- 1School of Medicine, I-Shou University, Kaohsiung, Taiwan
- 2Department of Neurosurgery, E-Da Hospital, Kaohsiung, Taiwan
- 3Department of Nephrology, E-Da Hospital, Kaohsiung, Taiwan
- 4Division of Neurology, China Medical University Hospital, Taichung, Taiwan
- 5Neurological Institute, Taichung Veterans General Hospital, Taichung, Taiwan
- 6Department of Neurology, Show Chwan Memorial Hospital, Changhua, Taiwan
- 7Department of Neurology, St. Martin de Porres Hospital, Chiayi, Taiwan
- 8Department of Neurology, Chang Bing Show Chwan Memorial Hospital, Changhua, Taiwan
- 9Department of Neurology, Tainan Municipal An-Nan Hospital-China Medical University, Tainan, Taiwan
- 10Department of Neurology, En Chu Kong Hospital, New Taipei, Taiwan
- 11Department of Neurology, Lin Shin Hospital, Taichung, Taiwan
- 12Department of Neurology, Tri-Service General Hospital, Taipei, Taiwan
- 13Department of Neurology, Cheng Hsin General Hospital, Taipei, Taiwan
- 14Department of Neurology, Shin Kong Wu Ho Su Memorial Hospital, Taipei, Taiwan
- 15Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
- 16College of Medicine, China Medical University, Taichung, Taiwan
- 17Department of Neurology, China Medical University Hospital, Taichung, Taiwan
- 18Graduate Institute of Clinical Medical Science, China Medical University, Taichung, Taiwan
Objective: Stroke in young adults is uncommon, and the etiologies and risk factors of stroke in young adults differ from those in older populations. Smoker's paradox is an unexpected favorable outcome, and age difference is used to explain the association between smoking and the favorable functional outcome. This study aimed to investigate the existence of this phenomenon in young stroke patients.
Methods: We analyzed a total of 9,087 young stroke cases registered in the nationwide stroke registry system of Taiwan between 2006 and 2016. Smoking criteria included having a current history of smoking more than one cigarette per day for more than 6 months. After matching for sex and age, a Cox model was used to compare mortality and function outcomes between smokers and non-smokers.
Results: Compared with the non-smoker group, smoking was associated with older age, higher comorbidities, and higher alcohol consumption. Patients who report smoking with National Institutes of Health Stroke Scale scores of 11–15 had a worse functional outcome (adjusted odds ratio, 0.81; 95% confidence interval, 0.76 – 0.87).
Conclusion: Smokers had a higher risk of unfavorable functional outcomes at 3 months after stroke, and therefore, we continue to strongly advocate the importance of smoking cessation.
Introduction
Stroke in young adults is relatively uncommon (1–4). Although the prognosis of young stroke is generally considered benign, young adults with stroke are at a higher risk of recurrent stroke and mortality than their healthy peers. Most survivors between 20 and 50 years may have emotional, social, or physical sequelae that impair their quality of life (4, 5). In addition, young stroke victims are often responsible for providing child care or generating income for their families. Therefore, young stroke is a major health and socioeconomic problem.
Smoking is one of the biggest public health threats associated with many chronic diseases, such as cardiovascular disease and cancer (6–8). More importantly, smoking is also aggregated with other adverse behaviors, such as chewing bet-but and drinking alcohol. However, several recent studies observed an improved outcome in smokers with antithrombotic therapy after an index cardiovascular event, a phenomenon called “smoker's paradox” (9–13). Sample sizes in these studies are small (10, 11). Moreover, no study has examined the effects of pre-stroke smoking on post-stroke long-term outcome.
In Taiwan, about 24,000 smokers die of smoking and nearly 2,600 non-smokers die of second-hand smoke each year. Since the enactment of the Tobacco Hazards Prevention Act (THPA) in 1997, smoking prevalence has decreased. However, Taiwan still records a 15% adult smoking rate. The purpose of this study was to evaluate the effect of smoking status on stroke outcome in young stroke.
Methods
Standard Protocol Approvals, Registrations, and Patient Consents
The Taiwan Stroke Registry (TSR) program was started in 2006. Until now, 56 hospitals participated in this registration project. This study obtained ethical approval from China Medical University (CMUH104-REC2-115) and the institutional review boards of the collaborating hospitals. The TSR enrolls patients who were taken to hospital due to stroke, including ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, and transient ischemic attack (14–16). The National Institutes of Health Stroke Scale (NIHSS), and the modified Rankin Scale (mRS) were used to check the severity and outcome by trained neurologists in hospital. After discharge, study nurses followed up those patients every 3 months for at least 12 months. The Taiwan Stroke Registry investigators are listed in Appendix 1.
Study Design and Eligibility Criteria
All registered patients aged between 20 and 50 years from August 1, 2006, to May 20, 2016, were included in our study. Stroke type, NIHSS, pre-existing comorbidities, and functional outcomes were collected according to a pre-defined system. A smoker was defined as active tobacco smoking, more than one cigarette per day for more than 6 months at the time of stroke—a binary variable to distinguish between smokers and non-smokers. Due to assessment of young stroke, we excluded patients aged <20 and >50 years. Those who stopped smoking more than 2 years before stroke or did not complete the 3-month follow-up were excluded. Finally, 9,087 young stroke patients were included in this cohort study.
Main Outcome Measures and Statistical Analysis
The potential confounding factors in the present study, including age, gender, hypertension, diabetes mellitus, hyperlipidemia, heart disease, previous stroke, uremia, alcohol consumption, stroke type, and NIHSS score, were defined in accordance with the consensus TSR criteria (https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.110.936526).
All descriptive data are expressed as numbers (N) and percentages (%) of patients. Hazard ratios (HRs) and 95% confidence intervals (CIs) were assessed by Cox proportional hazards models in univariate analyses to compare demographic variables and risk factor prevalence at baseline and, in stratified multivariable analyses, to detect the independent predictors of mortality. HRs were adjusted for 11 variables: age, gender, hypertension, diabetes mellitus, hyperlipidemia, heart disease, previous stroke, uremia, alcohol consumption, stroke type, and NIHSS score. Statistical significance was considered at a p-value of <0.05.
NIHSS and mRS scores were used to assess stroke severity and functional outcomes. An mRS score of 3 or higher was considered an unfavorable outcome. Then, we used logistic regression analysis to calculate the odds ratios (ORs) for the evaluation of potential factors associated with discharging stroke patients for poor functional outcome (mRS score of 3–5) in the derivation group. Covariates, including age, gender, hypertension, diabetes mellitus, hyperlipidemia, heart disease, previous stroke, uremia, alcohol consumption, stroke type, and NIHSS score, were adjusted. Statistical significance was considered at a p-value of <0.05.
Data Availability Statement
The TSR raw data are not publicly available and are maintained by the Management Office for Health Data (Dry Lab), China Medical University Hospital (http://stroke.cmuh.org.tw/). All researchers can submit their proposals to the research committee of the TSR (dGFpd2Fuc3Ryb2tlcmVnaXN0cnlAZ21haWwuY29t). After permission, the results will be sent to investigators.
Results
Baseline Characteristics of Young Stroke Patients
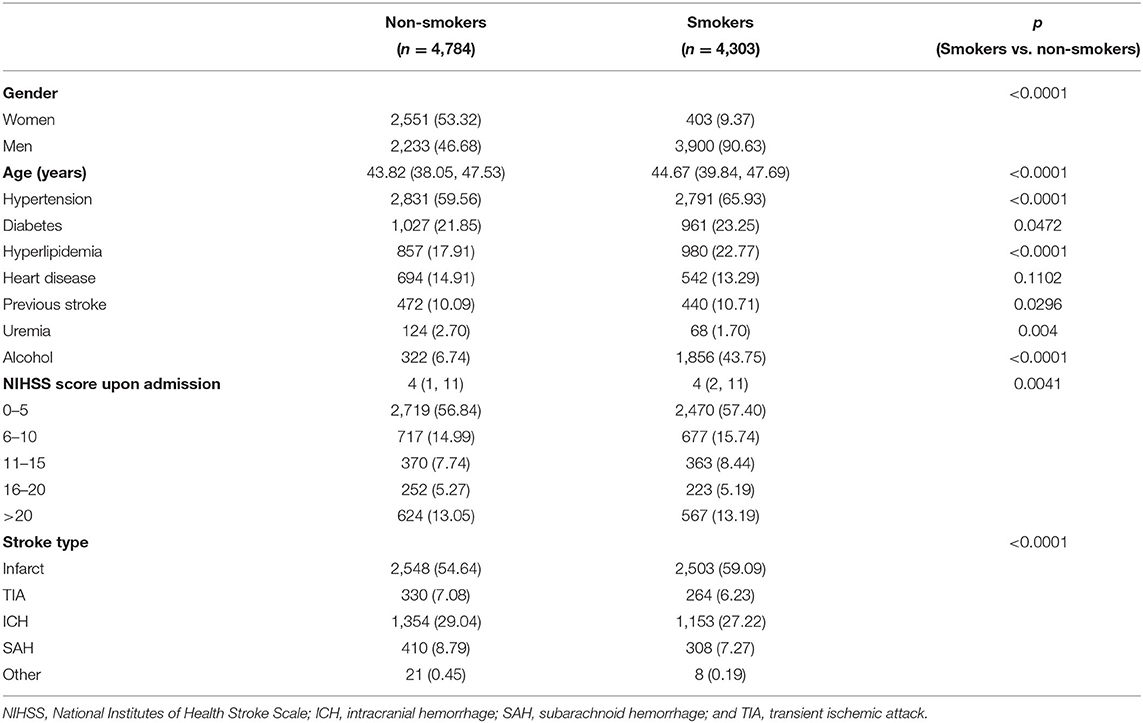
In the TSR, 9,087 young stroke patients were identified, including 4,303 smokers and 4,784 non-smokers. The smoker group had an older age and a higher stroke severity (NIHSS on admission) than the non-smoker group (Table 1). Compared with the non-smoker group, the smoker group had higher proportions of certain stroke risk factors, such as hypertension, diabetes, hyperlipidemia, previous stroke, and alcohol consumption.
Smoking and Mortality in Young Stroke Patients
No significant association was observed between smoking categories and mortality (adjusted HR, 0.89; 95%CI, 0.72–1.10) in the multivariate Cox regression model (Table 2). We further analyzed the adjusted HR values stratified by gender. The adjusted HRs in the male and female groups were 0.91 (95%CI 0.71–1.15) and 0.78 (95%CI 0.47–1.28), respectively. In smokers, higher mortality was noted only in the intracerebral hemorrhage (ICH) group (HR, 1.25; 95%CI, 1.03–1.51). However, after adjustment, the difference in ICH risk between smokers and non-smokers remains not statistically significant (adjusted HR, 1.08; 95%CI, 0.81–1.44).
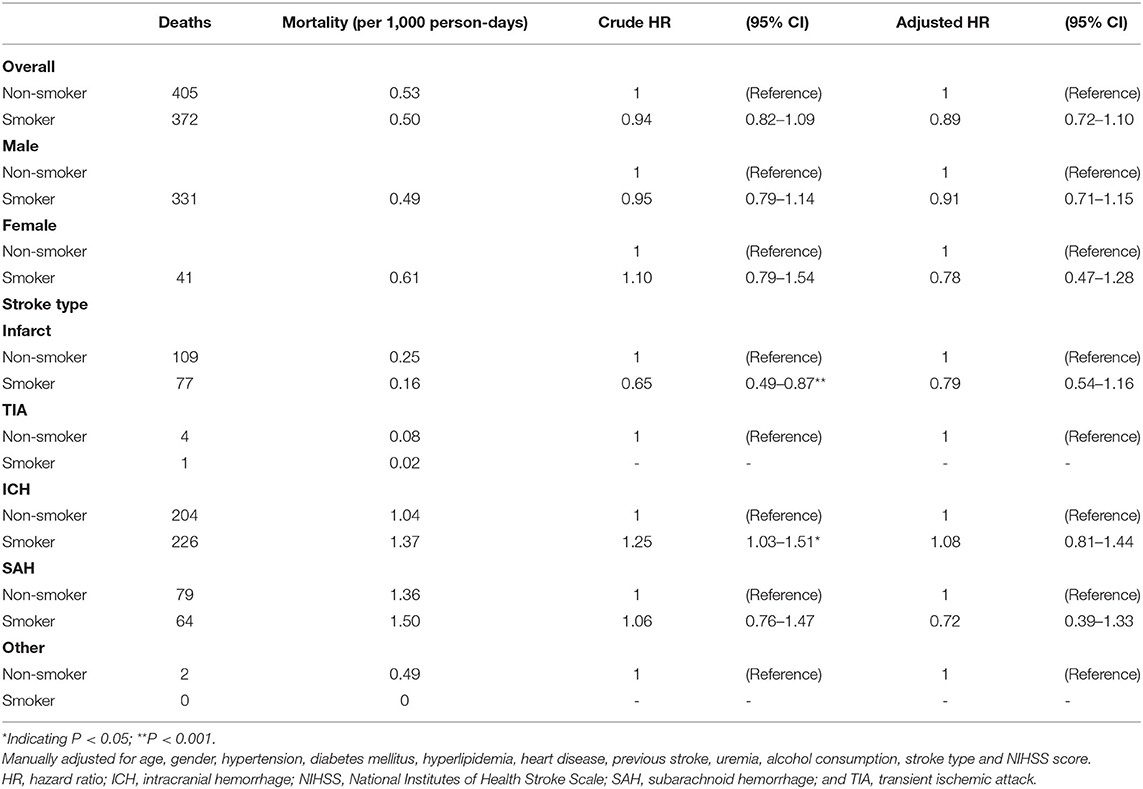
Table 2. Mortality and hazard ratio (HR) for stroke events in smokers compared to non-smokers in all stroke patients.
Smoking and the Functional Outcome in Young Stroke Patients
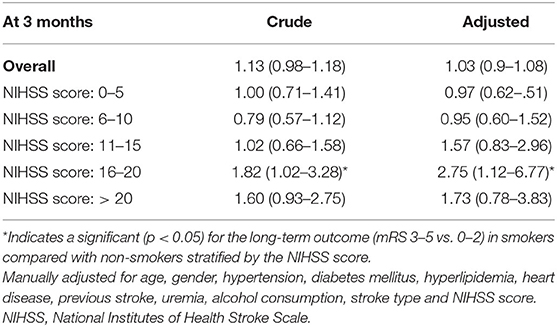
The poor functional outcome (with the mRS score of 3–5) between the two cohorts was assessed (Table 3). For NIHSS scores ranging between 16 and 20, adjusted ORs were only significant in smokers (OR, 2.75, 95% CI, 1.12– 6.77, respectively).
Discussion
In our community-based longitudinal study in young stroke, a total of 9,087 strokes were identified among patients aged ≤ 50 years. We observed a gender difference between smokers and non-smokers. Smokers were associated with the higher severity of the initial stroke (NIHSS score upon admission) and more ischemic stroke. In addition, modifiable risk factors are prevalent in smokers, including hypertension (66.41%), diabetes (23.59%), hypercholesterolemia (31.52%), previous stroke (11.50%), and alcohol consumption (42.35%). According to the stratified analysis, smoking has detrimental effects on post-stroke outcomes. However, only lower crude ratios for mortality, not adjusted HRs, were observed in the smoker group. Smoking cessation is recommended to improve post-stroke functional outcome.
Approximately 10% of strokes occur at ages ≤ 50 years, and the proportion of strokes in young adults has increased over time (3, 4). Despite their more favorable stroke outcomes, younger adult patients still have an obvious socioeconomic consequence because a large proportion of them are at a higher risk of future cardiovascular events and labor productivity loss. Besides this, the burden of disease is heavier in the case of recurrent events. Stroke is far more common in the geriatric population, and associations between risk factors for acute stroke and the clinical outcomes are stronger among older adults (1–4). However, the knowledge gleaned from research on older adults cannot always be applied to younger adults. Lutski et al. show that young adults have a high prevalence of modifiable vascular risk factors and, in particular, a high rate of smoking (17). In our study, we found that most strokes in young smokers were related to the existence of traditional stroke risk factors. There are several reasons why smokers may have a higher risk of developing stroke. Smoking increases the risk of complex atherosclerotic cardiovascular events, including deleterious effects on the endothelial function, inflammation, lipids, and thrombosis (9, 10). Nicotine exposure could also induce a reduction in insulin release, and negatively affect insulin action, suggesting that nicotine could be a cause for the development of insulin resistance. Therefore, young stroke patients who smoked are more likely to have those comorbidities.
Initially, the term “smoker's paradox” was an observational phenomenon of an unexpected favorable outcome in smokers who experienced acute myocardial infarction and had a smoking duration of over 25 years (9). Recent studies in stroke indicate a strong positive correlation between recanalization and smokers, indicating that thrombolytic therapy acts more effectively in smokers (11, 12). However, they had some shortcomings, including short observation durations or their patients' low clinical risk profiles and low NIHSS scores on admission. In addition, those studies ignore that smoking is associated with a younger age of stroke. The risk of recurrent stroke after the first stroke is about 10% at 1 year, 25% at 5 years, and 40% at 10 years, and about 40% of stroke survivors become disabled after stroke (18). Recurrent strokes often have a higher rate of death and disability. In our present study, we only investigated young stroke patients, and the data suggest that smoking is associated with higher severity of the initial stroke, more modifiable risk factors, and poor functional outcome recorded at 3 months after stroke. Therefore, the smoker's paradox is misleading.
The difference in the incidence of stroke between the two sexes are well-established. Several epidemiological studies report higher age-specific stroke rates in men (19–21). However, women still experience more frequent stroke events because of their increased longevity and high stroke incidence at older ages. The higher prevalence of traditional vascular risk factors, including hypertension, diabetes mellitus, and hyperlipidemia in middle-aged men may contribute to this result (22, 23). Our findings are consistent with those of a meta-analysis and certain community-based reports on the relationship between stroke and sex. More interestingly, age-specific stroke rates are higher in men, and the higher prevalence of traditional vascular risk factors is associated with smoking.
Patients who cease smoking are expected to live longer and be less likely to develop tobacco-related diseases, including coronary heart disease, stroke, cancer, and pulmonary disease (24–27). In 1997, Taiwan established its first comprehensive policy package for tobacco control, the THPA, to include pictorial health warnings, smoke-free worksites and restaurants, and a ban on most tobacco advertising (24, 25). In 2018, Taiwan recorded an adult smoking rate of 13%—its lowest rate since 1990. This resulted from the efforts of the government to discourage smoking since the enactment of the THPA in 1997. Taiwan was the second Asian country after Bhutan to institute an indoor smoking ban. However, Taiwan's tobacco price still remains too low, and now, the Taiwan government only levies one package of 20 cigarettes at NT$10 (US$0.3). According to a World Bank study, a 10% rise in the cigarette price leads to a 4–8% reduction in cigarette consumption. Therefore, it is imperative to raise the price of tobacco.
The TSR provides the opportunity to investigate these issues owing to its large sample size, the homogeneous demographic characteristics and clinical phenotypes of the study subjects, and the standard diagnostic workup (16, 28, 29).
However, the present study has a number of limitations that need to be addressed. First, the baseline characteristics of the study groups were only obtained in the hospitals; hence, certain unadjusted potential confounders may still exist. Second, the sample sizes were sufficiently large, representing 3% of the total adult population in Taiwan. However, our cohort consisted of participants with an above-average socioeconomic status engaging in a medical screening program. This may affect the generalizability of our findings. Third, the smoking paradox refers to a better outcome following intravenous thrombolysis as well as endovascular therapy in smokers. However, TSR does not include data on patients who accepted endovascular therapy, leading to the possible underestimation of the reperfusion rate. Fourth, our body begins a series of positive changes that continue for years after quitting smoking. Being smoke-free not only adds years to your life, but also greatly improves your chances of a disease-free old age. Our data included patients who stopped smoking more than 2 years before stroke defined as past smokers, leading to the possible underestimation of the benefit of smoking cessation.
Conclusion
In conclusion, this study uncovers an intriguing relation between smoking and young stroke. High smoking rates are found among male young stroke patients, compared with much lower rates among females. Smoking is associated with higher comorbidities and poor long-term function outcomes. Smoking cessation would substantially reduce those effects. This implies that physicians should put more efforts into reducing cigarette smoking in Taiwan.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: The TSR raw data in this study are managed by the Management Office for Health Data (Dry Lab), China Medical University Hospital (http://stroke.cmuh.org.tw/). All researchers can submit their proposals to the research committee of the TSR (dGFpd2Fuc3Ryb2tlcmVnaXN0cnlAZ21haWwuY29t). After study proposals are accepted, the results will be sent back to investigators.
Ethics Statement
The studies involving human participants were reviewed and approved by the China Medical University Hospital Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
P-LC, W-LC, P-YY, C-YW, M-JT, YS, C-HL, J-TL, T-CL, L-ML, M-CL, C-LLin, and H-KW: designed research. C-LLia, H-JC, Y-CL, C-CW, C-HT, and H-KW: analyzed data. H-KW and CH wrote the paper. All authors contributed to the article and approved the submitted version.
Funding
This study was supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003-), Tseng-Lien Lin Foundation, Taichung, Taiwan.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.658582/full#supplementary-material
References
1. Synhaeve NE, Arntz RM, Maaijwee NA, Rutten-Jacobs LC, Schoonderwaldt HC, Dorresteijn LD, et al. Poor long-term functional outcome after stroke among adults aged 18 to 50 years: follow-up of transient ischemic attack and stroke patients and unelucidated risk factor evaluation (FUTURE) study. Stroke. (2014) 45:1157–60. doi: 10.1161/STROKEAHA.113.004411
2. Ekker MS, Verhoeven JI, Vaartjes I, Jolink WMT, Klijn CJM, de Leeuw FE. Association of stroke among adults aged 18 to 49 years with long-term mortality. JAMA. (2019) 321:2113–23. doi: 10.1001/jama.2019.6560
3. Crespo Pimentel B, Willeit J, Töll T, Kiechl S, Pinho E, Melo T, et al. Etiologic evaluation of ischemic stroke in young adults: a comparative study between two European centers. J Stroke Cerebrovasc Dis. (2019) 28:1261–6. doi: 10.1016/j.jstrokecerebrovasdis.2019.01.019
4. Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, Tuladhar AM, et al. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. (2018) 17:790–801. doi: 10.1016/S1474-4422(18)30233-3
5. Putaala J, Haapaniemi E, Metso AJ, Metso TM, Artto V, Kaste M, et al. Recurrent ischemic events in young adults after first-ever ischemic stroke. Ann Neurol. (2010) 68:661–71. doi: 10.1002/ana.22091
6. Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. (2010) 8:917–32. doi: 10.1586/erc.10.56
7. Chu NF, Lin FH, Wu YC. Prevalence and trends of cigarette smoking among. military personnel in Taiwan: results of 10-year anti-smoking health. Promotion programs in military. Mil Med. (2017) 182:e1933–7. doi: 10.7205/MILMED-D-16-00361
8. Kivioja R, Pietilä A, Martinez-Majander N, Gordin D, Havulinna AS, Salomaa V, et al. Risk factors for early-onset ischemic stroke: a case-control study. J Am Heart Assoc. (2018) 7:e009774. doi: 10.1161/JAHA.118.009774
9. Venkatason P, Salleh NM, Zubairi Y, Hafidz I, Ahmad WA, Han SK, et al. The bizzare phenomenon of smokers' paradox in the immediate outcome post acute myocardial infarction: an insight into the Malaysian National Cardiovascular Database-Acute Coronary Syndrome (NCVD-ACS) registry year 2006-2013. Springerplus. (2016) 5:534. doi: 10.1186/s40064-016-2188-3
10. Aune E, Røislien J, Mathisen M, Thelle DS, Otterstad JE. The “smoker's paradox” in patients with acute coronary syndrome: a systematic review. BMC Med. (2011) 9:97. doi: 10.1186/1741-7015-9-97
11. Dasenbrock HH, Rudy RF, Rosalind Lai PM, Smith TR, Frerichs KU, Gormley WB, et al. Cigarette smoking and outcomes after aneurysmal subarachnoid hemorrhage: a nationwide analysis. J Neurosurg. (2018) 129:446–57. doi: 10.3171/2016.10.JNS16748
12. Kufner A, Nolte CH, Galinovic I, Brunecker P, Kufner GM, Endres M, et al. Smoking-thrombolysis paradox: recanalization and reperfusion rates after intravenous tissue plasminogen activator in smokers with ischemic stroke. Stroke. (2013) 44:407–13. doi: 10.1161/STROKEAHA.112.662148
14. Wang IK, Liu CH, Yen TH, Jeng JS, Hsu SP, Chen CH, et al. Cholesterol levels are associated with 30-day mortality from ischemic stroke in dialysis patients. J Stroke Cerebrovasc Dis. (2017) 26:1349–56. doi: 10.1016/j.jstrokecerebrovasdis.2017.02.007
15. Wang IK, Liu CH, Yen TH, Jeng JS, Sung SF, Huang PH, et al. Renal function is associated with 1-month and 1-year mortality in patients with ischemic stroke. Atherosclerosis. (2018) 269:288–93. doi: 10.1016/j.atherosclerosis.2017.11.029
16. Wen CP, Liu CH, Jeng JS, Hsu SP, Chen CH, Lien LM, et al. Pre-stroke physical activity is associated with fewer post-stroke complications, lower mortality and a better long-term outcome. Eur J Neurol. (2017) 24:1525–31. doi: 10.1111/ene.13463
17. Lutski M, Zucker I, Shohat T, Tanne D. Characteristics and outcomes of young patients with first-ever ischemic stroke compared to older patients: the national acute stroke Israeli registry. Front Neurol. (2017) 8:421. doi: 10.3389/fneur.2017.00421
18. Hardie K, Hankey GJ, Jamrozik K, Broadhurst RJ, Anderson C. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study. Stroke. (2004) 35:731–5. doi: 10.1161/01.STR.0000116183.50167.D9
19. Hiraga A. Gender differences and stroke outcomes. Neuroepidemiology. (2017) 48:61–2. doi: 10.1016/S1474-4422(08)70193-5
20. Fraticelli L, Freyssenge J, Claustre C, Buisson M, Bischoff M, Nighoghossian N, et al. Sex-related differences in management and outcome of acute ischemic stroke in eligible patients to thrombolysis. Cerebrovasc Dis. (2019) 47:196–204. doi: 10.1159/000500901
21. Giroud M, Delpont B, Daubail B, Blanc C, Durier J, Giroud M, et al. Temporal trends in sex differences with regard to stroke incidence: the dijon stroke registry (1987-2012). Stroke. (2017) 48:846–9. doi: 10.1161/STROKEAHA.116.015913
22. Förster A, Gass A, Kern R, Wolf ME, Ottomeyer C, Zohsel K, et al. Gender differences in acute ischemic stroke: etiology, stroke patterns and response to thrombolysis. Stroke. (2009) 40:2428–32. doi: 10.1161/STROKEAHA.109.548750
23. Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: a systematic review. Stroke. (2009). 40:1082–90. doi: 10.1161/STROKEAHA.108.540781
24. Sanna M, Gao W, Chiu YW, Chiou HY, Chen YH, Wen CP, et al. Tobacco control within and beyond WHO MPOWER: outcomes from Taiwan SimSmoke. Tob Control. (2020) 29:36–42. doi: 10.1136/tobaccocontrol-2018-054544
25. Huang WH, Hsu HY, Chang BC, Chang FC. Factors correlated with success rate of outpatient smoking cessation services in Taiwan. Int J Environ Res Public Health. (2018) 15:1218. doi: 10.3390/ijerph15061218
26. Wen CP, Cheng TY, Lin CL, Wu HN, Levy DT, Chen LK, et al. The health benefits of smoking cessation for adult smokers and for pregnant women in Taiwan. Tob Control. (2005) 14(Suppl. 1):i56–61. doi: 10.1136/tc.2004.007997
27. Bak S, Sindrup SH, Alslev T, Kristensen O, Christensen K, Gaist D. Cessation of smoking after first-ever stroke: a follow-up study. Stroke. (2002) 33:2263–9. doi: 10.1161/01.str.0000027210.50936.d0
28. Tang SC, Yin JH, Liu CH, Sun MH, Lee JT, Sun Y, et al. Low pulse pressure after acute ischemic stroke is associated with unfavorable outcomes: the Taiwan stroke registry. J Am Heart Assoc. (2017). 6:e005113. doi: 10.1161/JAHA.116.005113
Keywords: stroke, smoking, Taiwan Stroke Registry, smoking cessation, proportional hazards regression analysis
Citation: Liang C-L, Chen H-J, Lee Y-C, Wu C-C, Tsai C-H, Chen P-L, Chang W-L, Yeh P-Y, Wei C-Y, Tsai M-J, Sun Y, Lin C-H, Lee J-T, Lai T-C, Lien L-M, Lin M-C, Lin C-L, Wang H-K, Hsu CY and the Taiwan Stroke Registry Investigators (2021) Smoking Status and Functional Outcomes in Young Stroke. Front. Neurol. 12:658582. doi: 10.3389/fneur.2021.658582
Received: 26 January 2021; Accepted: 27 July 2021;
Published: 01 September 2021.
Edited by:
Johannes Boltze, University of Warwick, United KingdomReviewed by:
Natasha A. Lannin, Monash University, AustraliaYilong Wang, Capital Medical University, China
Copyright © 2021 Liang, Chen, Lee, Wu, Tsai, Chen, Chang, Yeh, Wei, Tsai, Sun, Lin, Lee, Lai, Lien, Lin, Lin, Wang, Hsu and the Taiwan Stroke Registry Investigators. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao-Kuang Wang, ZWQxMDEzOTNAZ21haWwuY29t
†A complete list of the Taiwan Stroke Registry Investigators is provided in Appendix 1
 Cheng-Loong Liang
Cheng-Loong Liang Han-Jung Chen1,2
Han-Jung Chen1,2 Cheng-Chun Wu
Cheng-Chun Wu Po-Lin Chen
Po-Lin Chen Po-Yen Yeh
Po-Yen Yeh Cheng-Yu Wei
Cheng-Yu Wei Yu Sun
Yu Sun Jiunn-Tay Lee
Jiunn-Tay Lee Mei-Chen Lin
Mei-Chen Lin Cheng-Li Lin
Cheng-Li Lin Hao-Kuang Wang
Hao-Kuang Wang Chung Y. Hsu
Chung Y. Hsu