- 1Department of Anthropology and Archaeology, Dickinson College, Carlisle, PA, United States
- 2Programa de Pós-Graduação em Antropologia Social-PPGAS, Federal University of Amazonas, Manaus, Brazil
- 3Anthropology Department, University of Maryland, College Park, MD, United States
- 4University of Maryland, Center for Research and Collaboration in the Indigenous Americas, Center for Research and Collaboration in the Indigenous Americas, College Park, MD, United States
- 5Institute of Anatomy, Faculty of Medicine, University of Zurich, Zurich, Switzerland
Introduction: Indigenous peoples of the Amazon basin, in Peru and elsewhere, suffered disproportionately from the impacts of the COVID-19 pandemic. In part, this was due to an initial lack of support by the Ministry of Health, who did not prioritize their care despite their vulnerable situation. Consequently, during the first wave of the pandemic, health professionals in public health facilities in Amazonian Indigenous communities had to handle the disease with limited information and resources. This article analyzes the actions carried out by Indigenous nurse technicians during the first wave of the pandemic.
Methods: Recurrent semi-structured interviews with six Indigenous nurse technicians focusing on their measures toward disease prevention and caring during the first wave of the COVID-19 pandemic in the Atalaya province, Ucayali region, in the Peruvian Amazon.
Results: Nurse technicians worked closely with local authorities and volunteer health promotors. The limited resources they had at the health facilities, coupled with no training about how to treat COVID-19 symptoms led them to resort to their knowledge of traditional Indigenous medicine in combination with biomedical approaches, and support from Indigenous healers. Our analyses shows that this approach proved essential to alleviate symptoms and prevent complications and new infections.
Conclusions: The actions implemented by the Indigenous nurse technicians strongly contributed to the management of COVID-19 in their Indigenous communities, being both effective and culturally appropriate. Our data is in support of a health provision concept that bridges medical knowledge systems in contexts of diversity, avoiding a view on Indigenous health practices as antagonistic or in competition with biomedical practices provided by public health services.
1 Introduction
The arrival of the COVID-19 pandemic in Peru in March 2020 found the Peruvian health system in crisis: deficient infrastructure, lack of necessary health facilities, personnel, supplies, and equipment (1, 2). This situation was even worse in the most remote areas of the Andes and Amazon regions, where Indigenous peoples suffer from poverty, exclusion, and unequal access to health services (3). In fact, Indigenous peoples in these remote areas have poorer health indicators than the rest of the population (4). Although in the last ten years there has been an effort by the Ministry of Health of Peru (MoH) to improve care for Indigenous peoples from the Amazon, the health system in the region continued to be precarious and limited, especially at the Primary Health Care level. By 2017, only 865 Indigenous communities, that is, 32%, had any public health facility. Of these 32%, 92% had a Health Post (the most basic Primary Health Care facility), 5% had Health Centers without a space to hospitalize patients; and 1.7% had Health Centers with a hospitalization area (5).
Despite the vulnerable situation of Amazonian Indigenous peoples prior to the pandemic, the first anti-COVID-19 strategies adopted by the MoH did not prioritize their care with an appropriate approach to their specific needs. It was not until May 2020, three months after the first case of COVID-19 was confirmed in Peru, and in the face of pressure from Indigenous organizations and allies, that the MoH designed a specific health plan for this population (6). While the plan began to be implemented in June of 2020, it took time to reach certain regions (6). This could explain the difference between the national lethality rate from COVID-19 (4.89%) and the lethality rate in Ucayali (7.2%), where this research was conducted (7). The lethality rate in this Amazonian region does not account for several Indigenous deaths that occurred at the beginning of the pandemic when there were no rapid tests available and there was no established system to report deaths occurring in Amazonian Indigenous communities.
During the first wave of the pandemic (April to September 2020), health professionals in public health facilities in Amazonian Indigenous communities, had to manage the pandemic with their own resources and with limited information about the disease, as they waited for the measures of the MoH to be implemented. The goal of this article is to present and analyze the actions performed by Indigenous nurse technicians trained in intercultural health, to combat the first wave of the COVID-19 pandemic in the Atalaya province, Ucayali region in the Peruvian Amazon. We provide a qualitative analysis of the effectiveness and cultural pertinence of their actions as a basis for future health concepts appropriate for Indigenous communities. The analysis of their experiences points to the importance of ensuring that public health strategies adopted in the Amazon region take into account the characteristics of the official health system at the local level, its interaction with Indigenous health systems and its limitations to provide culturally-relevant care for Indigenous people.
2 Methods
Six Indigenous nurse technicians (hereafter “nurse technicians”) participated in this qualitative study. Between 2005 and 2008 they had undergone a Training Program for Nurse Technicians in Intercultural Health designed by the Interethnic Association for the Development of the Peruvian Amazon (AIDESEP) to ensure healthcare provision that is relevant and respectful of the sociocultural characteristics of Amazonian Indigenous communities (8). The program comprised both training in biomedicine and Indigenous medicine with the goal of having an Indigenous health workforce capable of providing culturally appropriate health care, and of recognizing and building bridges between Western and Indigenous health systems (9). At the time of the interviews, the six nurse technicians had been working for at least 10 years in public health care facilities in the province of Atalaya, Ucayali region, Peru, where they were based at the time of the arrival of COVID-19 in April 2020.
The province of Atalaya has a large Indigenous population from the Shipibo-Konibo, Ashaninka, Asheninka and Yine ethnic groups, among others (5, 10). For decades these groups have faced the progressive invasion of their territories by settler populations, illegal logging of wood in their territories, and pollution of the Ucayali and Urubamba rivers as a result of fluvial traffic brought by the hydrocarbon companies that operate in the region (11). The latter has reduced the availability of fish, which is a major source of protein for the Indigenous population. Throughout the region, they increasingly depend on processed foods, which has had a negative health impact, particularly on the nutritional status of children (11). Furthermore, this dependency implies they have to go to the city of Atalaya on a regular basis to buy foods that have become part of their everyday diet, such as pasta, rice, cooking oil, etc. This need to travel to urban areas, helps explain how COVID-19 reached their communities and facilitated the spread of the virus.
Each nurse technician served at least five communities, as shown in Table 1.
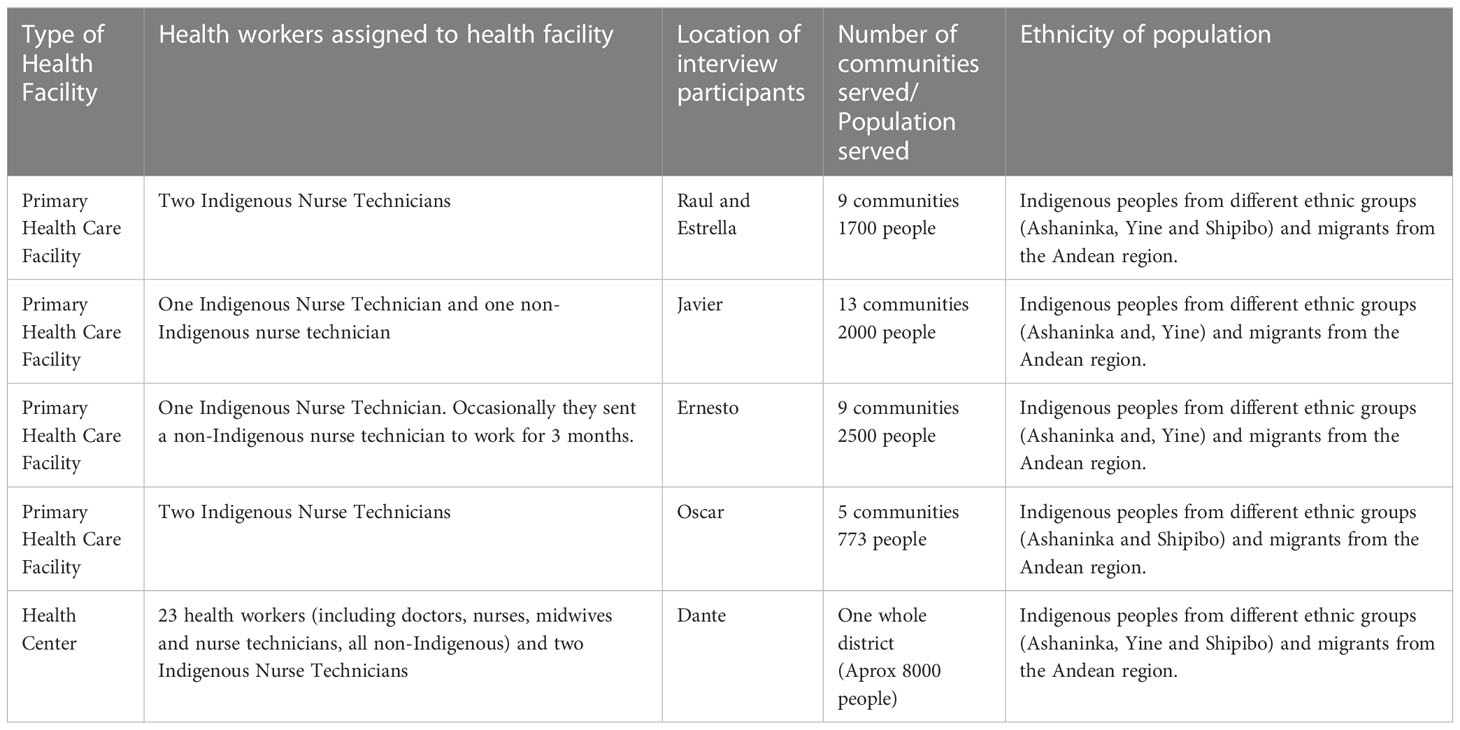
Table 1 Number of communities and population served by the health facilities where nurse technicians work.
With each nurse technician, we held two to four in-depth interviews with semi-structured guides focused on their experiences in preventing and treating symptoms of SARS CoV-2 in Indigenous communities within the jurisdiction of their health facility. The interviews were conducted between the months of April and July 2021 by telephone and lasted approximately 50 minutes each. All interviews were conducted in Spanish, and during times and days proposed by the nurse technicians. This was often at night when the internet or phone services worked better in their communities, but occasionally when they were in the city of Atalaya during the weekends or at the end of the month when they travel to submit their monthly reports. All interviews were conducted by two anthropologists with experience in qualitative research and who had known the participants for at least 10 years. Before each interview, all participants received an explanation of the goal of the study and the future use of the data, they were asked for their consent to record the conversations, were informed that their participation was voluntary, and that the information shared will remain anonymous. We began each initial interview with an open question about the characteristics of the health facility where they worked. We then asked them to remember when they first heard about COVID-19. All follow-up questions were based on the responses the nurse technicians provided to capture the nuances of their specific experiences and actions during the pandemic. The interviews were recorded and transcribed verbatim. They were then read several times to identify the themes that emerged from the narratives and organized according to such themes. If there was a need to better understand a particular aspect of the transcript we would contact the nurse technician to clarify their accounts. To protect the anonymity of the nurse technicians we are using pseudonyms throughout this manuscript.
3 Results
Analyses of the interviews revealed that the experiences of the nurse technicians during the first wave of COVID-19 can be grouped into three themes: coordination actions with different community authorities to prevent COVID-19 from reaching the communities; care for patients with COVID-19, and preventive actions to avoid contagion within communities where they worked.
3.1 Coordination actions with local authorities and with promotores
Before the arrival of COVID-19 and as part of their approach to providing health services, Indigenous nurse technicians had already established close relationships with the local community authorities. In Peru, Indigenous communities have an elected chief (sometimes called “apu” or “community president”), a vice president and four members of his council. Prior to the beginning of the pandemic, nurse technicians collaborated with them when organizing visits to communities for vaccination campaigns, prenatal check-ups, and consultations on general health problems.
The first news about COVID-19 reached the communities in March 2020 through the radio, television or phone from relatives living in urban areas. In response to such news, many local leaders decided to design and deploy actions aimed at preventing the virus from entering the communities, which included closing access to the community (by river and by road), and restricting the number of people who left the community to buy essential things from Atalaya, the closest city. Through their existing relationships with community authorities, nurse technicians actively participated in these actions aimed at stopping people from outside the communities entering these territories, and monitoring the exit of people from the community who could later come back infected. At that point in time, they did not have access to any type of COVID-19 testing. In some cases, nurse technicians were designated to coordinate with governmental authorities to implement protection measures to prevent the entry of COVID-19 into the community. As one interviewee stated:
“[People told me that there were COVID-19 patients in Atalaya] It was like a time bomb that will eventually reach this area. Those who came from Pucallpa came in boats, stayed on the shore, and entered the community [without permission]. I coordinated with the prosecutor, with the Navy, the Police, so that they would arrest people who entered like this. I was [in charge of] calling the Prosecutor, I was [in charge of] bringing the Police to the passenger boat that docked so that they would take the passengers [who wanted to enter the community] away.” (Javier)
Additionally, measures were implemented to regulate the number of people who were authorized to leave the community to buy groceries in Atalaya. Nurse technicians took turns to participate in these control actions. The stories shared by them highlight that initially all the actions were locally-planned by the communal authorities without much support from state entities such as the Municipality or the health authorities:
“The response [of the state authorities] was late, we were the ones fighting the pandemic [alone]. Both the [communal] authorities and the community members have fought this pandemic. Finally, the [regional health authorities] came to equip us, to give us medicines, but it was too late. The pandemic was over.” (Raúl)
Eventually, in May, despite the efforts made to control the entry and exit of people from these Indigenous communities, COVID-19 arrived and infected the majority of residents, as tests done months later by health authorities confirmed. Faced with the infection of the population, as well as their own infection with COVID-19, the nurse technicians had to develop actions to prevent more infections and care for the sick, without neglecting actions to ensure outsiders would not enter the communities and further increase the number of cases. For this, coordinated work with the health promoters (promotores) was essential.
Promotores are residents of the community who are selected by the community members to provide volunteer basic health assistance and who receive some training from the MoH to deliver such care. Promotores who work in Indigenous communities, are Indigenous themselves and are usually the first to whom the family of a sick person turns to. They have essential training to provide basic care to patients before taking the patient to the Primary Health Care facility (Postas) or requesting that the nurse technician travel to the patient’s home. Nurse technicians told us that, to the extent possible, they train the promotores in the use of medicines and, when available, provide medicines for them to administer, so that promotres can care for the population affected by minor health problems: “Promotores are like the right hand of us technicians.” (Ernesto) Given the distances that usually exist between the community where the posta is located and the communities they serve, it is necessary for nurse technicians to have a trained person who can respond quickly and in a timely manner while they travel to the patient’s community.
During the pandemic, closeness with the promotores proved essential, both to disseminate information about the preventive measures to be taken, as well as to share information about some medicinal plant treatments that, as we will see in the next section, were key to providing care during the pandemic: “During COVID [the promoters] were also supporting me, and they continue to support me in one way or another, they are helping us.” (Oscar) However, since promotores are not officially recognized by the health authorities, there was no protective equipment for them, and this worried nurse technicians because they knew that this could result in the promotor becoming ill: “Imagine, suddenly a promotor does a home visit, enters the house, touches people … and without protection, he is going to get infected.” (Oscar) While Oscar appreciated the support of the promotores during the first wave, he was also concerned that he did not have enough biosafety equipment to protect both the promotores and himself.
3.2 Health care provision during the first wave of COVID-19
3.2.1 Unprepared for the pandemic
In April 2020, when cases of people with COVID-19-like symptoms started to appear in the community, the nurse technicians did not have enough medicines or training to treat the patients: “At the beginning of COVID we did not have any masks, no aprons. We didn’t even have [medications] at that time, we didn’t have any [medication] at all.” (Javier)
All the nurse technicians felt unprepared in the first moments of the arrival of COVID-19. During April, the only official indication received from the regional health authorities was that they should close the health facilities. But community members and promotores sought them out to receive care they felt they had to provide.
“We had only heard [of COVID-19], they [health authorities] did not equip us, there was no training or anything. We were totally unprepared. In June or July, more or less, when people were dying, they started giving us information [on the virus and its treatment] because we really didn’t know [anything] or why they didn’t care for us (…) practically … the health posts had come to a standstill. (…) There was no guidance on how to refer patients or what treatment to give. Without knowing, we provided treatment.” (Estrella)
The information that both nurse technicians and the population had about COVID-19 came mainly from radio news programs, what people were saying in their community, and what they heard from friends and relatives in other places. The nurse technicians remember that until approximately June 2020 (at which time Atalaya had the highest peak of infections); they still had not received any medicines against symptoms of COVID-19, training on treatment concepts, or biosafety equipment to protect the population or themselves. However, they were aware of the fear and concern in the communities they served. So, despite the limited information nurse technicians had, they provided words of reassurance:
“[The local population] was not informed; they said that the disease is going to come and it is going to kill them all … That is what they thought: “we are going to die”. Listening, and putting together the information [I had at hand] (…), I told them: “This is how it is: COVID is like the flu (gripe); if [the symptoms] increase [intensify], it can become a serious pneumonia and you can die from pneumonia. So, before it turns into pneumonia or bronchopneumonia, you have to prevent it. How? Washing your hands, wearing a mask, distancing one meter. Those are mostly the prevention actions that can be done [to prevent it from becoming] a serious disease.” (Raúl)
Although communities with smaller health posts were facing a complicated situation due to the increasing number of cases, things were worse in the Health Centers where patients with complications were referred to. The level of misinformation and lack of preparation among health workers was the same as in the health posts:
“We had nothing, we didn’t even have a thermometer, we didn’t have an oximeter. The [Health Network] only sent an oximeter to each staff member in December. With those limited resources we have been working and we have controlled the disease to some extent … The Health Center was contaminated, it had to be fumigated and that is why a separate COVID area was opened. Our oxygen supply was very low: three or four canisters came for the patients we had, and also for other [non-COVID] patients … We only had a nebulizer, but we couldn’t ask for more. In other words, there was oxygen, but it was not enough. Supplies have never been enough, there have always been deficits … And, besides that, since it was a very new disease, we did not know what the treatment was. [We treated patients] with antibiotics and corticosteroids. So, instead of curing, we made the patient get worse, we made his health condition more complicated. These are experiences that have happened to us … Just two or three weeks ago, more or less (April 2021), a doctor from Lima came to train us on the management and types of medications we need to use [to treat a COVID patient] according to the severity and stages [of COVID].” (Dante)
But in the year between the arrival of the pandemic and the arrival of proper training many people had died and, meanwhile, the nurse technicians in the health posts tried to cope with the situation by combining elements of Western medicine and traditional Indigenous medicine to care for patients who developed flu-like symptoms.
3.2.2 Taking care of patients during the COVID-19 pandemic
Not having enough biomedical drugs in their health facilities, nor clear guidelines on how to treat COVID-19, the nurse technicians resorted to their knowledge of Indigenous medicine:
“Our decision has been to use medicinal plants. If there was no Western medicine, you had to resort to traditional medicine, it was the only alternative … For this reason, we have coordinated with the wise men (sabios) of the community and we have all come together to provide a solution to the problem of the COVID disease.” (Raúl)
One of the key therapies to treat symptoms of COVID-19 during the acute phase and reconvalescence were vaporizations (vaporizaciones) that consisted of boiling one or more medicinal plants in a big pot and covering the patient with a blanket, ensuring the patient inhales the steam and heat its body with it. The vaporizaciones were sometimes prescribed by nurse technicians who, in addition to applying or prescribing Western medicines, recommended that the patient either vaporize at home or looked for the vaporadoras, (traditional healers who heal with vapor). Not all communities had vaporadoras, but in those where they had, their traditional knowledge proved essential to alleviate COVID-19 symptoms:
“Matico (Buddleja globosa) and kion (ginger) were mixed and patients were steamed three times [with this mix], especially in the afternoon. The best thing was to steam patients at noon and then use that same hot water to bathe, since it was necessary to avoid the cold, both from the environment and from the water with which they bathed, since the cold could make the patient go into a shock. The vaporadoras also indicated that after steaming the patient, he should bathe and go to bed so that he does not get cold again and fall sick. [People who do not follow these recommendations get worse].” (Ernesto)
Nurse technicians would sometimes go with the vaporadoras to patients’ homes and tried to help out, while vaporadoras steamed and bathed patients. Patients had to use the warm water used for steaming to bathe afterwards. After the treatment was completed, the nurse technicians gave additional instructions to ensure the vaporization would take effect such as: not exposing themselves to cold air, not bathing with cold water, not eating cold things and staying at home. Home visits by vaporadoras occurred in communities where families called them, or the nurse technicians sent for them when they knew there was someone in the community showing COVID-19 -like symptoms. However, when the cases began to increase, the vaporadoras could not handle such high demand. As a result, some people began to learn some basic skills in treating with vapor, such as Estrella, one of the nurse technicians who learned to vaporize in order to offer this therapy herself:
“I learned to vaporize because of the pandemic; because they told us “Eucalyptus is good”. So we started to buy Eucalyptus, [a big] quantity, to be able to vaporize patients. And well, here in the community there is Matico with which we vaporized. …. We vaporized people in the mornings and evenings and gave them (Western) treatment, after vaporizing them…. We used Eucalyptus so that it opens up the patient’s lungs and he can breathe better. The Mucura (Petiveria alliacea) because it is good for the flu, for the nose; and the Matico is good for the lungs. That is why we mixed these three things: Eucalyptus, Mucura, and Matico. And I also brought Chamomile and I made them drink [chamomile tea] with two Eucalyptus leaves; and they drank that with a little sugar.” (Estrella)
The vaporization that Estrella learned was not the same as the one applied by vaporadoras. These Indigenous healers use hot stones to warm up the water, in addition to plants. Specialized vaporization is only done by people who “know”. Some of them provided this treatment to COVID-19 patients, as seen in this description:
“…He prepared his plants, brought them from the mountains, began to release the stones in the water. When they release the stones, more steam comes out, it’s not like when you take a pot, put the eucalyptus, your menthol, a cinnamon stick and you will see steam coming out. No, vaporadores drop the stones in the pot and the steam intensifies … If your back hurts, [the vapor] relieves your lungs. The vaporador vaporizes in a very calm way, the patient does not wear any clothes, the vaporador begins to rub the back [massage] and those vapors are very good because all that hot air kills [COVID].” (Javier)
Eventually, vaporization as an effective measure to help patients breathe better was adopted by the entire population in the different communities where the nurse technicians worked. People vaporized themselves at home:
“The population already knew [what the treatment was]: if they felt unwell, with a headache, with shortness of breath, they would first had to vaporize and then for the headache, they would take the pill.” (Javier)
Both the nurse technicians and the population made complementary use of Indigenous and Western medical treatments to calm the symptoms and relieve the patient. Some nurse technicians, like Oscar, taught and promoted the use of vaporization at home by the patient’s family members:
“When I had a strong hunch that a person had COVID I knew the virus would directly attack the throat and that is when complications begin [for the patient]. [In those cases], I would request that somebody, a single person from that household, would be responsible of the vaporization. This person would make the patient inhale [the medicinal steam], would prepare warm drinks…. First, I show him how it is done and then, the next day, they will do it [alone]. It is their responsibility to continue the treatment at home … but someone [in the family] has to know to prepare the vaporization in order to cure the patient.” (Oscar)
In addition to the steam treatments, the nurse technicians assisted patients by promoting the consumption of hot herbal remedies such as Chamomille with Eucalyptus. Additionally, people drank “preparados” which were a mixture of strong liquor from sugar cane with honey, toasted onion, garlic, and other ingredients (this preparation varied, there was no standard preparation). In other words, there were different medical strategies that families and nurse technicians pursued to alleviate the symptoms and strengthen their bodies to avoid relapses or getting sick.
Information about treatments that worked was exchanged:
“The entire population began to use medicinal plants, that is, they all began to make their “preparados”, they went to the neighbor, the neighbor told them, about the plants they were using [to prevent COVID or to alleviate the symptoms]. Everyone was using plants, traditional medicine, all the families [were using it]. I sometimes taught them [which plants to use] and others already knew and taught themselves. They began to look for the plants and almost everybody used them as a preventive measure. A great majority used the [medicinal] plants here in the communities.” (Oscar)
“In the context of COVID, people shared and used their common knowledge around medicinal plants. For example, there is no Eucalyptus, here in the community, it is only available in other regions. It does not grow in the jungle. In that case, we thought, “eucalyptus is like a menthol”; (then) we began to look for an alternative in the jungle, such as Matico. If in the city [the treatment] is being done with Eucalyptus, here it can be with the Matico or with the Mucura. [The community members] have tested the plants and have had positive results.” (Raúl)
The care provided by the nurse technicians shows that they were learning not only about the plants that were effective for the symptoms of COVID-19 but also about the treatment length, how many times a day it was necessary to do it, and at what time people should be vaporized: “There are people who have a high fever and cannot receive the vapor treatment because [they can] have a seizure” (Estrella)
That trust to exchange knowledge, treatment recipes, and care advice, was possible in the context of the pandemic because there was already a trustful relationship between the local Indigenous population and the nurse technicians, who, even before the pandemic, used medicinal plants or gave people advice about Indigenous treatments with plants that they could use in addition to the pills or syrups.
The nurse technicians used both medical systems, Western and Indigenous, to treat COVID-19 symptoms. Each medical system fulfilled a different function:
“[Our efforts] have been a combination [of medical systems], because the medicinal plant was simply used to relieve the discomfort in the lung that was obstructed; besides that, Western medicine was also used.” (Raul)
Generally, Western drugs were prescribed to reduce fever while Indigenous medicine was prescribed to relieve respiratory difficulties. Some nurse technicians would visit patients’ homes where they would first perform a vaporization and then give them an injection. Once the patient felt better, “we explained to them how and with what to vaporize and the relatives had to continue the treatment.” (Raúl)
In those communities where people had less knowledge of medicinal plants, in addition to providing Western treatment, the nurse technician taught them which plants they could use for vaporizations:
“Those who don’t know [about medicinal plants] are the ones who live further away; you have to teach them [about the medicinal plants for COVID]. (…) I told them “This plant with a small leaf, this one and this one.” (…) And people told me “Nurse, we have a lot of those where we live!” “Sure, there is a lot.” And I made them smell the Ajosacha [local garlic variety], because they did not know the Ajosacha (…) Now the population knows what plant is [effective] and we are making them take their Matico, their Ajosacha, their Mucura, the boiled banana peels. You have to take honey from the hive so that it clears out all your airways. And people will tell you: “You have to wait for a full moon to be able to take out the hive.” That’s what they’re telling me now: that they are going to eat [boiled] banana peels.” (Javier)
Teaching community members about suitable plants, i.e. species that could protect them from the disease and how to use them, was key when families decided to move away from town. Being far from the health post, they needed to know how to treat themselves in the event of COVID-19 illness. Additionally, some nurse technicians shared their personal treatment schemes, implemented when they themselves were affected by COVID-19. Telling the local population about their personal experience served to encourage people who were afraid of dying when they found out they had COVID-19, because at that time, people had heard about the lethality of the virus.
All the examples that the nurse technicians shared, demonstrate that there was not only an openness to learn but also a willingness to share knowledge and help each other:
“We resorted more to medicinal plants than to [Western] medicines, because we did not know exactly what the treatment for COVID was like. We resorted more to medicinal plants, because [although] we were previously working with them (treating with medicinal plants), [we] didn’t used them as much. In the pandemic, the most valuable thing [we did] was to use what each place provides, [including] the plants…. We have tried to investigate all the plants [that could help] fight this disease, with our preparados with Matico, with ginger. It really helped us to be able to experiment more with the different types of plants that were already being used in other places. Community members came and wanted to know about what had been used by people who have been cured. Somehow, we also gave people support and shared the knowledge that we acquired in our training as intercultural nurse technicians. The other co-workers (non-Indigenous) didn’t [use medicinal plants], they just use [Western] medicine, but we did use traditional medicine.” (Dante)
Since the initial symptoms of COVID-19 resembled the flu, similar treatments and plants were chosen, such as Ajosacha, which, according to a nurse technician, is commonly used together with the Mucura against the common cold. On several occasions throughout the interviews, nurse technicians will mention that people with COVID-19 should avoid exposing themselves to “cold” since COVID-19 is regarded as being a “cold” disease or related to coldness. Therefore treatment should be aimed at getting rid of that cold from the body and keeping the body warm:
“When COVID enters your body, it is necessary to drink hot things because that soothes the entire throat … With this disease, you must protect yourself from the cold: [you should stay away from cold things], you should not touch cold water, nor bathe in cold water. Because if you touch or drink something cold, the throat will be immediately compromised; you will get an unbearable discomfort in your throat. And if you bathe (with cold water), you will get the chills and that’s how complications from the disease begin. Instead of bathing in cold water, we have to take steam baths, clean ourselves with something hot. This is the way to take care of yourself and kill the coronavirus. Because the coronavirus does not like hot things, it likes cold [things]. He likes the cold and attacks the patient’s [respiratory system], their breathing … and [you get] pneumonia and [that’s it], goodbye. That is when the person dies.” (Oscar)
This same principle of warming the body to heal one’s self and to prevent the disease from attacking you was mentioned by other nurse technicians. They also shared that people in the community used plants in “preparados” to warm the body and counteract the cold caused by COVID-19. They used these principles to guide their healing actions:
“[After steaming] you have to drink something hot, hot, be it tea, chamomile or orange, because if we give something cold [to the patient], [symptoms] become difficult (worse) for the patient. And it is true, I have verified it, everything has to be eaten hot. Because once, it happened that we have managed to treat the poor clinical status of the patient, [and then the] patient said: “I’m fine,” and drank [something] cold and everything (all the symptoms) started [again]. After the vaporization, he got rid of the disease [inside the body], he was relieved, he was able to breathe. We then used the other medicine, Western [medicine] and he felt good. I recommend not to bathe with cold water, always with lukewarm water, because if they don’t, the patient relapses.” (Raúl)
We can see that nurse technicians not only have knowledge about treatments from the two medical systems, but also understand the rationality behind each treatment. The length of treatment is based on different factors. For example, vaporization should be continued for as many days as necessary until the patient is relieved, while Western treatments usually have a certain, specific, duration:
“The vaporization is not done four or five times, [it is done] until the patient comes out of the pneumonia. [Until then] you have to vaporize the patient, in the morning, in the afternoon. If he suddenly feels unwell [you have to vaporize], at noon too. And in the afternoon if the patient again feels unwell you have to perform another vaporization, until the patient feels well. There is no limit, it is until the patient gets better. You have to observe how the patient evolves. If he says: “I can’t breathe”, then we would give him another vaporization or use some Western medicine as well. You vaporize them until they are fine, until they feel well, relieved. (…), until he is already breathing well. Until he does not feel pain, the vaporization treatment continues. It is not four days, three days, but it is until he improves.” (Raúl)
Treatments based on biomedicine on the other hand have established doses and durations, as is the case with antibiotics, since they respond to another logic.
3.3 Preventive and protective practices implemented by indigenous nurse technicians
Other actions, that show the fluidity with which the nurse technicians interconnected the knowledge of both medical systems, were obvious from their practices to avoid getting infected with COVID-19. In addition to biosafety protection measures such as masks, gloves, and aprons, some nurse technicians told us that they also used plants to protect themselves from contagion, either by smelling them, bathing with them, or consuming them:
“So, before going to visit a patient, I always carried my Mucura and my Ajosacha in my hand, always smelling them. I carried them in my pocket to avoid the disease, because these medicinal plants have the property of protecting against many diseases. In other words it is as if they were a shield. In order to defend myself against this disease, I smelled and brought the plants with me.” (Raúl)
“Before you get COVID-19, you have to make a medicine out of: garlic, lemon, honey and take it before you get it [COVID-19]. After that they are boiled and combined with lemon, with red pinion (Jatropha gossypifolia L.) and put it in a big bowl, and you soak your head. That is the treatment I have been recommending in these cases. (…) The lemon leaves are also very good, before we didn’t use them so much, but now we do. Even honey with lemon, ginger, garlic, onion and everything is mixed in a pot and kept in a bottle. Every day you must take half a teaspoon, to prevent COVID, so you have [in your body] a good concentration of this. It strengthens your bones, it warms your body and protects you from COVID, it boosts your immune system.” (Oscar)
The use of medicinal plants to avoid contracting the virus and to alleviate its symptoms is something that later, when the threat of a second wave arrived, was activated:
“… we are getting ready with our medicinal plants now that the second wave is coming. Here we are prepared for the second wave. … Some people do not have these plants, some are going to buy them because they do not have any. They are procuring them and getting ready for the second wave, or they are planting. We are already prepared, we are vaporized and we are fine, the communities are taking prevention measures for COVID. In addition to talking with the promoters, I have coordinated with the authorities that we are going to prepare a plot this year to have our medicinal plants: the Mucura, the Matico… “ (Raúl)
Thus, the experiences from the different measures put into practice during the first wave of the pandemic, when there was still no significant support from the health authorities, were relevant to prepare strategies for the second wave. These incorporated, on the one hand, lessons learned from preventive treatments to strengthen the body before the virus infects you, and, on the other, practices and care, in case of an outbreak.
4 Discussion
Even though Peru has regulations and policies that promote the use of an intercultural approach in health care for the Indigenous population, the official measures implemented during the COVID-19 pandemic did not consider this approach, showing that having regulatory mechanisms alone is insufficient (12). We argue that what is needed to ensure Indigenous people receive the health care they deserve, is having a workforce prepared to put such intercultural measures into practice, especially, but not exclusively, during a crisis such as the pandemic and at the Primary Health Care level.
A report from the Pan American Health Organization states that during the COVID-19 pandemic, the health systems in Latin America “turned to try to create, albeit late, hospital care measures, forgetting primary care and access of Indigenous peoples to health services respecting economic, social, spiritual, cultural aspects and the issue of quality” (13). The lack of specific public health policies for Indigenous people during the pandemic that resulted in many preventable deaths, showcases the disconnection between the Indigenous and the official public health systems. While Indigenous people and health workers certainly need governmental support to address the most complicated cases, it is notable that no spaces were created to facilitate or recognize that Indigenous medical systems also have strategies to prevent and treat some of the symptoms caused by COVID-19, as shown in our study. As Menendez argues, the health mandates for the prevention of COVID-19 in Latin America were based exclusively on biomedical concepts and resources, ignoring Indigenous knowledge and the possibility that both knowledge systems could work together (14).
In our study we show that Indigenous nurse technicians trained in intercultural health, who provided care in remote Indigenous communities in the Peruvian Amazon during the first wave of the pandemic were in fact capable of bringing together elements of the Western and the Indigenous medical systems. Their testimonies presented here underline the value of Indigenous-led intercultural training programs (such as the one implemented by AIDESEP), which allow for culturally appropriate Primary Health Care, especially given the lack of information, medicines, or protection supplies for COVID-19. The nurse technicians sought to understand COVID-19 using conceptualizations from both medical systems, and at all times tried to learn the best way to alleviate symptoms and prevent new infections. Furthermore, they also worked to learn from those Indigenous healers who shared their treatments with them. The care provided by the nurse technicians thus, specifically addressed the symptoms, and the apparently high acceptance by the Indigenous patients may have led – as a basis for treatment success - to a high compliance with therapies. While Indigenous peoples of the Amazon basin suffered disproportionately from the impacts of the COVID-19 pandemic (15), it can be suspected that the number of fatalities due to the disease would have been significantly higher without the intercultural health care given by Indigenous experts, including nurse technicians.
Studies in the Peruvian Amazon have documented the use of medicinal plants by other Indigenous groups during the COVID- 19 pandemic (16–18). For example, a study among the Urarina of Loreto reported on the use of plants for preventing or combating COVID-19 symptoms or to heal or strengthen the spirit against COVID-19 and other diseases (18). Similar to results from our interviews, plants used to alleviate COVID-19 symptoms were also commonly used to treat flu-like symptoms and fever (18). Furthermore, media reports about the use of medicinal plants by Indigenous Amazonians during the COVID-19 pandemic in Ecuador (19–21), Brazil (22) and Colombia (23) suggest that, while our study is based on a small sample (six nurse technicians), their experiences are representative of the COVID-19 response amongst Indigenous communities in the Amazon.
Beyond the medical practices, the interviews with these nurse technicians, demonstrate the significant and successful efforts of the Indigenous nurse technicians to coordinate with the community authorities and the health promoters, and to disseminate information on the preventive and curative treatments they learned to use. They also made an important contribution in ensuring that the government at least provided minimum health care. The actions developed by the nurse technicians are aligned with basic values of Primary Health Care such as solidarity, participation, sustainability, and ability to respond to the needs of the population (24). Their measures to care for patients and prevent new infections leave us with some reflections on those elements that should have been activated to support local self-care strategies in places where there are various forms of care and where medical knowledge from different health systems is synthesized to care for the sick and to explain the causes of the disease (14). Furthermore, the experiences narrated by the nurse technicians also point to the need of giving official recognition to the promotores who play a key role in the health of Indigenous communities on a voluntary basis, and who were essential during the COVID-19 pandemic (25).
Our interviews reveal that bridging different medical knowledge systems is not a rigid process, but a flexible one, and we provide strong evidence that flexibility is precisely what is required to face future pandemics, crises or health emergencies in contexts of medical pluralism. The experiences of the nurse technicians reported here may thus set the stage for a future intercultural health care strategy in Indigenous communities. However, for this endeavor to be successful, care should be taken to avoid presenting the Indigenous health system as opposite to, antagonistic or in competition with the Western biomedical system on which public health services are based on (26). Furthermore, the testimonies collected, show the actions of Indigenous health personnel and the value of their training with an intercultural approach.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not provided for this study on human participants because this work was done in the context of the COVID-19 pandemic and the IRB of our local institution was experiencing delays from the disruption caused by the lockdown. The first conversations with participants were done based on our concern for their safety and to learn about their needs as health care workers. When we asked them about the possibility of recording their experiences as part of a research process, they were eager to share. Oral informed consent was obtained and recorded after explaining the goal of the research, the volunteer nature of their participation, the measures to ensure anonymity, and discussed the potential harm and ways in which results will be shared. Written informed consent was not provided because all interviews were done via telephone calls.
Author contributions
MP, CP and CH contributed to conception and design of the study. MP and CP collected, organized and analyzed the data for interpretation. MP wrote the first draft of the manuscript and CP provided extensive feedback on that first draft. CH and CM critically reviewed subsequent drafts of the manuscript and provided important intellectual feedback and comments. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was possible thanks to the Swiss Programme for Research on Global Issues for Development (r4d programme) funded by the Swiss National Science Foundation grant IZ08Z0_177385.
Acknowledgments
We want to acknowledge all the intercultural nurse technicians who amidst all their responsibilities and difficulties, including losing colleagues, friends and family members to COVID-19, were willing to share their experiences with us.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Defensoría del Pueblo. Informe defensorial 169. Lima, Peru: La defensa del derecho los pueblos indígenas una salud intercultural (2015).
2. Maguiña-Vargas C. El COVID-19 en el Perú. Rev Soc Peru Med Interna. (2020) 33(4):129–31. doi: 10.36393/spmi.v33i4.558
3. Defensoría del Pueblo. Informe 134. la salud de las comunidades nativas: un reto para el estado. Lima, Peru: Defensoría del Pueblo (2008).
4. Alcazar L. Las brechas que perduran: una radiografia de la exclusion social en Peru. Lima, Peru: Grupo de Analisis Para el Desarrollo (GRADE) y Banco Interamericano de Desarrollo (BID (2019).
5. INEI. III censo de comunidades nativas 2017. resultados definitivos. tomo I Vol. 1. . Lima, Peru: Instituto Nacional de Estadistica e Informatica (2018).
6. Cardenas Palacios C. A agência indígena amazônica na pandemia de covid-19 no Peru. Wamon - Rev Alunos Programa Pós-grad Em Antropol Soc UFAM. (2021) 6(2):89–107. doi: 10.29327/217579.6.2-8
7. Ministerio de Salud del Peru. Situación del COVID-19 en el Perú. CDC MINSA. Available at: https://www.dge.gob.pe/portalnuevo/covid-19/situacion-del-covid-19-en-el-peru/. Accessed on: March 12, 2023.
8. Cardenas C, Pesantes MA, Rodríguez ,A. Interculturalidad en salud: reflexiones a partir de una experiencia indígena en la amazonía peruana. Anthropologica (2017) XXXV(39):151–69. doi: 10.18800/anthropologica.201702.007
9. Cárdenas CG, Pesantes MA. Entrecruzando ríos: sistematización de la propuesta pedagógica de formación de enfermeros técnicos en salud intercultural de AIDESEP. Lima, Peru: Instituto de Estudios Peruanos y Asociación Interétnica de Desarrollo de la Selva Peruana (2017).
10. Atalaya M de. Municipalidad provincial de atalaya . Municipalidad de atalaya. Available at: https://muniatalaya.gob.pe.
11. AIDESEP. Atalaya: miles de indígenas exigen soluciones y trato con presidente vizcarra - AIDESEP (2018). Available at: https://aidesep.org.pe/noticias/atalaya-miles-de-indigenas-exigen-soluciones-y-trato-con-presidente-vizcarra/.
12. Pesantes MA, Gianella C. ¿Y la salud intercultural?: lecciones desde la pandemia que no debemos olvidar. Mundo Amaz. (2020) 11(2):93–110. doi: 10.15446/ma.v11n2.88659
13. OPS. El Impacto de la COVID-19 en los pueblos indigenas de la region de las americas. perspectivas y oportunidades. informe de la reunion regional de alto nivel. Santiago de Chile, Chile: Organizacion Panamericana de la Salud OPS (2021).
14. Menéndez EL. Consecuencias, visibilizaciones y negaciones de una pandemia: los procesos de autoatención. Salud Colect. (2020) 16:e3149. doi: 10.18294/sc.2020.3149
15. Defensoría del Pueblo. Informe de adjuntía N°001-2020-DP/AMASPPI/PPI, “COVID -19: recomendaciones para un plan de atención con pertinencia cultural para los pueblos indígenas de loreto. Lima: Defensoría del Pueblo (2020).
16. Araujo Usseglio V. Haciendo frente a la COVID-19 desde las comunidades en nuestra amazonía. Derecho Ambiente y Recursos Naturales (2021). Available at: https://dar.org.pe/haciendo-frente-a-la-covid-19-desde-las-comunidades-en-nuestra-amazonia/. Accessed on: November 14, 2022.
17. Chacón L. Comando matico y su aporte para atender a indígenas contagiados por COVID-19. SPDA Actualidad Ambiental (2020). Available at: https://www.actualidadambiental.pe/comando-matico-y-su-aporte-para-atender-a-indigenas-contagiados-por-covid-19/. Accessed on: November 14, 2022.
18. Del-Aguila-Villacorta M, Martín-Brañas M, Fabiano E, Zárate-Gómez R, Palacios-Vega JJ, Nuribe-Arahuata S, et al. Plantas usadas para combatir la pandemia del COVID-19 en una comunidad indígena urarina del departamento de loreto, Perú. Folia Amaz. (2021) 30(1):87–106. doi: 10.24841/fa.v30i1.542
19. Riederer R. Fighting COVID-19 in the Amazon, with herbs and the Internet. (2020). The New Yorker. Available at: https://www.newyorker.com/news/news-desk/fighting-covid-19-in-the-amazon-with-herbs-and-the-internet. Accessed: April 13, 2023.
20. Kaleidos Collective. Experiencing covid-19 in the Ecuadorian Amazon rainforest. ACM Interact. Available at: https://interactions.acm.org/enter/view/experiencing-covid-19-in-the-ecuadorian-amazon-rainforest. Accessed on: April 13, 2023.
21. Constante S. Cómo usan los indígenas las plantas medicinales para aliviar los síntomas del coronavirus. El País: Planeta Futuro (2020). Available at: https://elpais.com/planeta-futuro/2020-10-26/lo-que-pueden-aportar-las-plantas-medicinales-a-la-lucha-contra-el-coronavirus.html.
22. Hindustan Times. In Brazil’s Amazonas, plants used to counter COVID-19 symptoms (2020). Available at: https://www.hindustantimes.com/photos/world-news/photos-in-brazil-s-amazonas-plants-used-to-counter-covid-19-symptoms/photo-sqeIHd8iJ93mMv4ZufixXL.html.
23. Carranza Jimenez DC. La medicina tradicional con la que los pueblos indígenas de Colombia hacen frente al COVID-19 (2020). Available at: https://www.aa.com.tr/es/mundo/la-medicina-tradicional-con-la-que-los-pueblos-indígenas-de-colombia-hacen-frente-al-covid-19/1858464.
24. OPS. Renovacion de la atencion primaria de salud en las americas. Washington DC: Documento de Posicion de la Organizacion Panamericana d e la Salud/OMS (2005). Organizacion Panamericana de la Salud20-.
25. Cardenas C. Promotores de salud, una alternativa para atender el COVID-19 en las comunidades indígenas (2020). Available at: https://redaccion.lamula.pe/2020/08/09/promotores-de-salud-una-alternativa-para-atender-el-covid-en-las-comunidades-indigenas/redaccionmulera/.
Keywords: COVID-19, Indigenous people, intercultural (studies), Peru, Primary Health Care (PHC)
Citation: Pesantes MA, Cardenas Palacios C, Hewlett C and Maake C (2023) Primary Health Care in the Peruvian Amazon during COVID-19: perspectives from Indigenous nurse technicians. Front. Trop. Dis 4:1119499. doi: 10.3389/fitd.2023.1119499
Received: 08 December 2022; Accepted: 17 April 2023;
Published: 28 April 2023.
Edited by:
Ida Kolte, Oswaldo Cruz Foundation (Fiocruz), BrazilReviewed by:
Luciana Vitorino, Goiano Federal Institute (IFGOIANO), BrazilAmy Yomiko Vittor, University of Florida, United States
Copyright © 2023 Pesantes, Cardenas Palacios, Hewlett and Maake. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. Amalia Pesantes, bWFyaWEuYW1hbGlhLnBlc2FudGVzQGdtYWlsLmNvbQ==
†ORCID: Cynthia Cardenas, orcid.org/0000-0001-6621-2020
 M. Amalia Pesantes
M. Amalia Pesantes Cynthia Cardenas Palacios2†
Cynthia Cardenas Palacios2† Caroline Maake
Caroline Maake