- 1School of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan, China
- 2Department of Rehabilitation, Jinan Children's Hospital, Jinan, China
Objective: Cerebral palsy (CP), a pediatric neuromotor disorder, profoundly impacts functional independence and participation. Virtual reality (VR) has developed as a potential neurorehabilitation tool, yet its therapeutic efficacy remains inconsistently validated. This overview aims to synthesize evidence from systematic reviews (SRs) and meta-analyses (MAs) to evaluate VR’s effectiveness in CP rehabilitation.
Methods: Systematic searches across ten databases—Embase, Web of Science, Cochrane Library, PubMed, CINAHL, JBI, China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database (VIP), China Bio-Medical Literature Service System (Sino-Med), and Wanfang Database—identified SRs/MAs on VR for CP from inception to November 10, 2024. The duplicate rate of primary studies was assessed by calculating the corrected covered area (CCA) through the establishment of a literature overlap matrix. Methodological rigor, reporting quality, bias risk, and evidence quality were appraised using the Assessment of Multiple Systematic Reviews 2 (AMSTAR-2), the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 (PRISMA2020), the Risk of Bias in Systematic Reviews (ROBIS), and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tools, respectively.
Results: Sixteen SRs/MAs (5 low quality, 11 very low quality, according to AMSTAR-2) were included. The CCA was calculated as 0.135, indicating a high degree of overlap. PRISMA 2020 compliance revealed incomplete reporting in 37% of items. ROBIS indicated low bias risk in 13 studies. GRADE assessments classified 58 outcomes: 9 moderate (15.5%), 21 low (36.2%), and 28 very low (48.3%) quality. VR demonstrated clinical potential for improving motor function and activities of daily living (ADL), particularly in younger children with higher intervention dosages. However, heterogeneity in outcome measures, CP subtypes, and VR protocols limited generalizability.
Conclusion: VR shows potential in improving motor dysfunction and ADL in CP. However, the included SRs/MAs typically exhibited low methodological and evidence quality. Therefore, caution must be taken when interpreting these findings. Moreover, high-quality randomized controlled trials and standardized VR protocols are urgently needed to establish evidence-based guidelines for CP rehabilitation.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024614631, CRD42024614631.
1 Introduction
Cerebral palsy (CP), a nonprogressive neurodevelopmental disorder originating from prenatal or perinatal brain insults, manifests as persistent motor and postural dysfunction with associated activity limitations (1). This central motor disorder is commonly comorbid with multisystem impairments, including sensory deficits, perceptual-cognitive dysfunction, communication-behavioral disorders, epilepsy, and secondary musculoskeletal pathologies (2). In the United States, large-scale surveys reported the prevalence of CP among children as 3.2 per 1,000 children aged 3–17 years, aligning with global estimates (3). Of note, the prevalence of pediatric physical disabilities overall, including conditions like cerebral palsy, varies by country, region, and population subgroup (4). Rehabilitation for children with CP aims to improve mobility, correct posture, and address abnormal movement patterns to enhance daily functioning (5). However, common barriers to adherence are fatigue, lack of motivation, and the repetitive or unengaging nature of traditional rehabilitation activities. Children are less likely to consistently participate in therapies that do not capture their interest or provide variety (6).
Virtual reality (VR) has developed as a promising neurorehabilitation tool for CP (7). VR is a three-dimensional, computer-generated virtual environment that supports work, education, entertainment, and health by simulating real-world or fictional settings and interactions (8). Currently, VR technologies are classified based on two primary dimensions: application type, which encompasses commercial systems versus rehabilitation-specific systems, and immersion level, ranging from non-immersive (screen-based interfaces) to semi-immersive (projection environments) and fully immersive configurations utilizing head-mounted displays (9). Notably, VR technologies can enhance emotionally relevant experiences and social interactions, offer safe, repeatable, and diversifiable interventions, and reduce anxiety levels in children (10). Neurophysiological studies reveal that when children display actions such as smiling, laughing, dancing, or screaming during virtual games, the bioelectrical signals in their brains reflect activation of the reward system, excitation of motor areas, and increased emotional and cognitive load. These changes are not only associated with the emotional experiences within the game but also linked to neuroplasticity in the brain (11). Furthermore, the VR training protocols, characterized by task-specific movement and adaptive difficulty modulation based on individualized capacity, enhance the transferability of motor skill acquisition to real-world functional task performance (12). VR systems also optimize rehabilitation dosing through patient-driven task selection, sustaining intrinsic motivation to achieve higher intervention intensity and frequency than traditional protocols (13). Moreover, the multisensory feedback mechanisms inherent in VR systems generate real-time performance metrics through audiovisual signals, enabling some degree of dynamic movement correction and contributing to improvements in motor skills (14). Collectively, these mechanisms address the International Classification of Functioning, Disability, and Health domains by mitigating environmental barriers and enhancing participation in educational and social contexts (15).
As evidence-based medicine has developed, researchers have performed an increasing number of systematic reviews (SRs) and meta-analyses (MAs) to assess the safety and effectiveness of VR for treating CP. However, due to differences in study design, limitations in sample size, and heterogeneity of outcomes, conflicting conclusions have emerged from various SRs/MAs, thereby compromising the reliability of the results. To address this issue, overviews of SRs use explicit and systematic methods to search for and identify multiple SRs on related research questions within the same topic area. Summarizing the evidence from multiple SRs allows for a more comprehensive analysis and summary of the findings, thereby providing higher quality evidence for clinical practice (16). This overview utilized the Assessment of Multiple Systematic Reviews 2 (AMSTAR-2) for methodological rigor evaluation (17), the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 (PRISMA2020) for reporting quality assessment (18), the Risk Of Bias In Systematic Reviews (ROBIS) for bias risk evaluation (19), and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) for evidence quality grading (20). Specifically, the AMSTAR-2 tool focuses on a comprehensive evaluation of methodological quality in SRs/MAs, identifying critical design flaws (17). The PRISMA 2020 checklist evaluates the clarity, completeness, and transparency of SRs/MAs reporting through its standardized framework that spans from study design to result presentation, thereby helping to identify critical information omissions (18). The ROBIS tool specializes in assessing bias risks in SRs/MAs, particularly identifying factors across various domains that may compromise the reliability of conclusions (19). The GRADE approach systematically classifies evidence quality by appraising the quality of evidence based on key factors, enabling clinicians and policymakers to evaluate the credibility and applicability of research findings (20). Through this integrative approach, the purpose of this overview is to assess the methodological quality, reporting quality, risk of bias, and quality of evidence of SRs/MAs of VR for CP and to objectively and comprehensively evaluate the efficacy and safety of VR for CP, thereby providing an evidence-based basis for clinical decision-making.
2 Methods
The methodology of this overview follows the Cochrane Handbook, and its report is in line with the PRISMA 2020 checklist. This overview has been prospectively registered on PROSPERO (CRD42024614631).
2.1 Inclusion and exclusion criteria
This research incorporated SRs/MAs of randomized controlled trials (RCTs) that exclusively examined VR-based interventions for pediatric CP. Eligible studies were required to (1) have participants who were diagnosed with cerebral palsy and were aged ≤18 years; (2) compare VR monotherapy or VR-augmented conventional rehabilitation against control groups receiving conventional therapy or no intervention; and (3) report quantitative outcomes in at least one functional domain, specifically upper extremity motor function, gross motor capacity, balance, ambulation, or activities of daily living (ADL). Exclusion criteria comprised SRs/MAs incorporating non-RCT designs, studies involving non-CP populations, studies with non-extractable data or inaccessible full texts, and non-Chinese/English literature.
2.2 Search strategy
A comprehensive search for literature was executed across ten online databases: Embase, Web of Science, Cochrane Library, PubMed, CINAHL, JBI, China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database (VIP), China Bio-Medical Literature Service System (Sino-Med), and Wanfang Database, targeting SRs/MAs evaluating VR interventions for CP. The search strategy includes Chinese and English terms, combining MeSH/Emtree terms and free-text keywords. Chinese search terms included “脑瘫” (cerebral palsy), “脑性瘫痪” (cerebral paralysis), “虚拟现实” (virtual reality), “虚拟环境” (virtual environment), “虚拟康复” (virtual rehabilitation), “虚拟游戏” (virtual gaming), “虚拟治疗” (virtual therapy), “系统评价” (systematic review), “Meta分析” (meta-analysis), “荟萃分析” (pooled analysis), “系统综述” (systematic overview), and “元分析” (meta-synthesis). English terms comprised “cerebral palsy,” “virtual reality,” “virtual reality exposure therapy,” “meta-analysis as topic,” “meta-analysis,” and “systematic review.” The search encompassed all available records from each database’s inception through November 10, 2024. The reference list was also manually screened to ensure comprehensiveness. Two reviewers independently conducted the literature search, and the search results were cross-checked. Discrepancies were resolved through consensus discussions. If conflicts remained unresolved, a third reviewer made the final decision. The complete search syntax, with database-specific adaptations, is detailed in Supplementary Material 1.
2.3 Study selection and data extraction
Duplicates were eliminated after importing the retrieved SRs/MAs to EndNote 21. Two independent reviewers performed a primary screening by reading the title and abstract and a secondary screening by reading the full text. Consensus discussions were employed to resolve discrepancies, with unresolved conflicts adjudicated by a third reviewer. Two reviewers independently extracted data from the included literature and cross-checked the results for accuracy. Extracted data included authors, publication year, country, number of included studies, sample size, CP subtypes, VR protocols, comparator therapies, risk of bias assessment tools, evidence quality instruments, adverse events, and outcome measures.
2.4 Overlapping of studies
To evaluate the degree of overlap among primary studies included in multiple SRs/MAs, a literature overlap matrix was constructed to calculate the corrected covered area (CCA) (21). This metric accounts for redundant inclusions by using the formula CCA = (n − r)/(rc − r), where n represents the total number of primary studies across all SRs/MAs, r denotes the number of unique primary studies after deduplication, and c indicates the number of SRs/MAs included in the study. The CCA values were interpreted as follows: 0–5% (slight overlap), 6–10% (moderate overlap), 11–15% (high overlap), and >15% (very high overlap).
2.5 Assessment methods
In the PROSPERO-registered protocol of this overview, we initially planned to assess the quality of SRs/MAs exclusively using AMSTAR-2 and GRADE. However, during implementation, we additionally incorporated the PRISMA 2020 checklist and ROBIS tool. We made this decision because AMSTAR-2 and GRADE alone could not comprehensively evaluate reporting quality or risk of bias. PRISMA 2020 provides a more rigorous assessment of reporting transparency, complementing AMSTAR-2’s methodological focus. ROBIS systematically addresses potential biases that neither AMSTAR-2 nor GRADE explicitly covers. This expansion aimed to enhance the robustness of our quality assessment framework. The included SRs/MAs were assessed independently by two reviewers, and the results were cross-checked. Consensus discussions were utilized to resolve discrepancies. A third reviewer then adjudicated any unresolved conflicts.
2.5.1 Methodological rigor assessment
We evaluated the methodological rigor of the included SRs/MAs using the AMSTAR-2, which comprises 16 appraisal items. Each item was rated as “Yes,” “No,” or “Partial Yes.” The final quality categorization was determined by 7 critical items (items 2, 4, 7, 9, 11, 13, and 15) according to the AMSTAR-2 criteria: High (no non-critical deficiencies or only one non-critical deficiency), Moderate (more than one non-critical deficiency), Low (one critical deficiency with or without non-critical deficiencies), and Critically Low (more than one critical deficiency with or without non-critical deficiencies) (17).
2.5.2 Report quality assessment
The PRISMA 2020 is based on PRISMA 2009 and has been revised through a rigorous literature review, expert consultation, and consensus conference, and its methodology is scientifically rigorous and highly credible. The PRISMA 2020 has a broader scope of application, primarily for systematic reviews assessing the effectiveness of health interventions, including those with and without meta-analyses. The completeness of reporting was assessed using the PRISMA 2020 checklist, comprising 27 reporting items across seven methodological domains. Each item was scored using a three-tiered classification system: full compliance, partial compliance, and non-compliance (18).
2.5.3 Risk of bias assessment
The ROBIS tool employs a three-phase structured evaluation protocol: Phase 1 (Relevance Assessment) examines the congruence between the review’s objectives and the research questions addressed. Phase 2 (Risk of Bias Determination) systematically evaluates four methodological domains: (1) eligibility criteria: whether predefined inclusion/exclusion criteria align logically with the research question; (2) search and selection: adequacy of literature retrieval strategies to minimize missed eligible studies; (3) data extraction and quality appraisal: rigor in data collection processes and validity of critical appraisal tools; (4) synthesis and presentation: appropriateness of statistical methods for data integration and result reporting. Phase 3 (final risk judgment): the overall bias risk is adjudicated by evaluating whether reviewers appropriately addressed the identified biases from Phase 2, critically appraised the relevance of the included studies to the research question, and avoided overemphasis on statistically significant outcomes. Each domain receives a categorical rating: high risk, low risk, or unclear risk (19).
2.5.4 Evidence quality assessment
The GRADE approach evaluates the quality of evidence across five dimensions: risk of bias, inconsistency, indirectness, imprecision, and publication bias. Specifically, risk of bias refers to the extent of systematic errors introduced during study design or execution, which may compromise the validity and reliability of findings. Consistency reflects the similarity of effect estimates across studies; significant variability between estimates indicates substantial inconsistency. Indirectness describes the applicability of study populations, interventions, or outcomes to the target clinical context; evidence is deemed indirect when direct extrapolation is unjustified. Imprecision arises when confidence intervals for effect estimates are extensive, reflecting substantial uncertainty. Publication Bias occurs when the likelihood of a study’s publication is influenced by statistical significance or effect magnitude, potentially skewing synthesized evidence. Final evidence quality is classified into four tiers: High (no downgrading), Moderate (1-level downgrade), Low (2-level downgrade), and Very Low (≥3-level downgrade), based on the cumulative impact of these dimensions (20).
3 Results
3.1 Search results
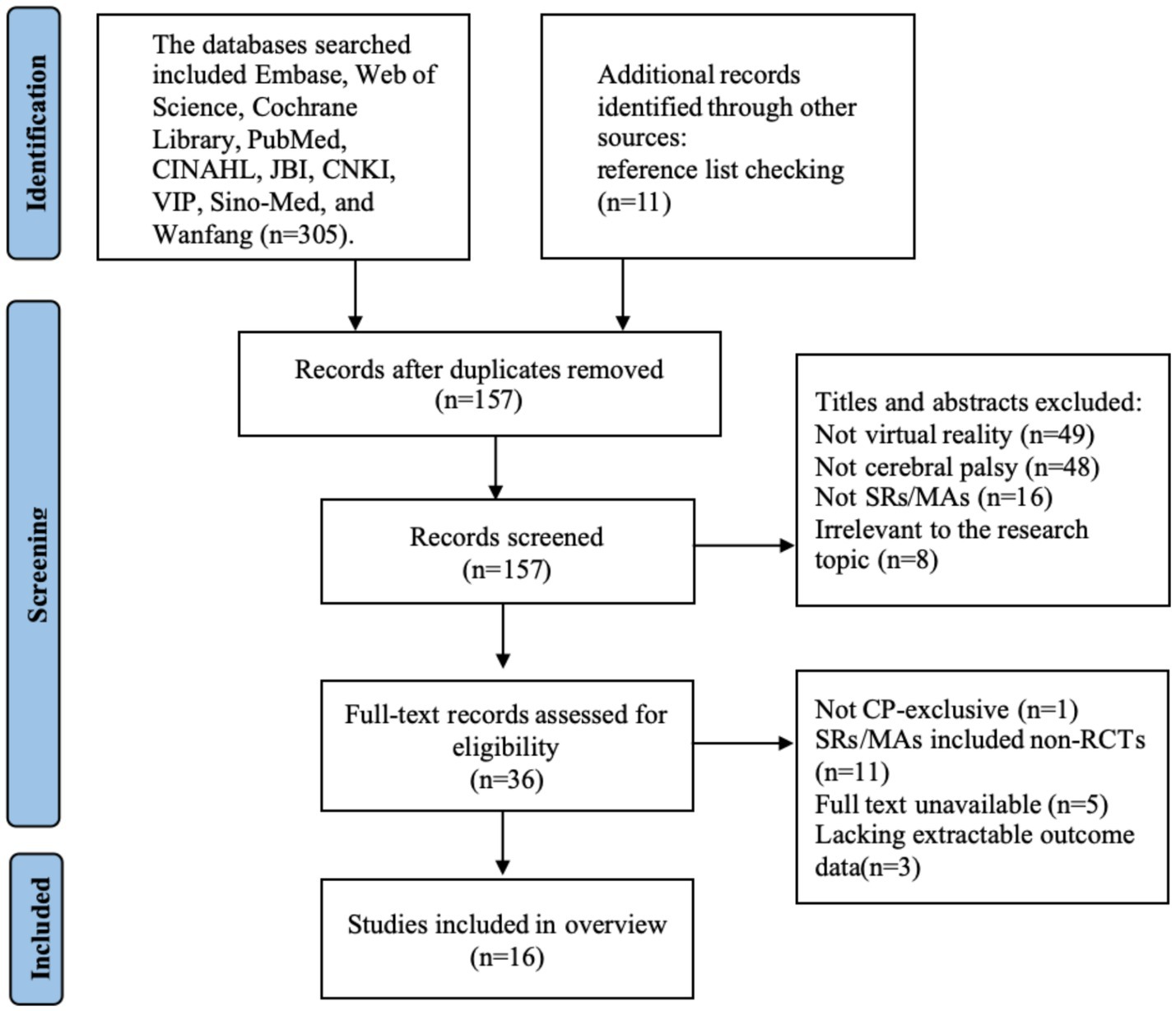
A total of 316 records were identified. During the systematic screening, 159 duplicate records were excluded, yielding 157 records for title/abstract screening. Applying predefined inclusion criteria, exclusions at this stage included non-virtual reality interventions (n = 49), non-cerebral palsy populations (n = 48), non-SRs/MAs (n = 16), and irrelevance to the research topic (n = 8), resulting in 36 records proceeding to full-text retrieval. Critical appraisal of full texts led to further exclusions: one study for mixed population inclusion, 11 SRs/MAs containing non-RCTs, five studies with inaccessible full texts, and three studies lacking extractable outcome data. Ultimately, 16 studies met eligibility criteria for final inclusion. The selection procedure is presented in Figure 1.
3.2 Literature characteristics
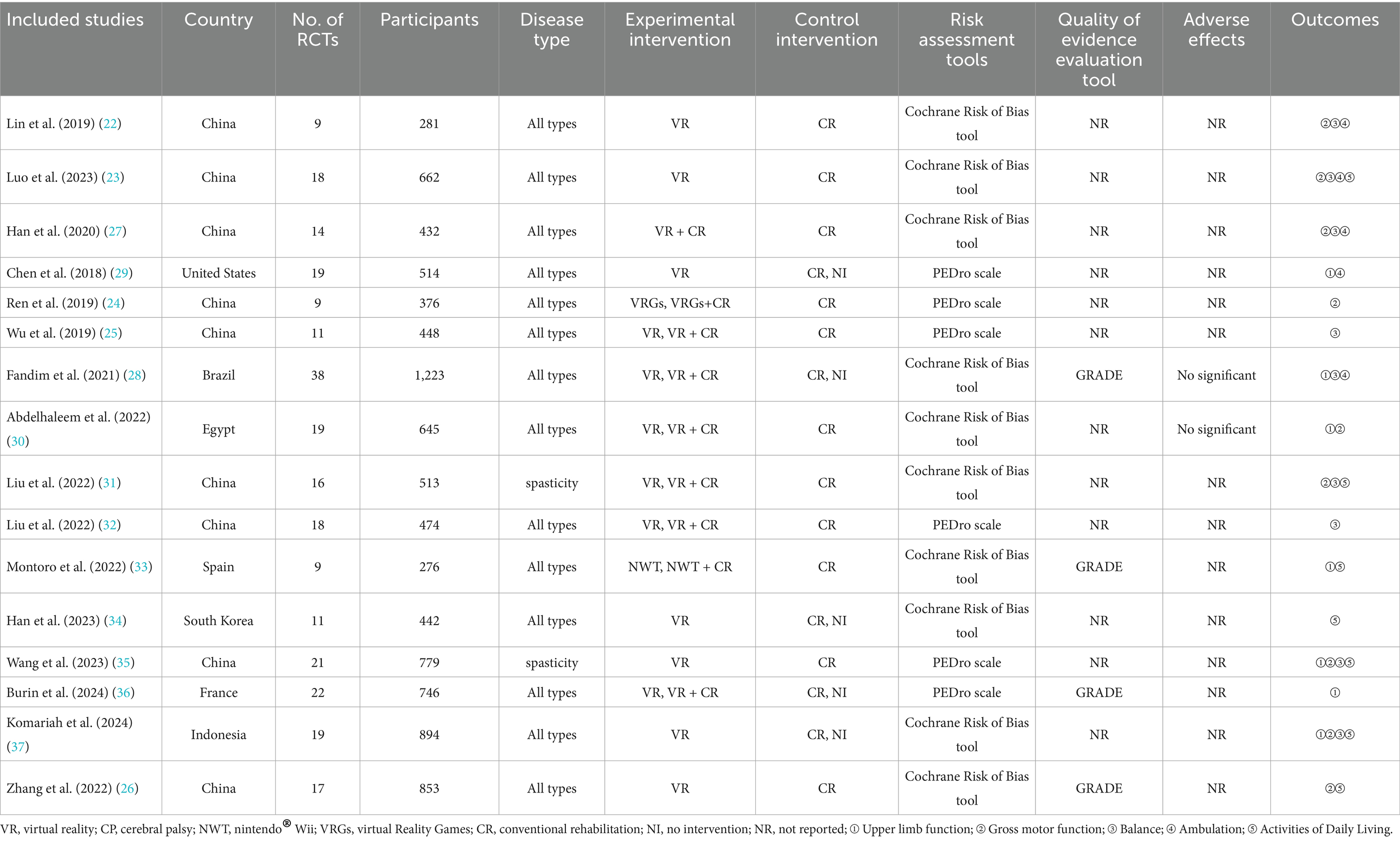
The 16 SRs/MAs comprised 13 English-language and 3 Chinese-language publications. Five studies (22–26) were classified as meta-analyses, two studies (27, 28) were classified as systematic reviews, and nine studies (29–37) were classified as a combination of systematic review and meta-analysis. Two SRs/MAs were specific to children with spastic CP, while the remaining encompassed all CP subtypes. The quantity of original RCTs per SR/MA ranged from 9 to 38, with aggregate sample sizes spanning 276 to 1,223 pediatric participants. The included SRs/MAs demonstrated variable focus across functional outcome domains: upper extremity motor function was evaluated in 7 SRs/MAs (28–30, 33, 35–37); gross motor function in 9 SRs/MAs (22–24, 26, 27, 30, 31, 35, 37); balance function in 9 SRs/MAs (22, 23, 25, 27, 28, 31, 32, 35, 37); ambulation function in 5 SRs/MAs (22, 23, 27–29); and ADL function in 7 SRs/MAs (23, 26, 31, 33–35, 37). The literature characteristics are detailed in Table 1.
3.3 Overlapping of studies
This study included a total of 16 SRs/MAs, encompassing 270 primary studies before deduplication and 89 unique studies after deduplication. The CCA was calculated as 0.135, indicating a high degree of overlap (Supplementary Materials 2 contains a spreadsheet used to calculate CCA). As the aim of this study was to summarize outcome measures rather than perform quantitative synthesis, no statistical methods were applied to address overlapping studies.
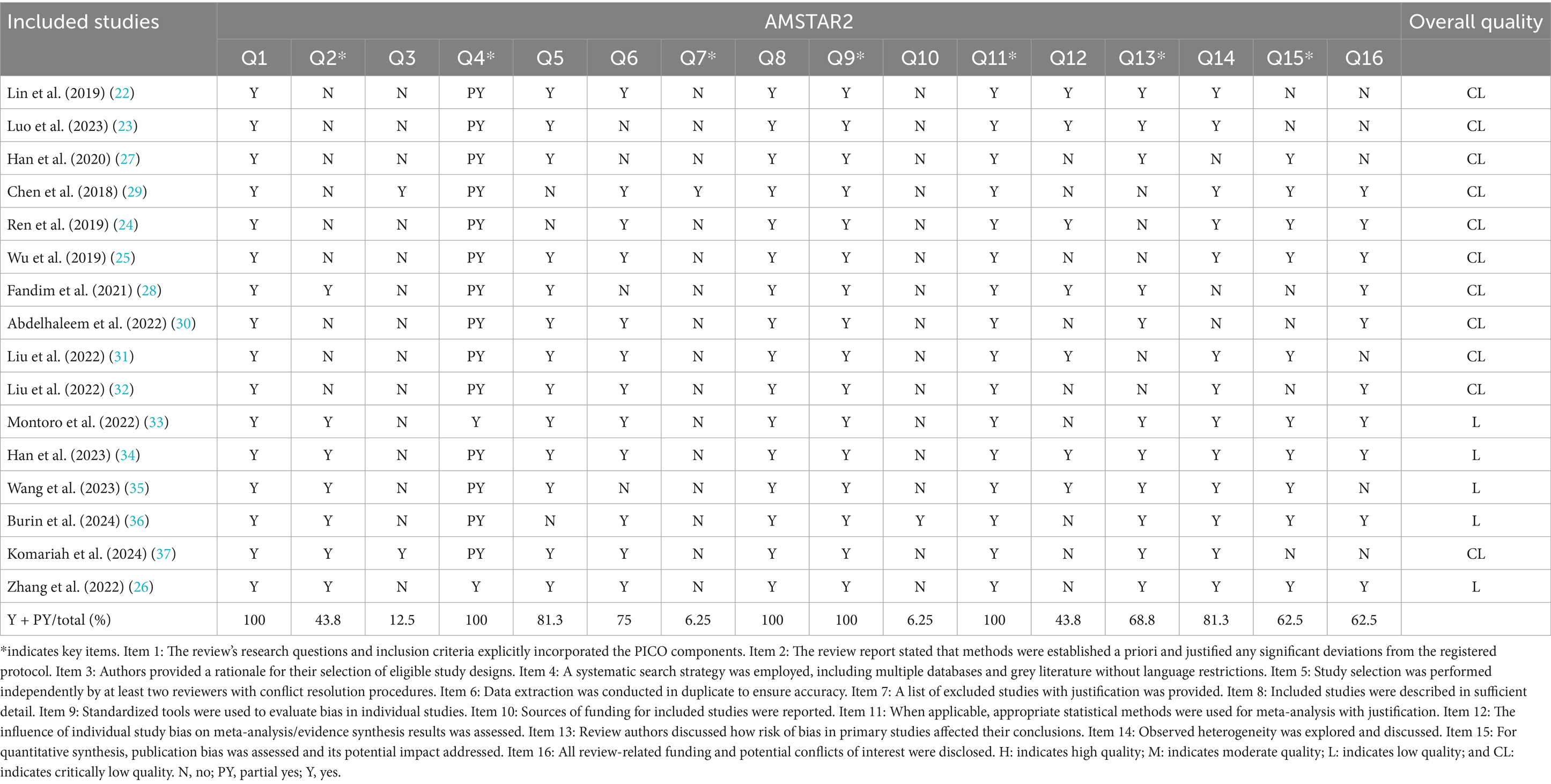
3.4 Results of methodological rigor assessment
The AMSTAR-2 assessment revealed significant methodological limitations across the 16 SRs/MAs, with 5 rated as low quality and 11 as very low quality. Critical domain deficiencies included protocol registration in only 7 SRs/MAs (26, 28, 33–37), comprehensive search strategies in 2 (26, 33), provision of excluded study lists with justifications in 1 (29), and failure to address risk of bias in 5 (24, 25, 29, 31, 32) or publication bias impacts in 6 (22, 23, 28, 30, 32, 37). While all SRs/MAs utilized validated tools for bias assessment and appropriate synthesis methods, deficiencies across ≥1 critical domain and multiple non-critical items collectively downgraded methodological rigor. The AMSTAR-2 evaluation results are presented in Table 2.
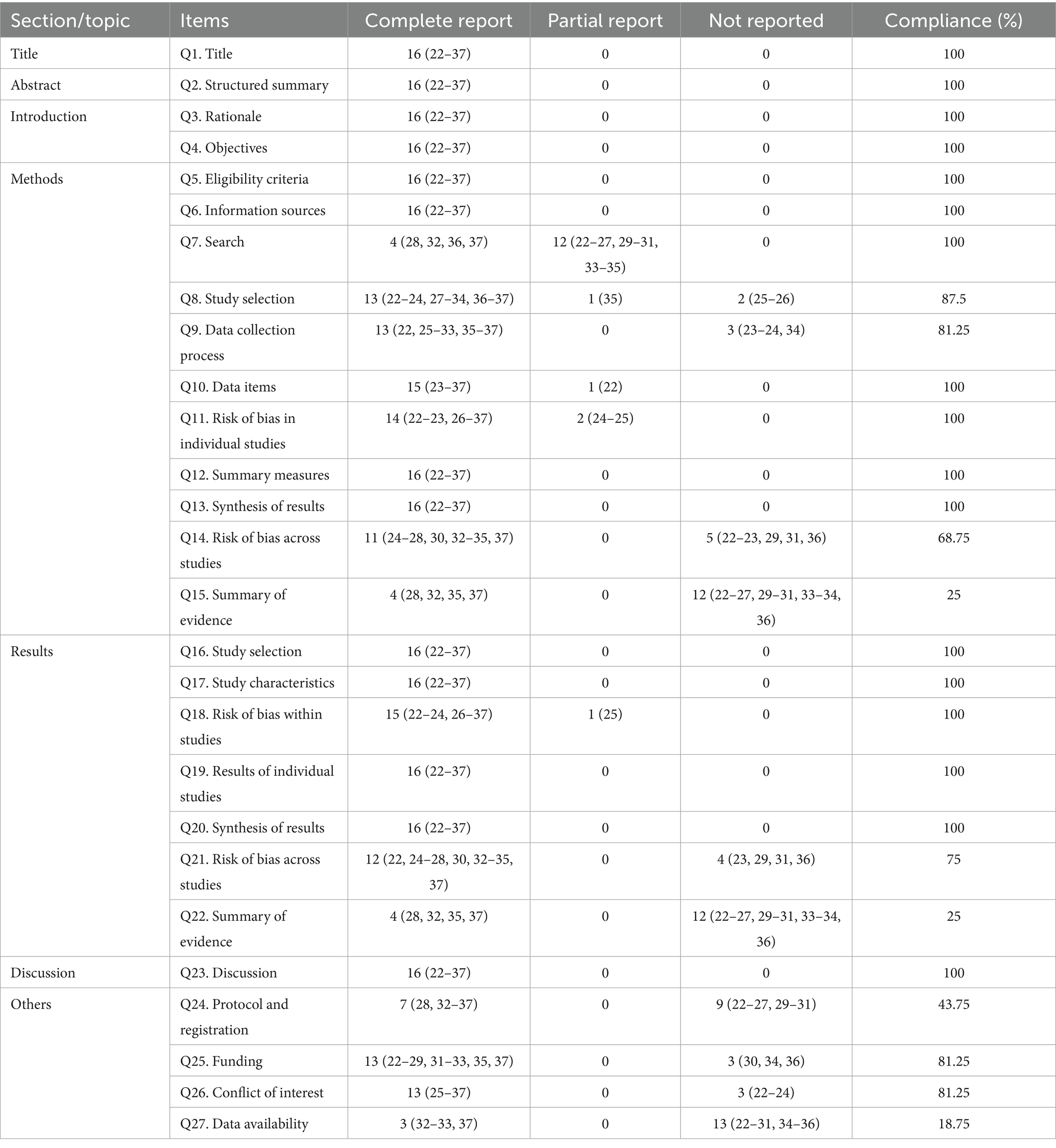
3.5 Results of reporting quality assessment
The PRISMA 2020 checklist identified that 17 of 27 items were fully reported, while 10 were inadequately reported. Methodological deficiencies included (1) omission of study selection processes in 2 SRs/MAs (24, 29); (2) undocumented data extraction protocols in 3 SRs/MAs (23, 27, 35); and (3) failure to assess cross-study risk of bias in 5 SRs/MAs (22, 23, 30, 32, 37). Only 25% of SRs/MAs explicitly described evidence synthesis methodologies (26, 28, 33, 36). In results reporting, 4 SRs/MAs neglected publication bias analysis (23, 30, 32, 37), and only 25% implemented evidence quality grading (26, 28, 33, 36). Transparency shortcomings comprised protocol registration in 7 SRs/MAs (26, 28, 33–37), undisclosed funding sources in 3 (31, 35, 37), omitted conflict-of-interest statements in 3 (22, 23, 27), and publicly accessible data in only 3 SRs/MAs (26, 33, 34). The results of the PRISMA 2020 are presented in Table 3.
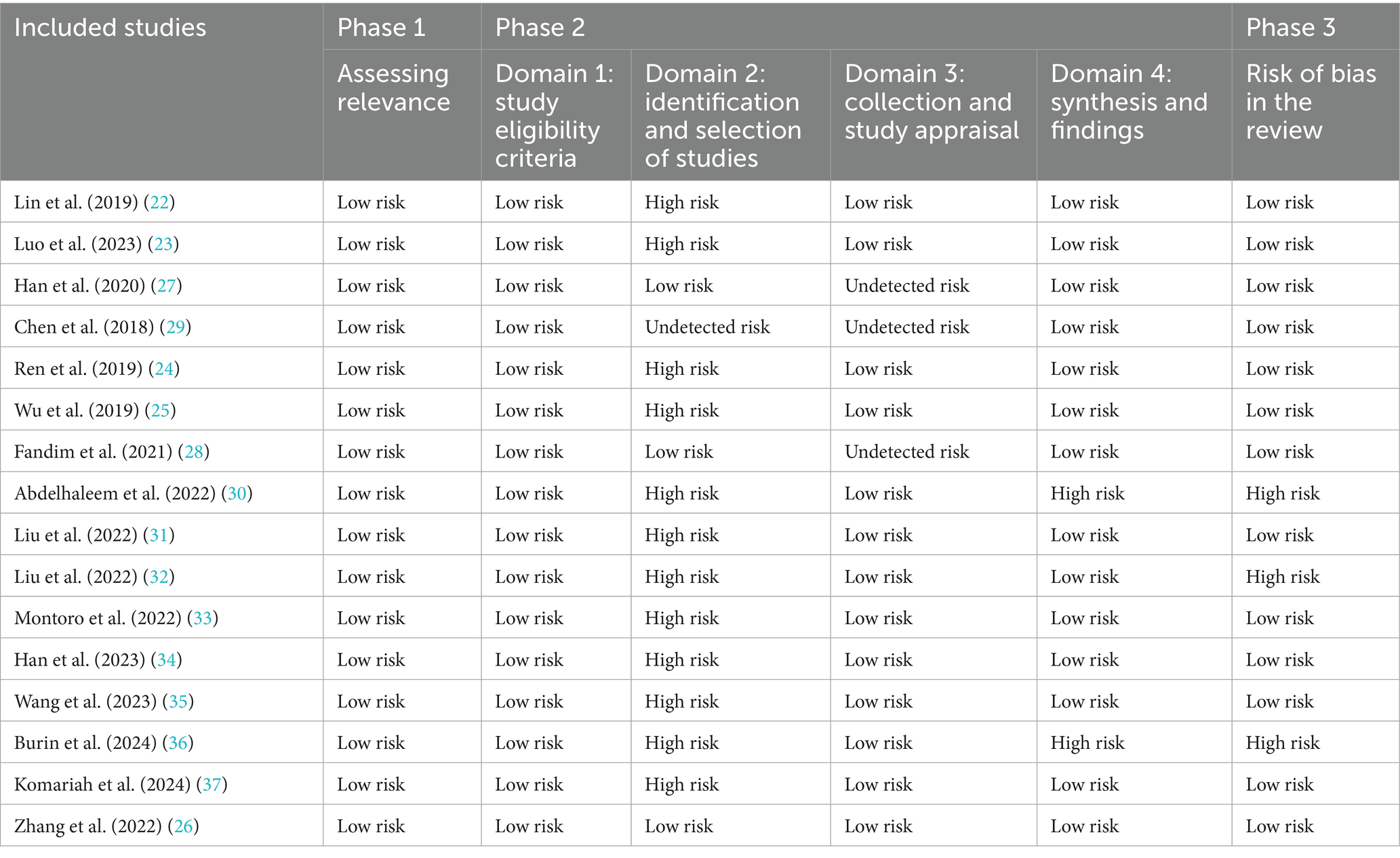
3.6 Results of risk of bias assessment
During phase 1, all 16 SRs/MAs were classified as low risk of bias, confirming alignment with the research objectives. In phase 2, domain 1 achieved universal low-risk compliance. In contrast, domain 2 revealed critical deficiencies, with only 3 SRs/MAs meeting low-risk standards (26–28). One SR/MA could not be conclusively rated due to ambiguous search syntax and unspecified screening personnel (29), while 12 SRs/MAs exhibited high-risk bias from non-exhaustive database searches, notably omitting clinical trial registries. In domain 3, 3 SRs/MAs were unrated due to undocumented extractor roles (27–29), and 13 SRs/MAs maintained low-risk ratings. Domain 4 identified instability risks in 2 SRs/MAs due to absent sensitivity analyses (30, 36), while 14 SRs/MAs retained low-risk status. In phase 3, 3 SRs/MAs were escalated to high-risk classification for insufficient bias rationale (30, 32, 36), and the remaining 13 SRs/MAs preserved low-risk ratings. The results of the bias risk evaluation are presented in Table 4.
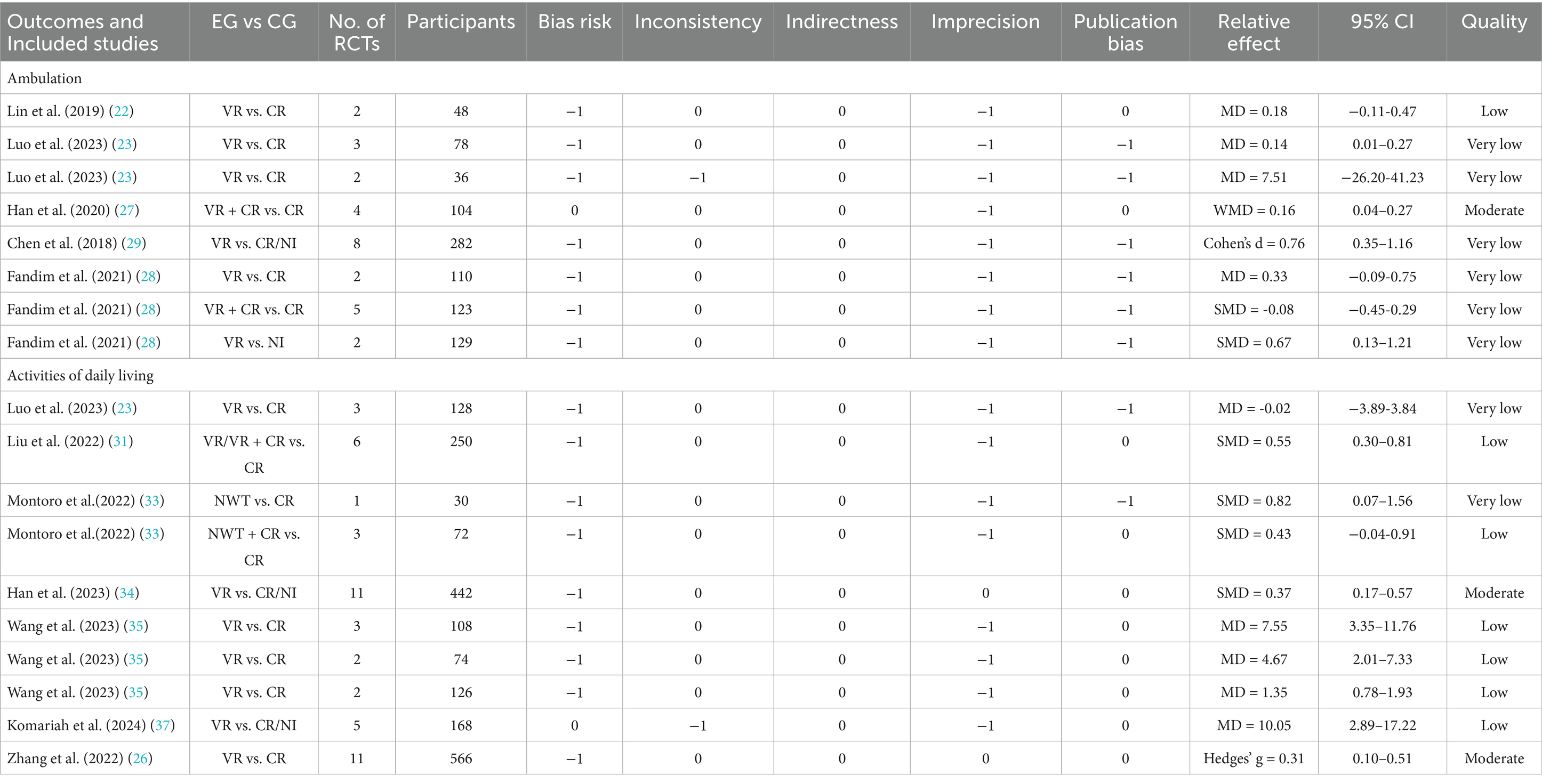
3.7 Results of evidence quality assessment
The GRADE evidence quality assessment of the five outcome indicators identified 58 evidence bodies, with only 9 (15.5%) classified as moderate quality, while 21 (36.2%) and 28 (48.3%) were categorized as low and very low quality, respectively.
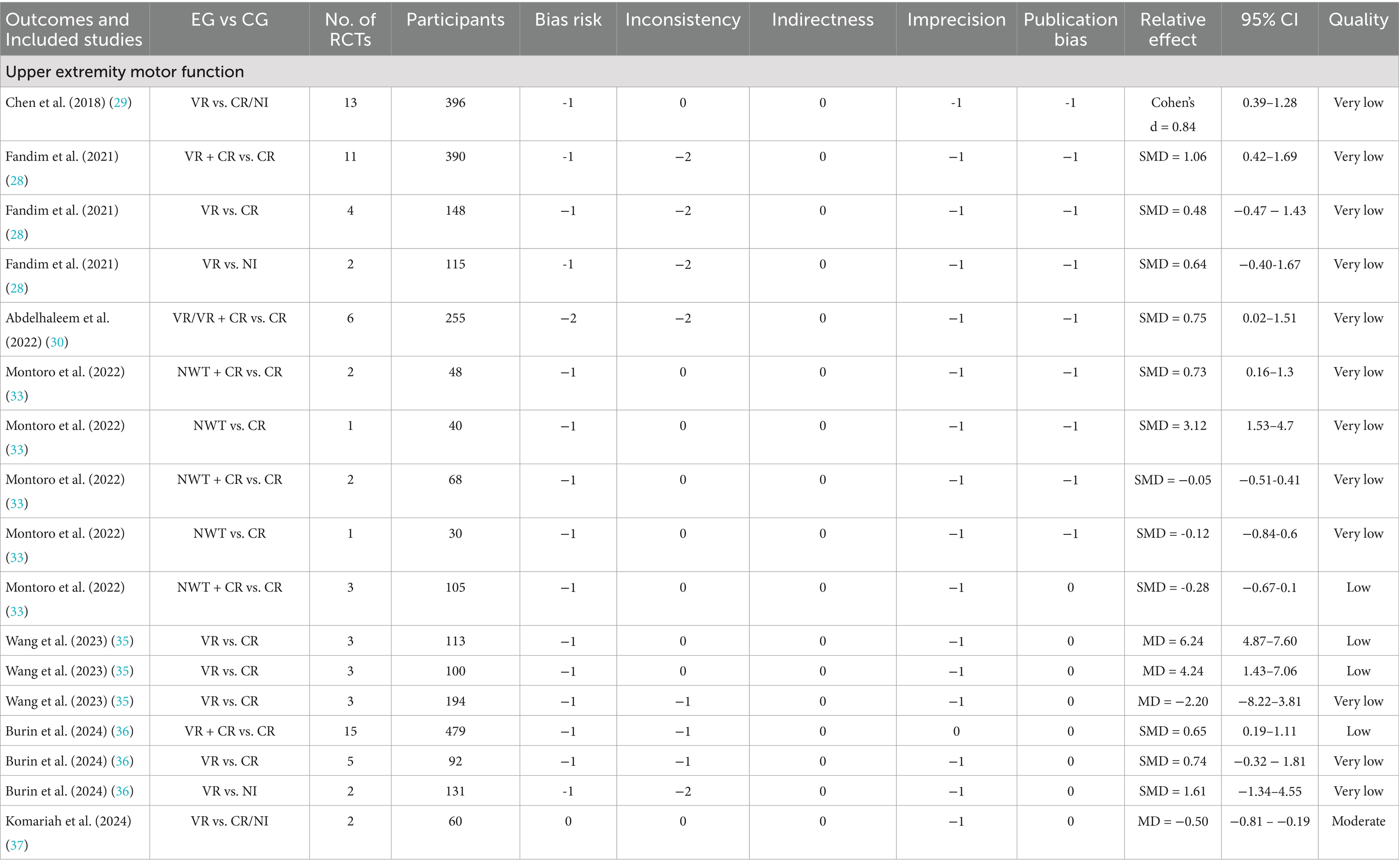
3.7.1 Improvement of upper extremity motor function
VR interventions were evaluated for upper limb motor function among children with CP by seven SRs/MAs (28–30, 33, 35–37). The results of the GRADE evaluations for upper extremity motor function are shown in Table 5.
3.7.1.1 Assessment tools
Significant improvements in upper limb function were observed using the Childhood Health Assessment Questionnaire (moderate evidence) and Peabody Developmental Motor Scales-2/Quality of Upper Extremity Skills Test (low-to-very-low evidence) (33, 35, 37). However, no significant differences were found in the Jebsen-Taylor Hand Function Test between VR and conventional rehabilitation (very low evidence) (33).
3.7.1.2 Intervention types
VR combined with conventional rehabilitation showed superior efficacy compared to conventional therapy alone in improving upper limb coordination (low-to-very-low evidence) (28, 36). In contrast, isolated VR training demonstrated conflicting results: while Montoro et al. reported significant benefits in fine motor coordination (very low evidence) (33), Abdelhaleem et al. found improvements only with combined interventions (very low evidence) (30), highlighting potential synergies between modalities.
3.7.1.3 Subgroup analyses
A significant negative correlation emerged between participant age and effect size, with younger children achieving better outcomes, alongside a positive correlation between higher daily VR dosage and functional gains (29). Regarding system design, engineer-developed VR systems demonstrated superior therapeutic effects compared to commercial systems (moderate evidence) (29). Although both commercial video games and rehabilitation-specific systems outperformed conventional therapy (low evidence), no statistically significant difference was observed between these two VR modalities (36). It is important to note that the results of the subgroup analyses described above are based on a limited number of SRs/MAs. Therefore, the results should be interpreted with caution.
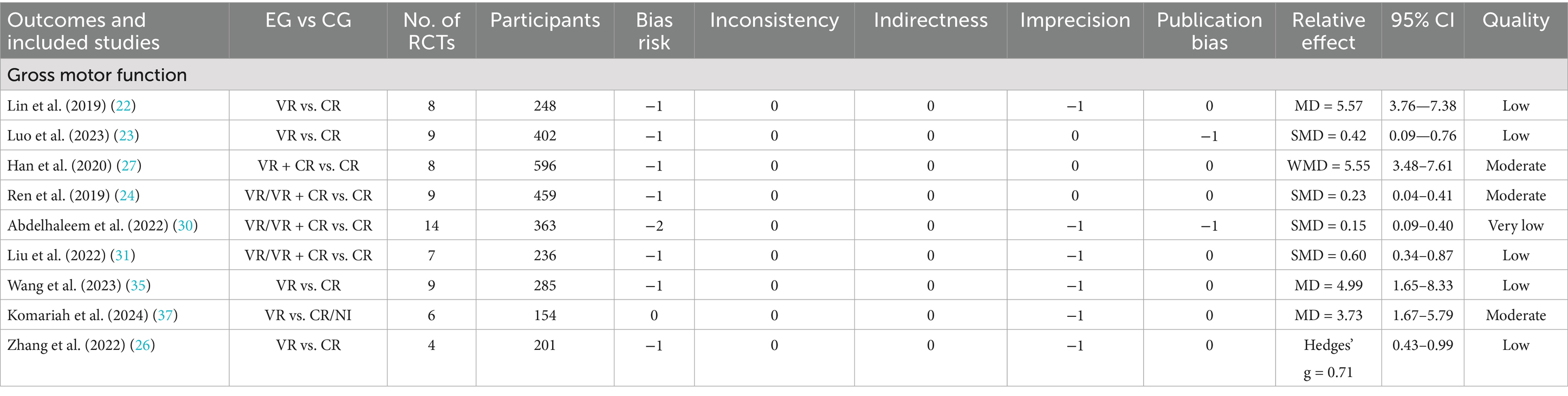
3.7.2 Improvement of gross motor function
Gross motor function refers to the ability to coordinate the movement of large muscles, strengthen the core body position, and maintain balance during movement and postural changes (e.g., standing on one leg, walking, running, or jumping) (38–40). It lays the foundation for participation in physical activities, sports, and daily tasks and is linked to cognitive and social development (41). VR interventions were evaluated for gross motor function among children with CP by nine SRs/MAs (22–24, 26, 27, 30, 31, 35, 37). The results of the GRADE evaluations for gross motor function are shown in Table 6.
3.7.2.1 Assessment tools
Of these, eight SRs/MAs employing the Gross Motor Function Measure (GMFM) demonstrated that VR interventions (either standalone or combined with conventional rehabilitation) significantly improved gross motor function versus conventional therapy or no intervention (moderate-to-very-low evidence) (22–24, 26, 27, 31, 35, 37). Specifically, VR showed superior efficacy in enhancing standing (GMFM-D) and walking/running/jumping (GMFM-E) compared to conventional rehabilitation (low evidence) (22). Notably, while significant improvements were observed in GMFM-88 scores across studies, no significant changes were detected in GMFM-66 scores (23, 27). Furthermore, Abdelhaleem et al. reported VR-induced enhancements in gross motor coordination (low evidence) (30).
3.7.2.2 Subgroup analyses
Regarding the level of immersion, semi-immersive systems exhibited greater therapeutic effects than non-immersive or fully immersive systems (37). For intervention parameters, optimal outcomes were achieved with sessions lasting 17–40 min, delivered ≥5 times weekly, over >12 weeks, and cumulatively exceeding 1,000 min—aligning with evidence linking higher frequency and prolonged duration to enhanced motor adaptation (24, 25, 28, 31). Notably, VR demonstrated significant gross motor improvements exclusively in children with hemiplegia (31). The subgroup analysis results reported above were based on a limited number of SRs/MAs, which may restrict the generalizability and external validity of the findings. Thus, these results should be interpreted with caution.
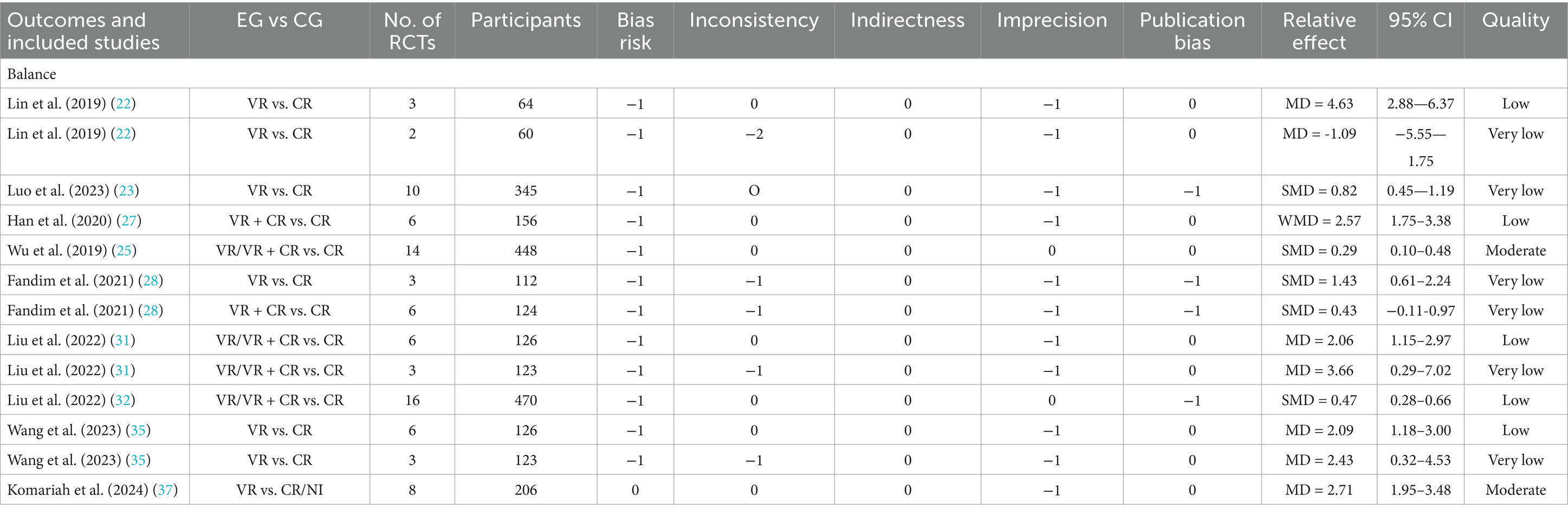
3.7.3 Improvement of balance
VR interventions were evaluated for balance function among children with CP by nine SRs/MAs (22, 23, 25, 27, 28, 31, 32, 35, 37). The results of the GRADE evaluations for balance function are shown in Table 7.
3.7.3.1 Assessment tools
Significant improvements were observed using the Berg Balance Scale and Pediatric Balance Scale when combining VR with conventional rehabilitation (low-to-very-low evidence) (27, 31, 35). However, no significant differences were detected in Timed Up and Go Test scores between VR and conventional therapy alone (very low evidence) (22).
3.7.3.2 Intervention types
Isolated VR training showed superior efficacy compared to conventional rehabilitation in two studies (very low evidence) (28, 32). In contrast, combined VR-conventional rehabilitation demonstrated consistent benefits across studies (low evidence) (32), indicating potential synergistic effects of multimodal interventions.
3.7.3.3 Subgroup analyses
Regarding immersion levels, semi-immersive systems significantly outperformed non-immersive systems in balance improvement (moderate evidence) (37), likely due to enhanced spatial awareness and proprioceptive feedback. For intervention parameters, longer intervention duration (≥12 weeks) enhanced therapeutic effects (very low evidence) (23). However, no significant associations were found between balance outcomes and session frequency/duration or total intervention time (moderate evidence) (25). Notably, the subgroup analysis results shown above were generated from a limited number of SRs/MAs, and they should be interpreted with caution.
3.7.4 Improvement of ambulation
VR interventions were evaluated for ambulation function among children with CP by five SRs/MAs (22, 23, 27–29). The results of the GRADE evaluations for ambulation function are shown in Table 8.
3.7.4.1 Assessment tools
Meta-analyses of the 10-Meter Walk Test revealed conflicting evidence: while two SRs/MAs reported significant walking speed improvements with VR (alone or combined with conventional rehabilitation) compared to conventional therapy (moderate-to-very-low evidence) (23, 27), one study conversely found no intergroup differences (low evidence) (22). Notably, no significant benefits were observed in the 2-Minute Walk Test (very low evidence) (23).
3.7.4.2 Intervention types
VR demonstrated superiority over no intervention (very low evidence). However, it showed no significant advantage over conventional rehabilitation alone, indicating comparable efficacy between modalities for ambulation improvement (28).
3.7.4.3 Subgroup analyses
Subgroup analyses revealed that ambulation improvement was greater in the bilateral/mixed CP subtype compared to hemiplegia. Moreover, age and effect size exhibited a substantial negative linear relationship, with younger children exhibiting stronger therapeutic responses (29). These findings collectively suggest developmental-stage-dependent neuroplasticity and functional adaptability in pediatric populations. A limited number of SRs/MAs served as the basis for the subgroup analysis results presented above. This limitation may affect the generalizability and external validity of the findings, necessitating cautious interpretation.
3.7.5 Improvement of ADL
Activities of daily living include the fundamental skills typically needed to manage basic physical needs (e.g., eating, dressing, personal hygiene, and toileting) and more complex activities related to independent living in the community (e.g., managing finances and medications) (42). Seven SRs/MAs evaluated VR interventions for ADL improvement in children with CP (23, 26, 31, 33–35, 37). The results of the GRADE evaluations for ADL are shown in Table 8.
3.7.5.1 Assessment tools
Significant ADL improvements were observed using the Pediatric Evaluation of Disability Inventory and Canadian Occupational Performance Measure (low evidence) (35). However, conflicting results emerged from Functional Independence Measure for Children assessments: three SRs/MAs reported VR superiority (low evidence) (31, 35, 37), while one found no significant difference (very low evidence) (23).
3.7.5.2 Intervention types
Isolated VR training demonstrated significant benefits over conventional rehabilitation (low evidence) (33). In contrast, combined VR-conventional approaches showed inconsistent efficacy, with no clear additive advantage observed (33).
3.7.5.3 Subgroup analyses
Regarding system types, Kinect-based VR and depth-sensing motion capture systems outperformed digital imaging platforms in ADL outcomes (moderate evidence) (26, 31). Notably, non-immersive systems achieved greater functional gains compared to semi-immersive systems (37). For intervention parameters, optimal effects were achieved when sessions exceeded 30 min and cumulative exposure surpassed either 40 sessions or 1,200 min (26, 34). Specifically, task-specific VR protocols without combined conventional therapy yielded superior outcomes (moderate evidence) (26), indicating that focused VR training may better align with ADL-related neuroplastic adaptations. It should be noted that the subgroup analysis results described above were derived from a limited number of SRs/MAs, and careful interpretation is warranted.
3.8 Adverse reactions
Only two SRs/MAs reported adverse effects following VR treatment, with both indicating that no serious adverse effects were observed (28, 30).
4 Discussion
4.1 Results-based discussion
The methodological quality of the included SRs/MAs was predominantly rated as low or critically low according to the AMSTAR-2 assessment. A major concern was the frequent absence of a priori study protocols, which casts doubt on whether the analysis strictly followed predefined methodologies and increases the risk of bias. Many reviews also failed to justify their exclusive inclusion of RCTs, omitted lists of excluded studies, and did not report funding sources of the included trials. Additionally, most SRs/MAs did not adequately address the risk of bias in primary RCTs or sufficiently investigate sources of heterogeneity. The lack of sensitivity and subgroup analyses further undermined the reliability of the findings.
Evaluation using the PRISMA 2020 checklist revealed significant reporting deficiencies in the published SRs/MAs. Many studies did not disclose funding sources, raising concerns about potential conflicts of interest and publication bias. Transparency was further compromised by the absence of excluded study lists, preventing readers from assessing the rigor of study selection. Critical methodological details, such as protocol registration, were often missing, making it difficult to distinguish between preplanned and post hoc analyses. Furthermore, most reviews neglected to assess the quality of evidence for individual outcomes or employ statistical methods to detect publication bias, such as funnel plots or Egger/Begg tests.
The ROBIS tool identified several SRs/MAs with unclear or high risk of bias, primarily due to incomplete reporting of search strategies and study selection processes. Some reviews did not search clinical trial registries, potentially missing relevant studies, while others failed to document the number of reviewers involved in data extraction. A notable limitation was the lack of subgroup or sensitivity analyses to explore heterogeneity or test result stability. These shortcomings suggest that certain reviews may have overlooked key biases in their methodology, affecting the reliability of their conclusions.
According to the GRADE framework, the overall quality of evidence in the included SRs/MAs was mostly low or very low, with only a few exceptions rated as moderate. The primary reasons for downgrading included risk of bias in the original RCTs, particularly due to unclear randomization, allocation concealment, and blinding procedures. Substantial heterogeneity, often unexplained, further reduced confidence in the pooled results. Small sample sizes in many RCTs led to imprecise effect estimates with wide confidence intervals. Additionally, the inability to assess publication bias in reviews with few included studies weakened the overall evidence base.
While our PROSPERO protocol initially proposed using only AMSTAR-2 and GRADE for quality assessment, we expanded the evaluation to include PRISMA 2020 and ROBIS to ensure a more comprehensive appraisal. This decision was driven by the need to assess reporting transparency and domain-specific biases, which are not fully captured by AMSTAR-2 or GRADE alone. Although this deviation introduced additional analytical complexity, it significantly strengthened the validity of our findings. By integrating multiple assessment tools, we systematically identified common methodological limitations in published SRs/MAs, which may inform future research improvements and ultimately enhance the quality of evidence-based clinical decision-making.
4.2 Mechanisms of VR-based interventions in CP
4.2.1 Motor learning and neuroplasticity
Motor rehabilitation approaches for cerebral palsy should be individualized, age and developmentally appropriate, goal-directed, skill-based, and intensive and time-limited (43). VR operationalizes core motor learning principles—including high-intensity repetition, progressive task difficulty, and multisensory feedback—to enhance neuroplasticity and skill acquisition (44). Neuroimaging studies have demonstrated that VR can significantly enhance the activation of brain regions associated with motor control, such as the primary motor cortex and supplementary motor area, indicating an increased responsiveness of the brain to motor tasks (45). Moreover, VR interventions also normalize aberrant neural activation patterns in CP, particularly by engaging the contralateral primary sensorimotor cortex, which correlates with improved functional motor skills (e.g., reaching, self-care activities) (46).
4.2.2 Cognitive engagement and motivation
VR augments traditional rehabilitation paradigms by integrating cognitive-motor engagement during task execution, promoting neuroplasticity through combined motor repetition and problem-solving strategies (47, 48). The immersive environment imposes task-driven challenges that require continuous adaptive motor planning and error correction, reinforcing cognitive-motor strategy development in children with CP (49). Critically, VR’s gamified framework enhances treatment adherence through positive affective engagement, transforming repetitive exercises into goal-oriented activities. This dual focus sustains motivation during prolonged rehabilitation, potentially amplifying functional gains by increasing training tolerance and cortical activation (50).
4.2.3 Sensorimotor integration
VR enhances sensorimotor integration in CP by improving visual perception, enabling precise body position and movement trajectory awareness, which optimizes motor accuracy and coordination (51, 52). Visual feedback within VR systems facilitates sensorimotor circuit reorganization and supports the development of compensatory behavioral strategies for functional deficits, critical for daily activity performance (53). Furthermore, VR environments allow safe, task-specific practice of complex motor patterns that are physically unfeasible in real-world settings, fostering neuroadaptive skill acquisition and functional independence (54).
4.2.4 Postural control optimization
Research indicates that shifting attention from internal focus (movement accuracy) to external focus (task/goal-oriented stimuli) enhances balance acquisition and motor automaticity (55). VR facilitates this process by providing an immersive, task-oriented environment, directing children’s attention toward external goals, thereby specifically improving balance dysfunction and related motor control deficits (56). Unlike conventional therapy, VR frameworks embed purposeful tasks with multisensory feedback, prompting active engagement in hip flexion, abduction, and external rotation during standing exercises. This approach facilitates neurological recovery and balance improvement through task-specific kinematic reinforcement (57). Furthermore, VR training strengthens lower limb musculature, promoting symmetrical weight distribution and dynamic stability, which collectively enhance postural control and ambulatory capacity (58).
4.3 Interpretation of SRs/MAs results
The SRs/MAs included in this overview demonstrate that VR can improve the gross motor function of children with CP. Although VR has had a positive impact on balance, ambulation, ADL, and upper extremity motor function, not all SRs/MAs have reached positive conclusions. This discrepancy may be related to the different assessment tools used in the various SRs/MAs, the different RCTs included, and the varying quality of the studies. Additionally, the results of the meta-analyses are also affected by the size of the sample. Therefore, we need to interpret these results with caution.
It is essential to highlight that, among the 16 included SRs/MAs, only 10 SRs/MAs performed subgroup analyses (23–26, 28, 29, 31, 34, 36, 37). These subgroup analysis results were based on a limited number of SRs/MAs, necessitating a cautious approach to their interpretation. Subgroup analyses identified a significant negative linear association between participant age and VR efficacy (younger children showed greater functional improvements) and a positive dose–response relationship (higher intervention doses correlated with larger effect sizes) (29). These patterns may reflect heightened neuroplasticity in younger populations and the neurophysiological requirement for repetitive task-specific training to induce synaptic reorganization (59, 60). Discrepancies emerged regarding VR system efficacy: While some studies reported comparable outcomes between commercial gaming platforms and rehabilitation-specific systems (36), others demonstrated superior functional gains with engineer-developed, rehabilitation-tailored VR interfaces (29, 61). Customized systems allow precise calibration of task difficulty to individual functional levels and integration of co-design principles involving clinicians and patients, potentially enhancing therapeutic relevance and clinical adoption (62). Notably, non-immersive systems demonstrated greater ADL improvement than immersive systems in one study (37), possibly due to enhanced real-world skill transfer when maintaining environmental awareness (63). However, substantial heterogeneity, small sample sizes, and limited studies precluded definitive conclusions regarding critical moderators, including CP subtype, immersion level, and optimal intervention duration.
4.4 Study limitations
This overview has several methodological constraints. First, this overview only included published studies in Chinese and English, which may have omitted some studies conducted in other languages. Second, although the two reviewers received professional training and reached consensus on the assessment results through discussion or by consulting a more experienced third reviewer (Lihong Ma) when disagreements arose, some degree of evaluation bias may still exist, as quality assessment essentially relies on the judgment of the assessors. Third, outcome measures were limited to subjective scales, lacking complementary objective data. Fourth, significant heterogeneity across studies precluded meta-analytic synthesis, limiting consolidated efficacy interpretations. Fifth, recent RCTs not yet incorporated into existing SRs/MAs were excluded, narrowing the scope of evidence re-evaluation. Sixth, while restricting inclusion to RCT-focused SRs/MAs aimed to enhance quality, this approach excluded mixed-design reviews and may have underrepresented adverse events, potentially compromising risk–benefit assessments. Finally, the overall sample size greatly increased because many of the 16 SRs/MAs shared the same original studies. These results may have exaggerated the true efficacy and accuracy of VR interventions in the field of cerebral palsy. The differences between studies might not have been fully recognized because there were not enough truly independent studies, which could hide important variations and make the findings of this review less reliable and applicable.
4.5 Implications for further study
To handle substantial overlap among primary studies in systematic reviews, a two-step selection method is recommended. All non-overlapping systematic reviews should be included first. For overlapping reviews, priority should be assigned to Cochrane reviews, followed by an assessment of publication date, methodological quality, and relevance to the research question. Beyond addressing overlap, future SRs/MAs on VR interventions for CP should prioritize methodological rigor and transparency. Researchers are advised to prospectively register protocols on established platforms and adhere strictly to PRISMA 2020 guidelines to enhance reporting quality. Additionally, a comprehensive literature search strategy must be implemented, integrating database queries, reference screening, clinical trial registries, grey literature, and study registrations to minimize selection bias. Full-text exclusions should be explicitly documented with rationales to ensure reproducibility and mitigate reporting bias. When substantial heterogeneity is observed, subgroup or sensitivity analyses are warranted to explore underlying causes. Methodological limitations of included studies, including potential sources of bias and their implications for outcomes, must be critically discussed. Publication bias should be assessed using funnel plots alongside statistical tests to address small-study effects. Ultimately, the clinical relevance of findings should be supported by GRADE evaluations of critical outcome measures.
5 Conclusion
Current evidence suggests VR demonstrates therapeutic potential for improving upper limb function, gross motor skills, balance, ambulation, and ADL in children with CP, with no significant safety concerns reported. However, the robustness of these findings is compromised by the methodological limitations of the included SRs/MAs. Nevertheless, the cumulative evidence underscores VR as a viable adjunctive intervention for functional rehabilitation in this population. Further high-quality RCTs employing standardized protocols, objective biomarkers, and long-term follow-ups are imperative to validate efficacy, optimize implementation strategies, and strengthen translational relevance for clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
EF: Writing – original draft, Conceptualization, Methodology, Project administration. HG: Writing – original draft, Methodology, Project administration. BD: Writing – original draft, Project administration. XM: Writing – review & editing, Methodology. LM: Writing – review & editing, Methodology, Supervision.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank all participants and colleagues who contributed to this study. Special thanks go to the staff at the Department of Rehabilitation, Jinan Children’s Hospital, for their support and assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1582110/full#supplementary-material
Abbreviations
ADL, activities of daily living; AMSTAR-2, A Measurement Tool to Assess Systematic Reviews 2; CP, cerebral palsy; GMFM, Gross Motor Function Measure; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; MAs, meta-analyses; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomized controlled trial; ROBIS, Risk of Bias in Systematic Reviews; SRs, systematic reviews; VR, virtual reality.
References
1. Sadowska, M, Sarecka-Hujar, B, and Kopyta, I. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. (2020) 16:1505–18. doi: 10.2147/ndt.S235165
2. Christine, C, Dolk, H, Platt, MJ, Colver, A, Prasauskiene, A, Krägeloh-Mann, I, et al. Recommendations from the SCPE collaborative group for defining and classifying cerebral palsy. Dev Med Child Neurol Suppl. (2007) 109:35–8. doi: 10.1111/j.1469-8749.2007.tb12626.x
3. McGuire, D, Tian, L, Yeargin-Allsopp, M, Dowling, N, and Christensen, D. Prevalence of cerebral palsy, intellectual disability, hearing loss, and blindness, National Health Interview Survey, 2009-2016. Disabil Health J. (2019) 12:443–51. doi: 10.1016/j.dhjo.2019.01.005
4. Olusanya, BO, Kancherla, V, Shaheen, A, Ogbo, FA, and Davis, AC. Global and regional prevalence of disabilities among children and adolescents: analysis of findings from global health databases. Front Public Health. (2022) 10:977453. doi: 10.3389/fpubh.2022.977453
5. Demont, A, Gedda, M, Lager, C, De Lattre, C, Gary, Y, Keroulle, E, et al. Evidence-based, implementable motor rehabilitation guidelines for individuals with cerebral palsy. Neurology. (2022) 99:283–97. doi: 10.1212/WNL.0000000000200936
6. Santer, M, Ring, N, Yardley, L, Geraghty, A, and Wyke, S. Treatment non-adherence in pediatric long-term medical conditions: systematic review and synthesis of qualitative studies of caregivers’ views. BMC Pediatr. (2014) 14:63. doi: 10.1186/1471-2431-14-63
7. Voinescu, A, Sui, J, and Stanton, FD. Virtual reality in neurorehabilitation: an umbrella review of Meta-analyses. J Clin Med. (2021) 10:1478. doi: 10.3390/jcm10071478
8. Abbas, J, O'Connor, A, Ganapathy, E, Isba, R, Payton, T, McGrath, B, et al. What is virtual reality? A healthcare-focused systematic review of definitions. Health Policy Techn. (2023) 12:100741. doi: 10.1016/j.hlpt.2023.100741
9. Huygelier, H, Mattheus, E, Abeele, VV, van Ee, R, and Gillebert, CR. The use of the term virtual reality in post-stroke rehabilitation: a scoping review and commentary. Psychol Belg. (2021) 61:145–62. doi: 10.5334/pb.1033
10. Parsons, T, Riva, G, Parsons, S, Mantovani, F, Newbutt, N, Lin, L, et al. Virtual reality in pediatric psychology. Pediatrics. (2017) 140:S86–91. doi: 10.1542/peds.2016-1758I
11. Palaus, M, Marron, EM, Viejo-Sobera, R, and Redolar-Ripoll, D. Neural basis of video gaming: a systematic review. Front Hum Neurosci. (2017) 11:248. doi: 10.3389/fnhum.2017.00248
12. Chen, YP, Kang, LJ, Chuang, TY, Doong, JL, Lee, SJ, Tsai, MW, et al. Use of virtual reality to improve upper-extremity control in children with cerebral palsy: a single-subject design. Phys Ther. (2007) 87:1441–57. doi: 10.2522/ptj.20060062
13. Wille, D, Eng, K, Holper, L, Chevrier, E, Hauser, Y, Kiper, D, et al. Virtual reality-based paediatric interactive therapy system (PITS) for improvement of arm and hand function in children with motor impairment—a pilot study. Dev Neurorehabil. (2009) 12:44–52. doi: 10.1080/17518420902773117
14. Huber, M, Rabin, B, Docan, C, Burdea, GC, AbdelBaky, M, and Golomb, MR. Feasibility of modified remotely monitored in-home gaming technology for improving hand function in adolescents with cerebral palsy. IEEE Trans Inf Technol Biomed. (2010) 14:526–34. doi: 10.1109/titb.2009.2038995
15. Levac, D, Rivard, L, and Missiuna, C. Defining the active ingredients of interactive computer play interventions for children with neuromotor impairments: a scoping review. Res Dev Disabil. (2012) 33:214–23. doi: 10.1016/j.ridd.2011.09.007
16. Pollock, M, Fernandes, RM, and Becker, LA. Chapter V: overviews of reviews In: JPT Higgins, J Thomas, and J Chandler, editors. Cochrane handbook for systematic reviews of interventions. Version 6.1. London, UK: Cochrane (2020)
17. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
18. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
19. Whiting, P, Savović, J, Higgins, JP, Caldwell, DM, Reeves, BC, Shea, B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. (2016) 69:225–34. doi: 10.1016/j.jclinepi.2015.06.005
20. Atkins, D, Best, D, Briss, PA, Eccles, M, Falck-Ytter, Y, Flottorp, S, et al. Grading quality of evidence and strength of recommendations. BMJ. (2004) 328:1490. doi: 10.1136/bmj.328.7454.1490
21. Pieper, D, Antoine, SL, Mathes, T, Neugebauer, EA, and Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. (2014) 67:368–75. doi: 10.1016/j.jclinepi.2013.11.007
22. Lin, ST, Luo, MN, Wang, D, and Li, ZK. Meta-analysis of the effects of telerehabilitation in patients with cerebral palsy. Chin Nurs Manag. (2019) 19:842–9. doi: 10.3969/j.issn.1672-1756.2019.06.009
23. Luo, TW, Zhang, N, Tang, Q, Song, QQ, Xiang, YQ, and Zhu, LH. Effects of virtual reality technology on motor function of children with cerebral palsy:a Meta-analysis. Mil Nurs. (2023) 40:5–11. doi: 10.3969/j.issn.2097-1826.2023.07.002
24. Ren, Z, and Wu, J. The effect of virtual reality games on the gross motor skills of children with cerebral palsy: a Meta-analysis of randomized controlled trials. Int J Environ Res Public Health. (2019) 16:3885. doi: 10.3390/ijerph16203885
25. Wu, JL, Loprinzi, PD, and Ren, ZB. The rehabilitative effects of virtual reality games on balance performance among children with cerebral palsy: a Meta-analysis of randomized controlled trials. Int J Environ Res Public Health. (2019) 16:4161. doi: 10.3390/ijerph16214161
26. Zhang, Y, Li, R, Miao, X, Cheng, LJ, and Lau, Y. Virtual motor training to improve the activities of daily living, hand grip, and gross motor function among children with cerebral palsy: Meta-regression analysis. Gait Posture. (2022) 91:297–305. doi: 10.1016/j.gaitpost.2021.10.046
27. Han, J, Liang, M, and Xie, R. Meta analysis for effectiveness of virtual reality training on improving lower extremity function of children with cerebral palsy. Chin J Rehabil. (2020) 35:541–6. doi: 10.3870/zgkf.2020.10.009
28. Fandim, JV, Saragiotto, BT, Porfírio, GJM, and Santana, RF. Effectiveness of virtual reality in children and young adults with cerebral palsy: a systematic review of randomized controlled trial. Braz J Phys Ther. (2021) 25:369–86. doi: 10.1016/j.bjpt.2020.11.003
29. Chen, Y, Fanchiang, HD, and Howard, A. Effectiveness of virtual reality in children with cerebral palsy: a systematic review and Meta-analysis of randomized controlled trials. Phys Ther. (2018) 98:63–77. doi: 10.1093/ptj/pzx107
30. Abdelhaleem, N, El Wahab, MSA, and Elshennawy, S. Effect of virtual reality on motor coordination in children with cerebral palsy: a systematic review and meta-analysis of randomized controlled trials. Egypt J Med Hum Genet. (2022) 23:71. doi: 10.1186/s43042-022-00258-0
31. Liu, C, Wang, X, Chen, R, and Zhang, J. The effects of virtual reality training on balance, gross motor function, and daily living ability in children with cerebral palsy: systematic review and Meta-analysis. JMIR Serious Games. (2022) 10:e38972. doi: 10.2196/38972
32. Liu, W, Hu, Y, Li, J, and Chang, J. Effect of virtual reality on balance function in children with cerebral palsy: a systematic review and Meta-analysis. Front Public Health. (2022) 10:865474. doi: 10.3389/fpubh.2022.865474
33. Montoro-Cárdenas, D, Cortés-Pérez, I, Ibancos-Losada, MD, Zagalaz-Anula, N, Obrero-Gaitán, E, and Osuna-Pérez, MC. Nintendo® Wii therapy improves upper extremity motor function in children with cerebral palsy: a systematic review with Meta-analysis. Int J Environ Res Public Health. (2022) 19:12343. doi: 10.3390/ijerph191912343
34. Han, Y, and Park, S. Effectiveness of virtual reality on activities of daily living in children with cerebral palsy: a systematic review and meta-analysis. PeerJ. (2023) 11:e15964. doi: 10.7717/peerj.15964
35. Wang, N, Liu, N, Liu, S, and Gao, Y. Effects of nonimmersive virtual reality intervention on children with spastic cerebral palsy: a Meta-analysis and systematic review. Am J Phys Med Rehabil. (2023) 102:1130–8. doi: 10.1097/phm.0000000000002321
36. Burin-Chu, S, Baillet, H, Leconte, P, Lejeune, L, Thouvarecq, R, and Benguigui, N. Effectiveness of virtual reality interventions of the upper limb in children and young adults with cerebral palsy: a systematic review with meta-analysis. Clin Rehabil. (2024) 38:15–33. doi: 10.1177/02692155231187858
37. Komariah, M, Amirah, S, Abdurrahman, MF, Handimulya, MFS, Platini, H, Maulana, S, et al. Effectivity of virtual reality to improve balance, motor function, activities of daily living, and upper limb function in children with cerebral palsy: a systematic review and Meta-analysis. Ther Clin Risk Manag. (2024) 20:95–109. doi: 10.2147/tcrm.S432249
38. Calero-Morales, S, Del Consuelo, V-BG, Yance-Carvajal, C, and Paguay-Balladares, W. Gross motor development in preschoolers through Conductivist and constructivist physical recreational activities. Compar Res Sports. (2023) 11:61. doi: 10.3390/sports11030061
39. Fu, T, Zhang, D, Wang, W, Geng, H, Lv, Y, Shen, R, et al. Functional training focused on motor development enhances gross motor, physical fitness, and sensory integration in 5–6-year-old healthy Chinese children. Front Pediatr. (2022) 10:936799. doi: 10.3389/fped.2022.936799
40. Zhao, H, Deng, Y, Song, G, Zhu, H, Sun, L, Li, H, et al. Effects of 8 weeks of rhythmic physical activity on gross motor movements in 4-5-year-olds: a randomized controlled trial. J Exerc Sci Fit. (2024) 22:456–62. doi: 10.1016/j.jesf.2024.10.001
41. Zhou, Y, and Tolmie, A. Associations between gross and fine motor skills, physical activity, executive function, and academic achievement: longitudinal findings from the UK millennium cohort study. Brain Sci. (2024) 14:121. doi: 10.3390/brainsci14020121
42. Mlinac, M, and Feng, M. Assessment of activities of daily living, self-care, and Independence. Arch Clin Neuropsychol. (2016) 31:506–16. doi: 10.1093/arclin/acw049
43. Faccioli, S, Pagliano, E, Ferrari, A, Maghini, C, Siani, M, Sgherri, G, et al. Evidence-based management and motor rehabilitation of cerebral palsy children and adolescents: a systematic review. Front Neurol. (2023) 14:1171224. doi: 10.3389/fneur.2023.1171224
44. Levin, MF, and Demers, M. Motor learning in neurological rehabilitation. Disabil Rehabil. (2021) 43:3445–53. doi: 10.1080/09638288.2020.1752317
45. Golomb, MR, McDonald, BC, Warden, SJ, Yonkman, J, Saykin, AJ, Shirley, B, et al. In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch Phys Med Rehabil. (2010) 91:1–8. doi: 10.1016/j.apmr.2009.08.153
46. You, SH, Jang, SH, Kim, YH, Kwon, YH, Barrow, I, and Hallett, M. Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev Med Child Neurol. (2005) 47:628–35. doi: 10.1017/S0012162205001634
47. Fu, W, and Ji, C. Application and effect of virtual reality Technology in Motor Skill Intervention for individuals with developmental disabilities: a systematic review. Int J Environ Res Public Health. (2023) 20:4619. doi: 10.3390/ijerph20054619
48. Doniger, GM, Beeri, MS, Bahar-Fuchs, A, Gottlieb, A, Tkachov, A, Kenan, H, et al. Virtual reality-based cognitive-motor training for middle-aged adults at high Alzheimer's disease risk: a randomized controlled trial. Alzheimers Dement. (2018) 4:118–29. doi: 10.1016/j.trci.2018.02.005
49. Deutsch, JE, Borbely, M, Filler, J, Huhn, K, and Guarrera-Bowlby, P. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys Ther. (2008) 88:1196–207. doi: 10.2522/ptj.20080062
50. Qian, J, McDonough, DJ, and Gao, Z. The effectiveness of virtual reality exercise on individual's physiological, psychological and rehabilitative outcomes: a systematic review. Int J Environ Res Public Health. (2020) 17:4133. doi: 10.3390/ijerph17114133
51. Bilde, PE, Kliim-Due, M, Rasmussen, B, Petersen, LZ, Petersen, TH, and Nielsen, JB. Individualized, home-based interactive training of cerebral palsy children delivered through the internet. BMC Neurol. (2011) 11:32. doi: 10.1186/1471-2377-11-32
52. Snider, L, Majnemer, A, and Darsaklis, V. Virtual reality as a therapeutic modality for children with cerebral palsy. Dev Neurorehabil. (2010) 13:120–8. doi: 10.3109/17518420903357753
53. Chiang, VC, Lo, KH, and Choi, KS. Rehabilitation of activities of daily living in virtual environments with intuitive user interface and force feedback. Disabil Rehabil Assist Technol. (2017) 12:672–80. doi: 10.1080/17483107.2016.1218554
54. Şahin, S, Köse, B, Aran, OT, Bahadır Ağce, Z, and Kayıhan, H. The effects of virtual reality on motor functions and daily life activities in unilateral spastic cerebral palsy: a single-blind randomized controlled trial. Games Health J. (2020) 9:45–52. doi: 10.1089/g4h.2019.0020
55. Chiviacowsky, S, Wulf, G, and Wally, R. An external focus of attention enhances balance learning in older adults. Gait Posture. (2010) 32:572–5. doi: 10.1016/j.gaitpost.2010.08.004
56. Mouhamed, H, Abo-Zaid, N, Khalifa, H, Ali, M, Elserty, N, Behiry, M, et al. Efficacy of virtual reality on balance impairment in ataxic cerebral palsy children: randomized controlled trial. Eur J Phys Rehabil Med. (2024) 60:949–55. doi: 10.23736/S1973-9087.24.08617-9
57. Lange, BS, Requejo, P, Flynn, SM, Rizzo, AA, Valero-Cuevas, FJ, Baker, L, et al. The potential of virtual reality and gaming to assist successful aging with disability. Phys Med Rehabil Clin N Am. (2010) 21:339–56. doi: 10.1016/j.pmr.2009.12.007
58. Cho, C, Hwang, W, Hwang, S, and Chung, Y. Treadmill training with virtual reality improves gait, balance, and muscle strength in children with cerebral palsy. Tohoku J Exp Med. (2016) 238:213–8. doi: 10.1620/tjem.238.213
59. Morgan, C, Novak, I, and Badawi, N. Enriched environments and motor outcomes in cerebral palsy: systematic review and meta-analysis. Pediatrics. (2013) 132:e735–46. doi: 10.1542/peds.2012-3985
60. Gordon, AM. Impaired voluntary movement control and its rehabilitation in cerebral palsy. Adv Exp Med Biol. (2016) 957:291–311. doi: 10.1007/978-3-319-47313-0_16
61. Demers, M, Fung, K, Subramanian, SK, Lemay, M, and Robert, MT. Integration of motor learning principles into virtual reality interventions for individuals with cerebral palsy: systematic review. JMIR Serious Games. (2021) 9:e23822. doi: 10.2196/23822
62. Brassel, S, Power, E, Campbell, A, Brunner, M, and Togher, L. Recommendations for the design and implementation of virtual reality for acquired brain injury rehabilitation: systematic review. J Med Internet Res. (2021) 23:e26344. doi: 10.2196/26344
Keywords: virtual reality, cerebral palsy, neurorehabilitation, overview, systematic review
Citation: Fang E, Guan H, Du B, Ma X and Ma L (2025) Effectiveness of virtual reality for functional disorders in cerebral palsy: an overview of systematic reviews and meta-analyses. Front. Neurol. 16:1582110. doi: 10.3389/fneur.2025.1582110
Edited by:
Mariella Pazzaglia, Sapienza University of Rome, ItalyReviewed by:
Claudia Covarrubias, McGill University, CanadaJie Hao, Southeast Colorado Hospital, United States
Copyright © 2025 Fang, Guan, Du, Ma and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lihong Ma, bGhtYTIwMDJAMTYzLmNvbQ==
 Enhui Fang
Enhui Fang Hui Guan1
Hui Guan1 Lihong Ma
Lihong Ma