- 1Department of Medical Imaging, Taipei Medical University Hospital, Taipei, Taiwan
- 2Research Center of Translational Imaging, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 3Department of Radiology, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 4Department of Diagnostic Radiology, Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Chiayi, Taiwan
- 5Department of Respiratory Care, Chang Gung University of Science and Technology, Chiayi, Taiwan
- 6Department of Psychology, National Chung Cheng University, Chiayi, Taiwan
- 7Department of Imaging Physics, Division of Diagnostic Imaging, University of Texas MD Anderson Cancer Center, Houston, TX, United States
Background: Recent trials have proved the efficacy of mechanical thrombectomy over medical treatment for patients with acute ischemic stroke, with the balance of equivalent rates of adverse events. Stent retrievers were applied predominantly in most trials; however, the role of other thrombectomy devices has not been well validated. A direct aspiration first-pass technique (ADAPT) is proposed to be a faster thrombectomy technique than the stent retriever technique. This meta-analysis investigated and compared the efficacy and adverse events of first-line ADAPT with those of first-line stent retrievers in patients with acute ischemic stroke.
Methods: A structured search was conducted comprehensively. A total of 1623 papers were found, and 4 articles were included in our meta-analysis. The Critical Appraisal Skills Programme tools were applied to evaluate the quality of studies. The primary outcome was defined as the proportion of patients with the Thrombolysis in Cerebral Ischemia (TICI) scale of 2b/3 at the end of all procedures. Secondary outcomes were the proportion of patients with functional independence (modified Rankin scale of 0–2) at the third month, the proportion of patients with the Thrombolysis in Cerebral Ischemia (TICI) scale of 2b/3 by primary chosen device, and the proportion of patients who received rescue therapies. Safety outcomes were the symptomatic intracranial hemorrhage (sICH) rate and the mortality rate within 3 months.
Results: One randomized controlled trial, one prospective cohort study, and two retrospective cohort studies were included. No significant difference between these 2 strategies of management were observed in the primary outcome (TICI scale at the end of all procedures, odds ratio [OR] = 0.78), two secondary outcomes (functional independence at the third month, OR = 1.16; TICI scale by primary chosen device, OR = 1.25), and all safety outcomes (sICH rate, OR = 1.56; mortality rate, OR = 0.91). The proportion of patients who received rescue therapies was higher in the first-line ADAPT group (OR = 0.64).
Conclusions: Among first-line thrombectomy devices for patients with ischemic stroke, ADAPT with the latest thrombosuction system was as efficient and safe as stent retrievers.
Introduction
Recent trials and meta-analyses have proved the efficacy of mechanical thrombectomy over medical treatment for patients with acute ischemic stroke, with the balance of equivalent rates of adverse events (1–7). In most of these trials, stent retrievers, such as the Solitaire (Covidien, Plymouth, MN) and Trevo (Stryker, Kalamazoo, MI), have been used. However, the role of aspiration thrombectomy devices has not been well validated.
A direct aspiration first-pass technique (ADAPT) was introduced in July 2013 (8) and has been proposed as a faster thrombectomy technique than the stent retriever technique (9–12). Because better clinical outcomes have been correlated with early vessel recanalization (13), an initial attempt at recanalization by using ADAPT may be warranted with an improvement in the time required for the procedure. Several observational studies have reported comparable rates of recanalization and 90-day functional independence in patients treated with ADAPT and stent retrievers (14–16). It was also proposed that ADAPT technique is a cheaper technique than the stent retriever thus it should be recommended (10). However, the latest Contact Aspiration vs Stent Retriever for Successful Revascularization (ASTER) trial demonstrated that first-line ADAPT did not result in an increased successful revascularization rate at the end of the procedure (17). The rate of the introduction of rescue therapy was also higher in the ADAPT group than in the stent retriever group. Therefore, the purpose of this meta-analysis is to investigate and compare the efficacy and adverse events of first-line ADAPT with those of first-line stent retrievers in patients with acute ischemic stroke.
Methods
Article Search Strategy
A structured search on PubMed, Web of Science, and LISTA (EBSCO) was conducted using the keywords intra-arterial thrombectomy, thrombosuction, stent retriever, stent-retriever, and acute ischemic stroke through August 2017. We identified all studies that related to comparisons of stent retrievers and ADAPT in patients with acute ischemic stroke. This study was conducted and the results were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (18) (Supplementary Material).
Article Selection
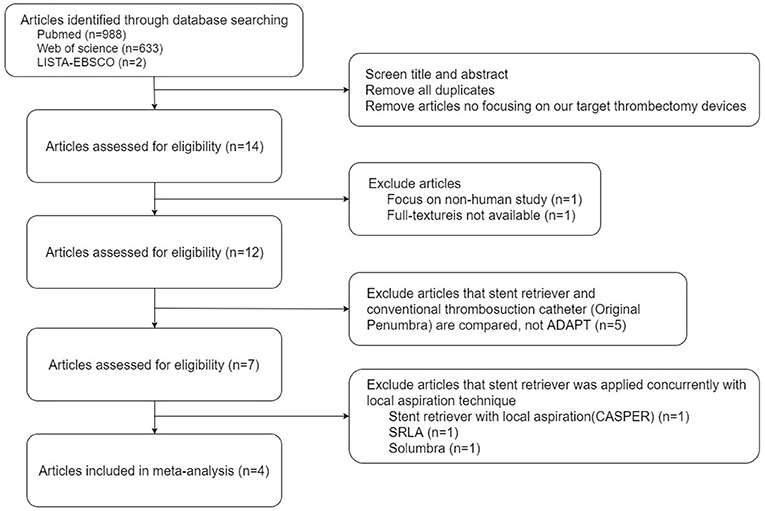
A total of 1623 papers were found. The titles and abstracts of all articles were screened by a first investigator (KH). The second and third investigators (KC and CC) reached a consensus when disagreement occurred. After excluding duplicates, articles that did not focus on our target thrombectomy devices, nonhuman studies, and articles without an available full text, 12 papers were recorded. The 5 studies that included the conventional thrombosuction catheter (Original Penumbra System) but not ADAPT were excluded (19–23). From the remaining 7 articles, 3 were excluded because they used a stent retriever concurrently with the local aspiration technique [stent retriever with local aspiration; CASPER (24), SRLA (10), or Solumbra (25)].
Finally, 4 articles were included in our meta-analysis, and the full texts of selected articles were reviewed for further study (17, 26–28) (Figure 1).
Data Extraction and Study Appraisal
Data were extracted independently by KH. and KC. and verified by other authors. Any disparities in prevalence data were resolved by consensus-based discussions among authors. The following parameters were extracted from the articles: demographic profiles (number of patients, sex, and age), disease status [lesion location and the initial National Institute of Health Stroke Scale (NIHSS)], therapeutic information [the use of intravenous tissue plasminogen activator (IV-tPA)] and the interval between arterial puncture and recanalization), and information regarding applied thrombectomy devices (first-line stent retriever or first-line ADAPT, and the detailed device model). The primary outcome was the proportion of patients with the Thrombolysis in Cerebral Ischemia (TICI) scale of 2b or 3 at the end of all procedures, corresponding to the reperfusion of at least 50% of the affected vascular territory. Secondary outcomes were the proportion of patients with functional independence [the Modified Rankin Scale (mRS) of 0–2 at the third month], the proportion of patients with the Thrombolysis in Cerebral Ischemia (TICI) scale of 2b or 3 by primary chosen device, and the proportion of patients who received rescue therapies. Rescue therapy was defined as the application of other endovascular techniques, devices, or medication different from those used primarily. Safety outcomes were the proportion of patients with symptomatic intracranial hemorrhage (sICH) and the all-cause mortality rate within 3 months.
After the final list of full-text articles was obtained, 2 authors (KH and KC) independently reviewed all the included studies and evaluated them using the Critical Appraisal Skills Programme (CASP) tools, including the CASP randomized controlled trial (RCT) checklist (29) and the CASP cohort study checklist (30), which consisted of 11 questions for RCTs and 12 questions for cohort studies, respectively. The impact of publication bias on the results of the meta-analysis was assessed by using Deek funnel plots (Supplementary Material) (31).
Statistical Analysis
A meta-analysis was conducted using the software Comprehensive Meta-Analysis (Version 3, Biostat, Englewood, NJ, USA). Six major factors, including the primary outcome (the TICI scale at the end of all procedures), secondary outcomes (the mRS at the third month, the TICI scale by primary chosen device, and the proportion of patients who received rescue therapies), and safety outcomes (the proportion of patients with postprocedural sICH and the mortality rate within 3 months), were compared because these factors are of important value in clinical practice and correlate with the long-term outcomes of patients with stroke. Study-level odds ratios (ORs) with 95% confidence intervals (CIs), P-values, and results of tests for heterogeneity (Cochran Q test, Tau2 value, I2 value, and P-value) were all calculated. We also assumed that statistical heterogeneity existed when the I2 value was higher than 50%. Otherwise, forest plots based on ORs and 95% CIs were illustrated to compare pooled treatment effects and major complications between first-line stent retriever and first-line ADAPT groups.
Results
Study Characteristics
All 4 studies included in our meta-analysis had been published from 2016 to 2017. Of these 4 studies, one was a RCT, one was a prospective nonrandomized cohort study, and the remaining 2 were retrospective cohort studies. The CASP score of the RCT was 11, and the CASP scores of other non-RCT studies were all greater than or equal to 10. The quality of the evidence of all these studies was satisfactory (Table 1).
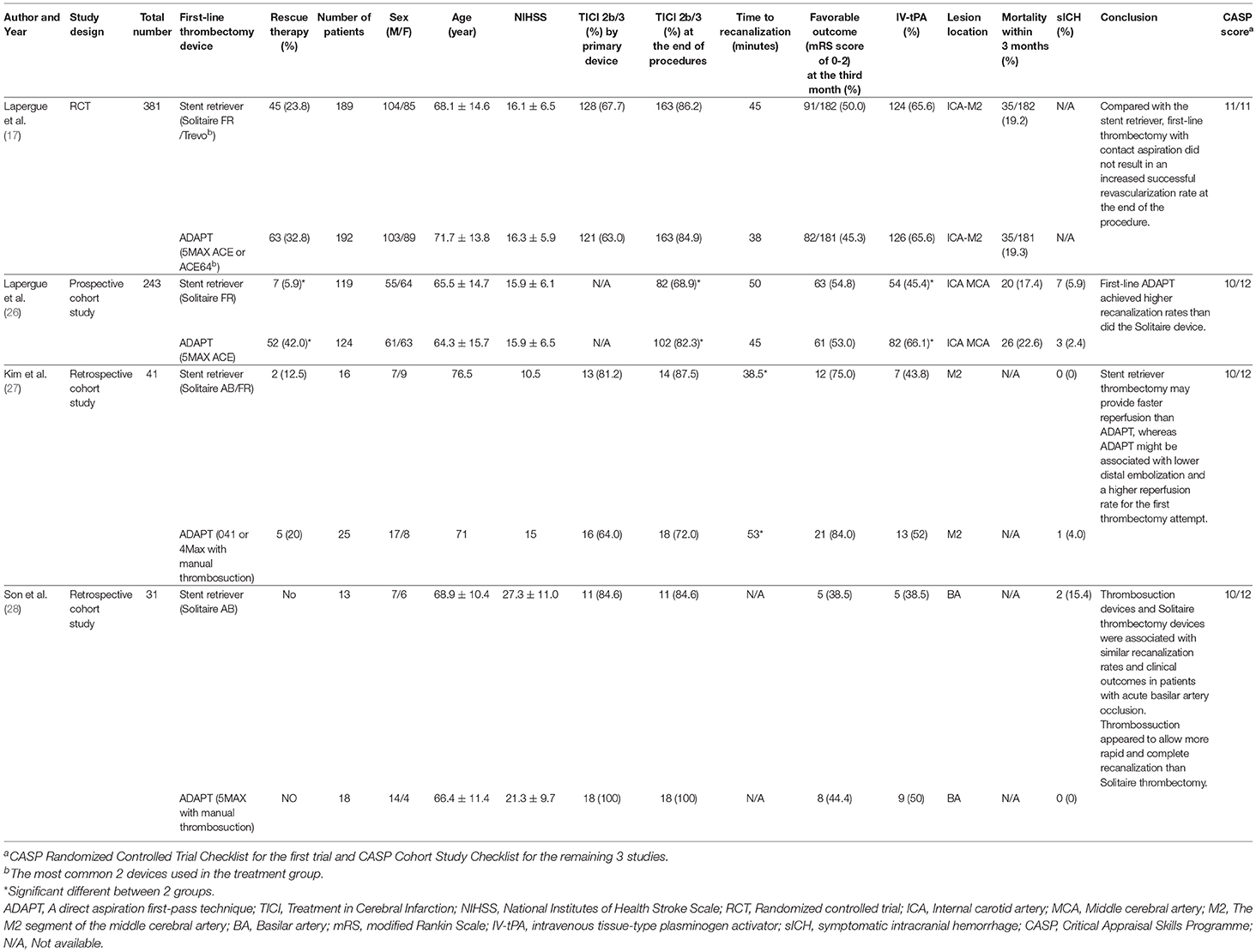
Table 1. Comparison of major demographic profiles; disease statuses; therapeutic information; the applied thrombectomy devices; and primary, secondary, and safety outcomes of the studies included.
Patient Profiles
In the meta-analysis, 696 patients were eligible for analysis, including 368 men, and 328 women with mean age ranging from 64.3 to 76.5 years. A stent retriever was used as the first-line thrombectomy device in 337 patients (48.4%), and ADAPT was used as the first-line therapy in 359 patients (51.6%). The initial mean NIHSS ranged from 10.5 to 27.3; the mean time to recanalization ranged from 38 to 53 min; the percentage of synchronized IV-tPA usage ranged from 38.5 to 66.1%. The lesions included in these studies were in the internal carotid artery, middle cerebral artery (M1 and M2 segments), and basilar artery (Table 1).
Primary Outcome—TICI Scale at the End of All Procedures
Regarding the proportion of patients with TICI scale of 2b or 3 at the end of all procedures, 2 of the included studies reported that the first-line ADAPT group had a higher proportion of patients with TICI scale of 2b or 3. By contrast, the other 2 studies tended to favor first-line stent retriever usage. The pooled primary outcome (TICI scale at the end of all procedures) showed a tendency to be more favorable in the first-line ADAPT group; however, no significant difference was observed between the 2 groups (OR = 0.78, 95% CI = 0.52-1.16, P = 0.22). Because there is heterogeneity between studies (I2 = 59.43%), we excluded the study conducted by Lapergue et al. (26) to eliminate the heterogeneity. The pooled proportion of patients with TICI scale of 2b or 3 at the end of all procedures were 86.2% in first-line stent retriever group and 84.7% in first-line ADAPT group. The revised primary outcome still showed no significant difference between the 2 groups (OR = 1.14, 95% CI = 0.67-1.95, P = 0.63, I2 = 31.56%, Figure 2).
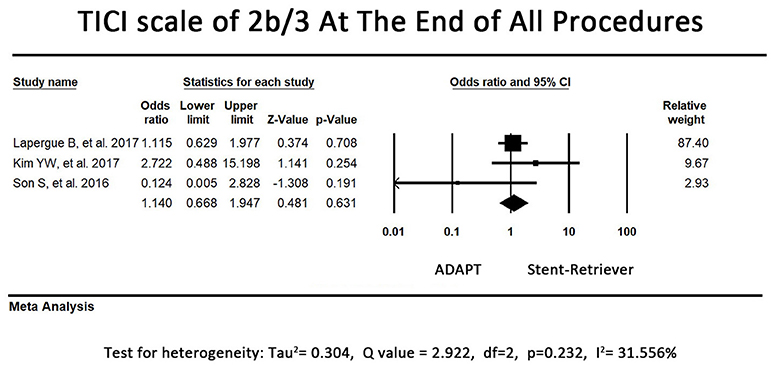
Figure 2. Forest plot of the primary outcome (TICI 2b/3 at the end of all procedures). There is no difference between the first-line ADAPT group and the first-line stent retriever group. (TICI: Treatment in Cerebral Infarction).
Secondary Outcome – mRS at the Third Month
The direction of the effect favored first-line ADAPT use in 2 of the included studies. The other 2 included studies revealed a tendency to be more favorable in the first-line stent retriever group, although adjusted ORs for the treatment were not significant. The pooled rates of functional independence in the third month did not differ between the first-line ADAPT group and the first-line stent retriever group (OR = 1.16, 95% CI = 0.86-1.56, P = 0.35, I2 = 0.00%, Figure 3).
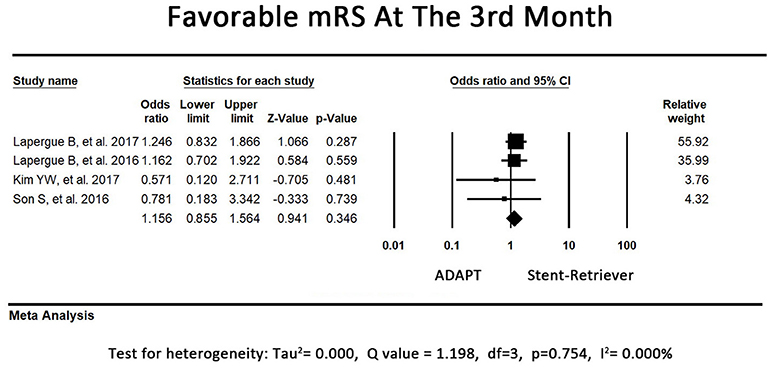
Figure 3. Forest plot for secondary outcome (mRS at the third month). There is no difference between the first-line ADAPT group and the first-line stent retriever group. (mRS: modified rankin scale).
Secondary Outcome—TICI Scale by Primary Chosen Device
Regarding the proportion of patients with TICI scale of 2b or 3 by primary chosen device alone, one study (26) was excluded because the data of TICI scale by primary chosen device was not available. 2 of the included studies reported that the first-line stent-retriever group had a higher proportion of patients with TICI scale of 2b or 3 when stent-retriever was used alone. However, another study tended to favor primary ADAPT usage. The pooled proportion of patients with TICI scale of 2b or 3 by primary chosen device were 69.7% in first-line stent retriever group and 65.6% in first-line ADAPT group. The pooled secondary outcome (TICI scale by primary chosen device) showed no significant difference between the 2 groups (OR = 1.25, 95% CI = 0.83-1.86, P = 0.29, I2 = 30.19%, Figure 4).
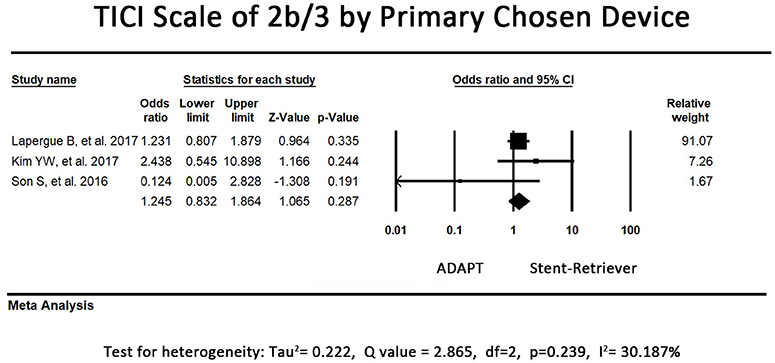
Figure 4. Forest plot for the secondary outcome (TICI 2b/3 by primary chosen device). There is no difference between the first-line ADAPT group and the first-line stent retriever group. (TICI: Treatment in Cerebral Infarction).
Secondary Outcome—Proportion of Patients Who Received Rescue Therapies
The rescue therapy data was available in 3 articles and the pooled meta-analysis showed significantly higher rates of application of rescue therapy in the first-line ADAPT group (OR = 0.42, 95% CI = 0.28-0.61, P < 0.001). The pooled recanalization rates of applied rescue therapy in the stent-retriever group and the first-line ADAPT group were 76.6% and 64.7%, respectively (p = 0.17).
Safety Outcomes—sICH
In 3 of the included studies, the first-line stent retriever group tended to have a higher rate of postprocedural sICH. However, an opposite result was observed in the remaining study. The pooled result of sICH did not significantly differ between the first-line ADAPT group and the first-line stent retriever group (OR = 1.56, 95% CI = 0.78-3.13, P = 0.21, I2 = 0.00%, Figure 5).
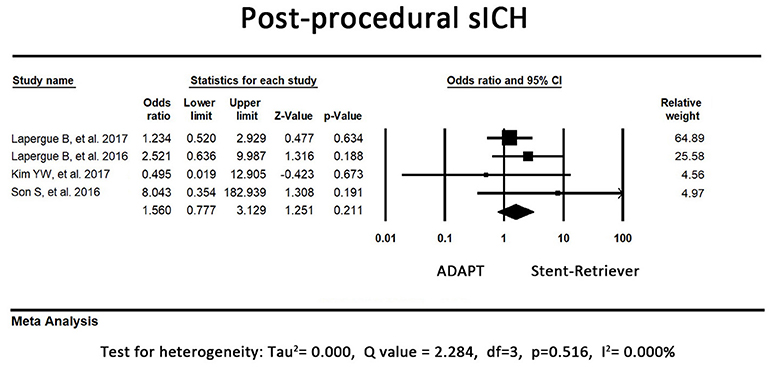
Figure 5. Forest plot for the postprocedural sICH. There is no difference between the first-line ADAPT group and the first-line stent retriever group. (sICH: symptomatic intracranial hemorrhage).
Safety Outcomes—All-Cause Mortality Rate Within 3 Months
In one study, the first-line stent retriever group tended to have a higher mortality rate within 3 months. Another study revealed a controversial result. The remaining 2 studies did not record the exact time of mortality after the procedure; thus, their results were not included in our analysis. The pooled all-cause mortality rate within 3 months did not differ between the first-line ADAPT group and the first-line stent retriever group (OR = 0.91, 95% CI = 0.61-1.36, P = 0.65, I2 = 0.0%, Figure 6).
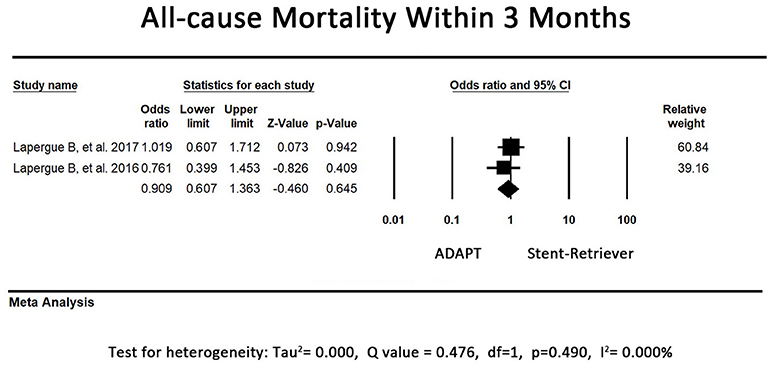
Figure 6. Forest plot for the all-cause mortality rate within 3 months. There is no difference between the first-line ADAPT group and the first-line stent retriever group.
Comparison of Time to Recanalization
The time to recanalization was defined as the time interval between arterial puncture and the recanalization of the occluded artery. The weighted average time to recanalization was 46.5 min in the first-line stent retriever group versus 41.6 min in the ADAPT group.
Discussion
Our results revealed no significant difference between these 2 strategies of management in the primary outcome (TICI scale score at the end of all procedures), secondary outcomes (mRS score in the third month, TICI scale score by primary chosen device), and all safety outcomes (proportion of patients with sICH and the all-cause mortality rate within 3 months). The proportions of patients with TICI scale of 2b or 3 by primary chosen device were not significant different in studies managed occlusions in the M2 segment of MCA (27), basilar artery (28) and internal carotid artery to the M2 segment of MCA (17). The result suggested that the efficacies of stent-retriever and ADAPT were equivalent for clots in these different locations.
In ADAPT, the largest caliber aspiration catheter that the vessel could accommodate was applied, including ACE68, ACE64, ACE60, 5MAX, 4MAX, 041, and 3MAX reperfusion catheters. The coaxial system was navigated and positioned immediately in contact with the clot (32). Aspiration was then performed using either a syringe or the Penumbra aspiration pump. Theoretically, ADAPT should take less time to recanalize the target artery because a stent retriever must be passed through the clot. On the basis of the weighted average data, the procedure time for both techniques was comparable, but ADAPT could be completed marginally faster than the stent retrieval technique (41.6 vs. 46.5 min). However, we could not evaluate whether the procedure time was significantly different between these 2 techniques because most of the studies did not provide detailed statistical data of time to recanalization. It is noteworthy that the overall time spent for revascularization in the 2 groups was equivalent, despite the truth that the ADAPT group applied salvage therapies more frequently. This may be a consequence of the fact that ADAPT does not preclude the operator from incorporating other devices if the front-line aspiration is not working. Having the large bore aspiration catheter at the face of the clot facilitates the use of adjunctive devices for rescue therapies because it provides a direct conduit to the thrombus (9). Since longer time in occlusion has been proved to result in more quantities of tissue at risk of becoming infarcted core (33), ADAPT may provide some advantages in the management of acute stroke.
The reperfusion rate was chosen as the primary outcome because a high reperfusion rate is associated with superior clinical outcomes (1, 2, 4, 5, 7). Obtaining a TICI score of 2b or 3 was defined as successful revascularization. This score was assessed before and after the application of rescue therapies because we would like to assess the efficacy of the first-line endovascular strategy after the entire procedure and when they were used alone. Despite the recanalization rate by primary chosen devices were comparable in both groups (Figure 4), the ADAPT group applied more rescue therapies. It means not all cases failed in first-line device received rescue therapy. The reason why ADAPT group had higher proportion of rescue therapy application may also be related to the advantage of its large bore aspiration system, making it less complicated to apply adjunctive devices such as stent retrievers or angioplasty balloon catheter for rescue therapy. The overall TICI 2b/3 rates at the end of all procedures in both groups were comparable, ranging from 68.9 to 100%. The revascularization rate was higher than that reported for patients treated using IV-tPA, which ranged from approximately 21.25 to 33% (34, 35).
The mRS at the third month was chosen as the major secondary outcome, which is a crucial indicator of functional independence. Our results showed that the functional independence rates were similar in the first-line ADAPT and the first-line stent retriever groups, ranging from 38.5 to 84%. We chose the proportion of patients with postprocedural sICH and the all-cause mortality rate within 3 months as our safety outcomes. Several studies have reported lower rates of symptomatic hemorrhages in ADAPT groups than in stent retriever groups (26, 28). However, our overall results revealed no difference in the proportion of patients with sICH between the 2 groups. The mortality rate within 3 months also showed no difference between the 2 groups, though 2 studies were not included in this analysis because they did not report detailed statistical data regarding mortality (27).
In addition to therapeutic outcomes, the choice of thrombectomy devices is also an issue of value-based care (36). Value in health care is a relationship between cost and clinical outcomes. The most cost-effective method of achieving favorable outcomes in patients with acute stroke with large vessel occlusion has been debated in a new trial (37). On the basis of the practice environment in the United States, the average estimated cost for first-line ADAPT with 5MAX ACE alone was $4,916 per case compared with an estimated cost of $9,620 if a first-line stent retriever was used (38). Thus, it seems that first-line ADAPT is a more cost-effective approach in terms of its technical success rate and functional independence rate compared with the stent retriever technique (10). However, our results also showed a significantly higher rate of application of salvage therapies in the first-line ADAPT group, which indicates that up to 31% of patients who received front-line ADAPT also received additional therapies, mostly stent retrievers, at an additional cost. Therefore, which technique is the most cost effective therapy still remains controversial.
Limitations
This study is constrained by several limitations. Studies that applied ADAPT and stent retrievers simultaneously as the first-line strategy were excluded because this was not acceptable in our experimental design. The excluded techniques included CASPER (24), SRLA (10), and Solumbra (25). The efficacy of combining ADAPT and stent retrievers to obtain a better rate of recanalization is a potential area of our future work. Second, though we have already excluded studies using different techniques, there is still minor heterogeneity of the ADAPT technique (various catheter sizes and aspiration techniques) and the patient population (includes anterior and posterior circulation stroke) between the included studies. Third, most included ADAPT studies were not RCT and had small sample sizes, which may result in overestimate the effect size of outcomes and limit the interpretation of pooled data. Fourth, the rescue therapies applied in studies are not concordant. ADAPT, stent retrievers, combined techniques and angioplasty with or without stenting were applied as rescue therapies in the study conducted by Lapergue et al. (17). In Kim et al. study, the applied rescue therapies were ADAPT, stent retrievers, and intra-arterial administration of tirofiban (27). In another study conducted by Lapergue et al. (26), ADAPT and stent retrievers were the only applied rescue techniques. Because detailed information of applied rescue therapies in different subgroups was lacking, we could not investigate the effects of different rescue strategies. Fifth, more detailed data for lesions in different locations are not accessible, so we were not able to evaluate the efficacy and safety of these two strategies in different segment and laterality of arteries. Finally, other important factors including the application of a balloon guide catheter and the type of anesthesia has been proved to affect functional outcomes in intra-arterial thrombectomy (39, 40). A comparison between these factors was not performed in this study and will be one of our future investigations.
Conclusion
Among first-line thrombectomy devices for patients with ischemic stroke, ADAPT with the latest Penumbra thrombosuction system was as efficient and safe as stent retrievers, irrespective of the post-thrombectomy TICI scale, mRS at the third month, sICH and all-cause mortality rate within 3 months.
Data Availability Statements
All datasets for this study are included in the manuscript and the supplementary files.
Author Contributions
KL-CH, K-IC, S-JC, and YC involved in article review, data collection, preparation, and revision of the manuscript. H-HW involved in statistical revision. C-YC involved in revision of the manuscript. All authors read and approved the final manuscript.
Funding
Ministry of Science and Technology, Taiwan (MOST 105-2314-B-038-049, 106-2314-B-038-033, and 105-2221-E-038-007-MY3).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2018.00801/full#supplementary-material
Data Sheet 1. Funnel plot of standard error by log odds ratio.
Data Sheet 2. PRISMA 2009 checklist.
References
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. (2015) 372:11–20. doi: 10.1056/NEJMoa1411587
2. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. (2015) 372:1009–18. doi: 10.1056/NEJMoa1414792
3. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. (2015) 372:1019–30. doi: 10.1056/NEJMoa1414905
4. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. (2015) 372:2296–306. doi: 10.1056/NEJMoa1503780
5. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. (2015) 372:2285–95. doi: 10.1056/NEJMoa1415061
6. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA (2016) 316:1279–88. doi: 10.1001/jama.2016.13647
7. Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet (2016) 387:1723–31. doi: 10.1016/s0140-6736(16)00163-x
8. Turk AS, Spiotta A, Frei D, Mocco J, Baxter B, Fiorella D, et al. Initial clinical experience with the ADAPT technique: A direct aspiration first pass technique for stroke thrombectomy. J NeuroIntervent Surgery (2014) 6:231–7. doi: 10.1136/neurintsurg-2013-010713
9. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. (2014) 6:260–4. doi: 10.1136/neurintsurg-2014-011125
10. Turk AS, Turner R, Spiotta A, Vargas J, Holmstedt C, Ozark S, et al. Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. (2015) 7:666–70. doi: 10.1136/neurintsurg-2014-011282
11. Frei D, McGraw C, McCarthy K, Whaley M, Bellon RJ, Loy D, et al. A standardized neurointerventional thrombectomy protocol leads to faster recanalization times. J Neurointerv Surg. (2016). doi: 10.1136/neurintsurg-2016-012716
12. Simon SD, Grey CP. Hydrodynamic comparison of the Penumbra system and commonly available syringes in forced-suction thrombectomy. J Neurointerv Surg. (2014) 6:205–11. doi: 10.1136/neurintsurg-2012-010638
13. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke (2007) 38:967–73. doi: 10.1161/01.STR.0000258112.14918.24
14. Kowoll A, Weber A, Mpotsaris A, Behme D, Weber W. Direct aspiration first pass technique for the treatment of acute ischemic stroke: initial experience at a European stroke center. J Neurointerv Surg. (2016) 8:230–4. doi: 10.1136/neurintsurg-2014-011520
15. Maegerlein C, Prothmann S, Lucia KE, Zimmer C, Friedrich B, Kaesmacher J. Intraprocedural thrombus fragmentation during interventional stroke treatment: a comparison of direct thrombus aspiration and stent retriever thrombectomy. Cardiovasc Intervent Radiol. (2017) 40:987–93. doi: 10.1007/s00270-017-1614-4
16. Kim SK, Yoon W, Moon SM, Park MS, Jeong GW, Kang HK. Outcomes of manual aspiration thrombectomy for acute ischemic stroke refractory to stent-based thrombectomy. J Neurointerv Surg. (2015) 7:473–7. doi: 10.1136/neurintsurg-2014-011203
17. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA (2017) 318:443–52. doi: 10.1001/jama.2017.9644
18. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
19. Kass-Hout T, Kass-Hout O, Sun CH, Kass-Hout T, Belagaje S, Anderson A, et al. Clinical, angiographic and radiographic outcome differences among mechanical thrombectomy devices: initial experience of a large-volume center. J Neurointerv Surg. (2015) 7:176–81. doi: 10.1136/neurintsurg-2013-011037
20. Choi JH, Park HS, Kim DH, Cha JK, Huh JT, Kang M. Comparative analysis of endovascular stroke therapy using urokinase, penumbra system and retrievable (Solitare) stent. J Korean Neurosurg Soc. (2015) 57:342–9. doi: 10.3340/jkns.2015.57.5.342
21. Hann S, Chalouhi N, Starke R, Gandhe A, Koltz M, Theofanis T, et al. Comparison of neurologic and radiographic outcomes with Solitaire versus Merci/Penumbra systems for acute stroke intervention. Biomed Res Int. (2013) 2013:715170. doi: 10.1155/2013/715170
22. Hentschel KA, Daou B, Chalouhi N, Starke RM, Clark S, Gandhe A, et al. Comparison of non-stent retriever and stent retriever mechanical thrombectomy devices for the endovascular treatment of acute ischemic stroke. J Neurosurg. (2017) 126:1123–30. doi: 10.3171/2016.2.JNS152086
23. Deshaies EM, Singla A, Villwock MR, Padalino DJ, Sharma S, Swarnkar A. Early experience with stent retrievers and comparison with previous-generation mechanical thrombectomy devices for acute ischemic stroke. J Neurosurg (2014) 121:12–7. doi: 10.3171/2014.2.JNS131372
24. Stapleton CJ, Leslie-Mazwi TM, Torok CM, Hakimelahi R, Hirsch JA, Yoo AJ, et al. A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg (2017) 128:567–74. doi: 10.3171/2016.11.JNS161563
25. Delgado Almandoz JE, Kayan Y, Young ML, Fease JL, Scholz JM, Milner AM, et al. Comparison of clinical outcomes in patients with acute ischemic strokes treated with mechanical thrombectomy using either Solumbra or ADAPT techniques. J Neurointerv Surg. (2016) 8:1123–8. doi: 10.1136/neurintsurg-2015-012122
26. Lapergue B, Blanc R, Guedin P, Decroix JP, Labreuche J, Preda C, et al. A Direct Aspiration, First Pass Technique (ADAPT) versus stent retrievers for acute stroke therapy: an observational comparative study. AJNR Am J Neuroradiol. (2016) 37:1860–5. doi: 10.3174/ajnr.A4840.PubMedPMID:27256852.
27. Kim YW, Son S, Kang DH, Hwang YH, Kim YS. Endovascular thrombectomy for M2 occlusions: comparison between forced arterial suction thrombectomy and stent retriever thrombectomy. J Neurointerv Surg. (2017) 9:626–30. doi: 10.1136/neurintsurg-2016-012466
28. Son S, Choi DS, Oh MK, Hong J, Kim SK, Kang H, et al. Comparison of Solitaire thrombectomy and Penumbra suction thrombectomy in patients with acute ischemic stroke caused by basilar artery occlusion. J Neurointerv Surg. (2016) 8:13–8. doi: 10.1136/neurintsurg-2014-011472
29. CASP (Randomised Controlled Trial) Checklist, Critical Appraisal Skills Programme (2017). Available online at: http://docs.wixstatic.com/ugd/dded87_4239299b39f647ca9961f30510f52920.pdf (Accessed January 20, 2018)
30. CASP (Cohort Study) Checklist, Critical Appraisal Skills Programme (2017). Available online at: http://docs.wixstatic.com/ugd/dded87_5ad0ece77a3f4fc9bcd3665a7d1fa91f.pdf (Accessed January 20, 2018)
31. Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. (2005) 58:882–93. doi: 10.1016/j.jclinepi.2005.01.016
32. Altenbernd J, Kuhnt O, Hennigs S, Hilker R, Loehr C. Frontline ADAPT therapy to treat patients with symptomatic M2 and M3 occlusions in acute ischemic stroke: initial experience with the Penumbra ACE and 3MAX reperfusion system. J Neurointerv Surg. (2017) 10:434–9. doi: 10.1136/neurintsurg-2017-013233
33. Becktepe JS, You SJ, Berkefeld J, Neumann-Haefelin T, Singer OC. Clinical outcome after mechanical recanalization as mono- or adjunctive therapy in acute stroke: importance of time to recanalization. Cerebrovasc Dis. (2011) 32:211–8. doi: 10.1159/000328814
34. Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke (2010) 41:2254–8. doi: 10.1161/STROKEAHA.110.592535
35. Seners P, Turc G, Maier B, Mas JL, Oppenheim C, Baron JC. Incidence and predictors of early recanalization after intravenous thrombolysis: a systematic review and meta-analysis. Stroke (2016) 47:2409–12. doi: 10.1161/STROKEAHA.116.014181
36. Burwell SM. Setting value-based payment goals–HHS efforts to improve U.S. health care. N Engl J Med. (2015) 372:897–9. doi: 10.1056/NEJMp1500445
37. Chandra RV, Leslie-Mazwi TM, Mehta BP, Derdeyn CP, Demchuk AM, Menon BK, et al. Does the use of IV tPA in the current era of rapid and predictable recanalization by mechanical embolectomy represent good value? J Neurointerv Surg. (2016) 8:443–6. doi: 10.1136/neurintsurg-2015-012231
38. Vidal GA, Milburn JM. The Penumbra 5MAX ACE catheter is safe, efficient, and cost saving as a primary mechanical thrombectomy device for large vessel occlusions in acute ischemic stroke. Ochsner J. (2016) 16:486–91.
39. Ouyang F, Chen Y, Zhao Y, Dang G, Liang J, Zeng J. Selection of patients and anesthetic types for endovascular treatment in acute ischemic stroke: a meta-analysis of randomized controlled trials. PLoS ONE (2016) 11:e0151210. doi: 10.1371/journal.pone.0151210
Keywords: ADAPT, stent-retriever, intra-arterial thrombectomy, stroke, thrombosuction, penumbra
Citation: Hsieh KL-C, Chuang K-I, Weng H-H, Cheng S-J, Chiang Y and Chen C-Y (2018) First-Line A Direct Aspiration First-Pass Technique vs. First-Line Stent Retriever for Acute Ischemic Stroke Therapy: A Meta-Analysis. Front. Neurol. 9:801. doi: 10.3389/fneur.2018.00801
Received: 29 March 2018; Accepted: 05 September 2018;
Published: 25 September 2018.
Edited by:
Camilo R. Gomez, Loyola University Chicago, United StatesReviewed by:
Angelos A. Konstas, Massachusetts General Hospital, Harvard Medical School, United StatesNabil Kitchener, Cairo University, Egypt
Copyright © 2018 Hsieh, Chuang, Weng, Cheng, Chiang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng-Yu Chen, c2FuZHkwOTMyQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Kevin Li-Chun Hsieh
Kevin Li-Chun Hsieh Kai-I Chuang
Kai-I Chuang Hsu-Huei Weng
Hsu-Huei Weng Sho-Jen Cheng1
Sho-Jen Cheng1 Yu Chiang
Yu Chiang