Turner syndrome (TS), a chronic childhood disease, requires growth hormone (GH) treatment for short stature in pediatrics and sex hormone replacement therapy (HRT) in the adult health-care setting with transition during adolescence managed by gynecologists or endocrinologists (1). However, many women with TS are reported to be receiving inadequate health care. Only 24 of 39 (63%) TS patients received regular follow-up in an Australian study (2), and 13 of 102 were lost to follow-up in a Belgian study (3). Thus, the current management of transition of TS patients seems to be inadequate. This is because there are limited numbers of gynecologists or endocrinologists who are familiar with adult TS, and a reliable management plan for TS during transition has not yet been fully established.
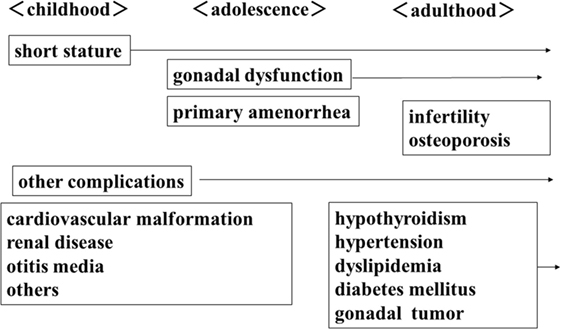
Turner syndrome women with complete or partial deletion of an X chromosome will develop various complications in each life stage (Figure 1). In addition to short stature, cardiovascular disease, kidney disease, and otitis media are often observed in childhood. GH therapy is performed for short stature in childhood and in adolescence they require HRT to acquire secondary sexual characteristics due to ovarian dysfunction. In adulthood, ovarian dysfunction causes infertility and osteoporosis. Endocrine/metabolic abnormalities, such as thyroid dysfunction, impaired glucose tolerance, hypertension, dyslipidemia, and gonadal tumors due to Y chromosome components are also observed. Therefore, all health problems that present during childhood should be followed-up in later life.
In our department, health management of TS adults is performed in Women’s Health Care Clinic by gynecologists who are familiar with the above conditions. Women’s health problems, due to the female-specific endocrine environment, change throughout every life stage (4). The salient points for TS health management are (1) commencement of HRT for ovarian dysfunction, (2) management of childhood onset complications, and (3) screening for complications that may develop in adulthood. At every visit, blood pressure and body weight were measured. Blood liver function, renal function, glucose tolerance, lipids, thyroid function, and urine analysis were measured once a year. Bone mineral density, ultrasound measurement of uterine size, and aortic MRI were performed at first visit. When a complication developed in a patient, she was referred to the relevant health-care professionals. Gawlik and Malecka-Tendera (5) have also demonstrated that all medical problems that present during childhood should be followed in adult life, with particular importance assigned to screening for hypertension, diabetes mellitus, dyslipidaemia, and osteoporosis.
It has been recommended in the guidelines (1) that transition care should be continued up to 18 years of age before transfer to adult health care, in which a gynecologist who is familiar with the unique problems of TS adults, such as ovarian dysfunction and infertility, is involved. HRT is recommended to start at 12–15 years old. However, in our department, the age at completion of GH therapy, in patients referred from pediatrics, was 17.7 ± 2.1 years old, the age of commencement of HRT was 17.9 ± 2.2 years of age, and the age at the time of transition was 23.4 ± 4.1 years of age. On the other hand, in survivors of childhood cancer, the starting age for HRT was 14.1 ± 1.2 years of age and the age of transition was 14.5 ± 1.9 years old (6). Our data shows that transition was not fully completed, although HRT was initiated and GH therapy had been completed. The transition from pediatrics was later than that recommended because of a delay in the end of GH therapy and initiation of HRT.
Since there is a lifetime increased risk of complications in TS women, the needs for a systematic and holistic approach in the provision of health care and the establishment of an optimal model of transition to adult health care in TS women are essential (7). A pediatric gynecology clinic was opened in Kanagawa Children’s Medical Center for the management of HRT in childhood and to ensure a smooth transition to our department from the time of GH therapy completion to starting HRT.
We conclude that in the future, gynecologists should be more involved in coordinating the initiation of HRT in order to create a smoother transition from pediatrics to adult health care for the management of women with TS.
Author Contributions
The author confirms being the sole contributor of this work and approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Bondy CA; Turner Syndrome Study Group. Care of girls and women with Turner syndrome: a guideline of the Turner Syndrome Study Group. J Clin Endocrinol Metab (2007) 92:10–25. doi:10.1210/jc.2006-1374
2. Pedreira CC, Hameed R, Kanumakala S, Zacharin M. Health-care problems of Turner syndrome in the adult woman: a cross sectional study of a Victorian cohort and a case for transition. Intern Med J (2006) 36:54–7. doi:10.1111/j.1445-5994.2005.00990.x
3. Verlinde F, Massa G, Lagrou K, Froidecoeur C, Bourguignon JP, Craen M, et al. Health and psychosocial status of patients with Turner syndrome after transition to adulthood: the Belgian experience. Horm Res (2004) 62:161–7. doi:10.1159/000080099
4. Sakakibara H, Yoshida H, Takei M, Katsuhata Y, Koyama M, Nagata T, et al. Health management of adults with Turner syndrome: an attempt at multidisciplinary medical care by gynecologists in cooperation with specialists from other fields. J Obstet Gynaecol Res (2011) 37:836–42. doi:10.1111/j.1447-0756.2010.01448.x
5. Gawlik A, Malecka-Tendera E. Transition in endocrinology; treatment of Turner’s syndrome during transition. Eur J Endocrinol (2013) 170:R57–74. doi:10.1530/EJE-13-0900
6. Ushihio E, Nagata T, Nakashima I, Tsuburai T, Sato M, Takei M, et al. Study on the starting age of estrogen therapy for the patients with Turner syndrome and their transition age from pediatrics to adult health care. Adolescentology (2016) 34:411–6.
Keywords: Turner syndrome, transition, hormone replacement therapy, health-care surveys, adolescent
Citation: Sakakibara H (2017) Transition of Women with Turner Syndrome from Pediatrics to Adult Health Care: Current Situation and Associated Problems. Front. Pediatr. 5:28. doi: 10.3389/fped.2017.00028
Received: 28 July 2016; Accepted: 01 February 2017;
Published: 17 February 2017
Edited by:
Yuko Ishizaki, Kansai Medical University, JapanReviewed by:
Kenichi Kashimada, Tokyo Medical and Dental University, JapanCopyright: © 2017 Sakakibara. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hideya Sakakibara, sakakih@yokohama-cu.ac.jp
 Hideya Sakakibara
Hideya Sakakibara