- 1Department of Diagnostic Imaging, Foothills Medical Center, University of Calgary, Calgary, AB, Canada
- 2Department of Clinical Neurosciences, Foothills Medical Center, University of Calgary, Calgary, AB, Canada
- 3Department of Medical Imaging, St. Anne's University Hospital Brno and Faculty of Medicine, Masaryk University, Brno, Czech Republic
- 4Department of Radiology, University Hospital of Basel, Basel, Switzerland
- 5Department of Diagnostic Imaging, University of Alberta Hospital, University of Alberta, Edmonton, AB, Canada
- 6Department of Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 7Department of Neurological Sciences, Rush University Medical Center, Chicago, IL, United States
- 8Department of Neurosurgery, Kobe City Medical Center General Hospital, Kobe, Japan
- 9Department of Neuroradiology, Toronto Western Hospital, Toronto, ON, Canada
- 10Department of Neuroradiology, Vancouver General Hospital, Toronto, ON, Canada
- 11Department of Radiology and Nuclear Medicine, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, Netherlands
Background: Endovascular treatment (EVT) for stroke due to medium vessel occlusion (MeVO) can be technically challenging. Devices and tools are rapidly evolving. We aimed to gain insight into preferences and global perspectives on the usage of endovascular tools in treating MeVOs.
Methods: We conducted an international survey with seven scenarios of patients presenting A3, M2/3, M3, M3/4, or P2/3 occlusions. Respondents were asked for their preferred first-line endovascular approach, and whether they felt that the appropriate endovascular tools were available to them. Answers were analyzed by occlusion location and geographical region of practice, using multinomial/binary logistic regression.
Results: A total of 263 neurointerventionists provided 1836 responses. The first-line preferences of physicians were evenly distributed among stent-retrievers, combined approaches, and aspiration only (33.2, 29.8, and 26.8%, respectively). A3 occlusions were more often treated with stent-retrievers (RR 1.21, 95% CI: 1.07–1.36), while intra-arterial thrombolysis was more often preferred in M3 (RR 2.47, 95% CI: 1.53–3.98) and M3/4 occlusions (RR 7.71, 95% CI: 4.16–14.28) compared to M2/3 occlusions. Respondents who thought appropriate tools are currently not available more often chose stent retrievers alone (RR 2.07; 95% CI: 1.01–4.24) or intra-arterial thrombolysis (RR 3.35, 95% CI: 1.26–8.42). Physicians who stated that they do not have access to optimal tools opted more often not to treat at all (RR 3.41, 95% CI: 1.11–10.49). Stent-retrievers alone were chosen more often and contact aspiration alone less often as a first-line approach in Europe (RR 2.12, 95% CI: 1.38–3.24; and RR 0.49, 95% CI 0.34–0.70, respectively) compared to the United States and Canada.
Conclusions: In EVT for MeVO strokes, neurointerventionalists choose a targeted vessel specific first-line approach depending on the occlusion location, region of practice, and availability of the appropriate tools.
Introduction
Given the high efficacy of endovascular treatment (EVT) for acute ischemic stroke due to large vessel occlusion (LVO) and recently recognized substantial morbidity associated with stroke due to medium vessel occlusions (MeVO; distal M2/3, A2/3, P2/3 vessel segments) (1), EVT is now increasingly considered as a treatment for MeVO stroke (2), despite the lack of high-level evidence for MeVO EVT (3, 4). The smaller caliber, more distal location, and longer and more tortuous course of the affected vessels of MeVO compared to LVO makes EVT for MeVO stroke more challenging. Thinner, more fragile arterial walls could increase the risk of dissection, perforation, and vasospasm—complications that could offset any benefit of EVT (3, 4).
Currently, EVT tools and techniques are rapidly evolving, resulting in improved efficacy and safety of MeVO EVT. Several authors report promising results of primary aspiration as a first-line approach in MeVO stroke (5–9). Mini stent-retrievers are designed specifically for more distal occlusion locations, and novel approaches like the blind exchange mini-pinning (10, 11) technique may lead to higher rates of first-pass recanalization and a lower incidence of symptomatic intracranial hemorrhage compared to the use of mini stent retrievers alone (10).
However, in light of these developments, and in the absence of guideline-based treatment recommendations, clinical practice with regard to EVT techniques for MeVO stroke may vary greatly between countries or individual physicians. Currently, there are little data on the variability in MeVO EVT approaches. Therefore, we sought to determine global patterns in preferences and utilization of EVT devices in MeVO stroke. In addition, we explored interventionalists' access to the appropriate EVT devices, and whether they thought that appropriate tools already exist and are available to them in their current practice.
Methods
We conducted an international, cross-sectional, anonymous, invitation-only survey: MeVO-FRONTIERS (MeVO-Finding Rationales and Objectifying New Targets for IntervEntional Revascularization in Stroke). Approximately 1,400 stroke physicians from 44 countries were invited to participate in this survey through Qualtrics (www.qualtrics.com). There were no restrictions for respondents based on country, years of experience, career stage, or hospital setting. The current study analyzes the survey questions on EVT technique and includes responses from interventionalists who identified themselves as neuroradiologists, neurosurgeons performing endovascular procedures, and interventional neurologists.
Response data were obtained from November 12, 2020 to December 31, 2020. Data are available from the corresponding author upon request. Approval by the local research ethics board of the University of Calgary was obtained (REB20-2086).
Survey Design
The survey consisted of seven narrative MeVO cases with illustrative images and three to six clinical case vignettes per scenario. The case vignettes included patient demographics, clinical symptoms, radiological images, and imaging-derived information like CT-perfusion volumes or early ischemic changes on non-contrast CT. At the end of each case, physicians were asked what their preferred first-line EVT approach for that particular case would be. Answer options were (a) stent-retriever alone, (b) aspiration alone, (c) combined stent-retriever and aspiration, (d) intra-arterial thrombolysis, or (e) no treatment. Participants were then asked whether they thought that optimal tools for treating MeVOs with EVT currently exist (Yes/No/There is substantial scope for improvement) and whether the appropriate material for MeVO EVT is available in their institution (full survey questions shown in Supplementary Methods). Prior to accessing the case scenarios, physicians provided basic personal data (age group, gender, subspecialty, years of experience in stroke treatment, annual center stroke treatment volume, and geographic region).
Statistical Analysis
Respondents' baseline characteristics were described using appropriate descriptive statistics. Univariable multinomial regression clustered by participant was used to assess the effect of occlusion site and respondent characteristics on preferred first-line EVT approach. Incidence rate ratios (IRRs) with 95% confidence intervals (CI) were reported.
For the following analysis, first-line approach was dichotomized into dummy variables (e.g., stent-retriever vs. others, aspiration vs. others, etc.). Then, preferred first-line EVT approach by occlusion site (M2/3, M3, M3/4, A3, P2/3) and region of practice (USA and Canada, Europe, rest of the world) were analyzed using binary logistic regression clustered by participant to calculate risk ratios (RRs) with 95% confidence intervals. M2/3 occlusion and responses from practitioners from the USA and Canada were chosen as reference values.
Multinomial regression analysis was used to determine treatment approach preference based on the existence and availability of specific endovascular tools and whether the interventionists thought they had adequate access to them in their current practice. In the multinomial regression model, the combined technique (stent retriever together with the contact aspiration) was chosen as the reference value and responses “Yes, tools exist” and “Yes, tools are available” were taken as base outcome.
The significance level was set at p < 0.05. Data analyses were performed in Stata 16.1 (StataCorp, College Station, TX, USA). Figures were created using the Microsoft PowerBI Platform.
Results
In total, 263 of 366 stroke physicians who participated were neurointerventionists and were included in the current study. Seven clinical scenarios (two M2/3 and two A3 cases; one M3, M3/4, and P2/3 case) resulted in 1,836 responses on treatment approaches for MeVOs. Detailed respondent characteristics are listed in Supplementary Table 1.
Overall, physicians opted for first-line stent-retrievers alone in 33.2% (610/1,836) of cases, a combined approach in 29.8% (547/1,836), aspiration only in 26.8% (492/1,836) cases, and intra-arterial thrombolysis in 6.5% (119/1,836) cases. In 2.9% (54/1,836) of cases, no treatment was preferred, and in 0.8% (14/1,836) of responses, another endovascular approach was preferred (e.g., combined aspiration and stent-retriever with additional intra-arterial thrombolysis, or guidewire/microcatheter manipulation only). There were no differences in the preferred first-line approach among physicians based on their age, gender, years of experience in neurointervention, career stage, or annual institutional EVT volumes (Supplementary Table 2).
First-Line Device Preference by Occlusion Site
First-line treatment approach for each occlusion site is shown in Figure 1 and Table 1. Preference for stent-retrievers alone did not differ between middle cerebral artery (MCA) occlusions (M2/3, M3, M3/4; Supplementary Table 2). In A3 occlusions, stent-retrievers were the most commonly preferred approach [39.4%, 207/525 responses; RR 1.22, 95% CI 1.08–1.37 (reference category: M2/3)]. For P2/3 occlusions, the combined approach (stent-retriever and aspiration) was frequently chosen (37% in P2/3). The combined technique was preferred less often in more distal MCA target occlusions (37.7% in M2/3 occlusions, 30.9% for M3, 15.3% for M3/4) with relative RRs indicating diminished use for very distal occlusions (Table 1). In more distal occlusions, respondents were also more likely to choose intra-arterial thrombolysis as a first-line approach (overall: RR 1.12; 95% CI 1.04–1.22) or to not treat with EVT at all (in M3/4: RR 8.30; 95% CI 3.54–19.48).
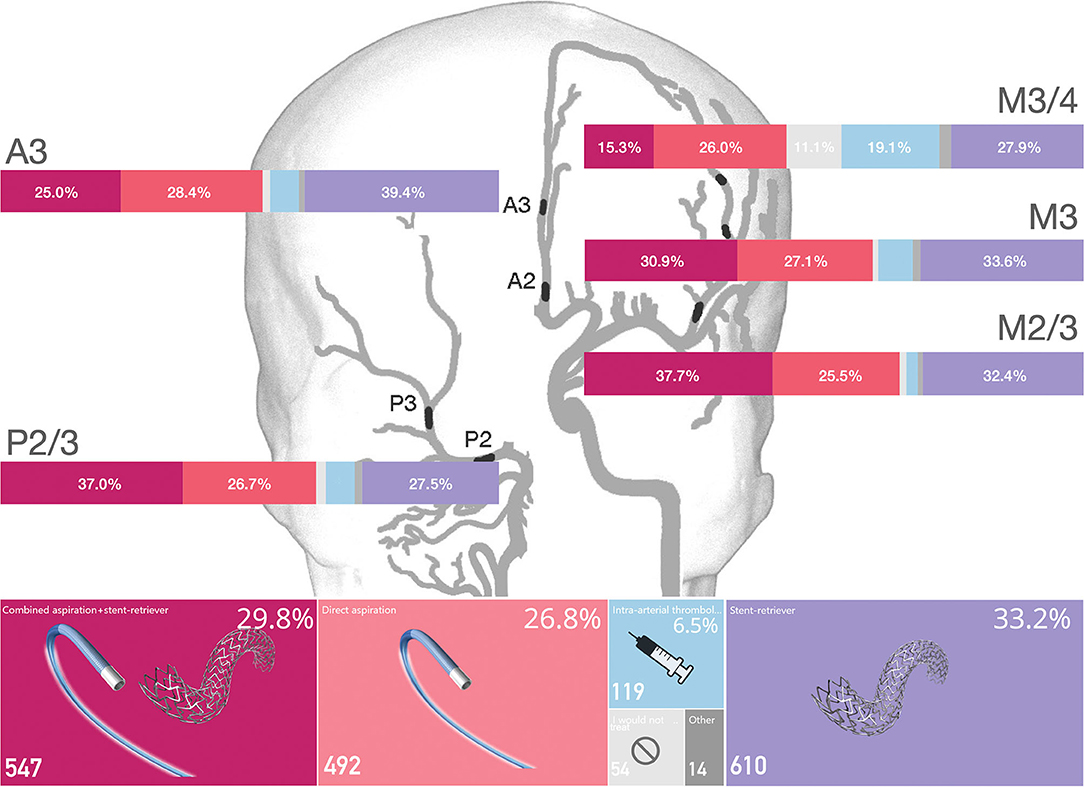
Figure 1. First-line treatment approach by MeVO occlusion site. Overall device usage and proportion of the respondents that chose each treatment approach in each specific vessel is shown in percentages.
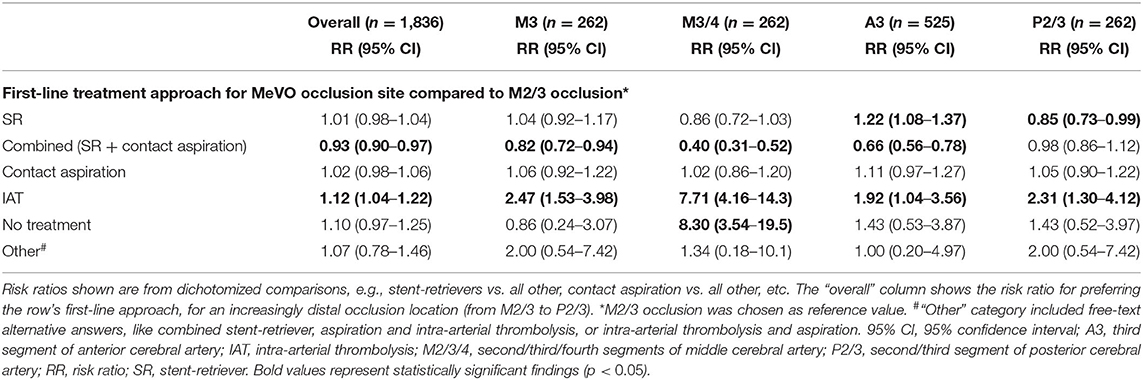
Table 1. Likelihood of preferred first-line approach (stent-retriever, combined stent-retriever and aspiration, aspiration, intra-arterial thrombolysis, or other) per occlusion site (reference: M2/3).
Geographic Variations in Endovascular Device Choice
Stent-retriever alone was the most frequently chosen first-line approach in Europe [37.3%, 340/912 responses, RR 2.09, 95% CI 1.38–3.18 (reference category: USA and Canada)] and the rest of the world (43.3%, 179/413 responses, RR 2.43, 95% CI 1.57–3.78).
In the USA and Canada, contact aspiration alone was the most frequently preferred first-line approach (43.3%, 221/511 responses); in contrast to that, it was significantly less often chosen by Europeans [RR 0.49, 95% CI 0.34–0.70 (reference category: USA and Canada)] and practitioners from the rest of the world (RR 0.44, 95% CI 0.27–0.71).
Combined aspiration and stent-retrievers were chosen by European practitioners in 35.3% of cases (322/911 responses), which was significantly a more frequent choice when compared to the USA and Canada respondents (RR 1.41, 95% CI 1.10–1.96). There was no difference in choice of combined aspiration and stent-retriever between interventionalists in the USA and Canada and the rest of the world (25.1%, 128/511 vs. 23.5%, 97/413, respectively). There was no significant difference in the preference of intra-arterial thrombolysis or other endovascular techniques based on the region of practice (Table 2).
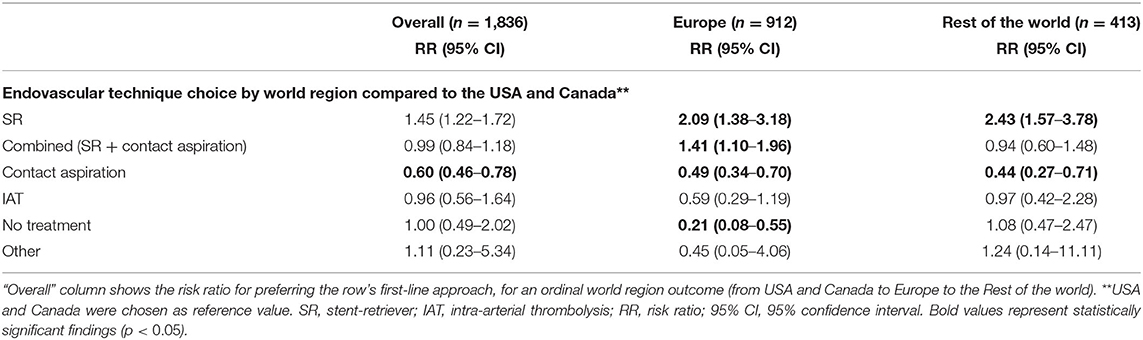
Table 2. Likelihood of preferred first-line endovascular treatment approach across world regions (reference: USA and Canada).
Influence of Availability and Access to Optimal MeVO EVT Tools
Overall, 162 (61.5%) participants felt that the current endovascular devices to treat MeVO stroke could be improved. Only 79 (30.0%) participants thought that the optimal tools already existed, and 22 (8.4%) thought that the appropriate tools currently do not exist. The interventionists who thought that the optimal tools to treat MeVO stroke do not exist were more likely to prefer stent-retrievers alone as a first-line approach [40.5%; RR 2.07, 95% CI 1.01–4.24 (ref category: tools exist)] and were more likely to treat MeVOs medically with IA tPA [12.43%; RR 3.25, 95% CI 1.71–6.12 (ref category: tools exist)].
Two-hundred-and-three (77.2%) neurointerventionists indicated that they had access to the best available tools, and 60 (22.8%) stated that they did not (always) have access to the ideal tools. Those without access to the optimal tools more frequently chose no EVT at all as a first-line approach [RR 3.41, 95% CI 1.11–10.49 (reference category: having the access to the best available tools)] (Table 3).
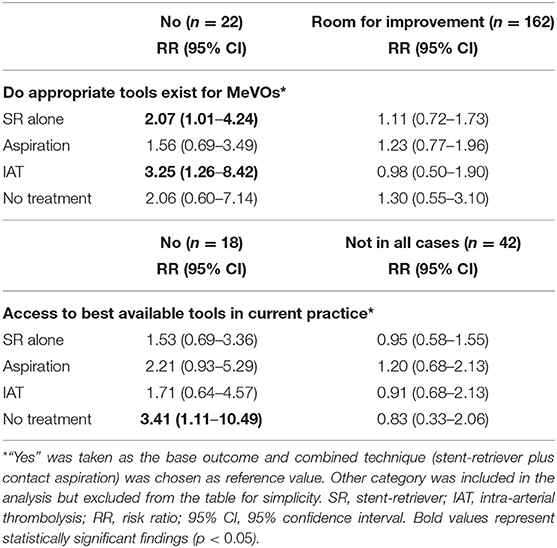
Table 3. Likelihood of preferred first-line approach (stent-retriever, combined stent-retriever and aspiration, aspiration, intra-arterial thrombolysis, or other) by physicians' opinion on whether the appropriate tools to treat MeVO exist, or whether they have access to the best available tools.
Discussion
This survey study found that the first-line device preferences of neurointerventionists for EVT in MeVO stroke vary based on the exact location of the occlusion, physician's region of practice, whether they think that adequate tools exist, and whether they have access to these tools in their current practice.
The optimal strategy for recanalizing MeVOs is currently not known, and the data on the efficacy of first-line aspiration vs. stent-retriever techniques are heterogenous and exclusively from non-randomized studies (12–15). Use of stent-retrievers, either alone (16–19) or combined with aspiration (10, 11), seems to be a widespread approach for MeVO EVT. Stent-retrievers alone or combined stent-retrievers and aspiration were the most commonly chosen first-line approaches, with the combined approach being preferred less often in more distal occlusions and stent-retriever alone more often in A3 occlusions.
EVT device choice in MeVO stroke is likely largely determined by the device's safety profile. Because the affected vessels in MeVO strokes are smaller, more distal, and more fragile, the risk of complications such as vasospasm, manipulation-related subarachnoid hemorrhage, and dissection is increased (3). These risks should be mitigated in order for EVT to result in a net benefit for the patients undergoing recanalization. Current large bore aspiration catheters may increase the risk of vascular damage, which is reflected in the decreased preference for first-line aspiration in more distal MCA occlusions in our study. Indeed, most intermediate catheters are 5–6Fr in diameter, and thus, they may be too large for MeVOs, considering the average diameter of the M2 middle cerebral artery segments is around 1.4–2.3 mm (20). Furthermore, when navigating the aspiration catheter to distal occlusion sites, there is the possibility of the device getting stuck at a vessel branch point, e.g., the middle cerebral artery bifurcation, although this risk can be mitigated by the use of wedge-shaped microcatheters (21), or coaxial microcatheters better size-matched to the aspiration catheter so as to reduce the step in transition. When using a primary combined approach on the other hand, limited lengths of currently available intermediate and microcatheters may render distal occlusions unreachable.
For stent-retrievers, the tortuosity and angle of the arteries may affect safety because of increased shearing at branch points during stent retrieval as well as and displacement of the arterial tree, both of which may result in subarachnoid hemorrhage. Use of stent-retrievers may hence be more desirable in straight arteries, such as the A3 where there is less tortuosity compared to the MCA branches (22).
Combined aspiration and stent-retrieval was shown to reduce the risk of distal embolization in large vessel occlusion stroke in some studies, with subsequent improved reperfusion quality and clinical outcomes (21). We found that a substantial number of physicians preferred this combined approach in the more proximal MeVO locations (M2/3 and P2/3). Recently proposed techniques such as blind exchange mini-pinning (11), in which the aspiration catheter is advanced introduced over the bare pusher wire once the stent-retriever is deployed, can circumvent problems related to catheter length and, at the same time, provide effective aspiration during the retrieval process. Techniques and specific tools for medium-sized arteries, such are mini stent-retrievers, are under development (17, 23); thus, it can be expected that more data on the safety and efficacy of these techniques will emerge soon.
Access to neurovascular tools and materials plays an important role in EVT decisions and first-line device choice for treating MeVOs as observed in this study. When practitioners thought that the appropriate tools do not exist, they more often chose to treat with stent-retrievers alone or opt for intra-arterial thrombolysis as a first-line approach. Those that felt they did not have access to the best available tools in their practice often chose not to treat at all.
Overall, interventionalists from Europe more often opted for stent-retrievers or combined stent-retrievers and aspiration as a first-line approach, whereas direct aspiration only was the more frequently preferred first-line approach in the USA and Canada. Availability of material and devices in different regions as well as local experience with these tools could potentially account for this variation in physicians' preferences as suggested in previous studies (24), in which the willingness to treat M2 occlusions increased under assumed ideal conditions in some regions. There is variability in the distribution and supply of stent retrievers across the world with some centers having access only to earlier generation devices, although device availability per country and center is hard to check and changing quickly. Physicians with no access to the optimal devices more often opted either to use stent-retrievers alone or not treat with EVT at all forgoing endovascular treatment that could potentially benefit the patient.
Limitations
Our study has several limitations. First, decisions in endovascular treatment are highly dependent on details of patient anatomy and factors such as patient motion during EVT. Radiologic images were presented with all case scenarios to make them as realistic as possible; however, details in these images or cases may limit the generalizability of our study results to real clinical practice. Secondly, the landscape of EVT materials and tools changes fast, hence the results represent a snapshot in time and availability would differ as the tools continue to evolve in each region. In addition, the survey did not ask for the specific device brands that were available at respondents' institutions. As such, we do not know the exact EVT materials on which our results reflect, other than the devices that are currently approved in general for EVT. Our intention was to provide a general overview of the field. Thirdly, our respondent sample was collected through personal and professional networks of the study authors, which may introduce selection bias in the results (e.g., overrepresentation of teaching hospitals). Models of financial compensation for MeVO EVT may also have differed between respondents' practice settings.
Conclusion
In this study, neurointerventionalists chose a targeted vessel-specific approach when treating MeVOs. Stent-retrievers alone or combined stent-retriever and aspiration were the most commonly used first-line approach, with the combined approach being preferred less often in more distal occlusions and stent-retriever alone more often in A3 occlusions as a first-line approach. Interventionalists from Europe used stent-retrievers and combined stent-retriever and aspiration more often as a first-line treatment, whereas direct aspiration only was more frequently preferred in North America. Physicians without access to the optimal devices more often used stent-retrievers alone or chose not to treat endovascularly at all, forgoing potential benefit.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The Conjoint Health Research Ethics Board of the University of Calgary reviewed and approved this study (REB20-2086). Written informed consent to participate in this study was provided by the participants. Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author Contributions
NK: study conception, data collection, graphical analysis, design of the work, interpretation of data, and manuscript drafting. PC, MG, and MK: study conception, data collection, design of the work, statistical analysis, interpretation of data, and manuscript drafting. JO: study conception, data collection, design of the work, interpretation of data, and manuscript editing. NSi: study conception, data collection, design of the work, statistical analysis, interpretation of data, and manuscript editing. MA: study conception, interpretation of data, and critical manuscript revision. JR: critical manuscript revision. JF and MC: study conception, data collection, design of the work, interpretation of data, and critical manuscript revision. NSa: study conception, data collection, and critical manuscript revision. RA: manuscript revisions. MH: manuscript drafting and critical manuscript revisions. All authors contributed to the article and approved the submitted version.
Conflict of Interest
NK is an informatics consultant for Circle Neurovascular. JF reports grants and personal fees from Stryker, Acandis, Microvention, Medtronic, personal fees from Codman, Ceronovus, Penumbra, Phenox, other (stock ownership) from Tegus, outside the submitted work; and Executive functions with University Medical Center Hamburg-Eppendorf, Eppdata GmbH. MC reports personal fees from Stryker, personal fees from Microvention, Medtronic, Genentech, Ceronovus, Penumbra, outside the submitted work. MG reports personal fees from Stryker, personal fees from Mentice, personal fees from Microvention, personal fees from Medtronic, outside the submitted work; in addition, MG has a patent for Systems of acute stroke diagnosis issued and licensed.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge all survey participants for their time and effort invested in answering the survey. We thank Moiz Hafeez for assisting in data preparation, conversion, and organization.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.735899/full#supplementary-material
References
1. Ospel JM, Menon BK, Demchuk AM, Almekhlafi MA, Kashani N, Mayank A, et al. Clinical course of acute ischemic stroke due to medium vessel occlusion with and without intravenous alteplase treatment. Stroke. (2020) 51:3232–40. doi: 10.1161/STROKEAHA.120.030227
2. McTaggart RA, Ospel JM, Psychogios MN, Puri AS, Maegerlein C, Lane KM, et al. Optimization of endovascular therapy in the neuroangiography suite to achieve fast and complete (expanded treatment in cerebral ischemia 2c-3) reperfusion. Stroke. (2020) 51:1961–8. doi: 10.1161/STROKEAHA.119.026736
3. Ospel JM, Goyal M. A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg. (2021) 13:623–30. doi: 10.1136/neurintsurg-2021-017321
4. Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. (2020) 51:2872–84. doi: 10.1161/STROKEAHA.120.028956
5. Romano DG, Frauenfelder G, Napoletano R, Botto A, Locatelli G, Panza MP, et al. ADAPT with new catalyst 5 reperfusion catheter for distal M2 ischemic stroke: preliminary experience. World Neurosurg. (2020) 135:e650–6. doi: 10.1016/j.wneu.2019.12.098
6. Altenbernd J, Kuhnt O, Hennigs S, Hilker R, Loehr C. Frontline ADAPT therapy to treat patients with symptomatic M2 and M3 occlusions in acute ischemic stroke: Initial experience with the Penumbra ACE and 3MAX reperfusion system. J Neurointerv Surg. (2018) 10:435–40. doi: 10.1136/neurintsurg-2017-013233
7. Navia P, Larrea J-A, Pardo E, Arce A, Martínez-Zabaleta M, Díez-González N, et al. Initial experience using the 3MAX cerebral reperfusion catheter in the endovascular treatment of acute ischemic stroke of distal arteries. J Neurointerv Surg. (2016) 8:787–90. doi: 10.1136/neurintsurg-2015-011798
8. Crockett MT, Phillips TJ, Chiu AHY. Dual suction Headway27 microcatheter thrombectomy for the treatment of distal intracranial arterial occlusion strokes: Initial experience with the micro-ADAPT technique. J Neurointerv Surg. (2019) 11:714–8. doi: 10.1136/neurintsurg-2018-014385
9. Vargas J, Spiotta AM, Fargen K, Turner RD, Chaudry I, Turk A. Experience with a direct aspiration first pass technique (ADAPT) for thrombectomy in distal cerebral artery occlusions causing acute ischemic stroke. World Neurosurg. (2017) 99:31–6. doi: 10.1016/j.wneu.2016.11.035
10. Pérez-Garciá C, Moreu M, Rosati S, Simal P, Egido JA, Gomez-Escalonilla C, et al. Mechanical thrombectomy in medium vessel occlusions: blind exchange with mini-pinning technique versus mini stent retriever alone. Stroke. (2020) 51:3224–31. doi: 10.1161/STROKEAHA.120.030815
11. Haussen DC, Al-Bayati AR, Eby B, Ravindran K, Rodrigues GM, Frankel MR, et al. Blind exchange with mini-pinning technique for distal occlusion thrombectomy. J Neurointerv Surg. (2020) 12:392–5. doi: 10.1136/neurintsurg-2019-015205
12. de Castro Afonso LH, Borghini Pazuello G, Seizem Nakiri G, Monsignore LM, Antunes Dias F, Pontes-Neto OM, et al. Thrombectomy for M2 occlusions and the role of the dominant branch. Interv Neuroradiol. (2019) 25:697–704. doi: 10.1177/1591019919847693
13. Grossberg JA, Rebello LC, Haussen DC, Bouslama M, Bowen M, Barreira CM, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke. (2018) 49:1662–8. doi: 10.1161/STROKEAHA.118.020567
14. Phan K, Maingard J, Kok HK, Dmytriw AA, Goyal S, Chandra R, et al. Contact aspiration versus stent-retriever thrombectomy for distal middle cerebral artery occlusions in acute ischemic stroke: meta-analysis. Neurointervention. (2018) 13:100–9. doi: 10.5469/neuroint.2018.00997
15. Atchaneeyasakul K, Malik AM, Yavagal DR, Haussen DC, Jadhav AP, Bouslama M, et al. Thrombectomy outcomes in acute ischemic stroke due to middle cerebral artery M2 occlusion with stent retriever versus aspiration: a multicenter experience. Interv Neurol. (2020) 8:180–6. doi: 10.1159/000500198
16. Pfaff J, Herweh C, Pham M, Schieber S, Ringleb PA, Bendszus M, et al. Mechanical thrombectomy of distal occlusions in the anterior cerebral artery: recanalization rates, periprocedural complications, and clinical outcome. Am J Neuroradiol. (2016) 37:673–8. doi: 10.3174/ajnr.A4594
17. Rikhtegar R, Mosimann PJ, Weber R, Wallocha M, Yamac E, Mirza-Aghazadeh-Attari M, et al. Effectiveness of very low profile thrombectomy device in primary distal medium vessel occlusion, as rescue therapy after incomplete proximal recanalization or following iatrogenic thromboembolic events. J Neurointerv Surg. (2021) 1–6. doi: 10.1136/neurintsurg-2020-017035
18. Bhogal P, Bücke P, Aguilar Pérez M, Ganslandt O, Bäzner H, Henkes H. Mechanical thrombectomy for M2 occlusions: a single-centre experience. Interv Neurol. (2017) 6:117–25. doi: 10.1159/000458161
19. Menon BK, Hill MD, Davalos A, Roos YBWEM, Campbell BCV, Dippel DWJ, et al. Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: meta-analysis of data from the HERMES Collaboration. J Neurointerv Surg. (2019) 11:1065–9. doi: 10.1136/heartjnl-2014-307109.258
20. Umansky F, Juarez SM, Dujovny M, Ausman JI, Diaz FG, Gomes F, et al. Microsurgical anatomy of the proximal segments of the middle cerebral artery. J Neurosurg. (1984) 61:458–67. doi: 10.3171/jns.1984.61.3.0458
21. Ospel JM, Volny O, Jayaraman M, McTaggart R, Goyal M. Optimizing fast first pass complete reperfusion in acute ischemic stroke—the BADDASS approach (BAlloon guiDe with large bore Distal Access catheter with dual aspiration with Stent-retriever as Standard approach). Expert Rev Med Devices. (2019) 16:955–63. doi: 10.1080/17434440.2019.1684263
22. Perlmutter D, Rhoton AL. Microsurgical anatomy of the distal anterior cerebral artery. J Neurosurg. (1978) 49:204–28. doi: 10.3171/jns.1978.49.2.0204
23. Hofmeister J, Kulcsar Z, Bernava G, Pellaton A, Yilmaz H, Erceg G, et al. The Catch Mini stent retriever for mechanical thrombectomy in distal intracranial occlusions. J Neuroradiol. (2018) 45:305–9. doi: 10.1016/j.neurad.2018.01.051
Keywords: acute ischemic stroke, endovascular thrombectomy, aspiration thrombectomy, medium vessel occlusions, endovascular treatment (EVT), MeVO, stroke, neurointervention
Citation: Kashani N, Cimflova P, Ospel JM, Singh N, Almekhlafi MA, Rempel J, Fiehler J, Chen M, Sakai N, Agid R, Heran M, Kappelhof M and Goyal M (2021) Endovascular Device Choice and Tools for Recanalization of Medium Vessel Occlusions: Insights From the MeVO FRONTIERS International Survey. Front. Neurol. 12:735899. doi: 10.3389/fneur.2021.735899
Received: 03 July 2021; Accepted: 11 August 2021;
Published: 15 September 2021.
Edited by:
Nishant K. Mishra, Yale University, United StatesReviewed by:
Mahesh Jayaraman, Brown University, United StatesNaoki Kaneko, University of California, Los Angeles, United States
Copyright © 2021 Kashani, Cimflova, Ospel, Singh, Almekhlafi, Rempel, Fiehler, Chen, Sakai, Agid, Heran, Kappelhof and Goyal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mayank Goyal, bWdveWFsMjQxMkBnbWFpbC5jb20=
 Nima Kashani
Nima Kashani Petra Cimflova
Petra Cimflova Johanna M. Ospel
Johanna M. Ospel Nishita Singh
Nishita Singh Mohammed A. Almekhlafi2
Mohammed A. Almekhlafi2 Jens Fiehler
Jens Fiehler Michael Chen
Michael Chen Nobuyuki Sakai
Nobuyuki Sakai Manraj Heran
Manraj Heran Manon Kappelhof
Manon Kappelhof