- 1Priority Research Centre for Stroke, University of Newcastle and Hunter Medical Research Institute, Newcastle, NSW, Australia
- 2Discipline of General Practice, University of Newcastle, Newcastle, NSW, Australia
- 3Institute of Applied Health Research, University of Birmingham, Birmingham, United Kingdom
- 4Department of Neurology, John Hunter Hospital, Newcastle, NSW, Australia
- 5Health Service & Policy Research Group, University of Exeter – Saint Lukes Campus, Exeter, United Kingdom
- 6Faculty of Medicine, Nursing and Health Sciences, Box Hill Hospital, Monash University, Melbourne, VIC, Australia
- 7Department of Medicine, University of Auckland, Auckland, New Zealand
- 8Stroke and Aging Research, School of Clinical Sciences at Monash Health, Monash University, Clayton, VIC, Australia
- 9Florey Institute of Neuroscience and Mental Health, University of Melbourne, Melbourne, VIC, Australia
- 10AUT University, National Institute for Stroke & Applied Neurosciences, Auckland, New Zealand
- 11Nuffield Department of Clinical Neuroscience, Centre for Prevention of Stroke and Dementia, University of Oxford, Oxford, United Kingdom
- 12The Ingham Institute, SPHERE, Sydney, NSW, Australia
Background: Transient ischemic attack (TIA) and minor stroke (TIAMS) are risk factors for stroke recurrence. Some TIAMS may be preventable by appropriate primary prevention. We aimed to recruit “possible-TIAMS” patients in the INternational comparison of Systems of care and patient outcomes In minor Stroke and TIA (INSIST) study.
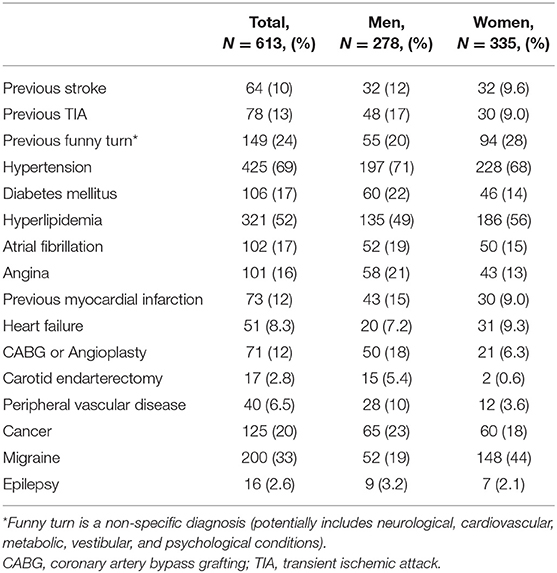
Methods: A prospective inception cohort study performed across 16 Hunter–Manning region, Australia, general practices in the catchment of one secondary-care acute neurovascular clinic. Possible-TIAMS patients were recruited from August 2012 to August 2016. We describe the baseline demographics, risk factors and pre-event medications of participating patients.
Results: There were 613 participants (mean age; 69 ± 12 years, 335 women), and 604 (99%) were Caucasian. Hypertension was the most common risk factor (69%) followed by hyperlipidemia (52%), diabetes mellitus (17%), atrial fibrillation (AF) (17%), prior TIA (13%) or stroke (10%). Eighty-nine (36%) of the 249 participants taking antiplatelet therapy had no known history of cardiovascular morbidity. Of 102 participants with known AF, 91 (89%) had a CHA2DS2-VASc score ≥ 2 but only 47 (46%) were taking anticoagulation therapy. Among 304 participants taking an antiplatelet or anticoagulant agent, 30 (10%) had stopped taking these in the month prior to the index event.
Conclusion: This study provides the first contemporary data on TIAMS or TIAMS-mimics in Australia. Community and health provider education is required to address the under-use of anticoagulation therapy in patients with known AF, possibly inappropriate use of antiplatelet therapy and possibly inappropriate discontinuation of antiplatelet or anticoagulation therapy.
Introduction
Transient ischemic attack and minor stroke (TIAMS) account for ~40% of all cerebral ischemic events (1, 2) and can precede a disabling or fatal stroke (3) and major cardiovascular events (4, 5). Recurrent stroke usually occurs very early after TIAMS (6) and rapid specialist assessment and intervention has been shown to reduce this risk (7, 8). Therefore, a rapid response within the system of care is required to initiate secondary prevention strategies (4, 8). Current evidence-based guidelines include recommendation for rapid treatment and/or rapid specialist referral (9). Clinical diagnosis of TIAMS is often challenging and it can be difficult to distinguish TIAMS from benign, low risk “stroke-mimic” syndromes (10, 11). Further, it is uncertain how compliant primary health care practitioners are with guidelines directed at the management of TIAMS and how applicable the guidelines are in primary care settings.
In the INternational comparison of Systems of care and patient outcomes In minor Stroke and Tia (INSIST) study (12), we recruited “possible-TIAMS” patients presenting to primary and secondary care settings. The aim of this study was to describe baseline patient characteristics, outcomes and systems of care of all patients enrolled into the INSIST study.
Methods
The rationale and methods of the INSIST study have been previously reported (12). Patients were recruited from the Hunter and Manning valley regions of New South Wales, within the referral territory of the Acute Neurovascular Clinic (ANVC) at the John Hunter Hospital between August 2012 and August 2016. The John Hunter Hospital is the major teaching and referral hospital of the Hunter New England Local Health District. Patients attended one of 16 general practices (11 urban and 5 rural practices including 2 where general practitioners (GPs) staff the local hospitals) within the geographic footprint of the Hunter New England and Central Coast Primary Health Network (HNECCPHN) (Figure 1). The estimated population within the HNECCPHN region is 1,200,000 of whom 18.3% are aged 65+ years (compared to 14.4% nationally) and 18.5% have circulatory system disease (17.3% prevalence nationally) (13).
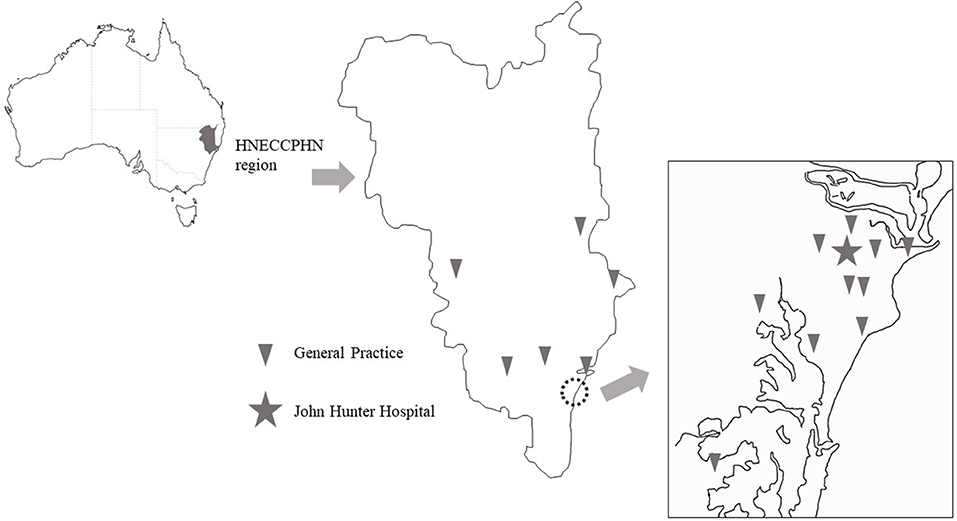
Figure 1. Locations of participating general practices in the Hunter New England and Central Coast Primary Health Network (HNECCPHN) region.
In this study, TIAMS was ascertained using multiple overlapping methods; primarily general practice records but also from hospital emergency departments, after-hours GP services, hospital inpatient admissions and discharges and ANVC attendance at John Hunter Hospital (12). All patients with a possible diagnosis of TIAMS were invited to participate. Episodes with symptoms lasting <24 h were classified as TIAs, and prolonged (>24 h) episodes with National Institute of Health Stroke Scale < 5 at presentation were classified as minor strokes. Patients with both (i) symptoms lasting more than 24 h and (ii) National Institute of Health Stroke Scale >5 at presentation, were excluded. Information recorded at the baseline interview included demographics (age, sex, ethnicity, residence, marital status, education, pre-event employment status, recent occupation, socioeconomic status of area residence [Socio-Economic Index for Area, Index of Relative Socio-economic Disadvantage [SEIFA IRSD] (14)], lifestyle factors (smoking status, alcohol consumption, exercise hours), past medical history and pre-event medications. Further data was obtained from participants' clinical notes.
Results
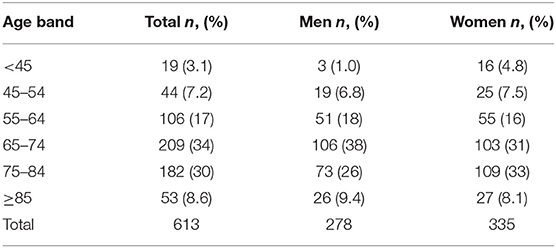
During this study, there were 1,363 patients where TIAMS was considered a possible diagnosis whereby 643 consented to participate (response rate 47%), and 613 (335 women; mean [SD] age, 69.8 [12.0] years) completed the baseline interview. Among 613 participants, 298 were adjudicated as TIAMS of whom 175 (29%) had TIA and 123 (20%) had minor stroke. Prior to the index event, 550 (90%) participants were functionally independent (Modified Rankin Scale 0–2).
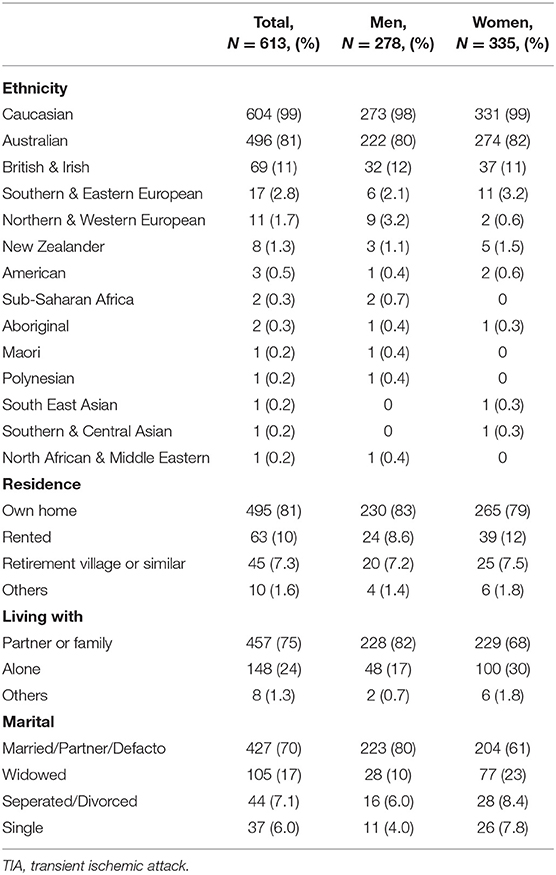
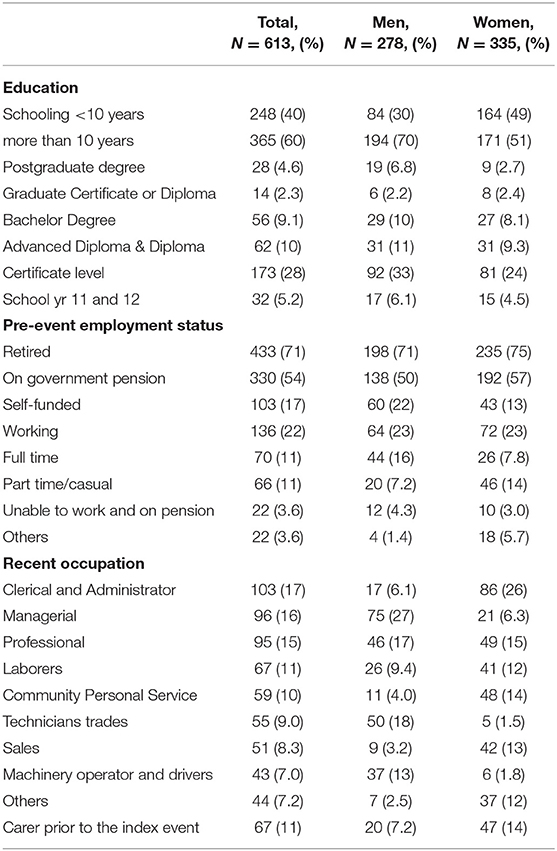
Participants were somewhat older (on average, by 3 years), and more frequently had focal neurological symptoms, compared to non-participants (Supplemental Material). Most patients were represented across three age bands; 65–74 years (209, 34%), 75–84 years (182, 30%) and 55–64 years (106, 17%) (Table 1). Almost all the participants (604, 99%) were Caucasian. There were differences between male and female participants in marital status and living arrangements with women more likely to be widowed (77, 23% of women vs. 28, 10% of men), living alone (100, 30% vs. 48, 17%) and living in rental accommodation (39, 12 vs. 24, 9%) (Table 2). Education status was divided into more or less than 10 years of schooling with 365 (60%) having education beyond 10 years (Table 3). Attainment of high school certificate was the most common education level of men (92, 33%) and women (81, 24%). Most of the participants (433, 71%) were retired (330, 54% on a government pension and 103, 17% on a self-funded retirement) and 136, 22% were working (70, 11% in full time and 66, 11% in part time/casual employment). The distribution of socioeconomic status of area (SEIFA IRSD—an area-based weighted measure of social and economic resources of people and household, expressed as a decile) is shown in Figure 2.
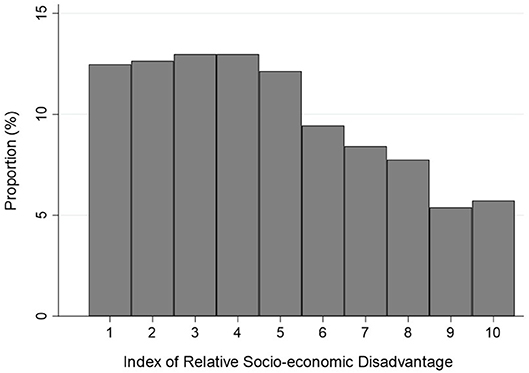
Figure 2. Index of Relative Socio-economic Disadvantage. This index is a general socio-economic index that summarizes a wide range of information about the economic and social resources of people and households within an area. Because this index focuses on disadvantage, only measures of relative disadvantage are included. This means that a high score reflects a relative lack of disadvantage rather than relative advantage.
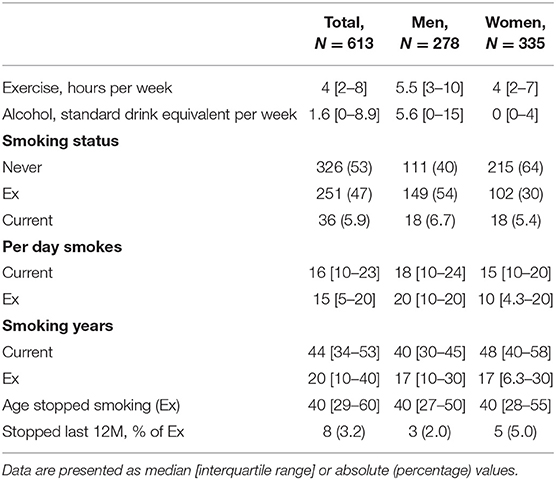
In terms of vascular risk factors, 326 (53%) had never smoked tobacco, 251 (41%) were ex-smokers and 36 (5.9%) were current smokers (Table 4). The median age at which the ex-smokers stopped was 40 years for both men and women. Alcohol intake ranged from 0 standard drink equivalents per week in 42% (79, 28% men and 180, 54% women), to 1–5 standard drink equivalents per week in 24% (61, 22% men and 88, 26% women). Ten percent of the population reported no exercise (22, 8% men and 42, 13% women).
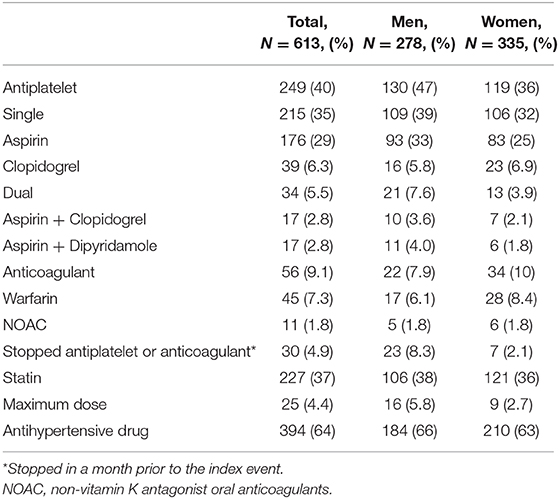
Hypertension was the most common (425, 69%) risk factor, followed by hyperlipidemia (321, 52%), diabetes mellitus (106, 17%), atrial fibrillation (AF) (102, 17%), previous TIA (78, 13%) and previous stroke (64, 10%) (Table 5). At the time of the possible TIAMS, 249 (40%) participants were taking antiplatelet therapy (215, 35% single and 34, 5.5% dual antiplatelet therapy) with aspirin being the most common single agent (176, 29% of all participants) (Table 6).
Two hundred and thirty-one participants (38%) had at least one known cardiovascular morbidity (stroke, transient ischemic attack, angina, myocardial infarction, coronary artery bypass grafting or angioplasty, carotid endarterectomy and peripheral vascular disease) at the time of the event, of whom 158 (68%) were taking an antiplatelet agent, 33 (14%) were taking an anticoagulation agent, including 28 with AF. 89 (36%) of the 249 people taking antiplatelet therapy had no known history of cardiovascular morbidity. Among these 89 patients, 19 (21%) had a history of “funny turn” (funny turn is not a specific diagnosis and potentially includes neurological, cardiovascular, metabolic, vestibular and psychological condition), 7 (7.9%) had an AF history and 5 (5.6%) had both history of a funny turn and AF. Of these 12 participants with AF, six had a CHA2DS2-VASc score ≥2.
We found that 56 of 613 (9.1%) participants were taking an anticoagulant agent at the time of the event, 45 (7.3%) warfarin and 11 (1.8%) a non-vitamin K antagonist oral anticoagulant (NOAC). In patients with a known diagnosis of AF, 47 (46%) were taking an anticoagulant despite 91 (89%) having a CHA2DS2-VASc score ≥ 2. Among 304 participants taking an antiplatelet or anticoagulant agent, 30 (10%) had stopped taking in the month prior to the index event. Anti-platelet or anti-coagulant medications were stopped in preparation for an invasive procedure in 14 (47%), by the participant on their own volition in 9 (30%), because the participant forgot to take the medication in 4 (13%), and because of bleeding in 1 (3.3%). 227 (37%) participants were taking a statin (11% at recommended maximum dose) and 394 (64%) were taking antihypertensive agents.
Discussion
The diagnosis of TIAMS and its management are complex, This study provides a comprehensive and contemporary description of “possible-TIAMS” patients who have engaged with medical care.
Generalizability of Findings—Ethnicity and Socioeconomic Status
All but nine participants were Caucasian, which is in stark contrast to the situation in Auckland, New Zealand where 78% of TIA patients were of European origin, 11% Maori/Pacific and 10% Asian/Other (15). In our study region, 48,002 (4.2%) identify as Aboriginal and/or Torres Strait Islanders (compared to 2.5% nationally) and a lower proportion of people reported being from non-English speaking backgrounds (4.5% compared to 15.7% nationally) (13). Aboriginal and Torres Strait Islander people have a three-fold greater risk of cerebrovascular diseases, and two-fold neurological conditions risk, compared to non-Indigenous Australians (16). The low proportion of Aboriginal or Torres Strait Islander participants may reflect the fact that none of the Aboriginal Medical Services in the region (where an appreciable proportion of the Aboriginal and Torres Strait Islander community access health care) elected to participate in the study. It is also possible that our findings reflect lower rates of presenting to primary or secondary care with neurological symptoms in this group.
Our study population was of relatively lower socioeconomic status compared to the distribution in the HNECCPHN population (IRSD decile 6 was the most common (42%) followed by decile 7 (32%) reported from the Australian Census 2016) (14). The proportion of participants in each SEIFA IRSD decile declining as socio-economic status decile increased. Low socioeconomic status has been associated with fatal stroke and non-fatal stroke incidence (17). Education is one of the many constituent measures included in the SEIFA– IRSD and we note that 40% of our study population had <10 years of education.
Baseline Antiplatelet and Anticoagulation Status
About one third of patients were taking antiplatelet therapy (38%) prior to the index event. This likely reflects the prior history of vascular disease. However, many of the participants were taking antiplatelet agents without an apparent indication. This finding of possible inappropriate prescription of antiplatelet agents is consistent with previous studies (18, 19). Anticoagulant therapy was underused considering the CHA2DS2-VASc score in the study population, with 46% of participants with a known diagnosis of AF treated (20). This is consistent with findings of previous studies where 23–30% of TIA patients with known AF were taking anticoagulation therapy at the time of the TIA (15, 21, 22).
This study provides evidence of a clear need for optimization of antiplatelet and anticoagulation therapy in patients with established vascular disease and AF. In particular, GPs should be encouraged to calculate CHA2DS2-VASc scores and consider the need for anticoagulation in patients presenting with AF. Presentation with possible-TIAMS provides a key opportunity to start anticoagulantion therapy if appropriate based on risk stratification and bleeding risk. The finding that antiplatelet or anticoagulation therapy had been stopped in the month prior to the index event in many patients is also a cause for concern. This highlights a need for GPs to carefully consider the potential risks and benefits when considering cessation of anticoagulation or antiplatelet therapy, and the need to promptly reinstitute therapy as soon as it is safe after temporary discontinuation.
Statin and Antihypertensive Preventive Treatment
The prevalence of statin (37%) and antihypertensive therapy (64%) used in the study population seems modest given prevalence of known hyperlipidaemia (52%) and hypertension (69%), as well as the prevalence of diabetes mellitus (17%) and previous stroke (13%). In an absolute cardiovascular risk (ACVR) analysis of a subgroup participating early in the INSIST study, 72% of participants in which ACVR could be calculated had high or moderate ACVR (23). Considering this risk proportion, the prevalence of statin and antihypertensive therapy seems relatively modest.
Strengths and Limitations
This study has a number of strengths. It is a comprehensive community-based study of TIAMS patients engaging with health systems at any level that used multiple overlapping case ascertainment methods for possible TIAMS. The study also has a number of limitations. There was a modest response or consent rate of 47%. This rate is typical of declining response rates for cohort studies (24). We did not record a past history of hemorrhage or other potential contraindications to anti-thrombotic therapy. The study was performed at a time when non-vitamin K antagonist oral anticoagulants were still relatively new with subsequent rapid uptake of these medicines and corresponding reductions in the use of warfarin (25, 26). There was a lack of representation of the Aboriginal and Torres Strait Islander community and lower number of culturally and linguistically diverse individuals than would be expected, reflecting the recruitment catchment demographics. We are therefore unable to generalize the findings to non-Caucasian populations.
Conclusions
This study provides the first contemporary data on TIAMS or TIAMS-mimics in Australia. Worryingly, we found under-use of anticoagulation therapy in patients with known AF prior to the index event and possibly inappropriate use of antiplatelet therapy. Community and health provider education is required to address the under-use of anticoagulation therapy in patients and possibly inappropriate discontinuation of antiplatelet or anticoagulation therapy.
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Ethics Statement
The studies involving human participants were reviewed and approved by Hunter New England Human Research Ethics Committee (The Reference No. is 12/04/18/4.02). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Study design: CL, PM, DL, and DQ. Data collection: DQ, HZ, CG-E, AD, NN, and MS. Data analysis: PM, DQ, and ST. Writing: ST, PM, and CL. Manuscript revision: DL, JV, HD, PB, NS, DC, and VF. All contributed for writing and revision: DL, PB, and PR.
Funding
The INSIST study was funded by NHMRC Project Grant ID 1027794. NS was the recipient of a co-funded National Health and Medical Research Council (NHMRC) Career Development/National Heart Foundation (NHF) Future Leader Fellowship (APP1110629/100827). VF's work was partly funded by the Health Research Council of New Zealand.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2020.00383/full#supplementary-material
References
1. Bamford J, Sandercock P, Dennis M, Warlow C, Jones L, Mcpherson K, et al. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project 1981-86 1. methodology, demography and incident cases of first-ever stroke. J Neurol Neurosurg Psychiatry. (1988) 51:1373–80. doi: 10.1136/jnnp.51.11.1373
2. Fischer U, Baumgartner A, Arnold M, Nedeltchev K, Gralla J, De Marchis GM, et al. What is a minor stroke? Stroke. (2010) 41:661–6. doi: 10.1161/STROKEAHA.109.572883
3. Coull AJ. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ. (2004) 328:326. doi: 10.1136/bmj.37991.635266.44
4. Amarenco P, Lavallée PC, Labreuche J, Albers GW, Bornstein NM, Canhão P, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med. (2016) 374:1533–42. doi: 10.1056/NEJMoa1412981
5. Amarenco P, Lavallée PC, Monteiro Tavares L, Labreuche J, Albers GW, Abboud H, et al. Five-year risk of stroke after TIA or minor Ischemic stroke. N Engl J Med. (2018) 379:1580–1. doi: 10.1056/NEJMc1808913
6. Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol. (2009) 8:235–43. doi: 10.1016/S1474-4422(09)70019-5
7. Rothwell PM, Warlow CP. Timing of TIAs preceding stroke: Time window for prevention is very short. Neurology. (2005) 64:817–20. doi: 10.1212/01.WNL.0000152985.32732.EE
8. Sehatzadeh S. Is transient ischemic attack a medical emergency? an evidence-based analysis. Ont Health Technol Assess Ser. (2015) 15:1–45.
9. National Stroke Foundation. Clinical Guidelines for Stroke Management. Melbourne, VIC: National Stroke Foundation (2017).
10. Castle J, Mlynash M, Lee K, Caulfield AF, Wolford C, Kemp S, et al. Agreement regarding diagnosis of transient ischemic attack fairly low among stroke-trained neurologists. Stroke. (2010) 41:1367–70. doi: 10.1161/STROKEAHA.109.577650
11. Davey AR, Lasserson DS, Levi CR, Magin PJ. Managing transient ischaemic attacks in Australia: a qualitative study. Fam Pract. (2017) 34:606–11. doi: 10.1093/fampra/cmx030
12. Levi CR, Lasserson D, Quain D, Valderas J, Dewey HM, Alan Barber P, et al. The International comparison of systems of care and patient outcomes In minor Stroke and Tia (InSIST) study: a community-based cohort study. Int J Stroke. (2019) 14:186–90. doi: 10.1177/1747493018799983
13. Hunter New England and Central Coast PHN Health Profile. (2015). Available online at: https://www.hneccphn.com.au/media/13742/hnecc-2-page-infographic.pdf (Accessed June 5, 2019).
14. Australian Bureau Statistics - Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA) Australia. (2016). Available online at: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by Subject/2033.0.55.001~2016~Main Features~SOCIO-ECONOMIC INDEXES FOR AREAS (SEIFA) 2016~1 (Accessed June 6, 2019).
15. Barber PA, Krishnamurthi R, Parag V, Anderson NE, Ranta A, Kilfoyle D, et al. Incidence of transient ischemic attack in Auckland, New Zealand, in 2011 to 2012. Stroke. (2016) 47:2183–8. doi: 10.1161/STROKEAHA.116.014010
16. Australian Burden of Disease Study Impact and Causes of Illness and Death in Aboriginal and Torres Strait Islander People. (2011). Available online at: https://www.aihw.gov.au/getmedia/e31976fc-adcc-4612-bd08-e54fd2f3303c/19667-bod7-atsi-2011.pdf.aspx?inline=true (accessed June 5, 2019).
17. Thrift AG, Dewey HM, Sturm JW, Paul SL, Gilligan AK, Srikanth VK, et al. Greater incidence of both fatal and nonfatal strokes in disadvantaged areas: the Northeast Melbourne Stroke Incidence Study. Stroke. (2006) 37:877–82. doi: 10.1161/01.STR.0000202588.95876.a7
18. Ardoino I, Rossio R, Di Blanca D, Nobili A, Pasina L, Mannucci PM, et al. Appropriateness of antiplatelet therapy for primary and secondary cardio- and cerebrovascular prevention in acutely hospitalized older people. Br J Clin Pharmacol. (2017) 83:2528–40. doi: 10.1111/bcp.13355
19. Averlant L, Ficheur G, Ferret L, Boulé S, Puisieux F, Luyckx M, et al. Underuse of oral anticoagulants and inappropriate prescription of antiplatelet therapy in older inpatients with atrial fibrillation. Drugs Aging. (2017) 34:701–10. doi: 10.1007/s40266-017-0477-3
20. ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. (2016) 37:2893–62. doi: 10.1093/eurheartj/ehw210
21. Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004. (Oxford Vascular Study). Lancet. (2004) 363:1925–33. doi: 10.1016/S0140-6736(04)16405-2
22. Huisman M V, Rothman KJ, Paquette M, Teutsch C, Diener HC, Dubner SJ, et al. The changing landscape for stroke prevention in AF: findings from the GLORIA-AF registry phase 2. J Am Coll Cardiol. (2017) 69:777–85. doi: 10.1016/j.jacc.2016.11.061
23. Clarey J, Lasserson D, Levi C, Parsonsd M, Deweyi H, Alan Barber P, et al. Absolute cardiovascular risk and GP decision making in TIA and minor stroke. Fam Pract. (2014) 31:664–9. doi: 10.1093/fampra/cmu054
24. Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol. (2006) 163:197–203. doi: 10.1093/aje/kwj036
25. Pratt NL, Ramsay EN, Caughey GE, Shakib S, Roughead EE. Uptake of novel oral anticoagulants in Australia. Med J Aust. (2016) 204:104–5. doi: 10.5694/mja15.01000
Keywords: transient ischemic attack, minor stroke, stroke-mimic syndrome, atrial fibrillation, anticoagulation therapy
Citation: Tomari S, Magin P, Lasserson D, Quain D, Valderas JM, Dewey HM, Barber PA, Spratt NJ, Cadilhac DA, Feigin VL, Rothwell PM, Zareie H, Garcia-Esperon C, Davey A, Najib N, Sales M and Levi CR (2020) The Characteristics of Patients With Possible Transient Ischemic Attack and Minor Stroke in the Hunter and Manning Valley Regions, Australia (the INSIST Study). Front. Neurol. 11:383. doi: 10.3389/fneur.2020.00383
Received: 23 January 2020; Accepted: 15 April 2020;
Published: 15 May 2020.
Edited by:
Nishant K. Mishra, Icahn School of Medicine at Mount Sinai, United StatesReviewed by:
Ioannis Leventis, University of Thessaly, GreeceDaniel Bereczki, Semmelweis University, Hungary
Copyright © 2020 Tomari, Magin, Lasserson, Quain, Valderas, Dewey, Barber, Spratt, Cadilhac, Feigin, Rothwell, Zareie, Garcia-Esperon, Davey, Najib, Sales and Levi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shinya Tomari, c255NTU4OEBnbWFpbC5jb20=
 Shinya Tomari
Shinya Tomari Parker Magin2
Parker Magin2 Daniel Lasserson
Daniel Lasserson Neil J. Spratt
Neil J. Spratt Dominique A. Cadilhac
Dominique A. Cadilhac Valery L. Feigin
Valery L. Feigin Carlos Garcia-Esperon
Carlos Garcia-Esperon Christopher R. Levi
Christopher R. Levi