- 1Department of Neurology, Parkinson's Disease Center and Movement Disorders Clinic, Baylor College of Medicine, Houston, TX, United States
- 2Neurology Care Line, Michael E. DeBakey VA Medical Center, Houston, TX, United States
Botulinum toxin is one of the most potent neurotoxins, but when injected into an overactive muscle, it can transiently alleviate an involuntary movement, such as dystonia. The primary aim of this article is to provide a comprehensive review of the various forms of dystonia observed in patients with Parkinson’s disease who can benefit from a therapeutic trial of botulinum toxin. Although most of these indications are not supported by randomized controlled clinical trials and, therefore, not approved by the Food and Drug Administration, there are many open-label trials supporting a large body of empirical experience testifying to the benefits of botulinum toxin treatment in these conditions.
1 Introduction
Dystonia is present in up to 30% of patients with Parkinson’s disease (PD) (Anandan and Jankovic, 2023; Matar and Bhatia, 2023). In some cases of PD or other parkinsonian disorders, dystonia may be one of the motor features, and in other cases, dystonia may be the dominant movement disorder with parkinsonism as the secondary phenomenon, classified as “‘combined’ dystonias” (Albanese et al., 2013). The form of dystonia can be a clue into the type of parkinsonism the patient has. For example, retrocollis/truncal extension is commonly seen in progressive supranuclear palsy (PSP), whereas anterocollis, Pisa sign, and levodopa-induced dyskinesia in the form of oromandibular dystonia are typically seen in multiple system atrophy (MSA), and asymmetric limb dystonia is often present in patients with corticobasal syndrome (CBS) (Vanek and Jankovic, 2001).
The non-aerobic bacteria Clostridium botulinum produces botulinum toxin (BoNT), the most potent biologic toxin (Anandan and Jankovic, 2023). BoNT acts by blocking the release of acetylcholine at the neuromuscular junction, thus causing muscle weakness. This property has been used for therapeutic purposes, including in the treatment of dystonia. There are many indications for BoNT in patients with PD and other parkinsonian disorders (Jankovic, 2009; Cardoso, 2018; Jost, 2021; Lapostolle et al., 2022; Anandan and Jankovic, 2023; Jabbari and Comtesse, 2023). This article will focus on the use of BoNT in PD-associated dystonia.
2 Method
On 11 December 2023, we conducted a PubMed advanced search with the title words “botulinum,” and “Parkinson” and the text word “dystonia.” This yielded 14 articles. We also conducted a PubMed advanced search with the title words “botulinum” and “parkinsonism” and the text word “dystonia.” This yielded eight articles. This article was formulated using these articles and other relevant articles.
3 Discussion
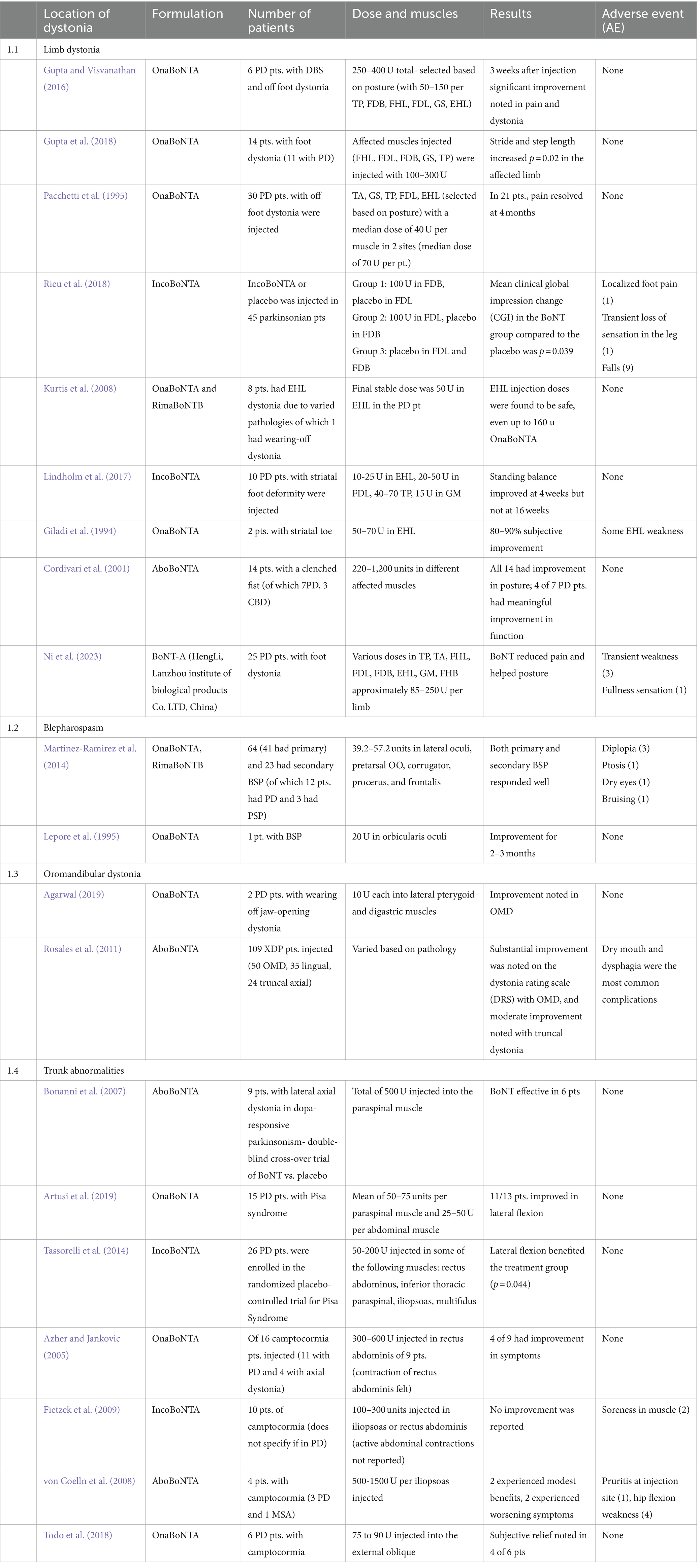
There are numerous forms of dystonia in patients with PD and other parkinsonian disorders that can benefit from BoNT (Table 1).
3.1 Limb dystonia
Foot dystonia, produced by involuntary, repetitive, twisting contractions of muscles in the foot, occurs most often when carbidopa-levodopa wears off (Jost, 2021; Anandan and Jankovic, 2023). This “wearing off” foot dystonia is usually characterized by ankle plantarflexion/inversion, with toes curling usually downward, but sometimes the toes (particularly the big toe) extend. There are several reports that have discussed the benefits of BoNT in “wearing off” foot dystonia (Gupta and Visvanathan, 2016; Rieu et al., 2018). In our clinic, we treat this form of dystonia with BoNT injections in the tibialis posterior, flexor digitorum brevis, flexor digitorum longus, and extensor hallucis longus. We occasionally also target the gastrocnemius if there is troublesome plantar flexion or associated calf cramps. Among 13 patients with upper limb dystonia due to X-linked dystonia parkinsonism (XDP), a median 12-week benefit after BoNT injection was noted, with 15% of patients experiencing weakness post-injection (Rosales et al., 2011).
“Striatal toe” is a form of fixed deformity, which is different from “wearing off” foot dystonia. Approximately 13% of patients with PD can have striatal limb deformities and the cause remains unknown (Wijemanne and Jankovic, 2019). This can affect gait and reduce the ability to stand and ambulate (Lindholm et al., 2017). Targeting the extensor hallucis longus with BoNT can be quite effective (Kurtis et al., 2008).
Clenched fists due to dystonia can be a late complication in PD and other parkinsonism disorders (Jocson and Lew, 2019). There are reports of this focal dystonia improving with BoNT, thus improving function and facilitating good hygiene (Cordivari et al., 2001). Striatal hand and foot deformities are not thought to derive from dystonia; hence, BoNT has not been traditionally used to treat these conditions (Wijemanne and Jankovic, 2019).
3.2 Cervical dystonia
Cervical dystonia (CD) is the most common form of focal dystonia encountered in movement disorders clinics. It can lead to abnormal head/neck posture and movement, tremors, and pain (Albanese et al., 2023). CD was found to be present in 33.9% of patients with PD (Jost, 2021). Oromandibular dystonia, anterocollis, and scoliosis (Pisa sign) are commonly seen in patients with parkinsonism, especially in those with MSA (Marsili and Truong, 2020). Dysphagia is a common complication of anterocollis, and this can be worsened with anterior neck muscle BoNT injections, particularly with bilateral injections; hence, it is crucial to start with low doses of BoNT in these instances. The usefulness of BoNT in the treatment of CD has been demonstrated in numerous trials (Hammoud and Jankovic, 2022). In one study of 144 patients with CD and 24 due to parkinsonism, the duration of benefit, dosage of BoNT, and occurrence of dysphagia after BoNT were similar in patients with CD and associated parkinsonism vs. CD without parkinsonism (Patterson et al., 2016). Of the 109 patients with XDP, 21 had torticollis, 11 had retrocollis, 14 had laterocollis, and 10 had anterocollis (Rosales et al., 2011). The median dose of abobotulinum toxin A injected per visit varied from 250 to 500 units. The authors reported improvement lasting approximately 12 weeks; the frequency of dysphagia ranged from 14% for torticollis to 20% for anterocollis (Rosales et al., 2011).
3.3 Blepharospasm
Blepharospasm is a form of focal dystonia that is characterized by involuntary eye closure due to contractions of the orbicularis oculi and other periorbital muscles (Romano et al., 2022). Blepharoclonus, manifested by repetitive spasms of the eyelids without actual eye closure, was noted in 84% of patients with PD in one recent study (Margolesky et al., 2024). Apraxia of eyelid opening, which is manifested by the inability to open eyes (presumably by inhibition of the levator oculi), typically associated with compensatory frontalis contraction, can also be seen in PD but is even more frequent in patients with atypical parkinsonism (Piccione et al., 1997; Yoon et al., 2005). A retrospective review of 64 patients with blepharospasm, 41 with primary blepharospasm, and 23 with secondary blepharospasm, of which 12 had PD and 3 had PSP, examined the effects of BoNT treatment. BoNT injections (either onabotulinumtoxin A or rimabotulinumtoxin B was used) into the periorbital muscles (including the lateral oculi, pretarsal, procerus, corrugator, and frontalis) resulted in benefits lasting 9.43 and 9.67 weeks in primary and secondary blepharospasm, respectively (Martinez-Ramirez et al., 2014). Onabotulinumtoxin A (12.5 units per eye injection into the junction of the preseptal and pretarsal portions) can produce relief in patients with apraxia of the eyelid opening associated with parkinsonism (Piccione et al., 1997). In another study, onabotulinumtoxin A 20 U into the pretarsal portion of orbicularis oculi produced benefits for 2–3 months (Lepore et al., 1995). There are additional reports of improved apraxia of eyelid opening after BoNT (Defazio et al., 1990; Jankovic, 1996).
3.4 Oromandibular dystonia
Oromandibular dystonia is relatively uncommon in PD, but it is a relatively common complication of levodopa therapy in MSA (Anandan and Jankovic, 2023). Wearing off jaw dystonia has been reported to improve after BoNT injections (Agarwal, 2019). In X-linked dystonia parkinsonism, 32 patients had jaw-opening dystonia, treated with BoNT injections into the lateral pterygoid and anterior digastric muscles with a median dose of 100 U of abobotulinumtoxin A. A total of 12 patients with jaw closing dystonia (injected into masseter, temporalis, and medial pterygoid with a median dose of 150 U of abobotulinumtoxin A) and 6 patients with jaw deviation (injected into lateral pterygoid and temporalis with a median dose of 100 U abobotulinumtoxin A) noted median improvement lasting 8–16 and 12–24 weeks, respectively; 17–19% experienced adverse effects such as dry mouth and dysphagia (Rosales et al., 2011). Many patients with PD and other parkinsonian disorders experience temporomandibular joint pain, most likely related to daytime or nocturnal bruxism (Ondo et al., 2018; Verhoeff et al., 2022; Minervini et al., 2023). Based on a double-blind, placebo-controlled trial, BoNT injections targeting the masseter and temporalis muscles have been found to be safe and effective in the treatment of bruxism (Ondo et al., 2018).
3.5 Laryngeal dystonia
Spasmodic dysphonia is a focal dystonia involving the laryngeal muscles associated with either adductor spasm (resulting in a strained voice and breaks in phonation) or, rarely, abductor spasm (associated with breathy voice and voiceless pauses) or both (Truong and Bhidayasiri, 2006; Simonyan et al., 2021). These can be successfully treated with BoNT injections into the thyroarytenoid muscle (for adductor spasmodic dysphonia) and the posterior cricoarytenoid muscle (for abductor spasmodic dysphonia). In one patient with PD who did not respond to BoNT-A (abobotulinumtoxin A followed by onabotulinumtoxin A was tried) for spasmodic dysphonia, BoNT-B (Neurobloc) was effective (Sachdev et al., 2019). It is unclear why there was no response to type A BoNT in this spurious single-case report.
3.6 Trunk abnormalities
One-third of PD patients have abnormal truncal postures, which may also include Pisa syndrome (leaning to one side due to scoliosis), lateral axial dystonia, and camptocormia (Wijemanne and Jankovic, 2019). Pisa syndrome occurs in 7–10% of PD patients (Artusi et al., 2019). An improvement in the axial posture was found in a double-blind placebo-controlled trial of incobotulinum toxin A injected into muscles individually identified for patients with Pisa syndrome (Tassorelli et al., 2014). A PD patient with Pisa syndrome improved after undergoing paraspinal muscle abobotulinumtoxin A injections and a rehabilitation program (Santamato et al., 2010). Pisa syndrome due to lateral axial dystonia (dystonic scoliosis) can be painful and affect mobility (Bonanni et al., 2007). Camptocormia is characterized by moderate to marked flexion of the thoracolumbar spine caused by isolated axial dystonia or complex dystonia related to underlying PD or other parkinsonian disorders (Azher and Jankovic, 2005; Wijemanne and Jankovic, 2019). Several case series have reported inconsistent improvement of camptocormia with BoNT injections, but BoNT targeting the rectus abdominis or external oblique muscle may be very effective in improving the axial posture (Azher and Jankovic, 2005; Colosimo and Salvatori, 2009; Fietzek et al., 2009). Among 109 patients with X-linked dystonia parkinsonism, 12 had trunk flexor dystonia, 7 had trunk extensor dystonia, and 5 had lateral trunk dystonia, and they were injected with abobotulinumtoxin A with a median dose of 400 U in rectus abdominis, 750 U in bilateral erector spinae, and 1,000 U in ipsilateral erector spinae, respectively (Rosales et al., 2011).
3.7 Levodopa-related dystonia
Levodopa-related dystonia is a well-recognized complication of levodopa therapy in patients with PD (Jameson, 1970; Cooper, 1972; Pfeiffer and LeDoux, 2015). One single case report described a patient with PD who developed jaw deviation dystonia during a peak dose of levodopa, which improved after medication reduction and onabotulinum toxin A injection of 40 U into each lateral pterygoid and 7.5 U into each submental muscle (Pfeiffer and LeDoux, 2015). In another PD patient with jaw-opening dystonia, a 40% improvement was noted after BoNT was injected into lateral pterygoids (Tee et al., 2019). The use of BoNT for levodopa-related dystonia is based on anecdotal case reports and our own experience. We have found that BoNT injections into the affected muscles, particularly those involved in wearing off-foot dystonia, are very effective in most patients. It is best for these conditions to be treated by movement disorder-trained neurologists who have excellent understanding and experience in BoNT use.
Orofacial dyskinesia, often in the form of oromandibular dystonia (discussed above), raises concern for MSA (Onder and Comoglu, 2023). In a retrospective chart review of 83 patients with PSP, 3 patients with levodopa-induced dyskinesias were identified (1 blepharospasm, 1 jaw closure dystonia, and 1 limb dystonia), testifying to the rare occurrence of this complication in patients with PSP (Barclay and Lang, 1997). This is also suggested by rare case reports of oromandibular dystonia (Tan et al., 2003; Modreanu et al., 2018), facial dystonia (Chung and Kim, 2012), and cranial dystonia (Onder and Comoglu, 2023) in PSP that resolved after discontinuation of levodopa.
4 Conclusion
BoNT usage is expanding across many fields of medicine and beyond. Isolated dystonia continues to be one of the most common indications for BoNT treatment, but BoNT is increasingly used in patients with combined and complex dystonia in the setting of PD and other parkinsonian disorders. Although most of these forms of dystonia are not yet supported by randomized controlled clinical trials, their improvement with BoNT is becoming well established. BoNT is also used for many other PD-related symptoms, such as tremors, sialorrhea, dyskinesia, urinary symptoms, and others. Patients receiving BoNT in multiple locations should have the injections administered on the same day, and the total dose of BoNT should be kept below 600 units to reduce the risk of generalized weakness or immunogenicity.
Author contributions
CA: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. JJ: Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The authors received funding to publish this article from Merz Therapeutics GmbH.
Conflict of interest
JJ has training or research grants from Abbvie Inc.; Dystonia Coalition; Merz Pharmaceuticals; and Revance Therapeutics Inc. He has served as a consultant for Abbvie Inc.; Aeon Biopharma; Neurocrine; Revance Therapeutics; and Teva Pharmaceutical Industries Ltd. JJ has received royalties from Cambridge; Elsevier; MedLink Neurology; Lippincott Williams and Wilkins; UpToDate; Wiley Blackwell and is a member of the following editorial boards: Expert Review of Neurotherapeutics; MedLink Neurology in Clinical Practice; Therapeutic Advances in Neurological Disorders; Neurotherapeutics; Toxins; Tremor and Other Hyperkinetic Movements; and Journal of Parkinson’s Disease.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Agarwal, P. A. (2019). Severe jaw‐opening dystonia as an unusual manifestation of levodopa‐related wearing‐off in Parkinson's disease, and successful treatment with botulinum toxin injection. Mov. Disord. Clin. Pract. 6, 500–501. doi: 10.1002/mdc3.12782
Albanese, A., Bhatia, K., Bressman, S. B., Delong, M. R., Fahn, S., Fung, V. S. C., et al. (2013). Phenomenology and classification of dystonia: a consensus update. Mov. Disord. 28, 863–873. doi: 10.1002/mds.25475
Albanese, A., Bhatia, K. P., Cardoso, F., Comella, C., Defazio, G., Fung, V. S. C., et al. (2023). Isolated cervical dystonia: diagnosis and classification. Mov. Disord. 38, 1367–1378. doi: 10.1002/mds.29387
Anandan, C., and Jankovic, J. (2023). Botulinum toxin treatment in parkinsonism. J. Neurol. Sci. 456:122810. doi: 10.1016/j.jns.2023.122810
Artusi, C. A., Bortolani, S., Merola, A., Zibetti, M., Busso, M., De Mercanti, S., et al. (2019). Botulinum toxin for Pisa syndrome: an MRI-, ultrasound- and electromyography-guided pilot study. Parkinsonism Relat. Disord. 62, 231–235. doi: 10.1016/j.parkreldis.2018.11.003
Azher, S. N., and Jankovic, J. (2005). Camptocormia. Neurology 65, 355–359. doi: 10.1212/01.wnl.0000171857.09079.9f
Barclay, C. L., and Lang, A. E. (1997). Dystonia in progressive supranuclear palsy. J. Neurol. Neurosurg. Psychiatry 62, 352–356. doi: 10.1136/jnnp.62.4.352
Bonanni, L., Thomas, A., Varanese, S., Scorrano, V., and Onofrj, M. (2007). Botulinum toxin treatment of lateral axial dystonia in parkinsonism. Mov. Disord. 22, 2097–2103. doi: 10.1002/mds.21694
Cardoso, F. (2018). Botulinum toxin in parkinsonism: the when, how, and which for botulinum toxin injections. Toxicon 147, 107–110. doi: 10.1016/j.toxicon.2017.08.018
Chung, E. J., and Kim, S. J. (2012). Levodopa-induced facial dystonia in a case of progressive Supranuclear palsy. J. Mov. Disord. 5, 28–32. doi: 10.14802/jmd.12008
Colosimo, C., and Salvatori, F. M. (2009). Injection of the iliopsoas muscle with botulinum toxin in camptocormia. Mov. Disord. 24, 316–317. doi: 10.1002/mds.22249
Cooper, I. S. (1972). Levodopa-induced dystonia. The Lancet. 2, 1317–1318. doi: 10.1016/s0140-6736(72)92694-3
Cordivari, C., Misra, P. V., Catania, S., and Less, A. J. (2001). Treatment of dystonic clenched fist with botulinum toxin. Mov. Disord. 16, 907–913. doi: 10.1002/mds.1186
Defazio, G., Lepore, V., Lamberti, P., Livrea, P., and Ferrari, E. (1990). Botulinum a toxin treatment for eyelid spasm, spasmodic torticollis and apraxia of eyelid opening. Ital. J. Neurol. Sci. 11, 275–280. doi: 10.1007/BF02333858
Fietzek, U. M., Schroeteler, F. E., and Ceballos-Baumann, A. O. (2009). Goal attainment after treatment of parkinsonian camptocormia with botulinum toxin. Mov. Disord. 24, 2027–2028. doi: 10.1002/mds.22676
Giladi, N. I. R., Meer, J., and Honigman, S. (1994). The use of botulinum toxin to treat "striatal" toes. J. Neurol. Neurosurg. Psychiatry 57:659. doi: 10.1136/jnnp.57.5.659
Gupta, A. D., Tucker, G., Koblar, S., Visvanathan, R., and Cameron, I. D. (2018). Spatiotemporal gait analysis and lower limb functioning in foot dystonia treated with botulinum toxin. Toxins (Basel) 10, 1–9. doi: 10.3390/toxins10120532
Gupta, A. D., and Visvanathan, R. (2016). Botulinum toxin for foot dystonia in patients with Parkinson’s disease having deep brain stimulation: a case series and a pilot study. J. Rehabil. Med. 48, 559–562. doi: 10.2340/16501977-2094
Hammoud, N, and Jankovic, J. (2022). Botulinum Toxin in the Treatment of Cervical Dystonia: Evidence-Based Review. Dystonia. Inaugural Issue of Dystonia. doi: 10.3389/dyst.2022.10655
Jabbari, B., and Comtesse, S. M. (2023). Botulinum toxin treatment of motor disorders in Parkinson disease—a systematic review. Toxins (Basel) 15:15. doi: 10.3390/toxins15020081
Jameson, H. D. (1970). Pyridoxine for levodopa-induced dystonia. JAMA: The Journal of the American Medical Association. 211:1700.
Jankovic, J. (1996). Pretarsal injection of botulinum toxin for blepharospasm and apraxia of eyelid opening. J. Neurol. Neurosurg. Psychiatry 60:704. doi: 10.1136/jnnp.60.6.704
Jankovic, J. (2009). Disease-oriented approach to botulinum toxin use. Toxicon 54, 614–623. doi: 10.1016/j.toxicon.2008.11.013
Jocson, A., and Lew, M. (2019). Use of botulinum toxin in Parkinson's disease. Parkinsonism Relat. Disord. 59, 57–64. doi: 10.1016/j.parkreldis.2018.12.002
Jost, W. H. (2021). Use of botulinum neurotoxin in parkinson's disease: a critical appraisal. Toxins (Basel) :87:13. doi: 10.3390/toxins13020087
Kurtis, M. M., Floyd, A. G., Yu, Q. P., and Pullman, S. L. (2008). High doses of botulinum toxin effectively treat disabling up-going toe. J. Neurol. Sci. 264, 118–120. doi: 10.1016/j.jns.2007.08.013
Lapostolle, A., Houot, M., Mongin, M., and Degos, B. (2022). Comparison of Botulinum neurotoxin efficiency in dystonia associated with Parkinson’s disease and atypical parkinsonism: a retrospective study with a self-reported improvement scale. J. Neurol. 269, 6021–6028. doi: 10.1007/s00415-022-11280-y
Lepore, V., Defazio, G., Acquistapace, D., Melpignano, C., Pomes, L., Lamberti, P., et al. (1995). Botulinum a toxin for the so‐called apraxia of lid opening. Mov. Disord. 10, 525–526. doi: 10.1002/mds.870100425
Lindholm, B., Beckman, A., Duzynski, W., and Ekvall Hansson, E. (2017). Outcome on balance and gait following botulinum toxin treatment for striatal foot in Parkinson's disease. Mov. Disord. Clin. Pract. 4, 309–315. doi: 10.1002/mdc3.12411
Margolesky, J., Feldman, M., Marmol, S., Shpiner, D. S., Luca, C., Moore, H. P., et al. (2024). Blepharoclonus in parkinsonism. Neurol. Clin. Pract. 14:14. doi: 10.1212/CPJ.0000000000200240
Marsili, L., and Truong, D. D. (2020). Orofacial dystonia and associated bulbar symptoms in multiple system atrophy: a blinded video analysis. J. Neurol. Sci. 417:116995. doi: 10.1016/j.jns.2020.116995
Martinez-Ramirez, D., Giugni, J. C., Hastings, E., Shukla, A. W., Malaty, I. A., Okun, M. S., et al. (2014). Comparable botulinum toxin outcomes between primary and secondary Blepharospasm: a retrospective analysis. Tremor Other Hyperkinet. Mov. (N.Y.) 4:286. doi: 10.5334/tohm.186
Matar, E., and Bhatia, K. (2023). Dystonia and Parkinson’s disease: do they have a shared biology? Int. Rev. Neurobiol. 169, 347–411. doi: 10.1016/bs.irn.2023.05.001
Minervini, G., Franco, R., Marrapodi, M. M., Ronsivalle, V., Shapira, I., and Cicciù, M. (2023). Prevalence of temporomandibular disorders in subjects affected by Parkinson disease: a systematic review and metanalysis. J. Oral Rehabil. 50, 877–885. doi: 10.1111/joor.13496
Modreanu, R., Özdemir, G., Buhmann, C., and Hauptmann, B. (2018). Levodopa-induced dystonia in a patient with possible progressive supranuclear palsy with progressive gait freezing. J. Neurol. Sci. 388, 139–140. doi: 10.1016/j.jns.2018.03.023
Ni, P., Xu, Y., Wang, L., Cao, J., Luo, W., Zhang, Q., et al. (2023). Evaluation of therapeutic benefits of botulinum toxin for foot dystonia associated with Parkinson’s disease. Toxicon 107587. doi: 10.1016/j.toxicon.2023.107587
Onder, H., and Comoglu, S. (2023). Levodopa‐induced jaw and facial dystonia in a case of progressive Supranuclear palsy with Blepharospasm. Mov. Disord. Clin. Pract. 10, 1806–1808. doi: 10.1002/mdc3.13881
Ondo, W. G., Simmons, J. H., Shahid, M. H., Hashem, V., Hunter, C., and Jankovic, J. (2018). Onabotulinum toxin-a injections for sleep bruxism: a double-blind, placebo-controlled study. Neurology 90, e559–e564. doi: 10.1212/WNL.0000000000004951
Pacchetti, C., Albani, G., Martignoni, E., Godi, L., Alfonsi, E., and Nappi, G. (1995). “Off” painful dystonia in Parkinson's disease treated with botulinum toxin. Mov. Disord. 10, 333–336. doi: 10.1002/mds.870100317
Patterson, A., Almeida, L., Hess, C. W., Martinez-Ramirez, D., Okun, M. S., Rodriguez, R. L., et al. (2016). Occurrence of dysphagia following botulinum toxin injection in parkinsonism-related cervical dystonia: a retrospective study. Tremor Other Hyperkinet Mov 6:6. doi: 10.5334/tohm.285
Pfeiffer, R. F., and LeDoux, M. S. (2015). Levodopa-induced lateral jaw deviation dystonia. Parkinsonism Relat. Disord. 21:808. doi: 10.1016/j.parkreldis.2015.02.012
Piccione, F., Mancini, E., Tonin, P., and Bizzarini, M. (1997). Botulinum toxin treatment of apraxia of eyelid opening in progressive supranuclear palsy: report of two cases. Arch. Phys. Med. Rehabil. 78, 525–529. doi: 10.1016/S0003-9993(97)90169-6
Rieu, I., Degos, B., Castelnovo, G., Vial, C., Durand, E., Pereira, B., et al. (2018). Incobotulinum toxin a in Parkinson's disease with foot dystonia: a double blind randomized trial. Parkinsonism Relat. Disord. 46, 9–15. doi: 10.1016/j.parkreldis.2017.10.009
Romano, M., Bagnato, S., Altavista, M. C., Avanzino, L., Belvisi, D., Bologna, M., et al. (2022). Diagnostic and therapeutic recommendations in adult dystonia: a joint document by the Italian Society of Neurology, the Italian academy for the study of Parkinson’s disease and movement disorders, and the Italian network on botulinum toxin. Neurol. Sci. 43, 6929–6945. doi: 10.1007/s10072-022-06424-x
Rosales, R. L., Ng, A. R., Santos, M. M. D. D., and Fernandez, H. H. (2011). The broadening application of Chemodenervation in X-linked dystonia-parkinsonism (part II): an open-label experience with botulinum toxin-a (Dysport®) injections for Oromandibular, lingual, and truncal-axial Dystonias. Int. J. Neurosci. 121, 44–56. doi: 10.3109/00207454.2011.558260
Sachdev, A., Costello, D., and Madge, S. (2019). Botulinum toxin-B injection into the lacrimal gland and posterior cricoarytenoid muscle for the treatment of epiphora and abductor spasmodic dysphonia secondary to Parkinson’s disease. Orbit (London) 38, 248–251. doi: 10.1080/01676830.2018.1490443
Santamato, A., Ranieri, M., Panza, F., Zoccolella, S., Frisardi, V., Solfrizzi, V., et al. (2010). Botulinum toxin type a and a rehabilitation program in the treatment of Pisa syndrome in Parkinson’s disease. J. Neurol. 257, 139–141. doi: 10.1007/s00415-009-5310-4
Simonyan, K., Barkmeier-Kraemer, J., Blitzer, A., Hallett, M., Houde, J. F., Jacobson Kimberley, T., et al. (2021). Laryngeal dystonia. Neurology 96, 989–1001. doi: 10.1212/WNL.0000000000011922
Tan, E. K., Chan, L. L., and Wong, M. C. (2003). Levodopa-induced oromandibular dystonia in progressive supranuclear palsy. Clin. Neurol. Neurosurg. 105, 132–134. doi: 10.1016/S0303-8467(02)00128-2
Tassorelli, C., De Icco, R., Alfonsi, E., Bartolo, M., Serrao, M., Avenali, M., et al. (2014). Botulinum toxin type a potentiates the effect of neuromotor rehabilitation of Pisa syndrome in Parkinson disease: a placebo controlled study. Parkinsonism Relat. Disord. 20, 1140–1144. doi: 10.1016/j.parkreldis.2014.07.015
Tee, T. Y., Khoo, C. S., and Norlinah, M. I. (2019). Prominent Oromandibular dystonia as levodopa‐induced dyskinesia in idiopathic Parkinson's disease. Mov. Disord. Clin. Pract. 6, 330–331. doi: 10.1002/mdc3.12759
Todo, H., Yamasaki, H., Ogawa, G., Nishida, K., Futamura, N., and Funakawa, I. (2018). Injection of Onabotulinum toxin a into the bilateral external oblique muscle attenuated Camptocormia: a prospective open-label study in six patients with Parkinson’s disease. Neurol. Ther. 7, 365–371. doi: 10.1007/s40120-018-0108-x
Truong, D. D., and Bhidayasiri, R. (2006). Botulinum toxin therapy of laryngeal muscle hyperactivity syndromes: comparing different botulinum toxin preparations. Eur. J. Neurol. 13, 36–41. doi: 10.1111/j.1468-1331.2006.01443.x
Vanek, Z., and Jankovic, J. (2001). Dystonia in corticobasal degeneration. Mov. Disord. 16, 252–257. doi: 10.1002/mds.1038
Verhoeff, M. C., Koutris, M., Berendse, H. W., Van Dijk, K. D., and Lobbezoo, F. (2022). Parkinson’s disease, temporomandibular disorder pain and bruxism and its clinical consequences: a protocol of a single-Centre observational outpatient study. BMJ Open 12:e052329. doi: 10.1136/bmjopen-2021-052329
von Coelln, R., Raible, A., Gasser, T., and Asmus, F. (2008). Ultrasound‐guided injection of the iliopsoas muscle with botulinum toxin in camptocormia. Mov. Disord. 23, 889–892. doi: 10.1002/mds.21967
Wijemanne, S., and Jankovic, J. (2019). Hand, foot, and spine deformities in parkinsonian disorders. J. Neural Transm. 126, 253–264. doi: 10.1007/s00702-019-01986-1
Yoon, W. T., Chung, E. J., Lee, S. H., Kim, B. J., and Lee, W. Y. (2005). Clinical analysis of Blepharospasm and apraxia of eyelid opening in patients with parkinsonism. J. Clin. Neurol. 1, 159–165. doi: 10.3988/jcn.2005.1.2.159
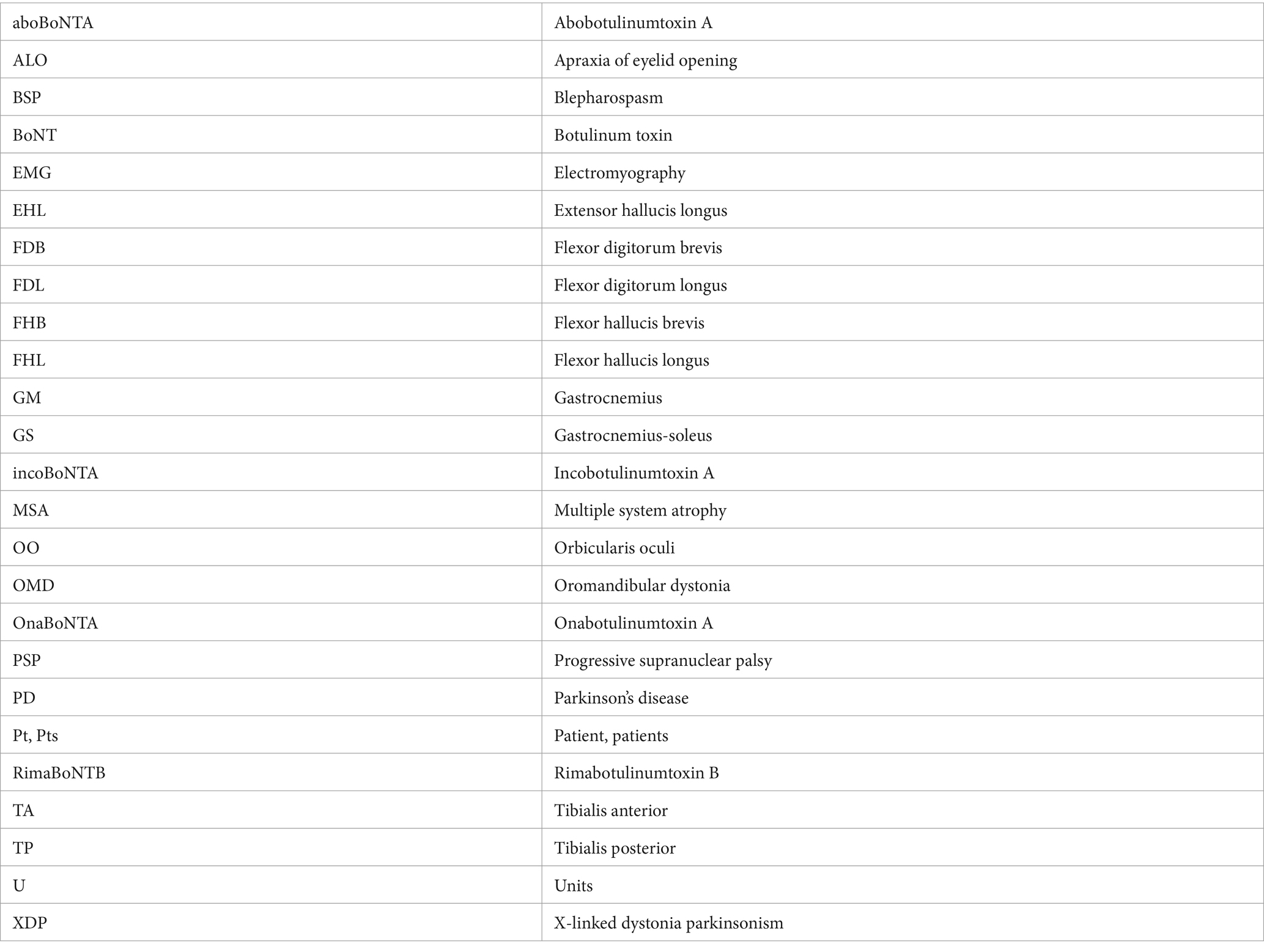
Glossary
Keywords: dystonia, Parkinson’s disease, botulinum toxin, blepharospasm, cervical dystonia
Citation: Anandan C and Jankovic J (2024) Use of botulinum toxin in the management of dystonia in Parkinson’s disease. Front. Neurosci. 18:1371601. doi: 10.3389/fnins.2024.1371601
Edited by:
Nicola Modugno, Mediterranean Neurological Institute Neuromed (IRCCS), ItalyReviewed by:
Philippe Picaut, AlgoTherapeutix, FranceMonika Rudzinska-Bar, Andrzej Frycz Modrzewski Krakow University, Poland
Copyright © 2024 Anandan and Jankovic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph Jankovic, am9zZXBoakBiY20uZWR1
 Charenya Anandan
Charenya Anandan Joseph Jankovic
Joseph Jankovic