- Institute of Immunology, University of Regensburg, Regensburg, Germany
Since the first description of dendritic cells (DCs) by Steinman and Cohn (1973), the myeloid lineage of leukocytes was investigated intensively. Nowadays it is obvious that myeloid cells, especially DCs, are crucial for the adaptive and innate immune response against intracellular pathogens such as Leishmania major parasites. Based on the overlapping expression of molecules that were commonly used to classify myeloid cells, it becomes difficult to denominate those cell types precisely. Of note, most of these markers used for myeloid cell identification are expressed on a broad range of myeloid cells, and should therefore be handled with care if used for subtyping of myeloid cells. In this mini-review we aim to discuss the relative impact of DCs that release TNF and nitric oxide (Tip-DCs) and myeloid cells with suppressive capacities (myeloid-derived suppressor cells, MDSCs) in infectious diseases such as experimental leishmaniasis. In our point of view it cannot be excluded that the novel subsets that were denominated as “Tip-DCs” and “MDSCs” might not be classical “subsets” but rather represent myeloid cells in a transient maturation stage expressing different genes, in response to the surrounding environment.
Introduction
Based on co-evolutionary processes pathogens have developed escape mechanisms to avoid rapid elimination by host-derived components of the immune system such as antimicrobial peptides and phagocytes. Especially the vector-borne parasites Leishmania (L.) major established efficient methods to have a lead over the host defense mechanism: they hide and replicate within host cells (Olivier et al., 2005). Most of the host cells for Leishmania parasites belong to the mononuclear phagocyte system that is divided into (i) differentiated macrophages, (ii) dendritic cells (DCs), and (iii) monocytes (Ritter et al., 2009; Yona and Jung, 2010). In addition, it is documented that neutrophils can harbor L. major parasites as well (Ritter et al., 2009). However, the number of such skin-resident host cells is limited. Given that limitation, a recruitment of additional host cells is pivotal for subsequent replication and spreading of the parasites (Ritter et al., 1996; Dupasquier et al., 2004). It appears somehow paradox that those innate defense mechanisms that are characterized by a massive inflammation process and attraction of further myeloid cells to the site of infection, give the parasites an advantage: the parasites expand within that recruited host cells.
The procedures involved in extravasation of myeloid cells from the blood stream to the site of infection are complex (Imhof and Aurrand-Lions, 2004) and will not be discussed in detail in this review due to space limitation. Nevertheless, it is important to mention that a broad spectrum of myeloid cells express adhesion molecules such as αMβ2-integrin (also known as CD11b–CD18) and αxβ2-integrin (also known as CD11c–CD18) that are involved in those homing processes (Imhof and Aurrand-Lions, 2004). Thus, it might be possible that a heterogeneous pool of different myeloid subsets is recruited to the inflamed tissue by similar mechanisms (Imhof and Aurrand-Lions, 2004; Leon and Ardavin, 2008). Once placed within the dermal compartment neutrophils and macrophages can release chemokines and pro-inflammatory cytokines, which in turn attract additional myeloid-derived host cells for further infection (Ritter and Korner, 2002; Peters et al., 2008).
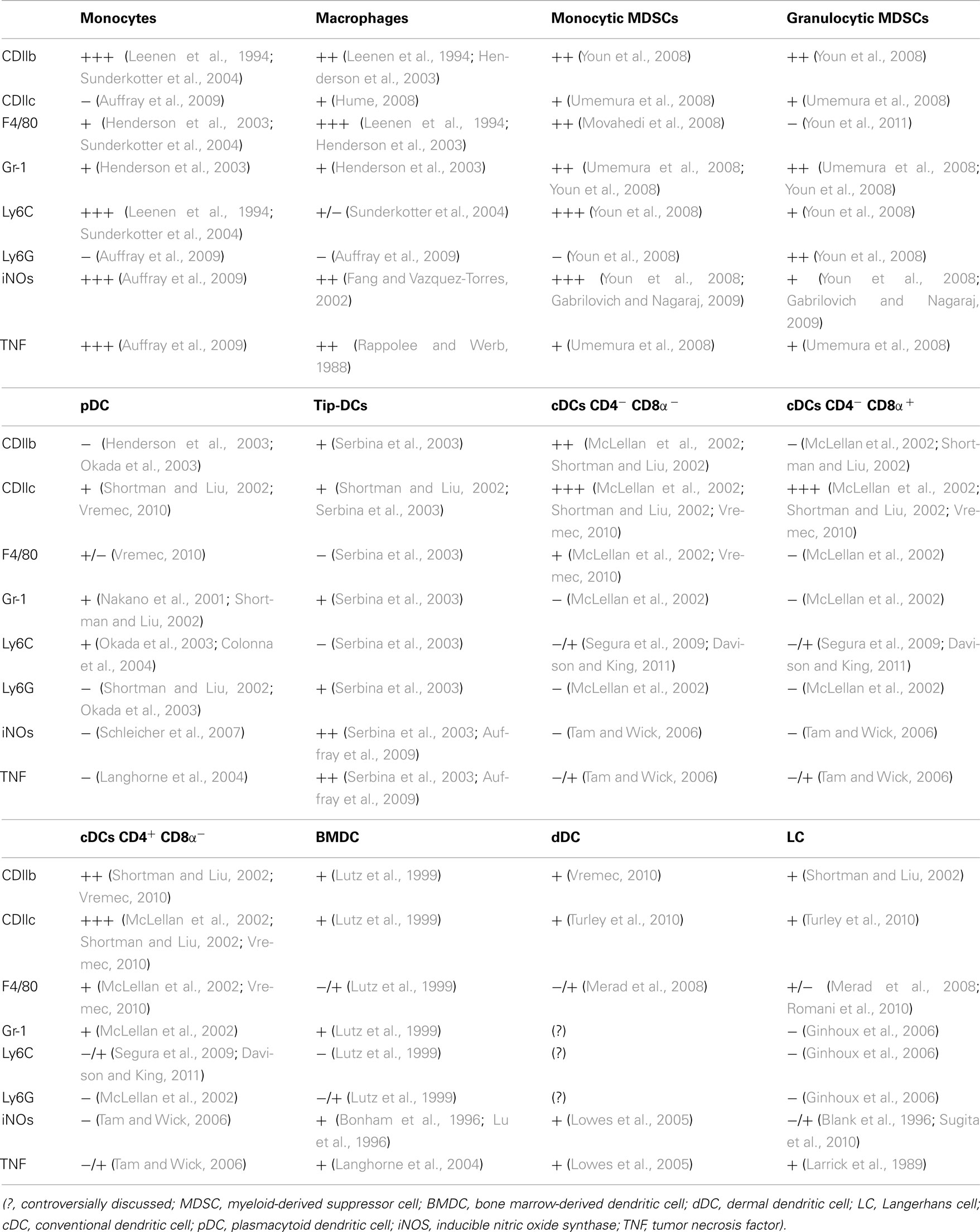
It is commonly accepted that terminally differentiated myeloid cells fulfill controversial functions in infectious diseases such as leishmaniasis: macrophages are crucial for parasite replication and parasite elimination (after appropriate activation), DCs are bridging the innate and adaptive immune response and infected neutrophils can be taken up by macrophages resulting in a pronounced replication of parasites (Bogdan and Rollinghoff, 1998; Bogdan et al., 2000). However, those “classical” myeloid cells, denominated as “macrophage” or “DC,” have been further subdivided into distinct subsets according to certain cluster of differentiation (CD)-patterns and the additional expression of additive molecules and cytokines. Based on that multi-parameter analysis it became difficult to precisely appoint distinct myeloid cell subsets (Table 1). Furthermore, it is obvious that such ex vivo or in situ characterization of a myeloid cell, represents one distinct snapshot in their life span. Thus, it is feasible that the identified phenotypes do not obligatory represent “myeloid subsets” but rather represent a transient stage in the life of these cells – influenced by the local environmental conditions.
In the following section we will discuss myeloid cells commonly known as “TIP-DCs” and “MDSCs” in more detail.
TNF/iNOS Producing DCs: Tip-DCs
In 1957 it was postulated that lymphocytes proliferate in response to antigens that matches their receptor (Burnet, 1976). Steinman and Cohn identified a novel cell type – denominated as DCs – that was discussed to be involved in presentation of antigens and subsequent T cell proliferation in 1973 (Steinman and Cohn, 1973; Katsnelson, 2006). Today it is a paradigm that DCs play a pivotal role in bridging innate and adaptive immunity and consequently in T cell priming. However, the characterization of distinct surface markers (e.g., CD11c, CD11b, CD4, CD8), revealed the diversity of the DCs (Table 1).
Dendritic cell differentiation can start with the stage of a common macrophage-DC progenitor (MDP) that has been described to be Lin− CXCR1+ CD11b− cKit+ CD135+ (Fogg et al., 2006). Those MDPs further differentiate into common DC progenitors (CDP) that in turn evolve to non-conventional plasmacytoid DCs (pDCs) and conventional DCs (cDCs; Fogg et al., 2006). Alternatively, DC maturation might occur from monocyte intermediate precursors (Fogg et al., 2006). The precursor of skin-associated DCs, such as epidermal Langerhans cells (LCs), is controversially discussed. There are data indicating that LCs and most likely dermal DCs (dDCs) are of myeloid origin with a monocytic intermediate (Palucka and Banchereau, 2006). However, other authors argue that LCs descent from fetal progenitor and belong to “‥macrophages of the central nerve system‥” (Auffray et al., 2009). Despite these developmental differences, most of the mentioned DC subsets renew under steady state conditions in lymphoid and non-lymphoid organs (Fogg et al., 2006; Liu et al., 2007; Waskow et al., 2008; Auffray et al., 2009).
Why is it essential to contemplate DC differentiation and progenitor options? Because infectious diseases, such as cutaneous leishmaniasis, are characterized by a massive turn over of myeloid cells – including immature DC precursors – at the site of infection. Thus, it is difficult to denominate a terminally differentiated DC subset correctly that might be involved in an immunological process in vivo. The changing view in the classification of LCs in experimental leishmaniasis represents a good example underlining the difficulties to dedicate the right function. In 1992 it was proposed that LCs are involved in inducing the local immune response against L. major parasites (Will et al., 1992). Twelve years later, based on the possibility for LC depletion, authors described a novel subset of a dermal DC (dDC) which were responsible for the induction of protective T helper (Th) 1 response in leishmaniasis whereas LCs were priming self-regulatory T cells (IL-10 producing type 1 regulatory T cells; Tr1 cells) and Tregs (Moreno, 2007; Brewig et al., 2009; Kautz-Neu et al., 2011).
A novel DC subset was introduced into the field in 2004 (Serbina et al., 2003). Those DCs (CD11bint CD11cint Gr-1+ DEC-205− CD14− F4/80−) were shown to produce TNF and iNOS/NO during Listeria (L.) monocytogenes infection (Serbina et al., 2003). Due to the fact that the presented DCs produce high levels of co-stimulatory molecules, prime alloreactive T cells, do not adhere, and have a DC-like morphology, these TNF/iNOS producing DCs were denominated Tip-DCs (Serbina et al., 2003). Considering that TNF (Virna et al., 2006) and iNOS expression (MacMicking et al., 1997) are pivotal for the control of L. monocytogenes, the authors concluded that Tip-DCs are crucial for antimicrobial defense. The accumulation of Tip-DCs in the liver was also detected in mice infected with Trypanosoma brucei, an extracellular blood-borne parasite that can cause sleeping sickness in humans (Bosschaerts et al., 2010). Based on their findings, the authors concluded that TNF released by Tip-DC is responsible for severe liver injury in trypanosomiasis (Bosschaerts et al., 2010). Thus, the presence of Tip-DCs in inflamed tissues can be either beneficial or destructive.
To review the relevance of Tip-DCs in experimental leishmaniasis, it is important to highlight the potential precursor of those cells and the factors that are involved in Tip-DC differentiation. As indicated above, Tip-DCs can be stained with the mAb RB6-8C5 (granulocyte-differentiation antigen/Gr-1). Notably, the mAb RB6-8C5 detects the lymphocyte antigen 6 complex, locus G and C (Ly6G and Ly6C; Ritter et al., 2009). Thus Tip-DCs can be positive for Ly6C and/or Ly6G, which are known to be expressed on immature monocytes, DCs, and neutrophils (Table 1; Lutz et al., 1999; Sunderkotter et al., 2004; Ritter et al., 2009).
In the murine infection model for T. brucei described by Bosschaerts et al. (2010), CCR2+ inflammatory monocytic cells derived from CD11b and Ly6C expressing cells were discussed to represent the precursor of liver Tip-DCs. In their experimental model, the differentiation to Tip-DCs from immature DCs (CD11c+ but CD80/CD86/MHC-class IIlow) is independent of IFN-γ and MyD88 signaling, whereas IFN-γ stimulation is necessary for TNF and iNOS/NO production (Bosschaerts et al., 2010). Based on the facts mentioned above, it is obvious that TiP-DCs can derive from CCR2+ Ly6Chigh (Serbina and Pamer, 2006) macrophage/DC progenitor (MDP) cells and have the potential to produce TNF/NO after appropriate stimulation.
In general the production of iNOS and TNF can be induced in different DC populations after appropriate stimulation (Munder et al., 1999). For instance, bone marrow-derived DCs (CD11c+, CD11b+, F4/80−) are known to produce TNF (Ritter et al., 2003) and iNOS (Wilkins-Rodriguez et al., 2010) after stimulation (Lu et al., 1996) and are positive for CCR2 (Jimenez et al., 2010). The only DC subset known so far that does not produce iNOS and TNF in parallel are pDCs (CD11b−, CD11cint, B220+, Ly6C+, Gr-1+, CD62L+, and CD45RA+ Colonna et al., 2004; Schleicher et al., 2007) and eventually epidermal LCs (Langerin+/CD103−; Blank et al., 1996). Thus, it is difficult to see the dissimilarity of TiP-DCs and other activated monocyte-derived cells (Taylor et al., 2005; Hume, 2008). In other words it cannot be excluded that TiP-DCs do not represent a distinct DC subset but rather belong to common monocyte-derived DC responding to their environment with TNF/NO production (Serbina et al., 2003).
Nevertheless, the molecules TNF and iNOS expressed by Tip-DCs, are substantial for the host defense against the obligatory intracellular pathogen L. major (Diefenbach et al., 1998; Wilhelm et al., 2001). Additionally, it was shown that Tip-DCs also release IFN-β that is known to promote healing of leishmaniasis (Mattner et al., 2004; Dresing et al., 2010; Solodova et al., 2011). There are very limited data published demonstrating the existence of iNOS producing DCs in experimental leishmaniasis (Leon et al., 2007). Furthermore, only a minor population of DCs in skin-draining lymph nodes (SDLNs; <2%) could be assigned to the phenotype of “Tip-DCs” (De Trez et al., 2009).
Summarizing published reports so far, we assume the following hypothetical scenario for the role of Tip-DCs in experimental leishmaniasis. Here, we focused on the early phase (parasite replication, innate immune response) and the intermediate phase (parasite control, adaptive immune response).
Early after Infection
Skin-resident macrophages and/or neutrophils get infected with promastigote Leishmania parasites after intra dermal inoculation (Peters et al., 2008). Thereafter, macrophages release TNF and the chemokine CCL2 after engulfment of the parasites (Ritter and Moll, 2000; Wenzel et al., 2011). These inflammatory mediators are important for the subsequent recruitment of other CCR2+ myeloid cells such as monocytes and/or DC precursors (Leon et al., 2007; Ritter et al., 2008). Remarkably, it was shown that the expression of IFN-γ at the site of infection increases rapidly, very short after s.c. infection (Liese et al., 2007; Ritter et al., 2008). Consequently, the recruited monocytes and DC precursor are exposed to an inflammatory environment (e.g., IFN-γ, TNF, CCL2) that might be responsible for the subsequent induction of iNOS and TNF production in monocyte-derived DCs: the phenotype of a “Tip-DCs” is induced (De Trez et al., 2009).
The expression of iNOS results in an accumulation of NO in the surrounding of the cell. Given the fact that NO exposure to DCs induces their apoptosis and NO exposure to T cells blocks T cell IFN-γ production, NO represents a central molecule involved in suppression of the T cell response (Lu et al., 1996; Ren et al., 2008). Serbina et al. (2003) reported that Tip-DCs are not essential for T cell priming in mice infected with L. monocytogenes. Other data show that human Tip-DCs can prime naïve T cells toward Th1 cells in vitro (Chong et al., 2011). Thus, NO-releasing Tip-DCs might play a minor role in the expansion of antigen-specific T cells in SDLNs but might be involved in polarizing naïve T cells.
In our notion, TiP-DCs are involved in controlling parasite replication at the site of infection based on the expression of the leishmanicidal molecule NO and the maintenance of TNF-induced inflammation.
Intermediate Phase
The T cell response is induced in SDLNs of infected mice within 1 week after infection (Brewig et al., 2009). However, it is not clear whether DCs or TiP-DCs that were recruited to the site of infection, are responsible/capable for the transfer of living parasites from the side of infection into the SDLNs (Kaye and Scott, 2011). Possibly, TiP-DCs might remain within the dermal compartment, whereas Th1-driving dDCs capture already fragmentized parasite-particles for subsequent processing (Ritter and Osterloh, 2007; Brewig et al., 2009). Keeping in mind that especially mature DC (CCR7high, CD40high) show the tendency to migrate to the SDLNs (Ritter et al., 2003, 2008) it is plausible that the TNF released by Tip-DCs might therefore potentiate the maturation and subsequent migration of Th1-driving dDCs to the SDLNs.
CD11b+/Gr-1+ Myeloid-Derived Cells: Suppressor or Effector Cells?
Ongoing immune reactions against pathogens are often associated with severe tissue damage. Thus, dampening mechanisms are important to narrow that severe side effect. However, such counter-regulating procedures must be well balanced to avoid limitations in host defense and subsequent spreading of the parasites over the entire organism.
Besides the lymphocytic population of regulatory T cells (Tregs), myeloid cells with suppressive functions were described in 1984/85 and referred as “natural suppressor cells” (Strober, 1984; Sakaguchi, 2011). During the last decades myeloid cells with suppressive capacities were rediscovered in the field of oncology (Gabrilovich and Nagaraj, 2009). Those cells – denominated as myeloid-derived suppressor cells (MDSCs) – represent a heterogeneous cell population that stains for CD11b and Gr-1 (Ly6G–Ly6C). Using antibodies specific for Ly6C and Ly6G, MDSCs were further dissected in granulocytic MDSCs (CD11b+Ly6G+Ly6Clow) and monocytic MDSCs (CD11b+Ly6G+Ly6Chigh; Gabrilovich and Nagaraj, 2009).
This further differentiation between sub-groups is helpful. However, the markers used for the classification of MDSCs (CD11b, Ly6G, and Ly6C) are not exclusively restricted to MDSCs. Myeloid progenitor cells and immature myeloid cells such as macrophages, granulocytes, and DC subsets are known to express the surface molecules as well (Table 1). Additionally, it is not clear whether all characteristics of tumor-associated MDSCs can be transferred to infected tissues that eventually show different cytokine expression patterns. Nevertheless, the appearance of myeloid cells showing a MDSC phenotype during inflammation processes have been described in different infection models such as Candida albicans (Mencacci et al., 2002), Porphyromonas gingivalis (Ezernitchi et al., 2006), and L. monocytogenes (Sunderkotter et al., 2004).
Those inflammatory myeloid cells might not necessarily have the adjudicated suppressive function of a “MDSC.” Therefore, the potential suppressive capacity of MDSCs was analyzed in in vitro assays. This data revealed that NO-secretion of immature Ly6G+/CD11b+ myeloid cells can suppress the proliferation of cells isolated from the lymph node in infection models such as experimental leishmaniasis (Pereira et al., 2011) and trypanosomiasis (Goni et al., 2002). It is believed that immunosuppressive activity of MDSCs requires cell–cell contact (Gabrilovich and Nagaraj, 2009). Consequently, cell-surface receptors and/or released short-lived soluble mediators might induce the suppression of the target cell. Furthermore, MDSC participate in the suppression of ongoing immune reactions by the expansion of regulatory T cells (Huang et al., 2006; Serafini et al., 2008). The mechanisms of MDSC mediated suppression are summarized in Table 2.
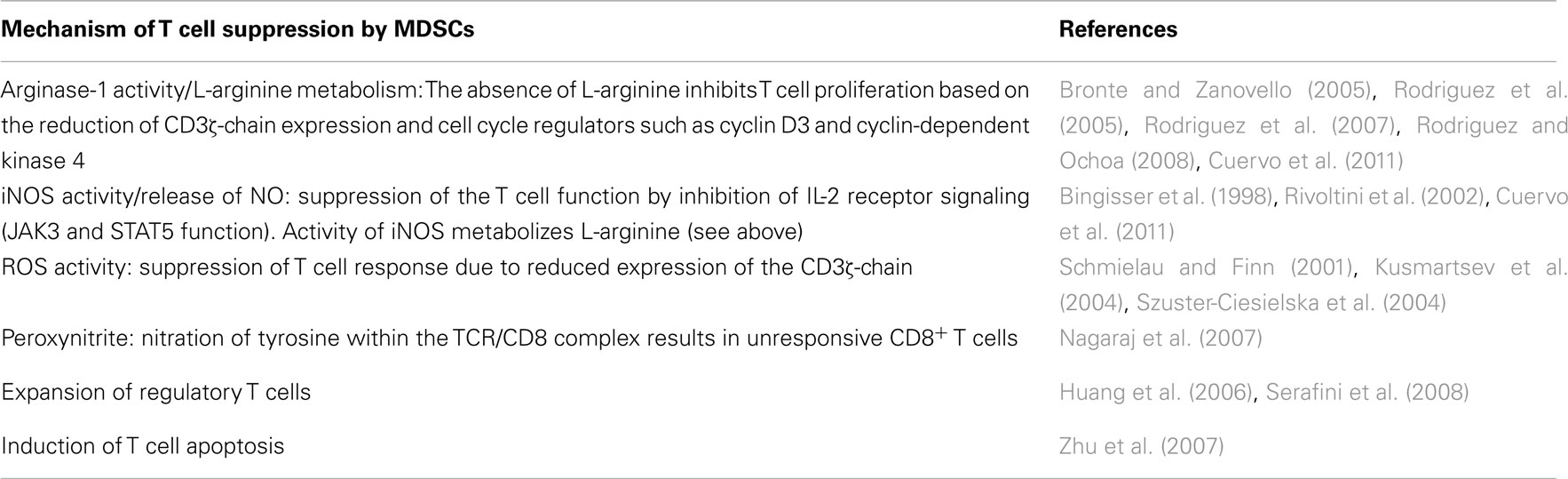
Table 2. Mechanisms driving MDSC suppressive activity (ROS, reactive oxygen species; iNOS, inducible nitric oxide synthase).
Some data indicate that MDSC mediated suppression of T cells is antigen-independent (Kusmartsev et al., 2000; Watanabe et al., 2008). Based on the fact that antigen-specific interactions between antigen-presenting cells and antigen-specific T cells prolong the antigen-specific cell–cell contact, it is most likely that MDSC-derived suppressive factors are more efficient on closed by antigen-specific T cells than on the surrounding antigen-independent T cells (Stoll et al., 2002; Miller et al., 2004; Nagaraj et al., 2007). However, this important aspect needs to be further investigated in the future.
Besides the in vitro studies, the inhibitory function and relevance of MDSCs in vivo is not well documented so far. Based on the data generated in experimental leishmaniasis it further remains unclear, which phase and tissue MDSCs might interfere with T cell activation in vivo. It is conceivable that MDSCs are involved in the elimination of the parasites and the suppression of T cell proliferation as well. Summarizing published reports so far, we assume the following hypothetical scenario for the role of MDSCs experimental leishmaniasis.
To avoid too many speculations we focused on the potential role of MDSCs in the early phase (parasite replication, innate immune response) and the intermediate phase (parasite control, adaptive immune response).
Initial Phase
CD11b+ Ly6Cmed-high monocytes (Sunderkotter et al., 2004) share homing receptors crucial for the extravasation from the blood to the infected tissue. Thus it is most likely that a pool of MDSCs cells is recruited to the site of infection. In this area immature myeloid cells get in contact with cytokines (IL-1, IL-6, CCL2, IL-10, IL-12, IL-13, IL-4, IFN-γ, TGF-β) that drive MDSC differentiation (for further reading; Gabrilovich and Nagaraj, 2009). Of note, IFN-γ and CCL2 are detectable shortly after infection or after phagocyte–parasite interactions (Ritter and Moll, 2000; Schleicher et al., 2007). Thus, immature CD11b+ Ly6Cmed-high myeloid cells can become MDSCs as a response to their inflammatory environment. They start to produce leishmanicidal molecules such as NO and oxygen metabolites and become important effector cells involved in skin-associated host defense. At that time cells of the innate immune system are dominating the inflammatory response at the site of infection. The adaptive Th1 cell mediated immune response is initiated within SDLNs but is not established at the site of infection yet.
Intermediate Phase
Shortly after infection Leishmania-specific Th1 cells expand within the SDLNs and accumulate at the site of infection (Brewig et al., 2009). Thus two different types of T cell suppression might be possible: (i) inhibition of T cell proliferation and (ii) inhibition of T cell effector functions.
Due to the fact that MDSCs show an enhanced L-arginine metabolism (e.g., increased arginase-1 activity) it might be possible that L-arginine consuming MDSCs are responsible for a local L-arginine deficiency. Given the fact that L-arginine is necessary for cell proliferation it is therefore most likely that T cell proliferation within SDLNs is reduced based on L-arginine limitation. Furthermore, it is possible that NO that is released by MDSCs directly inhibits the IL-2 receptor signaling and subsequently the proliferation of T cells (Bingisser et al., 1998). Therefore, MDSCs might be involved in the inhibition of T cell proliferation in SDLNs.
The situation at the site of infection is quite different. Already activated effector T cells migrate to the skin and the mechanism how MDSC could suppress these activated effector cell function is still not fully understood. However, it is possible that NO can inhibit the release of Th1 cytokines by T cells (Bauer et al., 1997) which might be mediated by reduced L-arginine availability in the presence of MDSCs (Cuervo et al., 2011). Alternatively, the induction of apoptosis of effector T cells would be an elegant way to suppress the ongoing T cell response.
Both MDSC mediated mechanisms such as controlling T cell proliferation and activity are hypothetical. However, it might represent a smart move to dampen the host-derived immune response that in turn gives some of the parasites the chance to survive within mammalians.
Summary
We aimed to highlight the potential role of TiP-DCs and MDSCs in infectious diseases such as leishmaniasis. Assuredly, pathogens such as Leishmania parasites interact with cells from the myeloid system. However, based on the overlapping phenotypes of myeloid cells, it becomes difficult to denominate those cell types precisely. In our point of view it cannot be excluded that the novel subsets of “Tip-DCs” and “MDSCs” might not be classical “subsets” but rather represent myeloid cells in a transient maturation stage expressing different genes, in response to environment.
However, those NO-releasing myeloid cells can fulfill distinct functions in the host defense against Leishmania parasites: they might be involved in either controlling the parasite spreading at the site of infection or dampening ongoing T cell responses. Whether parasites can influence the differentiation of immature myeloid cells to subsequent suppression of the adaptive immune response needs to be further investigated. Additional studies are therefore necessary to learn more about the factors regulating that fascinating plasticity and the subsequent biological relevance of phagocytic cell subsets after pathogen interaction.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to apologize to all colleagues whose work could not be cited due to space restrictions. The preparation of that article and the conduct of some studies reviewed here were supported by grants to Uwe Ritter (RI 1849/1-1, 2-1, and 4-1).
Abbreviations
DC, dendritic cell; L., Leishmania; MDSC, myeloid-derived suppressor cells; SDLN, skin-draining lymph nodes; TIP-DCs, tumor necrosis factor (TNF) and inducible nitric oxide synthase (iNOS) producing dendritic cell.
References
Auffray, C., Sieweke, M. H., and Geissmann, F. (2009). Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu. Rev. Immunol. 27, 669–692.
Bauer, H., Jung, T., Tsikas, D., Stichtenoth, D. O., Frolich, J. C., and Neumann, C. (1997). Nitric oxide inhibits the secretion of T-helper 1- and T-helper 2-associated cytokines in activated human T cells. Immunology 90, 205–211.
Bingisser, R. M., Tilbrook, P. A., Holt, P. G., and Kees, U. R. (1998). Macrophage-derived nitric oxide regulates T cell activation via reversible disruption of the Jak3/STAT5 signaling pathway. J. Immunol. 160, 5729–5734.
Blank, C., Bogdan, C., Bauer, C., Erb, K., and Moll, H. (1996). Murine epidermal Langerhans cells do not express inducible nitric oxide synthase. Eur. J. Immunol. 26, 792–796.
Bogdan, C., Donhauser, N., Doring, R., Rollinghoff, M., Diefenbach, A., and Rittig, M. G. (2000). Fibroblasts as host cells in latent leishmaniosis. J. Exp. Med. 191, 2121–2130.
Bogdan, C., and Rollinghoff, M. (1998). The immune response to Leishmania: mechanisms of parasite control and evasion. Int. J. Parasitol. 28, 121–134.
Bonham, C. A., Lu, L., Li, Y., Hoffman, R. A., Simmons, R. L., and Thomson, A. W. (1996). Nitric oxide production by mouse bone marrow-derived dendritic cells: implications for the regulation of allogeneic T cell responses. Transplantation 62, 1871–1877.
Bosschaerts, T., Guilliams, M., Stijlemans, B., Morias, Y., Engel, D., Tacke, F., Herin, M., De Baetselier, P., and Beschin, A. (2010). Tip-DC development during parasitic infection is regulated by IL-10 and requires CCL2/CCR2, IFN-gamma and MyD88 signaling. PLoS Pathog. 6, e1001045. doi:10.1371/journal.ppat.1001045
Brewig, N., Kissenpfennig, A., Malissen, B., Veit, A., Bickert, T., Fleischer, B., Mostbock, S., and Ritter, U. (2009). Priming of CD8+ and CD4+ T cells in experimental leishmaniasis is initiated by different dendritic cell subtypes. J. Immunol. 182, 774–783.
Bronte, V., and Zanovello, P. (2005). Regulation of immune responses by L-arginine metabolism. Nat. Rev. Immunol. 5, 641–654.
Burnet, F. M. (1976). A modification of Jerne’s theory of antibody production using the concept of clonal selection. CA Cancer J. Clin. 26, 119–121.
Chong, S. Z., Wong, K. L., Lin, G., Yang, C. M., Wong, S. C., Angeli, V., Macary, P. A., and Kemeny, D. M. (2011). Human CD8 T cells drive Th1 responses through the differentiation of TNF/iNOS-producing dendritic cells. Eur. J. Immunol. 41, 1639–1651.
Colonna, M., Trinchieri, G., and Liu, Y. J. (2004). Plasmacytoid dendritic cells in immunity. Nat. Immunol. 5, 1219–1226.
Cuervo, H., Guerrero, N. A., Carbajosa, S., Beschin, A., De Baetselier, P., Girones, N., and Fresno, M. (2011). Myeloid-derived suppressor cells infiltrate the heart in acute Trypanosoma cruzi infection. J. Immunol. 187, 2656–2665.
Davison, A. M., and King, N. J. (2011). Accelerated dendritic cell differentiation from migrating Ly6C(lo) bone marrow monocytes in early dermal West Nile virus infection. J. Immunol. 186, 2382–2396.
De Trez, C., Magez, S., Akira, S., Ryffel, B., Carlier, Y., and Muraille, E. (2009). iNOS-producing inflammatory dendritic cells constitute the major infected cell type during the chronic Leishmania major infection phase of C57BL/6 resistant mice. PLoS Pathog. 5, e1000494. doi:10.1371/journal.ppat.1000494
Diefenbach, A., Schindler, H., Donhauser, N., Lorenz, E., Laskay, T., Macmicking, J., Rollinghoff, M., Gresser, I., and Bogdan, C. (1998). Type 1 interferon (IFNalpha/beta) and type 2 nitric oxide synthase regulate the innate immune response to a protozoan parasite. Immunity 8, 77–87.
Dresing, P., Borkens, S., Kocur, M., Kropp, S., and Scheu, S. (2010). A fluorescence reporter model defines “Tip-DCs” as the cellular source of interferon beta in murine listeriosis. PLoS ONE 5, e15567. doi:10.1371/journal.pone.0015567
Dupasquier, M., Stoitzner, P., Van Oudenaren, A., Romani, N., and Leenen, P. J. (2004). Macrophages and dendritic cells constitute a major subpopulation of cells in the mouse dermis. J. Invest. Dermatol. 123, 876–879.
Ezernitchi, A. V., Vaknin, I., Cohen-Daniel, L., Levy, O., Manaster, E., Halabi, A., Pikarsky, E., Shapira, L., and Baniyash, M. (2006). TCR zeta down-regulation under chronic inflammation is mediated by myeloid suppressor cells differentially distributed between various lymphatic organs. J. Immunol. 177, 4763–4772.
Fang, F. C., and Vazquez-Torres, A. (2002). Nitric oxide production by human macrophages: there’s NO doubt about it. Am. J. Physiol. Lung Cell. Mol. Physiol. 282, L941–L943.
Fogg, D. K., Sibon, C., Miled, C., Jung, S., Aucouturier, P., Littman, D. R., Cumano, A., and Geissmann, F. (2006). A clonogenic bone marrow progenitor specific for macrophages and dendritic cells. Science 311, 83–87.
Gabrilovich, D. I., and Nagaraj, S. (2009). Myeloid-derived suppressor cells as regulators of the immune system. Nat. Rev. Immunol. 9, 162–174.
Ginhoux, F., Tacke, F., Angeli, V., Bogunovic, M., Loubeau, M., Dai, X. M., Stanley, E. R., Randolph, G. J., and Merad, M. (2006). Langerhans cells arise from monocytes in vivo. Nat. Immunol. 7, 265–273.
Goni, O., Alcaide, P., and Fresno, M. (2002). Immunosuppression during acute Trypanosoma cruzi infection: involvement of Ly6G (Gr1(+))CD11b(+)immature myeloid suppressor cells. Int. Immunol. 14, 1125–1134.
Henderson, R. B., Hobbs, J. A., Mathies, M., and Hogg, N. (2003). Rapid recruitment of inflammatory monocytes is independent of neutrophil migration. Blood 102, 328–335.
Huang, B., Pan, P. Y., Li, Q., Sato, A. I., Levy, D. E., Bromberg, J., Divino, C. M., and Chen, S. H. (2006). Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res. 66, 1123–1131.
Imhof, B. A., and Aurrand-Lions, M. (2004). Adhesion mechanisms regulating the migration of monocytes. Nat. Rev. Immunol. 4, 432–444.
Jimenez, F., Quinones, M. P., Martinez, H. G., Estrada, C. A., Clark, K., Garavito, E., Ibarra, J., Melby, P. C., and Ahuja, S. S. (2010). CCR2 plays a critical role in dendritic cell maturation: possible role of CCL2 and NF-κB. J. Immunol. 184, 5571–5581.
Katsnelson, A. (2006). Kicking off adaptive immunity: the discovery of dendritic cells. J. Exp. Med. 203, 1622.
Kautz-Neu, K., Noordegraaf, M., Dinges, S., Bennett, C. L., John, D., Clausen, B. E., and Von Stebut, E. (2011). Langerhans cells are negative regulators of the anti-Leishmania response. J. Exp. Med. 208, 885–891.
Kaye, P., and Scott, P. (2011). Leishmaniasis: complexity at the host-pathogen interface. Nat. Rev. Microbiol. 9, 604–615.
Kusmartsev, S., Nefedova, Y., Yoder, D., and Gabrilovich, D. I. (2004). Antigen-specific inhibition of CD8+ T cell response by immature myeloid cells in cancer is mediated by reactive oxygen species. J. Immunol. 172, 989–999.
Kusmartsev, S. A., Li, Y., and Chen, S. H. (2000). Gr-1+ myeloid cells derived from tumor-bearing mice inhibit primary T cell activation induced through CD3/CD28 costimulation. J. Immunol. 165, 779–785.
Langhorne, J., Albano, F. R., Hensmann, M., Sanni, L., Cadman, E., Voisine, C., and Sponaas, A. M. (2004). Dendritic cells, pro-inflammatory responses, and antigen presentation in a rodent malaria infection. Immunol. Rev. 201, 35–47.
Larrick, J. W., Morhenn, V., Chiang, Y. L., and Shi, T. (1989). Activated Langerhans cells release tumor necrosis factor. J. Leukoc. Biol. 45, 429–433.
Leenen, P. J., De Bruijn, M. F., Voerman, J. S., Campbell, P. A., and Van Ewijk, W. (1994). Markers of mouse macrophage development detected by monoclonal antibodies. J. Immunol. Methods 174, 5–19.
Leon, B., and Ardavin, C. (2008). Monocyte migration to inflamed skin and lymph nodes is differentially controlled by L-selectin and PSGL-1. Blood 111, 3126–3130.
Leon, B., Lopez-Bravo, M., and Ardavin, C. (2007). Monocyte-derived dendritic cells formed at the infection site control the induction of protective T helper 1 responses against Leishmania. Immunity 26, 519–531.
Liese, J., Schleicher, U., and Bogdan, C. (2007). TLR9 signaling is essential for the innate NK cell response in murine cutaneous leishmaniasis. Eur. J. Immunol. 37, 3424–3434.
Liu, K., Waskow, C., Liu, X., Yao, K., Hoh, J., and Nussenzweig, M. (2007). Origin of dendritic cells in peripheral lymphoid organs of mice. Nat. Immunol. 8, 578–583.
Lowes, M. A., Chamian, F., Abello, M. V., Fuentes-Duculan, J., Lin, S. L., Nussbaum, R., Novitskaya, I., Carbonaro, H., Cardinale, I., Kikuchi, T., Gilleaudeau, P., Sullivan-Whalen, M., Wittkowski, K. M., Papp, K., Garovoy, M., Dummer, W., Steinman, R. M., and Krueger, J. G. (2005). Increase in TNF-alpha and inducible nitric oxide synthase-expressing dendritic cells in psoriasis and reduction with efalizumab (anti-CD11a). Proc. Natl. Acad. Sci. U.S.A. 102, 19057–19062.
Lu, L., Bonham, C. A., Chambers, F. G., Watkins, S. C., Hoffman, R. A., Simmons, R. L., and Thomson, A. W. (1996). Induction of nitric oxide synthase in mouse dendritic cells by IFN-gamma, endotoxin, and interaction with allogeneic T cells: nitric oxide production is associated with dendritic cell apoptosis. J. Immunol. 157, 3577–3586.
Lutz, M. B., Kukutsch, N., Ogilvie, A. L., Rossner, S., Koch, F., Romani, N., and Schuler, G. (1999). An advanced culture method for generating large quantities of highly pure dendritic cells from mouse bone marrow. J. Immunol. Methods 223, 77–92.
MacMicking, J., Xie, Q. W., and Nathan, C. (1997). Nitric oxide and macrophage function. Annu. Rev. Immunol. 15, 323–350.
Mattner, J., Wandersee-Steinhauser, A., Pahl, A., Rollinghoff, M., Majeau, G. R., Hochman, P. S., and Bogdan, C. (2004). Protection against progressive leishmaniasis by IFN-beta. J. Immunol. 172, 7574–7582.
McLellan, A. D., Kapp, M., Eggert, A., Linden, C., Bommhardt, U., Brocker, E. B., Kammerer, U., and Kampgen, E. (2002). Anatomic location and T-cell stimulatory functions of mouse dendritic cell subsets defined by CD4 and CD8 expression. Blood 99, 2084–2093.
Mencacci, A., Montagnoli, C., Bacci, A., Cenci, E., Pitzurra, L., Spreca, A., Kopf, M., Sharpe, A. H., and Romani, L. (2002). CD80+Gr-1+myeloid cells inhibit development of antifungal Th1 immunity in mice with candidiasis. J. Immunol. 169, 3180–3190.
Merad, M., Ginhoux, F., and Collin, M. (2008). Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat. Rev. Immunol. 8, 935–947.
Miller, M. J., Safrina, O., Parker, I., and Cahalan, M. D. (2004). Imaging the single cell dynamics of CD4+ T cell activation by dendritic cells in lymph nodes. J. Exp. Med. 200, 847–856.
Moreno, J. (2007). Changing views on Langerhans cell functions in leishmaniasis. Trends Parasitol. 23, 86–88.
Movahedi, K., Guilliams, M., Van Den Bossche, J., Van Den Bergh, R., Gysemans, C., Beschin, A., De Baetselier, P., and Van Ginderachter, J. A. (2008). Identification of discrete tumor-induced myeloid-derived suppressor cell subpopulations with distinct T cell-suppressive activity. Blood 111, 4233–4244.
Munder, M., Eichmann, K., Moran, J. M., Centeno, F., Soler, G., and Modolell, M. (1999). Th1/Th2-regulated expression of arginase isoforms in murine macrophages and dendritic cells. J. Immunol. 163, 3771–3777.
Nagaraj, S., Gupta, K., Pisarev, V., Kinarsky, L., Sherman, S., Kang, L., Herber, D. L., Schneck, J., and Gabrilovich, D. I. (2007). Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat. Med. 13, 828–835.
Nakano, H., Yanagita, M., and Gunn, M. D. (2001). CD11c(+)B220(+)Gr-1(+) cells in mouse lymph nodes and spleen display characteristics of plasmacytoid dendritic cells. J. Exp. Med. 194, 1171–1178.
Okada, T., Lian, Z. X., Naiki, M., Ansari, A. A., Ikehara, S., and Gershwin, M. E. (2003). Murine thymic plasmacytoid dendritic cells. Eur. J. Immunol. 33, 1012–1019.
Olivier, M., Gregory, D. J., and Forget, G. (2005). Subversion mechanisms by which Leishmania parasites can escape the host immune response: a signaling point of view. Clin. Microbiol. Rev. 18, 293–305.
Palucka, A. K., and Banchereau, J. (2006). Langerhans cells: daughters of monocytes. Nat. Immunol. 7, 223–224.
Pereira, W. F., Ribeiro-Gomes, F. L., Guillermo, L. V., Vellozo, N. S., Montalvao, F., Dosreis, G. A., and Lopes, M. F. (2011). Myeloid-derived suppressor cells help protective immunity to Leishmania major infection despite suppressed T cell responses. J. Leukoc. Biol. 90, 1191–1197.
Peters, N. C., Egen, J. G., Secundino, N., Debrabant, A., Kimblin, N., Kamhawi, S., Lawyer, P., Fay, M. P., Germain, R. N., and Sacks, D. (2008). In vivo imaging reveals an essential role for neutrophils in leishmaniasis transmitted by sand flies. Science 321, 970–974.
Rappolee, D. A., and Werb, Z. (1988). Secretory products of phagocytes. Curr. Opin. Immunol. 1, 47–55.
Ren, G., Su, J., Zhao, X., Zhang, L., Zhang, J., Roberts, A. I., Zhang, H., Das, G., and Shi, Y. (2008). Apoptotic cells induce immunosuppression through dendritic cells: critical roles of IFN-gamma and nitric oxide. J. Immunol. 181, 3277–3284.
Ritter, U., Frischknecht, F., and Van Zandbergen, G. (2009). Are neutrophils important host cells for Leishmania parasites? Trends Parasitol. 25, 505–510.
Ritter, U., and Korner, H. (2002). Divergent expression of inflammatory dermal chemokines in cutaneous leishmaniasis. Parasite Immunol. 24, 295–301.
Ritter, U., Lechner, A., Scharl, K., Kiafard, Z., Zwirner, J., and Korner, H. (2008). TNF controls the infiltration of dendritic cells into the site of Leishmania major infection. Med. Microbiol. Immunol. 197, 29–37.
Ritter, U., Meissner, A., Ott, J., and Korner, H. (2003). Analysis of the maturation process of dendritic cells deficient for TNF and lymphotoxin-alpha reveals an essential role for TNF. J. Leukoc. Biol. 74, 216–222.
Ritter, U., and Moll, H. (2000). Monocyte chemotactic protein-1 stimulates the killing of Leishmania major by human monocytes, acts synergistically with IFN-gamma and is antagonized by IL-4. Eur. J. Immunol. 30, 3111–3120.
Ritter, U., Moll, H., Laskay, T., Brocker, E., Velazco, O., Becker, I., and Gillitzer, R. (1996). Differential expression of chemokines in patients with localized and diffuse cutaneous American leishmaniasis. J. Infect. Dis. 173, 699–709.
Ritter, U., and Osterloh, A. (2007). A new view on cutaneous dendritic cell subsets in experimental leishmaniasis. Med. Microbiol. Immunol. 196, 51–59.
Rivoltini, L., Carrabba, M., Huber, V., Castelli, C., Novellino, L., Dalerba, P., Mortarini, R., Arancia, G., Anichini, A., Fais, S., and Parmiani, G. (2002). Immunity to cancer: attack and escape in T lymphocyte-tumor cell interaction. Immunol. Rev. 188, 97–113.
Rodriguez, P. C., Hernandez, C. P., Quiceno, D., Dubinett, S. M., Zabaleta, J., Ochoa, J. B., Gilbert, J., and Ochoa, A. C. (2005). Arginase I in myeloid suppressor cells is induced by COX-2 in lung carcinoma. J. Exp. Med. 202, 931–939.
Rodriguez, P. C., and Ochoa, A. C. (2008). Arginine regulation by myeloid derived suppressor cells and tolerance in cancer: mechanisms and therapeutic perspectives. Immunol. Rev. 222, 180–191.
Rodriguez, P. C., Quiceno, D. G., and Ochoa, A. C. (2007). L-arginine availability regulates T-lymphocyte cell-cycle progression. Blood 109, 1568–1573.
Romani, N., Clausen, B. E., and Stoitzner, P. (2010). Langerhans cells and more: langerin-expressing dendritic cell subsets in the skin. Immunol. Rev. 234, 120–141.
Schleicher, U., Liese, J., Knippertz, I., Kurzmann, C., Hesse, A., Heit, A., Fischer, J. A., Weiss, S., Kalinke, U., Kunz, S., and Bogdan, C. (2007). NK cell activation in visceral leishmaniasis requires TLR9, myeloid DCs, and IL-12, but is independent of plasmacytoid DCs. J. Exp. Med. 204, 893–906.
Schmielau, J., and Finn, O. J. (2001). Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of T-cell function in advanced cancer patients. Cancer Res. 61, 4756–4760.
Segura, E., Wong, J., and Villadangos, J. A. (2009). Cutting edge: B220+CCR9- dendritic cells are not plasmacytoid dendritic cells but are precursors of conventional dendritic cells. J. Immunol. 183, 1514–1517.
Serafini, P., Mgebroff, S., Noonan, K., and Borrello, I. (2008). Myeloid-derived suppressor cells promote cross-tolerance in B-cell lymphoma by expanding regulatory T cells. Cancer Res. 68, 5439–5449.
Serbina, N. V., and Pamer, E. G. (2006). Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat. Immunol. 7, 311–317.
Serbina, N. V., Salazar-Mather, T. P., Biron, C. A., Kuziel, W. A., and Pamer, E. G. (2003). TNF/iNOS-producing dendritic cells mediate innate immune defense against bacterial infection. Immunity 19, 59–70.
Shortman, K., and Liu, Y. J. (2002). Mouse and human dendritic cell subtypes. Nat. Rev. Immunol. 2, 151–161.
Solodova, E., Jablonska, J., Weiss, S., and Lienenklaus, S. (2011). Production of IFN-beta during Listeria monocytogenes infection is restricted to monocyte/macrophage lineage. PLoS ONE 6, e18543. doi:10.1371/journal.pone.0018543
Steinman, R. M., and Cohn, Z. A. (1973). Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J. Exp. Med. 137, 1142–1162.
Stoll, S., Delon, J., Brotz, T. M., and Germain, R. N. (2002). Dynamic imaging of T cell-dendritic cell interactions in lymph nodes. Science 296, 1873–1876.
Strober, S. (1984). Natural suppressor (NS) cells, neonatal tolerance, and total lymphoid irradiation: exploring obscure relationships. Annu. Rev. Immunol. 2, 219–237.
Sugita, K., Kabashima, K., Yoshiki, R., Ikenouchi-Sugita, A., Tsutsui, M., Nakamura, J., Yanagihara, N., and Tokura, Y. (2010). Inducible nitric oxide synthase downmodulates contact hypersensitivity by suppressing dendritic cell migration and survival. J. Invest. Dermatol. 130, 464–471.
Sunderkotter, C., Nikolic, T., Dillon, M. J., Van Rooijen, N., Stehling, M., Drevets, D. A., and Leenen, P. J. (2004). Subpopulations of mouse blood monocytes differ in maturation stage and inflammatory response. J. Immunol. 172, 4410–4417.
Szuster-Ciesielska, A., Hryciuk-Umer, E., Stepulak, A., Kupisz, K., and Kandefer-Szerszen, M. (2004). Reactive oxygen species production by blood neutrophils of patients with laryngeal carcinoma and antioxidative enzyme activity in their blood. Acta Oncol. 43, 252–258.
Tam, M. A., and Wick, M. J. (2006). Differential expansion, activation and effector functions of conventional and plasmacytoid dendritic cells in mouse tissues transiently infected with Listeria monocytogenes. Cell. Microbiol. 8, 1172–1187.
Taylor, P. R., Martinez-Pomares, L., Stacey, M., Lin, H. H., Brown, G. D., and Gordon, S. (2005). Macrophage receptors and immune recognition. Annu. Rev. Immunol. 23, 901–944.
Turley, S. J., Fletcher, A. L., and Elpek, K. G. (2010). The stromal and haematopoietic antigen-presenting cells that reside in secondary lymphoid organs. Nat. Rev. Immunol. 10, 813–825.
Umemura, N., Saio, M., Suwa, T., Kitoh, Y., Bai, J., Nonaka, K., Ouyang, G. F., Okada, M., Balazs, M., Adany, R., Shibata, T., and Takami, T. (2008). Tumor-infiltrating myeloid-derived suppressor cells are pleiotropic-inflamed monocytes/macrophages that bear M1- and M2-type characteristics. J. Leukoc. Biol. 83, 1136–1144.
Virna, S., Deckert, M., Lutjen, S., Soltek, S., Foulds, K. E., Shen, H., Korner, H., Sedgwick, J. D., and Schluter, D. (2006). TNF is important for pathogen control and limits brain damage in murine cerebral listeriosis. J. Immunol. 177, 3972–3982.
Vremec, D. (2010). The isolation of mouse dendritic cells from lymphoid tissues and the identification of dendritic cell subtypes by multiparameter flow cytometry. Methods Mol. Biol. 595, 205–229.
Waskow, C., Liu, K., Darrasse-Jeze, G., Guermonprez, P., Ginhoux, F., Merad, M., Shengelia, T., Yao, K., and Nussenzweig, M. (2008). The receptor tyrosine kinase Flt3 is required for dendritic cell development in peripheral lymphoid tissues. Nat. Immunol. 9, 676–683.
Watanabe, S., Deguchi, K., Zheng, R., Tamai, H., Wang, L. X., Cohen, P. A., and Shu, S. (2008). Tumor-induced CD11b+Gr-1+ myeloid cells suppress T cell sensitization in tumor-draining lymph nodes. J. Immunol. 181, 3291–3300.
Wenzel, U. A., Bank, E., Florian, C., Forster, S., Zimara, N., Steinacker, J., Klinger, M., Reiling, N., Ritter, U., and Van Zandbergen, G. (2011). Leishmania major parasite stage-dependent host cell invasion and immune evasion. FASEB J. 26, 29–39.
Wilhelm, P., Ritter, U., Labbow, S., Donhauser, N., Rollinghoff, M., Bogdan, C., and Korner, H. (2001). Rapidly fatal leishmaniasis in resistant C57BL/6 mice lacking TNF. J. Immunol. 166, 4012–4019.
Wilkins-Rodriguez, A. A., Escalona-Montano, A. R., Aguirre-Garcia, M., Becker, I., and Gutierrez-Kobeh, L. (2010). Regulation of the expression of nitric oxide synthase by Leishmania mexicana amastigotes in murine dendritic cells. Exp. Parasitol. 126, 426–434.
Will, A., Blank, C., Rollinghoff, M., and Moll, H. (1992). Murine epidermal Langerhans cells are potent stimulators of an antigen-specific T cell response to Leishmania major, the cause of cutaneous leishmaniasis. Eur. J. Immunol. 22, 1341–1347.
Yona, S., and Jung, S. (2010). Monocytes: subsets, origins, fates and functions. Curr. Opin. Hematol. 17, 53–59.
Youn, J. I., Collazo, M., Shalova, I. N., Biswas, S. K., and Gabrilovich, D. I. (2011). Characterization of the nature of granulocytic myeloid-derived suppressor cells in tumor-bearing mice. J. Leukoc. Biol. 91, 167–181.
Youn, J. I., Nagaraj, S., Collazo, M., and Gabrilovich, D. I. (2008). Subsets of myeloid-derived suppressor cells in tumor-bearing mice. J. Immunol. 181, 5791–5802.
Keywords: dendritic cell, myeloid suppressor cell, nitric oxide synthase, Langerhans cells, Leishmania parasites
Citation: Schmid M, Wege AK and Ritter U (2012) Characteristics of “Tip-DCs and MDSCs” and their potential role in leishmaniasis Front. Microbio. 3:74. doi: 10.3389/fmicb.2012.00074
Received: 21 December 2011; Accepted: 13 February 2012;
Published online: 12 March 2012.
Edited by:
Nathan Peters, National Institute of Allergy and Infectious Diseases, USAReviewed by:
Mirko Trilling, Heinrich-Heine-University Düsseldorf, GermanyEmilio Luis Malchiodi, University of Buenos Aires, Argentina
Copyright: © 2012 Schmid, Wege and Ritter. This is an open-access article distributed under the terms of the Creative Commons Attribution Non Commercial License, which permits non-commercial use, distribution, and reproduction in other forums, provided the original authors and source are credited.
*Correspondence: Uwe Ritter, Institute of Immunology, University of Regensburg, Franz-Josef-Strauß-Allee-11, 93053 Regensburg, Germany. e-mail:dXdlLnJpdHRlckBrbGluaWsudW5pLXJlZ2Vuc2J1cmcuZGU=

 Anja K. Wege
Anja K. Wege