- 1Department of Chinese Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan
- 2School of Post-baccalaureate Chinese Medicine, Tzu Chi University, Hualien, Taiwan
- 3Department of Dermatology, MacKay Memorial Hospital, Taipei, Taiwan
- 4Department of Medicine, MacKay Medical College, New Taipei City, Taiwan
Background: Uremic pruritus causes sleep disturbances, poor quality of life, and increased morbidity in patients with chronic kidney disease. Acupuncture has been shown to improve uremic pruritus. There is limited evidence of the efficacy of traditional Chinese therapies. We conducted a systematic review and meta-analysis to evaluate the efficacy of acupoint stimulation therapy in patients with uremic pruritus.
Methods: A systematic search of seven databases (up to Sep 2022) was conducted for randomized controlled trials that evaluated the clinical efficacy of acupuncture, acupressure, auricular acupressure, acupoint injection, acupoint thermal therapy, acupoint sticking therapy, or transcutaneous electrical acupoint stimulation in the treatment of patients with uremic pruritus. Two reviewers selected eligible articles for inclusion in the meta-analysis and evaluated the risk of bias via Cochrane Collaboration. The results of pruritus assessments and uremic pruritus-related laboratory parameters were analyzed.
Results: Forty trials published between 2002 and 2022, including a total of 2,735 participants, were identified for inclusion in the meta-analysis. The effective rates for acupuncture, auricular acupressure, and the combination of acupoint injection and acupoint massage were significantly greater in patients with uremic pruritus compared to the control group. The levels of serum BUN, PTH, and histamine levels were significantly lower vs. control group.
Conclusions: Acupuncture, auricular acupressure, and the combination of acupoint injection and acupoint massage seem to be effective in improving uremic pruritus in patients with chronic kidney disease. However, further investigation of these potential treatments is now warranted in larger patient populations and over a longer time frame.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022354585, identifier: PROSPERO CRD42022354585.
Introduction
Uremic pruritus (UP) is a common cutaneous change that occurs in about 55% of patients with chronic kidney disease (CKD) who are undergoing dialysis (1). The manifestation of UP varies in severity, distribution, and duration, and UP can cause sleep disturbances, depressive symptoms, quality-of-life deterioration, and increased morbidity (2). Several pathophysiologic mechanisms and factors may be involved in UP, including inflammation, high serum calcium concentration, and histamine-dependent or non-histaminergic pruritogens, such as proteases, opioids, and substance P (3). Markers of dialysis inefficiency and mineral metabolism [e.g., high levels of phosphate, calcium, parathyroid hormone (PTH), and intact parathyroid hormone (iPTH)] may be associated with an increased risk of UP (4), for which treatments include topical, systemic, and immunomodulatory therapies (2); however, some UP patients remain refractory to traditional treatments (5).
Many complementary therapies have been evaluated in patients with UP, but with variable efficacy (5). Recently, traditional Chinese therapeutic methods, namely acupuncture, auricular acupressure (AA), acupoint massage (AM), acupoint injection (AI), and acupoint thermal therapy (ATT), demonstrated benefits in patients with UP. The benefit of acupuncture may be due to increased levels of anti-inflammatory cytokines, resulting from an altered type 1 to type 2 T-helper cell balance (6). Moreover, stimulation of Quchi (LI11) significantly reduced pruritus in patients with UP (7).
AI of autologous serum stimulates a non-specific immune response and decreases sensitivity to pruritus (8). Other medications, such as antihistamines, Gastrodin, Angelica, and Salvia, have also been administered as injections. For ATT, local acupoint infrared (AIR) radiation can improve nerve sensitivity and promote peripheral blood circulation, which may help patients with UP (9). Transdermal therapeutic administration of Chinese medicines at acupoints has also ameliorated pruritus (7).
Increased the number of the mast cells is one etiology for UP (7). Mast cells degranulation could release inflammatory markers such as histamine, tumor necrosis factors, and IL-6 (10). The activation of acupressure at LI11 can destroy mast cell which releasing inflammatory markers that might be the one etiology for UP and improve pruritus (7). Electroacupuncture (EA) at ST36 suppressing the activation of mast cells, leading to decrease of nerve growth factor (NGF) and tropomyosin receptor kinase A (TrkA) proteins (6). Acupuncture at ST36 can stimulate mast cell degranulation within the acupoint area and increase pain threshold (11). Interestingly, AA affects different parts of the body, by reconditioning the meridians, and is more easily accepted by patients (12). Transcutaneous electrical acupoint stimulation (TEAS) can also decrease the severity of UP (13), and the efficacy of TEAS is not statistically significantly different from that of acupressure (14). The combination of AI with acupressure (AI+A) is used to affect the endogenous opioid system, which might decrease anxiety and insomnia caused by pruritus (15).
To explore alternative treatments for UP, we performed a systematic review of several complementary therapies: acupuncture, AA, AM, AI, ATT, acupoint sticking therapy (AST), and TEAS.
Methods
Search strategy
We searched for articles published before 29 Sep 2022 from PubMed, Embase, CINAHL, Cochrane Library, China National Knowledge Infrastructure, Airiti Library, and Wanfang databases. The search string used was based on PubMed medical subject headings and Embase subject headings (Emtree): (chronic kidney disease OR kidney injury OR kidney failure OR chronic renal failure OR end-stage renal disease OR end stage renal disease OR dialysis OR hemodialysis OR peritoneal dialysis) OR (uremic OR uremia OR uremias) AND (pruritus OR itch OR xerosis OR skin problems OR skin disorders) AND (acupuncture OR acupressure OR Shiatsu OR Zhi Ya OR Chih Ya OR Shiatzu OR auricular acupuncture OR ear acupuncture OR auricular acupressure OR ear acupressure OR auricular therapy OR auriculotherapy OR auricular needle OR otopoint OR otoneedle OR auriculoacupuncture OR otopuncture OR acupressure point OR acupoints OR Tui Na).
We also searched for word combinations and free-text phrases containing the terms above and extended the search using the “related articles” function in PubMed. Further, all the retrieved abstracts, studies, and citations were reviewed. Finally, unpublished studies were obtained from the ClinicalTrials.gov registry (16). There were no language restrictions in the search. This systematic review and meta-analysis were registered online with PROSPERO, the international prospective register of systematic reviews of the National Institute for Health Research (ID: CRD42022354585) (17). The search protocol is attached in Supplementary material.
Study selection
Randomized controlled trials (RCTs) were chosen to assess the efficacy of acupuncture, AA, AM, acupoint far infrared (AFIR), AI, AIR, AST, acupoint ion implantation, and transcutaneous electrical acupoint stimulation (TEAS) in the treatment of patients with UP. The inclusion criteria were: chronic kidney disease under dialysis; the presence of UP; administration of a specified treatment; and the availability of quantitative data for itch severity. If necessary, we contacted study authors for original or missing data. For studies with overlapping data, we selected those with the largest populations to exclude duplicate articles.
Data extraction and quality assessment
Two reviewers independently screened the articles and extracted the following information: first author; publication date; participant characteristics; study design; inclusion, exclusion, and matching criteria; AA, AM, AFIR, AI, AIR, AST, or ATENS therapy; and quantitative data for itch severity. In line with the inclusion criteria, the two reviewers assessed the chosen articles for eligibility, and the reviewers' comments were recorded and compared. Any disagreements were submitted to, and reviewed by, a third investigator. Further, we performed a quality assessment of the studies using the “risk of bias” tool recommended by the Cochrane Collaboration (18). Several domains were evaluated, including method of allocation, blinding of participants and investigators, the integrity of outcome data, selective reporting, and other kinds of bias.
Risk of bias assessment
Randomization bias
All 40 studies were RCTs: 10 studies provided no information about randomization; whereas 16 studies described the methods of randomization (nine studies used tables of random numbers, eight used random number generators, one used the drawing of lots, one used blocked randomization, and one study used chart numbers) (Figure 1).
Blinding
Seven studies were double-blind, and 33 studies were unblinded.
Incomplete outcome data
Eleven studies failed to use intention-to-treat analysis. The rate of loss to follow-up was low for most studies, although 10 studies had a dropout rate of more than 5%. Ten studies were also missing more than 5% of the outcome data and lacked evidence to support that data consistency was maintained despite the missing data. Six studies had other reasons for missing data, and 4 failed to report the reason for missing data.
Data synthesis and analysis
We presented outcomes of the following tools for pruritus assessment to evaluate the efficacy of our chosen complementary therapies: visual analog scale (VAS) and numeric rating scale (NRS; 0–10 points for each scale); 5-dimensional itch scale (5DIS: 5–25 points, and comprising dimensions of degree, duration, direction, disability, and distribution of itching, with 1–5 points for each dimension); the modified Duo's pruritus score (mDuo; 0–40 points); four-item itch questionnaire [FIIQ; evaluations of pruritus localization (1–3 points), severity (1–5 points), frequency (1–5 points), and sleep disturbances due to itching (0–6 points); total 3–19 points]; Pauli-Magnus scale (PMS; 3–45 points); and Dirk R Kuypers score (DRKS; 27 points); Traditional Chinese medicine symptom scale, UP questionnaire, 12-Item Pruritus Severity Scale (12-PSS; 3–22) (19) and Serjip score (Assessment of severity and burden of pruritus) (20).
The statistical package Review Manager (version 5; Cochrane Collaboration, Oxford, England) was used for data analysis. A meta-analysis was conducted based on recommendations outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Standard deviations (SDs) were calculated from the provided confidence interval (CI) limits, standard errors, or ranges when necessary. We obtained the mean and SD from studies using the mean difference (MD) or standardized mean difference (SMD) with 95% CIs for continuous outcomes. The random-effects model was applied to pool estimates of SDs and SMDs, considering the diversity of pruritus assessment tools and possible heterogeneity across the trials. We considered heterogeneity in the studies by performing the I2 test and a null hypothesis test, in which p<0.05 confirmed significant heterogeneity among the outcomes. The Guideline Development Tool developed by the Grading of Recommendations Assessment, Development and Evaluation Working Group was applied to assign the quality of the evidence (21). All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
Results
Literature search
The selected studies were all RCTs from 2002 to 2022. A total of 2,735 patients were enrolled in the 36 studies (Figure 2). In total, we filtered out 847 citations: 62 duplicate articles, and 51 articles due to other reasons, were removed by EndNote and the reviewers; further, 734 articles were excluded following the screening criteria for titles and abstracts. We retrieved the full texts of the remaining 102 articles. After assessing for eligibility, we excluded 62 papers because 15 were reviews, 17 papers were studies conducted in patients undergoing treatments other than our chosen interventions, 18 papers were non-randomized studies, 2 papers did not focus on UP, 3 papers were conference abstracts, 6 papers were presented in the protocol, and 1 paper had incomplete data. After screening, 40 articles fulfilled the selection criteria and were included in the meta-analysis.
Study characteristics
Data for treatment frequency, duration, acupoint, the pruritus severity assessment tool, corresponding results, and follow-up duration are shown in Table 1. There were 16 studies in the acupuncture group, 13 studies in the AA group, 4 studies in the AM group, 1 study in the AI group, 1 study in the AST group, 1 study in the AFIR group, and 1 study in the ATENS group. There were 3 studies of combination therapies: two of AI+acupuncture; and one of AI+AM. Thirteen studies reported effective rates. Twenty studies reported pruritic scores including data on the VAS, mDuo, 5DIS, NRS, PMS, traditional Chinese medicine (TCM) symptom score, FIIQ, Serjip score, UP questionnaire, and DRKS.
All studies included patients with UP and CKD: in 38 studies, patients received regular hemodialysis, while in the Ding et al. and Chen et al. studies, patients underwent peritoneal dialysis and nocturnal dialysis, respectively (41, 43). There were 16 studies on acupuncture. The treatment frequency was about two to three times per week. The most common acupoint choices were Xuehai (SP10, 9 studies), LI11 (7 studies), Sanyinjiao (SP6), and Zusanli (ST36, each of these acupoints used in 7 studies). Chang et al. added citrate dialysate as UP therapy and the result revealed improved pruritus (31).
There were 13 studies of AA, and the treatment frequency was about three to eight times per day. The meridian in these studies included lung, kidney, heart, stomach, endocrine, subcortical, supracortical, adrenal, and Shenmen (TF4). Chen et al. also compared nocturnal dialysis with hemodialysis (41), and Lin et al. compared the efficacy of AA, fumigation, and the combination of AA+fumigation therapy (45), and Yu et al. used copper scraping therapy at auricular acupoint (35).
There was one study of AFIR, and the treatment frequency was once per day, on 2 days each week. The acupoint used for AFIR was SP6. There was one study of AI, for which the treatment frequency was twice per week. Wang et al. used gabapentin as a control arm, and the acupoints used were LI11 and ST36 (50). There was one study of AIR, in which the treatment frequency was twice per week, and in which the acupoints used were LI11, SP6, and SP10. There were four studies of AM, with a treatment frequency of three times per week, and with acupoints of SP6, SP10, ST36, and LI11. Chen et al. compared high-flux HD with AM+high flux HD in 12-PSS score (54). There was one study of AST, in which the treatment frequency was once every 2 days: that is, Jiu et al. used Di Fu Zi, Tu Si Zi, Mud An Pi, and Tao Ren as TCMs in sticking therapy applied at the umbilicus (56).
Four studies evaluated complementary-therapy combinations: AI+A (n = 2), AI+AM (n = 1), and AM+TEAS (n = 1). Deng et al. assessed AI+A with cetirizine and treated patients twice each week; the acupoints used were LI11, ST36, and SP10 (51). Wang et al. assessed AI+AM twice each week, or three times every 2 weeks; the acupoints used were Jianneiling (EM40), Fengshi (GB31), Hegu (LI4), LI11, ST36, SP6, Yinlingquan (SP9), and SP10 for AM, and Geshu (BI17) and Shenshu (BI23) for AI (52). Chen et al. evaluated AI+AM two to three times per week to treat UP; the acupoints used for AI were LI11 and ST36, and those used for AM were Dazhu (DU14), Shangxing (DU23), Sishencong (EM1), Yintang (EM2), Shenmen (HT7), Fengchi (GB20), LI4, SP6, SP10, and Ximen (PC4) (53).
Pruritus assessments
Visual analog scale (VAS) score
Meta-analysis of the 15 studies with VAS score assessments (Figure 3A) showed statistically significant experimental–control group improvements in VAS score for acupuncture (MD −2.58; 95% CI: 4.29, −0.87; p = 0.003), AA (MD −1.53; 95% CI: −1.82, −1.24; p < 0.00001), AI (MD −1.03; 95% CI: −1.54, −0.52; p < 0.0001), AI+AM (MD −2.04; 95% CI: −2.73, −1.35; p < 0.00001), AIR (MD −1.85; 95% CI: −3.42, −0.28; p = 0.02), AM (MD −1.72; 95% CI: −2.83, −0.61; p = 0.002), and TEAS (MD −1.96; 95% CI: −3.01, −0.91; p = 0.0003). No statistically significant improvement was evident for AFIR (MD 0.01, 95% CI: −0.66, 0.68; p = 0.98) or AST (MD −0.42; 95% CI: −0.96, 0.13; p = 0.13). Nonetheless, for all 15 studies combined, a significant decline in VAS score was evident in the experimental vs. control group (MD −1.64; 95% CI: −2.16, −1.11; p < 0.00001), with significant heterogeneity among the studies (I2 86%; p < 0.00001).
Figure 3. Forest plot comparison of pruritus scores on (A) visual analog scale, (B) Pauli-Magnus scale, (C) modified Duo's pruritus score, and (D) Dirk R. Kuypers scale in patients with uremic pruritus treated with acupuncture. CI, confidence interval; df, degrees of freedom; IV, independent variable; SD, standard deviation.
Pauli-Magnus scale (PMS) score
Significant experimental–control group decreases in PMS scores (Figure 3B) were also noticed in three studies that included a total of 189 patients with UP (overall MD −9.38; 95% CI: −18.09, −0.66; p = 0.03), with significant heterogeneity among the studies (I2 99%; p < 0.00001).
Modified Duo's (MDuo) pruritus score
Two studies in a total of 109 patients with UP showed no statistically significant overall improvement in mDuo score (Figure 3C) in the experimental vs. control group (MD −9.75; 95% CI: −21.50, +2.01; I2 96%; p = 0.10).
Dirk R. Kuypers scale (DRKS) score
Two studies in a total of 163 patients with UP showed no statistically significant overall improvement in DRKS score (Figure 3D) in the experimental vs. control group (MD −5.25; 95% CI: −11.49, +0.98; I2 97%; p = 0.10).
Effective rate
Nine studies recorded the number of patients that became better after the therapies. For acupuncture, three individual studies showed statistically significantly higher efficacy in the treatment vs. the control group [risk ratio (RR) 4.78–14.87; Figure 4]. Overall results for acupuncture (RR 1.48; 95% CI: 1.32, 1.66), AA (RR 1.27; 95% CI: 1.14, 1.41), and AI+AM (RR 1.35; 95% CI: 1.02, 1.79) all showed increased efficacy relative to control; among these complementary therapies, improvements were statistically significant for acupuncture (p < 0.00001), AA (p < 0.0001) and AI+AM (p = 0.04). Although AI + acupuncture showed no significant improvement in efficacy relative to control, the complementary therapies evaluated demonstrated significantly improved overall efficacy vs. control (RR 1.31; 95% CI: 1.23, 1.40; p < 0.00001).
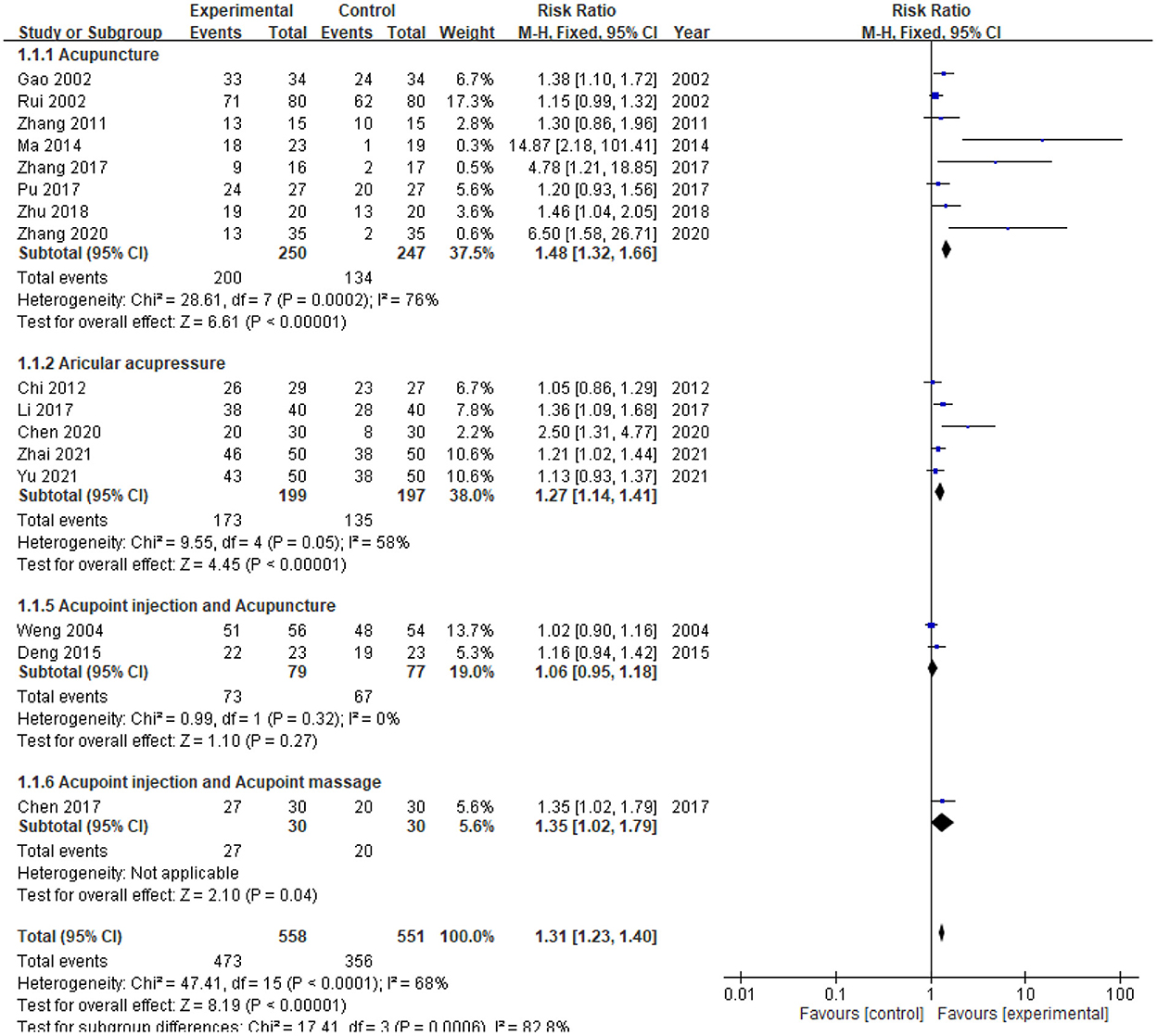
Figure 4. Forest plot comparison of effective rates in patients with uremic pruritus treated with acupuncture or related therapies. CI, confidence interval; df, degrees of freedom; M-H, Mantel-Haenszel.
Laboratory parameters
The table of serum data from the collected studies was attached in the Supplementary material. Statistically significant overall improvement vs. control were noted, and with mild to high heterogeneity, for the complementary therapies evaluated, regarding BUN (MD −0.85; 95% CI: −1.46, −0.24; p = 0.006; Figure 5), PTH (MD −29.18; 95% CI: −48.19, −10.18; p = 0.003), and histamine levels (MD −1.18; 95% CI: −1.62, −0.73; p < 0.0001). Changes in serum creatinine, phosphate, calcium, β2-microglobulin, C-reactive protein, hemoglobin, white blood cell count, and alkaline phosphatase were not statistically significant (p>0.05 for each; moderate to high heterogeneity).
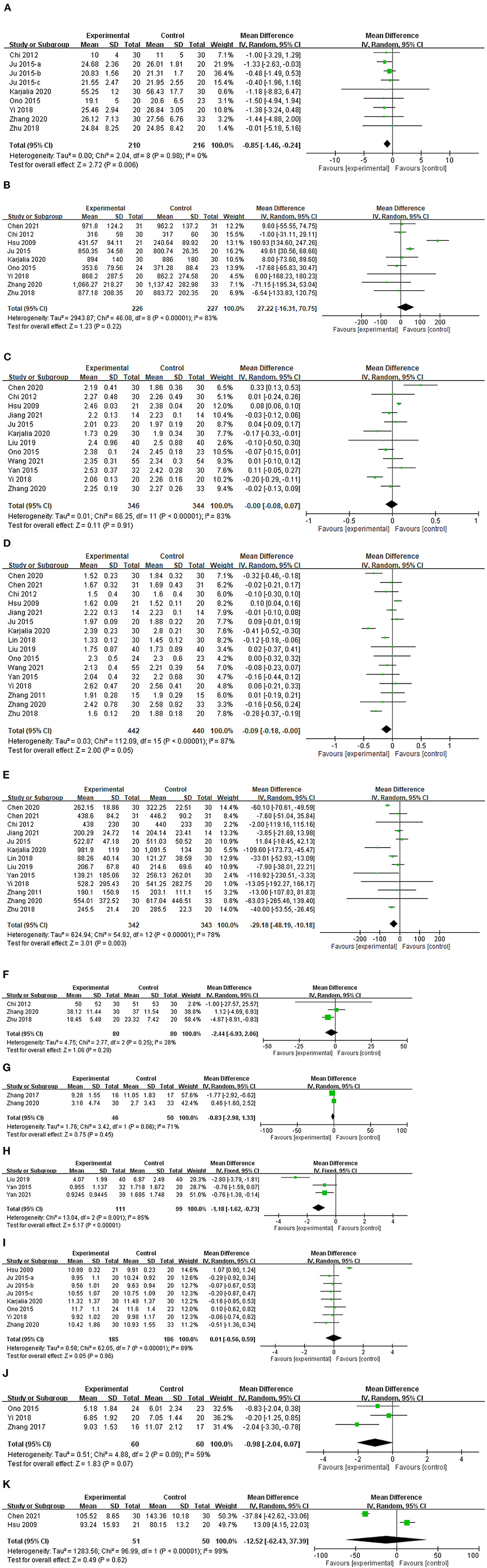
Figure 5. Forest plot comparison of serum levels of (A) blood urea nitrogen, (B) creatinine, (C) calcium, (D) phosphate, (E) parathyroid hormone, (F) β2-microglobulin, (G) C-reactive protein, (H) histamine, (I) hemoglobin, (J) white blood cells, and (K) alkaline phosphatase in patients with uremic pruritus treated with acupuncture or other related complementary therapies. CI, confidence interval; IV, independent variable; SD, standard deviation.
Discussion
In our review, acupoint acupuncture, AA, AI, AM, AIR, TEAS, and AI+AM statistically significantly improved mean VAS scores for pruritus in patients with UP (9, 12, 14, 27, 29, 34, 40, 42–44, 50, 53). Decreased mean PMS scores for treatment vs. control were noted in three studies: one study about acupuncture, and two about AA (5, 39, 44). Sixteen studies recorded effective rates for acupuncture, AA, acupuncture + AI, and AI+AM: results revealed significantly greater efficacy than control for acupuncture (RR 1.48; 95% CI: 1.32, 1.66), AA (RR 1.32; 95% CI: 1.00, 1.46), and AI+AM (RR 1.35; 95% CI: 1.02, 1.79) (25, 29, 30, 33, 34, 36–38, 41, 46, 48, 51, 53). In large populations, especially, small changes may be statistically significant, but can be irrelevant clinically. The minimal clinically important difference (MCID) is defined as the smallest change in any scale scoring that can be noticed by the patient (57). Several methods exist for determining MCID; however, currently no universal rule is established. Reich et al. suggested that the MCID for clinical improvement in itch, as rated on the VAS and NRS, ranks between a decrease of 2–3 points (57). Claudia et al. found MCID of 192 patients that the very severe baseline pruritus (>9) had to be reduced by at least 4.56 points, and the severe pruritus (7 to <9) by at least 3.65 (58). In our article, improvement of VAS is modest to minor, although statistically significant after pooling to meta-analyze the expanded study population.
Traditionally, acupuncture has been reported as a safe and effective treatment for pruritus, and has been used in China for many years (59). Yan et al. reported that acupuncture significantly reduced pruritus scores in hemodialysis patients with UP (60). Generally, the most frequently used method was manual acupuncture, although TEAS and auricular acupuncture have also been used for UP (14).
In our acupuncture group, the most common acupoint choices were SP10 (eight studies), LI11 (seven studies), SP6, and ST36 (each of these acupoints used in six studies) (5, 22, 25–34, 37, 38). EA at LI11 and SP10 could improve pruritus due to reducing the expression of TLR2, TLR4, MyD88 and NF-κB which increased in the morphine-induced pruritus model mice (61). Cold stimulation (20°C) at LI11 in compound 40/80-induced mice showed decreased c-fos expression in the dorsal horn at C2-C7 and decreased scratching bouts (62). The treatment frequency was about two to three times per week and decreased VAS, PMS, and DRKS scores confirmed the efficacy of the acupuncture. Overall, VAS scores showed significant improvements vs. control for acupuncture, AA, AI, AM, AIR, ATENS, and AI+AM (9, 12, 14, 27, 29, 34, 40, 42–44, 50, 53). Three studies revealed a significant decline in PMS scores, but with significant heterogeneity among the studies (I2 99%; p < 0.00001) (5, 39, 44). Ma et al., Zhang et al., and Chang et al. all reported improved effective rates after acupuncture therapies compared with control (25, 31, 33). Regarding complications, Che et al. used acupuncture at SP6, SP10, ST36, and LI11 in 40 patients and could report that 2 patients (one in acupuncture group, another in control group) complained about elbow soreness and 3 patients in the control group complained about minimal bleeding induced by acupuncture (5). Phan et al. performed 216 times (12× in 18 patients) in patients undergoing hemodialysis who received heparin. Bleeding was observed in 13 patients after the needle was removed from the spot, and the bleeding was mild and could be controlled with the use of cotton and the application of pressure. No serious cases of bleeding occurred. Hematoma, which occurred after bleeding, was observed in four (1.85%) patients. However, the hematoma disappeared without any therapy within 3–10 days (28).
Auricular acupoints affect the functioning of the visceral organs and meridians, skeleton, and limbs, and AA proved to be a useful treatment for UP in patients with end-stage renal disease (60). Indeed, in patients undergoing hemodialysis, AA had a beneficial effect on conditions such as sleep disorders, depression, pruritus, and xerostomia (63). Karjalian et al. reported improved pruritus in a study that evaluated AM as a treatment for UP (7), and PMS scores improved after AA in studies conducted by Mai et al. and He et al. (39, 44). For AA, the treatment frequency in studies in our review was about three to eight times per day, and the meridians used included lung, kidney, heart, stomach, endocrine, subcortical, supracortical, adrenal, and TF4. One study used auricular acupoint scraping therapy for UP patients (35). Scraping stimulation makes subcutaneous capillaries expand or break, creating skin eruptions with flush or purple-red skin, miliary and papuloid spots, patchy and stripy plaques, and local hot sensation or mild pain. Skin eruptions can improve blood circulation, promote cell metabolism, and strengthen immunity to cure diseases and promote recovery (64). Overall, AA produced significant relief of symptoms, and significantly improved effective rates, relative to control (39, 44).
AI uses a syringe needle instead of an acupuncture needle at acupoints (50). AI achieved the same or higher plasma concentrations than the intravenous injection of carbamyl β -methylcholine chloride injection at ST36 and femoral vein (65). There was a significantly increased phylloquinone plasma concentration found in a study of AI at SP6 as the trigger point (66). Several clinical studies have shown that AI has definite advantages and reliable curative effects for the treatment of pruritis in patients with CKD (51–53, 67).
AM stimulates the meridian points by pressure applied with the fingertips, palms, small beads, or special devices (68). The pressure on acupoints could promote blood circulation and neurotransmitter secretion (7). Chen et al. combined AI with AM for patients with UP and reported improved efficacy relative to a control group (53).
Thermal (including infrared and far infrared) therapy has been used to treat pain, depression, dysmenorrhea, and coronary vascular endothelial dysfunction (49). Far infrared radiation has a wavelength of 4–1,000 μm and can penetrate the subcutaneous tissues; as such, it may improve blood flow and endothelial and nervous-system function (49). Infrared rays can provide local warmth around acupoints and can have a similar effect to acupuncture; such rays may improve skin blood flow and the functioning of the cutaneous nervous system (69). Yi et al. found that AIR is effective in the treatment of UP, as evident from improvements in VAS and sleep quality scores (9).
Umbilical AST may increase immune function and amplify the effect of Traditional Chinese Medicine (TCM) (56). Indeed, for medications applied at the umbilical acupoint, bioavailability may be increased up to 6-fold (56). Jiu et al. used several Chinese medications with antioxidant and antiallergic properties and reported significantly improved VAS scores after AST (p < 0.01) (56).
Akca et al. assessed acupressure and TEAS applied at acupoint LI11 (14); TEAS provides a faint electrical current and causes a small amount of pressure at the acupoint. The researchers reported a significant decrease in pruritus severity, as evident from a significant improvement in the mean VAS score (p = 0.0003) (14).
Patients with UP have higher serum levels of iPTH, hemoglobin, BUN, and high-sensitivity C-reactive protein rather than patients without UP (70). In our results, there were significant decreases in serum BUN, phosphate, PTH, and histamine levels in patients with UP compared with controls. Increased calcium and phosphate levels increase the stimulation of peripheral nerves in the skin; indeed, Sunita et al. found that calcium phosphate-induced pruritus was mediated by interleukin-6, Bruton's tyrosine kinase, and extracellular signal-regulated kinase signaling in a murine model (71). PTH has also been associated with mast cell activation, leading to histamine release and pruritus (72). In an experimental study, Chinese herbal medicine (CHM) and acupoint thread implantation reduced serum PTH concentration in rats with CKD (73). Stockenhuber et al. observed increased histamine levels in patients with pruritus and CKD (74), and in another study, antihistamine therapy significantly improved the mean VAS score, indicating improved control of UP (75). Importantly, increased levels of calcium, phosphate, PTH, and histamine might cause a pruritic sensation in patients with UP.
A previous meta-analysis collected data from six studies of acupuncture in UP and showed, albeit with insufficient evidence, that acupuncture and acupressure were effective in UP; the researchers included articles in English, and only three trials recorded VAS scores (68). Importantly, our analysis collected data from a total of 36 studies, without language limits, and included ten different acupuncture techniques, several pruritus scores, and overall effective rates. However, the studies included in our analysis had considerable heterogeneity because of various clinical factors: the durations of each acupuncture method varied; some inter-study discrepancies in control groups existed, and overall effective rates were measured using different pruritus scores.
There were some limitations to our analysis: first, sample sizes of the included RCTs were small; second, all the selected articles lacked long-term follow-up; and third, the therapeutic mechanisms of effect for the different acupuncture techniques in UP were unclear. Nonetheless, our analysis is one of the first to endorse the therapeutic benefit of acupuncture and related techniques in the treatment of UP in patients with CKD.
Conclusion
In summary, our meta-analysis found that acupuncture and related techniques have clinical benefits, as evident from various pruritus scores, in patients with UP. Further investigations in larger study populations and well-designed studies focusing on the dosage, frequency, and long-term effects are now warranted.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
Po-HL designed the study and critically revised the manuscript. Po-HL, C-HC, H-EC, and I-HL contributed to the literature search, data extraction, quality assessment, and writing the first draft of the article. Pi-HL and C-HC performed statistical analysis and interpreted the results. All authors contributed to this article. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the Buddhist Tzu Chi Medical Foundation, Taiwan (TCMF-CM1-111-03 and TCMF-P 111-16) and Taipei Tzu Chi Hospital (TCRD-TPE-111-45).
Acknowledgments
We thank all our colleagues at Mackay Memorial Hospital and Taipei Tzu Chi Hospital for helping with this study. We greatly appreciate technical support from the Core Laboratory of the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1036072/full#supplementary-material
References
1. Hu X, Sang Y, Yang M, Chen X, Tang W. Prevalence of chronic kidney disease-associated pruritus among adult dialysis patients: a meta-analysis of cross-sectional studies. Medicine. (2018) 97:e10633. doi: 10.1097/MD.0000000000010633
2. Verduzco HA, Shirazian S. Ckd-associated pruritus: new insights into diagnosis, pathogenesis, and management. Kidney Int Rep. (2020) 5:1387–402. doi: 10.1016/j.ekir.2020.04.027
3. Westby EP, Purdy KS, Tennankore KK. A review of the management of uremic pruritus: current perspectives and future directions. Itch. (2020) 5:e38. doi: 10.1097/itx.0000000000000038
4. Lu PH, Chuo HE, Kuo KL, Liao JF, Lu PH. Clinical efficacy and safety of sodium thiosulfate in the treatment of uremic pruritus: a meta-analysis of randomized controlled trials. Toxins. (2021) 13:769. doi: 10.3390/toxins13110769
5. Che-Yi C, Wen CY, Min-Tsung K, Chiu-Ching H. Acupuncture in haemodialysis patients at the quchi (Li11) Acupoint for refractory uraemic pruritus. Nephrol Dial Transplant. (2005) 20:1912–5. doi: 10.1093/ndt/gfh955
6. Oh JE, Kim SN. Anti-inflammatory effects of acupuncture at St36 point: a literature review in animal studies. Front Immunol. (2021) 12:813748. doi: 10.3389/fimmu.2021.813748
7. Karjalian F, Momennasab M, Yoosefinejad AK, Jahromi SE. The effect of acupressure on the severity of pruritus and laboratory parameters in patients undergoing hemodialysis: a randomized clinical trial. J Acupunct Meridian Stud. (2020) 13:117–23. doi: 10.1016/j.jams.2020.05.002
8. Wang Q, Li M, Hu X, Luo Q, Hao P. Autologous blood or autologous serum acupoint injection therapy for psoriasis vulgaris: a protocol for a systematic review and meta-analysis. Medicine. (2020) 99:e20555. doi: 10.1097/MD.0000000000020555
9. Yi JC, Zheng MX. Therapeutic effect of infrared acupoint irradiation combined with local irradiation on uremic pruritus caused by maintenance hemodiaiysis. J Yichun Univ. (2018) 40:70–2.
10. Aoki R, Kawamura T, Goshima F, Ogawa Y, Nakae S, Nakao A. Mast cells play a key role in host defense against herpes simplex virus infection through Tnf-a and Il-6 production. J Invest Dermatol. (2013) 133:2170–9. doi: 10.1038/jid.2013.150
11. Zhang D, Ding G, Shen XY, Yao W, Zhang Z, Zhang Y, et al. Influence of mast cell function on the analgesic effect of acupuncture of “Zusanli” (St 36) in rats. Acupunct Res. (2007) 32:147–52.
12. Yan CN, Yao WG, Bao YJ, Shi XJ, Yu H, Yin PH, et al. Effect of auricular acupressure on uremic pruritus in patients receiving hemodialysis treatment: a randomized controlled trial. Evid Based Complement Alternat Med. (2015) 2015:593196. doi: 10.1155/2015/593196
13. Kiliç Akça N, Taşçi S, Karataş N. Effect of acupressure on patients in turkey receiving hemodialysis treatment for uremic pruritus. Altern Ther Health Med. (2013) 19:12–8.
14. Akça NK, Taşci S. Acupressure and transcutaneous electrical acupoint stimulation for improving uremic pruritus: a randomized, controlled trial. Altern Ther Health Med. (2016) 22:18–24.
15. Lin JG, Chen WL. Acupuncture analgesia: a review of its mechanisms of action. Am J Chin Med. (2008) 36:635–45. doi: 10.1142/S0192415X08006107
16. ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/home (accessed June 22, 2021).
17. National Institute for Health and Care Research. Available online at: https://www.nihr.ac.uk/ (accessed June 23, 2021).
18. Cochrane Collaboration. Available online at: https://www.cochrane.org/ (accessed June 22, 2021).
19. Adam Reich, Agnieszka Bohek, Katarzyna Janiszewska, Szepietowski JC. 12-Item Pruritus Severity Scale: Development and Validation of New Itch Severity Questionnaire. BioMed Research International. (2017). doi: 10.1155/2017/3896423
20. Manuel Pedro Pereira, St€ander S. Assessment of severity and burden of pruritus. Allergol Int. (2017) 66:3–7. doi: 10.1016/j.alit.2016.08.009
21. Grading Grading of Recommendations Assessment Development Evaluation Working Group. (2021). Available online at: https://www.gradeworkinggroup.org/ (accessed June 22, 2021).
22. Ardinata D, Zain-Hamid R, Roesyanto-Mahadi ID, Mihardja H. Interleukin-31 serum and pruritus dimension after acupuncture treatment in hemodialysis patients: a randomized clinical trial. Open Access Macedonian J Med Sci. (2021) 9:196–201. doi: 10.3889/oamjms.2021.5599
23. Juan F. Observation on the application of integrated traditional chinese and western medicine nursing on complications after hemodialysis. GuangMing J Chin Med. (2021) 36:3167–9. doi: 10.3969/j.issn.1003-8914.2021.18.053
24. Juan JJ, Shuang YX, Yue JL, Juan Y, Yan YW, Yan C, et al. Effect of hemoperfusion combined with acupuncture on pruritus in the elderly patients with uremia. Pract Geriatr. (2021) 35:1281–3. doi: 10.3969/j.issn.1003-9198.2021.12.018
25. Zhang S. Clinical observation on the acupuncture in the treatment of skin itching due to blood deficiency and wind-drying in maintenance hemodialysis (Graduate thesis). Guangzhou University of Chinese Medicine, Guangzhou, China. (2020).
26. Liu CF. Clinical observation on acupuncture of quchi and xuehai in maintenance hemodialysis. Res Integr Trad Chin Western Med. (2020) 10:256–7. doi: 10.3969/j.issn.1674-4616.2018.05.012
27. Nahidi Y, Badiee S, Torabi S, Abbasi SZ, Nazemian F, Saki A. acupuncture effect on pruritus in hemodialysis patients: a randomized clinical trial. Iranian Red Crescent Med J. (2018) 20:1–7. doi: 10.5812/ircmj.65521
28. Phan FA, Srilestari A, Mihardja H, Marbun MBH. Effects of acupuncture on uremic pruritus in patients undergoing hemodialysis. J Phys Conf Ser. (2018) 1073:062049. doi: 10.1088/1742-6596/1073/6/062049
29. Chu LC, Hsu WC, Li CJ, Huang HH, Chen HL. Clinical Effect for Pruritus of Replenishing and Reducing Acupuncture in Maintenance Hemodialysis and the Influence of Serum Ipth and B2-Mg. Chronic Pathematology J. (2018) 19:1763–6.
30. Pu LC. Effectiveness of the acupuncture combined hemodialysis plus hemoperfusion for uremic pruritus. For All Heath. (2017) 8:109–10.
31. Chang KS, Lei TS, Ju SR, Lan S, Shiu HJ, Fei TH, et al. Improvement of uremic pruritus in hemodialysis with citric acid: 17 cases. J Jiangxi Univ Tradit Chin Med. (2017) 6:40–2.
32. Ono S, Mukaino Y. Efficacy and cost effectiveness of the acupuncture treatment using a new skin stimulus tool called m-test which is a measure based on symptoms accompanied with body movements: a pragmatic rct targeting hemodialysis patients. Evid Based Complement Alternat Med. (2015) 2015:802846. doi: 10.1155/2015/802846
33. Ma LL, Chang PJ, Ren K. treatment of uremic pruritus with acupuncture combined hemodialysis plus hemoperfusion. J Beijing Univ Tradit Chin Med. (2014) 21:28–30. doi: 10.3969/j.issn.2095-6606.2014.05.008
34. Chang F, Chiu CL, Huang HS, Fang SS, Shen Y. The effectiveness of treatment of uremic puritus with acupuncture combined hemodialysis plus hemoperfusion. J Pract Med. (2011) 27:1687–9. doi: 10.3969/j.issn.1006-5725.2011.09.068
35. Rong Y, Ting YW, Jun CR, Ni HN, Mei LX. Auricular copper scarping therapy for uremic cutaneous pruritus: 50 cases. Fujian J TCM. (2021) 52:52–4.
36. Zhai J. Observation on the effect of auricular point on skin pruritus in hemodialysis patients with uremia. Contemporary Med Symp. (2021) 18:169–70.
37. Ruei HR, Lin WM, Sha JP. Observation on therapeutic effect of 80 cases of uremic cutaneous pruritus treated with acupuncture. Chin Acupunct Moxibustion. (2002) 22:235–6.
38. Kao HM, Chang WH, Wang Y. Acupuncture for Uremic cutaneous pruritus: 34 cases. J Tradit Chin Med. (2002) 5:312.
39. Mai DY. Auricular acupressure combined hemodialysis plus hemoperfusion for uremic cutaneous pruritus. World Latest Med Inform. (2021) 21:188–92. doi: 10.3969/j.issn.1671-3141.2021.27.074
40. Yan C, Li J, Gea L. The effection of the serum level of Il-6 on patients receiving hemodialysis treatment for uremic pruritus by auricular acupressure. J Integr Tradit Western Nephrol. (2021) 22:499–502.
41. Chen D, Ou Yang TP, Wen F. Clinical observation of patients with chronic kidney disease—mineral and bone abnormalities by auricular point pressing combined with nocturnal dialysis. Yunnan J Trad Chin Med Materia Med. (2020) 41:54–6.
42. Yan C, Yau WG, Liu G, Wang H, Li J, Shia M. Observation of auricular acupressure on the pruritus of the patients in maintenance hemodialysis. Chin J Integr Tradit Western Nephrol. (2020) 21:512–4.
43. Ding JF, Yau SM, Peng W, Wang H, Wang YM, Ju BB, et al. Observation and mechanism of auricular acupressure on uremic pruritus in peritoneal dialysis. Chin J Integr Trad Western Nephrol. (2019) 19:626–7.
44. He CC, Guo JJ, Shia A, Wu LC, Jau DS, Wu SC, et al. Therapeutic effect of auricuiar acupressure on the treatment of pruritus in maintenance hemodiaiysis patients. Tradit Western Nephrol. (2018) 19:919–21.
45. Lin L. The influence of chinese medication fumigation combined auricular acupressure on cutaenous pruritus of chronic kidney disease. Chin J Integr Tradit Western Nephrol. (2018) 19:626–7.
46. Li L, Ma J. Effects of auricular points taping and pressing with nursing intervention on esrd pruritus in maintenance hemodialysis patients. J Hubei Univ Chin Med. (2017) 19:92–4. doi: 10.3969/j.issn.1008-987x.2017.06.25
47. Tao C. Analysis of auricular acupressure on uremic cutaneous pruritus in hemodialysis. J SNAKE. (2016) 28:464–5. doi: 10.3969/j.issn.1001-5639.2016.04.035
48. Shr CJ, Shiu C, Shiu TY, Tzou SL, Hu PP, Wang M. Clinical observation on treating mhd complications by hemoperfusion joint auricular acupressure. Clin J Chin Med. (2012) 4:7–9. doi: 10.3969/j.issn.1674-7860.2012.22.004
49. Hsu MC, Chen HW, Hwu YJ, Chanc CM, Liu CF. Effects of thermal therapy on uremic pruritus and biochemical parameters in patients having haemodialysis. J Adv Nurs. (2009) 65:2397–408. doi: 10.1111/j.1365-2648.2009.05100.x
50. Wang J, Liu P, Tsai BL. Acupoint injection for uremic cutaneous pruritus in hemodialysis maintenance: 55 cases. Jiangsu J Tradit Chin Med. (2021) 53:51–4. doi: 10.19844/j.cnki.1672-397X.2021.09.019
51. Deng HY. Observation of acupoint injection combined acupuncture in uremic cutaneous pruritus: 23 cases. World Latest Med Inform. (2017) 15:233–4.
52. Wang M, Shr CJ, Hsiao HH. observation of acupoint injection combined acupuncture in uremic cutaneous pruritus: 56 cases. Pract Clin J Integr Trad Chin Western Med. (2004) 4:17–8.
53. Chen GM, Du JT, Kuang H, He YC, Li J. Clinical observation on treating skin itching in maintenance hemodialysis patients by self blood acupoint injection plus point massage. Clin J Chin Med. (2017) 9:100–2. doi: 10.3969/j.issn.1674-7860.2017.23.053
54. Yao C. The efficacy of high-flux hemodialysis combined with acupoint press for uremic pruritus in hemodialysis patients. World Latest Med Information. (2021) 21:132–3. doi: 10.3969/j.issn.1671-3141.2021.97.048
55. Jedras M, Bataa O, Gellert R, Ostrowski G, Wojtaszek E, Lange J, et al. Acupressure in the treatment of uremic pruritus. Dial Transpl. (2003) 32:8–10.
56. Jiu SG, Li YS, Li WY, Jin F, Miau HD. Umbilical acupoint sticking therapy combined different blood purification methods on cutaneous pruritus in hemodialysis patients. Gansu Zhongyi Xueyuan Xuebao. (2015) 32:44–7.
57. Adam Reich, Claudia Riepe, Ständer S. Itch assessment with visual analogue scale and numerical rating scale: determination of minimal clinically important difference in chronic itch. Acta Derm Venereol. (2016) 96:978–80. doi: 10.2340/00015555-2433
58. Riepe C, Osada N, Reich A, Augustin M, Zeidler C, Ständer S. Minimal clinically important difference in chronic pruritus appears to be dependent on baseline itch severity. Acta Derm Venereol. (2019) 99:1288–90. doi: 10.2340/00015555-3332
59. Yao Q, Li S, Liu X, Qin Z, Liu Z. The effectiveness and safety of acupuncture for patients with chronic urticaria: a systematic review. Biomed Res Int. (2016) 2016:5191729. doi: 10.1155/2016/5191729
60. Yan CN, Yao WG, Bao YJ, Shi XJ, Yu H, Yin PH, et al. Auricular acupressure for uraemic pruritus – a treatment in search of a problem. Focus Altern Complem Ther. (2015) 21:27–8. doi: 10.1111/fct.12231
61. Yea YS, Panb AZ, Zhenc Y, Kangc MR, Zhangc B, Yi WM. antipruritic effects of electroacupuncture on morphine-induced pruritus model mice through the Tlr2/4-Myd88-Nf-κb pathway. Neuroreport. (2019) 30:331–7. doi: 10.1097/WNR.0000000000001203
62. Tsai K-S, Chen Y-H, Chen H-Y, Shen E-Y, Lee Y-C, Shen J-L, et al. antipruritic effect of cold stimulation at the quchi acupoint (Li11) in mice. BMC Complement Altern Med. (2014) 14:341. doi: 10.1186/1472-6882-14-341
63. Yang T, Wang S, Zhang X, Liu L, Liu Y, Zhang C. Efficacy of auricular acupressure in maintenance haemodialysis patients: a systematic review and meta-analysis. J Clin Nurs. (2021) 31:508–19. doi: 10.1111/jocn.15966
64. Wang Y, Yang L, Yang J, Yang J, Liu Z, Chen F, et al. Curative effect of scraping therapies on lumbar muscle strain. J Tradit Chin Med. (2013) 33:455–60. doi: 10.1016/S0254-6272(13)60148-X
65. Wang Y-M, Gao J-H, Lu B, Peng J, Bin F, Cui J-J, et al. Comparison of the effects of carbamyl-B-methylcholine chloride administered by intravenous, intramuscular and intra-acupuncture point injections. J Tradit Chin Med. (2012) 32:93–8. doi: 10.1016/S0254-6272(12)60039-9
66. Maria T Chao, Christine M Wade, Booth SL. Increase in plasma phylloquinone concentrations following acupoint injection for the treatment of primary dysmenorrhea. J Acupunct Meridian Stud. (2014) 7:151–4. doi: 10.1016/j.jams.2014.01.004
67. Yang T, Zhao J, Guo Q, Wang Y, Si G. acupoint injection treatment for non-dialysis dependent chronic kidney disease: a meta-analysis of randomized controlled trials. Medicine. (2020) 99:e23306. doi: 10.1097/MD.0000000000023306
68. Aval SB, Ravanshad Y, Azarfar A, Mehrad-Majd H, Torabi S, Ravanshad S. A systematic review and meta-analysis of using acupuncture and acupressure for uremic pruritus. Iranian J Kidney Dis. (2018) 12:78–83.
69. Yang C-C, Lin G-M, Wang J-H, Chu H-C, Wu H-T, Chen J-J, et al. Effects of combined far-infrared radiation and acupuncture at St36 on peripheral blood perfusion and autonomic activities. Evid Based Complement Altern Med. (2017) 2017:1–7. doi: 10.1155/2017/1947315
70. Zhao J-H, Zhu Q-S, Li Y-W, Wang L-L. Determinants of the intensity of uremic pruritus in patients receiving maintenance hemodialysis: a cross-sectional study. Determin Intens Uremic Pruritus Hemodial Patients. (2021) 20:1–14. doi: 10.1371/journal.pone.0245370
71. Keshari S, Sipayung AD, Hsieh C-C, Su L-J, Chiang Y-R, Chang H-C, et al. Il-6/P-Btk/P-Erk signaling mediates calcium phosphate–induced pruritus. FASEB J. (2019) 33:12036–46. doi: 10.1096/fj.201900016RR
72. Bai Y-F, Wang C-L, Xu M-Z, Pan M-J, Sun Q-Y, Chen R-M. The clinical effectiveness and safety of traditional chinese medicine uremic clearance granule combined with high-flux hemodialysis in the treatment of uremic pruritus. Chin Commun Doctors. (2020) 36:128–9. doi: 10.1097/MD.0000000000026423
73. Chen K, Shi J, Lü M, He Z, Qin R. Effects of acupoint thread implantation and Chinese herb on Pth and Tgf-Beta1 in the rate of chronic renal failure. Zhongguo Zhen Jiu. (2006) 26:511–4.
74. Stockenhuber F, Kurz RW, Sertl K, Grimm G, Balcke P. Increased plasma histamine levels in uraemic pruritus. Clin Sci. (1990) 79:477–82. doi: 10.1042/cs0790477
Keywords: acupoint injection, acupressure, acupuncture, chronic kidney disease, uremic pruritus
Citation: Lu P-H, Chung C-H, Chuo H-E, Lin I-H and Lu P-H (2022) Efficacy of acupoint stimulation as a treatment for uremic pruritus: A systematic review and meta-analysis. Front. Med. 9:1036072. doi: 10.3389/fmed.2022.1036072
Received: 03 September 2022; Accepted: 14 October 2022;
Published: 01 December 2022.
Edited by:
Laurent Misery, Université de Bretagne Occidentale, FranceReviewed by:
Manuel Valdebran Canales, Medical University of South Carolina, United StatesLouise Lönndahl, Karolinska Institutet (KI), Sweden
Copyright © 2022 Lu, Chung, Chuo, Lin and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Po-Hsuan Lu, cG9oc3Vhbmx1LjQyMTdAbW1oLm9yZy50dw==
†These authors have contributed equally to this work
 Ping-Hsun Lu
Ping-Hsun Lu Chia-Hsiang Chung
Chia-Hsiang Chung Hui-En Chuo
Hui-En Chuo I-Hsin Lin2
I-Hsin Lin2