- 1The Second Clinical Medical College, Yunnan University of Traditional Chinese Medicine, Kunming, China
- 2Kunming Medical University, Kunming Medical University, Kunming, China
- 3Department of Rehabilitation Medicine, Affiliated Hospital of Yunnan University, Kunming, China
- 4The Third Affiliated Hospital, Yunnan University of Chinese Medicine, Kunming, China
- 5The Second Affiliated Hospital, Yunnan University of Traditional Chinese Medicine, Kunming, China
- 6Department of Rehabilitation Medicine, Yunnan Integrated Hospital of Traditional Chinese and Western Medicine, Kunming, China
Objective: This study aimed to evaluate the effects of acupuncture combined with hyperbaric oxygenation (HBO) compared with HBO alone in improving the disturbance of consciousness (DOC) of people with traumatic brain injury (TBI).
Methods: The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in this study. In accordance with the preestablished search strategy, all the literature was obtained from eight online databases. Following the stringent application of inclusion and exclusion criteria, two researchers conducted an independent extraction of valid data from eligible randomized controlled trials (RCTs). The risk of bias in each study was assessed using the Cochrane Risk of Bias 2.0 tool. The meta-analysis was conducted utilizing the RevMan software. Adverse events were determined based on data from each study assessing the safety of acupuncture treatment.
Results: A total of 11 RCTs with 896 participants were included in the analysis. Overall, the methodological quality of the RCTs encompassed within this meta-analysis was below standard. The pooled data demonstrated that acupuncture treatment combined with HBO was significantly superior to HBO alone, based on the Glasgow Coma Scale (GCS) scores [mean difference (MD) = 2.13, 95% confidence interval (CI): 1.64–2.62, p < 0.00001]. We also found that electroacupuncture (EA) combined with HBO improved GCS scores more than HBO alone in TBI patients (MD = 2.15, 95% CI: 1.95–2.36). The early intervention (MD = 3.09, 95% CI, 2.66–3.52) demonstrated significantly more significant improvement in GCS scores following combination therapy compared with the late intervention group (MD = 1.86, 95% CI, 1.47–2.25). Furthermore, compared with HBO alone, acupuncture combined with HBO significantly improved patients’ consciousness rate (CR) (RR = 2.26, 95% CI: 1.48–3.46). Statistical analysis also revealed that acupuncture combined with HBO improved the effective rate (ER) (RR = 1.47, 95% CI: 1.27–2.69). Additionally, no studies reported any significant adverse events.
Conclusion: Compared with HBO alone, acupuncture combined with HBO has a more substantial positive effect on GCS scores, AR, and ER in patients with TBI. However, given the limited availability of high-quality evidence and the dearth of RCTs in this area, the conclusions drawn herein warrant validation through additional research endeavours.
Clinical trial registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024576067, CRD42024576067.
1 Introduction
Traumatic brain injury (TBI) is a neurological disease caused mainly by violent injury to the head. This trauma can damage the brain and lead to a series of symptoms, such as disturbance of consciousness (DOC), cognitive impairment, and psychological and physiological dysfunctions (1). A document from the Lancet Neurology Commission states that by 2030, TBI is estimated to remain one of the top three causes of injury-related death and disability, with 50–60 million people affected by the disease each year worldwide, with 5.48 million cases classified as severe (2).
Currently, clinical treatments for TBI include hyperbaric oxygenation (HBO) (3), medication, brain stimulation (4), and traditional rehabilitation therapy (5). In addition, aural-musical therapy (6), robot-assisted therapy devices (7), and brain-computer interfaces (8) are garnering increasing attention and being incorporated into research and clinical practices. Although significant progress has been made over the past two decades in stimulating the resurgence of awareness in TBI patients, the available therapeutic modalities remain limited (9). Developing more efficacious, simplified, and comprehensive restorative and therapeutic approaches is vital for optimizing TBI treatment. Acupuncture is a commonly used technique in China for treating neurological disorders (10). Studies have shown its neuroprotective effects in traumatic brain injury (TBI), including improved consciousness, alleviated cognitive dysfunction, and reduced mortality rates (11). HBO is a crucial component in the comprehensive treatment of cranial brain injuries, offering a multitude of significant benefits (12). These include enhancing blood oxygen levels to combat hypoxia, alleviating cerebral edema and reducing intracranial pressure, stimulating the central reticular system to improve consciousness, fostering blood circulation and neural repair, exerting anti-inflammatory and immune-modulating effects, and hastening the clearance of lesions and the absorption of hematomas (13, 14).
There has been no known synthesis of evidence comparing acupuncture combined with HBO and HBO alone. Therefore, the core aim of this systematic review and meta-analysis is to determine whether acupuncture combined with HBO improves TBI symptoms more than HBO alone.
2 Materials and methods
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (15). This study was registered on the Prospective Register of Systematic Reviews (PROSPERO) on August 16th, 2024, with the registration number CRD42024576067.
2.1 Search strategy
In this study, the following databases were searched: Medline, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science (SCI), Chinese Biomedical Database (CBM), Chinese National Knowledge Infrastructure (CNKI), Wan Fang Data Knowledge Service Platform, and VIP Journal Integration Platform (VIP). All evidence published prior to September 7th, 2024, was included. Reference lists from studies identified through the Chinese Clinical Trial Register and ClinicalTrials.gov were also scrutinized, and any additional studies identified through this process were included. The MeSH function was utilized to locate studies using synonyms of the keywords entered in this search process. The keywords included “Acupuncture,” “Hyperbaric oxygenation,” and “Traumatic brain injury.” The specific search strategies employed have been detailed in the Supplementary material.
2.2 Selection criteria
Below are the criteria guiding this review:
(1) Subjects must have a diagnosis of TBI.
(2) The condition must be verified via magnetic resonance imaging (MRI) or computed tomography (CT).
(3) In the treatment group, acupuncture combined with HBO was used, while HBO was used as the primary treatment in the control group. Both groups also received the same basic treatments.
(4) The study type was an RCT.
2.3 Exclusion criteria
Studies that were excluded based on the following criteria:
(1) The study was a duplication of a previous study.
(2) The study compared different acupuncture therapies without the inclusion of HBO.
(3) The full text was not available.
2.4 Study selection and data extraction
Two researchers (BY-W and SC-F) conducted independent screenings of the studies, excluding duplicates and those deemed irrelevant. Each reviewer screened articles to ensure they met the inclusion criteria. Data extraction from eligible studies was conducted and verified, with discrepancies resolved through consultation. When consensus was not reached, a third researcher (SL-L) was invited to provide a decisive opinion. All excluded literature was systematically documented. Data extraction was conducted independently by CX-L and YJ-F, with validation performed by researcher BY-W. Extracted data included first author, publication year, number of participants, age, treatment duration, diagnostic criteria, types of outcomes, side effects and adverse events, and other relevant information. The results were recorded in an Excel spreadsheet.
2.5 Study quality assessment
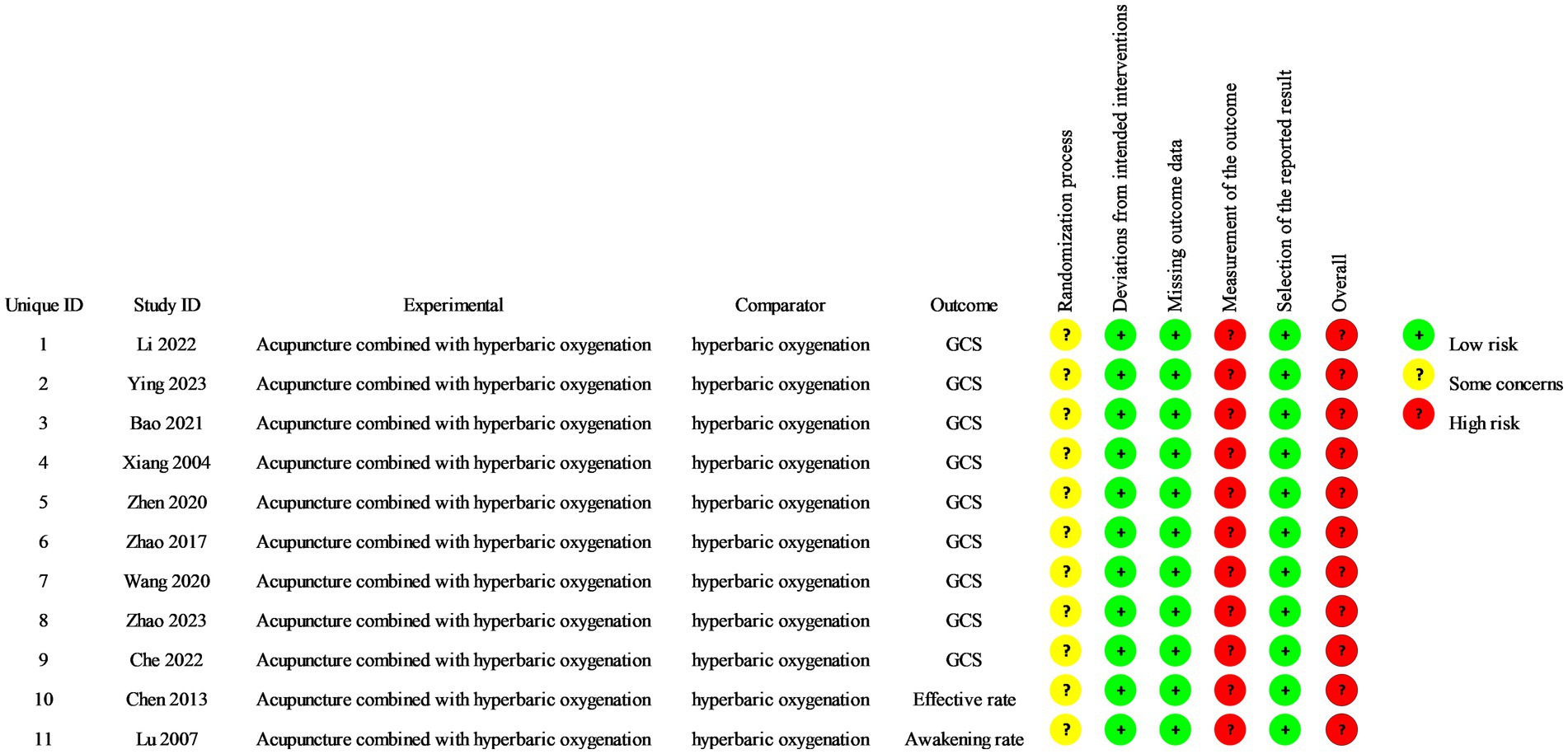
The quality of individual studies was assessed using the Cochrane Risk of Bias 2.0 tool (16). The following six items were extracted from each of the RCTs: (a) randomization process; (b) deviations from intended interventions; (c) missing outcome data; (d) measurement of the outcome; (e) selection of the reported results; (f) overall findings. Studies employing suitable methodologies and providing transparent descriptions were deemed to exhibit a low bias risk. In contrast, those lacking such methodological rigor and clarity in the description were categorized as having a high bias risk. SL-L and LS performed a bilateral evaluation of these factors, with a third researcher (BY-W) providing an objective opinion and helping to resolve any ensuing disputes.
2.6 Types of outcomes
The primary outcome measure was the Glasgow Coma Scale (GCS) score. The GCS was developed more than 50 years ago to measure the “depth and duration of impaired consciousness” of patients with TBI (17). Five decades of research support the efficacy of this tool in assessing and describing patients with neurological impairment (18).
One secondary outcome was the Consciousness Rate (CR), which included patients who reached a minimally conscious state (MCS) and those who emerged from MCS, as assessed by the Coma Recovery Scale-Revised (CRS-R), and were judged to be conscious. Another secondary outcome was the Effective Rate (ER), calculated as the sum of effective and improved cases divided by the total number of cases. Treatment effectiveness was determined if clinical symptoms completely disappeared, consciousness was clear, speech was fluent, and no assistance was needed in daily life. Clinical symptoms were considered improved if there was a significant improvement in DOC and daily life required only mild assistance. Treatment was deemed ineffective if there was no or only slight improvement in clinical symptoms or consciousness, and full assistance was required in daily life.
2.7 Statistical analysis
The RevMan 5.4 software package was used to perform the statistical analyses. For categorical variables, the risk ratio (RR) and its corresponding 95% confidence interval (CI) were applied. For continuous variables, the mean difference (MD) was chosen as the metric, with a 95% CI. Statistical significance was set at p < 0.05. The Q test and I2 statistics were used to assess heterogeneity between the included studies, and the effect model was selected based on these assessments. Statistically significant heterogeneity among the included studies was indicated by p < 0.1 and I2 > 50%. Consequently, a random-effects model was used to determine the effect size for each outcome. When p ≥ 0.1 and I2 < 50%, the heterogeneity among the studies was considered acceptable, leading to the use of a fixed-effects model for data synthesis in these cases. Combined results were assessed using the Z test, with p < 0.05 indicating a statistically significant difference. Publication bias within the included studies was assessed using funnel plots and Egger’s regression test. All forest plots were oriented with effect sizes calculated as experimental group minus control group MD or RR for the experimental group, with “Favors acupuncture + HBO” clearly labelled on the right side to prevent directional misinterpretation.
3 Results
3.1 Studies retrieved
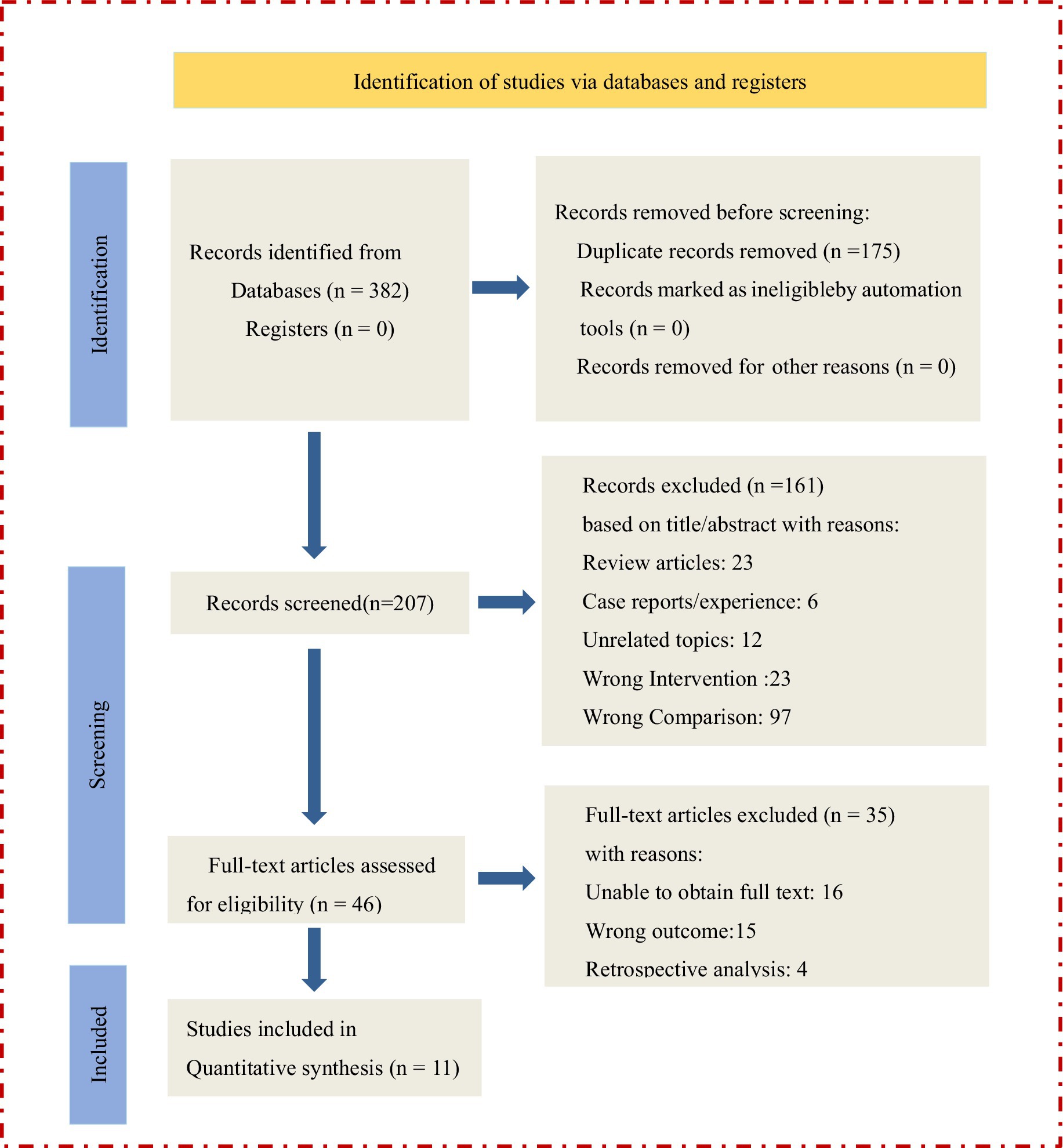
Figure 1 presents a detailed flow chart of the study selection process according to the PRISMA guidelines. First, we removed 175 duplicate articles, and the titles and abstracts of the remaining 207 articles were screened. After screening, 51 full texts were reviewed. A total of 11 RCTs were included in the meta-analysis (19–29).
3.2 Characteristics of the study participants
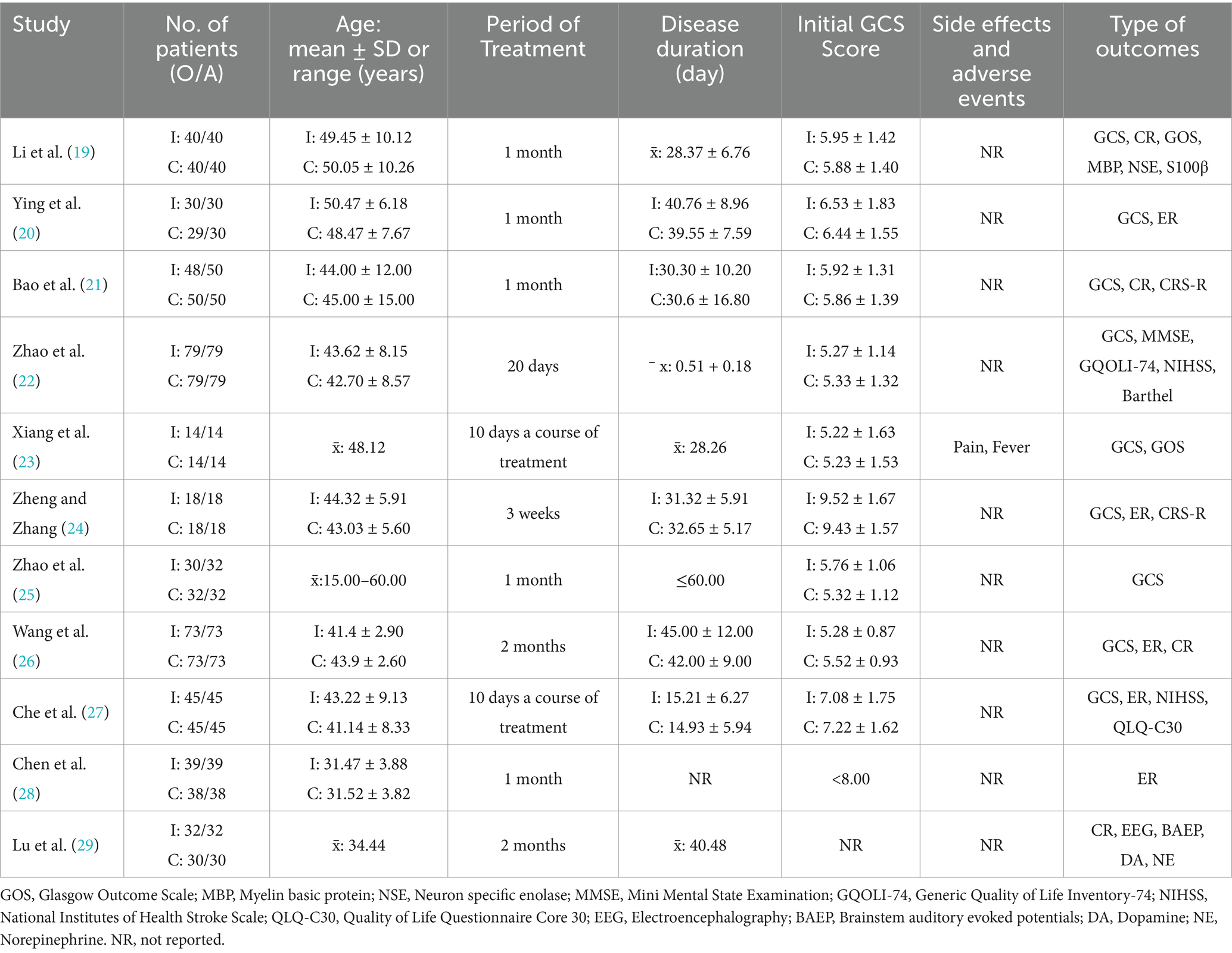
A total of 896 participants were included, 448 in the experimental group and 448 in the control group. The study sample sizes ranged from 28 to 158 participants. There were more males than females in the study population. No significant difference in the mean age was found between the two groups (p > 0.05). Demographic details of the 11 included RCTs are summarized in Table 1.
3.3 Description of interventions
Electroacupuncture (EA) was used most frequently (54.5%), followed by hand acupuncture (MA) (36.4%) and warm acupuncture (WA) (9%). All included studies utilized HBO as a control measure. The needle retention time was set at 30 min in 10 out of 11 studies. The frequency of treatment sessions varied between 5 and 7 times weekly, with an average frequency of 5 sessions (n = 5). The treatment periods in these studies ranged from 10 days to 8 weeks, with a 4-week treatment period being optimal (n = 5). Two studies (24, 27) did not report treatment periods, and the length of time was determined on the basis of the patients’ disease progression. The following points and frequencies were noted in the included studies: Shui-gou (63.6%), Nei-guan (54.5%), Bai-hui (54.5%), San-yin-jiao (45.5%), Yin-tang (36.4%), He-gu (36.4%), and Tai-chong (27.3%). These acupoints were employed with the most significant frequency. Table 2 depicts the characteristics of the interventions in the included studies.
3.4 Quality assessment results
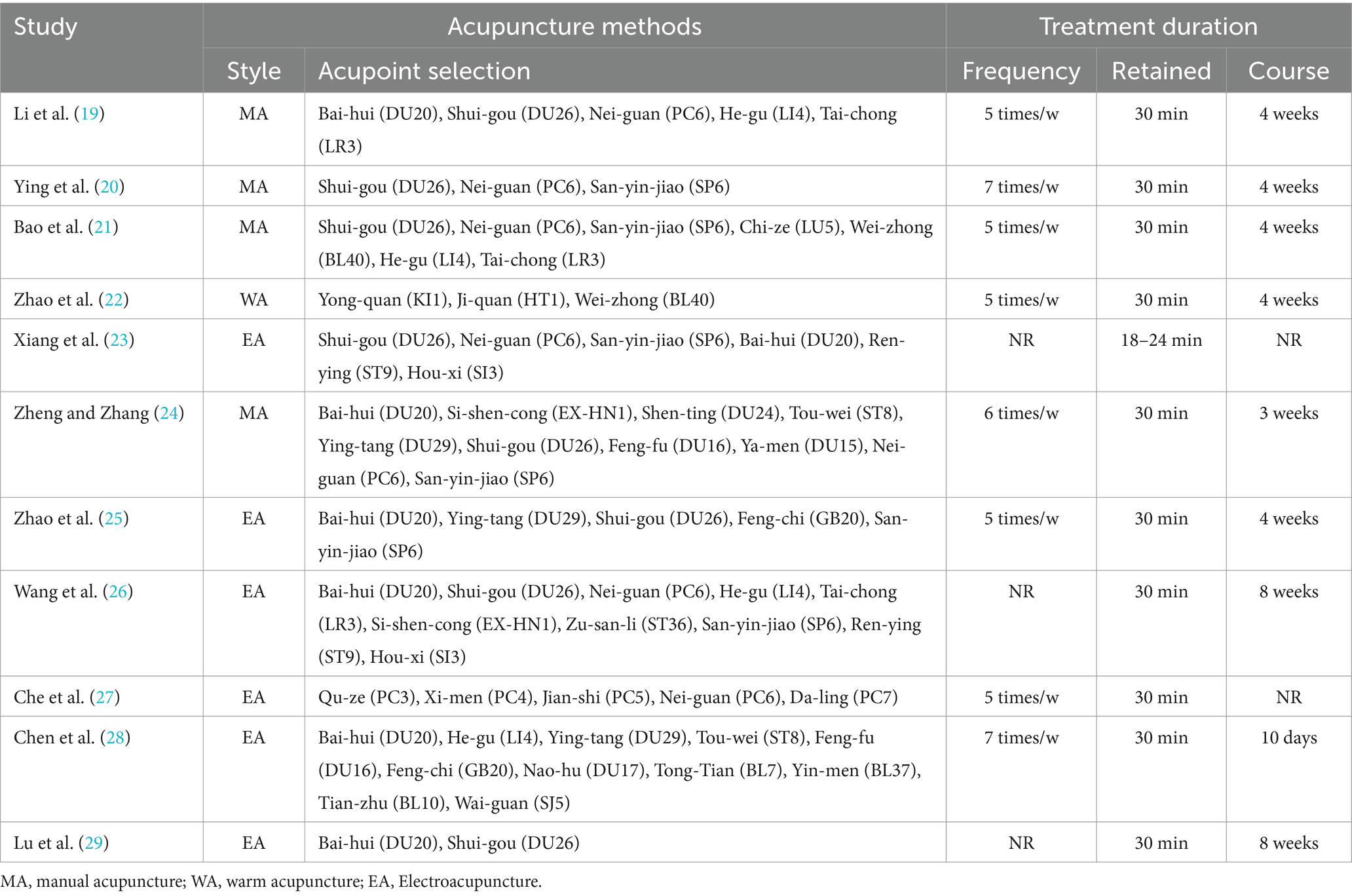
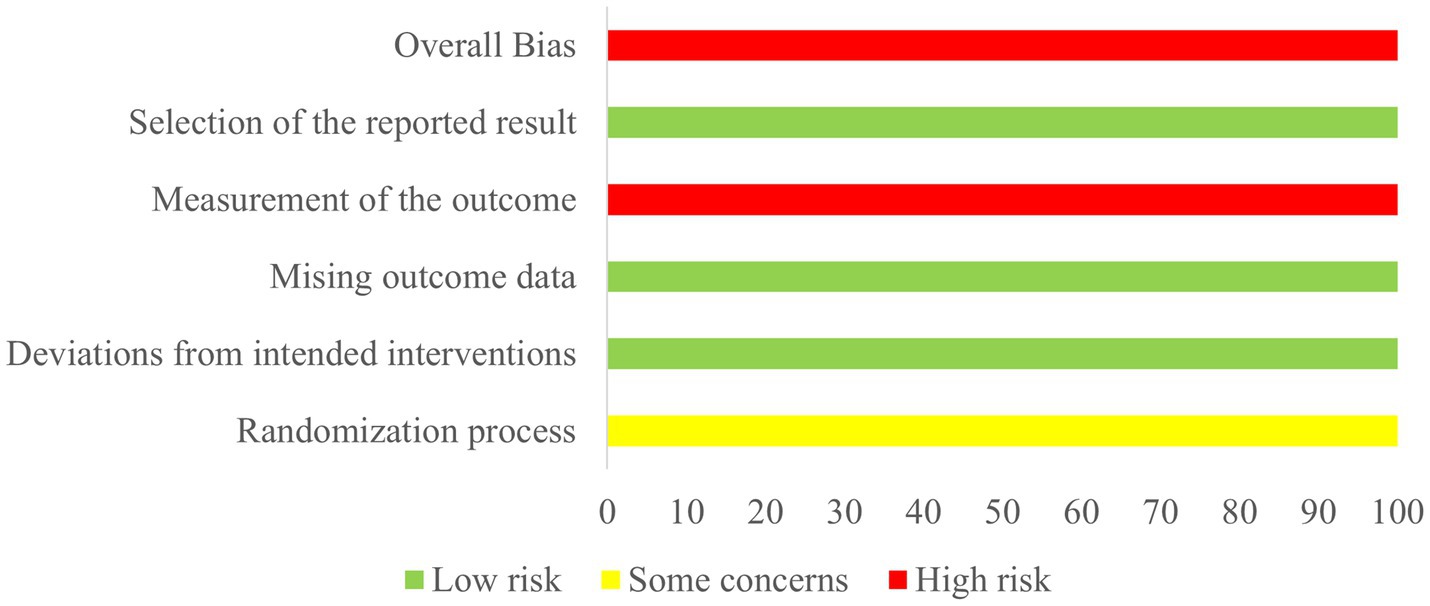
The methodological rigor of the encompassed studies was consistently found to be subpar. All included trials reported on randomization processes. Three studies (22, 26, 28) only mentioned the word ‘randomization’ without detailing the method used. None of the included studies detailed the methods of group allocation, leading to an assessment of moderate bias risk. None of the included studies reported blinding methods and were classified as exhibiting a high risk of bias. No other methodological deviations were found in the included studies (Figures 2, 3).
3.5 Meta-analysis
3.5.1 Glasgow coma scale
Nine studies (19–27) adopted the GCS score to evaluate patients’ level of consciousness impairment. Due to significant heterogeneity (p < 0.00001, I2 = 79%), a random-effects model was employed. Significantly higher Glasgow Coma Scale (GCS) scores were demonstrated in patients receiving combined acupuncture and HBO therapy compared to those undergoing HBO treatment alone. (MD = 2.13, 95% CI: 1.64–2.62, p < 0.00001) (Figure 4).
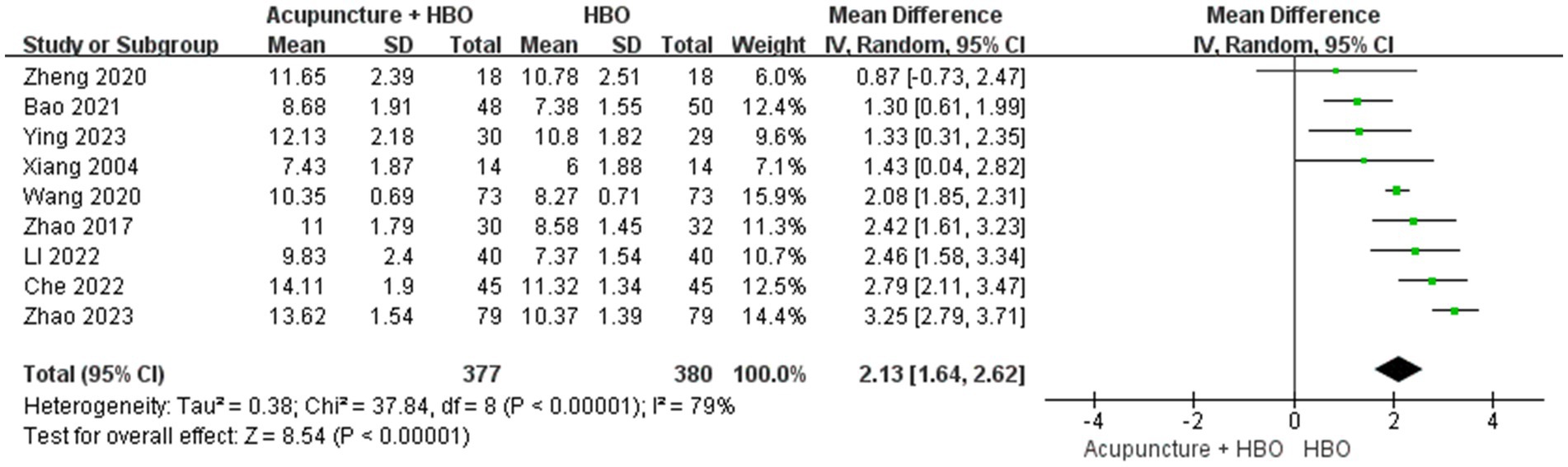
Figure 4. Forest plot of effects of acupuncture combined with HBO versus HBO alone on GCS score (Random effect model). MD > 0 indicates that the acupuncture combined with HBO group demonstrated higher GCS scores.
The stratified analyses were performed by acupuncture modality: manual acupuncture (MA), electroacupuncture (EA), and warm acupuncture (WA). Subgroup analysis revealed statistically significant between-subgroup heterogeneity (p < 0.00001, I2 = 92.6%). The EA subgroup demonstrated a superior improvement in GCS scores (MD = 2.15, 95% CI: 1.95–2.36) with low heterogeneity (I2 = 43%, p = 0.16), compared with the MA subgroup (MD = 1.59, 95% CI: 1.12–2.05, p < 0.00001, I2 = 45%, p = 0.14). The WA subgroup was excluded from the pooled analysis due to insufficient sample size (n = 1) (Figure 5).
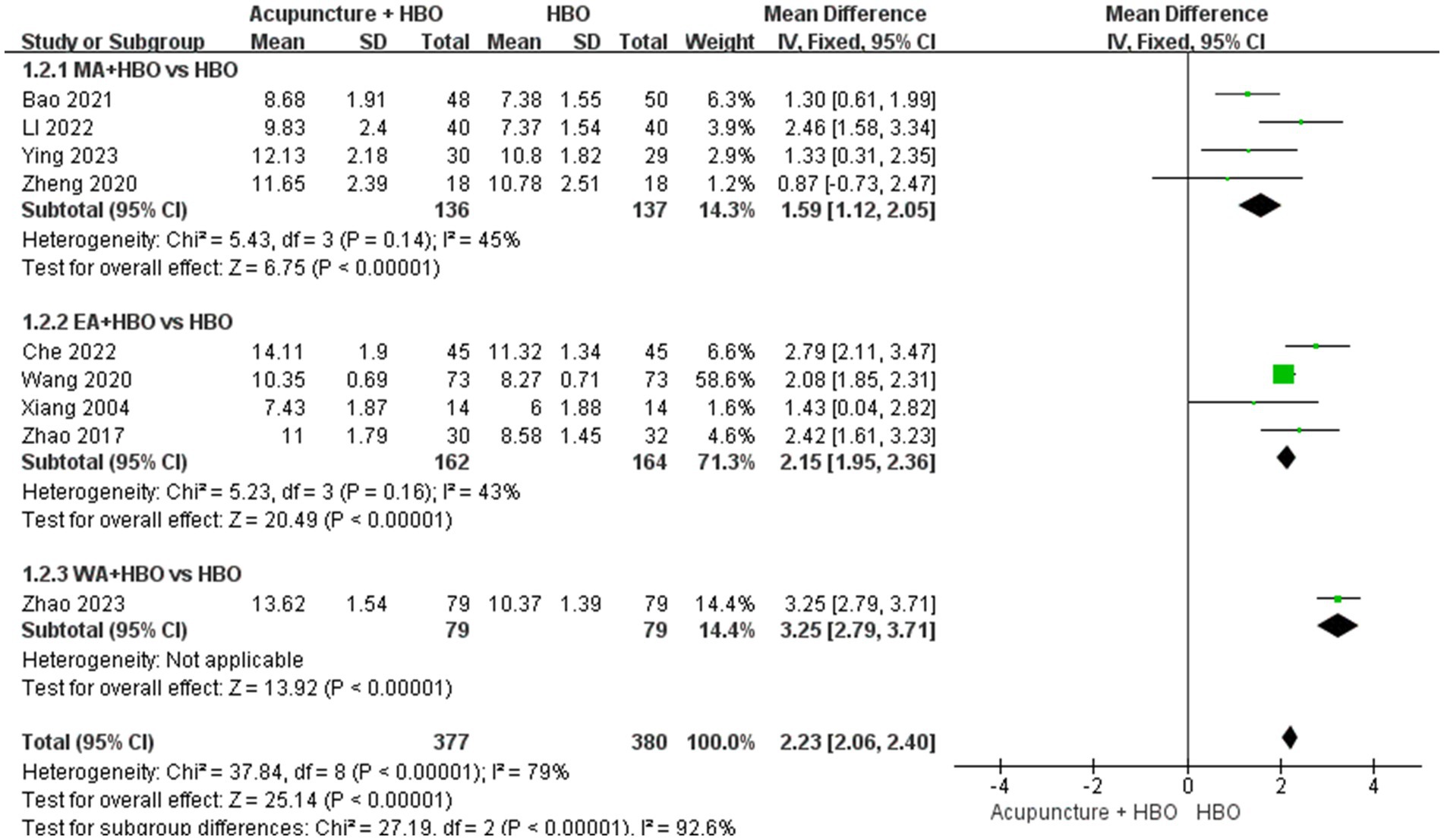
Figure 5. Forest plot of effects of acupuncture combined with HBO versus HBO alone on GCS score (Subgroup by the different acupuncture style). MD > 0 indicates that the acupuncture combined with HBO group demonstrated higher GCS scores.
Subgroup analysis accounting for baseline injury severity revealed critical methodological considerations. The heterogeneity in baseline GCS scores constituted a potential confounding factor, given established evidence of a graded association between initial GCS scores and neurological prognosis in TBI patients (30). As none of the included studies implemented GCS-stratified analysis or covariate adjustment, we conducted post hoc subgroup analyses. After excluding a single-centre study (24) enrolling patients with GCS > 8, the pooled effect size remained robust (MD = 2.21, 95% CI: 1.71–2.71) (Figure 6). The remaining eight studies focusing on severe TBI (GCS ≤ 8) were stratified using a cutoff of GCS score: very severe subgroup (GCS 3–5, n = 6) and severe subgroup (GCS 6–8, n = 2). Random-effects model synthesis demonstrated comparable efficacy between subgroups (test for subgroup differences: p = 0.27), though point estimates suggested marginally more significant improvement in the very severe subgroup (MD = 2.22, 95% CI: 1.63–2.82, p < 0.001) compared with the severe subgroup (MD = 2.11, 95% CI: 0.69–3.54, p = 0.004) (Figure 7).
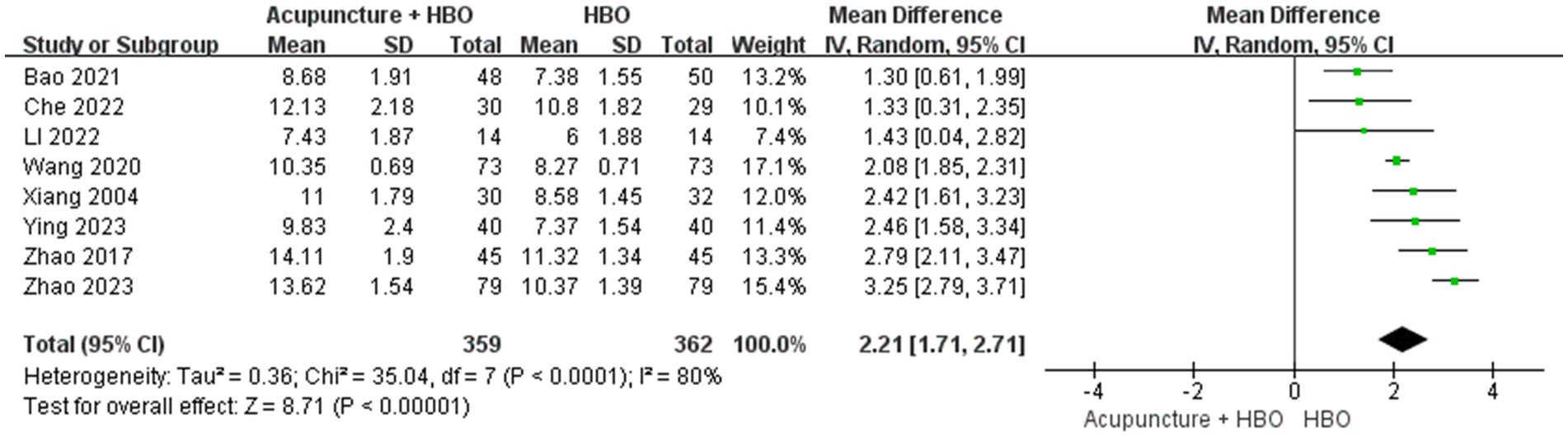
Figure 6. Forest plot of effects of acupuncture combined with HBO versus HBO alone on GCS score (Sensitivity analysis of TBI classification). MD > 0 indicates that the acupuncture combined with HBO group demonstrated higher GCS scores.
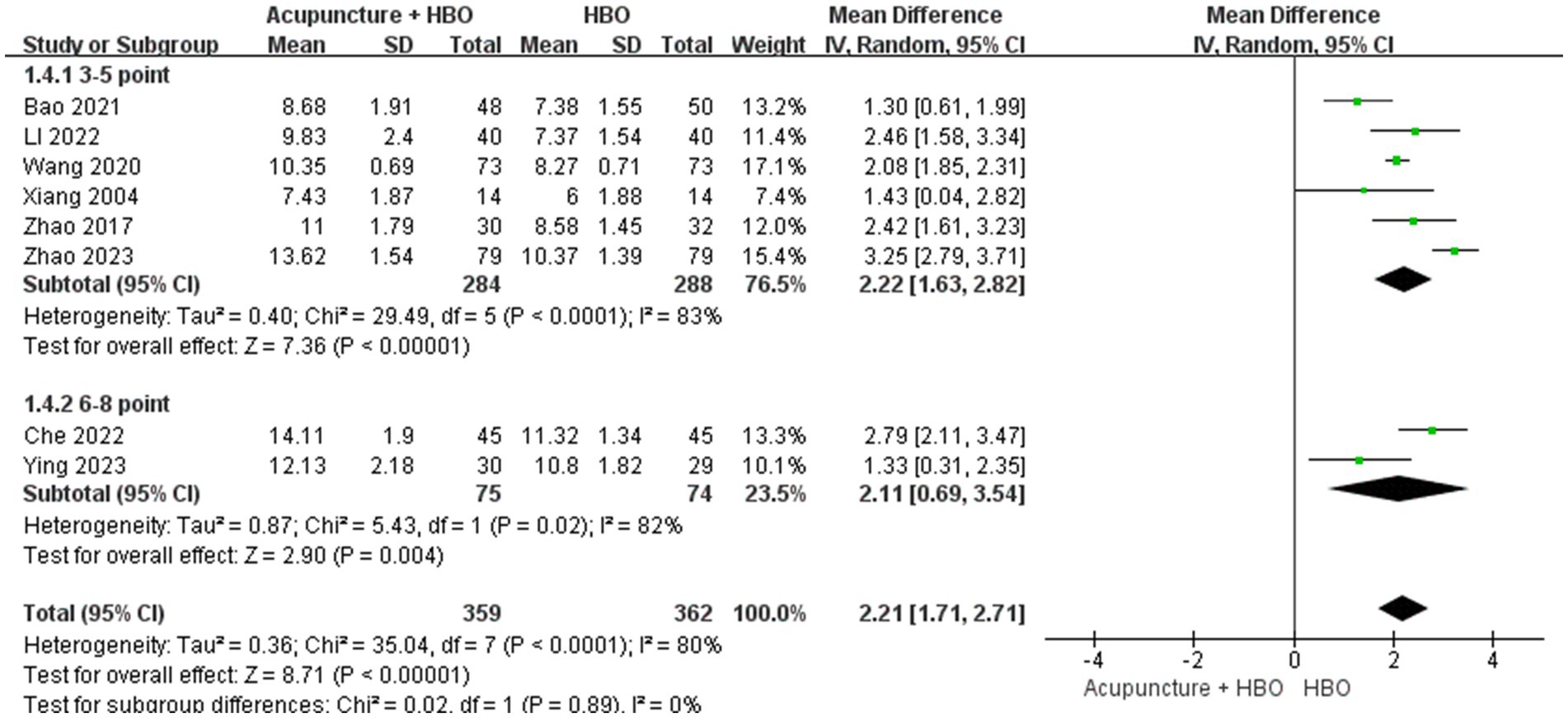
Figure 7. Forest plot of effects of acupuncture combined with HBO versus HBO alone on GCS score (Subgroup by the different varying degrees of severe TBI). MD > 0 indicates that the acupuncture combined with HBO group demonstrated higher GCS scores.
Notably, temporal heterogeneity remained unresolved. Although the 7- to 14-day post-injury window has been proposed as a critical period for neurological recovery in severe TBI (31), significant variability existed in time-to-intervention across original studies. To address this, we stratified the nine studies into early (≤14 days post-injury, n = 2) and late (>14 days, n = 7) intervention subgroups. Random-effects meta-analysis revealed substantial between-subgroup heterogeneity (p < 0.00001, I2 = 92.6%), with the early intervention subgroup demonstrating superior GCS improvement (MD = 3.09, 95% CI: 2.66–3.52) compared to the late subgroup (MD = 1.86, 95% CI: 1.47–2.25) (Figure 8).
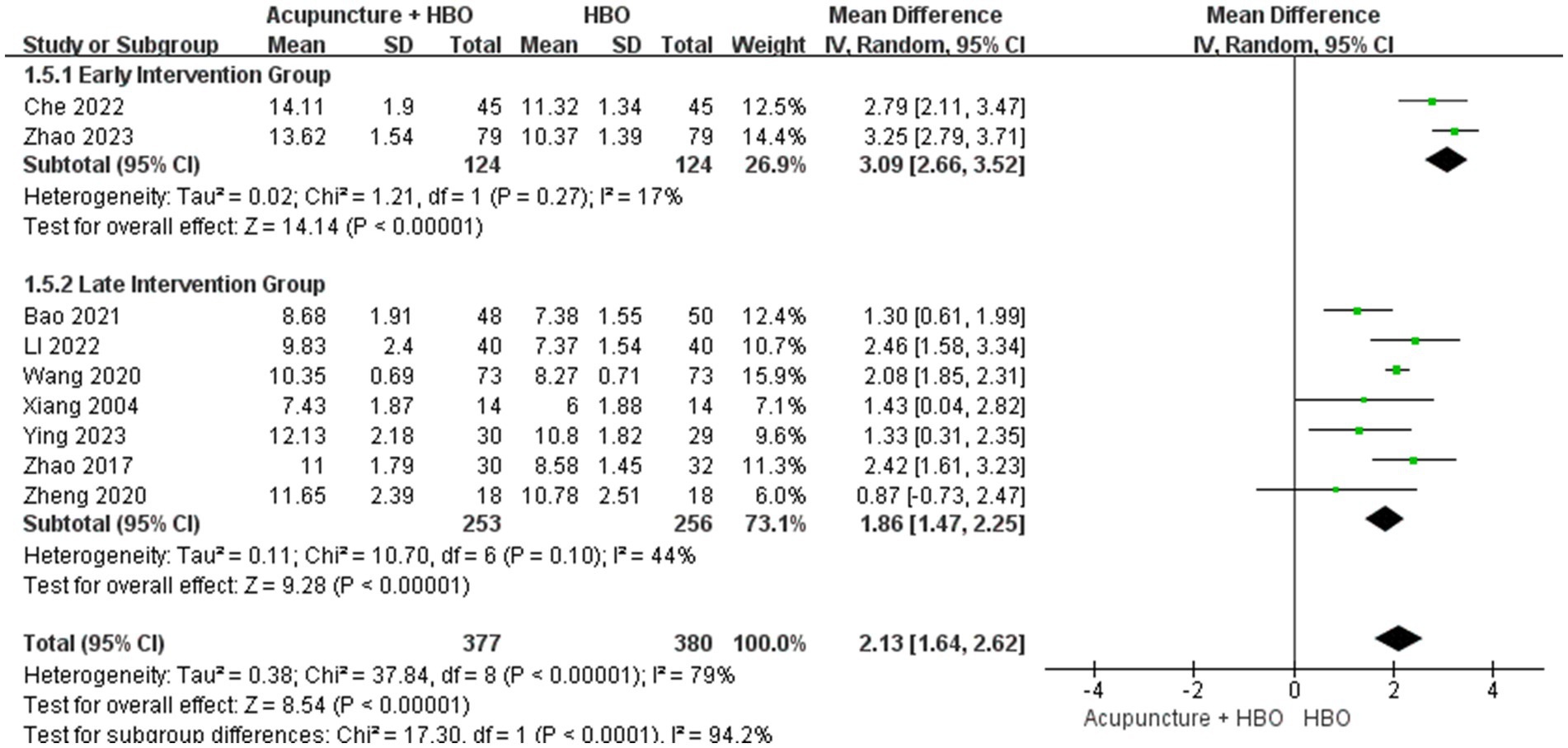
Figure 8. Forest plot of effects of acupuncture combined with HBO versus HBO alone on GCS score (Subgroup by the different acupoint combination). MD > 0 indicates that the acupuncture combined with HBO group demonstrated higher GCS scores.
3.5.2 Consciousness rate
Four studies implementing acupuncture combined with HBO reported the CR (19, 21, 26, 29). Among the 193 patients included in the control groups in these studies, 25 were awake after treatment, resulting in a CR of 12.95%. Among the 193 patients included in the test groups, 57 were awake, resulting in a CR of 29.53%. There was no significant heterogeneity among the studies (p = 0.73, I2 = 0). The results indicated a substantial difference in the post-treatment CR between the two groups (RR = 2.26, 95% CI: 1.48 to 3.46, p = 0.0002) (Figure 9).
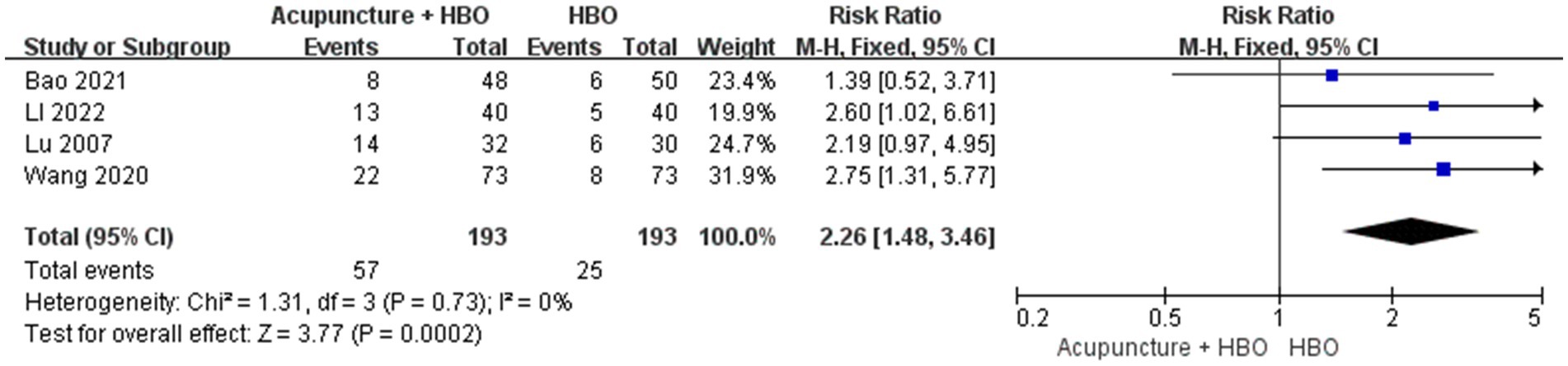
Figure 9. Forest plot of effects of acupuncture combined with HBO versus HBO alone on Consciousness rate. RR > 1 indicates that the acupuncture combined with HBO group demonstrated higher CR.
3.5.3 Effective rate
Four studies reported the ER (20, 24, 26–28). A total of 203 individuals were enrolled in the control group, while 110 patients exhibited a favourable prognosis for an ER of 54.19%. A total of 205 individuals were enrolled in the control group, while 163 patients exhibited a favourable prognosis for an ER of 79.51%. No significant heterogeneity was observed among the studies (p = 0.27, I2 = 23). Consequently, a fixed-effects model was employed in the meta-analysis. The results indicated that there was a significant difference in the RR between the two groups (RR = 1.47, 95% CI: 1.27 to 1.69, p < 0.00001) (Figure 10).
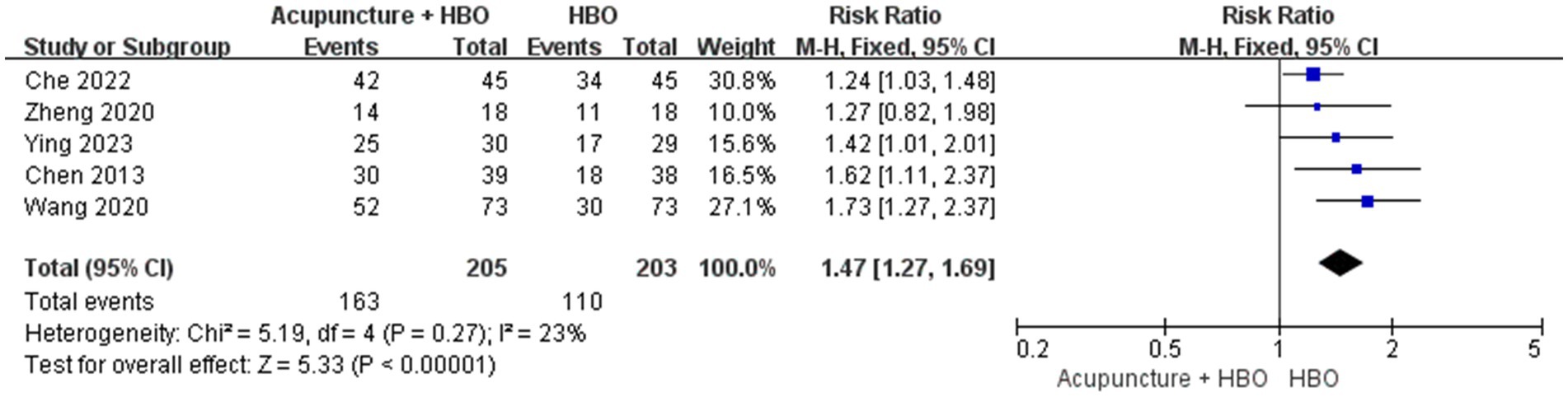
Figure 10. Forest plot of effects of acupuncture combined with hyperbaric oxygenation versus hyperbaric oxygenation alone on Effective rate. RR > 1 indicates that the acupuncture combined with HBO group demonstrated higher ER.
3.6 Side effects and adverse events
Only one study (23) reported that some patients who received acupuncture treatment experienced pain and fever, though there was no attrition.
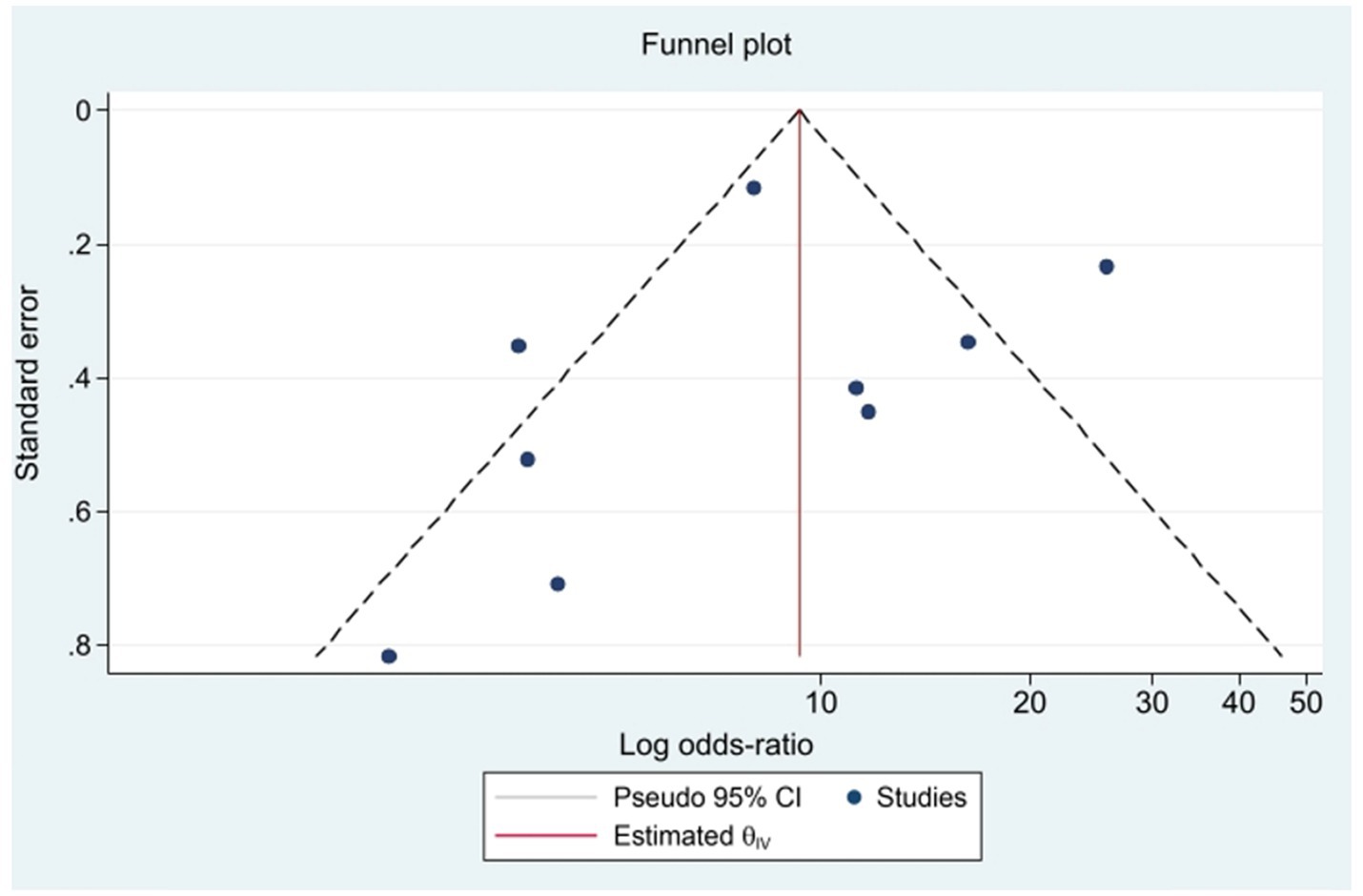
3.7 Publication bias
When the number of samples included in the GCS score change exceeded 8, an inverted funnel plot was drawn. Figure 11 shows the funnel plot, which appears symmetrical. Egger’s regression test and Begg’s funnel plot asymmetry test yielded p values > 0.05 for all tests, indicating the absence of significant publication bias.
4 Discussion
This study presents the first systematic meta-analysis evaluating the synergistic effects of acupuncture combined with HBO in TBI. Pooled data from 11 randomized controlled trials (n = 896 patients) demonstrated significantly more significant improvement in GCS scores with combination therapy (MD = 2.13, 95% CI: 1.64–2.62, p < 0.001), with the EA subgroup exhibiting the highest effect size (MD = 2.15, 95% CI: 1.95–2.36). These findings provide critical evidence for clinical translation, suggesting that EA-HBO combination therapy may overcome therapeutic resistance in severe TBI patients (GCS ≤ 8) refractory to conventional treatments.
The superior efficacy of EA may stem from its dual neuromodulatory mechanisms: (1). Electrical pulse stimulation enhances acupoint-mediated regulation of central neural circuits, potentially through increased neurotrophic factor release (e.g., BDNF) and cerebral blood flow optimization (32); (2). Direct current stimulation may reactivate residual neuronal networks in lesioned areas (33), creating spatiotemporal synergy with HBO’s neurorestorative effects through oxygen metabolism potentiation.
Subgroup analyses further elucidated critical effect modifiers: baseline injury severity and therapeutic timing. The very severe TBI subgroup (GCS 3–5) exhibited greater precision (CI Δ = 1.19 vs. 2.85), potentially attributable to lower therapeutic response thresholds (e.g., pupillary reflex recovery conferring disproportionate GCS gains), whereas the severe subgroup (GCS 6–8) required higher-order functional recovery (e.g., verbal response). Early intervention demonstrated superior efficacy (MD = 3.09 vs. 1.86), suggesting temporally stratified biological mechanisms: (1). Acute phase (≤14 days): Elevated blood–brain barrier permeability (34) enhances HBO-mediated oxygen diffusion, while acupuncture potentiates synaptic remodelling (35); (2). Microglial phenotypic shift from pro-inflammatory M1 to reparative M2 dominates (36), fostering anti-inflammatory niches; (3). Chronic phase (>14 days): Astroglial scar formation increases extracellular matrix stiffness, biomechanically impeding therapeutic agent delivery (37).
The conclusions of this study align with prior evidence while advancing the field methodologically. A 2018 meta-analysis (38) confirmed acupuncture’s efficacy in improving TBI-related consciousness disorders (RR = 1.58), but critical limitations persist: it neither stratified outcomes by acupuncture modality nor assessed combination therapies, and included studies only up to 2018, limiting its applicability to contemporary multimodal therapeutic strategies.
Having established the clinical superiority of combination therapy, elucidating its underlying synergistic mechanisms becomes pivotal for guiding precision treatment. Although numerous studies have proposed potential mechanisms of acupuncture or HBO monotherapy in TBI, research explicitly investigating the synergistic mechanisms of their combined application remains limited. Based on existing evidence, we hypothesize that the synergistic mechanisms of combined acupuncture-HBO therapy may involve the following dimensions: (1) HBO therapy enhances cerebral oxygen supply and optimizes metabolic homeostasis (39), thereby establishing an oxygen-enriched microenvironment that potentiates acupuncture-mediated neurotransmitter regulation and metabolic modulation (40); (2). The combined therapy of acupuncture and HBO exerts multi-pathway, multitarget anti-inflammatory effects, effectively mitigating cerebral tissue damage (41–43); (3) Both modalities enhance systemic antioxidant capacity, and their combined use synergistically augments free radical scavenging efficacy, thereby mitigating oxidative damage to cerebral tissue (44, 45). (4) The combination therapy promotes neuroplasticity through complementary mechanisms: HBO establishes an oxygen-repleted microenvironment post-hypoxia (46), while acupuncture directly enhances neuronal excitability and synaptic plasticity (47). (5) The combined therapy exerts neuroprotective effects by suppressing neuronal injury and apoptosis through distinct molecular pathways (48, 49). In summary, the synergistic mechanisms underlying the combined treatment of acupuncture and hyperbaric oxygen (HBO) therapy for traumatic brain injury (TBI) exhibit multi-dimensional and multitarget characteristics. However, these current hypotheses are predominantly based on experimental studies investigating their individual effects. Future research necessitates additional experimental studies and clinical trials to validate further and clarify the synergistic mechanisms of this combined therapeutic approach.
However, the reliability of evidence in this study is constrained by methodological limitations. Three studies (22, 26, 28) failed to describe randomization details, and all included studies lacked allocation concealment and blinding, resulting in elevated risks of selection bias and detection bias. Although subgroup analyses demonstrated significant GCS score improvement with manual acupuncture combined with HBO (MD = 1.59, 95% CI: 1.12–2.05) and superior consciousness recovery rates with the combination therapy (RR = 2.26, 95% CI:1.48–3.46), the wide confidence intervals indicate residual uncertainty, which likely stems from small-sample effects (only four studies were included across analyses, minimum sample size n = 36) and rare-event bias (limited awakening cases post-combination therapy in comatose TBI patients). The future studies must rigorously adhere to CONSORT guidelines by conducting large-scale RCTs with standardized interventions, explicitly reporting stimulation parameters, and implementing enhanced methodologies: double-blinding protocols, blockchain-based centralized randomization systems for real-time encrypted allocation sequencing, and auditable allocation processes with tamper-proof documentation.
5 Conclusion
In conclusion, our meta-analysis results indicate that the combination of acupuncture with HBO exerts a positive influence on GCS scores, CR, and ER in patients with TBI. However, given the limited availability of high-quality evidence and the dearth of RCTs in this area, our ability to definitively evaluate the comparative efficacy of acupuncture in conjunction with HBO versus HBO monotherapy for TBI treatment is compromised.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
GL: Investigation, Project administration, Software, Visualization, Writing – original draft. BW: Data curation, Formal analysis, Writing – original draft. SF: Data curation, Software, Writing – original draft. SL: Methodology, Software, Writing – original draft. LS: Methodology, Software, Writing – original draft. CL: Data curation, Resources, Writing – original draft. YF: Data curation, Software, Writing – original draft. JL: Methodology, Writing – original draft. MQ: Validation, Writing – original draft. YZ: Resources, Writing – original draft. LP: Funding acquisition, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Innovative Scientific Research Project of “key support and characteristic discipline of Yunnan first-class discipline traditional Chinese Medicine” (grant numbers 30371103900) and the Department of Science and Technology of Yunnan Province (grant numbers 202101AY070001-277 and 30360204700).
Acknowledgments
The authors express their deep gratitude to the committed researchers and respected institutions who have worked to create these valuable databases.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1538740/full#supplementary-material
References
1. Nelson, LD, Temkin, NR, Barber, J, Brett, BL, Okonkwo, DO, McCrea, MA, et al. TRACK-TBI Investigators. Functional Recovery, Symptoms, and Quality of Life 1 to 5 Years After Traumatic Brain Injury. JAMA Netw Open. (2023). 6:e233660. doi: 10.1001/jamanetworkopen.2023.3660
2. Maas, AIR, Menon, DK, Manley, GT, Abrams, M, Åkerlund, C, Andelic, N, et al. InTBIR participants and investigators. Traumatic brain injury: progress and challenges in prevention, clinical care, and research. Lancet Neurol. (2022) 21:1004–60. doi: 10.1016/S1474-4422(22)00309-X
3. Weaver, LK, Ziemnik, R, Deru, K, and Russo, AA. A double-blind randomized trial of hyperbaric oxygen for persistent symptoms after brain injury. Sci Rep. (2025) 15:6885. doi: 10.1038/s41598-025-86631-6
4. Wan, X, Zhang, Y, Li, Y, and Song, W. An update on noninvasive neuromodulation in the treatment of patients with prolonged disorders of consciousness. CNS Neurosci Ther. (2024) 30:e14757. doi: 10.1111/cns.14757
5. Kowalski, RG, Hammond, FM, Weintraub, AH, Nakase-Richardson, R, Zafonte, RD, Whyte, J, et al. Recovery of consciousness and functional outcome in moderate and severe traumatic brain injury. JAMA Neurol. (2021) 78:548–57. doi: 10.1001/jamaneurol.2021.0084
6. Mollica, A, Thaut, M, and Burke, MJ. Proposing music-based interventions for the treatment of traumatic brain injury symptoms: current evidence and future directions. Can. J Psychiatry. (2021) 66:707–9. doi: 10.1177/07067437211007811
7. Kamimoto, T, Hosoi, Y, Tanamachi, K, Yamamoto, R, Yamada, Y, Teramae, T, et al. Combined ankle robot training and robot-assisted gait training improved the gait pattern of a patient with chronic traumatic brain injury. Prog Rehabil Med. (2023) 8:20230024. doi: 10.2490/prm.20230024
8. Flint, RD, Li, Y, Wang, PT, Vaidya, M, Barry, A, Ghassemi, M, et al. Noninvasively recorded high-gamma signals improve synchrony of force feedback in a novel neurorehabilitation brain-machine interface for brain injury. J Neural Eng. (2022) 19:10. doi: 10.1088/1741-2552/ac7004
9. Lippert, J, and Guggisberg, AG. Diagnostic and therapeutic approaches in neurorehabilitation after traumatic brain injury and disorders of consciousness. Clin Transl Neurosci. (2023) 7:21. doi: 10.3390/ctn7030021
10. Xi, MH, Wang, L, Zhang, W, Zheng, QH, Qin, HY, and Yan, XY. Progress in research on the mechanism of acupuncture regulating programmed cell death of neurons. J Chongqing Med Univ. (2024) 49:362–9. doi: 10.13406/j.cnki.cyxb.003461
11. Lin, CC, Chen, HY, Tseng, CY, and Yang, CC. Effect of acupuncture on recovery of consciousness in patients with acute traumatic brain injury: a multi-institutional cohort study. Healthcare. (2023) 11:2267. doi: 10.3390/healthcare11162267
12. Chen, Y, Wang, L, You, W, Huang, F, Jiang, Y, Sun, L, et al. Hyperbaric oxygen therapy promotes consciousness, cognitive function, and prognosis recovery in patients following traumatic brain injury through various pathways. Front Neurol. (2022) 13:929386. doi: 10.3389/fneur.2022.929386
13. Cannellotto, M, Yasells García, A, and Landa, MS. Hyperoxia: effective mechanism of hyperbaric treatment at mild-pressure. Int J Mol Sci. (2024) 25:777. doi: 10.3390/ijms25020777
14. Schimmel, S, El Sayed, B, Lockard, G, Gordon, J, Young, I, D'Egidio, F, et al. Identifying the target traumatic brain injury population for hyperbaric oxygen therapy. Int J Mol Sci. (2023) 24:14612. doi: 10.3390/ijms241914612
15. Page, MJ, Mckenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 18:n71. doi: 10.1371/journal.pmed.1003583
16. Higgins, J, Sterne, J, Savovi, J, Page, M, Hrbjartsson, A, Boutron, I, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. (2016) 10:CD201601.
17. Teasdale, G, and Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet. (1974) 304:81–4. doi: 10.1016/S0140-6736(74)91639-0
18. Manley, GT, and Maas, AI. The Glasgow coma scale at 50: looking back and forward. Lancet. (2024) 404:734–5. doi: 10.1016/S0140-6736(24)01596-4
19. Li, SX, Wang, QL, Liang, LB, and Wu, JL. Analysis of the awakening effect of acupuncture with the meridian flow method on patients in vegetative state with severe craniocerebral injury. Chin J Folk Therapy. (2022) 30:33–6. doi: 10.19621/j.cnki.11-3555/r.2022.1411
20. Ying, MJ, Chen, S, Lv, ZL, Lai, ZL, Lai, YM, and Xu, J. Clinical observation on the treatment of patients with impaired consciousness due to craniocerebral injury by acupuncture combined with hyperbaric oxygen therapy. Chin J Emerg Med. (2023) 32:307–10. doi: 10.3969/j.issn.1004-745X.2023.02.032
21. Bao, YC, Zhang, F, Li, Q, Liu, M, Chen, XR, and Zhang, YB. Effect of “Xingnao Kaiqiao” acupuncture therapy on patients with cerebral trauma in vegetative state. J China Acupunct. (2021) 41:1225–8. doi: 10.13703/j.0255-2930.20201101-k0002
22. Zhao, HL, Lan, BL, and Pan, Y. Effect of acupuncture combined with hyperbaric oxygen on postoperative consciousness and neurological function in patients with craniocerebral injury. New TCM. (2023) 55:176–9. doi: 10.13457/j.cnki.jncm.2023.10.036
23. Xiang, ZX, Xie, ZY, Zhuang, MH, Bai, Y, and Ding, S. Effect of electroacupuncture and hyperbaric oxygen therapy on neurological function recovery in patients with protracted coma. China Clin Rehabilit. (2004) 28:6130–1. doi: 10.3321/j.issn:1673-8225.2004.28.072
24. Zheng, JC, and Zhang, J. Observation on the curative effect of Tongdu Xingnao acupuncture combined with hyperbaric oxygen on disturbance of consciousness after craniocerebral injury. J Integrat Tradit Chin Western Med Cardiovasc Dise. (2020) 18:3887–9. doi: 10.12102/j.issn.1672-1349.2020.22.042
25. Zhao, B, Dou, LN, Xiao, HB, Shao, J, LI, LY, and Wang, LY. Clinical study on the effect of electroacupuncture combined with hyperbaric oxygen on awakening in coma patients after brain injury. Contemp Med. (2017) 23:116–7. doi: 10.3969/j.issn.1009-4393.2017.36.051
26. Wang, DD, Pang, M, and Wang, H. Effect of electroacupuncture stimulation on coma degree in patients with protracted coma due to severe craniocerebral injury and its mechanism. Modern J Integrat Tradit Chin Western Med. (2020) 29:51–4. doi: 10.3969/j.issn.1008-8849.2020.01.012
27. Che, Y, Jiang, Y, Lin, LQ, Sun, Q, and Lu, SY. Application of electroacupuncture assisted hyperbaric oxygen in coma patients after cerebral trauma. Anhui Med. (2022) 26:2077–81. doi: 10.3969/j.issn.1009-6469.2022.10.039
28. Chen, L, Zhu, YY, Zhou, JM, and Li, C. Treatment of 39 cases of coma after cerebral trauma with integrated traditional Chinese and Western medicine. Modern Dist Educ TCM China. (2013) 11:62–3. doi: 10.3969/j.issn.1672-2779.2013.17.047
29. Lu, YZ, Zhou, JH, Lu, H, Chen, G, Tang, ZF, and Wu, WJ. Clinical observation on electroacupuncture at Xingnao Kaiqiao point for treating 32 cases of persistent vegetative state after craniocerebral trauma. Jiangsu TCM. (2007) 2:43–5. doi: 10.3969/j.issn.1672-397X.2007.02.025
30. McCrea, MA, Giacino, JT, Barber, J, Temkin, NR, Nelson, LD, Levin, HS, et al. Functional outcomes over the first year after moderate to severe traumatic brain injury in the prospective, longitudinal TRACK-TBI study. JAMA Neurol. (2021) 78:982–92. doi: 10.1001/jamaneurol.2021.2043
31. Wu, X, Xie, L, Lei, J, Yao, J, Li, J, Ruan, L, et al. Acute traumatic coma awakening by right median nerve electrical stimulation: a randomised controlled trial. Intensive Care Med. (2023) 49:633–44. doi: 10.1007/s00134-023-07072-1
32. Wang, L, Su, XT, Yang, NN, Wang, QY, Yang, JW, and Liu, CZ. Electroacupuncture improves cerebral blood flow in pMCAO rats during acute phase via promoting leptomeningeal collaterals. J Cereb Blood Flow Metab. (2025):271678X241270240. doi: 10.1177/0271678X241270240
33. Yang, Y, Xu, HY, Deng, QW, Wu, GH, Zeng, X, Jin, H, et al. Electroacupuncture facilitates the integration of a grafted TrkC-modified mesenchymal stem cell-derived neural network into transected spinal cord in rats via increasing neurotrophin-3. CNS Neurosci Ther. (2021) 27:776–91. doi: 10.1111/cns.13638
34. Gouvea Bogossian, E, Peluso, L, Creteur, J, and Taccone, FS. Hyperventilation in adult TBI patients: how to approach it? Front Neurol. (2021) 11:580859. doi: 10.3389/fneur.2020.580859
35. Dai, Y, Zhang, Y, Yang, M, Lin, H, Liu, Y, Xu, W, et al. Electroacupuncture increases the hippocampal synaptic transmission efficiency and Long-term plasticity to improve vascular cognitive impairment. Mediat Inflamm. (2022) 2022:5985143–15. doi: 10.1155/2022/5985143
36. Chio, CC, Lin, MT, and Chang, CP. Microglial activation as a compelling target for treating acute traumatic brain injury. Curr Med Chem. (2015) 22:759–70. doi: 10.2174/0929867321666141106124657
37. Vangansewinkel, T, Lemmens, S, Tiane, A, Geurts, N, Dooley, D, Vanmierlo, T, et al. Therapeutic administration of mouse mast cell protease 6 improves functional recovery after traumatic spinal cord injury in mice by promoting remyelination and reducing glial scar formation. FASEB J. (2023) 37:e22939. doi: 10.1096/fj.202201942RR
38. Zhang, Q, Liu, J, Cao, R, and Jin, Y. Acupuncture for patients in coma after traumatic brain injury: systematic review and meta-analysis. Altern Ther Health Med. (2020) 26:50–7.
39. Fischer, I, and Barak, B. Molecular and therapeutic aspects of hyperbaric oxygen therapy in neurological conditions. Biomol Ther. (2020) 10:1247. doi: 10.3390/biom10091247
40. Dai, R, Xu, W, Zhu, X, Sun, R, Cheng, L, Cui, L, et al. Acupuncture improves neuroendocrine defects in a preclinical rat model of reproductive aging. Life Sci. (2024) 357:123102. doi: 10.1016/j.lfs.2024.123102
41. Sunshine, MD, Bindi, VE, Nguyen, BL, Doerr, V, Boeno, FP, Chandran, V, et al. Oxygen therapy attenuates neuroinflammation after spinal cord injury. J Neuroinflammation. (2023) 20:303. doi: 10.1186/s12974-023-02985-6
42. Tsai, CY, Liao, WL, Wu, HM, Chang, CW, Chen, WL, and Hsieh, CL. Acupuncture improves neurological function and anti-inflammatory effect in patients with acute ischemic stroke: a double-blinded randomized controlled trial. Complement Ther Med. (2024) 82:103049. doi: 10.1016/j.ctim.2024.103049
43. Wang, Y, Chen, Y, Meng, L, Wu, B, Ouyang, L, Peng, R, et al. Electro-acupuncture treatment inhibits the inflammatory response by regulating γδ T and Treg cells in ischemic stroke. Exp Neurol. (2023) 362:114324. doi: 10.1016/j.expneurol.2023.114324
44. André-Lévigne, D, Pignel, R, Boet, S, Jaquet, V, Kalbermatten, DF, and Madduri, S. Role of oxygen and its radicals in peripheral nerve regeneration: from hypoxia to physoxia to hyperoxia. Int J Mol Sci. (2024) 25:2030. doi: 10.3390/ijms25042030
45. Xue, C, Kui, W, Huang, A, Li, Y, Li, L, Gu, Z, et al. Electroacupuncture suppresses neuronal ferroptosis to relieve chronic neuropathic pain. J Cell Mol Med. (2024) 28:e18240. doi: 10.1111/jcmm.18240
46. Yao, L, Ye, Q, Liu, Y, Yao, S, Yuan, S, Xu, Q, et al. Electroacupuncture improves swallowing function in a post-stroke dysphagia mouse model by activating the motor cortex inputs to the nucleus tractus solitarii through the parabrachial nuclei. Nat Commun. (2023) 14:810. doi: 10.1038/s41467-023-36448-6
47. Kan, B, Dong, Z, Tang, Z, Zhao, L, and Li, Z. Acupuncture improves synaptic plasticity of SAMP8 mice through the RhoA/ROCK pathway. Curr Alzheimer Res. (2023) 20:420–30. doi: 10.2174/1567205020666230828095826
48. Wang, SD, Fu, YY, Han, XY, Yong, ZJ, Li, Q, Hu, Z, et al. Hyperbaric oxygen preconditioning protects against cerebral ischemia/reperfusion injury by inhibiting mitochondrial apoptosis and energy metabolism disturbance. Neurochem Res. (2021) 46:866–77. doi: 10.1007/s11064-020-03219-4
Keywords: acupuncture, hyperbaric oxygenation, traumatic brain injury, Glasgow Coma Scale, systematic review, meta-analysis
Citation: Li G, Wang B, Fan S, Liu S, Shao L, Li C, Fang Y, Li J, Qiu M, Zhang Y and Pan L (2025) The effect of acupuncture combined with hyperbaric oxygenation compared with hyperbaric oxygenation alone for patients with traumatic brain injury: a systematic review and meta-analysis. Front. Neurol. 16:1538740. doi: 10.3389/fneur.2025.1538740
Edited by:
Jane McDevitt, Temple University, United StatesReviewed by:
Bradley Dengler, Uniformed Services University of the Health Sciences, United StatesYaoyao Bian, Nanjing University of Chinese Medicine, China
Copyright © 2025 Li, Wang, Fan, Liu, Shao, Li, Fang, Li, Qiu, Zhang and Pan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Pan, MTE5NTg3MDE0QHFxLmNvbQ==
†These authors share first authorship
 Geng Li
Geng Li Binyang Wang
Binyang Wang Shuochen Fan
Shuochen Fan Shuangli Liu1
Shuangli Liu1 Chuanxiong Li
Chuanxiong Li Lei Pan
Lei Pan