- 1University College London Ear Institute, London, United Kingdom
- 2Psychology and Language Sciences, University College London, London, United Kingdom
- 3APD Support, London, United Kingdom
- 4University College London Hospitals NHS Foundation Trust National Hospital for Neurology and Neurosurgery, Neuro-Otology, London, United Kingdom
- 5National Institute of Health Research (NIHR) University College London Hospitals Biomedical Research Centre, London, United Kingdom
- 6Audiological Medicine Department, Great Ormond Street Hospital, London, United Kingdom
Objective: To explore the views and experiences of individuals with Auditory Processing Disorder (APD) and/or their families in getting support from services and to receive their suggestions for improvement.
Design: Cross-sectional random sample survey with descriptive analysis.
Settings: Online survey.
Participants: One hundred and fifty six individuals with APD and/or their family members from the APD Support UK patient support organization and four associated APD Facebook groups.
Main Outcome Measure: A 16-item questionnaire on negative and positive experiences in getting a referral for diagnosis, funding for the FM system, and overall support for APD.
Results: The key findings that emerged included reports of difficulty in getting a referral for diagnosis (54%), obtaining funding for an FM system (45%), getting support for APD (61%), and poor recognition and awareness of APD (63%) in Education, Health or Work settings. The positive experiences reported were ease in getting a referral for diagnosis (46%), in obtaining an FM system (20%), and with diagnosis leading to help at school or to a better understanding of the condition and the required adjustments. The recommended improvement areas were raising awareness of APD and related management in Education (30%), the Health sector (25%), and the public (18%).
Conclusions: Individuals and families of individuals with APD overwhelmingly report a lack of awareness of APD across health, education, and work sectors, and difficulties in getting access to diagnosis and support. This information may provide an initial understanding of the patients' needs for clinical services for APD, identify research priorities, and influence longer-term public health decisions toward improved care.
Introduction
Auditory Processing Disorder (APD) is the commonly used term for the clinical presentation of listening difficulties in children and adults with normal audiograms but abnormal scores in complex psychoacoustic tests (1). It is classified under H93.25 in the current tenth version of the International Classification of Diseases (ICD-10). The subtypes according to risk factors include developmental APD, in children with a family history of language or developmental disorders and no other known risk factors (2) with symptoms that may persist into adulthood (3). Acquired APD may present after brain injury or stroke (4), or with aging (5, 6). Secondary APD may be present in individuals with a history of hearing impairment (2). Additionally, impaired perception of sound features corresponding to pathology in central auditory structures, that is disproportionate to the hearing levels, and not the direct result of a higher cognitive deficit, is a prominent feature of several genetic subtypes of dementia (7). APD may also be part of the phenotype in different schizophrenia subgroups (8) and may contribute to the psychiatric symptoms (9). Different aspects of non-speech sound processing show significant heritability (10, 11), and genetic work in the future may help to subclassify APD further in terms of the underlying pathophysiology.
The prevalence of APD was calculated to be 1.94 per 1,000 children by a recent retrospective study based on referrals and diagnoses made in a national audiology clinic (12). Hind et al. (13) estimated a prevalence of APD as 0.5–1% in the general population, based on a prevalence of normal audiometric findings. APD was prevalent in 5% of children and 0.9% of adults of all ages who were referred to a general audiology clinic (13). However, these estimates may be affected by ascertainment bias and the prevalence of APD is yet to be determined.
APD has a significant adverse impact on the affected individual's listening and communication, in both children (14) and adults (15). The condition often co-exists with developmental language (16), reading (17), attention disorders (18), in individuals with autism (19) and correlates with autism severity. Children with APD may differ from children with other developmental disorders but show similar performance on cognitive or language tests (20). In the UK education, these children are classified as having special educational needs (SEN). In 2018/19, only 30.4% of SEN children identified by year 11 achieved Level 2 by age 19, compared to 75.3% of non-SEN children (21). Children with APD and their parents report greater emotional difficulties, poor health, emotional and social skills than do normal-hearing children. The presence of a language disorder does not predict their psychosocial difficulties (22). Some children with APD have reported relying more on anger regulation and less on problem-solving as a coping strategy, but in the reported study, the sample size was small (N = 20) (23). Adults with APD similarly focus on restraining their emotions rather than on self-directed thinking (23, 24). APD in childhood may also affect the “sense of self” into early adulthood (3).
APD is diagnosed based on symptoms, poor performance on auditory processing tests, and consideration of other factors that may impact performance (25, 26). There are no uniform diagnostic criteria, with a varied diagnostic yield of criteria applied in previous studies (27). However, more recent consensuses and guidelines by several professional associations and societies appear to be better aligned (15, 28–32).
Management of APD may include listening exercises (i.e., auditory training) for children as well as adults (33, 34), metacognitive strategies (35), and remote microphone hearing aids (RMHAs). RMHAs may improve speech understanding by 53% (36). There is “moderate support” that RMHA systems use in the classroom improve children's speech perception and listening skills in that setting, with mixed evidence that they improve academic performance (37). There are similar reports of improved speech in noise perception with RMHAs in adults with neurological type APD (4, 38, 39).
Awareness about APD remains low. More than half of surveyed UK Audiologists report that they are poorly informed about APD (40), while 18% of South African Audiologists report receiving limited undergraduate training for APD, and 19% report difficulty accessing additional post-graduate training (41). Over 70% of ENT and 90% of GP UK professionals report limited awareness of APD and approximately half are unlikely to refer for further APD assessment (42). The majority of mainstream primary teachers similarly report “very poor” awareness regarding APD (43).
There are fewer than 10 dedicated APD clinics for children and only two for adults within the UK NHS. On the positive side, the UK Department for Education recommended standards for the acoustic design of schools classifies children with APD as having special hearing/communication needs. However, at present only half of the UK classrooms fully comply with these standards (44, 45). Anecdotal reports by parents of children with APD suggest that educational support provided to their children and teenagers is limited. Adult subjects with APD visiting the clinics similarly reported limited support in their workplace. To our knowledge, APD Support UK is currently the only UK organization providing support for those affected.
In this context, it is crucial to understand the challenges faced by patients and their families in accessing the diagnosis and management of APD and support after the diagnosis, to inform planning for education, research, and clinical services toward improved care in the long-term. The present study aimed to explore the views and experiences of individuals with Auditory Processing Disorder (APD) and/or their families about getting support from services and to receive their suggestions for improvement.
Methods
The Survey
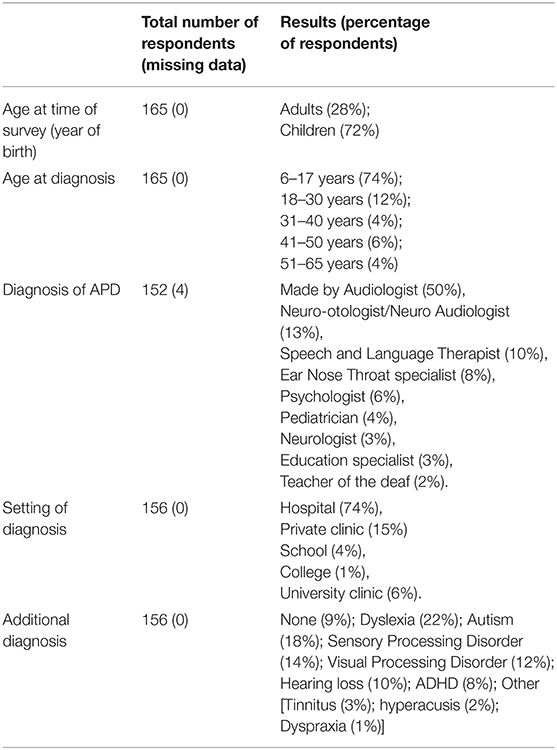
Following a pilot study (see Appendix 1), a questionnaire with 16 questions (10 open-ended and 6 closed) about patient experience with APD was developed by the last author. The purpose of the questionnaire was to collect information about APD diagnosis, access to services, support, positive and negative experiences and suggestions for improvements. The questions were then reviewed by all authors, who are experts in the field of hearing impairments and patient-reported measures and pilot-tested by a parent of a child with APD for usability, relevance and ease of completion. Minor revisions were made (see Appendix 2; Table 1). The final version of the questionnaire was administered online using the web-based survey tool Opinio (Opinio 7.10, Copyright 1998–2019 ObjectPlanet). The survey was open from May to July 2019.
Participants
Ethics approval was obtained by the UCL Research Ethics Committee (project ID 14813/001). Before completing the questions, participants provided informed consent. The online survey was circulated to a convenience sample through the APD Support UK Facebook groups (~2,300 members), for parents, teenagers, young adults, and adults. It was also posted on the APD Support UK website: https://apdsupportuk.yolasite.com/. Participation in the survey was anonymous and voluntary. Patients and/or relatives of patients with APD were invited to participate by following a web link to the survey.
Analysis
Responses to questions 1–6 (demographic data) were analyzed using descriptive statistics and reported as n (%). Open-ended responses (questions 7–16) were analyzed qualitatively. Three a priori domains were used as per the questions of the survey: Difficulties, Positive Experiences, and Recommendations. Analysis then focused on identifying subdomains within each of these domains following the content of the questions with analysis methods and steps introduced by Braun and Clarke (46, 47). Domains and subdomains were initially generated by author DA, scrutinized with GD and finally reviewed by all authors and finalized after consensus. Analyses were completed using Microsoft Excel for Office 365 and NVivo Pro v12.
Results
Demographics (Questions 1–6)
One hundred and fifty six participants completed the survey. Of these, 20% had been diagnosed with APD themselves, whereas 78% completed the survey on behalf of their son or daughter. Two participants responded for their partners and one for their grandchild. As some participants reported that there was more than one person with APD in the family, the responses represented 165 APD patients in total (mean age: 18 years old, standard deviation: 12.9, age range: 6–65 years). The demographic information is provided in Table 2.
Qualitative Data Analysis
The results of the descriptive analysis of the responses to questions 7–16 can be seen in Figure 1. As explained above, subdomains were identified within the 3 a priori domains. In the “Difficulties” domain, the subdomains corresponded to the survey questions (7–11), while for the other 2 domains (Positive Experiences and Recommendations/priorities) subdomains focused on questions 12 and questions 13–15, respectively. The responses are reported as percentages when relevant and informative. Domains and subdomains are presented below alongside illustrative quotes. Responses to specific domains and subdomains have been quoted in Tables 3, 4.
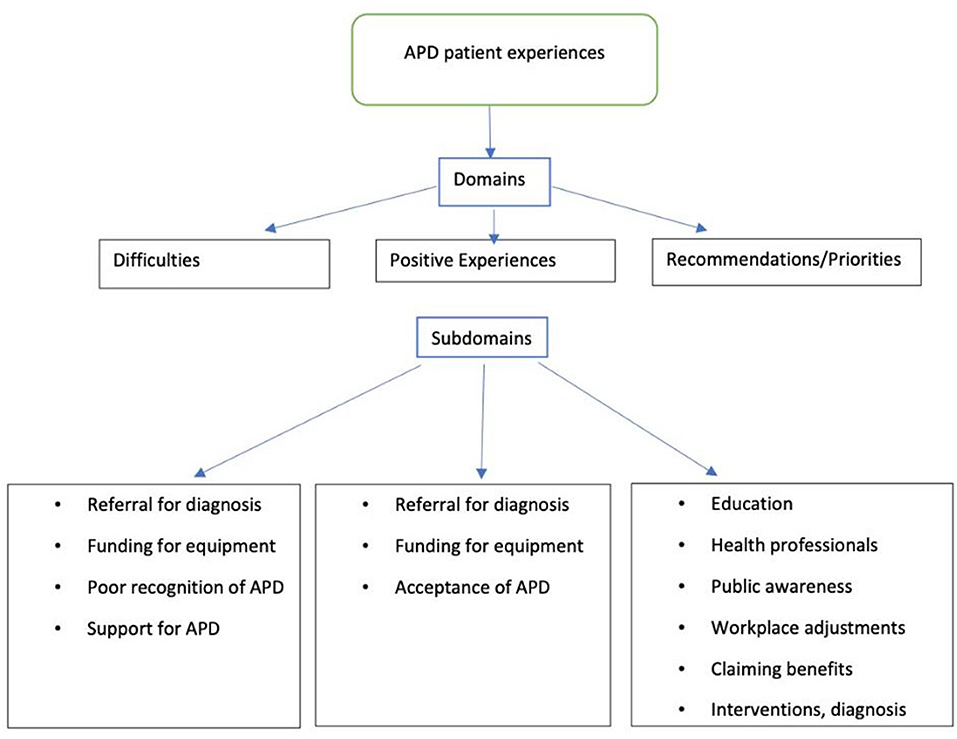
Figure 1. Subdomains identified within each of the 3 a priori domains, illustrating the experiences of people diagnosed with APD, and their families who participated in the present study.
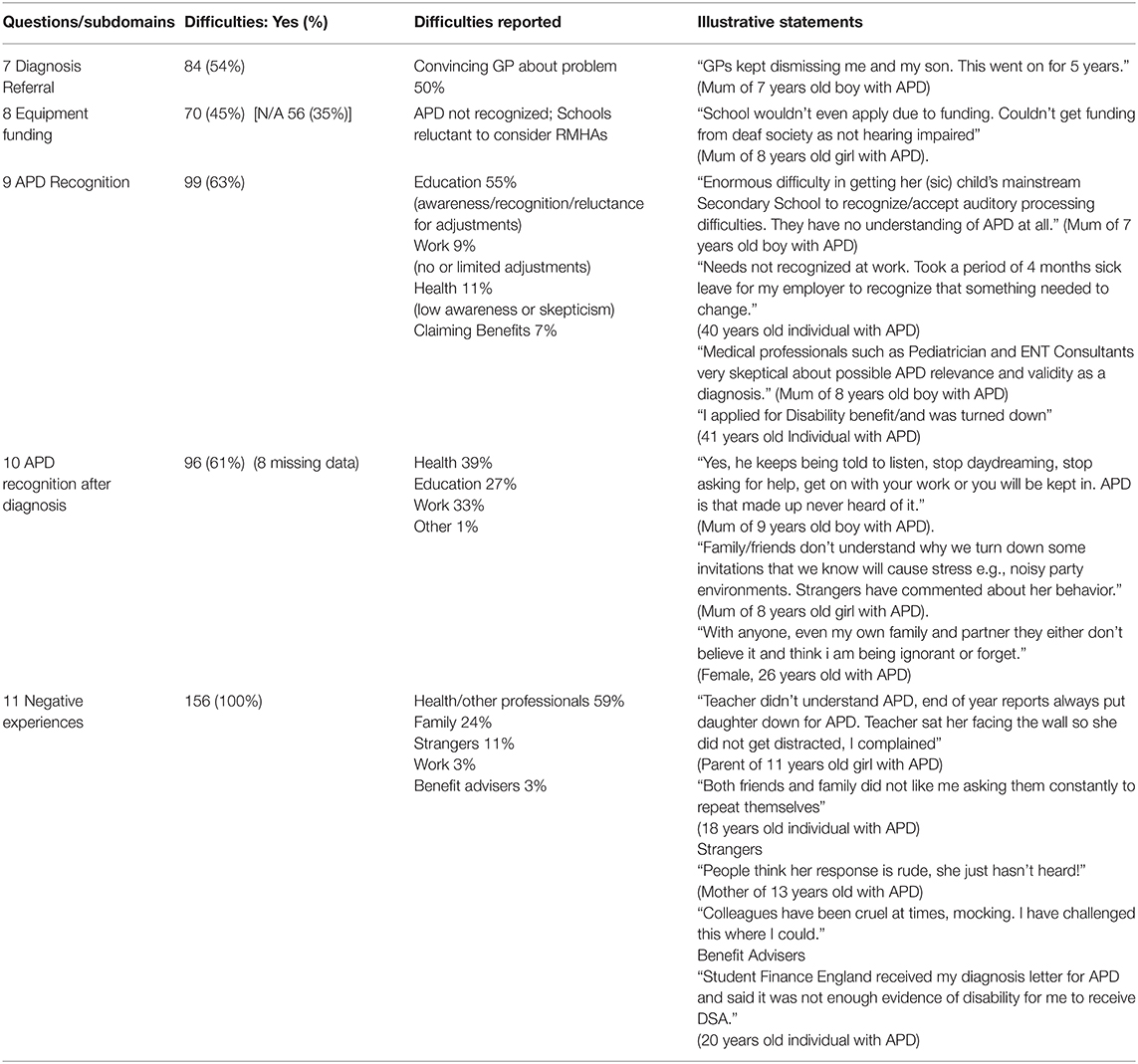
Table 3. Responses to the Domain: Difficulties faced, with the percentage of responses for each subdomain, and illustrative statements given by the respondents.
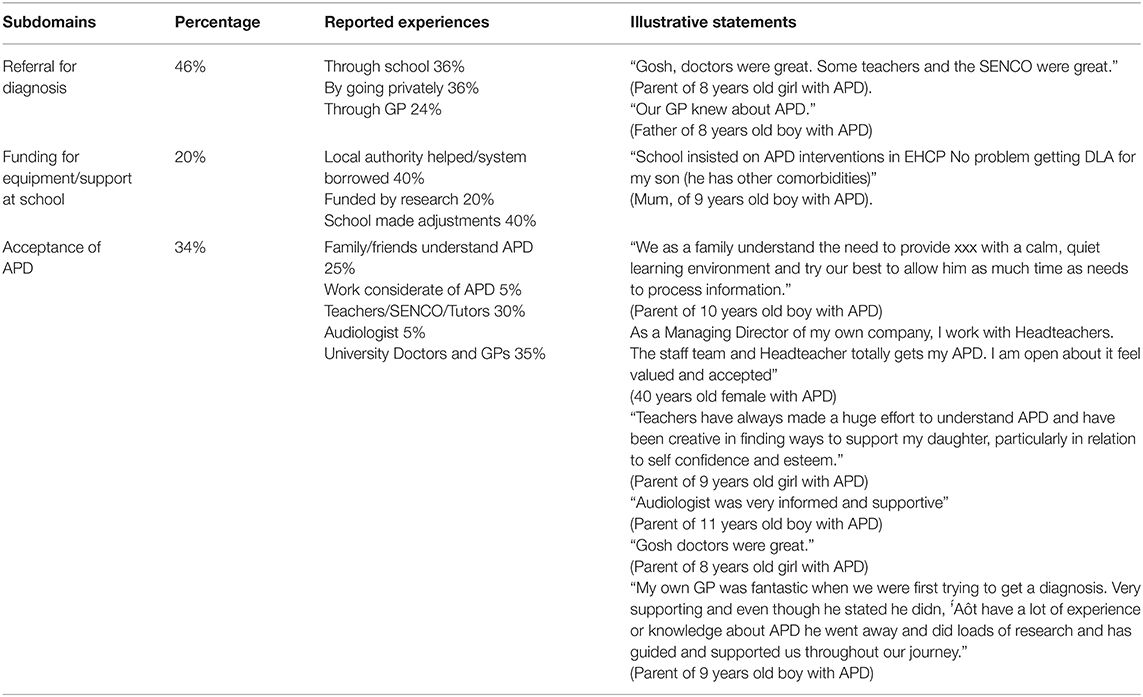
Table 4. Responses to the Domain: positive experiences, with percentage for each subdomain and illustrative statements given by the respondents.
Domain: Difficulties (Questions 7–11)
Respondents reported difficulties in getting a referral (54%), in getting funding for the recommended equipment (24%), whereas (63%) reported difficulties in getting APD recognized and accepted, and difficulties getting support for APD. All respondents reported negative experiences in interacting with others (Table 3).
Domain: Positive Experiences (Question 12)
Positive experiences were identified by 150 respondents in terms of subdomains of referral for diagnosis (46%), funding for equipment/support at school (24%), and acceptance of APD (36%) (Table 4).
Domain: Recommendations for Improvement (Questions 13–15)
Questions 13–15 (156 respondents) had overlapping responses and were divided into different subdomains as presented below.
Subdomain: Educating/Training
Thirty percentage of respondents suggested prioritizing the education of teachers regarding APD including coping strategies for APD, use of the equipment, and development of screening tests for school-aged children.
“More understanding by teaching professionals at a local level> NHS SALT looking at the big picture rather than just identifying speech sound difficulties”
(Grandmother of a 6 years old boy with APD)“Make it as important as children with dyslexia and autism”
(Parent of 9 years old child with APD)
Subdomain: Training Health Professionals
Twenty five percentage of recommended training for medical professionals regarding APD and the importance of RMHAs.
“Hearing aids, FM systems should be funded in schools”
(Parent of 11 years old girl with APD)
Subdomain: Public Awareness
Eighteen percentage of suggested raising public awareness.
“More public awareness! More cross-agency working”
(Mum of 11 years old boy with APD)
Subdomain: Workplace Adjustments
Six percent suggested educating employers.
“Rather than good practice, it needs to be an essential practice that any employer is made aware of that person's disability and that reasonable accommodations are made to put them on an equal footing with their colleagues”
(40 years old individual with APD)
Subdomain: Claiming Benefits
Seven percent recommended focusing on claiming benefits.
“CLAIMING BENEFITS 1. Qualified DWP government assessors to assess, NOT for-profit private enterprise assessors 2. Advocates for people with APD 3. Working knowledge of APD so that assessors don't make assumptions about what people with APD can and cannot hear etc. 4. Filming of assessments so that unscrupulous assessors cannot take advantage of people with APD.”(Parent of 13 years old boy with APD)
Subdomain: Research Into Interventions, Diagnosis, and Comorbidities
Out of 136 respondents, 59% recommended research focused on management, 31% on APD diagnosis, and 29% on symptoms and comorbidities.
“Effectiveness of Interventions—clinical evidence—research into auditory training programmes, computer-based learning programmes such as Earobics (recommended but not commercially available) or Fastforword, etc.”
(Parent of a 7 years old child with APD).
“Early diagnostic processes in schools. More trained audiologists to diagnose locally. Research as to better diagnosis and coping strategies”
(Parent of 12 years old with APD)
“Research on other combined issues that go hand in hand with APD”
(Parent of 7 years old with APD)
Thus, respondents reported, difficulty in getting a referral for diagnosis (54%), obtaining funding for an FM system (45%), getting support for APD (61%). The positive experiences reported were ease in getting a referral for diagnosis (46%), in obtaining an FM system (20%). The recommended improvement areas were raising awareness of APD and related management in Education (30%), the Health sector (25%), and the public (18%).
Discussion
Poor awareness and understanding of APD were reported by the majority of respondents of the present survey, particularly in professionals in relevant positions, in line with previous reports by surveyed professionals (41–43). This lack of knowledge among medical professionals is of concern, as it may lead to delayed diagnosis and management of APD in affected individuals, and failure to meet the guidelines of the National Service Framework (NSF) for “early recognition, prompt diagnosis, and treatment” (48). Children faced difficulties at school due to poor awareness/recognition of APD, despite the classification of APD as requiring SEN support by the Department for Education (44). Similarly, participants reported poor recognition and no support for APD at work. Reasonable adjustments both in education and in the workplace are a legal requirement.
The majority of respondents had negative experiences in getting RMHAs, with funding and other obstacles, despite the NSF requirement for people with long term conditions to receive “timely, appropriate assistive technology/equipment,” (48). RMHAs improve listening and attention skills in children (8), and adults with neurological-type APD (4, 38, 39), and are thus a reasonable adjustment as per the Equality Act 2010 (49). Our results highlight the need for teachers, in particular, to be better informed about APD (41, 43) not least because they may be the first to notice gaps in a child's language, social behavior, and communication skills (25).
The positive experiences reported by the participants were mixed, with some reporting that they did not have difficulty getting a diagnosis and with the diagnosis leading to help or a better understanding of their condition. The three key prioritized improvement areas were raising awareness of APD in Education and Health, reflecting concerns by Audiologists that they have access to limited training on APD (41). The identified research priorities were focused on intervention, diagnosis, and comorbidities of APD. These are in line with studies showing that APD overlaps with developmental disorders (20), reports that few audiologists treat APD (50), and that there are just a handful of studies on intervention benefits (51).
Results of the present patient survey indicate that there is little that has changed for patients and families with APD in the past 10 years. There is a need for continued discussion toward a definition of APD [e.g., (14)] that will be universally accepted. On the positive side, a definition of APD was discussed during the forthcoming ICD 11 beta version development, with the APD entry (under AB5Y Other specified disorders with hearing impairment) accepted by the International Federation of ORL Societies (52). There is a need for training not only for Audiologists, whose curricula already include APD, but also for teachers and general practitioners. Encouragingly, some information on APD is included on the NHS site (53), but further formal training is required. Guidelines and pathways for the provision of remote microphone hearing aids need to be agreed upon by the Health and Education sectors and established.
The study has some inherent limitations, notably that the authors had no quality control on the diagnosis of the individuals taking part in the survey. The convenience sample from four Facebook groups may not be representative of the broad UK population. There was no follow up with a face-to-face interview to investigate the domains and subdomains identified in more detail or depth. We did not look at socioeconomic factors or audiological data, to maintain patient anonymity. The potential bias in participant responses, which is an inherent limitation of qualitative research as a whole, also has to be mentioned. Nevertheless, this is the first UK survey of subjects with APD and their families and is consistent with previous surveys of professionals in Health and Education. These subjective reports have real-life validity and could contribute to planning for NHS services by giving people choice, through services planned and delivered around their individual needs, inform clinical decision making and guide future research.
Conclusions
In conclusion, individuals with APD and their families overwhelmingly reported difficulties in getting access to diagnosis and support. They request increased awareness of APD across health, education, and work sectors. Despite the study's limitations, this information may provide some initial understanding of the needs of the individuals with APD and their families. There is a pressing need to improve awareness and recognition of APD and address what patients perceive as research priorities.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by UCL Research Ethics Committee (project ID 14813/001). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DA performed the data analysis, literature review, interpretation of results, drafted the first version of the manuscript, and is responsible for submitting the manuscript. GD contributed toward developing the questionnaire, study design, data collection, data analysis, and editing the manuscript. AM is a patient collaborator who contributed equally with the other authors in research design, contact, analysis, and interpretation/write up. MM contributed to the editing of the manuscript. DB is responsible for designing the study, study coordination, data analysis and interpretation, and the editing and final version of the manuscript. All authors have contributed equally and approved the final manuscript.
Funding
Great Ormond Street Hospital in part supported the DA contribution to the study.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank all the participants for their active participation and response. We extend our gratitude to Great Ormond Street Hospital Charity for funding DA time for this research.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.607907/full#supplementary-material
References
1. American Academy of Audiology. Diagnosis, Treatment, and Management of Children and Adults with Central Auditory Processing Disorder (2010). Available online at: https://audiology-web.s3.amazonaws.com/migrated/CAPD%20Guidelines%208-2010.pdf_539952af956c79.73897613.pdf (accessed February 7, 2021).
2. BSA. Position Statement and Practice Guidance: Auditory Processing Disorder. (2017) Available online at: http://www.thebsa.org.uk/wp-content/uploads/2017/04/APD-Position-Statement-Practice-Guidance-APD-2017.pdf (accessed February 22, 2020).
3. Del Zoppo C, Sanchez L, Lind C. A long-term follow-up of children and adolescents referred for assessment of auditory processing disorder. Int J Audiol. (2015) 54:368–75. doi: 10.3109/14992027.2014.972523
4. Koohi N, Vickers D, Lakshmanan R, Hoskote C, Werring D, Warren J, et al. Hearing characteristics of stroke patients: prevalence and characteristics of hearing impairment and auditory processing disorders in stroke patients. J Am Acad Audiol. (2017) 28:491–505. doi: 10.3766/jaaa.15139
5. Gates GA. Central presbycusis: an emerging view. Otolaryngol. Head Neck Surg. (2012) 147:1–2. doi: 10.1177/0194599812446282
6. Quaranta N, Coppola F, Casulli M, Barulli MR, Panza F, Tortelli R, et al. The prevalence of peripheral and central hearing impairment and its relation to cognition in older adults. Audiol Neurootol. (2014) 19:10–4. doi: 10.1159/000371597
7. Hardy C, Marshall C, Golden H, Clark C, Mummery C, Griffiths T, et al. Hearing, and dementia. J Neurol. (2016) 263:2339–54. doi: 10.1007/s00415-016-8208-y
8. Moschopoulos N, Nimatoudis I, Kaprinis S, Iliadou V. Assessment of auditory processing deficits in schizophrenia: Literature review and suggestions for future research. Scand J Psychol. (2019) 60:116–27. doi: 10.1111/sjop.12514
9. Kraus M, Walker T, Jarskog L, Millet R, Keefe R. Basic auditory processing deficits and their association with auditory emotion recognition in schizophrenia. Schizophr Res. (2019) 204:155–61. doi: 10.1016/j.schres.2018.08.031
10. Brewer C, Zalewski C, King K, Zobay O, Riley A, Ferguson M, et al. Heritability of non-speech auditory processing skills. Eur J Hum Genet. (2016) 24:1137–44. doi: 10.1038/ejhg.2015.277
11. ASHA. (Central) Auditory Processing Disorders (Technical Report). (2015). Available online at: www.asha.org/policy (accessed February 20, 2020).
12. Nagao K, Riegner T, Padilla J, Greenwood LA, Loson J, Zavala S, et al. Prevalence of auditory processing disorder in school-aged children in the Mid-Atlantic Region. J Am Acad Audiol. (2016) 27:691–700. doi: 10.3766/jaaa.15020
13. Hind SE, Haines-Bazrafshan R, Benton C, Brassington W, Towel B, Moore DR. Prevalence of clinical referrals having hearing thresholds within normal limits. Int J Audiol. (2011) 50:708–16. doi: 10.3109/14992027.2011.582049
14. Iliadou V, Ptok M, Grech H, Pedersen E, Brechmann A, Deggouj N, et al. European 17 countries consensus endorses more approaches to APD than reported in Wilson. Int J Audiol. (2018) 57:395–6. doi: 10.1080/14992027.2018.1442937
15. Bamiou D, Iliadou V, Zanchetta S, Spyridakou C. What can we learn about auditory processing from adult hearing questionnaires? J Am Acad of Audiol. (2015) 26:824–37. doi: 10.3766/jaaa.15009
16. Sharma M, Purdy SC, Kelly AS. Comorbidity of auditory processing, language, and reading disorders. J Speech Lang Hear Res. (2009) 52:706–22. doi: 10.1044/1092-4388(2008/07-0226)
17. Dawes P, Bishop DV. The SCAN-C in testing for auditory processing disorder in a sample of British children. Int J Audiol. (2007) 46:780–6. doi: 10.1080/14992020701545906
18. Riccio CA, Hynd GW, Cohen MJ, Hall J, Molt L. Comorbidity of central auditory disorder and attention-deficit and hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. (1994) 33:849–957. doi: 10.1097/00004583-199407000-00011
19. Brandwein AB, Foxe JJ, Butler JS, Frey HP, Bates JC, Shulman L, et al. Neurophysiological indices of atypical auditory processing multisensory integration are associated with symptom severity in autism. J Autism Dev Disord. (2015) 45:230–44. doi: 10.1007/s10803-014-2212-9
20. de Wit E, Van Dijk P, Hanekamp S, Visser-Bochane MI, Steenbergen B, van der Schans CP, et al. Same or different: the overlap between children with auditory processing disorders and children with other developmental disorders: a systematic review. Ear Hear. (2018) 39:1–19. doi: 10.1097/AUD.0000000000000479
21. Department of Education. Special Educational Needs and Disability: An Analysis and Summary of Data Sources. (2020). Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/882802/Special_educational_needs_and_disability_-_an_analysis_and_summary_of_data_sources.pdf (accessed June 24, 2020).
22. Kreisman NV, John AB, Kreisman BM, Hall JW, Crandell CC. Psychosocial status of children with auditory processing disorder. J Am Acad Audiol. (2012) 23:222–33. doi: 10.3766/jaaa.23.3.8
23. Eschenbeck H, Gillé V, Heim-Dreger U, Schock A, Schott A. Daily stress, hearing-specific stress and coping: self-reports from deaf or hard of hearing children and children with auditory processing disorder. J Deaf Stud Deaf Educ. (2017) 22:49–58. doi: 10.1093/deafed/enw053
24. Obuchi C, Ogane S, Sato Y, Kaga K. Auditory symptoms and psychological characteristics in adults with auditory processing disorders. J Otol. (2017) 12:132–7. doi: 10.1016/j.joto.2017.05.001
25. Iliadou V, Bamiou DE. Psychometric evaluation of children with auditory processing disorder (APD): comparison with normal-hearing and clinical non-APD groups. J Speech Lang Hear Res. (2012) 55:791–9. doi: 10.1044/1092-4388(2011/11-0035)
26. Chermak GD, Bamiou DE, Iliadou VV, Musiek F. Practical guidelines to minimise language and cognitive confounds in the diagnosis of CAPD: a brief tutorial. Int J Audiol. (2017) 56:499–506. doi: 10.1080/14992027.2017.1284351
27. Wilson WJ, Arnott W. Using different criteria to diagnose (central) auditory processing disorder: how big a difference does it make? J Speech Lang Hear Res. (2013) 2013:56:63–70. doi: 10.1044/1092-4388(2012/11-0352)
28. International Bureau for Audiophonologie. (2007). Available online at: https://www.biap.org/en/recommandations/recommendations/tc-30-central-auditory-processes-cap (accessed June 24, 2020).
29. Canadian Interorganizational Steering Group for Speech-Language Pathology and Audiology. Canadian Guidelines on Auditory Processing Disorder in Children and Adults: Assessment & Intervention. (2012). Available online at: https://www.ooaq.qc.ca/media/qf4ar4jk/canadian_guidelines_en.pdf (accessed February 7, 2021).
30. Esplin J, Wright C. Auditory Processing Disorder: New Zealand Review. A Report Prepared for the Ministry of Health and Ministry of Education. (2014). Available online at: https://www.health.govt.nz/system/files/documents/publications/auditory processing_disorder.pdf (accessed June 24, 2020).
31. Danish Medical Audiological Society. Udredning og behandling af Auditory Processing Disorder. (2014). Available online at: http://dsohh.dk/wp-content/uploads/2015/04/DSOHH-KKR-APD1.pdf (accessed February 7, 2021).
32. Deutsche Gesellschaft für Phoniatrie und Pädaudiologie (DGPP). Leitlinie Auditive Verarbeitungs-und-Wahrnehmungs störungen. (2019). Available online at: https://www.awmf.org/uploads/tx_szleitlinien/049-012l_S1_Auditive-Verarbeitungs-Wahrnehmungsstoerungen-AVWS_2020-01.pdf (accessed February 7, 2021).
33. Cameron S, Glyde H, Dillon H. Efficacy of the LiSN & Learn auditory training software: randomized blinded controlled study. Audiol Res. (2012) 2:15. doi: 10.4081/audiores.2012.e15
34. Song J, Skoe E, Banai K, Kraus N. Training to improve hearing speech in noise: biological mechanisms. Cereb Cortex. (2012) 22:1180–90. doi: 10.1093/cercor/bhr196
35. Bamiou DE, Campbell N, Sirimanna T. Management of auditory processing disorders. Audiol Med. (2006) 4:46–56. doi: 10.1080/16513860600630498
36. Johnston KN, John AB, Kreisman NV, Hall JW III, Crandell CC. Multiple benefits of personal FM system use by children with auditory processing disorder (APD). Int J Audiol. (2009) 48:371–83. doi: 10.1080/14992020802687516
37. Reynolds S, Miller Kuhaneck H, Pfeiffer B. Systematic review of the effectiveness of frequency modulation devices in improving academic outcomes in children with auditory processing difficulties. Am J Occup Ther. (2016) 70:1–11. doi: 10.5014/ajot.2016.016832
38. Lewis MS, Hutter M, Lilly DJ, Bourdette D, Saunders J, Fausti SA. Frequency-modulation (fm) technology as a method for improving speech perception in noise for individuals with multiple sclerosis. J Am Acad Audiol. (2006) 17:605–16. doi: 10.3766/jaaa.17.8.7
39. Saunders GH, Frederick MT, Arnold ML, Silverman SC, Chisolm TH, Myers PJ. A randomized controlled trial to evaluate approaches to auditory rehabilitation for blast-exposed veterans with normal or near-normal hearing who report hearing problems in difficult listening situations. J Am Acad Audiol. (2018 29:44–62. doi: 10.3766/jaaa.16143
40. Hind S. Survey of care pathway for auditory processing disorder. Audiol Med. (2006) 4:12–24. doi: 10.1080/16513860500534543
41. Fouché-Copley C, Govender S, Khan N. The practices, challenges and recommendations of South African audiologists regarding managing children with auditory processing disorders. S Afr J Commun Disord. (2016) 63:132. doi: 10.4102/sajcd.v63i1.132
42. Baldry NA, Hind SE. Auditory processing disorder in children: awareness and attitudes of UK GPs and ENT consultants. Audiol Med. (2008) 6:193–207. doi: 10.1080/16513860802116668
43. Ryan A, Logue-Kennedy M. Exploration of teachers' awareness and knowledge of (Central) auditory processing disorder ((C) APD). Br J Spec Educ. (2013) 40:167–74. doi: 10.1111/1467-8578.12041
44. Department for Education, Education Funding Agency. Acoustic Design of Schools: Performance Standards. Building bulletin 93 (2015). Available online at: https://www.gov.uk/government/publications/bb93-acoustic-design-of-schools-performance-standards (accessed February 21, 2020).
45. Shield B, Conetta R, Dockrell J, Connolly D, Cox T, Mydlarz C. A survey of acoustic conditions and noise levels in secondary school classrooms in England. J Acoust Soc Am. (2015) 137:177–88. doi: 10.1121/1.4904528
46. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
47. Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. (2019) 11:589–97. doi: 10.1080/2159676X.2019.1628806
48. Department of Health. National Service Framework for Long Term Conditions. (2005). Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198114/National_Service_Framework_for_Long_Term_Conditions.pdf (accessed February 19, 2020).
49. UK Legislation. Equality Act 2010. (2010). Available online at: http://www.legislation.gov.uk/ukpga/2010/15/contents (accessed February 19, 2020).
50. Emanuel DC, Ficca KN, Korczak P. Survey of the diagnosis and management of auditory processing disorder. Am J Audiol. (2011) 20:48–60. doi: 10.1044/1059-0889(2011/10-0019)
51. Loo JH, Bamiou DE, Campbell N, Luxon LM. Computer-based auditory training (CBAT): benefits for children with language- and reading-related learning difficulties. Dev Med Child Neurol. (2010) 52:708–17. doi: 10.1111/j.1469-8749.2010.03654.x
52. ICD, Beta Version 2020 Available online at: https://www.who.int/classifications/icd/revision/icd11knownissues.pdf?ua=1 (accessed December 14, 2020).
53. NHS UK. Auditory Processing Disorder. (2020). Available online at: https://www.nhs.uk/conditions/auditory-processing-disorder (accessed December 14, 2020).
Keywords: auditory processing disorder, patient survey, qualitative, patient experience, questionnaire
Citation: Agrawal D, Dritsakis G, Mahon M, Mountjoy A and Bamiou DE (2021) Experiences of Patients With Auditory Processing Disorder in Getting Support in Health, Education, and Work Settings: Findings From an Online Survey. Front. Neurol. 12:607907. doi: 10.3389/fneur.2021.607907
Received: 18 September 2020; Accepted: 26 January 2021;
Published: 18 February 2021.
Edited by:
Konstantina M. Stankovic, Massachusetts Eye & Ear Infirmary and Harvard Medical School, United StatesReviewed by:
Denise Utsch Gonçalves, Federal University of Minas Gerais, BrazilTakeshi Tsutsumi, Tokyo Medical and Dental University, Japan
Copyright © 2021 Agrawal, Dritsakis, Mahon, Mountjoy and Bamiou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Doris E. Bamiou, ZC5iYW1pb3VAdWNsLmFjLnVr
 Deepashri Agrawal
Deepashri Agrawal Giorgos Dritsakis
Giorgos Dritsakis Merle Mahon2
Merle Mahon2 Alyson Mountjoy
Alyson Mountjoy Doris E. Bamiou
Doris E. Bamiou