- 1Department of Nursing, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
- 2Nursing College of Shanxi Medical University, Taiyuan, China
Objective: The incidence of post-stroke cognitive impairment (PSCI) has increased alongside the rising prevalence of stroke, making it one of the most serious and prevalent complications among stroke survivors. Growing interest has emerged in whether combined or multi-modal therapies can enhance outcomes through additive or synergistic effects, leading more researchers to investigate the efficacy of transcranial direct current stimulation (tDCS) combined with cognitive rehabilitation (CR) in this population. This study aims to systematically review and meta-analyze the effects of tDCS combined with CR on cognitive function and activities of daily living (ADL) in individuals with PSCI.
Methods: PubMed, Web of Science, Cochrane Library, Embase and China National Knowledge Infrastructure (CNKI) were systematically searched for articles published from inception of the databases through June 2024. Two independent authors screened studies and extracted data. The methodological quality of the included randomized controlled trials (RCTs) was evaluated with the Cochrane Risk of Bias Tool. Meta-analyses were performed using R statistical software (version 4.1.2).
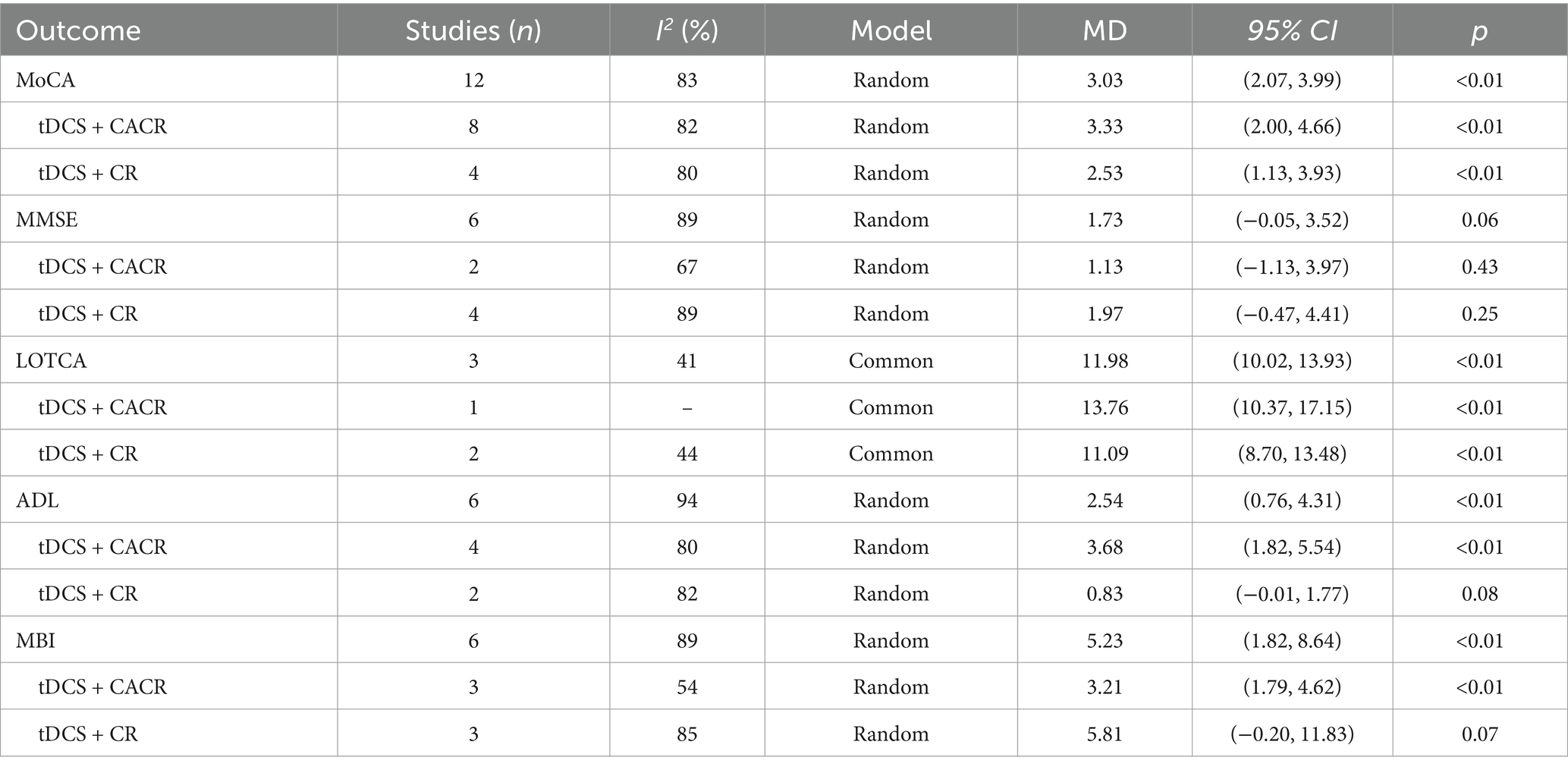
Results: A total of 663 participants across 11 RCTs published between 2013 and 2024 were included. The meta-analysis results indicated that tDCS combined with CR significantly improved cognitive function and ADL among PSCI patients compared to the control group, as evidenced by the Montreal Cognitive Assessment test (MoCA) (MD = 3.03, 95% confidence interval = 2.07 ~ 3.99, p < 0.0001), Mini-Mental State Examination (MMSE) (MD = 1.73, 95% confidence interval = −0.05 ~ 3.52, p < 0.05), Loewenstein Occupational Therapy Cognitive Assessment (LOTCA) (MD = 11.98, 95% confidence interval = 10.02 ~ 13.93, p < 0.0001), Activity of Daily Living Scale (ADLs) (MD = 2.54, 95% confidence interval = 0.76 ~ 4.31, p < 0.05), and Modified Barthel Index (MBI) (MD = 5.23, 95% confidence interval = 1.82 ~ 8.64, p < 0.01). Subgroup analysis results revealed that tDCS combined with computer-assisted cognitive rehabilitation (CACR) had a greater positive impact on ADL.
Conclusion: tDCS combined with CR significantly improves cognitive function and ADL among individuals with PSCI. Compared with conventional cognitive rehabilitation, the computer-assisted approach demonstrates greater effectiveness in improving ADL among PSCI patients.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier [CRD42024561767].
Introduction
The Global Burden of Disease (GBD) Study 2021 revealed significant global stroke statistics, 11.9 million new stroke cases, 93.8 million existing cases, and 7.3 million stroke-related deaths worldwide (1). Post-stroke cognitive impairment (PSCI) is a clinical condition characterized by cognitive deficits that emerge within 6 months following a stroke. It is recognized as one of the most prevalent and severe complications of stroke (2, 3). Current epidemiological data show significant variability in PSCI prevalence estimates, with reported rates ranging from 18.0 to 70.0% (4). The long-term functional impairment caused by PSCI often surpasses the initial brain injury, significantly affecting daily activities, rehabilitation progress, and overall prognosis, making it difficult for patients to reintegrate into family and social settings. Furthermore, it heightens the risk of recurrent vascular events, imposing a substantial burden on patients, caregivers, and healthcare systems (5–7).
Current PSCI treatments encompass both pharmacological and non-pharmacological approaches. However, pharmacotherapy often shows limited efficacy and is associated with various adverse effects (8). For example, prolonged use of acetylcholinesterase inhibitors may cause gastrointestinal issues (e.g., diarrhea, constipation), hepatotoxicity, and systemic symptoms such as insomnia and fatigue (9). Consequently, this treatment dilemma has propelled increased research attention toward non-pharmacological interventions such as acupuncture, transcranial magnetic stimulation (TMS), transcranial direct current stimulation (tDCS), and cognitive rehabilitation (CR), which have gained increased scholarly interest (10). Recent studies suggest that tDCS is a more potent non-invasive brain stimulation method compared to TMS (10). It has been shown to alter cortical excitability during stimulation by modulating neuronal resting membrane potentials (11) and to induce neuroplastic effects via prolonged stimulation through glutamatergic synaptic mechanisms (10). tDCS shows significant potential for treating motor dysfunction, mood disorders, and cognitive and speech disorders in stroke patients, owing to its safety, cost-effectiveness, and ease of use (12).
In recent years, tDCS combined with CR has emerged as a focal point of research, with growing interest in whether combined or multi-modal therapies could enhance outcomes through additive or synergistic effects (13–16). Nevertheless, existing research remains controversial regarding whether the combined interventions can achieve the expected effect (17, 18). Currently, the systematic review of tDCS therapy for patients with PSCI has largely overlooked the impact of tDCS combined with CR treatment on these patients (19). Consequently, a comprehensive systematic review and synthesis of the available evidence may be necessary to address this gap and provide clinical staff with the latest evidence-based insights for managing cognitive impairment in stroke patients. This systematic review and meta-analysis aims to evaluate the impact of tDCS combined with CR on both cognitive function and activities of daily living (ADL) in patients with PSCI.
Materials and methods
This systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered with the PROSPERO database (CRD42024561767) (20).
Search strategy
In accordance with the PRISMA Statement, this study conducted a comprehensive literature search to investigate the effects of tDCS combined with CR on the rehabilitation of patients with PSCI. Databases searched included PubMed, Web of Science, Cochrane Library, Embase, and China National Knowledge Infrastructure (CNKI), covering all entries up to June 2024. The search terms included “transcranial direct current stimulation,” “cognitive rehabilitation,” “cognitive rehabilitation training,” “cognitive training,” “stroke,” “post-stroke,” and “cognitive impairment.” These terms were combined using the Boolean operators “OR” and “AND” to construct a comprehensive search strategy.
Inclusion and exclusion criteria
Eligible studies were required to meet the following inclusion criteria: (1) P (Population) – Stroke patients with cognitive impairment confirmed by cognitive function assessment, where cognitive impairment was caused by stroke rather than other diseases. (2) I (Intervention) – tDCS combined with CR administered in either sequential or synchronized formats. (3) C (Comparison) – tDCS alone; sham tDCS alone; sham tDCS with CR; CR alone; or passive control (i.e., usual care or no treatment). (4) O (Outcomes) – Indicators of cognitive functioning include the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA) and Loewenstein Occupational Therapy Cognitive Assessment (LOTCA), as well as indicators of ADL, which include the Activity of Daily Living Scale (ADLs) and Modified Barthel Index (MBI). (5) S (Study design) – RCTs.
Exclusion criteria included: (1) Publications in languages other than English or Chinese. (2) Interventions involving additional therapies beyond tDCS and CR that could influence cognitive outcomes (e.g., reminiscence). (3) Animal studies, conference abstracts, protocols, quasi-experimental studies, or case reports. (4) Studies with inaccessible full texts or non-public outcome data.
Study selection and data extraction
Two investigators (LN and YF) independently conducted literature screening in strict accordance with the established inclusion and exclusion criteria. They independently extracted data using a pre-defined checklist that included publication details (year, country, and authors), participant information (sample size, age, and gender), intervention details (characteristics of both the intervention and control groups, frequency of intervention, and duration of follow-up), and outcome measures (cognitive functioning and daily living skills). Any disagreements were resolved through discussion or by involving a third team member (YM).
Quality assessment
Two researchers (LN and CL) independently assessed the risk of bias in the included studies using the Cochrane “Risk of Bias” tool (21), which evaluates selection, performance, detection, attrition, reporting, and other biases. Each study was rated as having a low, unclear, or high risk of bias. In cases of discrepancies, a third reviewer (JB) was consulted.
Statistical analysis
The meta-analysis was performed using R statistical software (version 4.1.2). Odds ratios (OR) were used for categorical variables, while mean differences (MD) or standardized mean differences (SMD) were utilized for continuous data. All effect sizes were reported with 95% confidence intervals (95% CI). Heterogeneity among the studies was assessed using the I2 statistic with corresponding p-values, where p ≥ 0.1 and I2 ≤ 50% indicated no significant heterogeneity, prompting the use of a fixed-effect model. Otherwise, a random-effects model was employed for the analyses. Subgroup analyses were performed as needed to explore potential sources of heterogeneity. When the number of included studies exceeded 10, a funnel plot and Egger’s test were used to assess publication bias. Sensitivity analyses were conducted to evaluate the stability and reliability of the results. p < 0.05 was considered statistically significant.
Result
Literature search results
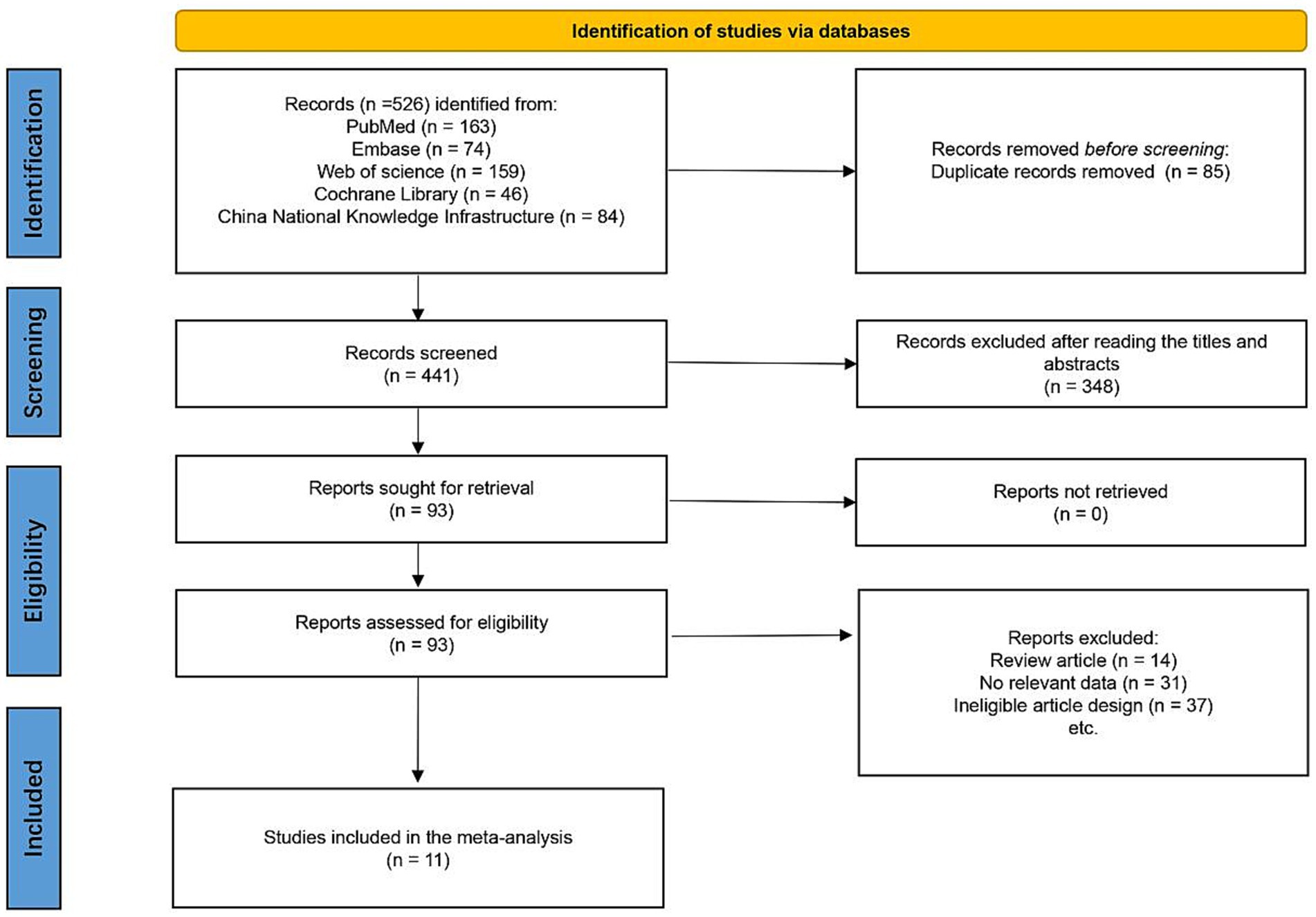
As illustrated in Figure 1, a total of 526 studies were initially retrieved. Among these, 85 were duplicates, and 348 studies were excluded after screening the titles and abstracts. During the full-text review, 82 studies were excluded for not meeting the inclusion criteria, resulting in 11 studies being included in the systematic review (13, 15–18, 22–27).
The basic characteristics of the included literature
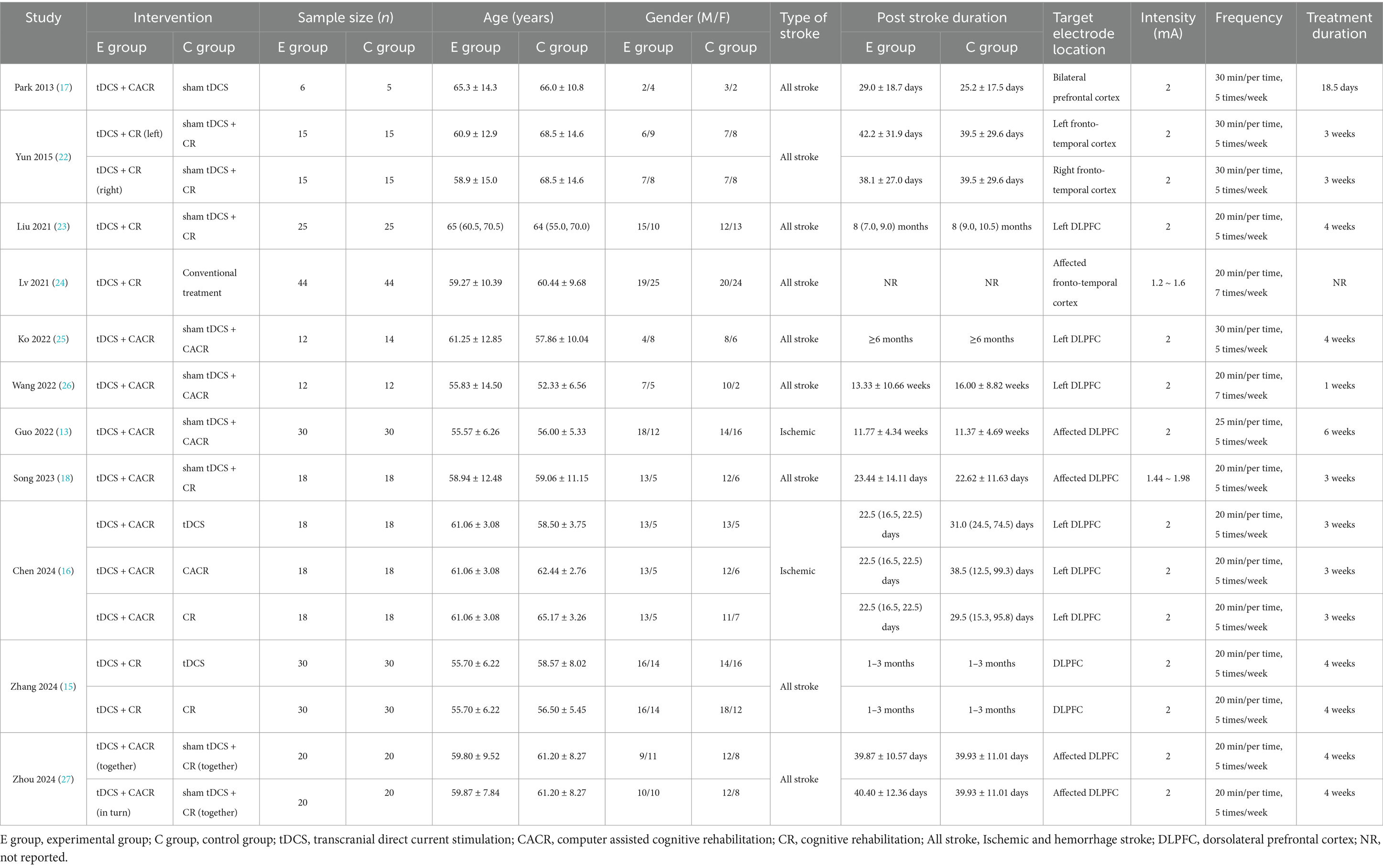
Table 1 summarizes the characteristics of the included studies. The publication years ranged from 2013 to 2024, with over 81.8% of these studies published after 2020. The total sample size of 663 was included, with individual study sample sizes ranging from 11 to 88. Of these, 331 patients were assigned to the experimental group and 332 to the control group. Interventions in the experimental group consisted of tDCS combined with CR or computer-assisted cognitive rehabilitation (CACR). The control group included standalone tDCS, sham tDCS, CR, CACR, sham tDCS combined with CR, sham tDCS combined with CACR, or conventional treatment.
Quality evaluation of included literature
Figure 2 presents the quality evaluation of the included literature. Out of the 11 randomized controlled trials, three studies were classified as having a low risk of bias, while eight studies had some concerns. Specifically, regarding potential bias in the randomization process, of the 11 studies that were described as randomized, four studies (17, 18, 22, 25) had an uncertain risk due to mentioning randomness without specifying the method, while the remaining seven (13, 15, 16, 23, 24, 26, 27) employed the random number table method, indicating a low risk. For the allocation concealment, three studies (27.27%) (16, 23, 26) showed a low risk of bias, while eight studies (72.73%) (13, 15, 17, 18, 22, 24, 25, 27) did not provide information on whether participants were blinded to group allocation, raising some concerns in this domain. Regarding blinding, six articles (15, 16, 22, 23, 26, 27) demonstrated a low risk, whereas five articles (13, 17, 18, 24, 25) did not mention blinding and were considered to have an uncertain risk. Overall, the quality of the included studies was relatively high.
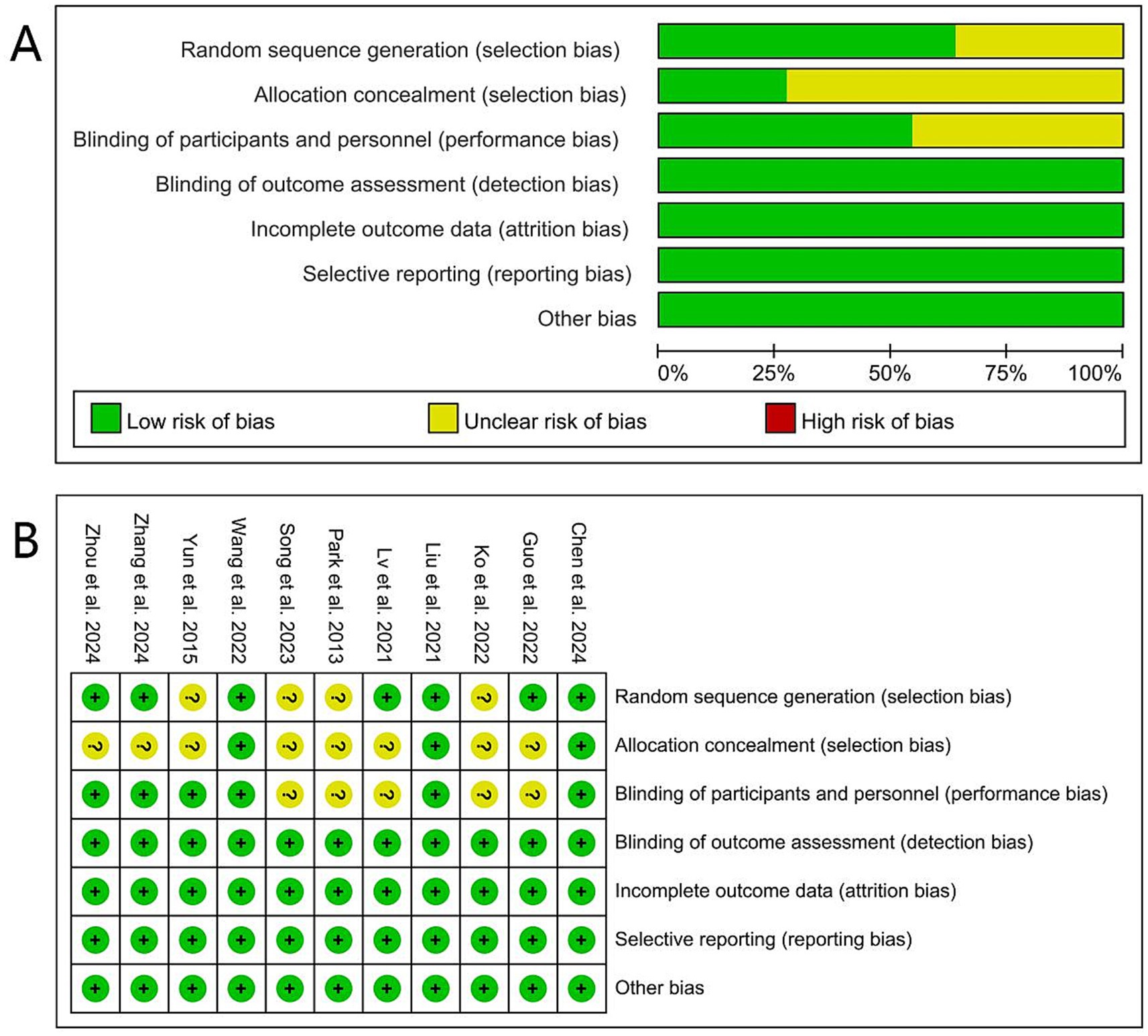
Figure 2. Risk of bias summary and graph: (A) The risk of bias profile across. (B) The detailed results of the risk of bias.
Effects of tDCS combined with CR versus control
Cognitive function
MoCA
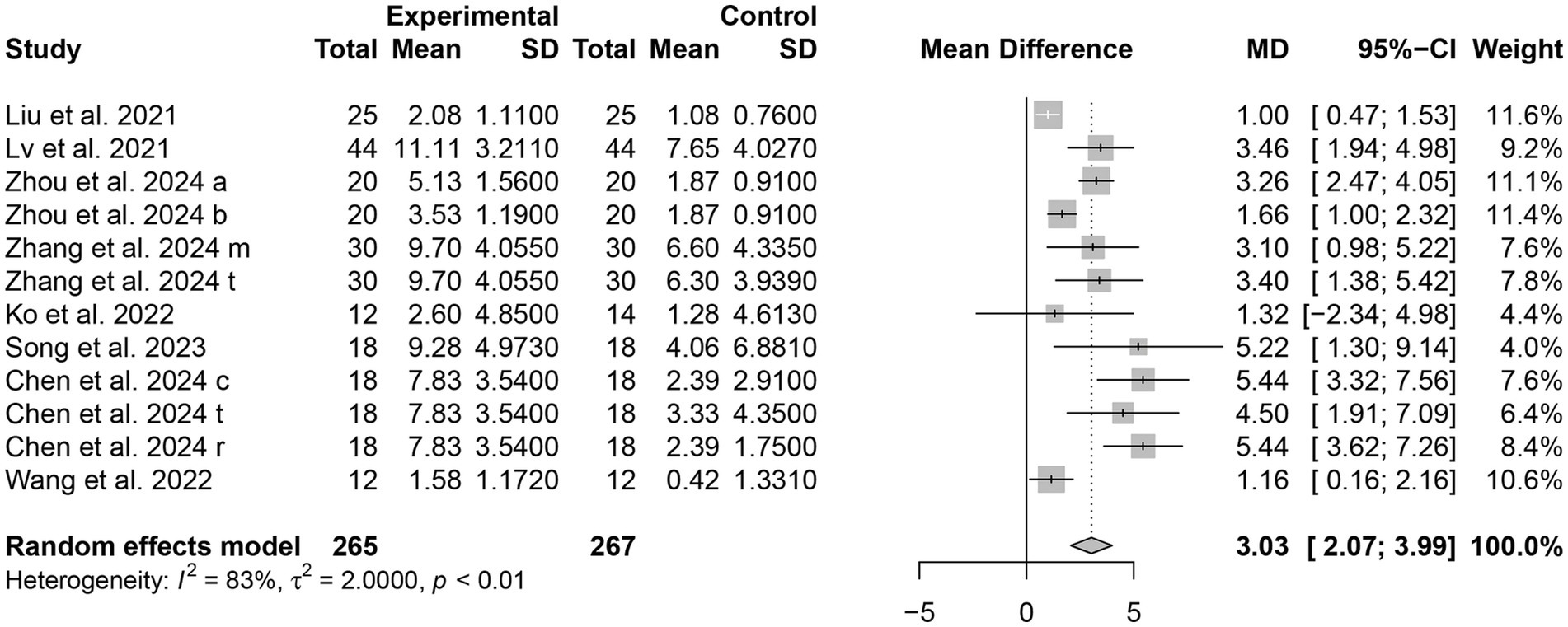
There are eight studies (15, 16, 18, 23–27) involving a total of 532 patients that assessed the scores of MoCA as an outcome. The results showed that MoCA scores were better in the tDCS combined with the CR group compared to the control group, with a statistically significant difference [MD = 3.03, 95% CI (2.07, 3.99), I2 = 83%, p < 0.0001] (Figure 3).
MMSE
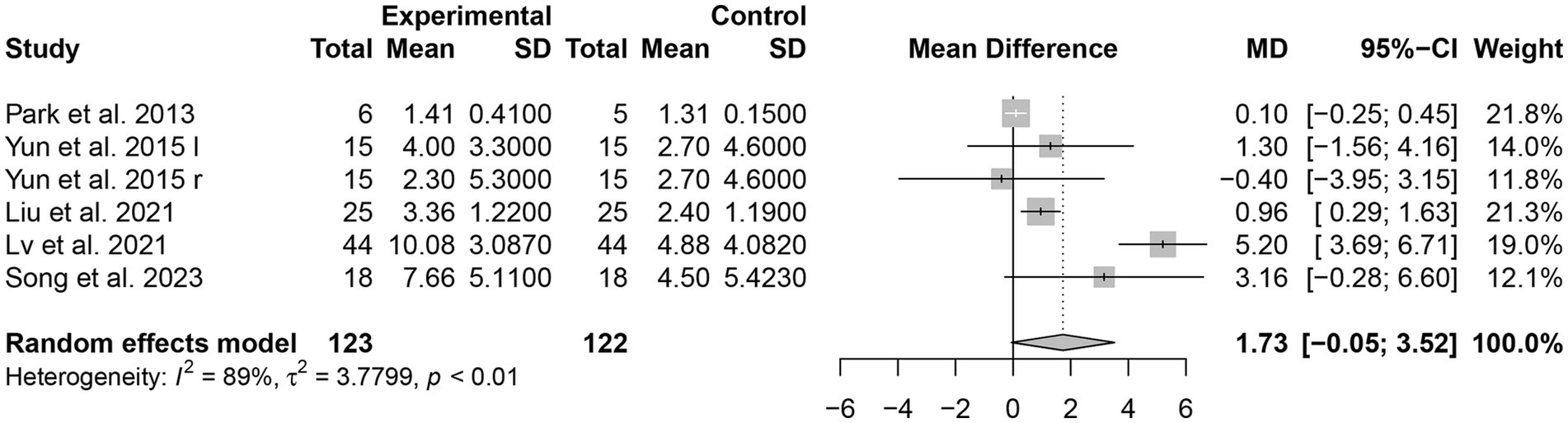
The effect of tDCS combined with CR intervention on the score of MMSE was evaluated in five studies (17, 18, 22–24) involving 245 patients. tDCS combined with CR demonstrated a significant effect on MMSE scores in patients with PSCI [MD = 1.73, 95% CI (−0.05, 3.52), I2 = 89%, p < 0.05] (Figure 4).
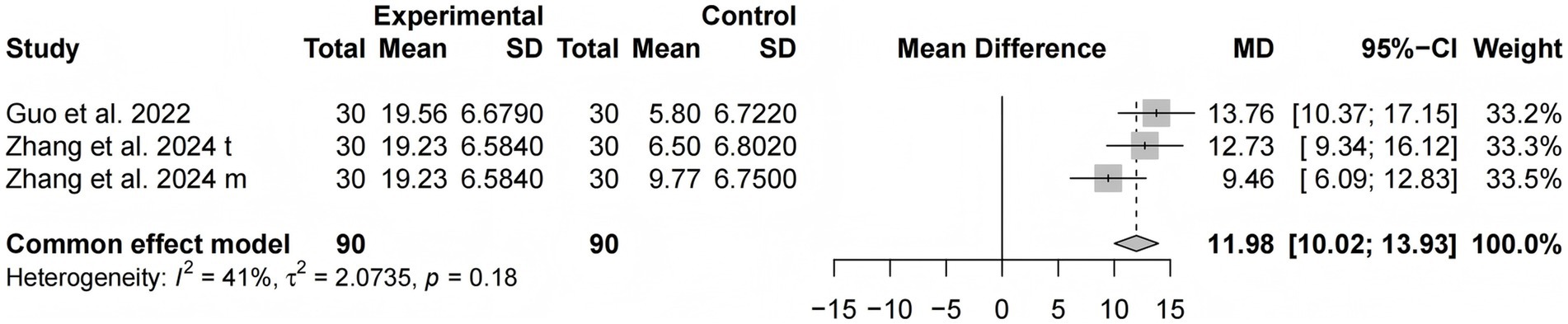
LOTCA
Two studies (13, 15) involving 180 participants used the LOTCA to evaluate cognitive function. The results of the meta-analysis revealed that the LOTCA scores in the tDCS combined with the CR group were significantly higher than those of the control group [MD = 11.98, 95% CI (10.02, 13.93), I2 = 41%, p < 0.0001] (Figure 5).
ADL
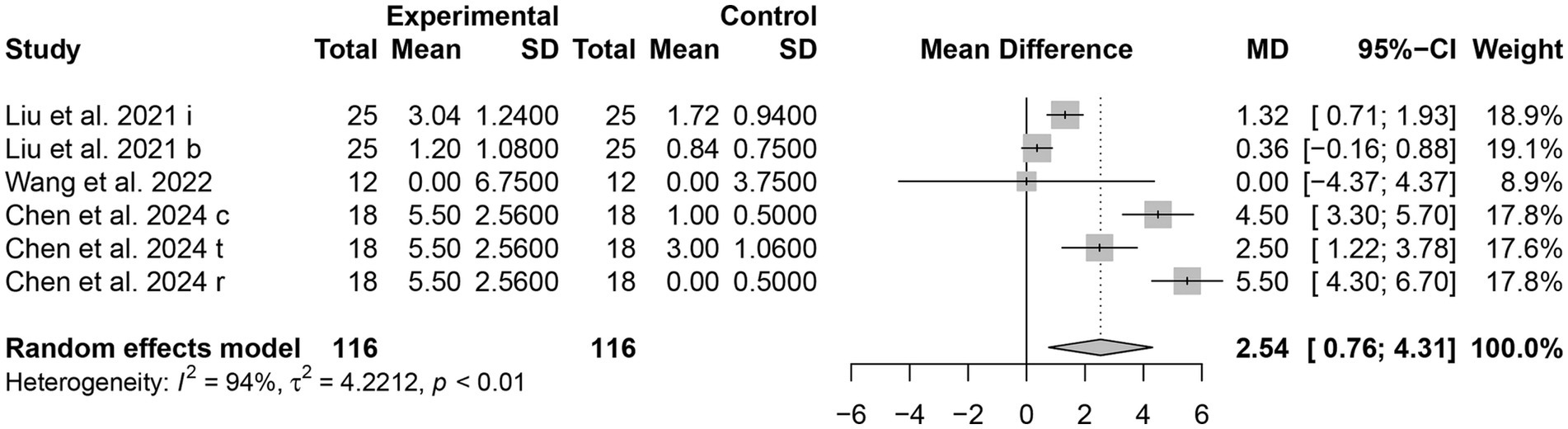
ADLs
Three trials (16, 23, 26) reported using ADLs as an outcome index. A total of 232 patients were included, with 116 in the tDCS combined with the CR group and 116 in the control group. The score of ADLs in the tDCS combined with CR group was significantly higher than those in the control group [MD = 2.54, 95% CI (0.76, 4.31), I2 = 94%, p < 0.05] (Figure 6). This indicates that the ADL of PSCI patients in the experimental group showed significant improvement.
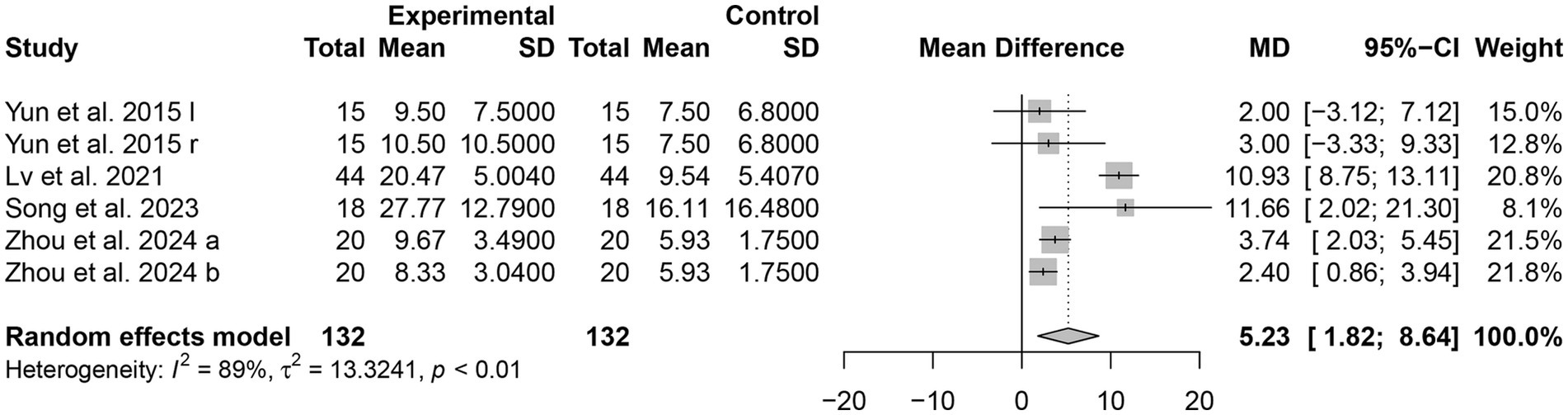
MBI
Four studies (18, 22, 24, 27) used the MBI score as an outcome indicator. The heterogeneity test shows that there is significant heterogeneity among the included studies (I2 = 89%, p < 0.01), prompting the use of a random-effect model for analysis. This indicates that the efficacy of the experimental group was significantly better than that of the control group, with a statistically significant difference [MD = 5.23, 95% CI (1.82, 8.64), p < 0.01] (Figure 7).
Subgroup analysis
We performed a subgroup analysis of the included studies according to the forms of CR and CACR. The analysis indicated that tDCS combined with CACR was superior to tDCS combined with CR in terms of MoCA, LOTCA, ADLs and MBI scores (Table 2).
Sensitivity analysis
We removed these studies one by one during the sensitivity analysis to assess the stability and reliability of the merger results. The results of the sensitivity analyses are presented in Supplementary Figures S1–S5. The results indicate that, except for the scores of MMSE, which were influenced by the included literature, the remaining four indicators were not affected by the removal of studies, demonstrating good stability. The stability of MMSE may be related to the small number of studies included.
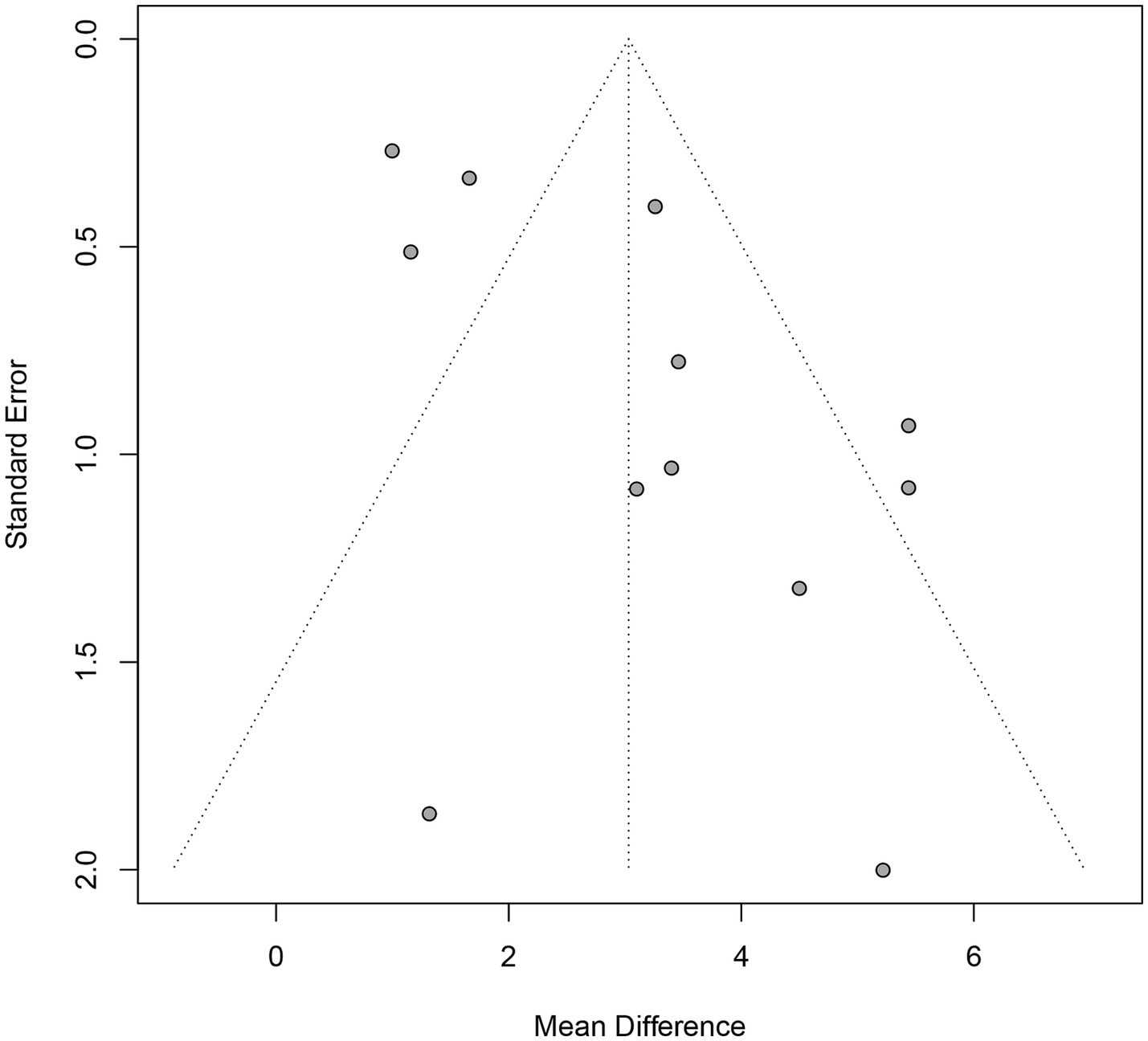
Publication bias analysis
Only the MoCA enrollment data in the final variable exceed 10. Publication bias for the included studies was evaluated using the funnel plot and Egger’s test. The distribution of the scatter points is not perfectly symmetrical (Figure 8). Further quantitative analyses of Egger’s test were performed to detect publication bias, which indicated the presence of publication bias (p = 0.02).
Discussion
In recent years, there has been a growing body of literature on tDCS combined with CR to enhance cognitive function in patients. The potential of tDCS combined with CR to improve cognitive function and ADL in patients with PSCI has been demonstrated, although results vary across studies. While a systematic review has evaluated this combination in healthy older adults, none have specifically addressed its impact and effectiveness in PSCI (28). To the best of our knowledge, this represents the first systematic review and meta-analysis to evaluate the synergistic effects of tDCS combined with CR on cognitive function and ADL among patients with PSCI. Our findings indicate that tDCS combined with CR is a relatively effective non-pharmacological intervention that significantly improves cognitive function and ADL in patients with PSCI. This study not only updates the current understanding of the efficacy of combined tDCS and CR but also provides further evidence supporting the advantages of this integrated approach.
This systematic review and meta-analysis analyzed 11 RCTs involving 663 participants. The results indicate that tDCS combined with CR is more effective than CR alone, tDCS alone, or conventional interventions in enhancing cognitive function and ADL in patients with PSCI. As synaptic plasticity is a fundamental property of neurons and is thought to underlie learning and memory (29). The proposed mechanism for the effectiveness of tDCS combined with CR in improving cognitive function in PSCI is that tDCS modulates synaptic plasticity by altering the concentrations of calcium ions and γ-aminobutyric acid in astrocytes (30) and the neural basis for the effectiveness of cognitive training lies in brain plasticity (31). Meanwhile, CR, informed by information processing theory, can further guide neuroplasticity and cerebral vasodilation, accelerating recovery in damaged areas of the brain (16, 31). Therefore, tDCS combined with CR suggests the possibility of inducing a positive synergistic effect (27). It aligns with the findings of Chen et al. (16) and Zhang et al. (15). The ADL is influenced by cognitive function, which is also thought to involve higher cognitive processes. In other words, patients’ ADL is also further improved with cognitive functioning (32). Collectively, this suggests that tDCS combined with CR provides an effective neurorehabilitation strategy for patients with PSCI.
We conducted subgroup analyses based on different intervention forms: traditional CR and CACR. We conducted subgroup analyses based on different intervention forms: traditional CR and CACR. The results indicated that tDCS combined with CACR showed greater benefits for ADL. CACR is a form of CR that employs computerized cognitive platforms integrating graphics, audio, video, and virtual reality technologies to enhance memory, attention, executive function, and reaction speed (33, 34). Distinct from traditional CR, CACR offers advantages such as individualization, convenience, entertainment, and objectivity (35, 36). It dynamically adjusts task difficulty levels to match patients’ conditions, ensuring continuity in training. Furthermore, it uses multimedia to stimulate interest and motivation, enhancing engagement and training effectiveness (37). These factors likely underlie the superior ADL improvements observed with CACR.
Among the 11 included trials, only four studies (15–17, 23) documented mild adverse effects associated with tDCS combined with CR, primarily manifested as tingling, skin redness, and itching. However, all were within the patients’ tolerance range and had no significant negative impact. Additionally, no patients were withdrawn from the study due to serious adverse effects based on the results reported in all studies. Thus, it indicates that tDCS combined with CR is a well-tolerated therapeutic approach that is relatively safe for clinical implementation.
Our systematic review and meta-analysis employed a rigorous methodology that included only RCTs, enhancing the comparability of the results. The use of multiple assessment tools for synthesizing the effects of tDCS combined with CR on cognitive function and ADL in PSCI patients improved the accuracy of the study. However, there were some limitations. First, our analysis was restricted to studies in Chinese and English, which may have excluded relevant studies published in other languages that could contain valuable data, resulting in a potential language bias. Second, the current analysis focused on overall cognitive function due to limited data from the included studies, which limits specific evaluations of language, attention, and executive functioning. This may limit our understanding of other specific functions in patients with cognitive impairment. Third, substantial heterogeneity in stimulation parameters (including frequency, intensity, and stimulation sites) and the areas affected by stroke among the included studies limited the feasibility of a more comprehensive subgroup analysis. To address these gaps, future studies should prioritize standardized reporting protocols for stroke lesion characterization. Meanwhile, multi-center RCTs with larger sample sizes are necessary to determine the optimal tDCS and CR protocols, aiming to provide more effective and targeted treatments for PSCI patients. In addition, there is evidence that cognitive function impairment is both long-lasting and dynamic, showing an accelerated decline over 6 years post-stroke (38). This systematic review primarily reflected short-term effects, as the outcomes were measured within one to 6 weeks after the intervention was administered. This limitation underscores the need for long-term follow-up studies examining the effectiveness of tDCS combined with CR on cognitive function and ADL in individuals with PSCI. This will provide more comprehensive and reliable evidence for the efficacy of tDCS combined with CR in treating PSCI.
Conclusion
This meta-analysis and systematic review suggest that tDCS combined with CR is more effective than tDCS alone, or CR alone, or conventional interventions in improving cognitive function and ADL in patients with PSCI. These findings provide essential guidance for healthcare practitioners on using tDCS combined with CR to support brain health in patients with PSCI, as well as for future empirical research. More comprehensive, high-quality trials with longer follow-up periods are essential for definitive conclusions. In-depth mechanistic studies that integrate brain imaging techniques, humoral biomarkers, and genomic data are also crucial for providing more reliable evidence-based clinical rehabilitation strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
NL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BZ: Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Visualization, Writing – review & editing. HW: Conceptualization, Data curation, Methodology, Project administration, Supervision, Writing – review & editing. JW: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. YL: Conceptualization, Data curation, Formal analysis, Software, Supervision, Visualization, Writing –review & editing. MY: Conceptualization, Data curation, Project administration, Software, Writing – review & editing. CX: Conceptualization, Data curation, Formal analysis, Software, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Tiantan Hospital -Hospital Fund -Nursing special (2023-YQN-10).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1523001/full#supplementary-material
References
1. GBD 2021 Stroke Risk Factor Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. (2024) 23:973–1003. doi: 10.1016/S1474-4422(24)00369-7
2. Wang, K, and Dong, Q. Expert Consensus on the Management of Cognitive Impairment After Stroke 2021. Chin J Stroke. (2021) 16:376–89. doi: 10.3969/j.issn.1673-5765.2021.04.01
3. Buvarp, D, Rafsten, L, Abzhandadze, T, and Sunnerhagen, KS. A prospective cohort study on longitudinal trajectories of cognitive function after stroke. Sci Rep. (2021) 11:17271. doi: 10.1038/s41598-021-96347-y
4. Huang, YY, Chen, SD, Leng, XY, Kuo, K, Wang, ZT, Cui, M, et al. Post-stroke cognitive impairment: epidemiology, risk factors, and management. J Alzheimers Dis. (2022) 86:983–99. doi: 10.3233/jad-215644
5. Jokinen, H, Melkas, S, Ylikoski, R, Pohjasvaara, T, Kaste, M, Erkinjuntti, T, et al. Post-stroke cognitive impairment is common even after successful clinical recovery. Eur J Neurol. (2015) 22:1288–94. doi: 10.1111/ene.12743
6. Fride, Y, Adamit, T, Maeir, A, Ben Assayag, E, Bornstein, NM, Korczyn, AD, et al. What are the correlates of cognition and participation to return to work after first ever mild stroke? Top Stroke Rehabil. (2015) 22:317–25. doi: 10.1179/1074935714Z.0000000013
7. Yu, J, and Wang, J. Effect of post-stroke cognitive impairment and dementia on stroke recurrence and functional outcomes: A systematic review and meta-analysis. PLoS One. (2024) 19:e0313633. doi: 10.1371/journal.pone.0313633
8. Farooq, MU, Min, J, Goshgarian, C, and Gorelick, PB. Pharmacotherapy for vascular cognitive impairment. CNS Drugs. (2017) 31:759–76. doi: 10.1007/s40263-017-0459-3
9. Marucci, G, Buccioni, M, Ben, DD, Lambertucci, C, Volpini, R, and Amenta, F. Efficacy of acetylcholinesterase inhibitors in Alzheimer's disease. Neuropharmacology. (2021) 190:108352. doi: 10.1016/j.neuropharm.2020.108352
10. Wang, Y, Xu, N, Wang, R, and Zai, W. Systematic review and network meta-analysis of effects of noninvasive brain stimulation on post-stroke cognitive impairment. Front Neurosci. (2022) 16:1082383. doi: 10.3389/fnins.2022.1082383
11. Hamzei, F, Ritter, A, and Güllmar, D. Implicit motor learning under anodal or cathodal tDCS during fMRI induces partially distinct network responses. Eur J Neurosci. (2025) 61:e70053. doi: 10.1111/ejn.70053
12. China Expert Consensus Group on Clinical Application of Transcranial Direct Current Stimulation in Stroke Rehabilitation. Expert consensus on the use of transcranial direct current stimulation in the rehabilitation of stroke patients. Chin J Phys Med Rehabil. (2021) 43:289–94. doi: 10.3760/cma.j.issn.0254-1424.2021.04.001
13. Guo, XX, Xia, SY, Cui, C, Ou, YY, and Zhang, LY. Effects of tDCS combined with cognitive intervention on memory and executive fuInction in patients with cognitive impairment after cerebral infarction. Chin J Rehabil Med. (2022) 37:1057–62. doi: 10.3969/j.issn.1001-1242.2022.08.008
14. Li, LY, Meng, Y, Hao, ZW, Lv, PY, and Dong, YH. Application of transcranial direct current stimulation and computerized cognitive training in patients with vascular cognitive impairment. Int J Cerebrovasc Dis. (2024) 32:133–9. doi: 10.3760/cma.j.issn.1673-4165.2024.02.010
15. Zhang, L, Zhou, L, Ye, Q, Zhang, L, Kong, Y, and Xia, S. Impact of transcranial direct current stimulation combined with motor-cognitive intervention on post-stroke cognitive impairment. Neurol Sci. (2024) 45:1581–8. doi: 10.1007/s10072-023-07156-2
16. Chen, Y, Zhao, Z, Huang, J, Wang, T, and Qu, Y. Computer-aided cognitive training combined with tDCS can improve post-stroke cognitive impairment and cerebral vasomotor function: a randomized controlled trial. BMC Neurol. (2024) 24:132. doi: 10.1186/s12883-024-03613-3
17. Park, SH, Koh, EJ, Choi, HY, and Ko, MH. A double-blind, sham-controlled, pilot study to assess the effects of the concomitant use of transcranial direct current stimulation with the computer assisted cognitive rehabilitation to the prefrontal cortex on cognitive functions in patients with stroke. J Korean Neurosurg Soc. (2013) 54:484–8. doi: 10.3340/jkns.2013.54.6.484
18. Song, MH, Zhu, QX, Gao, CF, Zhang, H, and Liu, YL. Effect and analysis of transcranial direct current stimulation combined with cognitive rehabilitation training on post-stroke cognitive impairment. Adv Clin Med. (2023) 13:8379–85. doi: 10.12677/ACM.2023.1351172
19. Jiang, YJ, Hu, MY, You, YM, Wang, J, Lin, ZC, Wei, W, et al. A meta-analysis of transcranial direct current stimulation to improve cognitive impairment after stroke. Chin J Rehabil Med. (2022) 37:660–5. doi: 10.3969/j.issn.1001-1242.2022.05.015
20. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
21. Higgins, JPT, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, MJ, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.5 (updated August 2024). Cochrane. (2024).
22. Yun, GJ, Chun, MH, and Kim, BR. The effects of transcranial direct-current stimulation on cognition in stroke patients. J Stroke. (2015) 17:354–8. doi: 10.5853/jos.2015.17.3.354
23. Liu, YW, Chen, ZH, Luo, J, Yin, MY, Li, LL, Yang, YD, et al. Explore combined use of transcranial direct current stimulation and cognitive training on executive function after stroke. J Rehabil Med. (2021) 53:jrm00162. doi: 10.2340/16501977-2807
24. Lv, XH, Liu, YP, Ma, Y, Hu, F, Lang, XG, Hao, PN, et al. The clinical effects of cognitive rehabilitation combined with transcranial direct current stimulation in treatment of patients with cognitive impairment after cerebral stroke. Hebei Yi Xue. (2021) 43:2786–9. doi: 10.3969/j.issn.1002-7386.2021.18.015
25. Ko, MH, Yoon, JY, Jo, YJ, Son, MN, Kim, DS, Kim, GW, et al. Home-based transcranial direct current stimulation to enhance cognition in stroke: randomized controlled trial. Stroke. (2022) 53:2992–3001. doi: 10.1161/strokeaha.121.037629
26. Wang, Z, Li, J, Wang, X, Liu, S, and Wu, W. Effect of transcranial direct-current stimulation on executive function and resting EEG after stroke: a pilot randomized controlled study. J Clin Neurosci. (2022) 103:141–7. doi: 10.1016/j.jocn.2022.07.010
27. Zhou, WX, Wang, SY, Gu, CC, Zhao, J, Ou, XL, and Gong, ZK. Improvement effects of cognitive training synchronized with transcranial direct current stimulation for the treatment of working memory in patients with post-stroke cognitive impairment. J Neurosci Ment Health. (2024) 24:88–93. doi: 10.3969/j.issn.1009-6574.2024.02.003
28. Lv, Y, Wu, S, Nitsche, MA, Yue, T, Zschorlich, VR, and Qi, F. A meta-analysis of the effects of transcranial direct current stimulation combined with cognitive training on working memory in healthy older adults. Front Aging Neurosci. (2024) 16:1454755. doi: 10.3389/fnagi.2024.1454755
29. Mateos-Aparicio, P, and Rodríguez-Moreno, A. Calcium dynamics and synaptic plasticity. Adv Exp Med Biol. (2020) 1131:965–84. doi: 10.1007/978-3-030-12457-1_38
30. Liu, YC, and Zhang, LX. Research progress in transcranial direct current stimulation therapy for cognitive impairment after stroke. Rehabil Med. (2024) 34:304–310. doi: 10.3724/SP.J.1329.2024.03013
31. Cognitive Training China Guideline Writing Group, Neurologists Branch, Chinese Medical Doctors' Association. Cognitive training China guide (2022 edition). Natl Med China. (2022) 102:2918–25. doi: 10.3760/cma.j.cn112137-20220606-01256
32. Bruderer-Hofstetter, M, Gorus, E, Cornelis, E, Meichtry, A, and De-Vriendt, P. Influencing factors on instrumental activities of daily living functioning in people with mild cognitive disorder - a secondary investigation of cross-sectional data. BMC Geriatr. (2022) 22:791. doi: 10.1186/s12877-022-03476-8
33. Mingming, Y, Bolun, Z, Zhijian, L, Yingli, W, and Lanshu, Z. Effectiveness of computer-based training on post-stroke cognitive rehabilitation: a systematic review and meta-analysis. Neuropsychol Rehabil. (2022) 32:481–97. doi: 10.1080/09602011.2020.1831555
34. Antian, C, Chenyu, W, Wei, L, Xin, L, Bin, Z, and Xiaoqin, D. Current situation and progress of computerized cognitive assessment and rehabilitation system for stroke patient. Chin J Robot Surg. (2021) 2:220–4. doi: 10.12180/j.issn.2096-7721.2021.03.011
35. Zhang, SX, and He, YS. Recent advance in computer -assisted cognitive rehabilitation in treatment of cognitive impairment after traumatic brain injury. Chin J Neuromed. (2019) 18:98–101. doi: 10.3760/cma.j.issn.1671-8925.2019.01.019
36. Han, Y, Liu, M, Zhou, SN, Lv, YT, Gu, Y, and Wang, SS. Effect of computer-aided cognitive rehabilitation training on executive dysfunction after cerebral infarction. Chin J Phys Med Rehabil. (2018) 40:544–6. doi: 10.3760/cma.j.issn.0254-1424.2018.07.020
37. Cho, HY, Kim, KT, and Jung, JH. Effects of computer assisted cognitive rehabilitation on brain wave, memory and attention of stroke patients: a randomized control trial. J Phys Ther Sci. (2015) 27:1029–32. doi: 10.1589/jpts.27.1029
Keywords: post-stroke cognitive impairment, cognitive rehabilitation, transcranial direct current stimulation, meta-analysis, cognitive function, activities of daily living
Citation: Luo N, Zhao B, Wang H, Wu J, Luo Y, Yuan M and Xu C (2025) Effect of transcranial direct current stimulation combined with cognitive rehabilitation on cognitive function and activities of daily living in patients with post-stroke cognitive impairment: a systematic review and meta-analysis. Front. Neurol. 16:1523001. doi: 10.3389/fneur.2025.1523001
Edited by:
Victor W. Mark, University of Alabama at Birmingham, United StatesReviewed by:
Mariagiovanna Cantone, Gaspare Rodolico Hospital, ItalyRajan Kashyap, National Institute of Mental Health and Neurosciences (NIMHANS), India
Copyright © 2025 Luo, Zhao, Wang, Wu, Luo, Yuan and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binbin Zhao, dHR5eXpoYW9iaW5iaW5AMTYzLmNvbQ==
 Nan Luo
Nan Luo Binbin Zhao
Binbin Zhao Hui Wang
Hui Wang Jiabei Wu
Jiabei Wu Yifan Luo1
Yifan Luo1