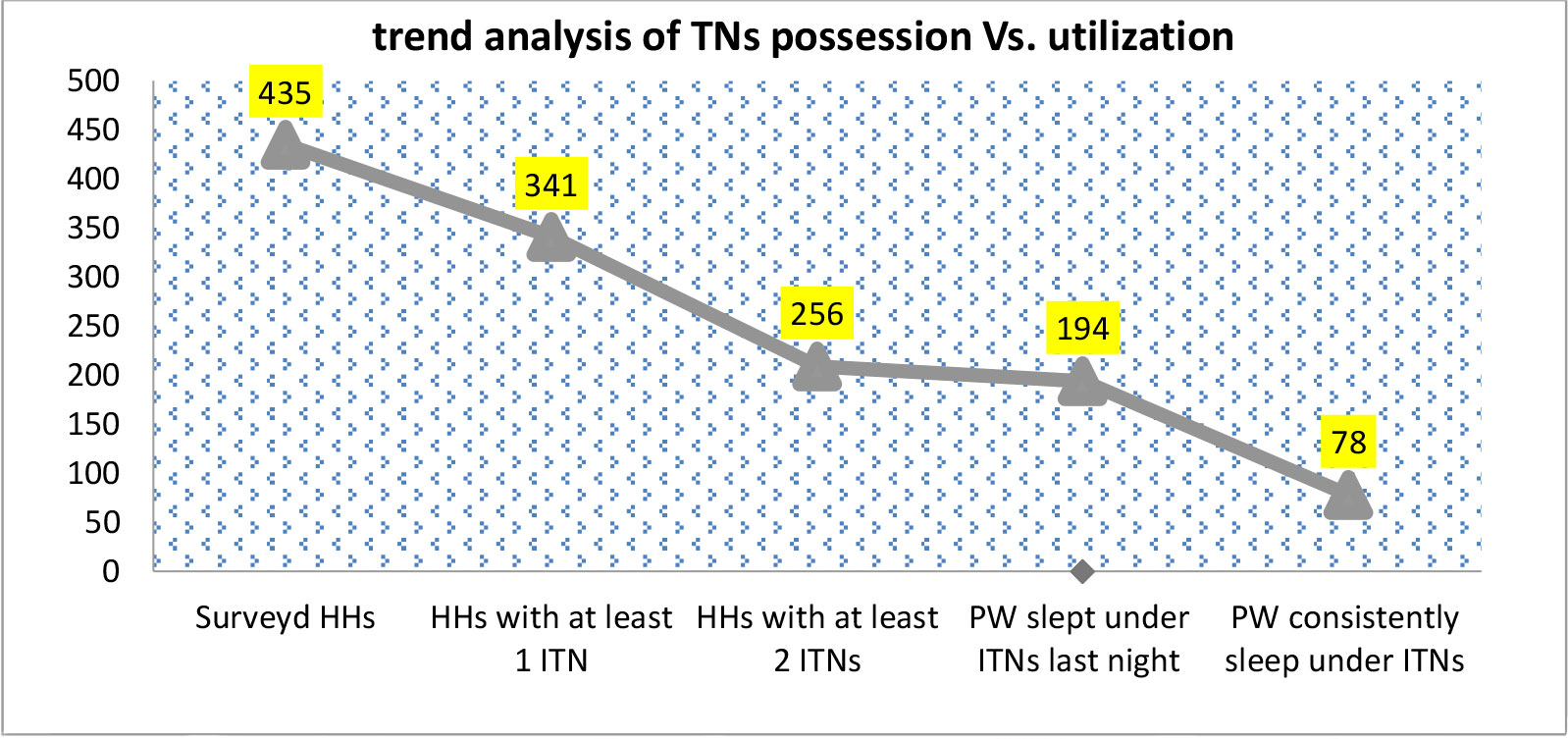
Results: Of 435 surveyed households with pregnant women, 341(78.39%) with 95% Confidence Interval (CI) (74.5%, 82.3%) possessed at least one insecticide treated net. Among them, 194(56.89%) with 95% CI (51.6%, 61.7%) interviewees had self-reported as they slept under insecticide treated net on the night preceding the data collection day. Utilization of insecticide treated nets by other family members, AOR: 6.615(95% CI: 3.358, 13.032), knowledge that the use of insecticide treated nets can prevent malaria, AOR: 3.221(95% CI: 1.737, 5.974), sleeping under insecticide treated nets, AOR: 3.726(95% CI: 1.974, 7.034), and attending ANC follow up visits, AOR: 1.956(95% CI: 1.097), were found to be significantly associated factors with pregnant women’s insecticide treated net utilization.
Conclusion: The number of households with pregnant women who had possession and utilization of ITNs was much lower than the recommendations set by WHO. Therefore, information dissemination to malaria high risk groups about insecticide treated net utilization and replacement of worn-out insecticide treated nets should be emphasized.
Background
In Ethiopia, malaria is a leading public health problem where approximately 68% of the population lives in malarious areas and three fourth of the total land mass is regarded as malarious (1). Malaria infection takes a heavy toll among pregnant women and young children (2). It is estimated that each year about 25 million pregnant women in sub-Saharan Africa (SSA) live at risk of malaria infection. Malaria infection during pregnancy carries substantial risks for pregnant woman, her fetus and the newborn child. It is frequently associated with the development of anemia, and complications like low birth weight and trans-placental parasitemia (3). Malaria transmission in Ethiopia is periodic, lasting for about three months usually from September to November (4).
The malaria control strategy has shown a progressive improvement to eliminate malaria through providing services and allocating resources (3). The two core globally accepted vector control interventions are long lasting insecticide treated net (LLITNs) and indoor residual spraying (IRS). The other ways of controlling malaria transmissions are keeping environmental hygiene and applying larvicides in mosquito breeding site (3). Ethiopia has been implementing national malaria strategic plans (NMSPs) phase III aiming to meet the ambitious goal of eliminating malaria in 50 districts by 2020 and entirely by 2030 (5)
The 2015 Ethiopian National Malaria Indicator (MIS) revealed that 65% of country’s districts were malarious, and 53% had a risk of moderate to high transmission (6). However, according to malaria epidemiological and interventional study in Ethiopia, the nation-wide ITN ownership has been relatively low. In Ethiopia, the ITN ownership was 65% in 2007, 55% in 2011, and 64% in 2015. The National malaria indicator survey of 2015 also revealed that, the household level coverage of ITNs was 64% (7).
The Federal Ministry of Health (FMoH) of Ethiopia widely introduced LLITNs as a method of malaria prevention strategy targeting all age groups residing areas below 2000 meter altitude (4). However, utilization of ITN shows significant variations among region, residency, and house hold income (5). According to Ethiopia national MIS of 2016, ITN utilization is the highest among women living in urban areas and in the households with highest wealth quintiles. The survey also revealed that ITNs utilization is the highest in Afar and Amhara, lowest in Harari and Dire Dawa (8).
To best of our knowledge there was no previous study on ITNs utilization and factors affecting its utilization among pregnant women in study area. Therefore, the findings of study will be helpful for policy makers and the partners to recommend and redesign appropriate vector control interventions or used to improve ITNs utilization
Methods and materials
Study setting and period
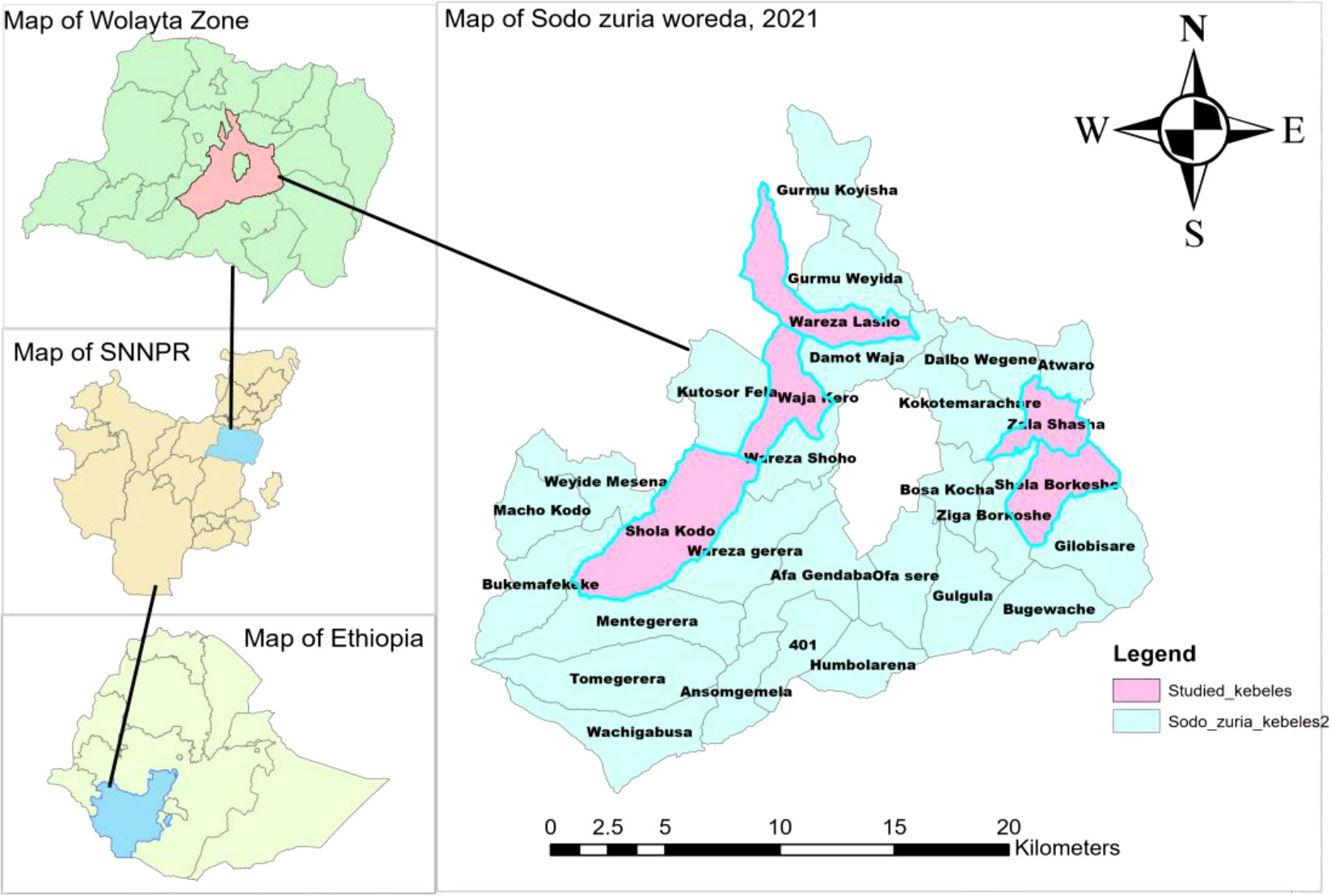
This community based cross sectional study was conducted in Sodo Zuria Woreda of Wolaita Zone, Southern Ethiopia from April 4, 2021 to April 15, 2021. Sodo Zuria Woreda is one of 16 rural Woredas and 6 town administrations in Wolaita zone. The administrative seat of Sodo Zuria Woreda is Sodo town, which is located 383 km far from Addis Ababa (the capital city of Ethiopia),. Administratively, Sodo Zuria Woreda is divided in to 25 kebeles (five urban kebeles and twenty rural kebeles)(Figure 1). This study covered six rural kebeles (Shola Kodo, Kodo Gawulia, Waja Shoya, Waraza Lasho, Zala Shasha, and Shella Borkoshe) out of 20 rural kebeles in Sodo Zuria Woreda.
Sodo Zuria Woreda is located at an altitude between 1500 meters at Tando village in Zala Shasha kebele and 2,950 meters at tip of mount Damot above sea level. The Woreda has 21 degree cilices annual temperature on average, maximum of 28 degree cilices and minimum of 18 degree cilices. In addition, the study area has average annual rain fall of 800 mm and it ranges from maximum of 1,300 mm and minimum of 600 mm. Major rainy season start from June and extend to October. Water bodies such as streams and rivers commonly exist in all kebeles of the Woreda. There are also small scale irrigation canals which surround five kebeles of the district. Around 84 permanent mosquito breeding sites were identified in the district which covers 5.04 KM2 areas.
NB: Waja Shoya kebele was separated from Waja Kero Kebele and Kodo Gawulia kebele was separated from Shola Kodo kebele. So these newly structured kebeles are not available in shape file.
Study design
A community based cross-sectional study supplemented with observation of current physical status of ITNs, caring practices done by the owners of ITNs (mending if torn, washing of ITNs, proper hanging of ITNs over sleeping spaces, and the like) was employed
Source Population
All pregnant women residences of rural kebeles of Sodo Zuria Woreda were source population of the study.
Study population
All pregnant women who were systematically selected from study households of Sodo Zuria Woreda.
Inclusion criteria
Pregnant women who resided for six months or more prior to data collection period in rural kebeles of Sodo Zuria Woreda and registered by rural HEWs of study area for identification of pregnant women for ANC follow up and other obstetric services were included in the study.
Exclusion criteria
Pregnant women who are severely sick and mentally ill during data collection period were excluded from the study.
Sample size determination and sampling technique
The sample size for the first objective was calculated using single population proportion formula with the following assumptions using EPI info version 7. The proportion of ITNs utilization among pregnant women in the previous night of data collection date was 72.5% (i.e., P = 0.725), taken from study conducted at Damot Pulasa district, Wolaita Zone, Southern Ethiopia, 95% confidence interval, 5% margin of error, design effect of 1.5, power of 80% (9) (Table 1).
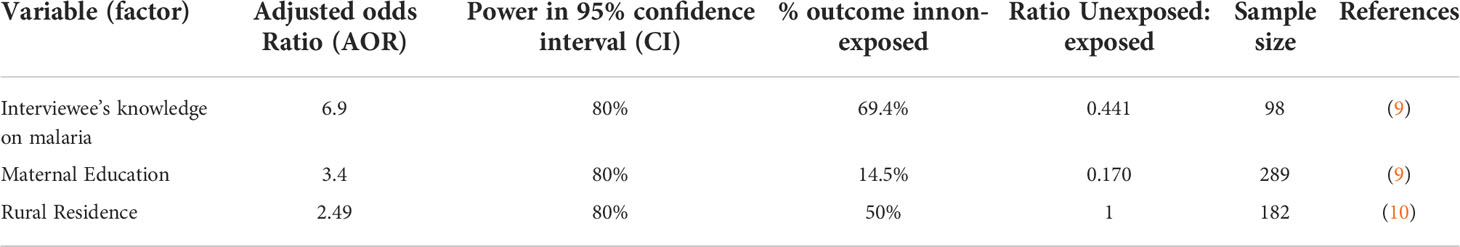
Table 1 Sample size calculation for the utilization of insecticide treated nets and associated factor among pregnant women, 2021.
The calculated sample size is 306.
Since, the sample size calculated for the first objective is greater than that of the rest two objectives; the first objective was used to calculate the final sample size. After considering design effect of 1.5 the final calculated sample size for this study was 306*1.5 = 459 (9, 10).
Sampling procedure
Multi stage sampling method was used to select the participants. Firstly, Sodo Zuria Woreda was selected out of 16 rural Woreda in Wolaita Zone by simple random sampling (SRS) method. Then, 6 kebeles were selected from 20 rural kebeles in Sodo Zuria Woreda by SRS technique. The number of study participants in each kebele was obtained by dividing estimated population of PW in the kebele by total number of PW in six sampled kebeles and then multiplying by sample size (459). Data registered at health posts or family folder of respective kebele was used to identify sampling frame of households with PW. This data contains health information of pregnant woman and house number. Finally, systematic random sampling technique was used to select the study participants from the family folder at respective health post. After that, data collectors took the house number of study participants and went to the identified household to interview PW. In each household, only one pregnant woman was interviewed (Table 2).
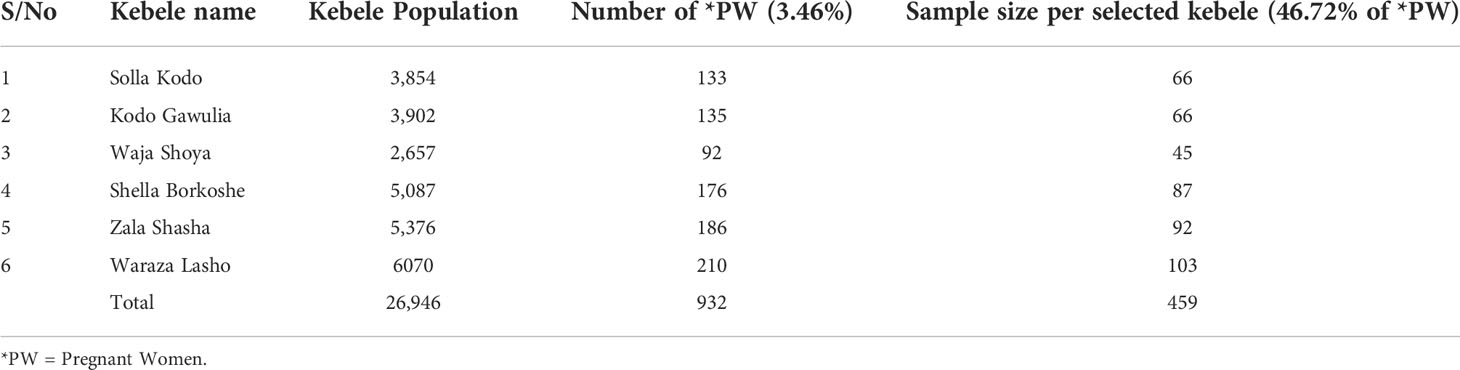
Table 2 Sample size allocation by kebele for the utilization of IINs and associated factors among pregnant women in Sodo Zuria Woreda of Wolaita Zone, SNNPR, 2021.
Adapted from different literatures with a few modification (9, 10).
Data collection
Data were collected using a pretested, structured interviewer-administered questionnaire prepared after reviewing the relevant literatures. The questionnaire was developed in English and then translated to Amharic, and then back translated to English by another public health officer to ensure its consistency in meaning and rationality. It was the Amharic version of the questionnaire that was used for data collection. Face-to-face interview was conducted by four degree holder nurses.
Operational definitions
ITN was defined as any LLIN designed to kill, repel, or block mosquitoes physically, that has been planned to remain effective for more than three years without retreatment (11).
ITN possession: proportion of households with at least one ITN.
ITN utilization- was defined as when study subjects responded positively as having slept under the ITN in the night preceding data collection day (12, 13). ITN utilization was measured based on respondents’ self-report together with direct observation. Accordingly, ITN utilization was recorded to be “yes” if a pregnant women and/or a child slept under ITN during the night prior to the survey date and ITN was observed to be hanged (mounted) over the bed/the sleeping area during the observation day. On the other hand, ITN utilization was labeled to be “no” if a pregnant women and/or a child slept under ITN during the night prior to the survey date or if the ITN was not observed to be hanged (mounted) over the bed/the sleeping area during the observation day despite a positive participant’s report [9].
Proper hanging of ITN: Hanging and putting net under all around mattress properly in a way that it doesn’t allow the entry of mosquitoes.
Proper care of ITN: Washing ITN by using mild soaps and not using detergents like Berekina at a quarterly (three months) interval and drying it under shadow.
Improper care of ITN: Washing of ITN by using detergents like sodium hypochlorite (bleach) and drying it by exposing to direct sun light and washing it more than expected frequently (every 2 to 3 months).
Pregnant woman: is a human female who was registered for ANC follow up by HEWs or a woman self-reported herself as pregnant during the study period.
Data management and analysis
Before the actual data collection, the questionnaires were pre-tested on similar setting but outside selected rural kebeles. The data collectors and supervisors were trained for three consecutive days on principles, ethical considerations, procedures, and details of the questionnaire. The principal investigator closely monitored the data collection process. Completed questionnaires were checked for their consistency and completeness every day and then entered into Epi-Info version 7 statistical software. Finally, the data were exported to SPSS for further cleaning and analyses. To avoid excessive number of variables and unstable estimates in the subsequent model, only variables reached a P value < 0.25 by bivariate analysis were kept in multivariable analysis. We performed logistic regression model using backward stepwise method for the predictors of ITN utilization. Backward stepwise regression approach was preferred because it reduces the number of predictors to reduce the multicollinearity problem and it is one of the ways to resolve the over fitting Statistical significance was set at P value < 0.05 in multivariable logistic regression with their 95% level of confidence interval and adjusted odds ratio.
Ethical considerations
Prior to data collection, ethical clearance was obtained from the Institutional Review Board (IRB) of Hawassa University, college of medicine and health sciences, school of public health under the reference number of Ref.No IRB/060/13. Written permission was obtained from Wolaita zone health department and Sodo Zuria Woreda health office. Informed written consent was attained from each study participant prior to data collection. The purpose of the study was explained to each respondent. During data collection, all study participants were communicated that their participation would be voluntary, and also they were told that they can quit participation at any time, even after the interview is ongoing. Address of the principal investigator was disclosed for participants to use it whenever they have any doubt. Data were collected by using codes. Name and other personal identifiers were not asked and all the confidentiality and private information were kept secret.
Results
Socio demographic characteristics of study participants
Of sampled 459 HHs with pregnant women, 435 were participated in this study making the response rate of 94.77%. The total population of the studied households was 1,908 with an average (± SD) family size of 4.39 ( ± 1.733). Of the total population identified, 435 (22.80%) were pregnant women. Mean age of respondents was 28.69 (SD ±5.48). Of the total respondents, 55 (12.64%), 425 (97.70%), and 314(72.18%) were with no formal education, married (leaving together), and housewife, respectively (Table 3).
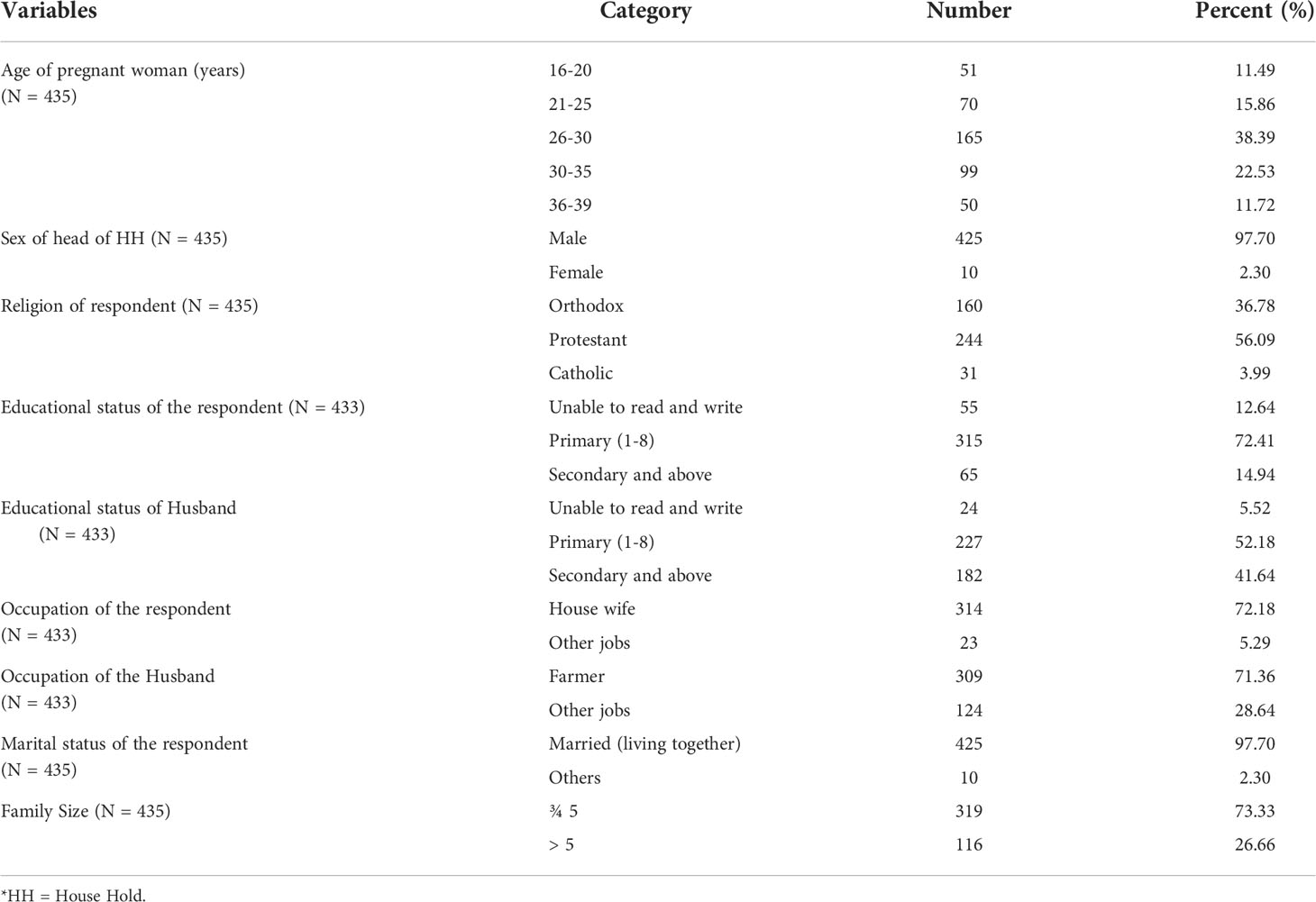
Table 3 Socio-demographic background of the respondents, Sodo Zuria District in Wolaita zone, Southern Ethiopia, 2021.
Household assets and characteristics of housing
Almost all, 430 (98.97) of the roof of houses of study participants were covered with corrugated sheets of iron. Only 51 (11.72%) households possess television. Three hundred sixty two (83.22%) of study participants reported that they use kitchen to cook food. A total of 876 separate sleeping places were identified, thus, making the average number of separate sleeping places per HH was 2.01 (SD ± 0.56) (Table 4).
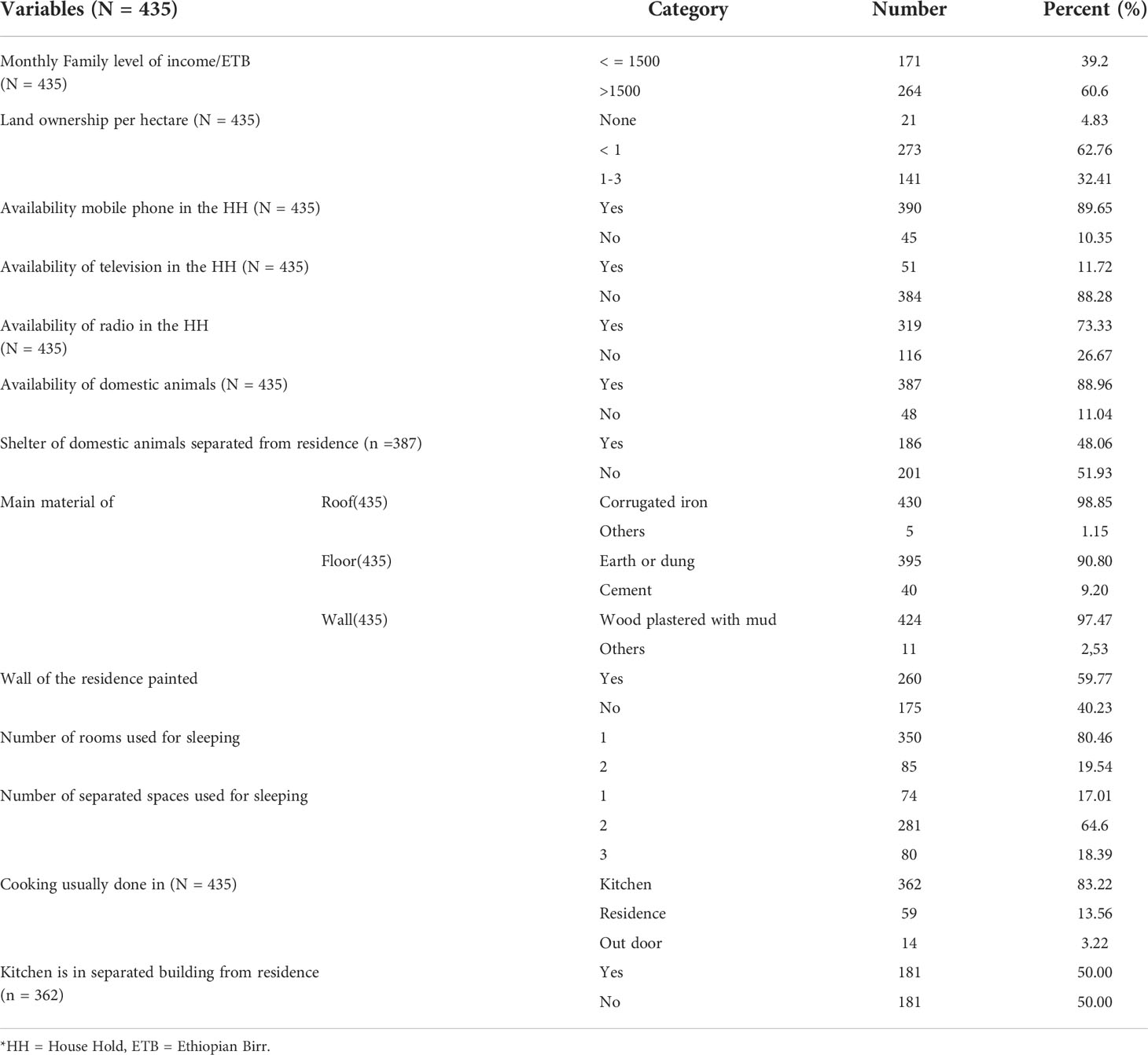
Table 4 Household assets and characteristics of surveyed households in Sodo Zuria Woreda, Wolaita zone, Southern Ethiopia, 2021.
Obstetric health characteristics of the study participants
Mean age at first pregnancy was 20.31 (SD ±2.22). Two hundred seventy four (63.99%) pregnancies were occurred by intention (plan). Concerning ANC follow up, 226 (51.59%) pregnant women were started ANC visit during current pregnancy. However, only 83 (36.73%) of them showed ANC follow up appointment cards for data collectors. Children under age five were 384 (20.13%) with mean of 0.88 (SD ± 0.60) (Table 5).
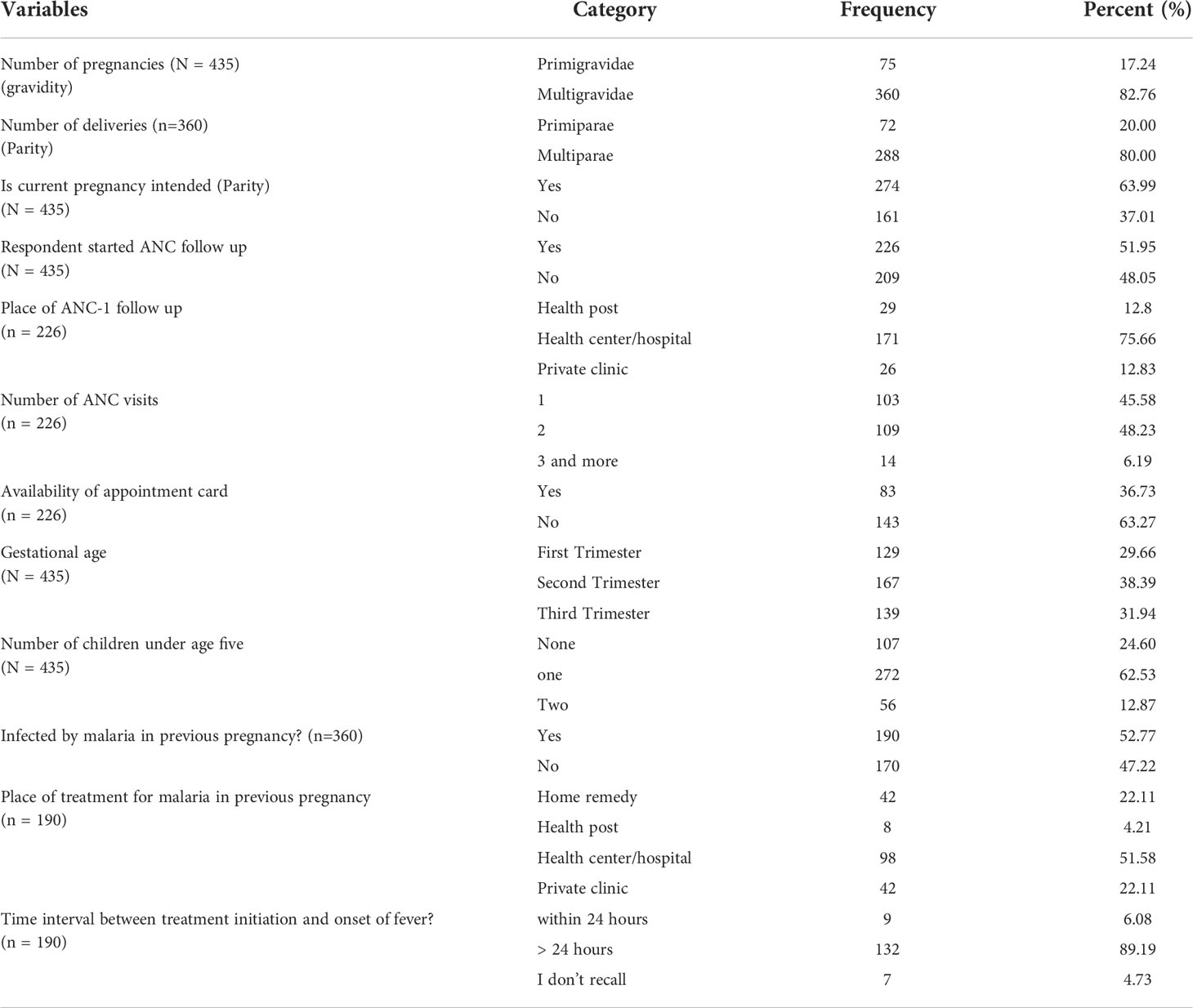
Table 5 Obstetric health information of study participants in Sodo Zuria Woreda, Wolaita zone, Southern Ethiopia, 2021.
Pregnant women’s knowledge towards malaria prevention and control
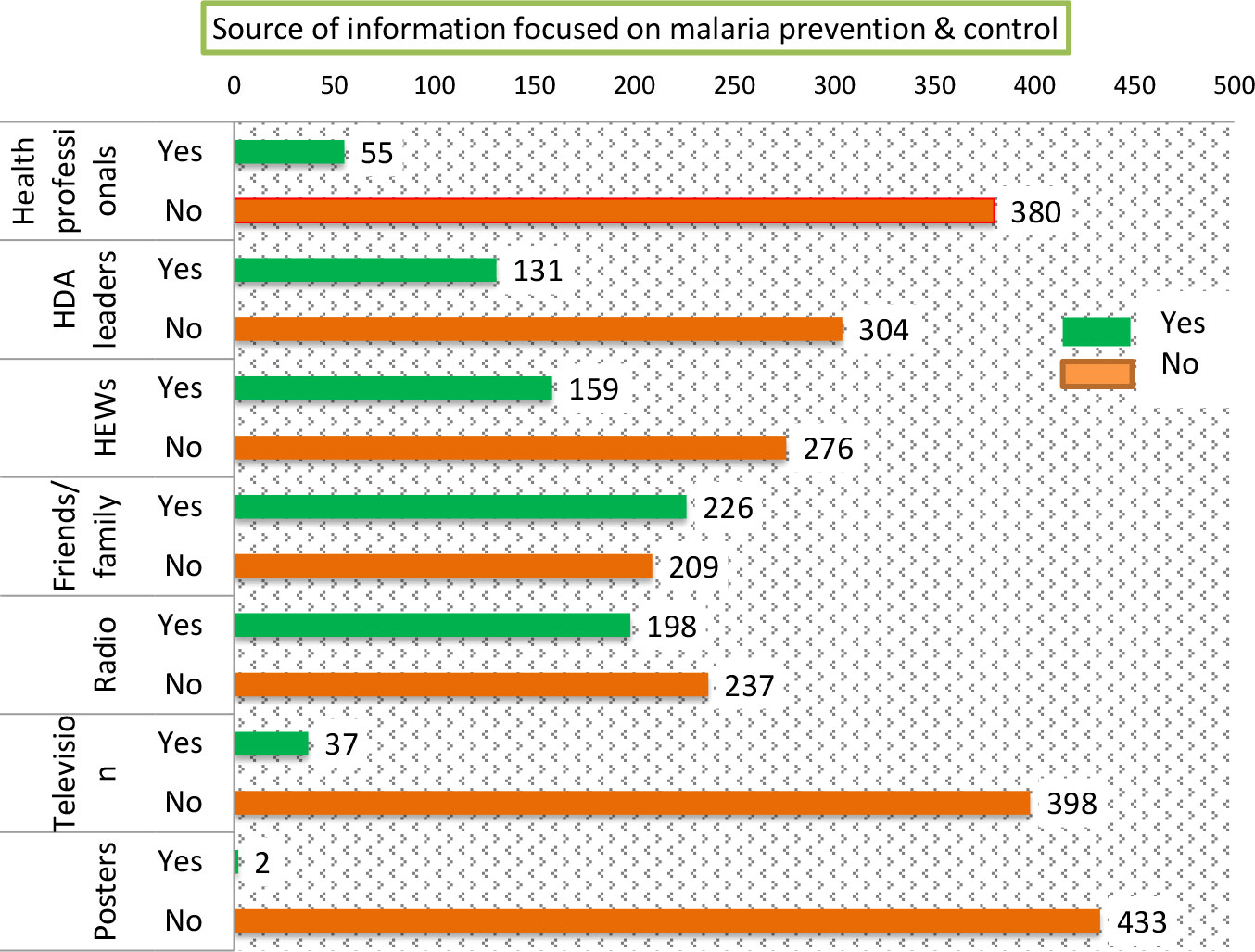
When we investigate study participants’ accessibility for information focusing on malaria prevention and control, 385 (88.51%) have ever heard about malaria. Most frequent 226 (51.95%) source of information responded by study participants was friends/family (Figure 2).
One hundred thirteen (25.98%) of study participants’ home was visited by health workers or HEWs within the last 12 months prior to data collection period. Time elapsed from the last home visit was < 3 months, 3 to 6 months, and > 6 months with proportion of 38.94% (44), 38.94% (44), and 22.12% (25) respectively.
Two hundred eighty two (64.82%) respondents replied that malaria can transmit from infected person to not infected individual and 136 (31.26%) of them recognized bite of mosquito as means of malaria transmission. Two hundred sixty nine (61 83%) interviewees cited that sleeping under ITNs prevents malaria; whereas, 202 (46.44%) study participants mentioned fever as major symptom of malaria.
Wrong perceptions responded by study participants as cause of malaria transmission include physical contact with malaria patients, exposure to bad odor, drinking unsafe water, eating sweet food items such as stalk of maize and sorghum. Two hundred sixty nine (61.84%) of interviewees mentioned sleeping under ITNs as main method of malaria prevention. Other replies include environmental control measures, treating febrile cases within 24 hrs of fever initiation, spray of house with insecticidal chemicals, and taking preventive medication.
Insecticide treated nets possession and utilization
Of the 435 households surveyed, 341(78.39%) with 95% CI (74.5%, 82.3%) possessed at least one ITN. Similarly, coverage of at least two ITNs was 256(58.85%). The number of ITNs identified per household fluctuates from 1 to 4 with an average ownership per HH of 1.89 ( ± SD) 0.628). Three hundred thirty six (98.54) respondents freely obtained ITNs from health institution/HP (Table 6). Of 341 pregnant women who reside in households with at least one ITN, 194 (56.89%) with 95% CI (51.6%, 61.7%) self reportedly slept under ITN on preceding night of data collection day. Among those who slept under ITNs, 78 (40.21%) and 116 (59.79%) used their ITNs consistently (throughout the year) and intermittently respectively.
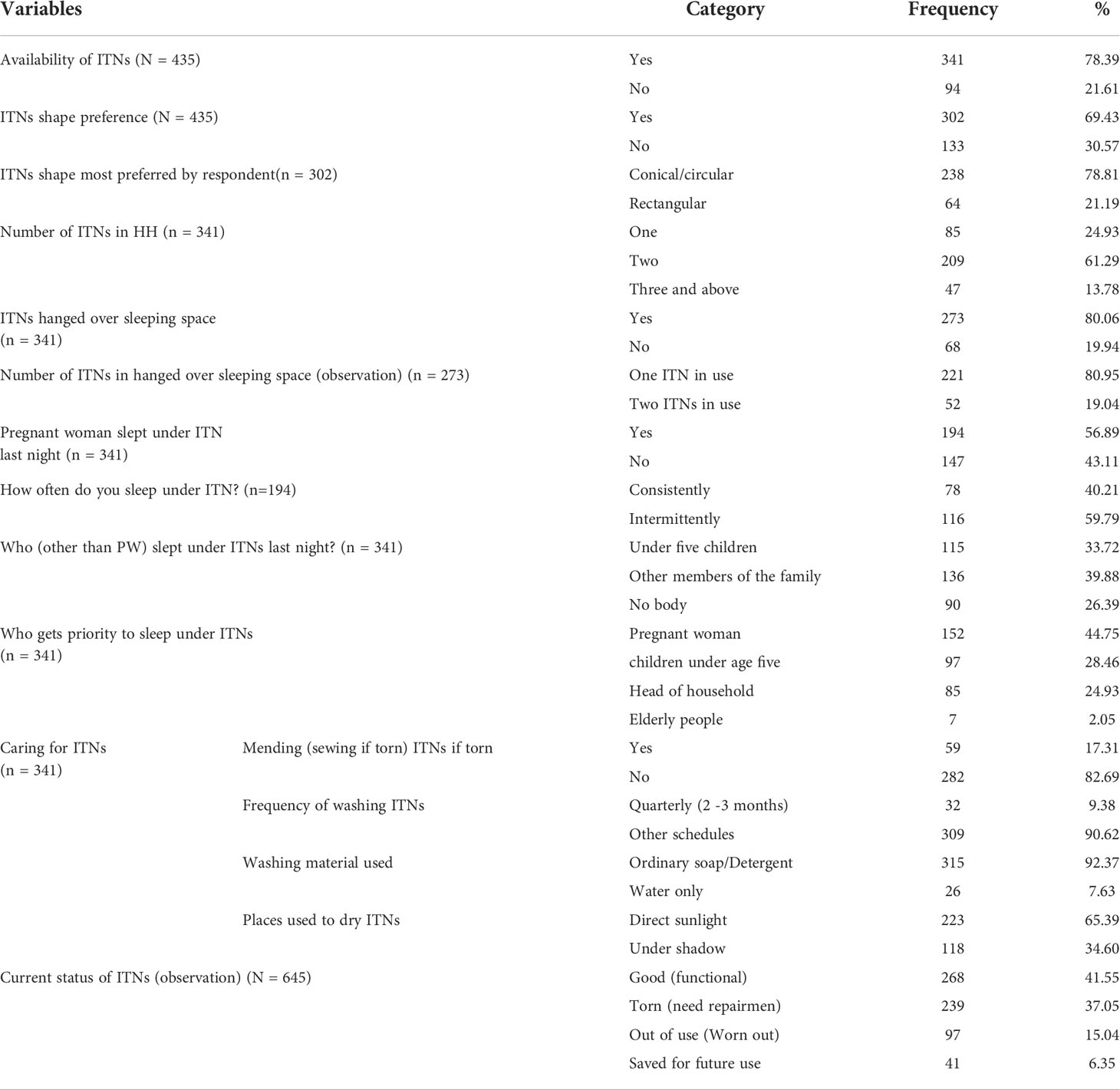
Table 6 ITNs possession and utilization among pregnant women in Sodo Zuria Woreda of Wolaita zone, Southern Ethiopia, 2021.
As witnessed by data collectors, among 341 ITNs possessor HHs, 273 (80.06%) hanged at least one ITN over sleeping spaces. Even if the availability of 645 ITNs was confirmed by data collectors, only 325 (50%) of available ITNs were hanged over sleeping spaces with mean of 0.95 (SD ± 0.592) (Figure 3).
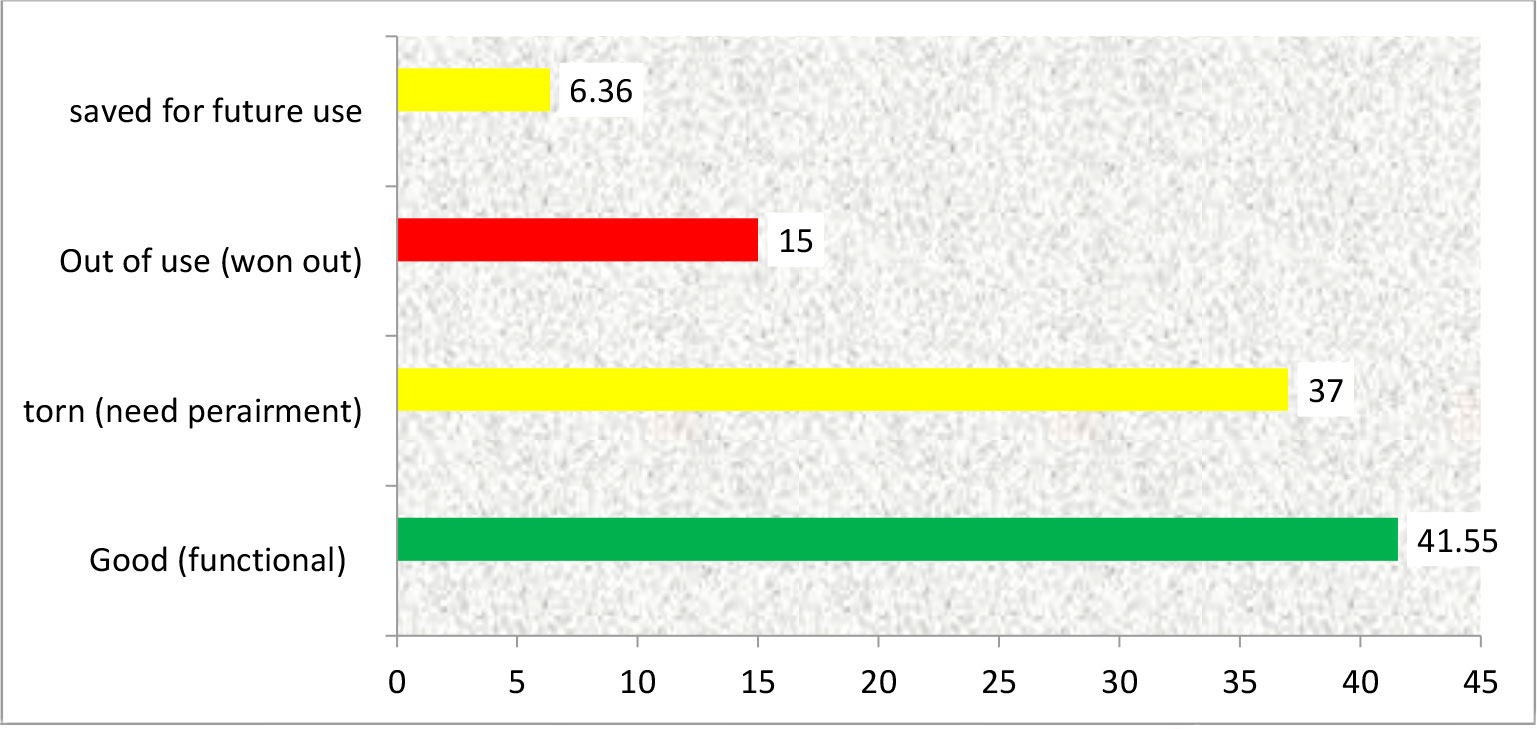
Among a total of 645 ITNs available in surveyed households, 336 (52.09%) ITNs were damaged. Even if it was not time to be worn out to ITNs in relation to mass distribution time (16 months prior to data collection period), more than half of visually inspected ITNs {97 (15.03%) and 239 (37.05%)} were out of use and torn (need repairment) respectively (Figure 4).
We attempted to assess whether pregnant women care for their ITNs or not. As a result, 282 (82.69%) respondents didn’t have experience of sewing (mending) an ITN when it gets damaged (torn). As well, only 104 (28.03%) respondents have positive attitude towards effectiveness of ITNs after washing (Table 6).
Of 116 study participants who use their ITNs intermittently, 67 (57.76%) replied that they use ITNs when they hear mosquito buzzing. Others who use their ITNs occasionally responded as they use ITNS after rainy season, during rainy season, and during dry season, 29 (25%), 14 (12.07%), and 6(5.17%) respectively. Among 341 at least one ITN owner interviewees, 147 (43.12%) didn’t sleep under ITN on preceding night of data collection day. Main reasons specified by them were shown in Figure 5.

Figure 5 Reasons why pregnant women not using ITNs in rural kebeles of Sodo Zuria Woreda, Southern Ethiopia, 2021.
Factors associated with insecticide treated nets possession
Categorical independent variables with P-value < 0.25 in bivariate logistic regression analysis were entered in multivariable stepwise backward logistic regression analysis to determine statistical associations between dependent and independent variables. These include husband’s occupation, time taken to reach health facility, age of respondent, attending ANC follow up, identifying mosquito bite as mode of malaria transmission, knowledge that the use of ITNs can prevent malaria, access to information on schedule of ITNs distribution, ITNs shape preference. On the other hand, respondent ever educated, Husband ever educated, respondent’s occupation, home visit by HEWs, family size, radio available and television available were not associated on bivariable analysis. Therefore, these variables were excluded from multivariable analysis.
After controlling for the effects of potentially confounding variables using multivariable stepwise backward logistic regression, independent variables with P-value < 0.05 with their 95% CI and AOR were identified to be statistically significant predictors of ITNs possession. These include occupation of husband (farmer), AOR = 1.940(95% CI: 1.143, 3.293), knowledge that the use of ITNs can prevent malaria AOR = 1.692(95% CI: 1.007, 2.845), access to information on schedule of ITNs mass distribution, AOR = 3.034(95% CI: 1.724, 5.341) and ITNs shape preference, AOR = 3.150(95% CI: 1.908, 5.200) (Table 7).
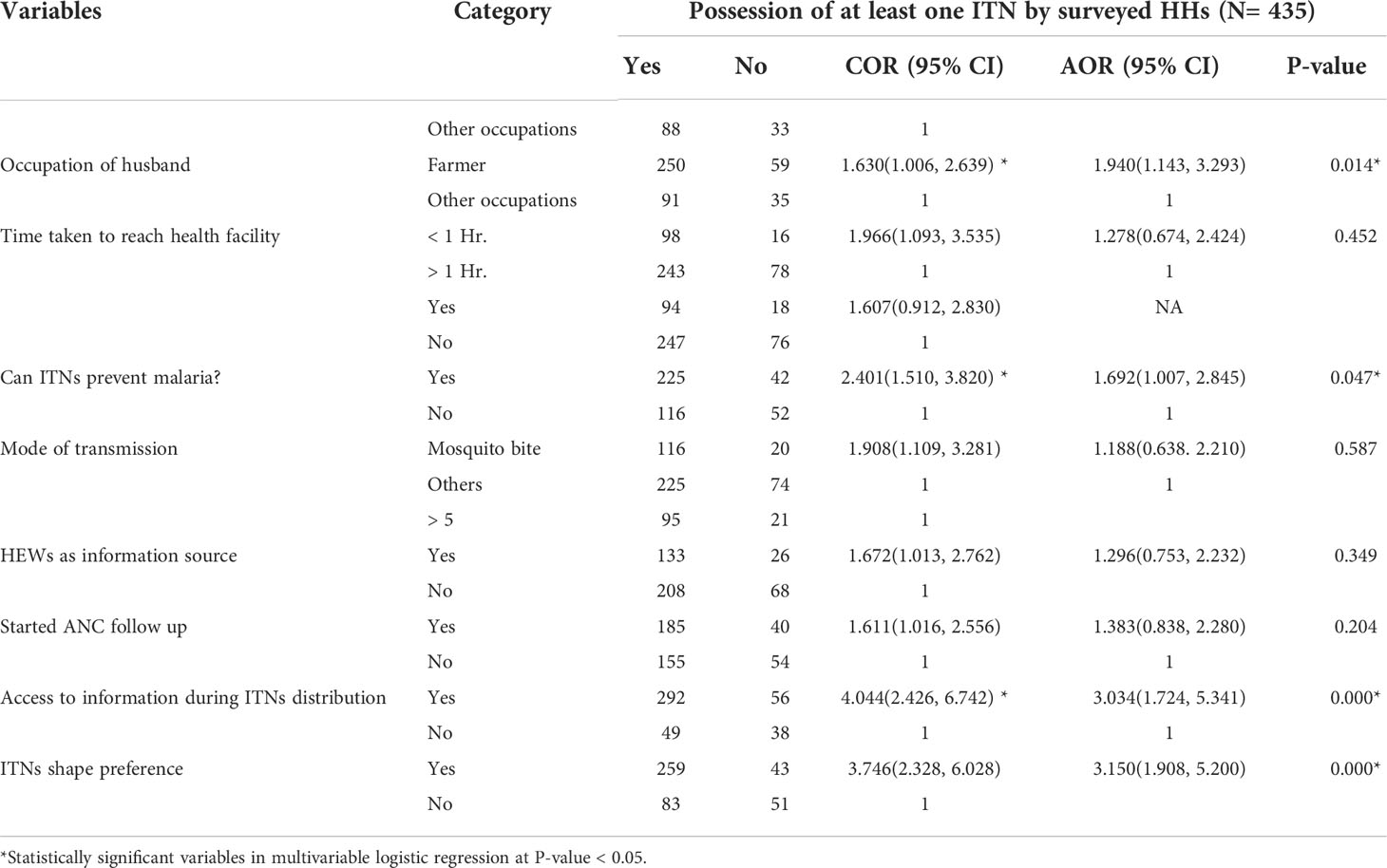
Table 7 Factors associated with Insecticide Treated Nets possession among pregnant women in Sodo Zuria Woreda, Southern Ethiopia, 2021.
Factors associated with utilization of ITNs by pregnant women
Categorical independent variables with P-value less than 0.25 in bivariable logistic regression analysis were entered in multivariable stepwise backward logistic regression analysis. These include attending ANC follow up, utilization of ITNs by other family members, home visit by HWs/HEWs, knowledge that the use of insecticide treated nets can prevent malaria, identifying mosquito bite as mode of malaria transmission, washing material of ITNs, the area cooking usually done, mending practice of torn ITNs, age of pregnant women, Prioritized family members to use ITNs in case of shortage, HEWs as source of information, wall of residential house painted, and access to information on mass ITNs distribution schedule. The investigation yielded eight dichotomized variables at P-value < 0.05 with their 95% CI and AOR to be significantly associated with ITNs utilization by pregnant women. These include utilization of ITNs by other family members, AOR: 6.615(95% CI: 3.358, 13.032), access to information on ITNs mass distribution schedule, AOR: 2.857(95% CI: 1.197, 6.818), knowledge that the use of insecticide treated nets can prevent malaria, AOR: 3.221(95% CI: 1.737, 5.974), identifying mosquito bite as mode of malaria transmission, AOR: 1.929(95% CI: 1.004, 3.706), giving priority to high risk groups (under five children and pregnant women) to sleep under ITNs, AOR: 3.726(95% CI: 1.974, 7.034), HEWs as source of information, AOR: 2.409(95% CI: 1.313, 4.420), Attending ANC follow up visits, AOR: 1.956(95% CI: 1.097, 3.487), and Age of PW, AOR: 0.527 (95% CI: 0.288, 0.965) (Table 8).
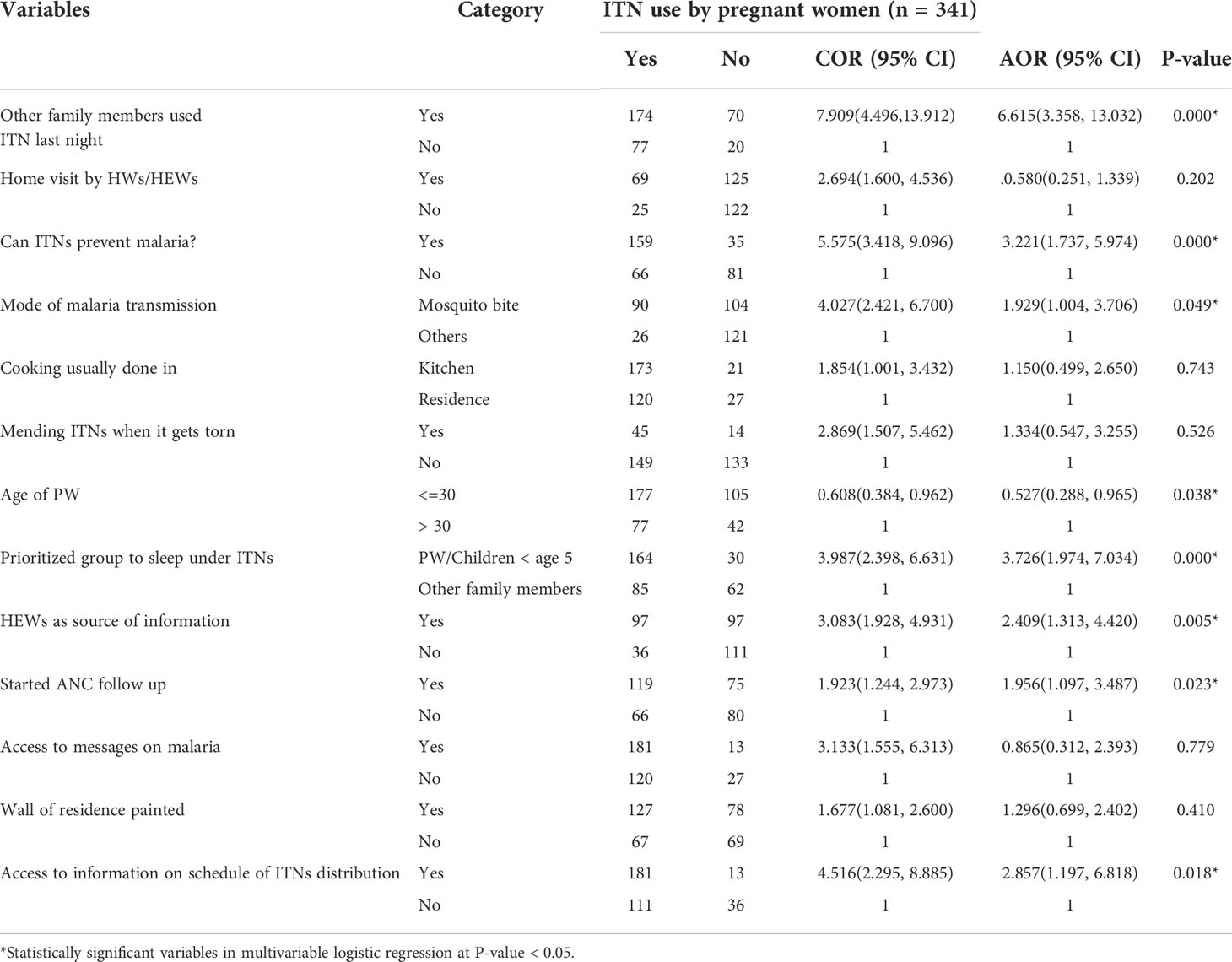
Table 8 Factors associated with ITNs utilization among pregnant women in Sodo Zuria Woreda, Southern Ethiopia, 2021.
Discussion
The aim of this study was to determine the coverage of ITNs, its utilization rate, and factors associated with ITN possession and utilization among pregnant women in rural kebeles of Sodo Zuria Woreda, Southern Ethiopia, 2021. Despite mass distribution of ITNs in January, 2020 in which the Woreda attained universal (100%) coverage of at least one ITN per household, its ownership was low among pregnant women participated in current study. Sixteen months after mass ITNs distribution campaign, only 194 (78.39%) of surveyed households possessed at least one ITN. Similarly, the coverage of at least two ITNs was 256 (58.85%). Thus, in reference to PMI (President’s Malaria Initiative) Ethiopia Malaria Operational Plan/2020 that aims to achieve 100% coverage in malaria endemic areas to own at least one ITN per two persons and to achieve and maintain utilization above 80% by all age and sex groups, the possession coverage of ITNs in the study area was low. As stated in 2017 National Malaria Guidelines, FMoH Ethiopia aims to achieve universal (100%) coverage with one ITN per sleeping space on average to households in malaria endemic areas (14, 15).
Other previous studies carried out in Ethiopia and Sudan also found that maternal knowledge on malaria, maternal educational level, bed room condition, and time taken to reach the health facility and ITNs condition negatively affects ITNs utilization (16–19). Study conducted in Arbaminch town, southern Ethiopia, shown that, education of head of household and rural residence of the household were found to be significant determinant factors of ITNs utilization (10).
In this study, ITNs coverage with one ITN per sleeping space was 62.56%. Our study finding for ITNs utilization by pregnant women was in accordance with a previous report of Halaba Kulito town 54.16% (17). In contrast, the coverage report of our study to possess at least one ITN at household level was higher than the ownership report of previous studies conducted in southern and northern Ethiopia (10, 20). Possible explanation for the difference might be variation in study period which may indicate the impact of interventions done on vector control strategies, especially ITNs distribution. In this study, out of 341 pregnant women who reside in at least one ITN owner households, 194 (56.89%) were self-reported that they slept under ITN the night preceding data collection day. This finding was lower than ITNs utilization reports of Damot Pulasa, and Raya Azebo 72.5%, and 74.3% respectively (9, 19). It was also lower than WHO recommendation (80%) for ITNs utilization by high risk groups and Ethiopia national MIS 2015(74%) (8, 14).
The present study also showed that the proportion between possession and utilization was 78.4% and 56.9% respectively. Possible reason for the disparity between ITNs possession and utilization is failure to supply ITNs in routine service delivery points including ANC follow up visits and EPI services (21–23). The finding of this study was higher than the finding of the study reported in Halaba Kulito (77.4% versus 54%) (9, 17), in Arbaminch district (35%), and National Malaria Indicator Survey of 2015 (44%) (8, 10, 24). This might be due to the progresses in ITNs coverage and improvement in health information dissemination strategies in current health systems. The difference between the report done by the national MIS 2015 and current study might be because the 2015 national indicator survey was carried out across the countrywide where there is low risk and high risk of malaria prevalence.
Our study also revealed that usage of ITNs by other family members encouraged the current utilization of ITNs. Pregnant women whose family members use ITNs are about 6 times more likely to use ITNs than those their family members didn’t use ITNs in previous night of data collection date. This finding was also reported by previous study in Sudan (16). The possible explanation for this result could be ITNs user family members act as role model for pregnant women and motivate their family members to use ITNs. Study participants who prefer ITNs shape were 3 times more likely to possess ITNs than their counterparts. This finding agrees with the finding of the study conducted on Long lasting insecticidal net use and its associated factors in Limmu Seka District, South West Ethiopia, in which the conical shaped ITN was more preferable due to the fact that conical ITNs are convenient for hanging (25).
Study participants who know how malaria transmits were 4 times more likely to utilize ITNs when compared to those who do not know about malaria transmission through mosquito bite. Similarly, a study conducted in Limmu Seka District in South Western Ethiopia reported that study participants who do not know how malaria is transmits were less likely utilize ITNs when compared to those who know about malaria transmission by mosquito bite (25). This study also revealed that respondents who have knowledge that the use of ITNs prevents malaria were 3 folds more likely use ITNs than their counterparts. This finding was consistent with previous report conducted in Uganda (2017) in which 98.1% of the respondents considered ITNs a key malaria prevention strategy (26).
The study participants’ knowledge that sleeping under ITN prevents the transmission of malaria was significantly associated with both ownership and utilization of ITNs. The respondents who know that ITNs prevents malaria by preventing mosquito bites were 1.7 times more likely to possess ITNs whereas, the respondents who know that TTNs prevents malaria were 3 times more likely to utilize ITNs when compared to those who do not know malaria preventive effect of ITNs. Similar finding was also reported in previous study (27).
As identified by current study, about 98.5% of surveyed households freely obtained ITNs from health institution. The report was slightly higher than the finding of the study reported in Arbaminch (10). The finding of the current study also showed that those who receive information about ITNs utilization from health extension are 2.5 folds more likely to use ITNs than their counterparts. Similar findings was reported by the study conducted in Limmu Seka District in South West Ethiopia (25).
Pregnant women whose husband’s occupation was farmer were about 2 times more likely to use ITNs than pregnant women whose husband were engaged in other occupation. However, this finding was negatively associated with ITNs utilization by pregnant women in previous study conducted on determinants of ownership and utilization of insecticide-treated bed nets for malaria control in Eastern Ethiopia (28, 29). Possible explanation for positive association between ITN utilization and partner’s occupation is that agricultural development team (organized by 30 to 40 household heads) and health development army (organized by averagely 30 house wives) work together in various health related issues including promotion of ITNs possession and its proper utilization.
Strengths and limitations of the study
Strengths of our study include data collectors verified the presence or absence of ITNs, its being hanged (mounted) over sleeping space or not, and physical status of the nets (pretense of hole or tear, washing material and drying place, if the net is used for other unintended purposes) by home to home survey. Data collection period was coinciding with the minor malaria transmission period of the year in other parts of the country, but as mentioned in methods and materials section, this period (April to June) seems major malaria transmission period in Wolaita Zone which needs further investigation. Because of the cross-sectional nature of the study design we failed to show trends of ITNs possession as well as its utilization over time. Likewise, the utilization of ITNs by pregnant women was measured by self-report of usage of only one night prior to survey date which may be affected by social desirability bias.
Conclusion
Despite the efforts made to scale up ITN distribution, ITN possession and regular utilization was much lower than recommendation set by WHO. Knowledge that the use of insecticide treated nets can prevent malaria, utilization of insecticide treated nets by other family members, giving priority to high risk groups to sleep under insecticide treated nets, and antenatal follow up visits were found to be significantly associated with ITN by pregnant women. Likewise, having information on schedule of ITNs distribution, and husband’s occupation (being farmer) and net shape preference are significantly associated with ITNs ownership by pregnant women. Premature attrition rate of ITNs was found to be major reason for an observed low ITN ownership and utilization.
Recommendations
Attention should be given to information dissemination and replacement of worn-out ITNs in special schedules such as antenatal follow up visits in addition to three yearly based mass distribution campaigns. There is also a need for implementation of sustainable behavioral change communication (BCC) focusing on caring practices and regular utilization of ITNs after ITN distribution coordinated with prioritizing most vulnerable groups such as Children less than age of 5 years and pregnant women. Furthermore, ITN shape should be considered before procurement to agree with the preference of the commonly.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Prior to data collection, ethical clearance was obtained from the Institutional Review Board (IRB) of Hawassa University, college of medicine and health sciences, school of public health. Written permission was obtained from Wolaita zone health department and Sodo Zuria Woreda health office. Informed written consent was attained from each study participant prior to data collection.
Author contributions
JN and YH was involved in the conception, study design, execution, acquisition of data, analysis and interpretation of data, took part in drafting the article or revising it critically for important intellectual content. AA and MO were involved in study design, execution, acquisition of data, analysis, interpretation, drafted and final manuscript writing. All authors reviewed and agreed on all versions of the manuscript before submission, agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Hawassa University for providing support to conduct this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nega D, Abebe A, Abera A, Gidey B, G/Tsadik A, Tasew G. Comprehensive competency assessment of malaria microscopists and laboratory diagnostic service capacity in districts stratified for malaria elimination in Ethiopia. PloS One (2020) 15:e0235151. doi: 10.1371/journal.pone.0235151
2. Campbell CC. Challenges facing antimalarial therapy in Africa. J Infect Dis (1991) 163:1207–11. doi: 10.1093/infdis/163.6.1207
3. Global technical strategy for malaria 2016-2030 (2021). Available at: https://www.who.int/publications-detail-redirect/9789240031357 (Accessed July 7, 2022).
4. Inungu JN, Ankiba N, Minelli M, Mumford V, Bolekela D, Mukoso B, et al. Use of insecticide-treated mosquito net among pregnant women and guardians of children under five in the democratic republic of the Congo. Malar Res Treat (2017) 2017:5923696. doi: 10.1155/2017/5923696
5. Misganaw A, Haregu TN, Deribe K, Tessema GA, Deribew A, Melaku YA, et al. National mortality burden due to communicable, non-communicable, and other diseases in Ethiopia, 1990–2015: findings from the global burden of disease study 2015. Population Health Metrics (2017) 15(1):1–7. doi: 10.1186/s12963-017-0145-1
6. Gontie GB, Wolde HF, Baraki AG. Prevalence and associated factors of malaria among pregnant women in sherkole district, benishangul gumuz regional state, West Ethiopia. BMC Infect Dis (2020) 20 (1):1–8. doi: 10.1186/s12879-020-05289-9
7. Eaton SL, Roche SL, Llavero Hurtado M, Oldknow KJ, Farquharson C, Gillingwater TH, et al. Total protein analysis as a reliable loading control for quantitative fluorescent Western blotting. PloS One (2013) 8(8):e72457. doi: 10.1371/journal.pone.0235189
8. Taffese HS, Hemming-Schroeder E, Koepfli C, Tesfaye G, Lee MC, Kazura J, et al. Malaria epidemiology and interventions in Ethiopia from 2001 to 2016. Infectious diseases of poverty (2018) 7(06):1–9.
9. Shonga AA, Boltena MT, Boltana TF, Sciences H. Insecticide treated bed nets utilization among pregnant mothers and associated factors in damot pulasa district , southern. J Health Med Nurs (2018) 46:224–30. doi: 10.1186/s40249-018-0487-3
10. Shonga AA, Boltena MT, Boltana TF. nsecticide-treated bed nets utilization among pregnant mothers and associated factors in Damot Pulasa District, Southern Ethiopia. J Health Med Nursing (2018) 46:224–30. doi: 10.4314/ejhd.v23i3.53241
11. Atiele H, Zouh G, Yaw A, Mwanzo I, Githeko A, Yan G. Insecticide-treated net (ITN) ownership, usage, and malaria transmission in the highlands of western Kenya. Parasit Vectors (2011) 4:1–10. doi: 10.1186/1756-3305-4-113
12. Atieli HE, Zhou G, Afrane Y, Lee MC, Mwanzo I, Githeko AK, et al. Insecticide-treated net (ITN) ownership, usage, and malaria transmission in the highlands of western Kenya. Parasites Vectors (2011) 4(1):1–10. doi: 10.1177/1178630220919393
13. Admasie A, Zemba A, Paulos W. Insecticide-treated nets utilization and associated factors among under-5 years old children in mirab-abaya district. Gamo-Gofa Zone Ethiopia (2018) 6:7. doi: 10.3389/fpubh.2018.00007
14. Admasie A, Zemba A, Paulos W. Insecticide-treated nets utilization and associated factors among under-5 years old children in Mirab-Abaya District, Gamo-Gofa Zone, Ethiopia. Frontiers in Public Health (2018) 6:7.
15. Tangena JA, Hendriks CM, Devine M, Tammaro M, Trett AE, Williams I, et al. Indoor residual spraying for malaria control in sub-Saharan Africa 1997 to 2017: an adjusted retrospective analysis. Malaria J (2020) 19(1):1–5.
16. Yassin IM, Rosnah S, Osman M. Factors influencing the usage of insecticide treated mosquito nets among pregnant women. Int J Health Res (2010) 3:139–44. doi: 10.4314/ijhr.v3i3.70278
17. Yeshaneh A, Adane D. Insecticide treated net (ITN) utilization and associated factors among pregnant women’s in halaba kulito town, south Ethiopia, 2016: Cross-sectional study. Int J Infect Dis Ther (2020) 5:34. doi: 10.11648/j.ijidt.20200502.13
18. Berkessa T, Oljira D, Tesfa B. Insecticide treated nets use and its determinants among settlers of southwest Ethiopia global health. BMC Public Health (2016) 16:1–8. doi: 10.1186/s12889-016-2768-8
19. Berkessa T, Oljira D, Tesfa B. Insecticide treated nets use and its determinants among settlers of Southwest Ethiopia. BMC Public Health (2015) 16(1):1–8. doi: 10.1155/2018/3647184
20. Belay M, Deressa W. Use of insecticide treated nets by pregnant women and associated factors in a pre-dominantly rural population in northern Ethiopia. Trop Med Int Health (2008) 13:1303–13. doi: 10.1111/j.1365-3156.2008.02159.x
21. Hill J, Hoyt J, van Eijk AM, ter Kuile FO, Webster J, Steketee RW. Prioritizing pregnant women for long-lasting insecticide treated nets through antenatal care clinics. PloS Med (2014) 11:9–12. doi: 10.1371/journal.pmed.1001717
22. Kilian A, Woods Schnurr L, Matova T, Selby RA, Lokko K, Blaufuss S, et al. Evaluation of a continuous community-based ITN distribution pilot in lainya county, south Sudan 2012-2013. Malar J (2017) 16:1–13. doi: 10.1186/s12936-017-2020-8
23. Kilian A, Woods Schnurr L, Matova T, Selby RA, Lokko K, Blaufuss S, et al. Evaluation of a continuous community-based ITN distribution pilot in Lainya County, South Sudan 2012–2013. Malaria J (2017) 16(1):1–3. doi: 10.1186/s12936-020-03164-1
24. Scates SS, Finn TP, Wisniewski J, Dadi D, Mandike R, Khamis M, et al. Costs of insecticide-treated bed net distribution systems in sub-Saharan Africa. Malaria J (2020) 19(1):1–8.
25. Hambisa MT, Debela T, Dessie Y, Gobena T. Long lasting insecticidal net use and its associated factors in limmu seka district, south West Ethiopia. BMC Public Health (2018) 18:1–7. doi: 10.1186/s12889-018-5022-8
26. Hambisa MT, Debela T, Dessie Y, Gobena T. Long lasting insecticidal net use and its associated factors in limmu seka district, south West Ethiopia. BMC Public Health (2018) 18:1–7. doi: 10.1186/s12889-018-5022-8
27. Tassew A, Hopkins R, Deressa W. Factors influencing the ownership and utilization of long-lasting insecticidal nets for malaria prevention in Ethiopia. Malar J (2017) 16:1–9. doi: 10.1186/s12936-017-1907-8
28. Tassew A, Hopkins R, Deressa W. Factors influencing the ownership and utilization of long-lasting insecticidal nets for malaria prevention in Ethiopia. Malaria J (2017) 16(1):1–19. doi: 10.1155/2012/235015
Keywords: insecticide treated bed nets, malaria, pregnant women, sodo zuria woreda, ITNs
Citation: Nadew J, Obsa MS, Alemayehu A and Haji Y (2022) Utilization of insecticide treated nets among pregnant women in sodo zuria woreda Southern Ethiopia. Front. Trop. Dis 3:926893. doi: 10.3389/fitd.2022.926893
Received: 25 April 2022; Accepted: 18 July 2022;
Published: 18 August 2022.
Edited by:
Meghnath Dhimal, Nepal Health Research Council, NepalReviewed by:
Debora C. Kajeguka, Kilimanjaro Christian Medical University College, TanzaniaGabriel O. Dida, Technical University of Kenya, Kenya
Copyright © 2022 Nadew, Obsa, Alemayehu and Haji. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed Suleiman Obsa, bXN1bGVpbWFuNDNAZ21haWwuY29t
 Jemaneh Nadew
Jemaneh Nadew Mohammed Suleiman Obsa
Mohammed Suleiman Obsa Akalewold Alemayehu1
Akalewold Alemayehu1 Yusuf Haji
Yusuf Haji