- 1Department of Neurology, South Valley University Qena Faculty of Medicine, Qena, Egypt
- 2Department of Neurology, Marcus Stroke and Neuroscience Center, Emory University School of Medicine, Grady Memorial Hospital, Atlanta, GA, United States
- 3Department of Neurosurgery, College of Medicine, University of Illinois at Chicago, Chicago, IL, United States
- 4Department of Neurology, Faculty of Medicine, Assiut University, Assiut, Egypt
Background and Purpose: Successful reperfusion is a significant predictor of a good clinical outcome after mechanical thrombectomy (MT). However, some patients have a poor clinical outcome even with successful reperfusion. We aimed to study factors that predict a poor clinical outcome (90-day modified Rankin Scale ≥ 3) in patients with anterior circulation large vessel occlusion (LVO) treated by successful MT within 6 h of symptom onset.
Methods: We performed a retrospective review of a prospectively maintained MT database of all patients who underwent MT within 6 h of symptom onset for an anterior circulation LVO at our institution from May 2016 to June 2018. Uni- and multivariable analyses were performed to identify predictors of poor outcome.
Results: A total of 56 patients met the criteria for inclusion in this study. A poor outcome occurred in 31 (55.4%) patients. On univariate analysis, compared to patients with good clinical outcome, patients with poor outcome had higher mean baseline NIHSS scores (23.3 vs. 13.8, P < 0.001), were more likely to have internal carotid artery (ICA) occlusions (38.7 vs. 8%, P = 0.008), and had a higher incidence of distal clot migration (DCM) (48.4 vs. 8%, P = 0.028). Age, gender, other baseline clinical characteristics, MT technique, and incidence of hemorrhagic transformation did not differ between the two cohorts. On multivariable regression analysis, baseline NIHSS score [OR; 1.3, 95%CI [1.11–1.52], P = 0.001], site of occlusion (ICA) [OR; 8.9, 95%CI [1.3–60.9], P = 0.026], and DCM [OR; 5.77, 95%CI [1.09–30.69], P = 0.04] were independent predictors of poor outcome at 90-days.
Conclusion: Baseline NIHSS score, ICA occlusion, and DCM are independent predictors of a poor outcome after MT for anterior circulation LVO performed within 6 h of symptoms onset.
Introduction
Stroke is the third leading cause of death in developed countries and the most common cause of permanent disability (1). Mechanical thrombectomy (MT) within 6 h of symptom onset is the standard treatment for acute ischemic stroke (AIS) due to anterior circulation emergent large vessel occlusion (ELVO) (2). The guidelines extended the eligibility of MT after the results of the Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke (DEFUSE 3) (3) and the DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention with Trevo (DAWN) (4) trials up to 16 and 24 h, respectively in well-selected patients with clinical/imaging mismatch (2).
The outcome after MT depends mainly on the degree of recanalization, with the failure of recanalization is the strongest predictor of poor outcome (5). Despite the use of modern era devices and techniques for MT, which has enhanced the speediness and completeness of reperfusion of the downstream territory, the likelihood of a good functional outcome (modified Rankin Scale, mRS0-2) at 90 days was 46% with many procedures are futile (6).
In this study, we aimed to evaluate the predictors of poor functional outcome at 90-days in patients with successful recanalization within 6 h of symptom onset.
Methods
Patients
We performed a retrospective review of a prospectively maintained MT database at our tertiary comprehensive stroke center from May 2016 to June 2018. Patients were included in the study if they had anterior circulation LVO, presented within 6 h of symptom onset, and underwent MT with successful reperfusion defined as achievement of modified Thrombolysis In Cerebral Infarction (mTICI) of 2b-3. The institutional review board approved the study.
Baseline Assessment
Patient demographics, stroke risk factors, baseline National Institute of Health Stroke Scale (NIHSS) score, time since last known well (LKW), and pre-procedure intravenous tissue plasminogen activator (IV-tPA) administration were reviewed and recorded as well as Alberta Stroke Program Early Computed Tomography Score (ASPECTS) which was assessed by a stroke neurologist across our database.
Endovascular Procedure
The decision to perform MT was based on multidisciplinary discussions between the vascular neurology and neuroendovascular teams. All patients were treated with MT using stent-retrievers or contact aspiration techniques according to the most recent guidelines. Procedural data with regard to the site of occlusion; internal carotid artery (ICA) or middle cerebral artery (MCA), time from groin puncture to successful recanalization, and the numbers of passes were recorded. No proximal balloon guide catheter was used in any of those cases.
Complication and Outcome
Hemorrhagic transformation was assessed by post-treatment head computed tomography (CT). Symptomatic intracranial hemorrhage (sICH) was defined as any ICH on follow-up CT leading to neurologic deterioration, as reflected by NIHSS score worsening of ≥ 4 points. Distal clot migration (DCM) to the same or new territory was identified from post-MT angiography and compared to pre-treatment CT angiography, with corresponding cerebral infarction on cross-sectional imaging. A 90-day mRS 3–6 was considered a poor outcome.
Statistical Analysis
Quantitative variables were described as mean ± standard deviation (SD) after normality testing with the Shapiro-Wilk test. Categorical variables were presented as frequencies and percentages. For the univariate analysis, data were compared using Student's t-tests for continuous variables and chi-square or Fisher's exact tests for categorical variables as appropriate. On multivariable regression analysis, all variables with P < 0.1 in the univariate analyses were included in the regression model to determine the independent predictors of poor outcome. Statistical significance was set at P < 0.05. Statistical evaluations were performed using STATA/SE software, version 10.1 (StataCorp, College Station, TX).
Results
Baseline Characteristics
A total of 56 patients met the criteria for inclusion in this study. Poor outcomes occurred in 31 (55.4%) patients, of whom 17 (54.8%) were females, with a mean age of 68.4 years. There were no significant differences in baseline medical comorbidities between patients with good vs. poor 90-day functional outcomes. LKW to puncture time, ASPECTS, and pre-procedure IV-tPA also did not differ between the two groups. The mean ± SD baseline NIHSS score was significantly higher in patients with poor 90-day outcomes (21.3 ± 5.3 vs. 13.8 ± 5.7, P < 0.001) (Table 1).
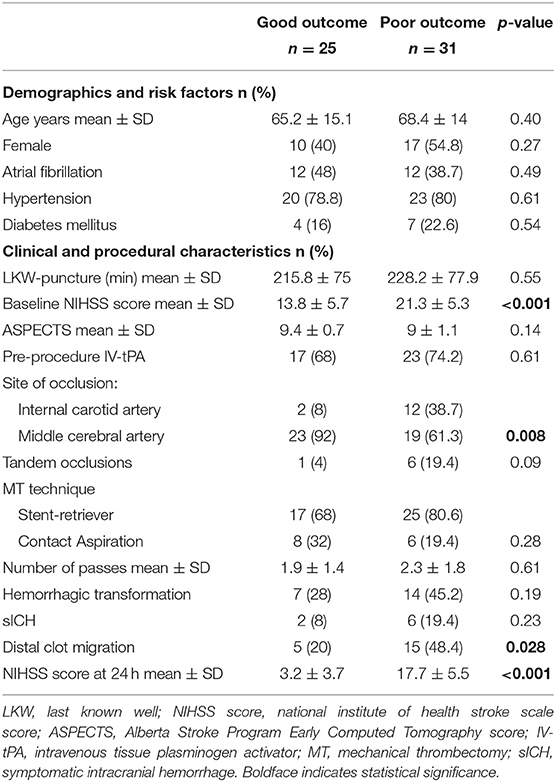
Table 1. Baseline, clinical characteristics, angiographic findings between good (90-day mRS 0–2) and poor outcome (90-day mRS 3–6).
Procedural Findings
Patients with poor outcomes were more likely to have ICA occlusions (38.7 vs. 8%, P = 0.008). There was a trend of higher rates of tandem occlusions in patients with poor outcome (19.4 vs. 4%, P = 0.09). The mean time from puncture to successful reperfusion (mTICI 2b/3) was comparable between the two groups (51.1 ± 36.7 vs. 37.1 ± 23.3, P = 0.16) (Table 1).
Complications and Outcome
There were no significant differences between the two groups in the overall rates of hemorrhagic transformation (45.2 vs. 28%, P = 0.19) or sICH (19.4 vs. 8%, P = 0.23). Patients with poor outcomes had higher rates of DCM (48.4 vs. 20%, P = 0.028) and higher mean NIHSS scores at 24 h post-procedure (17.7 ± 5.5 vs. 3.2 ± 3.7, P < 0.001) (Table 1).
Predictors of Poor Outcome
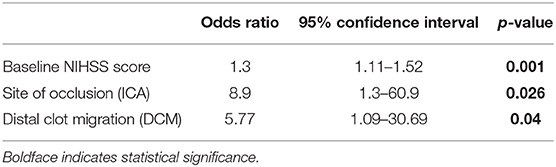
On multivariable regression analysis, baseline NIHSS score [OR; 1.3, 95%CI [1.11–1.52], P = 0.001], site of occlusion (ICA) [OR; 8.9, 95% CI [1.3–60.9], P = 0.026], and DCM [OR; 5.77, 95% CI [1.09–30.69], P = 0.04] were independent predictors of poor outcome (Table 2).
Discussion
Our study demonstrated that baseline NIHSS score, ICA occlusion, and DCM are independent predictors of poor functional outcome despite successful recanalization after MT within 6 h of symptom onset. Our finding of higher NIHSS score and its association with the poor functional outcome is consistent with several previous studies which evaluated the prognostic factors of outcome after MT (7–9). A high NIHSS on admission was also associated with both proximal ICA occlusion and poor collateral circulation (10).
Previous studies have shown that IV-tPA was associated with better recanalization of MCA occlusions as compared to more proximal ICA occlusions, (11) an observation that has held true even in the era of endovascular intervention, which can be explained by the fact that ICA occlusions are more complex than MCA occlusions as they can be either a single artery occlusion or a tandem lesion. Moreover, ICA terminus occlusion often extends into both the M1 segment of MCA and/or A1 segment of the anterior cerebral artery and usually exhibit large clot burdens and impair collateral circulations (12). Tandem occlusions involve both the cervical ICA and either the intracranial ICA (Figure 1), MCA-M1, or ACA-A1. Our results did not report a significant difference in the outcome of MT in patients with tandem occlusion and those without which indicates that ICA occlusion per se is a predictor of poor outcome.
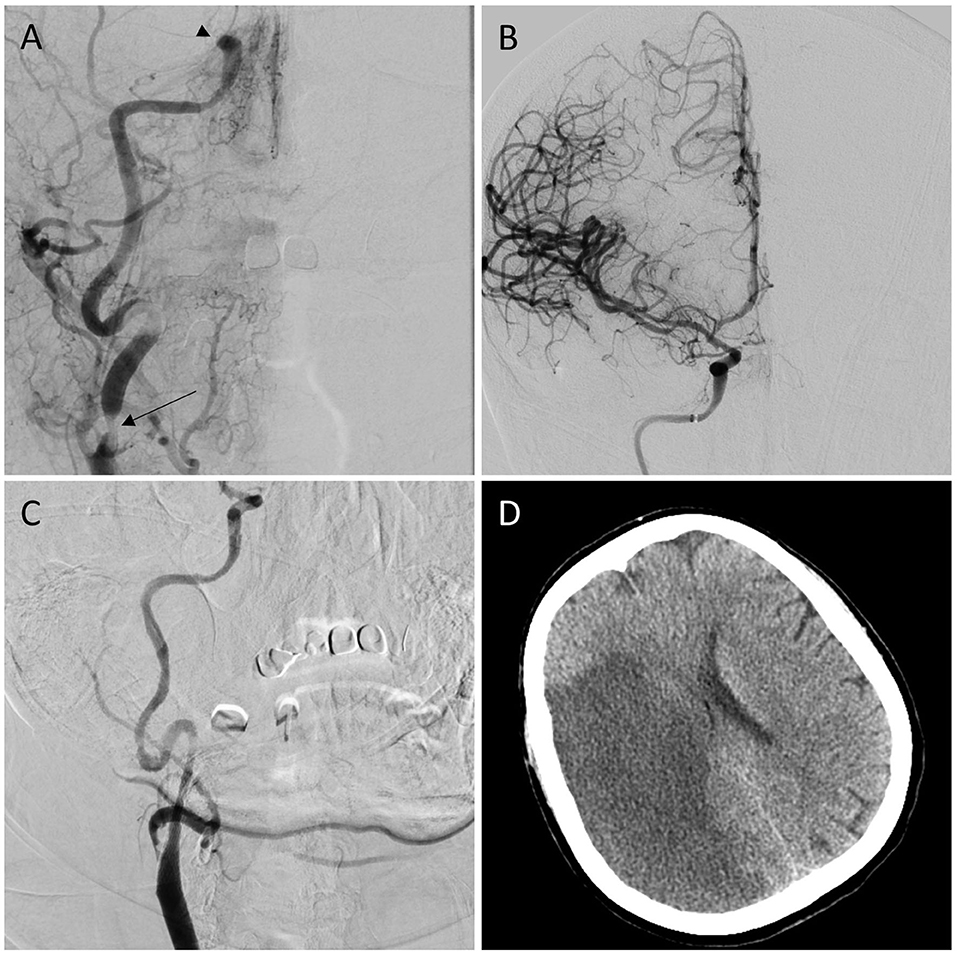
Figure 1. (A) Anterior-posterior (A–P) projection of cerebral angiogram shows the right internal carotid artery terminus occlusion (arrowhead) with stenosis in the cervical portion (arrow). (B) A–P projection of cerebral angiogram after mechanical thrombectomy shows Complete recanalization (mTICI 3). (C) A–P projection after carotid artery stenting shows successful angioplasty and stenting of cervical carotid artery stenosis. (D) Corresponding CT brain shows cerebral infarction at the right middle cerebral artery territory.
In this study, we found that DCM either to the same or to an unaffected territory resulted in a poor functional outcome. We believe this is due to the compromise of collateral vessels that result in loss of salvageable brain tissue (13). Recanalization via stent-retrievers or aspiration thrombectomy did not result in different outcomes nor did time to recanalization or the number of thrombectomy passes (14, 15).
Finally, our study demonstrated that pre-MT IV-tPA administration did not improve outcomes after MT, which is consistent with a recent randomized controlled trial that reported non-inferiority of direct MT without prior IV-tPA to MT preceded by IV-tPA in terms of functional outcome (16).
Our study has all the limitations inherent to any retrospective analysis. Moreover, the small sample size might limit the generalizability of our results. Also, there was no core laboratory adjudication of final reperfusion grades. The strength of our study is the inclusion of only patients who achieved successful reperfusion.
Conclusions
Our study demonstrates that baseline NIHSS score, ICA occlusion, and DCM are independent predictors of poor functional outcome in patients undergoing MT within 6 h of symptom onset. Identifying factors which lead to poor clinical outcome and modification of these factors if possible can result in an improvement of functional independence of patients with AIS treated with MT. Large multicenter prospective studies are warranted.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the institutional review board of the University of Illinois at Chicago Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
MM: study conception, design of the work, data acquisition, interpretation of data, and drafting of the manuscript. CS, DB, AH, EK, and GA: critical revision of the manuscript. AA: interpretation of data and critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
AA: Consultant: Cerenovus.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Stroke−1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke. (1989) 20:1407–31. doi: 10.1161/01.STR.20.10.1407
2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
3. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for Stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. (2018) 378:708–18. doi: 10.1056/NEJMoa1713973
4. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. (2017) 378:11–21. doi: 10.1056/NEJMoa1706442
5. Nogueira RG, Liebeskind DS, Sung G, Duckwiler G, Smith WS, MERCI; Multi MERCI Writing Committee. Predictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the mechanical embolus removal in cerebral ischemia (MERCI) and multi MERCI trials. Stroke. (2009) 40:3777–83. doi: 10.1161/STROKEAHA.109.561431
6. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. (2016) 387:1723–31. doi: 10.1016/S0140-6736(16)00163-X
7. Shi ZS, Liebeskind DS, Xiang B, Ge SG, Feng L, Albers GW, et al. Predictors of functional dependence despite successful revascularization in large-vessel occlusion strokes. Stroke. (2014) 45:1977–84. doi: 10.1161/STROKEAHA.114.005603
8. Jiang S, Fei A, Peng Y, Zhang J, Lu YR, Wang HR, et al. Predictors of outcome and hemorrhage in patients undergoing endovascular therapy with solitaire stent for acute ischemic stroke. PLoS ONE. (2015) 10:e0144452. doi: 10.1371/journal.pone.0144452
9. van Horn N, Kniep H, Leischner H, McDonough R, Deb-Chatterji M, Broocks G, et al. Predictors of poor clinical outcome despite complete reperfusion in acute ischemic stroke patients. J NeuroIntervent Surg. (2020). doi: 10.1136/neurintsurg-2020-015889. [Epub ahead of print].
10. Arsava EM, Vural A, Akpinar E, Gocmen R, Akcalar S, Oguz KK, et al. The detrimental effect of aging on leptomeningeal collaterals in ischemic stroke. J Stroke Cerebrovasc Dis. (2014) 23:421–6. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.014
11. Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. (2002) 33:2066–71. doi: 10.1161/01.STR.0000021001.18101.A5
12. Fischer U, Mono ML, Schroth G, Jung S, Mordasini P, El-Koussy M, et al. Endovascular therapy in 201 patients with acute symptomatic occlusion of the internal carotid artery. Eur J Neurol. (2013) 20:1017–24.e87. doi: 10.1111/ene.12094
13. Jung S, Gilgen M, Slotboom J, El-Koussy M, Zubler C, Kiefer C, et al. Factors that determine penumbral tissue loss in acute ischaemic stroke. Brain. (2013) 136(Pt 12):3554–60. doi: 10.1093/brain/awt246
14. Turk AS, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. (2019) 393:998–1008. doi: 10.1016/S0140-6736(19)30297-1
15. Lapergue B, Labreuche J, Piotin M. Contact aspiration versus stent retriever front-line for recanalisation in acute cerebral infarction: the ASTER trial. J Neuroradiol. (2017) 44:71. doi: 10.1016/j.neurad.2017.01.014
Keywords: acute ischemic stroke, mechanical thrombectomy, internal carotid artery occlusion, distal clot migration, poor functional outcome
Citation: Mohammaden MH, Stapleton CJ, Brunozzi D, Hussein AE, Khedr EM, Atwal G and Alaraj A (2020) Predictors of Poor Outcome Despite Successful Mechanical Thrombectomy of Anterior Circulation Large Vessel Occlusions Within 6 h of Symptom Onset. Front. Neurol. 11:907. doi: 10.3389/fneur.2020.00907
Received: 09 May 2020; Accepted: 14 July 2020;
Published: 04 September 2020.
Edited by:
Osama O. Zaidat, Northeast Ohio Medical University, United StatesReviewed by:
Mohamed Osman, St. Vincent Mercy Medical Center, United StatesSamer Abdul Kareem, St. Vincent Mercy Medical Center, United States
Copyright © 2020 Mohammaden, Stapleton, Brunozzi, Hussein, Khedr, Atwal and Alaraj. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Alaraj, YWxhcmFqQHVpYy5lZHU=
 Mahmoud H. Mohammaden
Mahmoud H. Mohammaden Christopher J. Stapleton3
Christopher J. Stapleton3 Eman M. Khedr
Eman M. Khedr Ali Alaraj
Ali Alaraj