Abstract
Introduction:
Currently, acupuncture therapy is widely used for post-stroke upper-limb spasticity. However, the available evidence remains insufficient to determine the relative effectiveness of different acupuncture protocols.
Methods:
This study retrieved relevant databases and systematically reviewed randomized controlled trials (RCTs) on acupuncture treatment for post-stroke upper-limb spasticity. A total of 28 trials involving 14 acupuncture treatment protocols were included. A network meta-analysis was performed using Stata 18 software.
Results:
The results indicated that the Balanced Yin-Yang Acupuncture + Rehabilitation yielded the best outcomes in improving Fugl–Meyer Assessment scores, while Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling + Rehabilitation was most effective in reducing modified Ashworth scale scores.
Discussion:
A comparison of efficacy indicators across 14 different acupuncture methods combined with rehabilitation showed that Balanced Yin-Yang Acupuncture + Rehabilitation and Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling + Rehabilitation were more effective in treating post-stroke upper-limb spasticity. Owing to limitations in the current body of research, these conclusions need to be further verified by more high-quality randomized controlled trials.
Systematic review registration:
https://www.crd.york.ac.uk/PROSPERO, identifier CRD420251110982.
1 Introduction
Post-stroke spastic paralysis is one of the most common disabling complications in stroke patients. Approximately 43% of stroke survivors experience spasticity within 12 months of the acute episode, and the prevalence increases to as high as 97% in the chronic phase (1). With the annual increase in the global number of stroke cases, post-stroke spastic paralysis has become a core issue leading to motor dysfunction and reduced quality of life in patients (2). Spasticity is a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes, elevated muscle tone, and hyperactive tendon reflexes (3). Upper-limb spasticity often manifests itself as shoulder adduction and internal rotation, accompanied by elbow flexion, wrist flexion, and finger flexion (4). Modern medical interventions primarily include oral antispastic medications, botulinum toxin injections, and rehabilitation therapy. However, these approaches often involve strong drug dependency and are prone to adverse reactions such as fatigue and drowsiness (5). Acupuncture, as a traditional Chinese medicine therapy, has shown considerable efficacy in treating post-stroke spasticity (6). Among various acupuncture techniques, filiform needle acupuncture is a fundamental clinical intervention due to its simplicity, high safety, and low cost. Nevertheless, the wide diversity of acupuncture protocols precludes a definitive conclusion regarding which approach is most effective for post-stroke upper-limb spasticity. Network meta-analysis (NMA) can simultaneously compare the effects of multiple interventions and rank the efficacy of each (7). This study aims to use NMA to evaluate the therapeutic effects of different acupuncture methods to identify the optimal treatment, thereby providing evidence-based support for clinical decision-making.
2 Methods
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines and has been registered on the PROSPERO platform under registration number CRD420251110982. Clinical trial number: not applicable.
2.1 Inclusion criteria
The inclusion criteria were as follows: ① Study type: Randomized controlled trials (RCTs) on filiform needle acupuncture for post-stroke spasticity.
② Participants: Patients meeting the diagnostic criteria for stroke and presenting clinical features such as increased muscle tone, abnormal tendon reflexes, and clonus.
③ Interventions: The control group received rehabilitation alone. The treatment group received filiform needle acupuncture in addition to rehabilitation. In both groups, conventional internal medicine treatments for underlying diseases were permitted.
④ Primary outcome measures: (a) Fugl–Meyer Assessment (FMA) scores (b) Modified Ashworth Scale (MAS). The included trials were required to report at least one outcome measure related to upper-limb spasticity.
2.2 Exclusion criteria
The exclusion criteria were as follows: ① Duplicate publications, for which only the most recent study was included. ② Trials with incomplete data and or unavailable full texts. ③ Reviews, animal experiments, conference proceedings, dissertations, and experience summaries. ④ Trials involving the use of muscle relaxants. ⑤ Trials in which outcome measures did not distinguish between upper and lower limbs.
2.3 Search strategy
A comprehensive computerized search was conducted across multiple electronic databases, including China National Knowledge Infrastructure (CNKI), Wanfang Database, VIP Database (VIP), China Biology Medicine disc (CBM), PubMed, Embase, Cochrane Library, and Web of Science. The search strategy used a combination of subject headings and free-text terms. The search terms included stroke, cerebral infarction, cerebral hemorrhage, spasm, spasticity, spastic paralysis, muscle tonus, randomized controlled trials, RCT, and acupuncture. The search encompassed all records from inception to October 2025. Detailed information on the literature search terms can be found in Supplementary file 1.
2.4 Literature retrieval and data extraction
Literature screening and review were conducted independently by two researchers. Discrepancies were resolved through discussion or, when necessary, consultation with a third researcher. After a consensus was reached, data were extracted, including the following primary information: first author, publication date, sample size, mean age, treatment measures and course, outcome indicators, and elements for risk bias assessment.
2.5 Literature quality assessment
The Cochrane Risk of Bias tool was used to assess the included trials (8). The assessment covered the following aspects: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, selective reporting, and other potential biases.
2.6 Statistical analysis
RevMan 5.4 software was used to generate the literature quality assessment graph. Stata 18 software was used for data analysis. For continuous variables, the mean difference (MD) was selected as the effect size. A p-value of < 0.05 was considered statistically significant. Stata 18 software was used to construct the network evidence graph, in which each node represents an intervention, the size of the node corresponds to the number of cases for that intervention, and the solid lines between nodes indicate direct comparison between two interventions, with the thickness of the line reflecting the amount of direct comparison evidence. If the network evidence graph did not form closed loops, the consistency model was used for the NMA. If closed loops were present, the node-splitting method was applied for inconsistency testing. The surface under the cumulative ranking curve (SUCRA) was calculated to rank the efficacy of various interventions. A comparison-adjusted funnel plot was generated using Stata 18 software to assess publication bias and small-study effects within the intervention network.
3 Results
3.1 Literature search results
The initial search retrieved 11,330 articles (10,634 in Chinese and 696 in English). After removing 5,736 duplicates, 5,594 articles remained for initial screening. Following a detailed review of abstracts and full texts, 28 articles were ultimately included. The detailed screening process is shown in Figure 1.
Figure 1

Screening flow diagram.
3.2 Basic characteristics of included trials
The 28 included trials involved a total of 2,626 patients, of which 1,317 were in treatment groups and 1,309 in control groups. All included trials were two-arm trials. They involved 14 acupuncture methods, including: Governor Vessel Acupuncture + Rehabilitation, Xingnao Kaiqiao Acupuncture + Rehabilitation, Xingnao Kaiqiao Acupuncture combined with Scalp Acupuncture + Rehabilitation, Scalp Acupuncture + Rehabilitation, Jin’s Three-Needle Technique + Rehabilitation, Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling + Rehabilitation, Penetrating Needling + Rehabilitation, Meridian Sinew Acupuncture + Rehabilitation, Acupuncture at Shangjiejing Point Plus Jing-Well Points + Rehabilitation, Balanced Yin-Yang Acupuncture + Rehabilitation, Acupuncture at Jiaji Points + Rehabilitation, Acupuncture at Antagonist Muscles + Rehabilitation, Scalp Acupuncture combined with Yangming Meridian Acupuncture + Rehabilitation, and Yangming Meridian Acupuncture + Rehabilitation. The baseline characteristics of the included trials are presented in Table 1.
Table 1
| Author | Year | Treatment group | Control group | Treatment duration (days) | Outcome measures | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | Intervention | Mean age | n | Intervention | Mean age | ||||
| Zhang Junyu | 2023 | 32 | B | 68 ± 8 | 31 | A | 66 ± 9 | 28 | ①② |
| Zhang Zhixin | 2024 | 40 | B | 63.92 ± 4.14 | 40 | A | 63.86 ± 4.17 | 42 | ① |
| Li Guanglin | 2025 | 30 | B | 58.49 ± 5.8 | 30 | A | 58.96 ± 5.9 | 28 | ② |
| Yang Man | 2018 | 42 | C | 65.53 ± 4.19 | 42 | A | 65.59 ± 4.24 | 28 | ① |
| Liu Hongjie | 2023 | 30 | C | 55.23 ± 7.86 | 29 | A | 54.83 ± 13.92 | 30 | ①② |
| Lou Anhua | 2023 | 65 | C | 54.76 ± 9.98 | 60 | A | 53.68 ± 9.25 | 14 | ① |
| Ma Xiaoli | 2023 | 53 | C | 61.83 ± 8.18 | 53 | A | 62.76 ± 7.36 | 28 | ② |
| Du Liangbin | 2023 | 31 | D | 63.12 ± 8.45 | 34 | A | 62.26 ± 8.26 | 90 | ① |
| Wang Zhihong | 2023 | 90 | D | 35 ~ 85 | 90 | A | 35 ~ 85 | 56 | ①② |
| Jin Lihui | 2023 | 46 | E | 59.48 ± 9.16 | 46 | A | 58.72 ± 8.93 | 28 | ① |
| Qi Lili | 2018 | 30 | E | 64 ± 10 | 30 | A | 65 ± 9 | 30 | ② |
| Lv Lili | 2022 | 51 | F | 63.15 ± 4.19 | 51 | A | 62.08 + 4.32 | 28 | ① |
| Lang Jianying | 2013 | 47 | F | 65 ± 9 | 47 | A | 64 ± 9 | 28 | ① |
| Xu Shifen | 2016 | 36 | F | 60 ± 10 | 35 | A | 65 ± 6 | 28 | ① |
| Ye Weibin | 2019 | 60 | G | 67.3 ± 3.4 | 60 | C | 62.3 ± 2.1 | 20 | ② |
| Zhu Jinmei | 2020 | 30 | H | 63 ± 10 | 30 | A | 64 ± 13 | 28 | ①② |
| Tan Shihong | 2018 | 44 | H | 54.93 ± 7.82 | 44 | A | 54.78 ± 7.69 | 28 | ①② |
| Wen Hongyuan | 2022 | 41 | I | 53.38 ± 4.69 | 40 | A | 53.25 ± 4.70 | 28 | ①② |
| Ni Huanhuan | 2012 | 50 | J | 40–79 | 50 | A | 40–79 | 28 | ① |
| Chen Hailing | 2020 | 60 | J | 62.53 ± 2.14 | 60 | A | 62.45 ± 2.18 | 28 | ① |
| Hu Yinghua | 2017 | 45 | K | 55.30 ± 5.20 | 45 | A | 54.80 ± 4.90 | 14 | ①② |
| Chen Lijun | 2020 | 39 | K | 53.7 ± 4.4 | 39 | A | 53.5 ± 4.1 | 14 | ①② |
| Wang Ya | 2021 | 58 | K | 58.46 ± 6.71 | 58 | A | 58.32 ± 5.24 | 30 | ①② |
| Liao Mingxuan | 2018 | 37 | L | 51.5 ± 4.65 | 35 | A | 50.9 ± 5.65 | 28 | ① |
| Zhao Juanjuan | 2021 | 71 | L | 65.65 ± 8.15 | 71 | A | 65.62 ± 8.11 | 56 | ① |
| Cao Qinning | 2012 | 30 | M | 62.51 ± 7.18 | 30 | A | 61.74 ± 7.68 | 75 | ①② |
| Qiu Lin | 2014 | 45 | N | 60.2 ± 10.4 | 45 | A | 59.6 ± 9.7 | 56 | ① |
| Xia Zhaoxin | 2018 | 84 | P | 67 ± 5.99 | 84 | A | 68 ± 5.43 | 21 | |
Characteristics of included trials.
A: Rehabilitation only, B: Governor Vessel Acupuncture + Rehabilitation, C: Xingnao Kaiqiao Acupuncture + Rehabilitation, D: Xingnao Kaiqiao Acupuncture combined with Scalp Acupuncture + Rehabilitation, E: Scalp Acupuncture + Rehabilitation, F: Jin’s Three-Needle Technique + Rehabilitation, G: Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling + Rehabilitation, H: Penetrating Needling + Rehabilitation, I: Meridian Sinew Acupuncture + Rehabilitation, J: Acupuncture at Shangjiejing Point Plus Jing-Well Points + Rehabilitation, K: Balanced Yin-Yang Acupuncture + Rehabilitation, L: Acupuncture at Jiaji (EX-B2) Points + Rehabilitation, M: Acupuncture at Antagonist Muscles + Rehabilitation, N: Scalp Acupuncture combined with Yangming Meridian Acupuncture + Rehabilitation, and O: Yangming Meridian Acupuncture + Rehabilitation. Outcome measures: ① FMA and ② MAS. Detailed information for each individual study can be found in Supplementary file 2, which includes specific scoring of the outcome measures.
3.3 Literature quality assessment
Randomization method: Among the 28 included trials, 17 trials (9–25) used a random number table and 1 trial (26) used random drawing, which were rated as low risk. Nine trials (27–35) only mentioned “randomization” without any specification, and one trial (36) only referred to computer grouping without a detailed description; these were rated as unclear risk.
Allocation concealment: Two trials (10, 18) adopted sealed-envelope methods and were therefore rated as low risk. The remaining trials did not mention whether allocation concealment was implemented and were rated as unclear risk.
Blinding: None of the trials described blinding procedures or implementation details. One trial (10) reported blinding of outcome assessors and was rated as low risk, whereas the remaining trials did not specify the method of outcome assessment and were rated as unclear risk.
Incomplete outcome data: Four trials (10, 12, 24, 29) reported data attrition, but dropout rates were low and unlikely to affect the intervention effect estimate; thus, they were rated as low risk.
Selective reporting: None of the included trials provided protocols or pre-registered plans, making it impossible to assess selective reporting risk; all were rated as unclear risk.
Other biases: Sources of other potential biases were unclear across all trials, resulting in an unclear risk rating. The risk of bias assessment results for the included trials are presented in Figure 2.
Figure 2
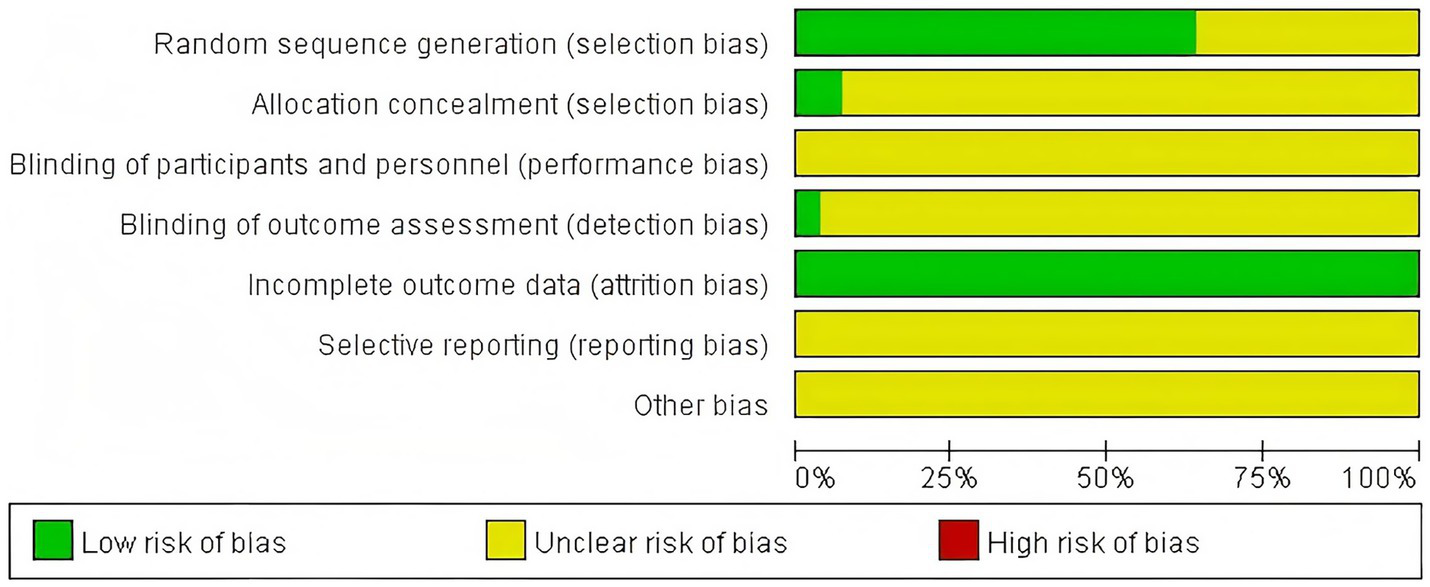
Risk of bias.
3.4 Network geometry
Twenty-three trials reported the FMA involving 12 different acupuncture methods. The network graph for FMA is shown in Figure 3. Fifteen trials reported MAS, involving 10 different acupuncture methods. The network graph for MAS is shown in Figure 4. No closed loops were formed between interventions, making inconsistency testing unnecessary.
Figure 3

Network evidence graph of FMA.
Figure 4
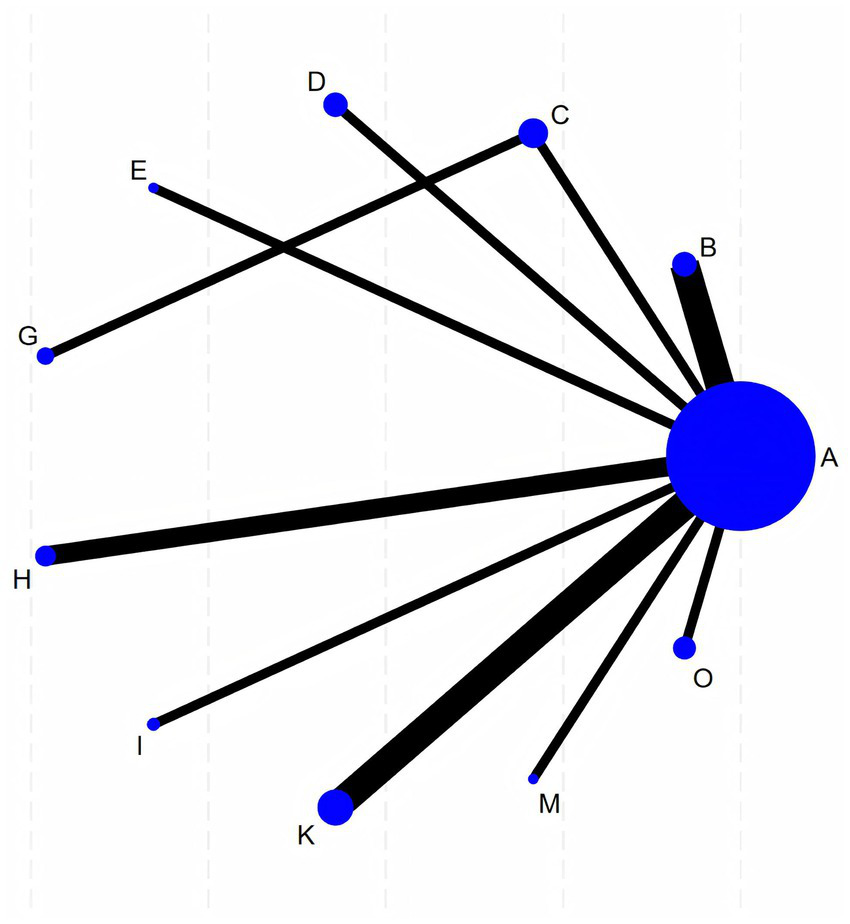
Network evidence graph of MAS. In the figures above, each lettered node represents an intervention (the corresponding acupuncture method for each letter is shown in Table 1). Both network evidence graphs feature A (rehabilitation) as the central node. The size of a node is proportional to the total sample size of that intervention. Lines connecting nodes indicate the existence of RCTs with direct comparisons between the interventions, and the thickness of a line is proportional to the number of studies providing direct comparative evidence. The network geometry indicates that most interventions lack direct comparative evidence, and the efficacy evaluation relies heavily on indirect comparisons using rehabilitation training as a common comparator.
3.5 Network meta-analysis results
For FMA, the following interventions combined with rehabilitation were superior to rehabilitation alone (p < 0.05): Xingnao Kaiqiao Acupuncture [MD = 6.74, 95%CI (2.13, 11.35)], Xingnao Kaiqiao Acupuncture combined with Scalp Acupuncture [MD = 6.33, 95%CI (0.38, 12.28)], Jin’s Three-Needle Technique [MD = 8.47, 95%CI (3.33, 13.61)], Acupuncture at Shangjiejing Point Plus Jing-Well Points [MD = 6.17, 95%CI (0.83, 11.50)], Balanced Yin-Yang Acupuncture [MD = 10.63, 95%CI (6.06, 15.21)], and Acupuncture at Jiaji Points [MD = 7.60, 95%CI (2.07, 13.12)]. No statistically significant differences were observed in pairwise comparisons between the other interventions.
For MAS, the following interventions combined with rehabilitation were superior to rehabilitation alone (p < 0.05): Governor Vessel Acupuncture [MD = -0.60, 95%CI (−0.99, −0.22)], Scalp Acupuncture [MD = -0.90, 95%CI (−1.57, −0.23)], Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling [MD = -1.05, 95%CI (−1.95, −0.15)], Balanced Yin-Yang Acupuncture [MD = -0.79, 95%CI (−1.15, −0.42)], and Yangming Meridian Acupuncture [MD = -0.82, 95%CI (−1.43, −0.21)]. No statistically significant differences were observed in pairwise comparisons between the other interventions. Specific results are shown in Figure 5.
Figure 5
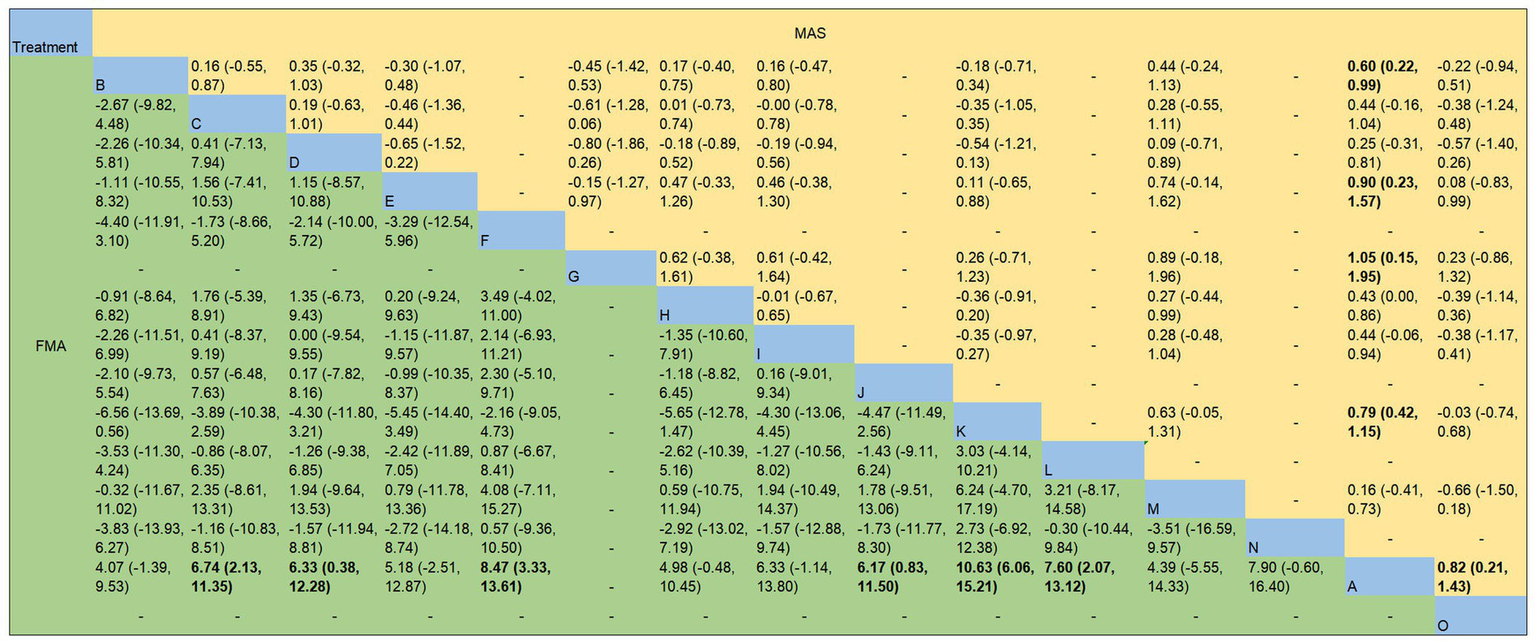
Network meta-analysis results for FMA and MAS. The figures display the mean differences and 95% confidence intervals for pairwise comparisons between interventions. When the confidence interval includes 0, it indicates that the difference is not statistically significant. Bold type denotes statistical significance. The corresponding acupuncture treatment methods for the English letters are as described in the notes of Table 1.
3.6 SUCRA ranking
Interventions were ranked from best to worst based on SUCRA values for FMA: Balanced Yin-Yang Acupuncture + Rehabilitation (86.3%) > Jin’s Three-Needle Technique + Rehabilitation (70.0%) > Scalp Acupuncture combined with Yangming Meridian Acupuncture + Rehabilitation (63.1%) > Acupuncture at Jiaji Points + Rehabilitation (62.5%) > Xingnao Kaiqiao Acupuncture + Rehabilitation (55.5%) > Xingnao Kaiqiao Acupuncture combined with Scalp Acupuncture + Rehabilitation (51.8%) > Meridian Sinew Acupuncture + Rehabilitation (51.7%) > Acupuncture at Shangjiejing Point Plus Jing-Well Points + Rehabilitation (50.3%) > Scalp Acupuncture + Rehabilitation (43.2%) > Penetrating Needling + Rehabilitation (39.8%) > Acupuncture at Antagonist Muscles + Rehabilitation (38.4%) > Governor Vessel Acupuncture + Rehabilitation (32.9%) > Rehabilitation alone (4.4%).
Interventions were ranked from best to worst based on SUCRA values for modified Ashworth scores: Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling + Rehabilitation (83.7%) > Scalp Acupuncture + Rehabilitation (78.0%) > Balanced Yin-Yang Acupuncture + Rehabilitation (73.9%) > Yangming Meridian Acupuncture + Rehabilitation (73.7%) > Governor Vessel Acupuncture + Rehabilitation (57.6%) > Meridian Sinew Acupuncture + Rehabilitation (43.4%) > Penetrating Needling + Rehabilitation (42.2%) > Xingnao Kaiqiao Acupuncture + Rehabilitation (41.8%) > Xingnao Kaiqiao Acupuncture combined with Scalp Acupuncture + Rehabilitation (27.9%) > Acupuncture At Antagonist Muscles + Rehabilitation (21.3%) > Rehabilitation alone (6.5%).
3.7 Publication Bias analysis
Figure 6 displays the funnel plot for FMA, while Figure 7 presents the corresponding funnel plot for MAS. The distribution pattern demonstrates moderate symmetry, with several studies located beyond the funnel plot’s confidence limits, indicating potential publication bias or influences from small-sample effects.
Figure 6
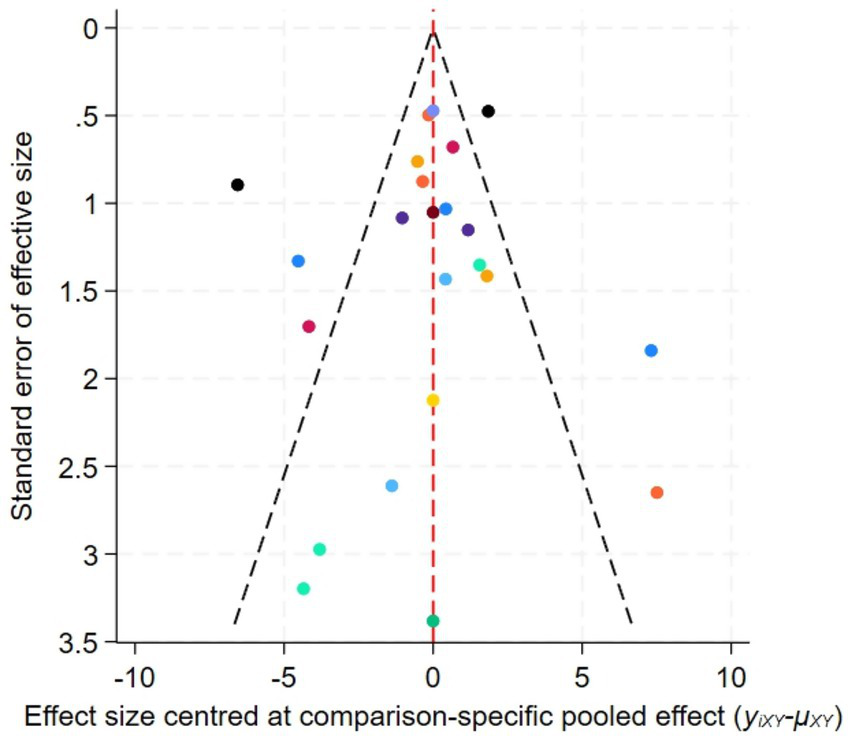
Funnel plot for the network meta-analysis of FMA.
Figure 7
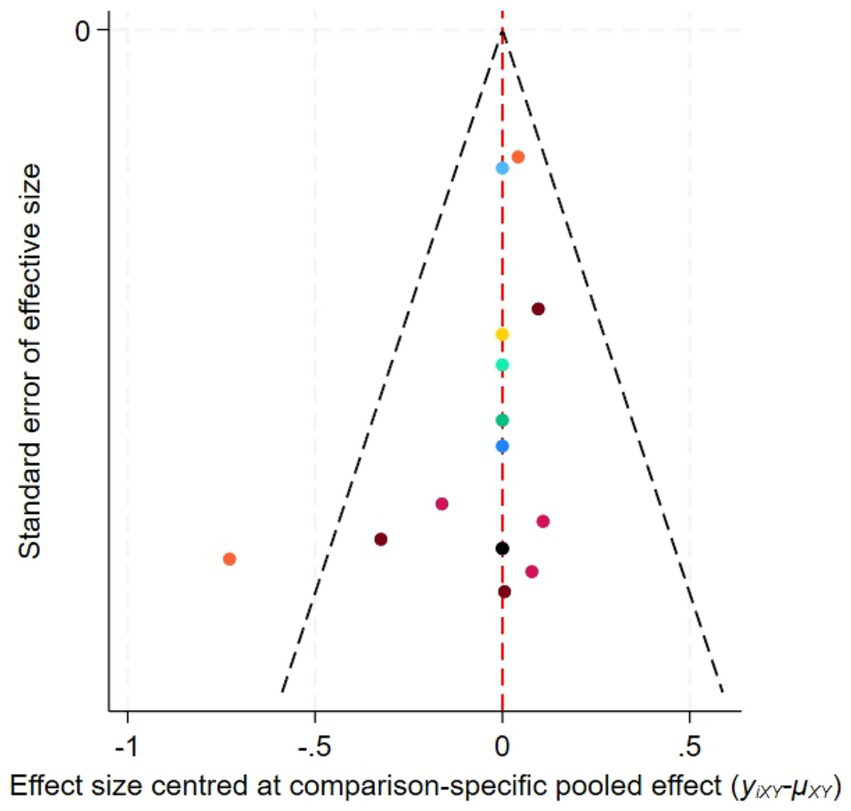
Funnel plot for the network meta-analysis of MAS.
4 Discussion
This study systematically evaluated the interventional effects of 14 acupuncture methods on post-stroke upper-limb spasticity using NMA. The NMA results indicated that Balanced Yin-Yang Acupuncture + Rehabilitation was the most effective in improving FMA scores. Balanced Yin-Yang Acupuncture uses point selection from both the medial and lateral aspects of the upper limb. For spastic muscle groups, shallow needling is applied, followed by rapid, small-amplitude lifting and thrusting with a reducing technique after obtaining qi. For antagonist muscle groups, appropriately deep needling is applied, followed by uniform, slow twisting with a reinforcing technique after obtaining qi. Modern studies suggest that Balanced Yin-Yang acupuncture can improve serum levels of transforming growth factor-β1 (TGF-β1) and neuron-specific enolase (NSE) in patients, which may help improve the prognosis of post-stroke spasticity (37). Furthermore, evidence from (24) indicates that acupuncture can effectively activate stretch receptors such as Golgi tendon organs, inhibit α motor neurons innervating spastic muscles, and simultaneously excite motor neurons of antagonist muscles. Through these mechanisms, acupuncture achieves the goal of inhibiting spastic muscles and activating antagonist muscles, thereby harmonizing limb muscle tone and restoring normal movement patterns.
Regarding the reduction of MAS scores, Luan’s Three-Needle Technique combined with Meridian Sinew Cluster Needling + Rehabilitation ranked first. The acupoints selected in Luan’s Three-Needle Technique are often adjacent to the main nerve trunks of the body, focusing on local points around the spastic joints. The acupoint selection for Luan’s Three-Needle Technique in the upper limb includes Neiguan (PC 6), Jiquan (HT 1), and Chize (LU 5). Modern research has found that acupuncture at Neiguan (PC 6) can activate the frontal lobe, the temporal lobe, and other brain areas, increase cerebral blood flow perfusion, improve brain blood supply, and promote the recovery of neurological function (38). From the perspective of local anatomy, beneath Jiquan (HT 1) lies the median nerve, the ulnar nerve, and the radial nerve, with both the ulnar and median nerves innervating flexor muscles. For spastic patients, acupuncture should primarily target the extensor muscles innervated by the radial nerve. When the upper limb extensor muscles are stimulated and become excited, leading to contraction, the flexor muscles are inhibited, thereby reducing muscle tone and alleviating upper limb flexor spasticity. Chize (LU 5) is located at the elbow, which is often the most severely affected site for upper limb muscle spasticity. One systematic review summarized the most commonly used acupoints for treating post-stroke spasticity, which included Neiguan (PC 6) and Chize (LU 5), among others (39). Furthermore, the meridian sinew cluster needling involves applying multiple needles along the Yangming Meridian. Multiple needling stimulation along the lateral aspect of the upper limb can extensively activate the nerves of the upper limb, improve neural nutrition, promote metabolic processes in nervous tissue, and enhance its excitability. Simultaneously, it can facilitate local blood circulation, induce contractions in the muscles on the low-tension side of the limb, and increase the strength of the upper limb extensors. Therefore, based on the commonalities of the above conclusions, for patients with post-stroke upper limb spasticity, acupuncture point selection should consider both the medial and lateral aspects of the limb, so as to better coordinate the balance between agonists and antagonists and restore optimal limb movement patterns.
This study has several limitations: (a) Among the 28 included trials, several exhibited suboptimal quality, lacking clear descriptions of key information such as randomization methods, allocation concealment, and blinding. (b) Differences in the selection of acupoints and treatment courses among the included trials may affect the precision of the results. (c) The network graphs did not form closed loops, meaning that efficacy comparisons between many interventions rely solely on indirect evidence. This implies that, although the SUCRA values provide an intuitive reference for ranking the efficacy of different acupuncture methods, the current rankings—particularly the minor differences between adjacently ranked interventions—have low statistical power and limited clinical confirmation. (d) All included studies were conducted in China. Therefore, the applicability of the conclusions in a global context still requires validation through the inclusion of more high-quality studies from diverse regions and healthcare systems.
In conclusion, this study provides a comprehensive assessment of the effects of various acupuncture methods on post-stroke upper upper-limb spasticity through network meta-analysis, clarifying the relative advantages of different acupuncture methods for two outcome measures (FMA and MAS). It offers valuable candidate protocols and priority research directions for clinical practice. However, given the limitations of this study, these findings are not yet sufficient to serve as strong evidence for altering clinical guidelines or practice standards. Future research urgently requires well-designed, rigorously reported large-sample randomized controlled trials, with particular emphasis on the strict implementation and clear reporting of core elements such as randomization, allocation concealment, and blinding. Such high-quality studies are needed to provide direct comparison evidence for verifying or refining the preliminary rankings derived from this network meta-analysis. Until such high-quality evidence is obtained, clinicians should integrate the findings of this study with patients’ specific conditions, clinical experience, and available resources when making treatment decisions.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
FX: Writing – original draft, Writing – review & editing. RZ: Writing – review & editing, Writing – original draft. YaG: Formal analysis, Writing – review & editing. YW: Data curation, Writing – review & editing. YuG: Software, Writing – review & editing. LYa: Data curation, Writing – review & editing. ZW: Methodology, Writing – review & editing. ZL: Data curation, Writing – review & editing. RJ: Data curation, Writing – review & editing. JW: Data curation, Writing – review & editing. YZ: Data curation, Writing – review & editing. JS: Resources, Supervision, Writing – review & editing. LYi: Funding acquisition, Resources, Writing – review & editing.
Funding
This study was funded by the Open Research Project of the National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion(NCRCOP20230016), National Administration of Traditional Chinese Medicine Special Research Project for Operational Construction of National Clinical Research Bases of Traditional Chinese Medicine(JDZX2015017) and Scientific Research Program of Hebei Provincial Administration of Traditional Chinese Medicine (T2025112).
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that Generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2026.1725618/full#supplementary-material
SUPPLEMENTARY FILE 1Detailed search terms.
SUPPLEMENTARY FILE 2Detailed information on individual studies.
Abbreviations
NMA, Network Meta-Analysis; MAS, Modified Ashworth Scale; FMA, Fugl-Meyer Assessment; SUCRA, Surface Under the Cumulative Ranking Curve.
References
1.
Dorňák T Justanová M Konvalinková R Říha M Mužík J Hoskovcová M et al . Prevalence and evolution of spasticity in patients suffering from first-ever stroke with carotid origin: a prospective, longitudinal study. Eur J Neurol. (2019) 26:880–6. doi: 10.1111/ene.13902,
2.
GBD 2021 Stroke Risk Factor Collaborators . Global, regional, and national burden of stroke and its risk factors, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet Neurol. (2024) 23:973–1003. doi: 10.1016/S1474-4422(24)00369-7
3.
Lee J Yang SN . Effectiveness of extracorporeal shock wave therapy after botulinum toxin injection for post-stroke upper extremity spasticity: a randomized controlled study. Toxins. (2024) 16:197. doi: 10.3390/toxins16040197
4.
Marciniak C . Poststroke hypertonicity: upper limb assessment and treatment. Top Stroke Rehabil. (2011) 18:179–94. doi: 10.1310/tsr1803-179,
5.
Satkunam L Dukelow SP Yu JC McNeil S Luu H Martins KJB et al . Post-stroke spasticity treatment: a retrospective cohort study from Alberta, Canada. Can J Neurol Sci J Can Sci Neurol. (2024) 11:1–9. doi: 10.1017/cjn.2024.342
6.
Xue C Jiang C Zhu Y Liu X Zhong D Li Y et al . Effectiveness and safety of acupuncture for post-stroke spasticity: a systematic review and meta-analysis. Front Neurol. (2022) 13:942597. doi: 10.3389/fneur.2022.942597,
7.
Puerto Nino AK Brignardello-Petersen R . How to read a network meta-analysis. Eur Urol. Focus. (2023) 9:701–4. doi: 10.1016/j.euf.2023.10.018
8.
Cumpston M Li T Page MJ Chandler J Welch VA Higgins JP et al . Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. (2019 Oct 3) 10:ED000142. doi: 10.1002/14651858.ED000142,
9.
Li GL Fang J Wang JA Dai QB . Application of governor vessel regulating-Spirit acupuncture combined with occupational therapy in the treatment of upper limb spasticity after stroke. Mod Med Health Res Electron J. (2025) 9:116–8.
10.
Zhang JY Mao W Dai F Wu MM Yang K Qin XF et al . Tongdu Tiaoshen acupuncture combined with Bobath rehabilitation training for upper limb spasm after stroke: a randomized controlled trial. Chin Acupunct Moxibustion. (2024) 44:43–7. doi: 10.13703/j.0255-2930.20230711-k0002
11.
Zhang ZX . Analysis of the effect of Xingnaotongdu acupuncture combined with task oriented training on spastic hemiplegia after stroke patients. Reflexology Rehabil Med. (2024) 5:24–8. doi: 10.16344/j.cnki.10-1669/r4.2024.14.007
12.
Liu HJ Pi TL Rong TC . Clinical observation on upper limb spastic hemiplegia after stroke by using Xingnao Kaiqiao needling and rehabilitation. Acta Neuropharmacol. (2023) 13:45–8.
13.
Ma XL Zhang SY Liu QW . Clinical study of xingshen tiaoxing acupuncture method combined with routine therapy for post-stroke spasticity. New Chin Med. (2023) 55:156–63. doi: 10.13457/j.cnki.jncm.2023.18.031
14.
Wang ZH Zhang SS Li B Cao HY Wang JL . Observation of curative effect of body-spirit integration acupuncture combined with rehabilitation training on spastic hemiplegia patients after ischemic stroke. Yunnan J Tradit Chin Med Mater Med. (2023) 44:23–8. doi: 10.16254/j.cnki.53-1120/r.2023.12.020
15.
Jin LH Wu P . Clinical study on scalp point cluster-needling combined with bobath technique for increased muscle tone of upper limbs after stroke. New Chin Med. (2023) 55:139–43. doi: 10.13457/j.cnki.jncm.2023.24.026
16.
Qi LL Han ZX Zhou YX Chen WH Chu LX Lu JY et al . Dynamic scalp acupuncture combined with PNF therapy for upper limb motor impairment in ischemic stroke spastic hemiplegia. Chin Acupunct Moxibustion. (2018) 38:234–8. doi: 10.13703/j.0255-2930.2018.03.002
17.
Lv LL Wang C Zhang HH Xu XW Wang YW . Clinical effect of Jin’s three needles combined with rehabilitation training in the treatment of increased muscle tone of the hind upper limbs after stroke. China Med Her. (2022) 19:163–6, 179. doi: 10.20047/j.issn1673-7210.2022.17.038
18.
Zhu JM Zhuang R He J Wang XX Wang H Zhu HY . Yin-yang balance penetrating acupuncture combined with rehabilitation training on upper limb spasticity in stroke hemiplegia. Chin Acupunct Moxibustion. (2020) 40:697–701. doi: 10.13703/j.0255-2930.20190531-k0005
19.
Ye WB Zhi CJ Chen QP Chen P Xie LH Kang Z et al . Clinical research of twin three needle combine jingjin needling method in the treatment of upper limb spasticity after cerebral stroke. Clin J Tradit Chin Med. (2019) 31:134–6. doi: 10.16040/j.cnki.cn15-1101.2019.10.048
20.
Wen HY Dai YQ Yang B Xia TT . Clinical observation of low-energy extracorporeal shock wave combined with acupuncture by tendons in the treatment of stroke with increased muscle tone. J Pract Tradit Chin Med. (2022) 38:1231–3.
21.
Ni HH Cui X Hu YS Wu Y Huang DQ Qu PY et al . Therapeutic observation on acupuncture plus rehabilitation for upper-limb spasticity after cerebral apoplexy. Shanghai J Acupunct Moxibustion. (2012) 31:789–91.
22.
Chen HL . Analysis of acupuncture and rehabilitation nursing for upper limb spasticity after stroke. Electronic J Practical Clinical Nursing Science. (2020) 5:23–4.
23.
Wang Y . Clinical observation of draining yin and tonifying yang acupuncture combined with proprioceptive neuromuscular facilitation for post-stroke spastic hemiplegia. J Pract Tradit Chin Med. (2021) 37:2091–3.
24.
Hu YH Wang Y Jiang XL Zhang LJ Liang ZH . Effect of early intervention with balanced yin-yang acupuncture on limb spasticity in patients during acute stage of stroke. J Emerg Tradit Chin Med. (2017) 26:1870–2.
25.
Zhao JJ . Effect of acupuncture at Huatuo Jiaji points combined with rehabilitation training on limb function in patients with spastic limb dysfunction after stroke. Chin J Conval Med. (2021) 30:513–5. doi: 10.13517/j.cnki.ccm.2021.05.022
26.
Du LB . Therapeutic effects of rehabilitation training combined with traditional Chinese medicine movement acupuncture on post-stroke upper limb spastic paralysis: a clinical study. Med Diet Health. (2023) 21:114–6.
27.
Yang M . Xingnao kaiqiao acupuncture combined with rehabilitation training and Western medicine for 42 cases of post-stroke upper limb spastic paralysis. Tradit Chin Med Res. (2018) 31:31–3.
28.
Lang JY Zhuang LX He J Jia C Zhou ZH Ke LP . Randomized controlled study on Jin’s three needle therapy on spastic hemiplesia after ischemic stroke. Shanghai J Acupunct Moxibustion. (2013) 32:440–3.
29.
Xu SF Gu JH . Clinical observation of Jin’s three-needle acupuncture plus rehabilitation for post-stroke spastic hemiplegia. Shanghai J Acupunct Moxibustion. (2016) 35:153–6. doi: 10.13460/j.issn.1005-0957.2016.02.0153
30.
Tan SH . Clinical observation on acupuncture combining Bobath in the treatment of spastic hemiplegia after stroke. Chin J Integr Med Cardio-Cerebrovasc Dis. (2018) 16:3044–7.
31.
Chen LJ Yu X Lu J Gao F Yuan Y Dang BQ . Ffects of balanced yin-yang acupuncture on neurological function, limb spasticity, and functional recovery in patients during acute stage of stroke. Mod J Integr Tradit Chin West Med. (2020) 29:1448–51.
32.
Liao MX Huang GF . Therapeutic effect of acupuncture at Jiaji points (EX-B2) combined with rehabilitation training on post-stroke spastic paralysis. World Latest Med Inf2018;18:129–130, 132. doi: 10.19613/j.cnki.1671-3141.2018.09.057
33.
Xia ZX . Analysis of curative effect of acupuncture combined with rehabilitative therapy in treatment of spastic hemiplegia after cerebrovascular accident. World J Complex Med. (2018) 4:4–6.
34.
Cao QN Qiao HF . Effects of acupuncture at antagonist muscles combined with rehabilitation on spasticity after acute stroke hemiplegia. Shaanxi J Tradit Chin Med. (2012) 33:1530–2.
35.
Qiu L Liu YC . Therapeutic observation of acupuncture combined with rehabilitation training for post-stroke spastic hemiplegia. Henan Tradit Chin Med. (2014) 34:1827–8. doi: 10.16367/j.issn.1003-5028.2014.09.070
36.
Lou AH Liu YX . Effect of acupuncture combined with rehabilitation training in patients with spastic paralysis of upper limbs after stroke. Henan Med Res. (2023) 32:1075–8.
37.
He L Zhong Q . Efficacy of Xieyin Buyang acupuncture combined withNeedling Wuquan points in treating post-stroke spasticParalysis and lts effect on serum levels of TGF-B1 andNSE. J Clin Acupunct Moxibustion. (2020) 36:21–4.
38.
Ma DY Pz Y Zhang QX . Analysis on mechanism of Neiguan(PC6) acupoint in awakening brain and opening orifice. Shandong J Tradit Chin Med. (2024) 43:982–6. doi: 10.16295/j.cnki.0257-358x.2024.09.011
39.
Li S Francisco GE . New insights into the pathophysiology of post-stroke spasticity. Front Hum Neurosci. (2015) 9:192. doi: 10.3389/fnhum.2015.00192,
Summary
Keywords
acupuncture, network meta-analysis, spasticity, stroke, upper limb
Citation
Xing F, Zhang R, Guo Y, Wang Y, Guo Y, Yang L, Wang Z, Liu Z, Jiang R, Wang J, Zhao Y, Shi J and Yin L (2026) Network meta-analysis of different acupuncture methods for post-stroke upper-limb spasticity. Front. Neurol. 17:1725618. doi: 10.3389/fneur.2026.1725618
Received
16 October 2025
Revised
27 December 2025
Accepted
20 January 2026
Published
10 February 2026
Volume
17 - 2026
Edited by
Simone Carozzo, Sant'Anna Crotone Institute, Italy
Reviewed by
Krishnakumar Sankar, Rajalakshmi Engineering College, India
Zhitao Hou, Heilongjiang University of Chinese Medicine, China
Updates
Copyright
© 2026 Xing, Zhang, Guo, Wang, Guo, Yang, Wang, Liu, Jiang, Wang, Zhao, Shi and Yin.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lili Yin, kintelili@163.com; Jiangwei Shi, acustone@163.com
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.