- 1Department of Acupuncture, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, China
- 2National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin, China
Background: Acupuncture therapy has been widely used to treat post-stroke cognitive impairment (PSCI). However, acupuncture therapy includes multiple forms. Which acupuncture therapy provides the best treatment outcome for patients with PSCI remains controversial.
Objective: We aimed to compare and evaluate the efficacy and safety of different acupuncture-related therapies for PSCI in an attempt to identify the best acupuncture therapies that can improve cognitive function and self-care in daily life for patients with PSCI, and bring new insights to clinical practice.
Method: We searched eight databases including PubMed, Embase, Web of Science, Cochrane Central Register of Controlled Trials, China Biomedical Literature Database (CBM), China Science and Technology Journal (VIP) database, China National Knowledge Infrastructure (CNKI) database, and Wan fang database to find randomized controlled trials (RCTs) of acupuncture-related therapies for PSCI from the inception of the database to January 2023. Two researchers independently assessed the risk of bias in the included studies and extracted the study data. Pairwise meta-analyzes for direct comparisons were performed using Rev. Man 5.4 software. Bayesian network meta-analysis (NMA) was performed using STATA 17.0 and R4.2.4 software. The quality of evidence from the included studies was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system. Adverse effects (AEs) associated with acupuncture therapy were collected by reading the full text of the included studies to assess the safety of acupuncture therapy.
Results: A total of 62 RCTs (3 three-arm trials and 59 two-arm trials) involving 5,073 participants were included in this study. In the paired meta-analysis, most acupuncture-related therapies had a positive effect on cognitive function and self-care of daily living in patients with PSCI compared with cognitive training. Bayesian NMA results suggested that ophthalmic acupuncture plus cognitive training (79.7%) was the best acupuncture therapy for improving MMSE scores, with scalp acupuncture plus cognitive training ranking as the second (73.7%). The MoCA results suggested that warm acupuncture plus cognitive training (86.5%) was the best acupuncture therapy. In terms of improvement in daily living self-care, scalp acupuncture plus body acupuncture (87.5%) was the best acupuncture therapy for improving MBI scores. The most common minor AEs included subcutaneous hematoma, dizziness, sleepiness, and pallor.
Conclusion: According to our Bayesian NMA results, ophthalmic acupuncture plus cognitive training and warm acupuncture plus cognitive training were the most effective acupuncture treatments for improving cognitive function, while scalp acupuncture plus body acupuncture was the best acupuncture treatment for improving the performance of self-care in daily life in patients with PSCI. No serious adverse effects were found in the included studies, and acupuncture treatment appears to be safe and reliable. However, due to the low methodological quality of the included studies, our findings need to be treated with caution. High-quality studies are urgently needed to validate our findings.
Systematic review registration: https://www.crd.york.ac.uk/prospero/#recordDetails, identifier: CRD42022378353.
1. Introduction
Post-stroke cognitive impairment (PSCI), Characterized by distractibility and impaired language, memory, and executive skills, has a serious impact on the quality of life and survival time of stroke survivors (1). The prevalence of PSCI is steadily climbing as the population ages and the number of stroke survivors continues to increase. In the latest meta-analysis involving 16 studies, approximately 53.4% of stroke survivors were reported to suffer from PSCI, with the incidence of mild and severe PSCI being 36.4 and 16.5%, respectively (2). One study based on 6,504 stroke patients evaluated outcomes from the first 3 months to 5 years after stroke and found that patients with PSCI were strongly associated with an increased risk of death, dependency, depression, and hospitalization (3). However, in many national and international guidelines for stroke treatment, few details about PSCI were mentioned. It is clear that PSCI is not receiving enough attention and is not effectively addressed.
Currently, the treatment of PSCI mainly consists of pharmacological and non-pharmacological treatments. Studies have confirmed that there is no strong evidence that pharmacological interventions, including cholinesterase inhibitors and memantine, can improve cognition or slow the progression of dementia (4). In addition, one study based on 168 patients with vascular cognitive impairment found no significant improvement in cognitive function or ADL with donepezil (5). Instead, we found side effects associated with these drugs, such as gastrointestinal reactions and liver toxicity (6). Therefore, non-pharmacological treatments such as acupuncture, cognitive training, and transcranial magnetic stimulation have gradually received widespread attention. A network meta-analysis (7) published in 2022 compared five nonpharmacological treatments for improving cognitive function and self-care in patients with PSCI, and its results indicated that acupuncture was the most effective treatment for improving MoCA scores in PSCI patients.
Acupuncture, as a basic treatment tool in Chinese medicine, has been widely used for thousands of years for the prevention and treatment of various diseases (8). Acupuncture indeed has better clinical efficacy for some hard-to-treat chronic diseases, such as chronic kidney disease and low back pain (9, 10). In recent years, studies (11–13) have continued to find that acupuncture has a better effect on improving cognitive function in patients with PSCI. Relevant animal experiments are also being conducted in an attempt to explore the potential mechanism of acupuncture for PSCI. However, there are many forms of acupuncture treatment, including scalp acupuncture, warm acupuncture, abdominal acupuncture, and auricular acupuncture, etc. To date, there is still no systematic review that comprehensively compares and evaluates the efficacy of multiple acupuncture therapies. The differences in efficacy between acupuncture therapies remain unclear. Similarly, it is not clear to PSCI patients and clinicians which acupuncture technique is the best choice. Therefore, we conducted this network meta-analysis. In this study, we included 62 RCTs that critically evaluated the efficacy of eight different acupuncture techniques for the treatment of PSCI to provide evidence for the clinical selection of appropriate treatment options.
2. Methods
2.1. Registration
The protocol for this meta-analysis was registered with the International Platform for the Registration of Systematic Review (PROSPERO) under registration number CRD42022378353. This study was conducted in strict accordance with the PRISMA Extension Statement for Reports of Systematic Reviews Incorporating Meta-Analyzes of Healthcare Intervention Networks (PRISMA-NMA) (14), as detailed in Supplementary Appendix S1.
2.2. Search strategy
We searched eight databases including PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), China Biomedical Literature Database (CBM), China Science and Technology Journal (VIP) database, and Wan Fang database, from their inception to January, 2023, to find eligible RCTs regarding acupuncture treatment of PSCI. The language was restricted to Chinese or English. Meanwhile, the reference lists of systematic review articles were read to determine if there was any missing literature. The following terms were used in the search strategies: (acupuncture therapy, scalp acupuncture, warm acupuncture, electro-acupuncture) and (stroke, cerebrovascular accident, post-stroke cognitive impairment, and PSCI). The search strategy for each database was shown in Supplementary Appendix S2.
2.3. Eligibility criteria
We included studies that met the inclusion and exclusion eligibility criteria listed in Table 1.
2.4. Date extraction
Two investigators (YL and LZ) independently performed literature screening and data extraction and cross-checked the results. Any inconsistencies in the information extraction process can be resolved by the third investigator (FY-C). Extraction included basic characteristics (first author, year of publication, diagnostic criteria, sample size, gender, stroke type, age, duration of disease), details of the intervention (type of acupuncture, duration of treatment, periodicity, frequency), outcomes and adverse events (AEs).
2.5. Quality assessment
Two investigators (YL and LZ) independently assessed the quality of the included literature according to the risk of bias assessment tool (ROB2) recommended by the Cochrane Handbook. The assessments included the randomization process, deviation from the intended intervention, missing outcome data, measurement of the outcome, selection of the reported result, and overall bias. Each assessment component was categorized as low risk, high risk, and some concern. Given that the majority of acupuncture studies were published in Chinese journals, we used the Consolidated Standards for Reporting Trials (CONSORT) reporting guidelines (15) to assess the quality of included literature. The percentages for each item in the corresponding specifications were calculated and presented. In addition, the quality of evidence for each outcome indicator was assessed using the Grading of Recommendations, Assessments, Developments and Evaluations (GRADE) system (16), which resulted in a high, moderate, low, or very low level of evidence. Disagreements encountered during the assessment process could be resolved by the third investigator (FY-C).
2.6. Statistical analysis
Paired meta-analysis was performed using Rev. Man 5.4 software (Cochrane Collaboration, Oxford, United Kingdom). Effect sizes were calculated using mean differences (MDs) and 95% confidence intervals (CI) for continuous variables. Effect sizes were calculated using odd ratios (OR) and 95%CI for dichotomous variables. Heterogeneity between included studies was assessed according to the Q test (p value) and I2 statistic. If p ≥ 0.1 and I2 ≤ 50%, it represented acceptable heterogeneity, and a fixed-effects model was selected for meta-analysis, and conversely, a random-effects model was selected for meta-analysis.
STATA version 17.0 (Stata Corp, College Station, Texas, United States) and R version 4.2.4 (R Core Team, Vienna, Austria) were used for Bayesian framework network meta-analysis. Considering the possible heterogeneity among the included studies, we merged the data using random effects models. Given that the outcome variables chosen for this study were all continuous, mean differences (MDs) and 95% CI were selected for calculation. Markov chain Monte Carlo (MCMC) was used to calculate the model with the following parameters: four chains, 20,000 sample iterations, 5,000 burns, and a lean interval of 1. Brooks-Gelman-Rubin diagnostic plots were used to assess the convergence of the model. In addition, we also observed trajectory and density plots. The node-splitting method was used to assess the agreement between direct and indirect comparisons. p > 0.05 indicates the existence of the agreement. When there was a closed loop, we used the inconsistency factor (IF) to make the judgment. When the 95% CI contains 0, it indicates the existence of consistency between direct and indirect evidence. The surface under the cumulative ranking area (SUCRA) was calculated to rank each intervention probabilistically. The value of SUCRA ranged from 0 to 100%, with higher values indicating better efficacy. The following formula was used to approximate the outcome data, taking into account possible differences in baseline conditions for outcome indicators in the included studies, where the correlation coefficient R-value was 0.5.
3. Results
3.1. Literature selection
We initially searched for 2,268 potentially relevant articles and excluded 1,075 articles due to duplication. The 1,094 articles were excluded by reading the titles and abstracts. The remaining 99 studies were evaluated by reading the full text. 62 studies (17–78) were ultimately included in the quantitative analysis. The PRISMA flowchart of the search process is shown in Figure 1.
3.2. Study characteristics
All 62 included studies were conducted in China, of which 59 and 3 RCTs were published in Chinese and English, respectively. These included studies were reported between 2012 and 2022. A total of 5,073 participants were included, of which 2,593 participants were in the experimental group and 2,480 participants were in the control group. Among the 62 studies, 3 (18, 53, 55) were three-arm trials and 59 were two-arm trials. The baseline data for participants in both groups were generally similar, but 5 studies (23, 25, 36, 41, 45) did not report the mean age and 17 studies (25, 31, 33, 34, 36–38, 41, 44–47, 50, 52, 57, 58, 69) did not report the mean duration of disease. 3 studies (23, 35, 36) reported patient drop-out and reported specific reasons, and the number of drop-outs ranged from 3 to 11. Treatment duration ranged from 2 weeks to 12 weeks. In terms of treatment measures, in addition to cognitive training (CT), 13 types of acupuncture-related therapies are included, which were body acupuncture (BA), scalp acupuncture (SA), body acupuncture plus cognitive training (BA+CT), scalp acupuncture plus cognitive training (SA + CT), ophthalmic acupuncture plus cognitive training (OA + CT), warm acupuncture plus cognitive training (WA + CT), electro-acupuncture plus cognitive training (EA + CT), auricular bloodletting plus cognitive training (AB+CT), abdominal acupuncture plus cognitive training (AA+CT), scalp acupuncture plus body acupuncture (SA + BA), abdominal acupuncture plus body acupuncture (AA+BA), warm acupuncture plus scalp acupuncture (WA + SA) and scalp acupuncture plus auricular bloodletting (SA + AB). Furthermore, 47 studies (17–23, 25–29, 31, 33–36, 38, 40, 41, 43–50, 52, 53, 55–57, 59, 60, 62–67, 70, 72, 73, 75, 77, 78) reported MMSE scores, 29 studies (18, 24, 28, 30–34, 37, 39, 42, 47–49, 52, 54, 58, 61–63, 67–72, 74, 76, 77) reported MoCA scores and 20 studies (22–24, 27, 30, 32–35, 41, 42, 47–50, 54, 60, 61, 73, 74) reported MBI scores. The characteristics of the included studies are shown in Table 2.
3.3. Risk of bias
According to ROB2, three studies (23, 35, 36) were rated at high risk of bias, two studies (19, 26) were rated at low risk of bias, and the remaining studies were rated at some risk of bias. The main issues included lack of description of allocation concealment, lack of blinding of outcome assessors, and lack of exploration of prospective protocols, which ultimately led to an increased risk of bias. The risk of bias assessment for the included studies is presented in Supplementary Figure S1. Many of the items in the CONSORT (18/25 items) statements did not achieve the desired reporting rate (>80%), which was shown in Supplementary Appendix 3.
3.4. Pairwise meta-analysis
After a comprehensive analysis of studies with the same treatment and outcomes, we conducted 19 direct-paired meta-analyzes to compare MMSE scores, 11 to compare MoCA scores, and 10 to compare MBI scores, respectively. As for MMSE scores,SA (two RCTs; WMD = 2.50, 95%CI: 0.67, 4.32, p = 0.007), BA+CT (one RCT; WMD = 5.29, 95%CI: 4.16, 6.42, P<0.00001), SA + CT (16 RCTs; WMD = 4.39, 95%CI: 3.08, 5.70, P<0.00001), OA + CT (one RCT; WMD = 5.85, 95%CI: 4.69, 7.01, P<0.00001), WA + CT (one RCT; WMD = 1.86, 95%CI: 0.16, 3.56, p = 0.03), AB+CT (one RCT; WMD = 2.57, 95%CI: 0.81, 4.33, p = 0.004), SA + BA (16 RCTs; WMD = 4.24, 95%CI: 3.28, 5.20, p<0.00001), SA + AB (one RCT; WMD = 3.84, 95%CI: 2.00, 5.68, p<0.00001) were effective than the CT group. In the comparison of different acupuncture treatments, we found that SA (one RCT; WMD = 0.88, 95%CI: 0.15, 1.61, p = 0.02), SA + CT (one RCT; WMD = 2.42, 95%CI: 0.74, 4.10, p = 0.005), SA + BA (two RCTs; WMD = 1.79. 95% CI: 1.05, 2.53, p < 0.00001) improved MMSE scores more than BA alone. Furthermore, SA + CT (one RCT; WMD = 2.48, 95%CI: 0.18, 4.78, p = 0.03) and WA + CT (one RCT; WMD = 1.22, 95%CI: 0.08, 2.36, p = 0.04) were more effective in improving MMSE scores compared with BA+CT. Meanwhile, SA + CT had a greater effect than SA alone (two RCTs; WMD = 3.23, 95%CI: 1.49, 4.97, p = 0.0003). However, there was no statistical difference in efficacy between BA and CT, EA and CT, AA+BA and CT, AA+CT and BA+CT, and SA + AB and BA+CT. In terms of MoCA scores, SA + CT (10 RCTs; WMD =3.75, 95%CI: 2.81, 4.69, P<0.00001), SA + BA (four RCTs; WMD = 3.26, 95%CI: 2.19, 4.34, P<0.00001), WA + CT (five RCTs; WMD = 3.96, 95%CI: 2.29, 5.62, P<0.00001), EA + CT (four RCTs; WMD = 3.16, 95%CI: 1.88, 4.45, p<0.00001), AA+CT (one CRT; WMD = 3.00, 95%CI: 0.26, 5.74, p = 0.03) were more effective than CT alone. Furthermore, compared with WA + CT, SA + CT (one RCT; WMD = 3.14, 95%CI: 2.15, 4.13, p<0.00001) and SA + BA (two RCTs; WMD = 3.61, 95%CI: 2.11, 5.11, p<0.00001) were more effective in improving MoCA scores. Meanwhile, SA + BA had a greater effect than BA alone (one RCT; WMD = 2.00, 95%CI: 1.37, 2.63, p<0.00001). However, there was no statistical difference in efficacy between SA + CT and SA, SA and CT, and WA + SA and CT. For MBI scores, BA+CT (one RCT; WMD = 7.23, 95%CI: 5.39, 9.07, p<0.00001), SA + CT (seven RCTs; WMD = 12.83, 95%CI: 5.06, 20.60, p = 0.001), WA + CT (three RCTs; WMD = 10.13, 95%CI: 5.31, 14.96, p<0.0001), SA + BA (two RCTs; WMD = 19.13, 95%CI: 18.08, 20.18, p<0.00001), EA + CT (one RCT; WMD = 1.74, 95%CI: 0.13, 3.35, p = 0.03) and AB + CT (one RCT; WMD =13.57, 95%CI: 6.23, 20.82, p = 0.0002) were more effective than CT group. Furthermore, compared with BA+CT, AA+CT (one RCT; WMD =6.00, 95%CI: 6.40, 7.40, p<0.00001), SA + BA (two RCTs; WMD = 10.40, 95%CI: 3.14, 17.66, p = 0.005) and WA + CT (one RCT; WMD = 3.23, 95%CI: 0.12, 6.34, p = 0.04) were more effective in improving MBI scores. However, there was no statistical difference in efficacy between AA+BA and CT. The results of paired meta-analysis and heterogeneity are presented in Table 3.
3.5. Network meta-analysis
The transferability hypothesis was assessed by evaluating the baseline differences in mean age and disease duration of patients in the included studies. As shown in Figure 2A, the mean age of PSCI patients showed a high degree of similarity among the included studies. Furthermore, as shown in Figure 2B, the mean duration of disease in patients with PSCI also showed a high degree of similarity. Therefore, this study satisfies the transferability hypothesis and reliable results can be obtained.
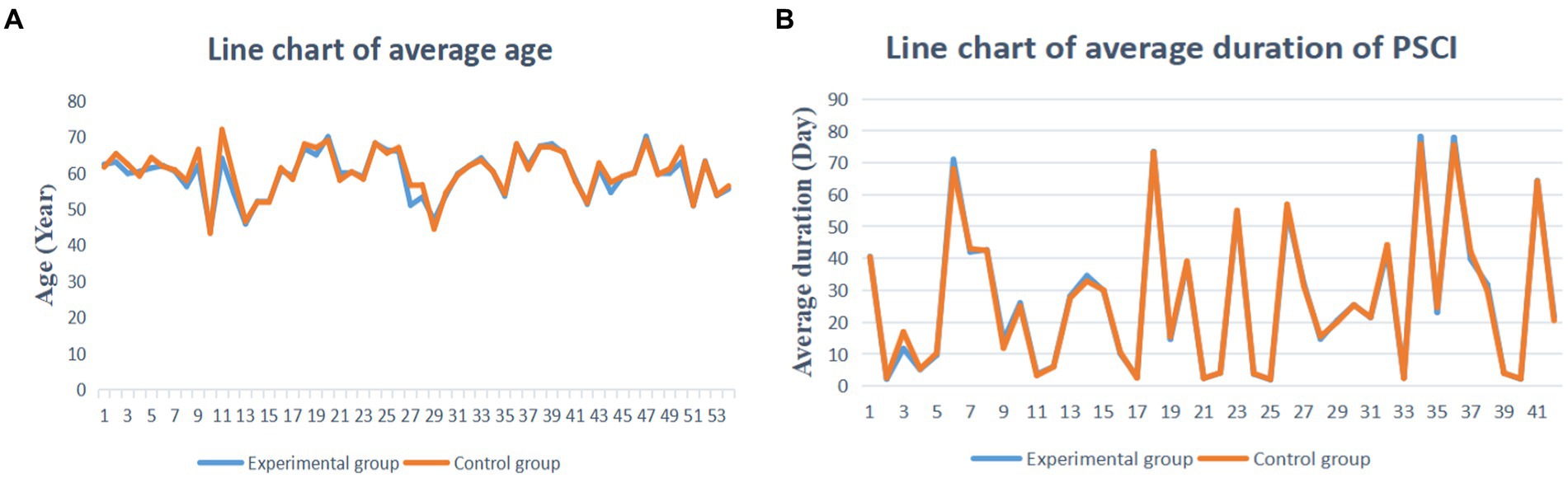
Figure 2. Baseline assessment. (A) The average age assessment. (B) The average duration PSCI assessment.
The inconsistency test results for MMSE, MoCA, and MBI scores were all greater than 0.05 (p = 0.9064, 0.7492, and 0.9231), so the consistency model was selected for analysis. We adopted the node-splitting method to test the internal inconsistency of NMA. The results showed no significant differences between direct or indirect comparisons for each split node (p > 0.05), which suggests no evidence of the existence of inconsistency (Supplementary Figure S2). The results of the closed-loop inconsistency test showed that all 95% CI contained 0, which indicated that the closed-loop comparisons possessed excellent consistency (Supplementary Table S1). The Brooks-Gelman-Rubin diagnostic plots showed that the shrink factor’s median and 97.5% value tended to be 1 and stabilized after 5,000 iterations, and then the Bayesian model was calculated up to 20,000 iterations (Supplementary Figure S3). Meanwhile, we observed the trajectory and density plots (Supplementary Figure S4). All these results indicate that the model has excellent convergence.
All included studies with 4,057 participants and 13 acupuncture-related therapies reported MMSE data (Figure 3A), including 3 (18, 53, 55) three-arm studies (6.4%) and 44 two-arm studies (93.6%). Among them, the CT group had the largest sample size. The two groups most commonly compared were scalp acupuncture plus cognitive training and cognitive training, and scalp acupuncture plus body acupuncture and cognitive training, respectively. 29 studies reported MoCA data involving 2,285 participants and 10 acupuncture-related therapies (Figure 3B). 20 studies reported MBI data involving 1,579 participants and 9 acupuncture-related therapies (Figure 3C).
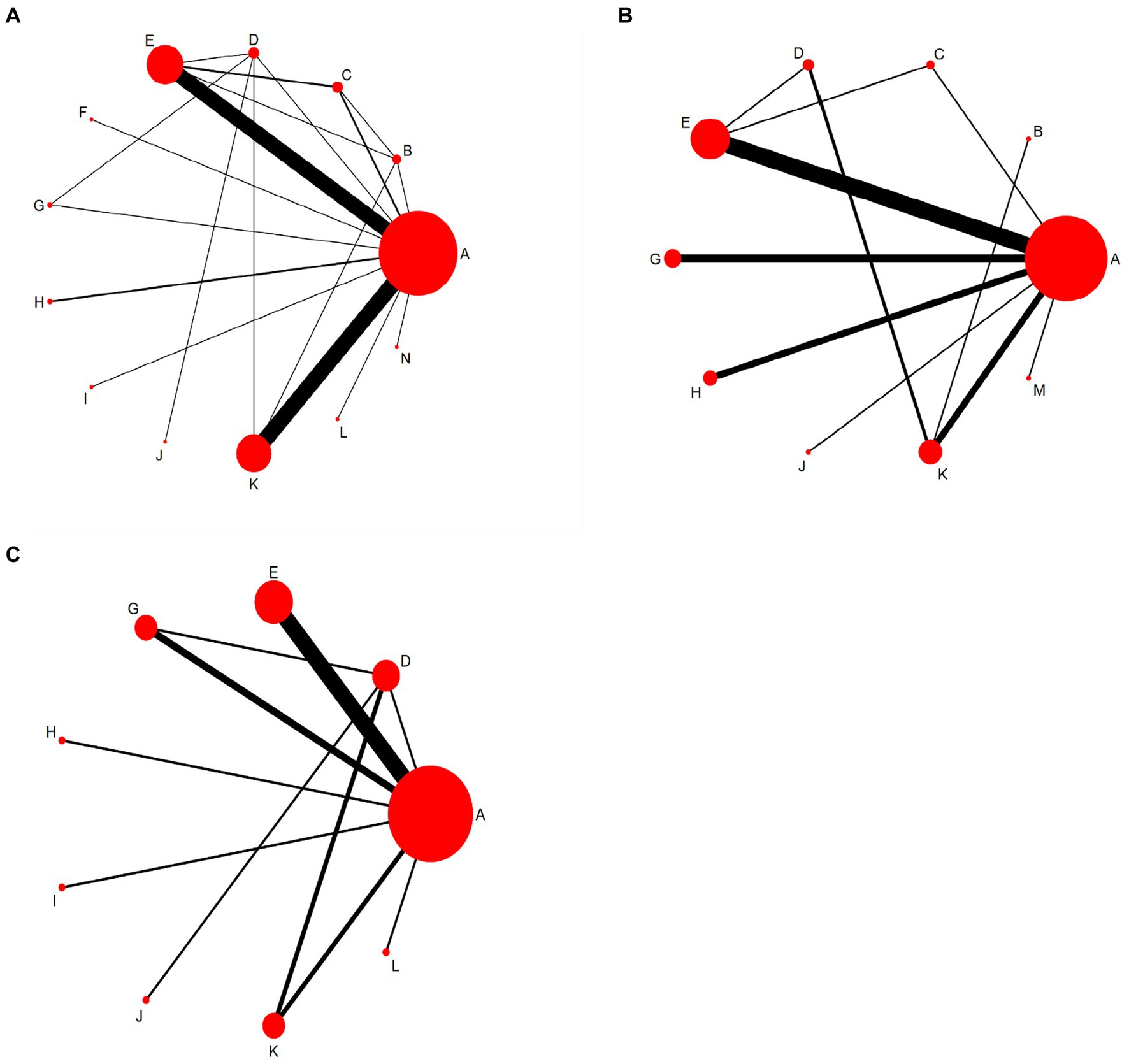
Figure 3. Network evidence diagram. A, Cognitive training; B, Body acupuncture; C, Scalp acupuncture; D, Body acupuncture plus cognitive training; E, Scalp acupuncture plus cognitive training; F, Ophthalmic acupuncture plus cognitive training; G, Warm acupuncture plus cognitive training; H, Electro-acupuncture plus cognitive training; I: Auricular bloodletting plus cognitive training; J, Abdominal acupuncture plus cognitive training; K, Scalp acupuncture plus body acupuncture; L: Abdominal acupuncture plus body acupuncture; M: Warm acupuncture plus scalp acupuncture; N: Scalp acupuncture plus auricular bloodletting. (A) The Minimum Mental State Examination scale (MMSE). (B) The Montreal Cognitive Assessment Scale (MoCA). (C) The Modified Barthel Index scale (MBI).
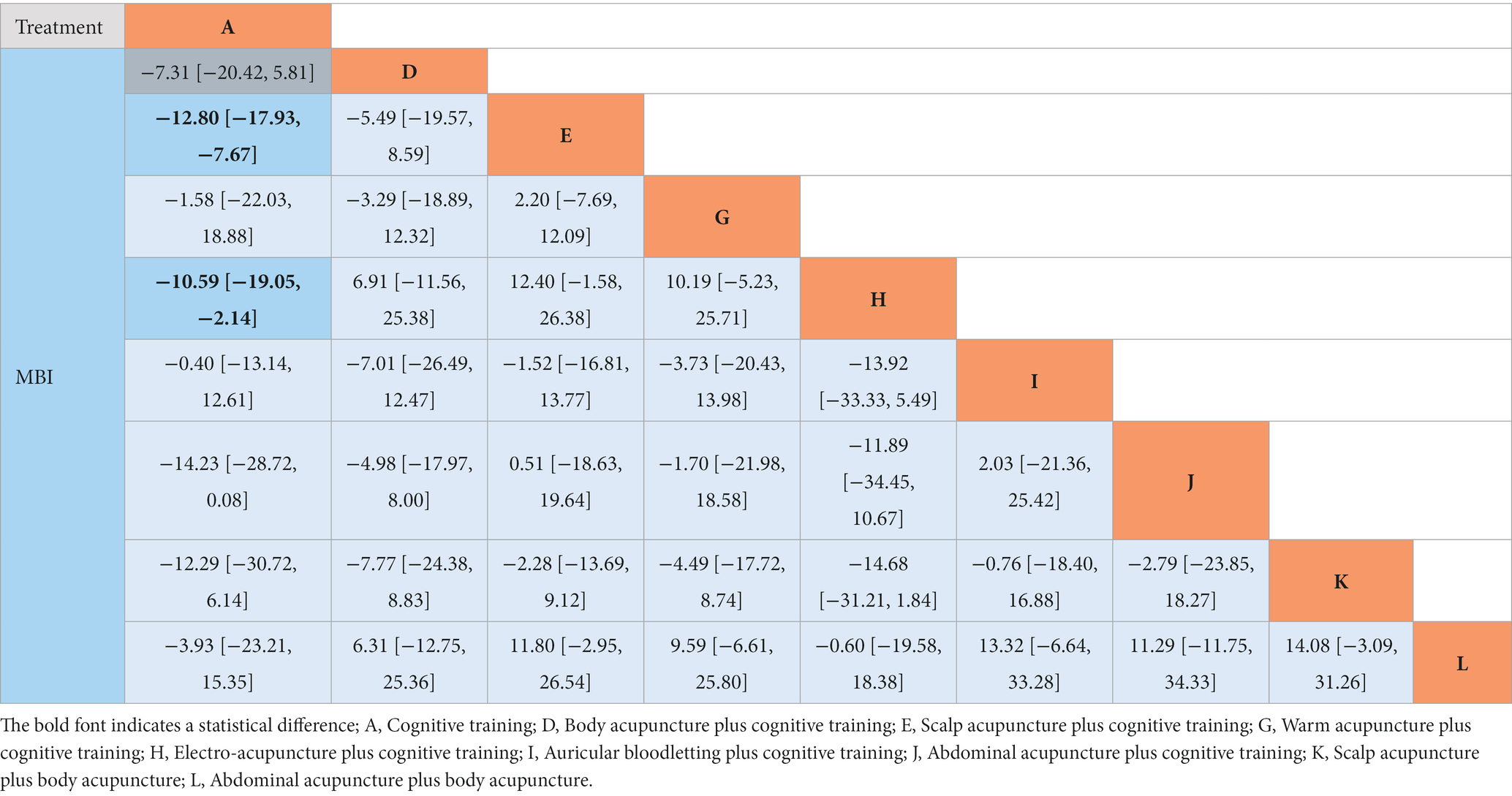
In terms of improving MMSE scores, the results (Table 4) showed that BA+CT (MD = −3.00, 95%CI: −5.94, −0.05), SA + CT (MD = −4.50, 95%: −5.85, −3.16), OA + CT (MD = −6.31, 95%CI: −11.64, −1.01) and SA + BA (MD = −3.92, 95%CI: −5.19, −2.64) were more effective for PSCI patients compared to the CT group. In addition, SA + CT (MD = −2.94, 95%CI: −5.85, −0.04) was more effective than BA when comparing different acupuncture treatments. Regarding the improvement of MoCA score, the results (Table 4) showed that SA + CT (MD = 3.54, 95%CI: 2.44, 4.59), WA + CT (MD = 4.04, 95%CI: 2.53, 5.50), EA + CT (MD = 3.33, 95%CI: 1.29, 5.38) and SA + BA (MD = 2.84, 95%CI: 1.10, 4.56) were more effective in patients with PSCI compared to the CT group. In addition, SA + CT (MD = 3.71, 95%CI: 1.43, 5.98), WA + CT (MD = 4.20, 95%CI: 1.51, 6.88), EA + CT (MD = 3.49, 95%CI: 0.45, 6.54) and SA + BA (MD = 3.01, 95%CI: 1.00, 4.96) were more effective than BA+CT when comparing different acupuncture treatments. In terms of improving MBI scores, the results (Table 5) showed that SA + CT (MD = −12.80, 95%CI: −17.93, −7.67) and EA + CT (MD = −10.59, 95%CI: −19.05, −2.14) were more effective than CT alone.
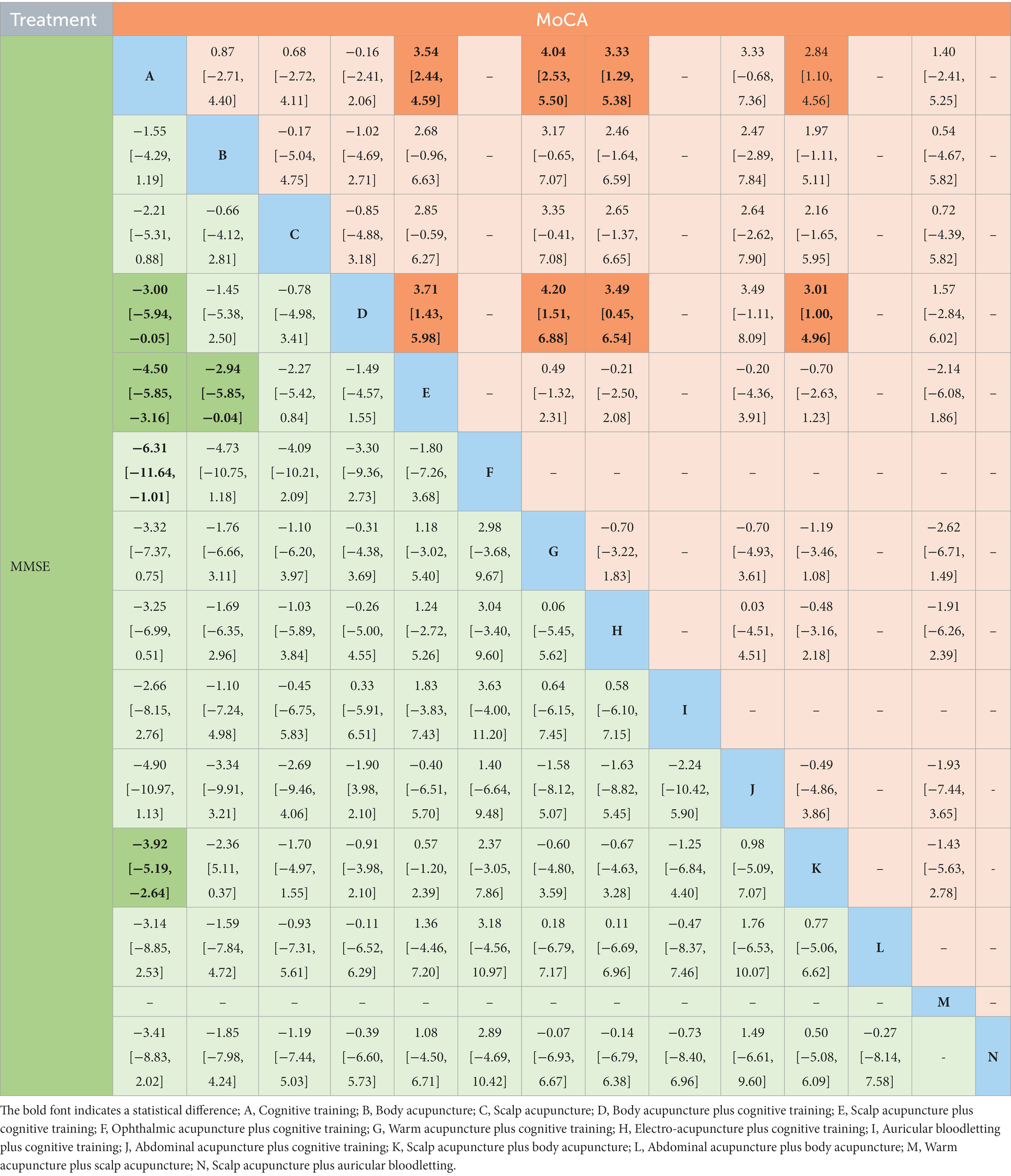
Table 4. Network meta-analysis results of Minimum Mental State Examination Scale (MMSE) and Montreal Cognitive Assessment Scale (MoCA).
We calculated the SUCRA values for each intervention for probability ranking (Supplementary Table S2) and constructed probability ranking histograms using R software (Figure 4). Figure 4A shows that among the 13 treatments, CT (6.2%) had the worst ability to improve MMSE scores. In addition, the top three acupuncture treatments that improved MMSE scores were OA + CT (79.7%), SA + CT (73.7%), and AA+CT (69.5%). WA + CT (86.5%), SA + CT (77.3%), and EA + CT (72.1%) were the three best acupuncture treatments for improving MoCA scores (Figure 4B). Furthermore, SA + BA (87.5%), AB+CT (75.4%), and SA + CT (72.6%) were the three most effective acupuncture treatments among the nine treatments for improving MBI scores (Figure 4C).
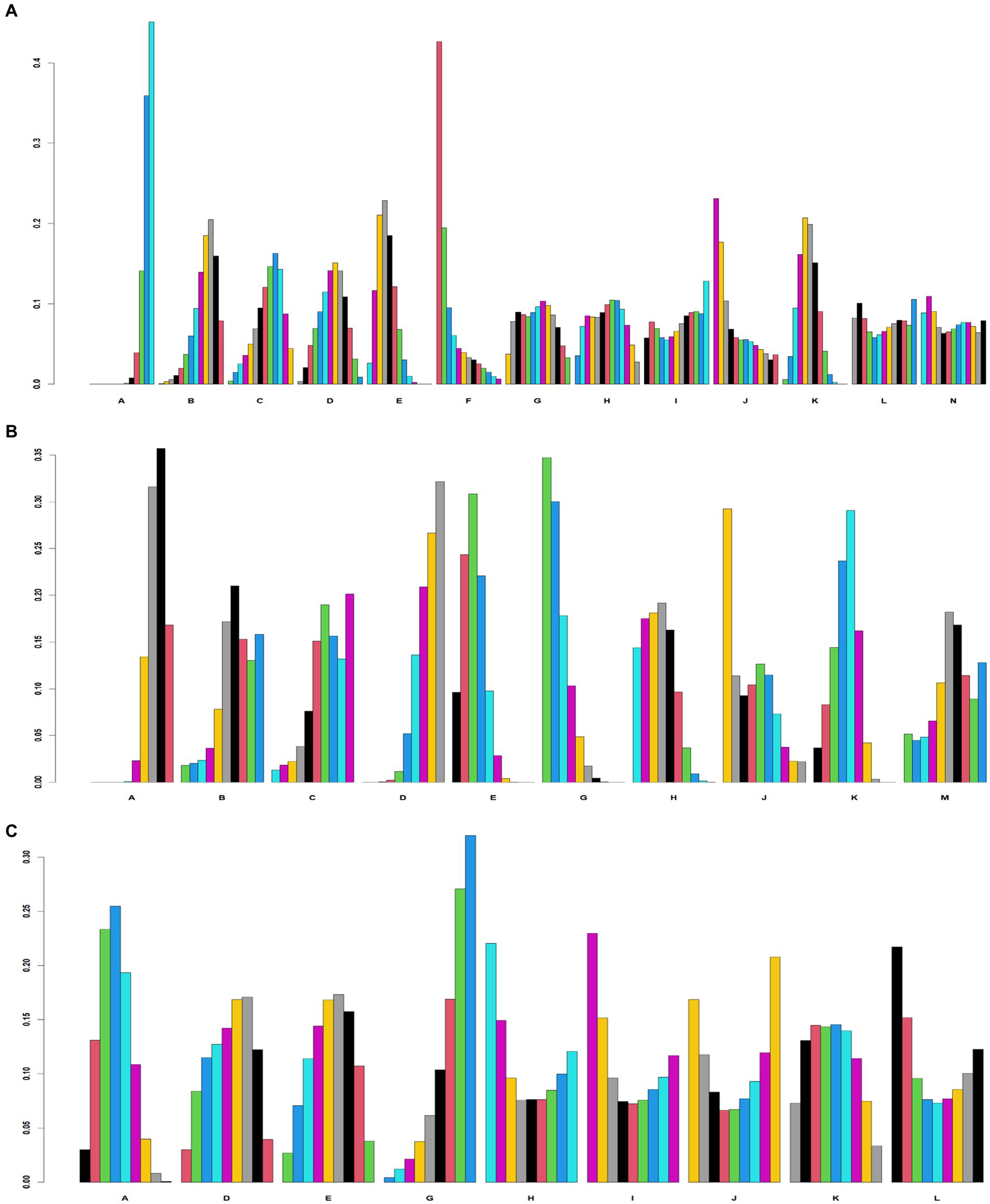
Figure 4. Probability ranking diagram. A, Cognitive training; B, Body acupuncture; C, Scalp acupuncture; D, Body acupuncture plus cognitive training; E, Scalp acupuncture plus cognitive training; F, Ophthalmic acupuncture plus cognitive training; G, Warm acupuncture plus cognitive training; H, Electro-acupuncture plus cognitive training; I, Auricular bloodletting plus cognitive training; J, Abdominal acupuncture plus cognitive training; K, Scalp acupuncture plus body acupuncture; L, Abdominal acupuncture plus body acupuncture; M, Warm acupuncture plus scalp acupuncture N: Scalp acupuncture plus auricular bloodletting. (A) Minimum Mental State Examination scale (MMSE). (B) Montreal Cognitive Assessment Scale (MoCA). (C) Modified Barthel Index scale (MBI).
3.6. Adverse effect
Of the 62 studies included, six studies (17, 18, 38, 43, 61, 67) (9%) reported adverse reactions (Supplementary Table S3). Three studies (17, 18, 38) reported no adverse reactions during treatment. One study (67) reported that patients in the electroacupuncture group experienced subcutaneous hematomas after treatment, but they recovered spontaneously without systematic treatment. Two studies (43, 61) reported that patients experienced adverse effects such as dizziness, pallor, and sleepiness, which were considered to be possibly related to the first time they received acupuncture treatment. In conclusion, acupuncture treatment seems to be safe and reliable, but there is no sufficient evidence to prove it.
3.7. Publication bias
Comparative adjustment funnel plots were plotted using STATA software to assess publication bias and small sample size effects for the MMSE, MoCA, and MBI, respectively (Figure 5). The results showed that the comparative adjustment funnel plots for the MoCA and MBI scales were symmetrical, with most points evenly distributed on either side of the midline, reflecting a moderate sample size of the included studies and a low likelihood of publication bias. However, in the comparative adjusted funnel plot for the MMSE scale, most studies were more dispersed, with some of them lying outside the 95% CI range, indicating possible publication bias.
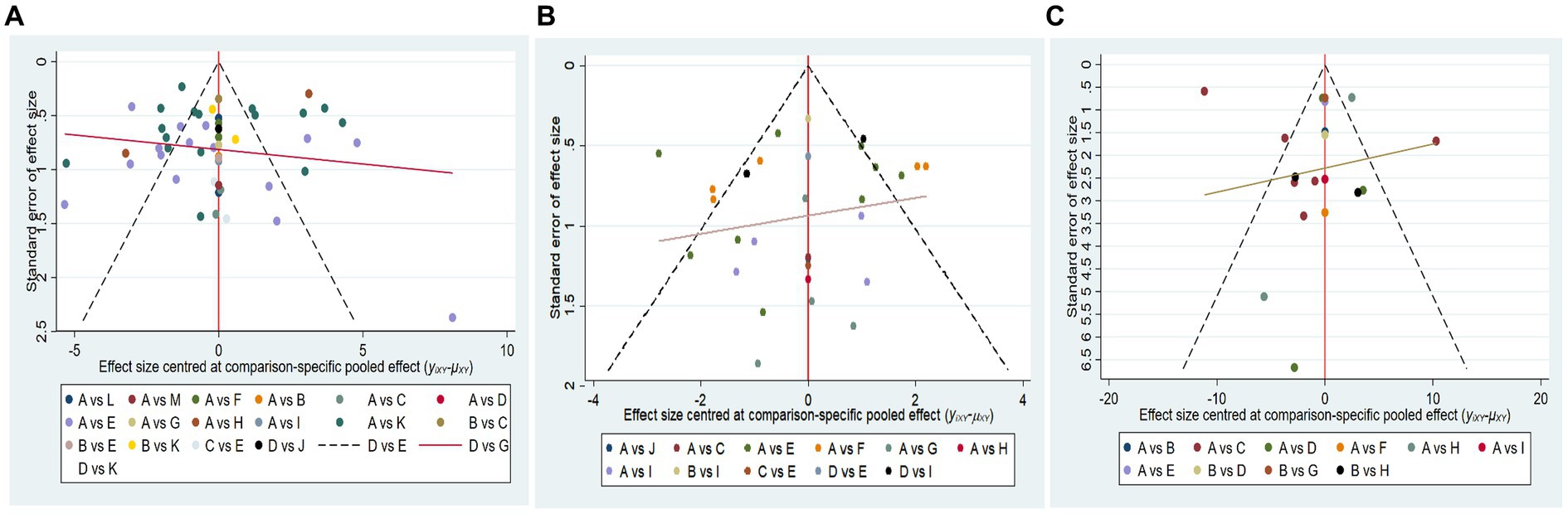
Figure 5. Comparative adjustment funnel plots. A, Cognitive training; B, Body acupuncture; C, Scalp acupuncture; D, Body acupuncture plus cognitive training; E, Scalp acupuncture plus cognitive training; F, Ophthalmic acupuncture plus cognitive training; G, Warm acupuncture plus cognitive training; H, Electro-acupuncture plus cognitive training; I, Auricular bloodletting plus cognitive training; J, Abdominal acupuncture plus cognitive training; K, Scalp acupuncture plus body acupuncture; L, Abdominal acupuncture plus body acupuncture; M, Warm acupuncture plus scalp acupuncture; N, Scalp acupuncture plus auricular bloodletting. (A) Minimum Mental State Examination scale (MMSE). (B) Montreal Cognitive Assessment Scale (MoCA). (C) Modified Barthel Index scale (MBI).
3.8. Evidence assessment of outcome measures
According to the GRADE scores, the strength of evidence for the three scales mentioned above ranged between very low and moderate. The main reasons for the reduced quality of evidence were flaws in study design and considerable statistical heterogeneity (Supplementary Table S4).
4. Discussion
4.1. Summary of main finding
In this systematic review, a total of 62 RCTs involving 5,073 participants and 13 acupuncture-related therapies were included. The results of the paired meta-analysis showed that most acupuncture-related therapies were effective in improving global cognitive ability (measured by MMSE and MoCA) and self-care of daily living (measured by MBI) in PSCI patients. Furthermore, BA, AA+BA, and WA + SA did not show sufficient advantages compared with the CT group. Notably, only one study of these three types of acupuncture therapy was compared with the CT group. The effect size may change as the sample size increases. The results of the NMA showed that in terms of improving MMSE scores, BA+CT, SA + CT, OA + CT, and SA + BA resulted in better outcomes for patients with PSCI compared with the CT group. In addition, the efficacy of SA + CT was better than BA alone. Based on the probability ranking results, it is clear that OA + CT is the most effective in improving MMSE scores. In terms of improving MoCA scores, SA + CT, WA + CT, EA + CT, and SA + BA were capable of delivering better outcomes than the CT group. Furthermore, the efficacy of the four acupuncture-related therapies was better than BA+CT. Based on the probability ranking results, it is clear that WA + CT is the most effective acupuncture therapy for improving MoCA scores. Regarding the improvement of MBI scores, SA + CT and EA + CT were more effective than CT alone. Furthermore, no statistically significant differences were found in the comparison of the various acupuncture therapies. Based on the probability ranking, it is clear that SA + BA is the most effective acupuncture measure for improving MBI scores in PSCI patients. Although the certainty of the evidence was rated as very low to moderate due to deficiencies in methodological quality and strong heterogeneity among studies, this review provides an up-to-date overview of the available RCTs of different types of acupuncture for PSCI.
4.2. Clinical practice applicability
Different from Alzheimer’s disease, there are still no symptomatic medications approved by authoritative official regulatory authorities for the treatment of PSCI (79). As a result, the focus of many medical associations has gradually shifted to whether nonpharmacologic interventions can help patients with PSCI improve cognitive function and maintain normal daily living independence (80). Based on clinical evidence, acupuncture is a relatively resource-intensive intervention that appears to be desirable for chronic conditions such as cognitive impairment that require long-term treatment (81). Studies (12, 13) have been conducted to demonstrate the effectiveness of acupuncture in the treatment of PSCI. However, acupuncture therapy encompasses a variety of forms and previous studies have tended to view acupuncture therapy as a whole. As for which acupuncture therapy can bring the best outcome for PSCI patients, it is still not clear. In clinical applications, ineffective acupuncture treatment inevitably delays optimal treatment time and wastes medical resources. Therefore, we conducted this study in an attempt to identify the best acupuncture treatment to improve cognitive function and self-care in daily life for patients with PSCI, providing new insights for clinical practice. We initially proposed pharmacological treatment and acupuncture techniques alone as the treatment measures for the control group. Unfortunately, we found that cholinesterase inhibitors are only used in China for the treatment of PSCI. Therefore, cognitive training and the acupuncture technique alone were finally set as the treatment measures for the control group in this study. The comparison between acupuncture therapy and cognitive training is meaningful because most guidelines on the treatment of PSCI include cognitive training as a treatment to improve PSCI patients.
The potential mechanisms of acupuncture for the treatment of PSCI have now been extensively studied. Therefore, we categorized the mechanisms into the following six aspects: (1) acupuncture can reduce the expression of inflammatory factors by inhibiting the degradation of IkB kinase or inhibiting the entry of NF-kB into the cell nucleus, which can result in the improvement of cognitive function (82), (2) acupuncture antagonizes neuronal apoptosis by increasing the transactivation activity of the PI3K/AKL signaling pathway (83), (3) acupuncture ameliorates neurological deficits by inhibiting the expression of autophagy-related proteins LC3-II and Beclin-1 in brain tissue (84), (4) acupuncture promotes axonal regeneration and improves synaptic plasticity by promoting the expression of PSD-95 and SYN proteins (85), (5) acupuncture improves neurological deficits and learning memory by upregulating the expression of VEGF and NGFs vascular endothelial factors (86), and (6) acupuncture reduces nerve cell damage by increasing the expression activity of endogenous oxidants such as SOD and GSH-PX proteins (87).
4.3. Study strengths and limitations
To the best of our knowledge, this study is the first network meta-analysis to comprehensively assess the efficacy and safety of different acupuncture therapies for PSCI based on currently available evidence. This study was conducted in strict accordance with PRISMA-NMA guidelines. Eight Chinese and English databases were searched to ensure the adequacy of the number of included studies, and references to systematic reviews of relevant topics were also reviewed. We used explicit inclusion and exclusion criteria, data extraction, and risk of bias assessment, and assessed the methodological quality of the included studies using the CONSORT statement guidelines. From the mesh evidence map, we found that only a small number of studies compared different acupuncture therapies directly. Therefore, in the absence of direct evidence, we used the method of network meta-analysis to provide indirect evidence. Finally, according to the nodal split model, it is clear that there is no significant difference between direct or indirect comparisons for each split node (p > 0.05), while the Brooks-Gelman-Rubin diagnostic plots for each outcome indicator show that the median and 97.5% values of the contraction factor converge to 1, which indicates that our findings are stable and reliable.
However, there are some limitations of this study that need to be considered. Firstly, acupuncture therapy is a unique non-pharmacological treatment in China, most of the literature related to acupuncture is published in Chinese databases. Therefore, a comprehensive search of Chinese databases is necessary. Unfortunately, most of the included studies were of low quality in terms of experimental design, mainly in the form of a lack of description of allocation concealment, blinding of outcome assessors, and detailed descriptions of prospective plans, which partly contributed to the overall quality of the evidence being rated as low. Seventy-two percent did not achieve the expected reporting rate (>80%) as assessed by the CONSORT statement. In addition, we found a high level of heterogeneity in some comparisons in the results of the paired meta-analysis. Through a review of the literature, we found that this heterogeneity may stem from clinical heterogeneity. Although we compared the same kinds of acupuncture therapies with cognitive training, some factors, such as acupuncture depth, retention time, and acupoint selection, still differed. Differences in the skill level of acupuncture therapists during clinical practice are among the factors that contribute to clinical heterogeneity. Furthermore, given that only thirteen trials in this review were pre-registered, the prospective registration of study protocols before conducting studies should be strongly urged so that others can follow their studies. Moreover, with regard to blinding, it is difficult to blind acupuncture therapists due to the inherent characteristics of acupuncture as a non-pharmacological therapy. However, it is feasible and necessary to blind participants and outcome assessors.
5. Conclusion
Based on the available evidence, most acupuncture therapies have positive effects on cognitive function and self-care in daily life in PSCI patients compared to cognitive training. Acupuncture-related therapies may be an effective alternative intervention for the treatment of PSCI. Ophthalmic acupuncture plus cognitive training may be the treatment of choice for improving MMSE scores in PSCI patients. Warm acupuncture plus cognitive training was the preferred therapy for improving MoCA scores, while scalp acupuncture plus body acupuncture was the preferred therapy for improving MBI scores. The methodological quality of the literature included in this study was low and the results should be treated with caution. Future high-quality studies are needed for further validation of our findings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YL, LZ, and FC conceived and designed the study and edited the final manuscript. XL and JH designed the research methodology. MB and XS developed the search strategy and performed data extraction. YL and LZ performed data analysis and wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a grant (The National Natural Science Foundation of China No. 81603684).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1218095/full#supplementary-material
References
1. Sun, JH, Tan, L, and Yu, JT. Post-stroke cognitive impairment: epidemiology, mechanisms and management. Ann Transl Med. (2014) 2:80. doi: 10.3978/j.issn.2305-5839.2014.08.05
2. Barbay, M, Diouf, M, Roussel, M, and Godefroy, O. Systematic review and Meta-analysis of prevalence in post-stroke neurocognitive disorders in hospital-based studies. Dement Geriatr Cogn Disord. (2018) 46:322–34. doi: 10.1159/000492920
3. Obaid, M, Douiri, A, Flach, C, Prasad, V, and Marshall, I. Can we prevent Poststroke cognitive impairment? An umbrella review of risk factors and treatments. BMJ Open. (2020) 10:e037982. doi: 10.1136/bmjopen-2020-037982
4. Quinn, TJ, Richard, E, and Teuschl, Y. European stroke organisation and European academy of neurology joint guidelines on post-stroke cognitive impairment. Eur J Neurol. (2021) 28:3883–920. doi: 10.1111/ene.15068
5. Dichgans, M, Markus, HS, and Salloway, S. Donepezil in patients with subcortical vascular cognitive impairment: a randomised double-blind trial in Cadasil. Lancet Neurol. (2008) 7:310–8. doi: 10.1016/s1474-4422(08)70046-2
6. Marucci, G, Buccioni, M, Ben, DD, Lambertucci, C, Volpini, R, and Amenta, F. Efficacy of acetylcholinesterase inhibitors in Alzheimer's disease. Neuropharmacology. (2021) 190:108352. doi: 10.1016/j.neuropharm.2020.108352
7. Li, Z, Yang, L, and Qiu, H. Comparative efficacy of 5 non-pharmacological therapies for adults with post-stroke cognitive impairment: a Bayesian network analysis based on 55 randomized controlled trials. Front Neurol. (2022) 13:977518. doi: 10.3389/fneur.2022.977518
8. Kaptchuk, TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. (2002) 136:374–83. doi: 10.7326/0003-4819-136-5-200203050-00010
9. Berman, BM, Langevin, HM, and Witt, CM. Acupuncture for chronic low Back pain. N Engl J Med. (2010) 363:454–61. doi: 10.1056/NEJMct0806114
10. Kim, KH, Lee, MS, and Kim, TH. Acupuncture and related interventions for symptoms of chronic kidney disease. Cochrane Database Syst Rev. (2016) 2016:CD009440. doi: 10.1002/14651858.CD009440.pub2
11. Liu, Y, Chen, F, and Qin, P. Acupuncture treatment vs. cognitive rehabilitation for post-stroke cognitive impairment: a systematic review and Meta-analysis of randomized controlled trials. Front Neurol. (2023) 14:1035125. doi: 10.3389/fneur.2023.1035125
12. Zhou, L, Wang, Y, and Qiao, J. Acupuncture for improving cognitive impairment after stroke: a Meta-analysis of randomized controlled trials. Front Psychol. (2020) 11:549265. doi: 10.3389/fpsyg.2020.549265
13. Kuang, X, Fan, W, and Hu, J. Acupuncture for post-stroke cognitive impairment: a systematic review and Meta-analysis. Acupunct Med. (2021) 39:577–88. doi: 10.1177/09645284211009542
14. Hutton, B, Salanti, G, and Caldwell, DM. The Prisma extension statement for reporting of systematic reviews incorporating network Meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/m14-2385
15. Schulz, KF, Altman, DG, and Moher, D. Consort 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ (Clinical research ed). (2010) 340:c332. doi: 10.1136/bmj.c332
16. Guyatt, GH, Oxman, AD, and Vist, GE. Grade: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed). (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
17. Bao, X, Li, L, and Liu, H. Effect of acupuncture combined with rehabilitation on cognitive and motor functions in Poststroke patients. Anat Rec. (2021) 304:2531–7. doi: 10.1002/ar.24700
18. Jiang, C, Yang, SL, and Tao, J. Clinical efficacy of acupuncture treatment in combination with Rehacom cognitive training for improving cognitive function in stroke: a 2 X 2 factorial design randomized controlled trial. J Am Med Dir Assoc. (2016) 17:1114–22. doi: 10.1016/j.jamda.2016.07.021
19. Xiong, J, Zhang, Z, and Ma, Y. The effect of combined scalp acupuncture and cognitive training in patients with stroke on cognitive and motor functions. NeuroRehabilitation. (2020) 46:75–82. doi: 10.3233/nre-192942
20. Bai, JLB, and Tang, Q. Effect of cluster needling of scalp point combined with cognitive Trajning on cognitive impairment after cerebral infarction. Chin J Rehabil Med. (2012) 27. doi: 10.3870/zgkf.2012.05.003
21. Y, P. Analysis of the effect of acupuncture on cognitive dysfunction after cerebral infarction. Shenzhen J Integr Med.. (2018) 28. doi: 10.16458/j.cnki.1007-0893.2018.24.016,
22. Qq, C. Efficacy of acupuncture combined with cognitive rehabilitation training for post-stroke cognitive impairment and its effect on cytokines. Reflexology Rehabil Med. (2020) 5. doi: 10.19589/j.cnki.issn2096-7950.2020.09.045
23. Zeng, LLZX, and Huang, Z. Clinical effects of Jin’s 3-needle combined with cognitive rehabilitation training in the treatment of convalescent cerebral apoplexy with cognitive impairment. Shandong. J Tradit Chin Med. (2018) 37. doi: 10.16295/j.cnki.0257-358x.2018.05.005
24. Chen, AZLZ, and Lan, L. Effect of prolonged head-acupuncture combined with cognitive rehabilitation training platform on cognitive function after stroke. Chinese J Rehabilitation Med. (2020) 5. doi: 10.19787/j.issn.1008-1879.2020.06.009
25. Fx, LJ. Electroacupuncture of Baihui and Shenting points with rehabilitation training clinical study on cognitive impairment after stroke. Chin Med. J. (2013) 28:608–10. doi: 10.16368/j.issn.1674-8999.2013.04.020
26. Chen, XYNQ. Effect of acupuncture combined with rehabilitation training on cognitive dysfunction and serum cytokines in stroke patients. Reflexology Rehabil Med. (2020) 29:40–2. doi: 10.19589/j.cnki.issn2096-7950.2020.13.040
27. Ding, XZH. Effect of head injection combined with motor relearning on cognitive impairment in post-stroke patients. Hebei Chin Med. (2016) 38. doi: 10.3969/j.issn.1002-2619.2016.04.033
28. Du, RRZY. The efficacy of acupuncture therapy combined with occupational function training on cognitive dysfunction after ischemic stroke. Chinese J Rehabilitation Med. (2019) 10. doi: 10.19787/j.issn.1008-1879.2019.02.006
29. Duan, LZZX. Study on the effect of combining rehabilitation training with nourishing kidney and marrow acupuncture in patients with cognitive impairment after stroke. Heilongjiang Med J. (2021) 45. doi: 10.3969/j.issn.1004-5775.2021.20.004
30. Feng, XDWM. Clinical efficacy of supervised Moxibustion on post-stroke cognitive impairment. Chin J Rehabil Theory Pract. (2014) 20. doi: 10.3969/j.issn.1006-9771.2014.10.015
31. Han, HYWZ. The effect of scalp acupuncture combined with cognitive training on cognitive dysfunction after stroke. J Med Inform. (2021) 34. doi: 10.3969/j.issn.1006-1959.2021.15.050
32. Jx, H. Clinical observation of 40 cases of cognitive dysfunction after cerebral hemorrhage treated with warm acupuncture. J Ethnobiol Ethnomedicine. (2019) 28:102–104.
33. Niu, LQH. Cognitive function training combined with long stay acupuncture at head point series clinical study on cognitive dysfunction after cerebral infarction. Res Integrat Tradition Chin Western Med. (2021) 13:377–80. doi: 10.3969/j.issn.1674-4616.2021.06.005
34. Kong, YFQH, and Niu, YQ. Clinical study on cognitive dysfunction after cerebral infarction treated with cephalic plexus acupuncture and long stay acupuncture with cognitive function training. J Tradit Chin Med. (2021) 37:1464–1466.
35. Leng, JWF, and Guo, W. Efficacy of long-time Moxibustion "Baihui" for post-stroke urinary incontinence with cognitive Dysfunction. Rehabil Med. (2020) 30:103–7. doi: 10.3724/SP.J.1329.2020.02004
36. Chen, LZWJ, and Wang, LJ. Acupuncturing five Zang -organs Yu combined with head-needling for cognitive function after stroke and the influence of plasma homocysteine. JCAM. (2016) 9:88–90. doi: 10.16808/j.cnki.issn1003-7705.2016.09.041
37. Q, L. Curative effect observation of warm needling method on patients with cognitive impairment after stroke. China Med Dev Inform. (2017) 23. doi: 10.15971/j.cnki.cmdi.2017.20.002
38. Lin, BRL, and Yao, JM. Clinical effects of acupuncture with rehabilitation training for cognitive dysfunction after cerebral infarction. Chronic Pathematology J. (2020) 20. doi: 10.16440/j.cnki.1674-8166.2020.01.056
39. Lin, ZCCL, and Tao, J. Effect of Electroacupuncture at Baihui point on auditory P300 in patients with cognitive impairment after cerebral infarction. Shanghai J Acupuncture Moxibustion. (2014) 33. doi: 10.13460/j.issn.1005-0957.2014.01.0014
40. Qian, LFYQ, and Luo, KT. The effect of Bai Changliu acupuncture with rehabilitation training on ischemic stroke with cognitive dysfunction in qi deficiency and blood stasis type. Shanghai J Acupuncture Moxibustion. (2018) 37. doi: 10.13460/j.issn.1005-0957.2018.05.0499
41. Feng, XDFH. Effective observation of ear Acupoint bloodletting combined with rehabilitation training on cognitive impairment after stroke. CJCM. (2015) 7:49–50. doi: 10.3969/j.issn.1674-7860.2015.14.025
42. Song, YZF, and Huang, WH. Therapeutic observation of acupuncture based on brain-kidney correlated theory combined with rehabilitation training for post-stroke cognitive impairment. Shanghai J Acupuncture Moxibustion. (2020) 39. doi: 10.13460/j.issn.1005-0957.2020.06.0657
43. Xq, S. Analysis of the therapeutic effect of nourishing the kidney and benefiting the marrow acupuncture method with rehabilitation training on patients with cognitive impairment after stroke. Modern Drug Applications China. (2019) 13. doi: 10.14164/j.cnki.cn11-5581/r.2019.05.093
44. Tan, SLX, and Liu, CQ. Effect evaluation of acupuncture and rehabilitation training on cognitive dysfunction after cerebral infarction. Clinical Res Chin Med. (2020) 12. doi: 10.3969/j.issn.1674-7860.2020.06.034
45. Sh, G. Evaluation of the efficacy of acupuncture with rehabilitation training in the treatment of cognitive dysfunction after cerebral infarction. China Foreign Med Treat. (2016) 18:167–8. doi: 10.16662/j.cnki.1674-0742.2016.18.167
46. Tian, YLSY, and Feng, XY. The efficacy of acupuncture combined with cognitive rehabilitation training in the treatment of post-stroke cognitive dysfunction. Clin Med. (2021) 41. doi: 10.19528/j.issn.1003-3548.2021.01.049
47. Wang, CXLX, and Yu, KF. Effect of ventral acupuncture combined with early rehabilitation training on motor function and cognitive impairment in patients with cerebrovascular disease. Modern J Integrat Chin Western Med. (2015) 24. doi: 10.3969/j.issn.1008-8849.2015.19
48. Wang, FGS, and Yang, L. Efficacy of acupuncture combined with cognitive training for cognitive dysfunction after ischemic stroke. Shanghai J Acupuncture Moxibustion. (2021) 40. doi: 10.13460/j.issn.1005-0957.2021.07.0795
49. Wang, HZY, and Cai, SF. Effect of indwelling scalp acupuncture combined with occupational therapy on patients with cognitive dysfunction after stroke. J Neurol Neurorehabil. (2021) 17. doi: 10.12022/jnnr.2020-0092
50. Wang, HLFX, and Chen, Z. Clinical efficacy of electro-acupuncturing on Baihui and Zusanli points plus rehabilitation training on post-stroke cognitive impairment. Clinic Res Chin Med. (2017) 9. doi: 10.3969/j.issn.1674-7860.2017.05.035
51. Wang, LNFX, and Liu, CM. Effect of needle warming Moxibustion on cognitive dysfunction after stroke. Chin J Rehabil Theory Pract. (2015) 21. doi: 10.3969/j.issn.1006-9771.2015.02.018
52. Wang, WLX, and Zhu, LS. Effect of long-time indwelling needle of Sculp acupuncture at early stage combined with rehabilitation training on cognitive disorder of stroke patients. J Tradit Chin Med. (2018) 50. doi: 10.13457/j.cnki.jncm.2018.03.044
53. Wang, YZL, and Li, SR. Effect of cranial acupuncture plexus combined with cognitive training on cognitive dysfunction in patients with cerebral infarction. Theory Prac Rehabil China. (2011) 17:316–318. doi: 10.3969/j.issn.1006-9771.2011.04
54. Lei, YFZG. Effect of computer-assisted cognitive training combined with Ziwu-Liu injection acupuncture on the rehabilitation effect of cognitive dysfunction after stroke. J External Therapy TCM. (2021) 4:72–4. doi: 10.3969/j.issn.1006-978X.2021.04.031
55. Wang, YXMW, and Zhang, HS. Effect of cluster needling of scalp acupuncture combined with cognitive rehabilitation on cognitive impairment after cerebral infarction. Chin Med Herald. (2018) 24. doi: 10.13862/j.cnki.cn43-1446/r.2018.17.025
56. Wang, ZGZH, and Wang, XW. Efficacy of acupuncture plus cognitive rehabilitation training for post-stroke cognitive impairment and its effect on cytokines. Shanghai J Acupuncture Moxibustion. (2019) 38. doi: 10.13460/j.issn.1005-0957.2019.10.1098
57. Zj, Z. Evaluation of the efficacy of acupuncture with rehabilitation training in the treatment of cognitive dysfunction after cerebral infarction. Heilongjiang Trad Chin Med. (2021) 4:94–5.
58. Wei, RPZJ, and Cong, WD. Analysis of the efficacy of acupuncture for cognitive function and Nhiss and Adl scores after cerebral infarction. Jilin Chin Med. (2019):10. doi: 10.13463/j.cnki.jlzyy.2019.10.029
59. Zhao, JYGY. Clinical efficacy of auricular Acupoint therapy combined with Zhisan acupuncture and Cephalopuncture in patients with cognitive dysfunction after stroke. RARM. (2021) 2:7–9.
60. Xu, WXFL, and Luo, JC. Effect of acupuncture at eight points of the nape combined with cognitive rehabilitation training for patients with post-stroke cognitive impairment. J Nurs Sci. (2022) 37. doi: 10.3870/j.issn.1001-4152.2022.14.050
61. Zheng, CJXW, and Duan, C. Combination of acupuncture and computer-assisted cognitive training for post-stroke cognitive dysfunction: a randomized controlled study. Chin Acupuncture Moxibustion. (2021) 41:247–51. doi: 10.13703/j.0255-2930.20200311-k0001
62. Yan, HLZC, and Wu, HB. Clinical observation on cognitive impairment after stroke treated with Moxibustion and Moxibustion of the Duoyuan Group of Points Combined with cognitive function training. J Anhui Univ Trad Chin Med. (2022) 41. doi: 10.3969/j.issn.2095-7246.2022.03.011
63. Yang, FLK, and Yang, XB. Clinical observation of long-time needle retaining at Baihui (Gv 20) on post-stroke cognitive disorder of qi deficiency and blood stasis. Chin Acupuncture Moxibustion. (2018) 38:1151–6. doi: 10.13703/j.0255-2930.2018.11.004
64. Gd, Y. Observation of clinical efficacy of acupuncture combined with cognitive rehabilitation training for cognitive dysfunction in stroke patients and the effect on serum cytokines. Reflexology Rehabil Med. (2020):8. doi: 10.19589/j.cnki.issn2096-7950.2020.08.024
65. Zhou, JRWB. A randomized controlled study on the effect of Tongdu and Tonifying acupuncture on the cognitive function of patients after stroke. J External Therap TCM. (2021) 30:26–7. doi: 10.3969/j.issn.1006-978X.2021.05.012
66. Yang, YZH. Clinical efficacy and impact on daily living activities of cognitive dysfunction after stroke treated with acupuncture method of Tonifying kidney and benefiting marrow together with rehabilitation training. Clin J Acupuncture Moxibustion. (2019) 35:24–27. doi: 10.3969/j.issn.1005-0779.2019.07.008
67. Yao, JJLS, and Yu, JF. Acupuncture combined with cognitive rehabilitation training for cognitive dysfunction after ischemic stroke. Asia-Pacific Trad Med. (2019) 15. doi: 10.11954/ytctyy.201909040
68. Yao, RGZ, and Zhang, KW. Clinical study of Jin san acupuncture therapy for post-stroke cognitive impairment. Acupuncture Tuina Med. (2020) 18:40–6. doi: 10.1007/s11726-020-1155-2
69. Yu, LYCM, and Ma, M. Effect of Bo’s abdominal acupuncture therapy on the resting-state Fmri in patients with cognitive impairment after stroke. Shanghai J Acupuncture Moxibustion. (2021) 40. doi: 10.13460/j.issn.1005-0957.2021.11.1293
70. Zhan, JPR, and Guo, YH. Acupuncture of Baihui and Shenting combined with basic treatment and conventional rehabilitation for cognitive impairment after stroke: a randomized controlled study. Chin Acupuncture Moxibustion. (2016) 36. doi: 10.13703/j.0255-2930.0216.08.007
71. Zhang, JBWR, and Yang, H. Head acupuncture combined with computer-assisted training for cognitive impairment after cerebral infarction in the elderly magnetic resonance spectroscopy imaging. Chin J Gerontol. (2020) 40. doi: 10.3969/j.issn.1005-9202.2020.19.011
72. Zhang, JZL, and Chen, XY. Clinical efficacy of nourishing the kidney and benefiting the marrow acupuncture method with rehabilitation training in 65 cases of post-stroke cognitive impairment. World J Int Chin Western Med. (2018) 13. doi: 10.13935/j.cnki.sjzx.180318
73. Zhang, YYSB, and Huang, GL. The efficacy of Sanjiao acupuncture combined with computer-assisted cognitive training in the treatment of cognitive impairment after acute stroke. Shandong. J Tradit Chin Med. (2019) 38. doi: 10.16295/j.cnki.0257-358x.2019.12.007
74. Zheng, MJY, and Chen, Y. Exploration of Tongdu Yiyang Moxibustion on improving cognitive dysfunction after cerebral infarction based on event-related electric potential P300. Acta Chin Med. (2019) 34:1546–50. doi: 10.16368/j.issn.1674-8999.2019.07.366
75. Zhou, HXQZ, and Kong, YF. Clinical study on cognitive impairment after ischemic stroke treated with eye acupuncture combined with cognitive function training. J Pract Tradit Chin Med. (2022) 38:711–733.
76. Zhuo, JBZC, and Zhang, LY. Clinical study of heart-brain acupuncture method combined with cognitive rehabilitation to improve cognitive impairment during recovery from cerebral infarction. Yunnan. J Tradit Chin Med. (2021) 42:24–27. doi: 10.3969/j.issn.1007-2349.2021.06.008
77. Zhou, LZZ. Evaluation of the efficacy of acupuncture with rehabilitation training in the treatment of cognitive dysfunction after cerebral infarction. RARM. (2020) 1:7–9.
78. Zhu, YLHC, and Xing, JL. 4o cases of post-stroke cognitive dysfunction treated with the "treatment from the governor" method of acupuncture. J Anhui Univ Chinese Med. (2014) 33:50–2. doi: 10.3969/j.issn.20957246.2014.02.019
79. van der Flier, WM, Skoog, I, and Schneider, JA. Vascular Cognitive Impairment. Nat Rev Dis Primers. (2018) 4:18003. doi: 10.1038/nrdp.2018.3
80. Yao, S, Liu, Y, and Zheng, X. Do nonpharmacological interventions prevent cognitive decline? A systematic review and Meta-analysis. Transl Psychiatry. (2020) 10:19. doi: 10.1038/s41398-020-0690-4
81. Wonderling, D, Vickers, AJ, and Grieve, R. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ (Clinical research ed). (2004) 328:747. doi: 10.1136/bmj.38033.896505.EB
82. Kong, LHSG, and Liu, SH. Effect of acupuncture on the expression and content of nuclear transcription factor-Κb in hippocampal tissue of rats with cerebral ischemia-reperfusion. Acupuncture Res. (2006) 31:140–4+93. doi: 10.13702/j.1000-0607.2006.03.003
83. Gao, MLB, and Tan, X. Effects of acupuncture Baihui and Sishencong on learning memory ability and cell apoptosis in ischemia-reperfusion injury model rats. World Chin Med. (2021) 16:1226–30. doi: 10.3969/j.issn.1673-7202.2022.08.009
84. Xu, SYLW, and Hong, H. Effect of acupuncture on the expression of autophagy-related proteins Lc3-ii and Beclin1 in cerebral ischemia-reperfusion rats. J Nanjing Univ Chin Med. (2021) 37:270–4. doi: 10.14148/j.issn.1672-0482.2021.0270
85. Xie, ZRXD, and Tang, YN. Effect of acupuncture on the expression of Synaptophysin and postsynaptic Mitogen-95 in serum and brain tissue of Mcao rats. China J Trad Chin Med Inform. (2021) 28:81–5. doi: 10.19879/j.cnki.1005-5304.202005293
86. Zhang, YKTL. Effects of acupuncture on learning memory ability and vascular endothelial growth factor expression in cerebral ischemia-reperfusion rats. J Huazhong Univ Sci Technol. (2013) 42:70–3.
Keywords: acupuncture treatment, post-stroke cognitive impairment, cognitive rehabilitation, non-pharmacological treatment, network meta analysis
Citation: Liu Y, Zhao L, Chen F, Li X, Han J, Sun X and Bian M (2023) Comparative efficacy and safety of multiple acupuncture therapies for post stroke cognitive impairment: a network meta-analysis of randomized controlled trials. Front. Neurol. 14:1218095. doi: 10.3389/fneur.2023.1218095
Edited by:
P. Hemachandra Reddy, Texas Tech University Health Sciences Center, United StatesReviewed by:
Aihong Yuan, First Affiliated Hospital of Anhui University of Traditional Chinese Medicine, ChinaQi AN, The Second Affiliated Hospital, Guangdong Provincial Hospital of Chinese Medicine, China
Copyright © 2023 Liu, Zhao, Chen, Li, Han, Sun and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fuyan Chen, ZWNmeV8yMDA1QDE2My5jb20=
†These authors have contributed equally to this work
 Yang Liu
Yang Liu Lu Zhao1,2†
Lu Zhao1,2† Xingping Li
Xingping Li