- 1China International Neuroscience Institute, Beijing, China
- 2Department of Neurosurgery, Xuanwu Hospital, Capital Medical University, Beijing, China
- 3Neuroradiology & Neurointervention Service, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, United States
- 4Pontifical Bolivarian University, Medellín, Colombia
- 5Department of Evidence-Based Medicine, Xuanwu Hospital, Capital Medical University, Beijing, China
- 6Medical Library, Xuanwu Hospital, Capital Medical University, Beijing, China
- 7Department of Neurology, Xuanwu Hospital, Capital Medical University, Beijing, China
- 8Department of Interventional Neuroradiology, Xuanwu Hospital, Capital Medical University, Beijing, China
Background: First-pass effect (FPE) is increasingly recognized as a predictor of good outcome in large vessel occlusion (LVO). This systematic review and meta-analysis aimed to elucidate the factors influencing recanalization after mechanical thrombectomy (MT) with FPE in treating acute ischemic stroke (AIS).
Methods: Main databases were searched for relevant randomized controlled trials (RCTs) and observational studies reporting influencing factors of MT with FPE in AIS. Recanalization was assessed by the modified thrombolysis in cerebral ischemia (mTICI) score. Both successful (mTICI 2b-3) and complete recanalization (mTICI 2c-3) were observed. Risk of bias was assessed through different scales according to study design. The I2 statistic was used to evaluate the heterogeneity, while subgroup analysis, meta-regression, and sensitivity analysis were performed to investigate the source of heterogeneity. Visual measurement of funnel plots was used to evaluate publication bias.
Results: A total of 17 studies and 6,186 patients were included. Among them, 2,068 patients achieved recanalization with FPE. The results of meta-analyses showed that age [mean deviation (MD):1.21,95% confidence interval (CI): 0.26–2.16; p = 0.012], female gender [odds ratio (OR):1.12,95% CI: 1.00–1.26; p = 0.046], diabetes mellitus (DM) (OR:1.17,95% CI: 1.01–1.35; p = 0.032), occlusion of internal carotid artery (ICA) (OR:0.71,95% CI: 0.52–0.97; p = 0.033), occlusion of M2 segment of middle cerebral artery (OR:1.36,95% CI: 1.05–1.77; p = 0.019), duration of intervention (MD: −27.85, 95% CI: −42.11–13.58; p < 0.001), time of onset to recanalization (MD: −34.63, 95% CI: −58.45–10.81; p = 0.004), general anesthesia (OR: 0.63,95% CI: 0.52–0.77; p < 0.001), and use of balloon guide catheter (BGC) (OR:1.60,95% CI: 1.17–2.18; p = 0.003) were significantly associated with successful recanalization with FPE. At the same time, age, female gender, duration of intervention, general anesthesia, use of BGC, and occlusion of ICA were associated with complete reperfusion with FPE, but M2 occlusion and DM were not.
Conclusion: Age, gender, occlusion site, anesthesia type, and use of BGC were influencing factors for both successful and complete recanalization after first-pass thrombectomy. Further studies with more comprehensive observations indexes are need in the future.
Introduction
Stroke is the second-leading cause of global morbidity and mortality (1, 2). Mechanical thrombectomy (MT) has been widely used to treat acute ischemic stroke (AIS) patients and has proved superior over intravenous tissue-type plasminogen activator (tPA) by several landmark randomized trials (RCTs) (3–6). Thus, the American Heart and American Stroke Association recommends MT as the first-line therapy for selected AIS patients with proximal artery large vessel occlusions (LVO) (2).
However, some trials showed that functional independence in AIS patients is only around 50% even with a high recanalization rate of over 70% (3, 6). Thrombectomy with first pass effect (FPE), an emerging new metric, is strongly correlated with improved functional outcomes (7–10). Thrombectomy with FPE may have many advantages such as less vessel wall injury, lower risk of clot fragments, and decreased time to reperfusion (8, 11). Also, FPE is associated with better outcomes than MPE after achieving successful or complete recanalization (12). Thus, identifying factors influencing FPE could help clinicians and interventionalists maximize the benefit of MT through suitable patient selection and pre-interventional risk modification. There are many studies seeking to explore this phenomenon, but with inconsistent results (7, 8, 11, 13–20). For example, balloon guide catheters (BGC) and non-internal carotid artery (ICA) terminus occlusion were correlated with FPE in the study of Zaidat et al. (7), but factors such as older age, a lower systolic blood pressure, and conscious sedation were not (17).
Thus, this systematic review and meta-analysis seeks to summarize the current literature investigating influencing factors of thrombectomy with first pass and elucidate associations with it.
Methods
This study was reported in conformity to the criterion of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (21).
Search Strategy
Eligible studies were independently searched by two reviewers from the following databases: MEDLINE, EMBASE, Web of Science, and the Cochrane Library. Clinical trial registers were also searched as potential sources. The included studies were restricted to the publication time before October 31, 2020, and the English language. The following key words were used: “acute ischemic stroke,” “mechanical thrombectomy,” “endovascular thrombectomy,” “first pass effect,” “first attempt,” “recanalization.” A search strategy Table is presented in detail in the online supplementary material (online Supplementary Table 1).
Study Selection
Patient Selection Criteria
Inclusion criteria included age ≥18 years with AIS due to large vessel occlusion, including the anterior or posterior circulation. Arterial occlusion was confirmed by computed tomographic angiography (CTA), magnetic resonance angiography (MRA), or digital subtraction angiography (DSA). Exclusion criteria included patients with baseline pre-stroke mRS score ≥3 and artery occlusion of non-atherosclerotic etiology such as dissection, moyamoya disease, vasospasm, or vasculitis. Patients with ICH, significant cerebellar mass effect, and acute hydrocephalus on CT or MRI before the onset of stroke were also excluded.
Definitions
FPE was defined as achieving successful or complete recanalization by MT after first pass regardless of thrombectomy device, such as contact aspiration and stent retriever. By contrast, non-FPE was defined as failure to achieve successful or complete recanalization by MT after first pass using different thrombectomy devices, such as contact aspiration and stent retriever.
Outcome
The primary outcome was successful recanalization with FPE, and secondary outcome was complete recanalization with FPE. The definitions of successful recanalization and complete recanalization were up to modified thrombolysis in cerebral ischemia (mTICI) score of 2b-3 and 2c-3 respectively after MT by post-interventional DSA as per usual convention (22, 23).
Studies
RCTs and observational studies including cohort studies, case-controlled studies, and case series where the number of patients exceeded 10 were included to avoid type II errors from low power (24, 25). Case reports, conference abstracts, or case series reports with the number of included patients <10 were excluded.
Selection of Studies and Data Extraction
Studies which qualified were extracted by two independent reviewers (YZ and RX). In the initial stage of screening, titles, keywords, and abstracts were screened, and irrelevant studies were then excluded. Subsequently, reviewers obtained the full articles of all the remaining studies and checked the full texts to ascertain the included variables. In addition, the reasons for inclusion or exclusion of studies after full-text check were recorded. Disagreement in study selection between two reviewers was resolved by a third reviewer (TW).
Two reviewers independently (LL and XW) extracted the data according to a standardized data extraction form. The extracted information of included studies was as follows: (1) Authors, publication time, country, number of patients in FPE and non-FPE groups, inclusion and exclusion criteria; (2) Mean age, gender, medical history, site of occlusion by angiography, admission NIHSS score, baseline ASPECTS, MT strategy, use of tPA, and procedural times. The resolution of disagreement regarding data extraction was achieved through assistance of a third reviewer (TW). For missing or unclear data in included studies, effort was made to contact the corresponding authors by e-mail in order to best guarantee the accuracy of data.
Assessment Risk Bias and Heterogeneity
Two reviewers (YF and CSM) independently assessed the risk of bias of each included study. The Cochrane Collaboration criteria were applied for RCTs, and the Newcastle–Ottawa scale was used for observational studies, including cohort studies and case–control studies (26). For case series, the method described in Methodological Quality and Synthesis of Case Series and Case Reports was applied (27). The heterogeneity of pooled outcomes was evaluated by the I2 statistic. The I2 statistic that was >60% demonstrated high heterogeneity, and the DerSimonian and Laird method for random-effect estimation was performed for pooling outcomes. If heterogeneity was mild or moderate, the Mantel–Haenszel method for fixed-effect estimation was applied. In instances where heterogeneity of outcomes and sufficient studies were high, we conducted subgroup analysis by site of occlusion, such as anterior circulation or posterior circulation. The meta-regression and sensitivity analysis were also used to explore the potential sources of heterogeneity.
Statistical Analysis
The STATA statistical software package (version 15.0, Stata Corp, College station, Texas, USA) was used for all data analysis and heterogeneity assessments. For dichotomous data, we adopted odds ratios (OR) with 95% confidential interval (CI), and the mean difference (MD) with 95% CI was used for continuous data. The standard of p-value <0.05 was regarded as statistically significant. If the number of included studies was more than 10, publication bias was assessed by visualization of a funnel plot.
Results
Study Selection and Study Characteristics
There were 924 records identified through the main database and clinical trials registers, and 16 studies were finally eligible for inclusion in the qualitative and quantitative analysis. The flow diagram of study selection is demonstrated in Figure 1.
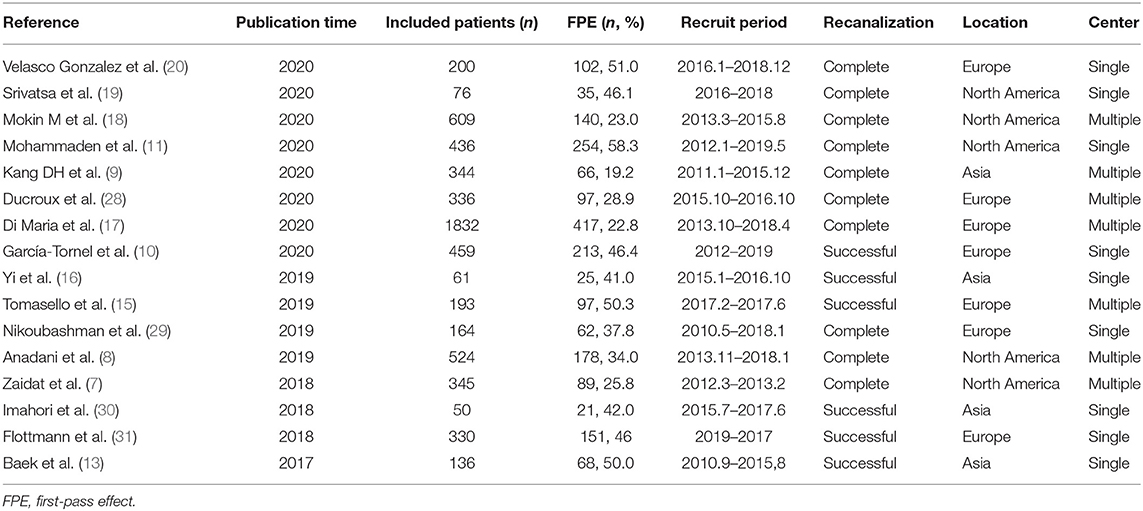
Table 1 depicts the characteristics of included studies. A total of 16 studies and 6,095 patients were eligible according to inclusion criteria. Among them, 2015 (33.1%) patients achieved recanalization with FPE. All studies were published after 2016, seven conducted in Europe, five conducted in North America, and four in Asia. There were seven multicenter studies, and the remaining were single-center investigations. The number of patients in each study ranged from 50 to 1,832, and the numbers of male and female patients were essentially equal [2,929 (50.05%) vs. 2,923 (49.95%)]. Mean NIHSS scores ranged from 2 to 28. The location of occlusion by angiography was mostly within the anterior circulation, such as ICA and middle cerebral artery (MCA), particularly the M1 and M2 segments (Online Supplementary Table 2).
Influencing Factors
The following factors were assessed: age, gender, hypertension, DM, coronary artery disease, smoking history, atrial fibrillation, dyslipidemia, previous anticoagulation therapy, initial NIHSS score, systolic blood pressure, diastolic blood pressure, suspected stroke etiology, IV thrombolysis, stroke laterality, location of occlusion, anterior communicating artery (AComA) and posterior communicating artery (PComA) presence, and intervention characteristics.
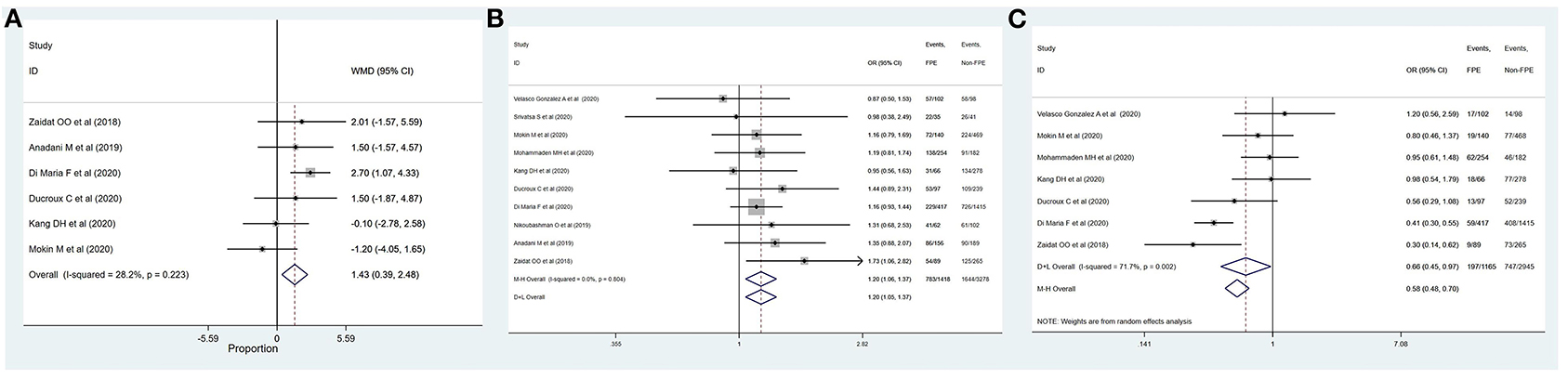
Determinants for Achieving Successful Recanalization With FPE
The outcomes of meta-analysis showed that age (MD: 1.21, 95% CI: 0.26–2.16; p = 0.012), female gender (OR: 1.12, 95% CI: 1.00–1.26; p = 0.046), DM (OR: 1.17, 95% CI: 1.01–1.35; p = 0.032), ICA location (OR: 0.71, 95% CI: 0.52–0.97; p = 0.033), M2 segment (OR: 1.36, 95% CI: 1.05–1.77; p = 0.019), duration of intervention (MD: −27.85, 95% CI: −42.11–13.58; p < 0.001), time of onset to recanalization (MD: −34.63, 95% CI: −58.45–10.81; p = 0.004), general anesthesia (OR: 0.63, 95% CI: 0.52–0.77; p < 0.001), and use of BGC (OR: 1.60, 95% CI: 1.17–2.18; p = 0.003) were significantly associated with successful recanalization with FPE (Table 2 and Figures 2, 3). The remainder were not significantly correlated with achieving successful recanalization with FPE (online Supplementary Figures 1, 2).
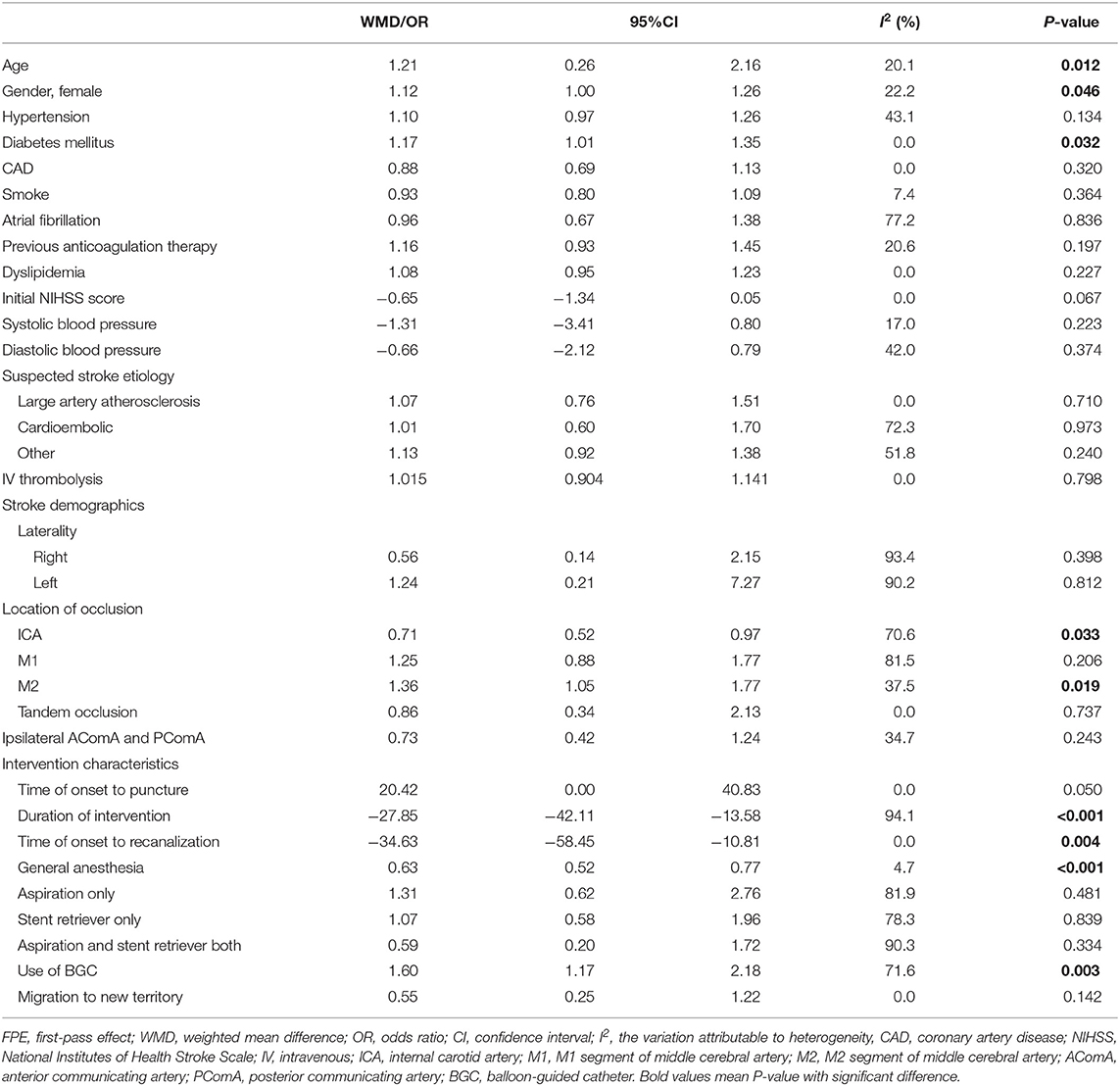
Table 2. Summary of meta-analysis of influencing factors for achieving successful recanalization with FPE.
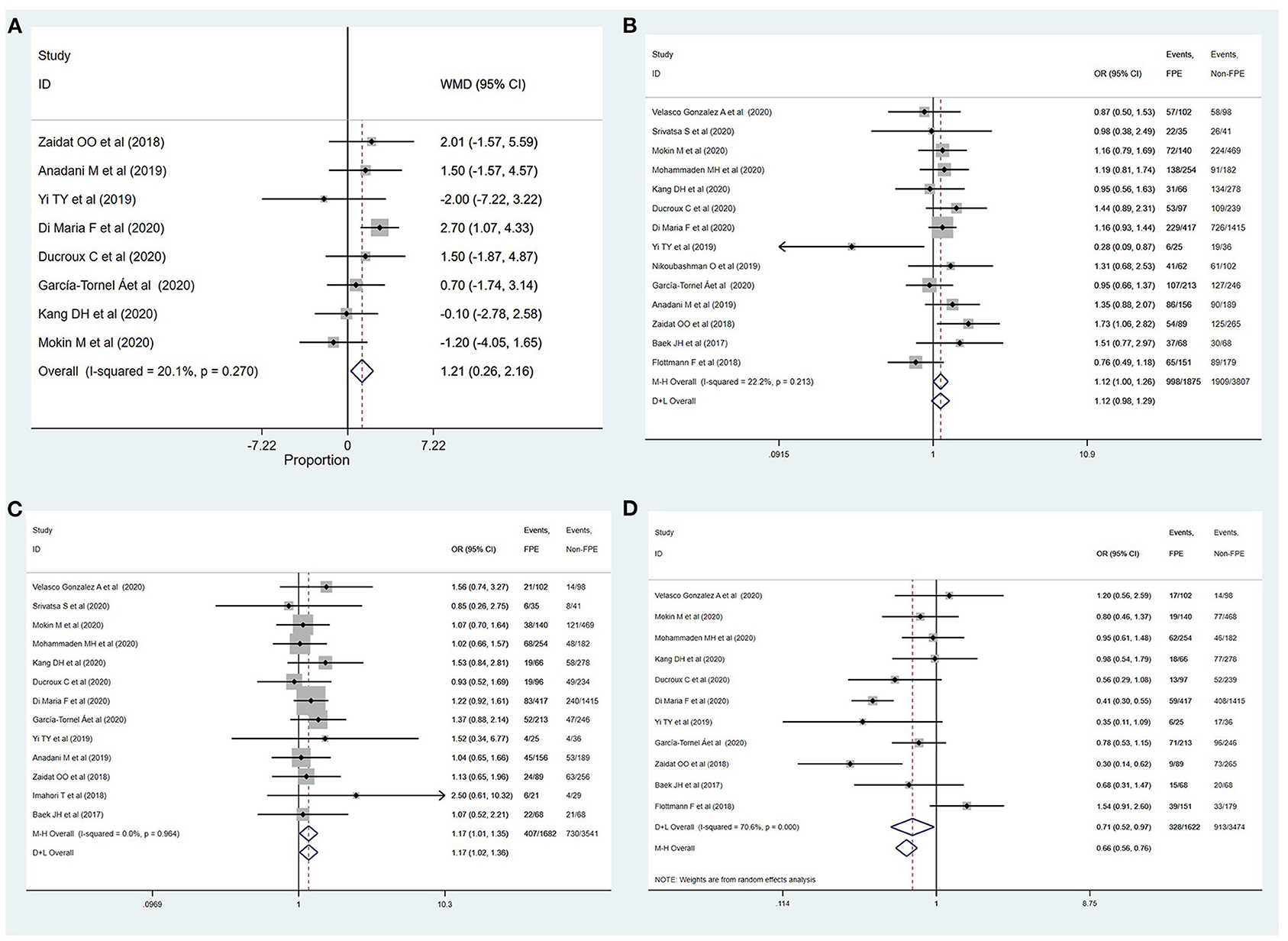
Figure 2. Determinants of achieving successful recanalization with FPE. (A) Age; (B) female; (C) diabetes mellitus; (D) ICA.
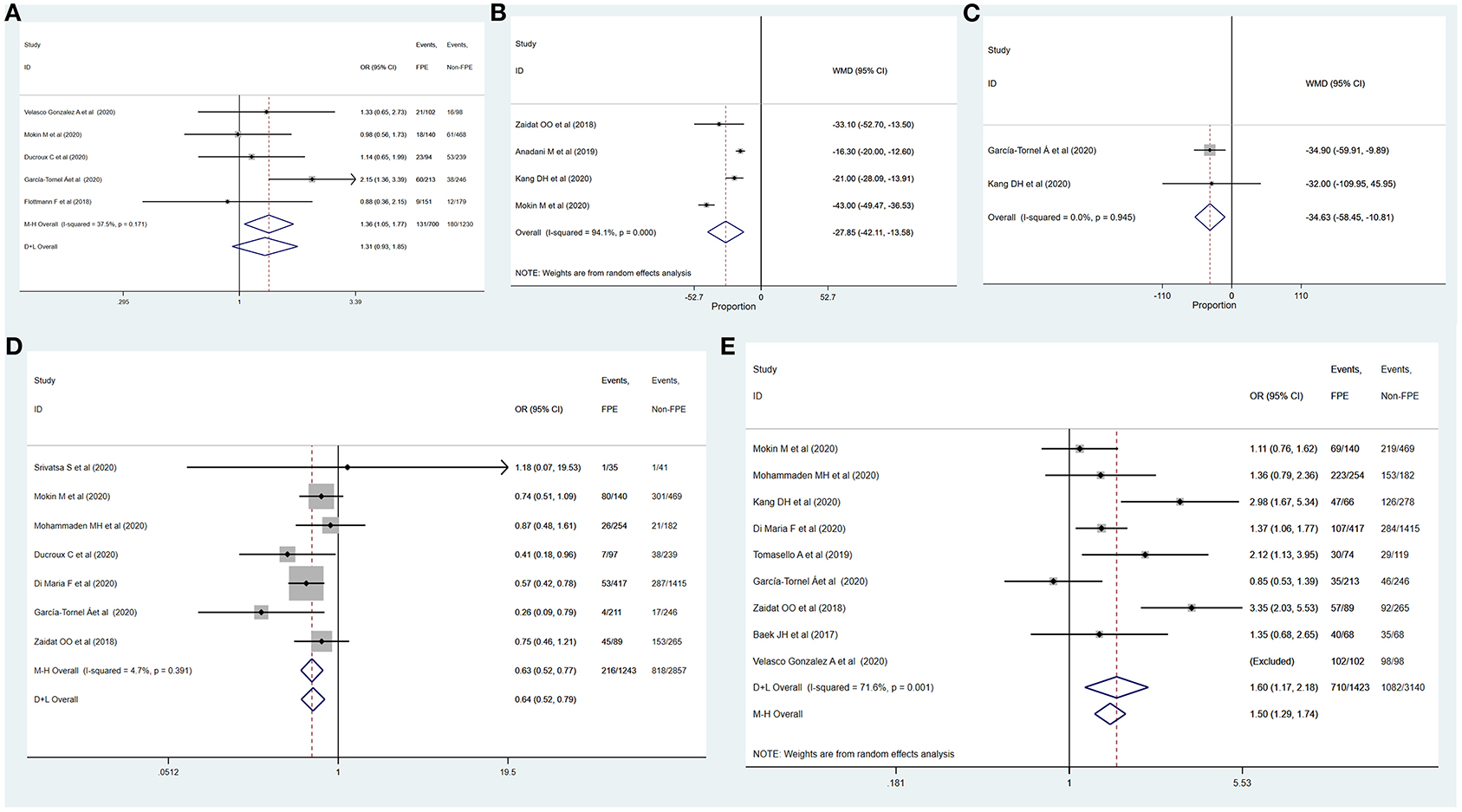
Figure 3. Determinants of achieving successful recanalization with FPE. (A) M2; (B) duration of intervention; (C) time of onset to recanalization; (D) general anesthesia; (E) use of BGC.
Determinants for Achieving Complete Recanalization With FPE
Table 3 summarizes the results of meta-analysis of factors influencing complete recanalization with FPE. Age (MD: 1.43, 95% CI: 0.39–2.48; p = 0.007), female gender (OR: 1.20, 95% CI: 1.06–1.37; p = 0.006), ICA (OR: 0.66, 95% CI: 0.45–0.97; p = 0.035), duration of intervention (MD: −27.85, 95% CI: −42.11–13.58; p < 0.001), general anesthesia (OR: 0.65, 95% CI: 0.54–0.80; p < 0.001), and use of BGC (OR: 1.81, 95% CI: 1.27–2.59; p = 0.001) were significantly associated with the complete recanalization with FPE (Figures 4, 5). The remainder were not significantly correlated with achieving successful recanalization with FPE (Online Supplementary Figures 3, 4).

Table 3. Summary of meta-analysis of influencing factors for achieving complete recanalization with FPE.
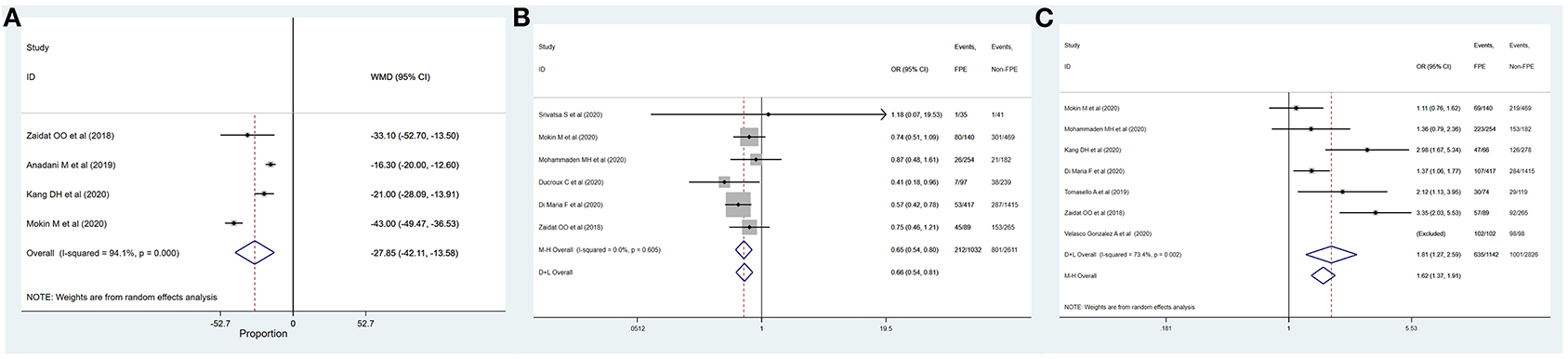
Figure 5. Determinants of achieving complete recanalization with FPE. (A) Duration of intervention; (B) general anesthesia; (C) use of BGC.
Risk of Bias in Studies Included
The Newcastle–Ottawa scale was used to assess the bias risk of observational studies, such as case–control studies, with the majority of included studies being low risk bias (online Supplementary Table 3). Both meta-regression and sensitive analysis were conducted to explore the potential heterogeneity. We also used funnel plots to explore the publication bias, with the results demonstrating no evident reporting bias (Supplementary Figures 5–16).
Discussion
In this systematic review and meta-analysis, the proportion of FPE ranged from 19 to 58% in the endovascular treatment of LVO inclusive of M2 occlusions. Factors contributing to successful recanalization with FPE included age, female gender, DM, general anesthesia, use of BGC, and occlusion of ICA and M2 segment. Among those, age, female gender, general anesthesia, use of BGC, and occlusion of ICA also increased the chance of complete reperfusion after first-pass thrombectomy.
BGC use has been widely accepted contributing to FPE during thrombectomy procedure (7, 9, 13, 15). One of the reasons may be decreased distal embolization and more importantly increased flow reversal. According to Kang et al. (9), additional positive effects of BGC use were suggested. One is the force needed for clot retrieving, including impaction force and combined force of friction and adhesion between the thrombus and vessel wall. The other is that inflating the BGC can markedly reduce systemic blood pressure on the proximal clot surface and decrease the pressure gradient across the clot.
It is difficult to explain why increased age was found a contributor to successful and complete recanalization after first-pass thrombectomy. One possible reason may be stroke etiology, as elderly patients are more likely to have cardioembolic cause (32). Clots from cardioembolic causes are more likely to be rich in red blood cells whereas thromboembolism due to preexisting atherosclerosis may be rich in fibrin and platelets. Clots composed predominantly of RBCs are considered fresh and less compact, and this may lead to easier recanalization through thrombectomy with first pass (33–37). Also, increased fibrin percentage could decrease the possibility of clot complete retrieval (38, 39). However, heterogeneous results exist among studies and we could not detect a relationship between FPE and stroke etiology, which may be due to limited data.
This study showed that females are more likely to achieve FPE than males. This phenomenon has been described by Zaidat et al. (7). Anatomical, pathophysiological, and biochemical factors may potentially account for observed difference in response to recanalization therapy between sexes (40). In addition, there was a difference of endogenous fibrinolytic activity between males and females (35, 41). Further studies are needed to explore the underlying biochemical interactions which are further felt to change with age/menopause (42).
Conscious sedation has been associated with better outcomes of MT than general anesthesia in previous researches (43). In this study, we further extended this preference of local anesthesia considering FPE, but the mechanisms remain unknown (17). One hypothesis is a shorter time to reperfusion by conscious sedation (44), as dynamic changes of clot composition found in previous studies, such as fibrin deposition, may increase the risk of re-occlusion (34, 36). However, some studies have mentioned that GA is associated with better outcome than conscious sedation. So, comparison of different anesthesia modalities needs further research (45). At the same time, difference in clot length may be a principal reason for the association between clot location and FPE. It was found that clots in ICA were with longer length and those in M2 segment were with relatively shorter length (7, 17).
There are some limitations of this study. Recruited studies were mostly retrospective with small sample size, and variables observed were not uniform. Some potentially important factors, such as clot volume (13), were only investigated occasionally and thus could not be reliably meta-analyzed. Potential differences may exist between anterior and posterior circulation stroke, and separate analysis may be more valuable. Also, device development could also influence the recanalization outcome, and comparison among different thrombectomy techniques may also be very important. However, it is unable to be analyzed due to high heterogeneity among studies. It remains elusive why DM was a contributor to successful recanalization with FPE (46). Maybe this is caused by bias from limited studies and should be further studied.
Conclusion
Age, gender, occlusion site, conscious sedation, and use of BGC were factors influencing both successful and complete recanalization after first-pass thrombectomy. Further studies with more comprehensive observational indices are needed to confirm these observations.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
XB, XZ, and LJ developed the initial idea for this study and formulated the study design. YZ, AD, TW, RX, YF, XW, and KY developed and revised the search strategy. LJ, YM, HS, and QM were consulted about clinical issues. XB, XZ, and JW contributed to the original draft. XB, XZ, AD, JW, YZ, TW, LL, KY, YM, HS, QM, and LJ were responsible for the revision of the draft. All authors approved the final version of the manuscript before submission.
Funding
This work was supported by the National Key Research and Development Project (Grant number 2016YFC1301703) and the Beijing Scientific and Technologic Project (Z201100005520019).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.628523/full#supplementary-material
References
1. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics-−2012 update: a report from the American Heart Association. Circulation. (2012) 125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046
2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. (2018) 49:e46–e110. doi: 10.1161/STR.0000000000000158
3. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. (2018) 378:11–21. doi: 10.1056/NEJMoa1706442
4. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for Stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. (2018) 378:708–18. doi: 10.1056/NEJMoa1713973
5. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. (2015) 372:11–20. doi: 10.1056/NEJMoa1411587
6. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after Symptom Onset in Ischemic Stroke. New England J Med. (2015) 372:2296–306. doi: 10.1056/NEJMoa1503780
7. Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First Pass Effect: a new measure for stroke thrombectomy devices. Stroke. (2018) 49:660–6. doi: 10.1161/strokeaha.117.020315
8. Anadani M, Alawieh A, Vargas J, Chatterjee AR, Turk A, Spiotta A. First attempt recanalization with ADAPT: rate, predictors, and outcome. J Neurointerv Surg. (2019) 11:641–5. doi: 10.1136/neurintsurg-2018-014294
9. Kang DH, Kim BM, Heo JH, Nam HS, Kim YD, Hwang YH, et al. Effects of first pass recanalization on outcomes of contact aspiration thrombectomy. J Neurointerv Surg. (2020) 12:466–70. doi: 10.1136/neurintsurg-2019-015221
10. Garcia-Tornel A, Requena M, Rubiera M, Muchada M, Pagola J, Rodriguez-Luna D, et al. When to stop. Stroke. (2019) 50:1781–8. doi: 10.1161/STROKEAHA.119.025088
11. Mohammaden MH, Haussen DC, Pisani L, Al-Bayati AR, Perry da Camara C, Bhatt N, et al. Baseline ASPECTS and hypoperfusion intensity ratio influence the impact of first pass reperfusion on functional outcomes. J Neurointerv Surg. (2020). doi: 10.1136/neurintsurg-2020-015953
12. Bai X, Zhang X, Yang W, Zhang Y, Wang T, Xu R, et al. Influence of first-pass effect on recanalization outcomes in the era of mechanical thrombectomy: a systemic review and meta-analysis. Neuroradiology. (2020). doi: 10.1007/s00234-020-02586-7. [Epub ahead of print].
13. Baek JH, Yoo J, Song D, Kim YD, Nam HS, Kim BM, et al. Predictive value of thrombus volume for recanalization in stent retriever thrombectomy. Sci Rep. (2017) 7:15938. doi: 10.1038/s41598-017-16274-9
14. Jindal G, Carvalho HP, Wessell A, Le E, Naragum V, Miller TR, et al. Beyond the first pass: revascularization remains critical in stroke thrombectomy. J Neurointerv Surg. (2019) 11:1095–9. doi: 10.1136/neurintsurg-2019-014773
15. Tomasello A, Ribo M, Gramegna LL, Melendez F, Rosati S, Moreu M, et al. Procedural approaches and angiographic signs predicting first-pass recanalization in patients treated with mechanical thrombectomy for acute ischaemic stroke. Interv Neuroradiol. (2019) 25:491–6. doi: 10.1177/1591019919847623
16. Yi TY, Chen WH, Wu YM, Zhang MF, Zhan AL, Chen YH, et al. Microcatheter “first-pass effect” predicts acute intracranial artery atherosclerotic disease-related occlusion. Neurosurgery. (2019) 84:1296–305. doi: 10.1093/neuros/nyy183
17. Di Maria F, Kyheng M, Consoli A, Desilles JP, Gory B, Richard S, et al. Identifying the predictors of first-pass effect and its influence on clinical outcome in the setting of endovascular thrombectomy for acute ischemic stroke: results from a multicentric prospective registry. Int J Stroke. (2020) 16:20–8. doi: 10.1177/1747493020923051
18. Mokin M, Primiani CT, Castonguay AC, Nogueira RG, Haussen DC, English JD, et al. First pass effect in patients treated with the trevo stent-retriever: a TRACK registry study analysis. Front Neurol. (2020) 11:83. doi: 10.3389/fneur.2020.00083
19. Srivatsa S, Duan Y, Sheppard JP, Pahwa S, Pace J, Zhou X, et al. Cerebral vessel anatomy as a predictor of first-pass effect in mechanical thrombectomy for emergent large-vessel occlusion. J Neurosurg. (2020):1–9. doi: 10.3171/2019.11.Jns192673
20. Velasco Gonzalez A, Görlich D, Buerke B, Münnich N, Sauerland C, Rusche T, et al. Predictors of successful first-pass thrombectomy with a balloon guide catheter: results of a decision tree analysis. Transl Stroke Res. (2020) 11:900–9. doi: 10.1007/s12975-020-00784-2
21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. (2010) 8:336–41. doi: 10.1016/j.ijsu.2010.02.007
22. Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, et al. Modified thrombolysis in cerebral infarction 2C/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights from the ASTER trial (contact aspiration versus stent retriever for successful revascularization). Stroke. (2018) 49:1189–96. doi: 10.1161/strokeaha.118.020700
23. Almekhlafi MA, Mishra S, Desai JA, Nambiar V, Volny O, Goel A, et al. Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv Neuroradiol. (2014) 20:21–7. doi: 10.15274/inr-2014-10004
24. Bai X, Feng Y, Yang K, Wang T, Luo J, Wang X, et al. Extracranial-intracranial bypass surgery for occlusive atherosclerotic disease of the anterior cerebral circulation: protocol for a systematic review and meta-analysis. Syst Rev. (2020) 9:70. doi: 10.1186/s13643-020-01325-6
25. Feng Y, Li L, Bai X, Wang T, Chen Y, Zhang X, et al. Risk factors for new ischaemic cerebral lesions after carotid artery stenting: protocol for a systematic review and meta-analysis. BMJ Open. (2019) 9:e030025. doi: 10.1136/bmjopen-2019-030025
26. Lo CK, Mertz D, Loeb M. Newcastle-ottawa scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
27. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. (2018) 23:60–3. doi: 10.1136/bmjebm-2017-110853
28. Ducroux C, Piotin M, Gory B, Labreuche J, Blanc R, Ben Maacha M, et al. First pass effect with contact aspiration and stent retrievers in the Aspiration versus Stent Retriever (ASTER) trial. J Neurointerv Surg. (2020) 12:386–91. doi: 10.1136/neurintsurg-2019-015215
29. Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect. Stroke. (2019) 50:2140–6. doi: 10.1161/STROKEAHA.119.025148
30. Imahori T, Okamura Y, Sakata J, Shose H, Yokote A, Matsushima K, et al. Stent expansion and in-stent thrombus sign in the trevo stent retriever predict recanalization and possible etiology during mechanical thrombectomy: a case series of 50 patients with acute middle cerebral artery occlusion. World Neurosurg. (2018). doi: 10.1016/j.wneu.2018.12.087. [Epub Ahead of Print].
31. Flottmann F, Leischner H, Broocks G, Nawabi J, Bernhardt M, Faizy TD, et al. Recanalization rate per retrieval attempt in mechanical thrombectomy for acute ischemic stroke. Stroke. (2018) 49:2523–2525. doi: 10.1161/STROKEAHA.118.022737
32. Grifoni E, Giglio D, Guazzini G, Cosentino E, Latini E, Dei A, et al. Age-related burden and characteristics of embolic stroke of undetermined source in the real world clinical practice. J Thromb Thrombolysis. (2020) 49:75–85. doi: 10.1007/s11239-019-01951-5
33. Zivin JA, Fisher M, DeGirolami U, Hemenway CC, Stashak JA. Tissue plasminogen activator reduces neurological damage after cerebral embolism. Science. (1985) 230:1289–92. doi: 10.1126/science.3934754
34. Niessen F, Hilger T, Hoehn M, Hossmann KA. Differences in clot preparation determine outcome of recombinant tissue plasminogen activator treatment in experimental thromboembolic stroke. Stroke. (2003) 34:2019–24. doi: 10.1161/01.STR.0000080941.73934.30
35. Forster A, Gass A, Kern R, Wolf ME, Ottomeyer C, Zohsel K, et al. Gender differences in acute ischemic stroke: etiology, stroke patterns and response to thrombolysis. Stroke. (2009) 40:2428–32. doi: 10.1161/STROKEAHA.109.548750
36. Pikija S, Magdic J, Trkulja V, Unterkreuter P, Mutzenbach JS, Novak HF, et al. Intracranial thrombus morphology and composition undergoes time-dependent changes in acute ischemic stroke: a CT densitometry study. Int J Mol Sci. (2016) 17:1959. doi: 10.3390/ijms17111959
37. Goldmakher GV, Camargo EC, Furie KL, Singhal AB, Roccatagliata L, Halpern EF, et al. Hyperdense basilar artery sign on unenhanced CT predicts thrombus and outcome in acute posterior circulation stroke. Stroke. (2009) 40:134–9. doi: 10.1161/STROKEAHA.108.516690
38. Duffy S, McCarthy R, Farrell M, Thomas S, Brennan P, Power S, et al. Per-pass analysis of thrombus composition in patients with acute ischemic stroke undergoing mechanical thrombectomy. Stroke. (2019) 50:1156–63. doi: 10.1161/STROKEAHA.118.023419
39. Gunning GM, McArdle K, Mirza M, Duffy S, Gilvarry M, Brouwer PA. Clot friction variation with fibrin content; implications for resistance to thrombectomy. J Neurointerv Surg. (2018) 10:34–8. doi: 10.1136/neurintsurg-2016-012721
40. Savitz SI, Schlaug G, Caplan L, Selim M. Arterial occlusive lesions recanalize more frequently in women than in men after intravenous tissue plasminogen activator administration for acute stroke. Stroke. (2005) 36:1447–51. doi: 10.1161/01.STR.0000170647.42126.a8
41. Hill MD, Kent DM, Hinchey J, Rowley H, Buchan AM, Wechsler LR, et al. Sex-based differences in the effect of intra-arterial treatment of stroke: analysis of the PROACT-2 study. Stroke. (2006) 37:2322–5. doi: 10.1161/01.STR.0000237060.21472.47
42. Towfighi A, Saver JL, Engelhardt R, Ovbiagele B. A midlife stroke surge among women in the United States. Neurology. (2007) 69:1898–904. doi: 10.1212/01.wnl.0000268491.89956.c2
43. Campbell BCV, van Zwam WH, Goyal M, Menon BK, Dippel DWJ, Demchuk AM, et al. Effect of general anaesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient data. Lancet Neurol. (2018) 17:47–53. doi: 10.1016/s1474-4422(17)30407-6
44. Powers CJ, Dornbos D 3rd, Mlynash M, Gulati D, Torbey M, Nimjee SM, et al. Thrombectomy with conscious sedation compared with general anesthesia: a DEFUSE 3 analysis. AJNR Am J Neuroradiol. (2019) 40:1001–5. doi: 10.3174/ajnr.A6059
45. Bai X, Zhang X, Wang T, Feng Y, Wang Y, Lyu X, et al. General anesthesia versus conscious sedation for endovascular therapy in acute ischemic stroke: a systematic review and meta-analysis. J Clin Neurosci. (2021) 86:10–7. doi: 10.1016/j.jocn.2021.01.012
Keywords: acute ischemic stroke, mechanical thrombectomy, first pass effect, influencing factors, systematic review, meta-analysis
Citation: Bai X, Zhang X, Wang J, Zhang Y, Dmytriw AA, Wang T, Xu R, Ma Y, Li L, Feng Y, Mena CS, Yang K, Wang X, Song H, Ma Q and Jiao L (2021) Factors Influencing Recanalization After Mechanical Thrombectomy With First-Pass Effect for Acute Ischemic Stroke: A Systematic Review and Meta-Analysis. Front. Neurol. 12:628523. doi: 10.3389/fneur.2021.628523
Received: 12 November 2020; Accepted: 08 March 2021;
Published: 09 April 2021.
Edited by:
Jin Soo Lee, Ajou University, South KoreaReviewed by:
Yong-Won Kim, Kyungpook National University Hospital, South KoreaTareq Kass-Hout, Rush University Medical Center, United States
Copyright © 2021 Bai, Zhang, Wang, Zhang, Dmytriw, Wang, Xu, Ma, Li, Feng, Mena, Yang, Wang, Song, Ma and Jiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liqun Jiao, bGlxdW5qaWFvQHNpbmEuY24=
†These authors have contributed equally to this work and share first authorship
 Xuesong Bai
Xuesong Bai Xiao Zhang1,2†
Xiao Zhang1,2† Adam A. Dmytriw
Adam A. Dmytriw Ran Xu
Ran Xu Long Li
Long Li Yao Feng
Yao Feng Xue Wang
Xue Wang Haiqing Song
Haiqing Song Qingfeng Ma
Qingfeng Ma Liqun Jiao
Liqun Jiao