- 1Department of Pain, The Third Xiangya Hospital and Institute of Pain Medicine, Central South University, Changsha, China
- 2Department of Anesthesiology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
- 3Hunan Key Laboratory of Brain Homeostasis, Central South University, Changsha, China
Background: Myofascial pain syndrome (MPS) is one of the most common causes of chronic skeletal muscle pain, which is closely related to skeletal muscle myofascial trigger point (MTRP). Since there is no first-line treatment for MPS, we investigated Loxoprofen Sodium Cataplasm combined with physiotherapy as a non-invasive therapy in patients at different levels to a protocol with superior efficacy that is safe and easy to promote. Moreover, this treatment could represent an alternative therapeutic strategy for low-income patients to a safer, more convenient, and more economical treatment scheme.
Methods: A randomized clinical study was aimed at evaluating the safety and efficacy of Loxoprofen Sodium Cataplasm combined with physiotherapy in patients diagnosed with MPS in the pain clinic. We screened 100 patients with MPS, and using a computer-generated random allocation sequence, we stratified patients in a ratio of 2:1:1:1 (A: B: C: D) to one of the four treatment groups. Group A received Loxoprofen Sodium Cataplasm combined with extracorporeal shock wave therapy (ESWT) and transcutaneous electrical nerve stimulation (TENS). Group B received Loxoprofen Sodium Cataplasm alone. Group C received physiotherapy alone. Group D received Flurbiprofen Cataplasm combined with physiotherapy. After 2 weeks of treatment, the overall efficiency and secondary assessment indicators, including visual analog scale (VAS) scores, chronic soft tissue injury (CSTI) scores, Oswestry Disability Index (ODI) scores, or Northwick Park Neck Pain Questionnaire (NPQ) scores, were evaluated before and after treatment to analyze the difference in efficacy of each group.
Results: All groups were well tolerated with no reported adverse events. Significant treatment differences in the change from baseline in overall efficiency (primary efficacy endpoint) (P = 0.0078) were observed in subjects of groups A and C.
Conclusion: Showing valuable data of efficacy in primary and secondary endpoints, Loxoprofen Sodium Cataplasm combined with physiotherapy is superior in the treatment of MPS.
Trial registration number: https://www.chictr.org.cn/ (ChiCTR2100054756).
Introduction
Myofascial pain syndrome (MPS) is one of the most common causes of chronic musculoskeletal pain. The main symptoms are asymmetric pain at the trigger point, local or systemic, and even some patients have symptoms of autonomic dysfunction, including flushing, lacrimation, dermatographia, diaphoresis, goose rash, and dizziness (1, 2). There are numerous treatment options available for MPS, mainly including oral non-steroidal anti-inflammatory drugs (NSAIDs), opioids, benzodiazepine sedatives, muscle relaxants, tricyclic antidepressants, topical drugs, moderate aerobic exercise, trigger point injections, transcutaneous electrical nerve stimulation (TENS), extracorporeal shock wave (ESWT), acupuncture, dry needling, botulinum toxin injection, Kinesio taping, and hot compress, but no treatment with significant clinical advantages has been summarized (2–6). In the treatment of MPS, first-line NSAIDs are widely used clinically and play an important role in the treatment of MPS (7). NSAIDs have definite therapeutic effects on pain mainly by inhibiting cyclooxygenase, reducing the synthesis of prostaglandins, reducing the stimulation of afferent nerve endings, and preventing the release of pain-causing substances (8). However, long-term use of NSAIDs and oral preparations may cause adverse reactions in the gastrointestinal tract and even the whole body. In severe cases, life-threatening side effects such as gastrointestinal bleeding and abnormal cardiac function may occur. In addition, some invasive treatment methods, such as dry needling and local injection have definite curative effects, are expensive, and may have adverse reactions such as bleeding and infection (9–16). In addition, limited by regional differences in medical level, invasive treatment is not conducive to widespread promotion.
Myofascial pain syndrome has a huge patient population, with a prevalence of up to 55–90% in pain clinics, and is prone to recurrence after treatment (2, 17, 18), causing a huge burden on society and individuals. Therefore, the unified use of a non-invasive, safe, effective, inexpensive, and popularized outpatient treatment plan is crucial.
Currently, topical analgesics such as Loxoprofen Sodium Cataplasm, Flurbiprofen Cataplasm, and Compound Methyl Salicylate Cataplasm are often used in the treatment of MPS in pain clinics. Physical therapy such as ESWT/TENS is also used. There is also a combination of the two treatment options, but there is no clear and more effective treatment.
Therefore, this study used the visual analog scale (VAS) scores, Oswestry Disability Index (ODI) scores, and NPQ scores as evaluation indicators to explore the efficacy and safety of different regimens in the treatment of MPS and to provide a safer, more effective, more convenient, and less expensive treatment plan for the treatment of MPS.
Subjects and methods
Research design
From 1 August 2021, to 31 December 2021, outpatients in the Pain Department of the Third Xiangya Hospital of Central South University aged 18–75 years were screened and diagnosed with MPS according to diagnostic criteria (7, 19). After excluding patients with pregnancy, fractures, liver and kidney insufficiency, immune diseases, using NSAIDs, opioids, glucocorticoids, receiving physical therapy within 1 month, and allergic to NSAIDs, patients included in the study were classified into 4 groups by random number table method. This study was reviewed and approved by the Clinical Trial Ethics Committee of the Third Xiangya Hospital of Central South University (No. 21136), and all patients signed informed consent. This trial was registered on www.chictr.org.cn/ with the following number: ChiCTR2100054756.
Group A received Loxoprofen Sodium Cataplasm combined with physiotherapy, and 40 patients were planned to be included. Physiotherapy used extracorporeal shock wave therapy (ESWT) and TENS. Group B received Loxoprofen Sodium Cataplasm alone, and 20 patients were planned to be included. Group C received physiotherapy alone, and 20 patients were planned to be included. Group D received Flurbiprofen Cataplasm combined with physiotherapy, and 20 patients were planned to be included.
In groups A, B, and D, the method of external drug use is 1 cataplasm once per day, stick to the painful area; each application exists 12 h to 24 h; and the course of treatment is 2 weeks. In groups A, C, and D, physiotherapy consisted of ESWT and TENS, once a week, with a total of two times, i.e., on the day of enrollment and 1 week after enrollment, and no topical drug was used on the day of treatment. The frequency of physiotherapy was once a week, the same as described by Kiraly et al. (20).The parameters of ESWT were 1,000 impulses, 1.5 bar, 10 Hz, energy density of 0.25 mJ/mm2, and 15 mm treating head diameter to the trigger point and its vicinities. The parameters of TENS were 100 Hz, pulse duration (width) of 250 μs, and treatment for 15 min. Patients in groups A, C, and D were treated with the same model, operated by the same physician, in the Pain Department of the Third Xiangya Hospital of Central South University. In addition, health education was provided to each enrolled patient, including moderate exercise, attention to the intensity of work, and correction of poor posture.
Assessment and follow-up
Main evaluation indicators are total effective rate: the VAS-weighted value was used to determine the curative effect, i.e., VAS-weighted value = (VAS scores before treatment-VAS scores after treatment)/VAS scores before treatment × 100%; recover: VAS weighted 75–100%; evident: VAS weighted 50–75%; effective: VAS weighted 25–50%; effectless: VAS weighted <25%.
Secondary evaluation indicators are (1) VAS scores, (2) chronic soft tissue injury (CSTI) scores, and (3) ODI scores or NPQ scores. The VAS scores range from 0 to 10, and are based on self-reporting with the VAS; lower scores indicate less pain. The CSTI score covers the degree of pain, the size of palpation of the taut band and/or nodule, and the functional status; lower scores indicate less pain, smaller taut band or nodule, and better functional status. The ODI assesses the change in the functional status of adults with low back pain. The ODI contains ten pain-related questions scored from zero (no pain) to five (most severe pain). Scores are expressed as a percentage of total points; lower scores indicate better functional status (21). The Northwick Park Neck Pain Questionnaire (NPQ), which measures the level of neck pain and the resulting disability, is a nine-item questionnaire with five possible responses for each question; lower scores indicate less neck pain and better functional status (22). All the above indicators were evaluated before treatment and on the 15th day after treatment.
Statistical methods
Differences in overall efficiency were compared using χ2 tests (e.g., possible χ2-corrected tests and Fisher's exact test), and non-parametric tests (Mann–Whitney U test) were used to compare differences in clinical symptom improvement rates and patient compliance between groups. Analyses were performed using IBM SPSS Statistics 24 (version 24.0.0.0) at a significance level of P < 0.05.
Results
Patient grouping flowchart and general semographics
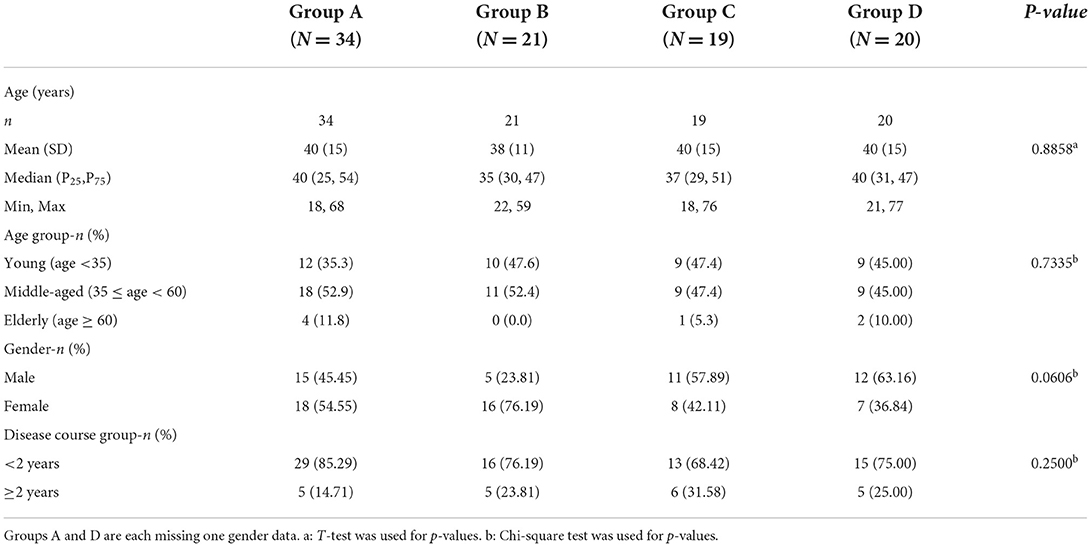
We included a total of 94 patients, including 34 in group A, 21 in group B, 19 in group C, and 20 in group D; the flowchart of patient grouping is shown in Supplementary Figure 1. The general demographics are shown in Table 1. The results showed that there was no significant difference in the age, course of the disease, and gender distribution of the patients in each group.
Intergroup comparison of overall efficiency in each group
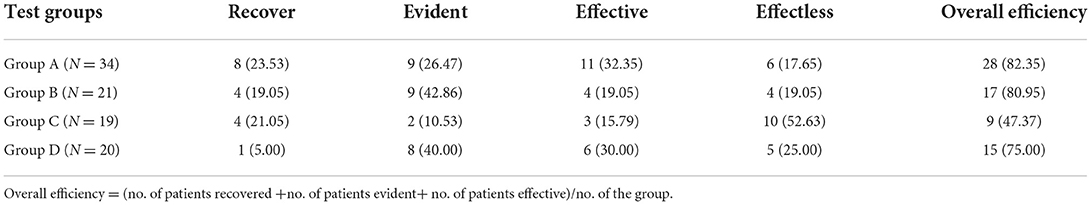
As shown in Table 2, the results show that each treatment method has a certain effect on patients with MPS. There was no significant difference in overall efficiency between group A vs. group B and group A vs. group D (P > 0.999, P = 0.7657), which was not statistically significant. There were significant differences between group A vs. group C, and group B vs. group C (P = 0.0078, P = 0.0262), with statistical significance. It is suggested that the combination of Loxoprofen Sodium Cataplasm and physiotherapy or Loxoprofen Sodium Cataplasm alone is better than physiotherapy alone.
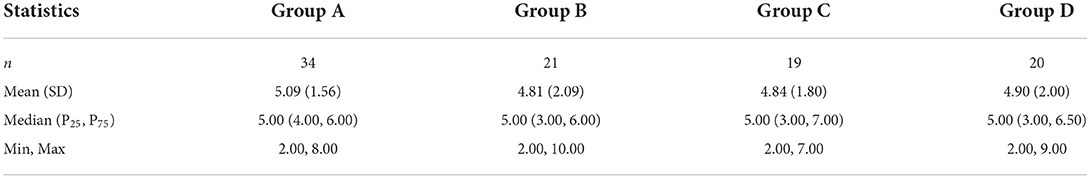
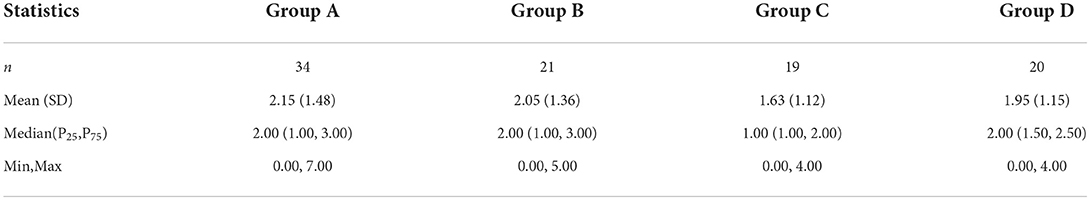
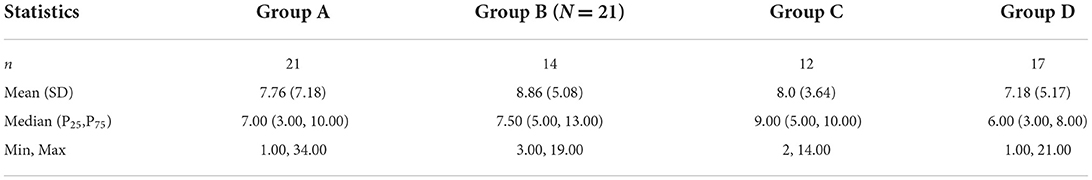
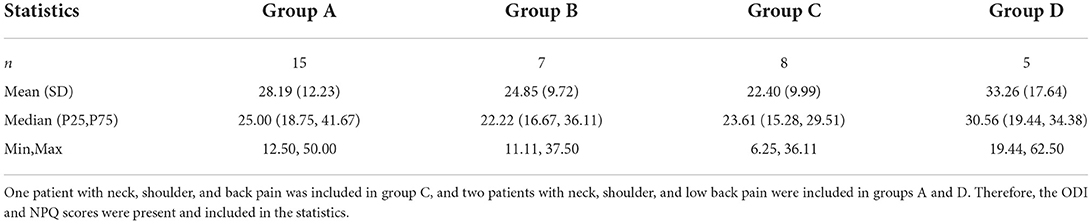
Comparison of results of secondary indicators before treatment between groups
As shown in Tables 3–6, there were no statistical differences in the VAS scores, CSTI scores, ODI scores, and NPQ scores between the groups before treatment (P > 0.05).
Intragroup comparison results of secondary indicators before and after treatment in each group
As shown in Supplementary Figures 2–5, the results showed that all four evaluation indicators in group A and group B were significantly improved, only VAS scores in group C were significantly improved, and three evaluation indicators in group D were significantly improved.
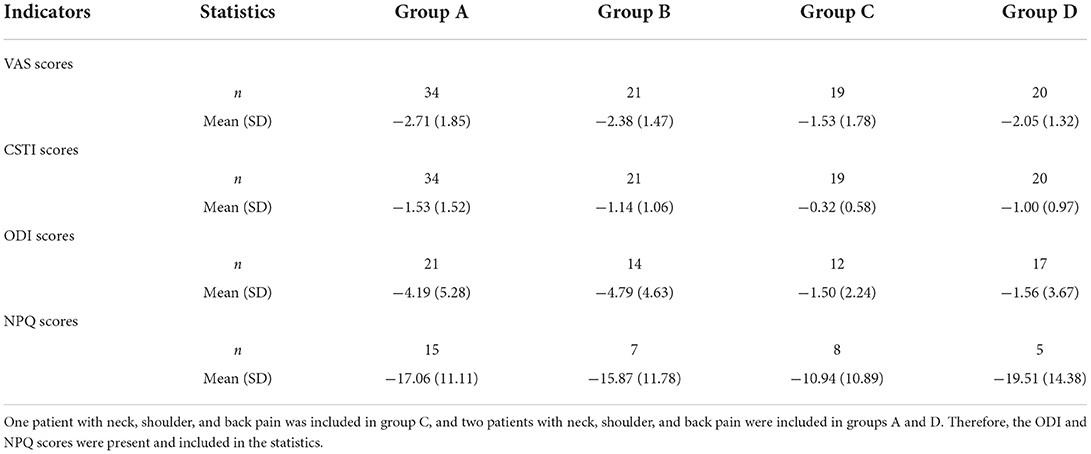
Intergroup comparison of changes in secondary indicators after treatment in each group from baseline
The results show that, as shown in Table 7, after 2 weeks of treatment, all secondary indicators in each group decreased to a certain extent compared with the baseline, and there was no statistical difference between groups A, B, and D (P > 0.05). All groups have an obvious curative effect. As shown in Supplementary Figures 6, 7, there were significant differences in VAS scores and CSTI scores before and after treatment in group A vs. group C (P = 0.0145, P = 0.0005); there were significant differences in CSTI scores in group B vs. group C before and after treatment (P = 0.0280).
Intragroup comparison of secondary indicators before and after treatment in patients with different pain sites in groups A and B
As shown in Table 8, patients with back pain had significant improvements in all indicators in both groups. However, for patients with neck and shoulder pain, group A improved more evaluation indicators, as shown in Table 9.
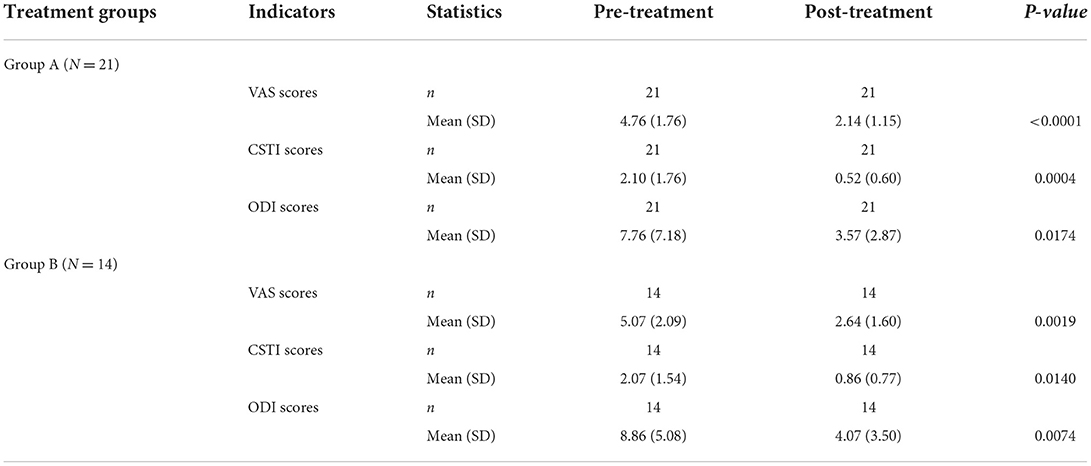
Table 8. Intragroup comparison of secondary indicators before and after treatment in patients with back pain.
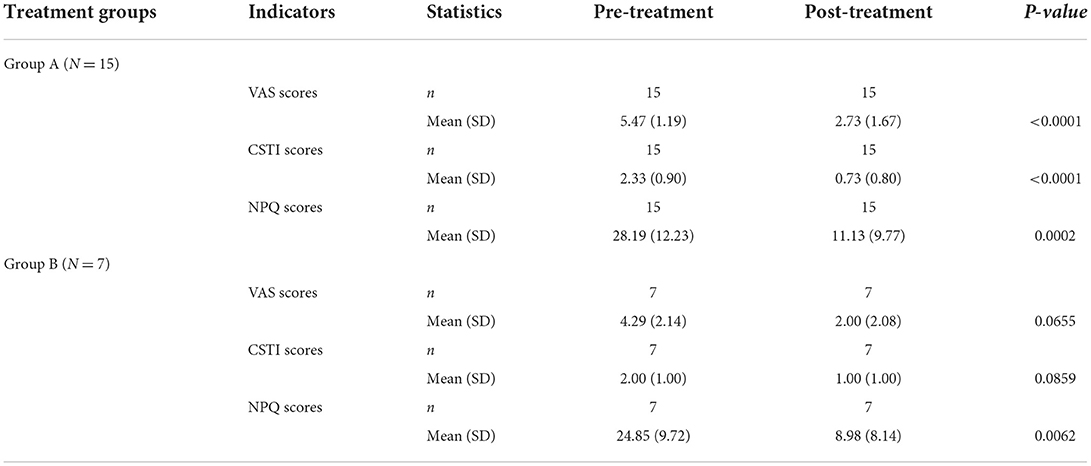
Table 9. Intragroup comparison of secondary indicators before and after treatment in patients with neck and shoulder pain.
Discussion
There are various treatment options for MPS, but there is still no optimal one (2). To summarize a simple, convenient, and popularized regimen, this study explored the safety and efficacy of different non-invasive treatment regimens for MPS. We found that Loxoprofen Sodium Cataplasm combined with ESWT and TENS therapy can help relieve pain in patients with MPS, relieve CSTI, and facilitate the recovery of patients' daily life functions. At the same time, this program has certain advantages over other control groups. NSAIDs topical patch is an alternative to oral medications, which has a local effect on the painful area and reduces the systemic impact (23). Even if adverse reactions such as allergic reactions occur, the allergen can be removed immediately by removing the cataplasm. ESWT and TENS are widely used in clinical practice because of their non-invasiveness, convenient operation, and short treatment time. The treatment of Loxoprofen Sodium Cataplasm combined with ESWT and TENS can be used safely even in areas with underdeveloped sanitary conditions, reducing the number of patients visiting the hospital, improving patient compliance with treatment, and facilitating widespread promotion.
We found that after 2 weeks of treatment, the different non-invasive treatment regimens were effective in terms of overall efficiency and evaluation of secondary indicators. There was no difference in the overall efficiency between group A, group B, and group D. Group C, the physiotherapy group, has a lower overall efficiency, which suggested that physiotherapy was not suitable for the clinical treatment of MPS alone. In addition, we found that there was no significant difference in the overall efficiency between group A and group B, indicating that after the external application of Loxoprofen Sodium Cataplasm, even combined ESWT and TENS would not significantly improve the overall efficiency of the treatment. This may suggest that the pain of MPS can be effectively relieved after the Loxoprofen Sodium Cataplasm is applied alone. Whether the Flurbiprofen Cataplasm alone can achieve the same effect remains to be further studied.
When analyzing secondary indicators for intragroup comparison, we found consistent and significant improvements in VAS scores, CSTI scores, ODI scores, and NPQ scores after loxoprofen, with or without physical therapy. With physiotherapy alone, only one secondary indicator, VAS scores, was improved, which did not relieve soft tissue injury and limitations in daily life. In addition, the Flurbiprofen Cataplasm combined with the physiotherapy group showed effectiveness in pain, CSTI, and neck and shoulder pain, but the improvement of ODI scores was not significant, suggesting that this regimen is not suitable for patients with back pain. In addition, when comparing between groups, we found that Loxoprofen Sodium Cataplasm combined with physiotherapy significantly improved CSTI and VAS scores compared with physical therapy alone, and Loxoprofen Sodium Cataplasm alone was associated with significant improvements in CSTI scores, which shows that Loxoprofen Sodium Cataplasm has a significant therapeutic effect on MPS, and a single application can significantly improve the quality of daily life of patients, which is helpful for patients' work and life.
To further analyze the efficacy of Loxoprofen Sodium Cataplasm alone and Loxoprofen Sodium Cataplasm combined with physiotherapy on MPS patients with different pain sites, we conducted intragroup comparisons of secondary evaluation indicators for patients with different pain sites in the two regimens. We found that compared with before treatment, Loxoprofen Sodium Cataplasm improved the secondary evaluation indicators in patients with back pain with or without combined physiotherapy. The possible reason is that the efficacy of ESWT and TENS physical therapy is dose-dependent (24, 25), and higher treatment intensity corresponds to more obvious efficacy. In patients with back pain, due to the deep location of myofascial trigger points (26), when we use the same ESWT and TENS treatment parameters as those of the neck and shoulders to treat back pain, the degree of tissue stimulation is relatively weak, so we get this result. However, in patients with neck and shoulder pain, Loxoprofen Sodium Cataplasm combined with physiotherapy had more significant improvements in secondary evaluation indicators.
This study has several limitations. First of all, although outpatients have been guided by doctors on daily-related precautions and exercise methods after patients leave the outpatient clinic, their exercise and rehabilitation cannot be objectively evaluated. We did not perform a systematic neurological examination of the patients, such as EMG or MRC scales. Especially in patients with MPS in the neck and shoulders, when the pain occurs, the activities of the neck and shoulders are limited. After ESWT and TENS treatment, the immediate improvement effect is obvious (27). The increase in joint activity also has a positive effect on relieving musculoskeletal pain (28, 29), which has a certain impact on the evaluation of the results of the study. Second, this study did not conduct relevant research on the long-term efficacy of patients. Finally, the sample size is small. It will be necessary to increase the sample size and long-term follow-up in the future.
Conclusion
Loxoprofen Sodium Cataplasm combined with physiotherapy can help relieve pain in patients with MPS, improve CSTI, and facilitate the recovery of patients' daily life functions. The treatment regimen in the control group has certain advantages.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the Clinical Trial Ethics Committee of the Third Xiangya Hospital of Central South University (No. 21136). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZW conceived and designed the experiments. XZ and XL wrote the paper. ZW and XL interpreted and analyzed the data. ZW, XZ, and XL performed the experiments and acquired the data. XL performed the statistical analysis. ZW and DH had full access to all the data in the study and had final responsibility for the decision to submit it for publication. All authors stated were involved in the critical revision of the manuscript and approved the final version of the article, including the authorship list.
Funding
This study was supported by Hunan Jiudian Pharmaceutical Co., Ltd. which made the Loxoprofen Sodium Cataplasm available to the investigators. Funders of the study had no role in study design, data analysis, data interpretation, or writing of the report.
Acknowledgments
We would like to thank the patients and their families for their participation in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.998327/full#supplementary-material
References
1. Money S. Pathophysiology of trigger points in myofascial pain syndrome. J Pain Palliat Care Pharmacother. (2017) 31:158–9. doi: 10.1080/15360288.2017.1298688
2. Borg-Stein J, Iaccarino MA. Myofascial pain syndrome treatments. Phys Med Rehabil Clin N Am. (2014) 25:357–74. doi: 10.1016/j.pmr.2014.01.012
3. Zhang Q, Fu C, Huang L, Xiong F, Peng L, Liang Z, et al. Efficacy of extracorporeal shockwave therapy on pain and function in myofascial pain syndrome of the trapezius: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2020) 101:1437–46. doi: 10.1016/j.apmr.2020.02.013
4. Zhang XF, Liu L, Wang BB, Liu X, Li P. Evidence for kinesio taping in management of myofascial pain syndrome: a systematic review and meta-analysis. Clin Rehabil. (2019) 33:865–74. doi: 10.1177/0269215519826267
5. Moraska AF, Schmiege SJ, Mann JD, Butryn N, Krutsch JP. Responsiveness of myofascial trigger points to single and multiple trigger point release massages: a randomized, placebo controlled trial. Am J Phys Med Rehabil. (2017) 96:639–45. doi: 10.1097/PHM.0000000000000728
6. Boonruab J, Nimpitakpong N, Damjuti W. The distinction of hot herbal compress, hot compress, and topical diclofenac as myofascial pain syndrome treatment. J Evid Based Integr Med. (2018) 23:2156587217753451. doi: 10.1177/2156587217753451
7. Cao QW, Peng BG, Wang L, Huang YQ, Jia DL, Jiang H, et al. Expert consensus on the diagnosis and treatment of myofascial pain syndrome. World J Clin Cases. (2021) 9:2077–89. doi: 10.12998/wjcc.v9.i9.2077
8. Shimodaira T, Mikoshiba S, Taguchi T. Nonsteroidal anti-inflammatory drugs and acetaminophen ameliorate muscular mechanical hyperalgesia developed after lengthening contractions via cyclooxygenase-2 independent mechanisms in rats. PLoS ONE. (2019) 14:e0224809. doi: 10.1371/journal.pone.0224809
9. Kocak AO, Ahiskalioglu A, Sengun E, Gur STA, Akbas I. Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: A prospective randomized study. Am J Emerg Med. (2019) 37:1927–31. doi: 10.1016/j.ajem.2019.01.015
10. Martín-Pintado-Zugasti A, Mayoral Del Moral O, Gerwin RD, Fernández-Carnero J. Post-needling soreness after myofascial trigger point dry needling: Current status and future research. J Bodyw Mov Ther. (2018) 22:941–6. doi: 10.1016/j.jbmt.2018.01.003
11. Park SC, Kim KH. Effect of adding cervical facet joint injections in a multimodal treatment program for long-standing cervical myofascial pain syndrome with referral pain patterns of cervical facet joint syndrome. J Anesth. (2012) 26:738–45. doi: 10.1007/s00540-012-1404-8
12. Dommerholt J. How have the views on myofascial pain and its treatment evolved in the past 20 years? From spray and stretch and injections to pain science, dry needling and fascial treatments. Pain Manag. (2020) 10:63–6. doi: 10.2217/pmt-2019-0055
13. Roldan CJ, Osuagwu U, Cardenas-Turanzas M, Huh BK. Normal saline trigger point injections vs conventional active drug mix for myofascial pain syndromes. Am J Emerg Med. (2020) 38:311–6. doi: 10.1016/j.ajem.2019.158410
14. Lee CY, Kim EJ, Hwang DG, Jung MY, Cho HG. The effect of trigger point injections on pain in patients with advanced cancer. Korean J Fam Med. (2019) 40:344–7. doi: 10.4082/kjfm.18.0065
15. Brennan K, Elifritz KM, Comire MM, Jupiter DC. Rate and maintenance of improvement of myofascial pain with dry needling alone vs. dry needling with intramuscular electrical stimulation: A randomized controlled trial. J Man Manip Ther. (2021) 29:216–26. doi: 10.1080/10669817.2020.1824469
16. Silva AB, Malheiro N, Oliveira B, Pereira D, Antunes F, Borges J, et al. Efficacy of ultrasound-guided infiltration with levobupivacaine and triamcinolone for myofascial pain syndrome of the quadratus lumborum: A retrospective observational study. Braz J Anesthesiol. (2021) S0104-0014(21)00325-0. doi: 10.1016/j.bjane.2021.06.026
17. Kim DH, Yoon KB, Park S, Jin TE, An YJ, Schepis EA, et al. Comparison of NSAID patch given as monotherapy and NSAID patch in combination with transcutaneous electric nerve stimulation, a heating pad, or topical capsaicin in the treatment of patients with myofascial pain syndrome of the upper trapezius: a pilot study. Pain Med. (2014) 15:2128–38. doi: 10.1111/pme.12611
18. Vulfsons S, Minerbi A. The case for comorbid myofascial pain-a qualitative review. Int J Environ Res Public Health. (2020) 17:5188. doi: 10.3390/ijerph17145188
19. Barbero M, Schneebeli A, Koetsier E, Maino P. Myofascial pain syndrome and trigger points: evaluation and treatment in patients with musculoskeletal pain. Curr Opin Support Palliat Care. (2019) 13:270–6. doi: 10.1097/SPC.0000000000000445
20. Kiraly M, Bender T, Hodosi K. Comparative study of shockwave therapy and low-level laser therapy effects in patients with myofascial pain syndrome of the trapezius. Rheumatol Int. (2018) 38:2045–52. doi: 10.1007/s00296-018-4134-x
21. Fairbank JC, Pynsent PB. The oswestry disability index. Spine. (2000) 25:2940–52. doi: 10.1097/00007632-200011150-00017
22. Leak AM, Cooper J, Dyer S, Williams KA, Turner-Stokes L, Frank AO. The Northwick park neck pain questionnaire, devised to measure neck pain and disability. Br J Rheumatol. (1994) 33:469–74. doi: 10.1093/rheumatology/33.5.469
23. Gudin JA, Brennan MJ, Harris ED, Hurwitz PL, Dietze DT, Strader JD. Changes in pain and concurrent pain medication use following compounded topical analgesic treatment for chronic pain: 3- and 6-month follow-up results from the prospective, observational Optimizing Patient Experience and Response to Topical Analgesics study. J Pain Res. (2017) 10:2341–54. doi: 10.2147/JPR.S143513
24. Park KD, Lee WY, Park MH, Ahn JK, Park Y. High- versus low-energy extracorporeal shock-wave therapy for myofascial pain syndrome of upper trapezius: A prospective randomized single blinded pilot study. Medicine. (2018) 97:e11432. doi: 10.1097/MD.0000000000011432
25. Takla MKN. Low-frequency high-intensity versus medium-frequency low-intensity combined therapy in the management of active myofascial trigger points: A randomized controlled trial. Physiother Res Int. (2018) 23:e1737. doi: 10.1002/pri.1737
26. Segura-Pérez M, Hernández-Criado MT, Calvo-Lobo C, Vega-Piris L, Fernández-Martín R, Rodríguez-Sanz D, et al. Multimodal approach for myofascial pain syndrome: A prospective study. J Manipulative Physiol Ther. (2017) 40:397–403. doi: 10.1016/j.jmpt.2017.06.001
27. Yoo JI, Oh MK, Chun SW, Lee SU, Lee CH. The effect of focused extracorporeal shock wave therapy on myofascial pain syndrome of trapezius: A systematic review and meta-analysis. Medicine (Baltimore). (2020) 99:e19085. doi: 10.1097/MD.0000000000019085
28. Guzmán-Pavón MJ, Cavero-Redondo I, Martínez-Vizcaíno V, Fernández-Rodríguez R, Reina-Gutierrez S, Álvarez-Bueno C. Effect of physical exercise programs on myofascial trigger points-related dysfunctions: A systematic review and meta-analysis. Pain Med. (2020) 21:2986–96. doi: 10.1093/pm/pnaa253
Keywords: myofascial pain syndrome, Loxoprofen Sodium Cataplasm, physiotherapy, extracorporeal shock wave therapy, transcutaneous electrical nerve stimulation
Citation: Zhou X, Li X, Wang Z and Huang D (2022) Preliminary evidence of safety and effectiveness of Loxoprofen Sodium Cataplasm combined with physiotherapy for myofascial pain syndrome treatment: A randomized controlled pilot clinical trial. Front. Neurol. 13:998327. doi: 10.3389/fneur.2022.998327
Received: 19 July 2022; Accepted: 31 October 2022;
Published: 22 November 2022.
Edited by:
Areerat Suputtitada, Chulalongkorn University, ThailandReviewed by:
Zhenyu Wang, Chongqing Medical University, ChinaCorrado Italo Angelini, University of Padua, Italy
Copyright © 2022 Zhou, Li, Wang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong Huang, aHVhbmdkb25nNjYxOUB2aXAuMTYzLmNvbQ==; Ziyang Wang, NDM4Nzc0MzMyQHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xuewen Zhou
Xuewen Zhou Xuelian Li
Xuelian Li Ziyang Wang
Ziyang Wang Dong Huang
Dong Huang