- 1Department of Community Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 2Center for Safety, Health and Environment of Chulalongkorn University, Bangkok, Thailand
- 3Department of Rehabilitation Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 4School of Health Sciences Research, Research Institute for Health Sciences, Chiang Mai University, Chiang Mai, Thailand
Objective: This cross-sectional study aimed to examine farmers' knowledge, awareness, practices regarding pesticide use, and prevalence of health symptoms related to pesticides exposure among farmers who applied organophosphates (OP) and pyrethroids (PY).
Methods: Data regarding demographic variables and health symptoms pertinent to pesticide use was collected from 67 farmers who applied OP and 50 farmers who applied PY using interviews from January to March 2021.
Results: The farmers who applied OP had lower knowledge, awareness, and prevention practices regarding pesticide use than those who applied PY. After adjustment of covariate variables, the farmers who applied OP had a significantly higher prevalence of respiratory conditions (OR = 8.29 for chest pain, OR = 6.98 for chest tightness, OR = 27.54 for dry throat, and OR = 5.91 for cough), neurological symptoms (OR = 10.62 for fatigue and OR = 6.76 for paresthesia), and neurobehavioral symptoms (OR = 13.84 for poor concentration, OR = 3.75 for short term memory, and OR = 8.99 for insomnia) related to pesticide exposure than those who applied PY.
Conclusion: Our findings suggest that OP had a more adverse effect on human health than PY, resulting in a higher prevalence of pesticide-related symptoms. The outcomes of this study have the benefit of providing vital information for all stakeholders with regard to the implementation of safe practices in the utilization of personal protective equipment (PPE) and pesticide use in a health intervention and health promotion program.
Introduction
Thailand's government has made efforts to enhance crop yields in recent decades (1). As a result, the importing of pesticides has steadily increased year on year to facilitate control of pests, including insects, weeds, and fungi (2, 3). The most commonly imported insecticide classes were organophosphates (OP) such as chlorpyrifos (1,723.02 tons) and pirimiphos-methyl (750.46 tons), followed by pyrethroids (PY) such as cypermethrin (675.52 tons) (1). The toxicity of both OP and PY can pollute the environment and pose a risk to animal and human health (4). Pesticides exposure may occur ingested, absorbed through the skin, or inhaled (5, 6). Most health concerns arise from farmers' exposure to pesticides via cutaneous and inhalation pathways when applying pesticides, whereas consumer ingestion of pesticide-contaminated food (7). Farmers may pose a higher health risk than consumers since they are routinely exposed to higher doses of pesticides (5, 8).
Pesticide exposure can have both acute and chronic health effects (5). The acute effects include blurred vision, vomiting, nausea, dizziness, cramp, numbness, and muscle weakness (8, 9). As regards chronic health effects, the evidence is inconsistent, and the mechanisms involved are unclear (7, 8). In several human studies, pesticides have been shown to be related to chronic adverse effects on the immune, neurological, respiratory, endocrine, and reproductive systems (7, 10–16). Symptoms indicating neurobehavioral, motor, and sensory dysfunction, have been reviewed in some symptom prevalence studies (11, 17–19).
Several studies indicate that OP has a negative impact on human health, nevertheless, the data pertinent to PY toxicity is inconsistent (20, 21). Organophosphate inhibits acetylcholinesterase leading to excessive activity at acetylcholine receptors. Pyrethroids act on sodium channels by delaying voltage-sensitive sodium channel closure (20). Even though PY are generally less hazardous than OP, poisoning with a high amount can be fatal (22). Some studies have shown that PY toxicity might have symptoms that are similar to organophosphate poisoning (20). Therefore, the impact of PY on human health is raising concern. Most previous studies on Thai farmers have been limited to reports of single pesticide exposure despite many farmers using a range of pesticides in the cultivation of multiple crops (2). To date, no studies comparing pesticide-related health problems among Thai farmers exposed to both OP and PY have been reported. Only one study has evaluated the effect of childhood exposure to OP and PY on neurobehavior, but results were not significant predictors of adverse neurobehavioral performance (23). They suggest that the impact of these pesticides might be dependent on the half-life of OP and PY (23). Therefore, the use of a questionnaire to assess the relationship between chronic health effects and pesticide exposure is warranted (23).
Previous studies provide evidence that perception influences the use of personal protective equipment (PPE) and pesticide safety practices (24). In reality, improper PPE and unsafe practices are frequently reported, information from some studies indicating factors affecting the use of PPE and pesticide safety practices are inadequate and inconsistent (24). Hence, understanding the reasons behind the knowledge, awareness, and practices regarding pesticide use is vital in order to facilitate the design of interventions to minimize exposure of pesticides among farmers.
To understand the extent of problem the prevalence of use of both OP and PY pesticides among Thai farmers is important. Therefore, the purpose of this study was to compare the knowledge, awareness, practices, and health symptoms associated with pesticide exposure in farmers who applied OP and PY in farms. The result of this study is useful to provide information for health surveillance systems and health intervention to raise safety awareness among farmers in the future.
Materials and Methods
Participants
This was a population-based cross-sectional study of farmers who were actively participating in farming production. Two subdistricts of the Chiang Dao district were chosen at random. Mueang Ngai and Thung Khao Phuang sub-districts, both in Chiang Dao district, Chiang Mai province, are shown in Figure 1. The socio-cultural contexts of all of these subdistricts were identical. The number of participants was decided by the number of pesticide-related hospitalizations in each subdistrict's health-promoting hospitals. Participants included farmers who used a single pesticide, such as OP or PY pesticides. The participants were 18 to 70 years old and had lived in the Mueang Ngai sub-district, or Thung Khao Phuang sub-district, Chiang Dao district, Chiang Mai province, northern Thailand, for at least 1 year. Farmers with underlying diseases including respiratory and cardiovascular disease, cancer, diabetes, or neurological problems were excluded. Those who met the inclusion criteria (n = 138) included 83 farmers who applied OP (67 males, 16 females) and 55 farmers who applied PY (28 males, 27 females). Of these 138 individuals, 67 farmers who applied OP [51 (76.1%) males, 16 (23.9%) females] and 50 farmers who applied PY [27 (54.0%) males, 23 (46.0%) females] agreed to volunteer as study subjects and signed a written consent form. Data were collected through interview forms from January to March 2021, which is the period when pesticides are applied on farms for pest control.
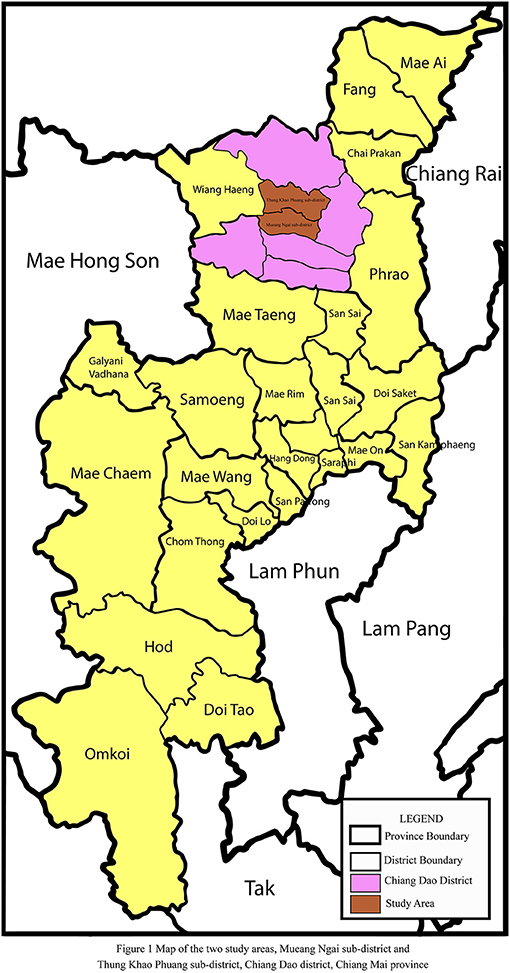
Figure 1. Map of the two study areas, Mueang Ngai sub-district and Thung Khao Phuang sub-district, Chiang Dao district, Chiang Mai province.
Interviews
The principal investigator trained all staff members before the participants were interviewed. The validated interview form was a structured questionnaire which was developed based on the manual for the Occupational Health Service Agricultural Health Clinics (Bureau of Occupational and Environmental Diseases, Center for Disease Control, 2015) and Department of Disease Control, Ministry of Public Health (MOPH) Thailand and from similar published studies (7, 11). Three experts in environmental and occupational health assessed the questionnaire's content validity, language suitability, and scoring criteria. The item-objective congruence index (IOC) was used to assess the content validity of questionnaires. The average IOC score of knowledge, awareness, practice regarding pesticide use, and health symptom related to pesticide exposure were 0.89, 0.93, 0.98, and 0.97 respectively. These results show that the questions are consistent with the objectives.
The questionnaire had five sections. The first section consisted of demographic details including age, education status, nationality, income, smoking status, alcohol drinking, and body mass index (BMI). The second section had five questions related to agricultural information including the number of years of farm work, frequency of pesticide use, working hours, type of sprayer, and the distance between farm and residence. The third section had 17 questions to assess knowledge and awareness regarding pesticide use. The fourth section included questions regarding practice, such as the use of PPE during pesticide application and pesticide exposure prevention. The responses were recorded as “yes” or “no” responses. A score of “1” was provided for each correct response, while a score of “0” was given for each incorrect response. In the fifth section, questions regarding health symptoms within 1 month of enrollment were asked. The questions were presented as 30 items in six sections focusing on: (1) respiratory tract symptoms (difficulty in breathing, chest pain, chest tightness, heart palpitation, dry throat, cough); (2) musculoskeletal symptoms (numbness, cramp, muscle weakness); (3) neurological symptoms (headache, dizziness, vomiting, fatigue, eye twitches, hand tremors, dysesthesia, paresthesia); (4) epithelial/mucosal surface symptoms (eye irritation, ulcer/blister, itchy, sweating); (5) neurobehavioral symptoms (poor concentration, short term memory, compulsion, depression, insomnia); (6) other symptoms (blurry vision, diarrhea, stomach ache, decreased sex drive).
Statistical Analysis
Data pertinent to demographic characteristics, knowledge, awareness, and practices regarding pesticide use were analyzed by using frequency, mean, median, standard deviation, range, and percentile (P25th-P75th). All parameters were tested for normality using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Comparison of demographic characteristics, agricultural information between farmers who applied OP and PY were performed using Chi-squared and independent sample t-tests. Due to the non-normal distribution of variables, the Mann-Whitney U test was used to compare agricultural information between farmers who applied OP and PY. Comparison of knowledge, awareness, and practices regarding pesticide use between farmers who applied OP and PY were performed using Chi-square. The odds ratios (OR) and 95% confidence intervals were calculated to assess symptoms related to pesticide exposure. The results were obtained from univariate analysis and multivariate logistic regression in a model adjusted for age, gender, nationality, body mass index, smoking status, alcohol consumption, pesticide group, frequency of pesticide use, the number of years of farm work, knowledge, awareness, and practice scores. p-values of < 0.05 were accepted as statistically significant.
Results
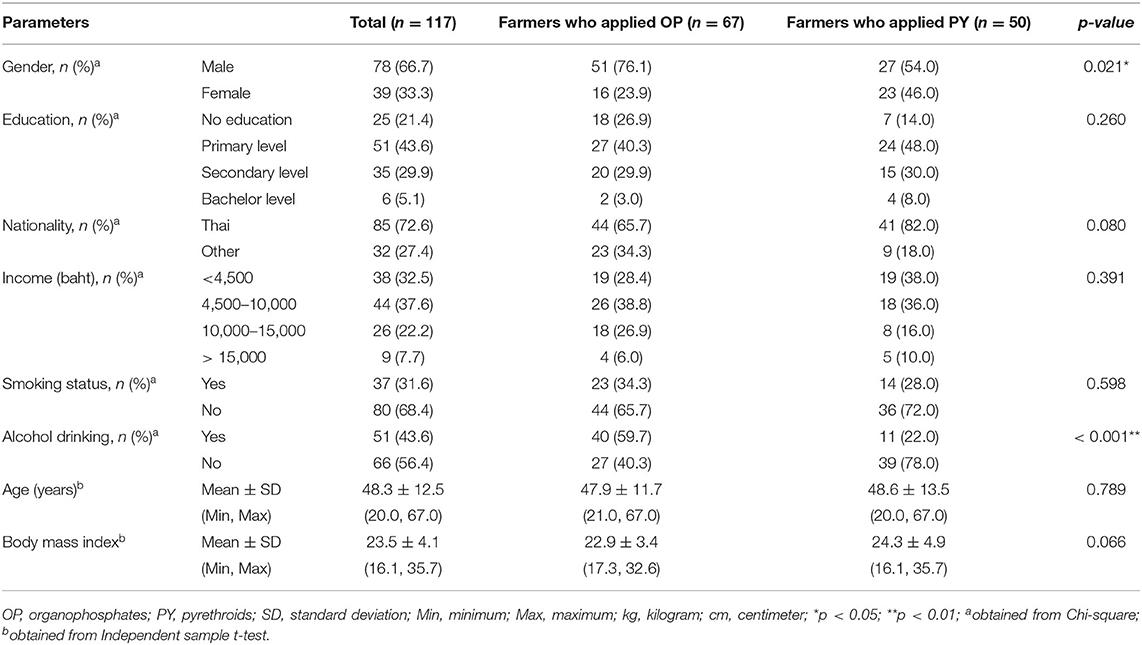
Table 1 shows the demographic characteristics among farmers who applied OP and PY. The majority of the farmers were male with a mean age of 48.3 ± 12.5 years. There were no statistical differences between the two groups in terms of education, nationality, income, smoking status, age, and BMI. However, there was a significantly higher number of men in the farmers who applied OP and a significantly higher level of alcohol use than in those who applied PY.
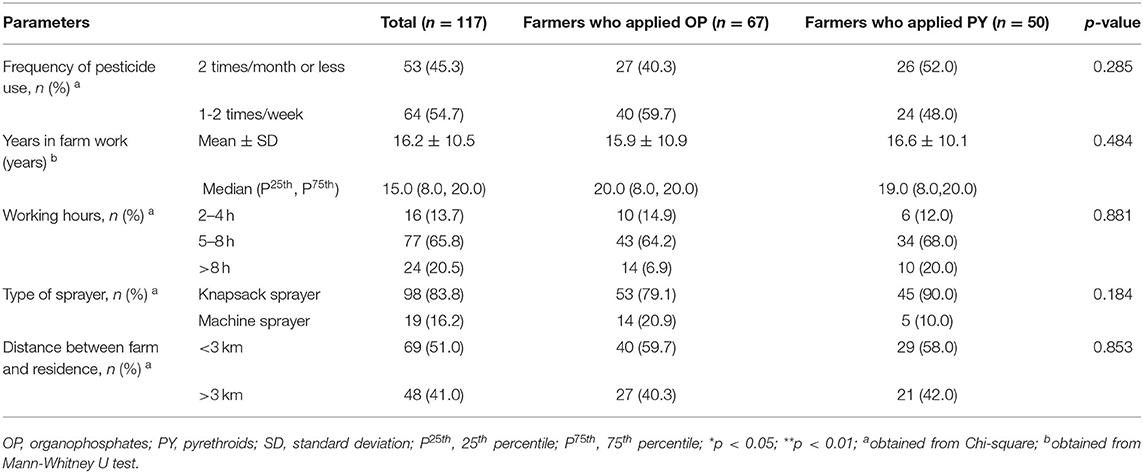
Table 2 presents the agricultural information among farmers who applied OP and PY. 54.7% of the farmers applied pesticides one to two times per week and had farm work experience of 16.2 ± 10.5 years. Most farmers had working hours of 5–8 h per day (65.8%), and use a knapsack sprayer (83.8%). There were no statistical differences regarding the agricultural information between the two groups of farmers who applied OP and PY.
The knowledge and awareness regarding pesticide use among farmers who applied OP and PY are presented in Table 3. The issues that the farmers who applied PY scored significantly higher knowledge than those who applied OP are as follows: route of entry of pesticide; mixing pesticide as described on the recommendations on the label; an adverse effect of pesticides on animal health and environment. The farmers who applied PY scored significantly higher awareness than those who applied OP are as follows: showering and changing the clothes after applying pesticides, using PPE, and not washing the spray tank in a river or waterway.
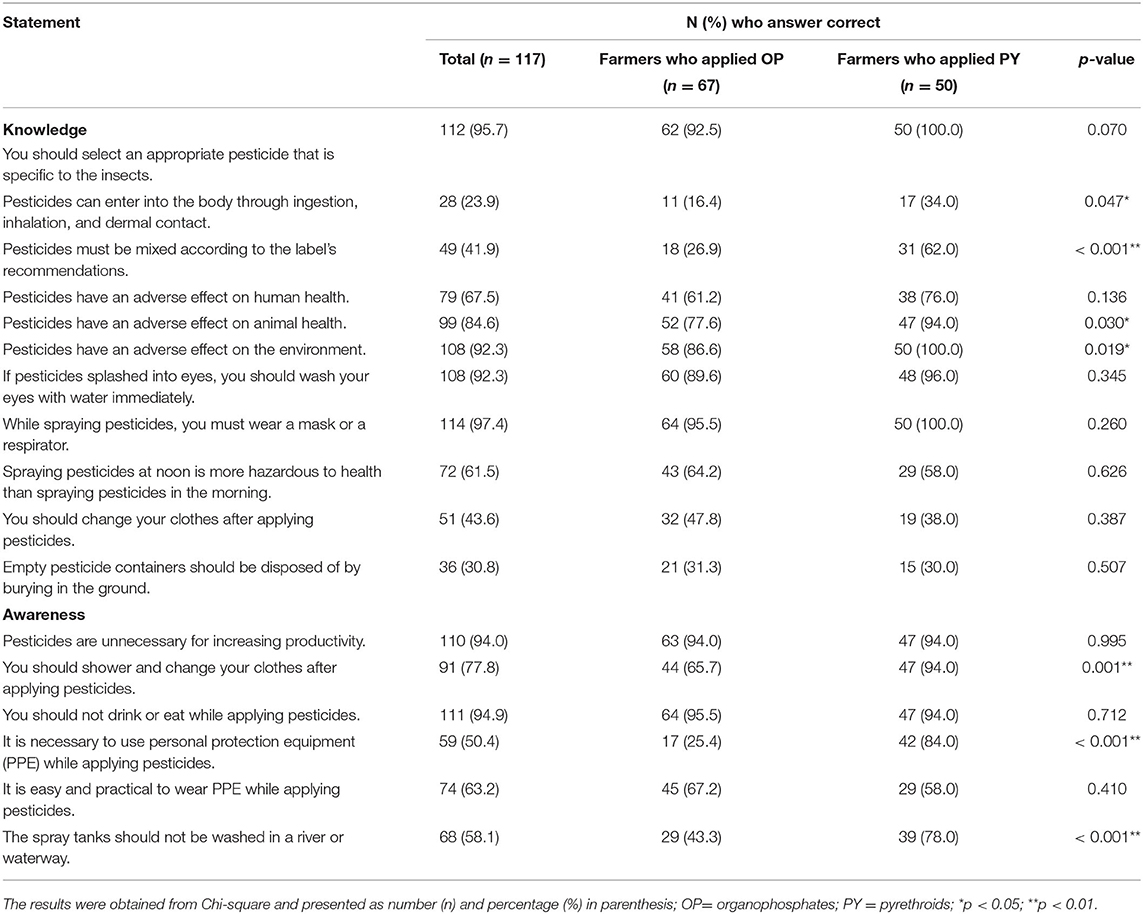
Table 3. Knowledge and awareness regarding pesticide use among farmers who applied OP and PY (n = 117).
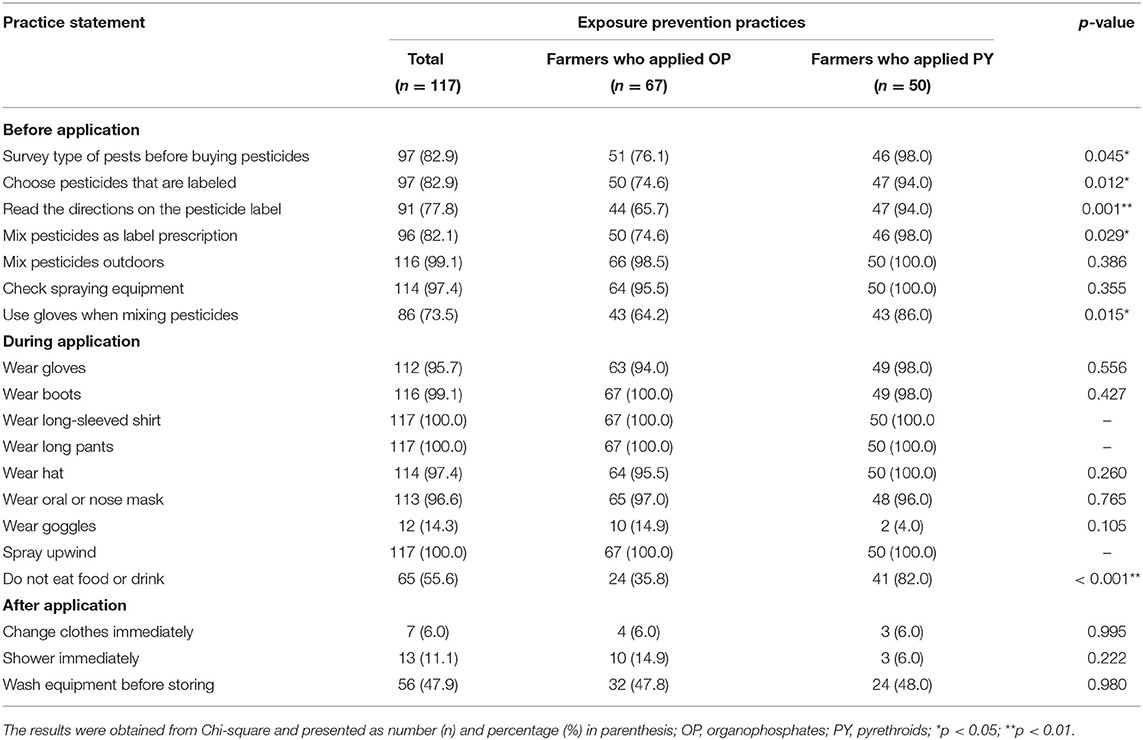
Table 4 shows the practices regarding pesticide use among farmers who applied OP and PY. The issues that the farmers who applied OP had lower significantly prevention practices in than those who applied PY are as follows: buying pesticides after survey; choosing pesticides that are labeled; reading the directions on the pesticides label; mixing pesticides as recommended on the label; using gloves when mixing pesticides; and not eating food and drinking water whilst working with pesticides.
Comparisons of the knowledge, awareness, and prevention practice scores regarding pesticide use among farmers who applied OP and PY are presented in Figure 2. The results show that farmers who applied OP had significantly lower knowledge, awareness, and practice scores than those who applied PY. The knowledge scores regarding pesticide use of the total cohort of farmers was 7.3 ± 1.5. For the farmers who applied OP and PY, the knowledge scores regarding pesticide use were 6.9 ± 1.4 and 7.9 ± 1.4, respectively. The awareness scores regarding pesticide use of the total cohort of farmers was 4.4 ± 1.1. For the farmers who applied OP and PY, the awareness scores regarding pesticide use were 3.9 ± 0.9 and 5.2 ± 0.9, respectively. The prevention practice score regarding pesticide use of the total cohort of farmers was 24.2 ± 3.5. For the farmers who applied OP and PY, the prevention practice scores regarding pesticide use were 23.2 ± 3.9 and 25.5 ± 2.5, respectively.
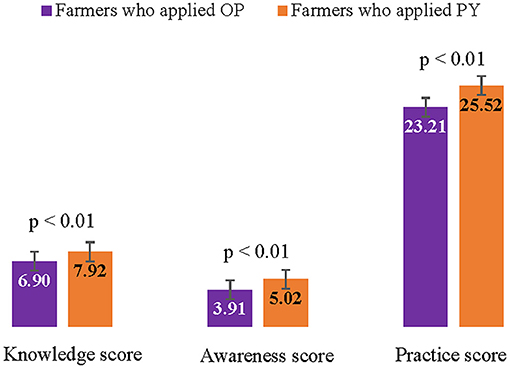
Figure 2. Comparison of knowledge, awareness, and prevention practice scores regarding pesticide use among farmers who applied OP and PY.
Table 5 presents the prevalence of health symptoms related to pesticide exposure among farmers who applied OP and PY. After adjusting for covariate variables, the farmers who applied OP had a significantly higher prevalence of health symptoms related to pesticide exposure than those who applied PY (OR = 8.29; 95% CI = 1.07–64.45 for chest pain, OR = 6.98; 95% CI = 1.18–40.58 for chest tightness, OR = 27.54; 95% CI = 2.83–268.42 for dry throat, OR = 5.91; 95% CI = 1.62-21.57 for cough, OR = 10.62; 95% CI = 1.88–59.93 for fatigue, OR = 6.76; 95% CI = 1.28–35.75 for paresthesia, OR = 13.84; 95% CI = 1.79–106.76 for poor concentration, OR = 3.75; 95% CI = 1.17–12.05 for short term memory, OR = 8.99; 95% CI = 2.58–31.26 for insomnia, OR = 5.10; 95% CI = 1.15–22.64 for blurry vision, and OR = 5.82; 95% CI = 1.54–21.99 for decreased sex drive). However, the results showed that the farmers who applied PY had a significantly higher prevalence of eye irritation (OR = 0.32; 95% CI = 0.10–0.96) and blisters (OR = 0.13; 95% CI = 0.03–0.62) than those who applied OP.
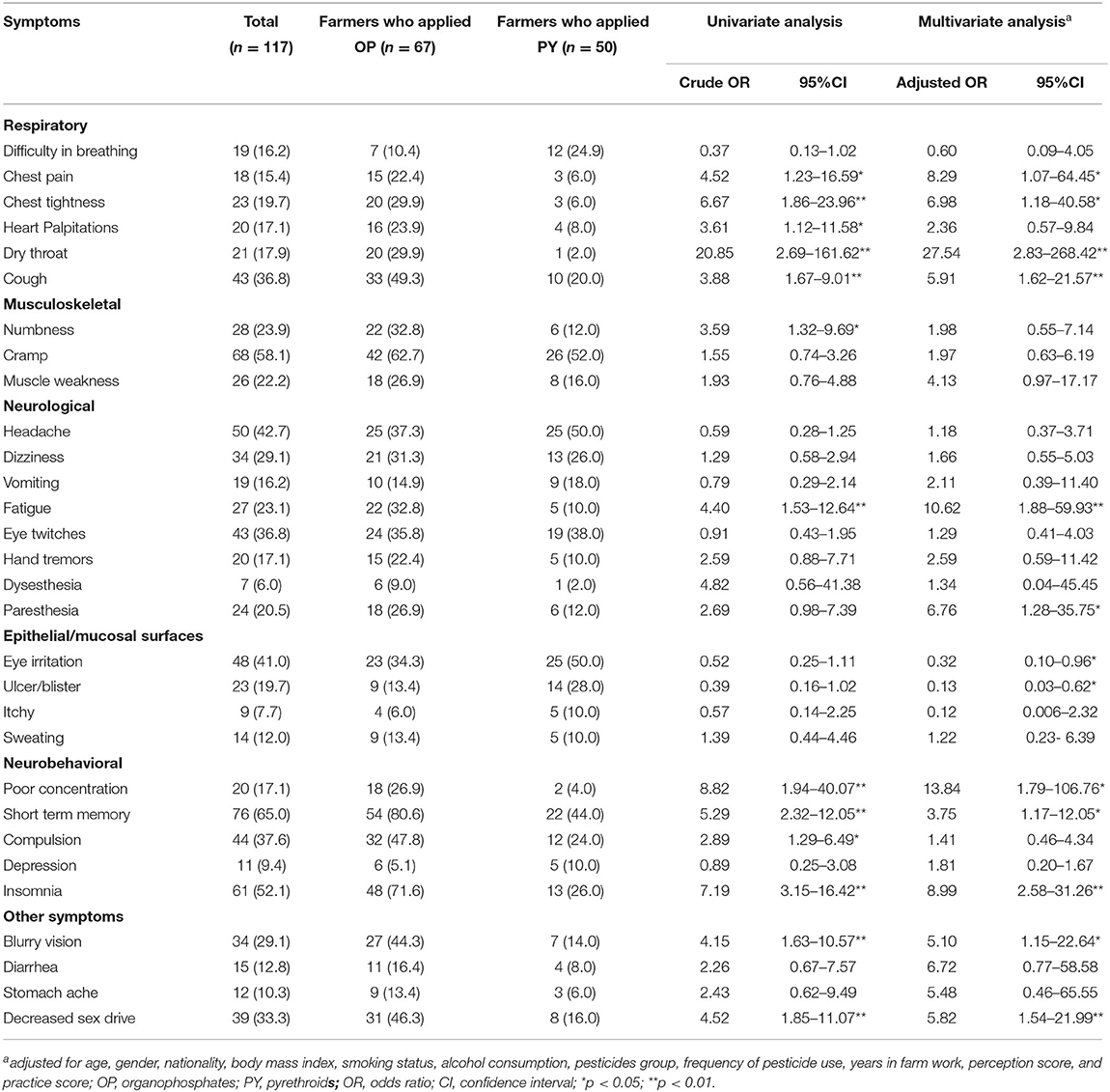
Table 5. Prevalence of health symptoms related to pesticide exposure among farmers who applied OP and PY (n = 117).
Discussion
Our study found that the farmers who applied OP had lower knowledge, awareness, and prevention practices regarding pesticide use than those who applied PY. It is possible that gender had an effect on knowledge, awareness, and prevention practice regarding pesticide use. In this study there were more female farmers in the PY group than in the OP group (46.0 and 23.9%, respectively). It has been postulated that females take fewer risks and have a higher knowledge and awareness of risk than males (24, 25). Therefore, females are more likely to engage in safety practices than males (25–28). In addition, female farmers are generally more concerned about health effects from pesticide exposure (24, 29). Consistent with previous findings, which showed that females wore long-sleeved shirts or jackets and took a shower immediately after spraying pesticides more than males (25, 30). On the other hand, males do not change out of their work clothes until bedtime and must attend to other farming activities after spraying (25, 30). These findings support the notion that risk knowledge, awareness, and the implementation of self-protective behaviors are linked. In addition, females have a different awareness of risk than males and engage in fewer risky behaviors (27). The first reason could be because of males on the farm played a larger role than females (30). As a result, males find it inconvenient to shower and change clothes immediately after spraying pesticides. The second reason could be due to their hygiene and lifestyle habits (30). Another explanation is that females received more information about pesticide exposure risks than males (25). Females may be more likely to adopt some integrated pest management (IPM) strategies than males and efforts to increase their participation in IPM training include biological control methods, bio-pesticides, organic farming, and other strategies. Female initiatives would be beneficial in terms of reducing pesticide exposure (24, 31, 32). Therefore, these findings suggest that gender could have had an effect on knowledge, awareness, and self-protective behavior in farmers.
Regarding the knowledge of pesticide use, our study found that the farmers had the lowest knowledge with regard to the entry route of pesticides (23.9%), followed by disposal empty of pesticide containers (30.8%) and mixing pesticides to the recommendations given on the label (41.9%). Most farmers perceived that pesticides could enter into the body only through inhalation resulting in a lack of protection from pesticide exposure through other routes (33, 34). Pesticides are commonly accepted to enter the body through skin absorption, ingestion, and inhalation, and farmers' knowledge of this needs to be raised (5, 6). The majority of farmers perceived that empty pesticide containers could be thrown away in agricultural land, trash, and river, and also be cleaned and reused. These findings agreed with several studies about misunderstanding regarding disposal of empty pesticide containers (35–39). These unsafe disposal practices are likely to contaminate the environment and pose a risk to both animal and human health (40). The data also indicated that farmers did not read the recommendations on the pesticide labels before mixing pesticides, and as a consequence pesticide were frequently inappropriately and unnecessarily used (7).
Concerning awareness of pesticide use, our study found that the farmers who had the lowest score of awareness were using PPE while applying pesticides (50.4%), followed by washing spray tanks in a river or waterway (58.1%) and wearing PPE while applying pesticides (63.2%). This finding was consistent with previous studies which found that farmers wore just partial PPE (39, 41). According to the reasons for not wearing protective equipment during pesticide handling, it is uncomfortable, expensive to buy, time-consuming to use, unavailable when needed, and unnecessary in each circumstance (5, 34, 39, 42). This finding agreed with several studies about unawareness of washing spray tanks in a river (35, 43). Most farmers stated they washed application equipment near or into irrigation canals (35). According to the findings of this study, indicating that there is a high risk of environmental contamination during that phase of pesticide handling.
Regarding practice of pesticide use, the lowest scoring practice was changing clothes immediately after pesticide application (6.0%), followed by showering immediately after pesticide application (11.1%) and wearing goggles during pesticide application (14.3%). These findings were consistent with previous studies which found that farmers did not change their clothes until they finished all of their work (44, 45). One possible explanation is that most farmers had a working period of 5–8 h or more than 8 h in their field and nearly half of them had a distance of more than 3 km between farm and residence. Therefore, it is impractical for farmers to shower and change clothes immediately after applying pesticides. With regard to PPE, only 14.3 % of farmers wore goggles, a finding consistent with a systematic review by Sapbamrer and Thammachai (46) which stated that farmers in Asia wore goggles for spraying pesticides 16.1% of the time (46).
A remarkable finding was that the farmers who applied OP had a significantly higher prevalence of health symptoms related to pesticide exposure than those who applied PY. Both OP and PY are toxic to humans (47). Organophosphate inhibits the enzyme acetylcholinesterase (AChE), which breaks down the neurotransmitter acetylcholine (48). Whereas, PY disrupts voltage-sensitive sodium channels to cause malfunctioning of nerve cell membranes (49). However, OP is more toxic to humans than PY due to OP toxicity being irreversible, the phosphorylation of the OP-serin bond, which inhibits AChE is a permanent change. Furthermore, OP is also rapidly absorbed through ingestion, inhalation, and dermal exposure (48). In contrast, PY has a lower rate of dermal absorption and is also rapidly metabolized to non-toxic metabolites (50, 51).
As regards respiratory symptoms, the adjusted prevalence of chest pain, chest tightness, dry throat, and cough in the farmers who applied OP indicated they were significantly higher than those who applied PY (OR = 8.29, 6.98, 27.54, and 5.91, respectively). These findings were consistent with the study by Chakrabory (52) that found respiratory symptoms have been reported in association with OP exposure, including chest tightness (OR = 3.26), sore throat or dry throat (OR = 1.76), and dry cough (OR = 2.83) (52). Furthermore, chest pain, dry throat, and cough have been found to be the most prevalent respiratory symptoms associated with OP exposure (53). OP affect the lungs due to increased acetylcholine, through peripheral muscarinic effects on the airway, nicotinic effects on the respiratory muscles, medulla center effects on the brain, and direct toxic effects on the alveolar-capillary membrane (6, 54). However, pulmonary toxicity of PY has not been studied in humans, despite a recent study suggesting a possible cardiovascular risk (55).
Concerning neurological symptoms, the farmers who applied OP had a significantly higher prevalence of fatigue and paresthesia than those who applied PY (OR = 10.62 and 6.76, respectively). These findings were consistent with the study by Farnham (18) that reported an association between pesticide poisonings and neurological symptoms such as paresthesia or tingling in hands or feet (OR = 3.23), dizziness (OR = 2.38), low energy (OR = 2.33), and tremor of the hands (OR = 3.50) (18). Long-term dermal exposure to OP may cause chronic adverse health effects such as paresthesia and organophosphate-induced delayed polyneuropathy (OPIDP) (56, 57). Symptoms are attributable to sensory effects such as paresthesia or tingling, numbness, and pain and motor affects including fatigue, weakness, and paralysis. It develops 2–3 weeks after the poisoning (57). PY exposure can also cause paresthesia especially following cutaneous exposure or intentional consumption (21, 58, 59). However, human toxicity concerning PY is rarely presented in the literature.
In the case of neurobehavioral symptoms, farmers who applied OP had significantly poorer concentration, short term memory, and insomnia than those who applied PY (OR = 13.84, 3.75, and 8.99, respectively). These findings support previous studies that found that organophosphate poisoning in workers had more psychological and affective problems, difficulty concentrating (OR = 2.07), trouble remembering things (OR = 2.54), and insomnia (OR = 2.53) (18, 60, 61). As a consequence of AChE inhibition, OP exposure causes brain hyperactivity and acetylcholine accumulation (62). These effects are the main causes of neurobehavioral and mood disorders (56, 63).
The result of this study is useful to provide information for health surveillance system and health intervention. However, some limitations should be concerned. Firstly, a cross-sectional study design might not clearly explain some causal relationships. Secondary, recall bias may have been reflected in the information of the farmers' behavior. Thirdly, the questionnaires were based on self-reporting potentially leading to a degree of bias in the data. Fourthly, a small sample size may not be representative of all study populations, resulting in statistical analysis with lower power. Fifthly, a control group of a worker who was not exposed to pesticides was not recruited to control the association between exposure and effect on the group of interest. Finally, biomarkers were not used to detect OP and PY exposure or other pesticide exposure. Further research should be conducted in longitudinal studies and biomarker analyses on pesticide health effects.
Conclusion
This study found that the farmers who applied OP had lower knowledge, awareness, and prevention practices regarding pesticide use than those who applied PY. In addition, farmers who applied OP had a significantly higher prevalence of respiratory, neurological, and neurobehavioral symptoms related to pesticide exposure than those who applied PY. Therefore, it can be concluded that OP had a more harmful impact on human health than PY, resulting in a higher prevalence of pesticide-related illnesses. To address these challenges, long-term training about information of pesticide hazard level should be done to raise awareness and permanently change farmers' behavior. Health professionals should be focused on more effective prevention and intervention programs for individuals, families, and the community. The findings of this study on pesticides' adverse effects are beneficial in motivating farmers to look for other ways to protect their crops. Adoption of biological and cultural practices, reduction of pesticide applications, and the use of reduced-risk pesticides are alternative ways. The policy by government should encourage farmers to use of biological control technology, bio-pesticides, organic farming, and other strategies to ensure long-term sustainability.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Chiang Mai University's Faculty of Medicine's Research Ethics in Humans (COM-2563-07707). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
RS, AJ, JR, ST, and SH: conceptualization. AJ, RS, JR, ST, SH, and KW: methodology. RS and AJ: validation, formal analysis, investigation, data curation, and funding acquisition. RS, ST, SH, JR: resources. AJ: Writing original draft preparation. RS: writing review and editing and project administration. RS, JR, ST, SH: supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research and innovation activity is funded by National Research Council of Thailand (NRCT) (Grant No. GSCMU(NRCT)/07/2564) and Faculty of Medicine, Chiang Mai University (Grant No. 059/2564).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to express their gratitude to the National Research Council of Thailand (NRCT) (Grant No. GSCMU(NRCT)/07/2564), the Faculty of Medicine at Chiang Mai University for funding (Grant No. 059/2564), and the Research Administration Section of the Faculty for their assistance with the English language editing. We also wish to thank all of the research assistants who helped us during the study, including health officers at a primary care unit in the Mueang Ngai sub-district, and the Thung Khao Phuang sub-district, and the Chiang Dao District Public Health Office.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.802810/full#supplementary-material
References
1. Sapbamrer R. Pesticide Use, Poisoning, and Knowledge and Unsafe Occupational Practices in Thailand. New Solut. (2018) 28:283–302. doi: 10.1177/1048291118759311
2. Laohaudomchok W, Nankongnab N, Siriruttanapruk S, Klaimala P, Lianchamroon W, Ousap P, et al. Pesticide use in Thailand: current situation, health risks, and gaps in research and policy. Hum Ecol Risk Assess. (2020) 27:1147–69. doi: 10.1080/10807039.2020.1808777
3. Panuwet P, Siriwong W, Prapamontol T, Ryan PB, Fiedler N, Robson MG, et al. Agricultural pesticide management in Thailand: status and population health risk. Environ Sci Policy. (2012) 17:72–81. doi: 10.1016/j.envsci.2011.12.005
4. Simaremare SRS, Hung CC, Hsieh CJ, Yiin LM. Relationship between Organophosphate and Pyrethroid Insecticides in Blood and Their Metabolites in Urine: A Pilot Study. Int J Environ Res Public Health. (2019) 17:34. doi: 10.3390/ijerph17010034
5. Damalas CA, Koutroubas SD. Farmers' exposure to pesticides: toxicity types and ways of prevention. Toxics. (2016) 4:1. doi: 10.3390/toxics4010001
6. Peiris-John RJ, Ruberu DK, Wickremasinghe AR. van-der-Hoek W. Low-level exposure to organophosphate pesticides leads to restrictive lung dysfunction. Resp Med. (2005) 99:1319–24. doi: 10.1016/j.rmed.2005.02.001
7. Sapbamrer R, Nata S. Health symptoms related to pesticide exposure and agricultural tasks among rice farmers from northern Thailand. Environ Health Prev. (2014) 19:12–20. doi: 10.1007/s12199-013-0349-3
8. Rivera EP, Siriwong W, Taneepanichskul N, Norkaew S, Robson MG. Health risk related to pesticide exposure in the agriculture system in thailand: a systematic review. J Health Res. (2016) 30:S71–80.
9. Thundiyil JG, Stober J, Besbelli N, Pronczuk J. Acute pesticide poisoning: a proposed classification tool. B World Health Organ. (2008) 86:205–9. doi: 10.2471/BLT.08.041814
10. Ritter L, Goushleff NCI, Arbuckle T, Cole D, Raizenne M. Addressing the linkage between exposure to pesticides and human health effects–Research trends and priorities for research. J Toxicol Env Heal B. (2006) 9:441–56. doi: 10.1080/10937400600755895
11. Sapbamrer R, Hongsibsong S, Sittitoon N, Amput P. DNA damage and adverse neurological outcomes among garlic farmers exposed to organophosphate pesticides. Environ Toxicol Phar. (2019) 72:103241. doi: 10.1016/j.etap.2019.103241
12. Sapbamrer R, Khacha-Ananda S, Sittitoon N, Wunnapuk K, Seesen M, Sidthilaw S, et al. A longitudinal follow-up study of oxidative stress and DNA damage among farmers exposed to pesticide mixtures. Environ Sci Pollut Res Int. (2019) 26:13185–94. doi: 10.1007/s11356-019-04650-z
13. Chittrakul J, Sapbamrer R, Sirikul W. Insecticide exposure and risk of asthmatic symptoms: a systematic review and meta-analysis. Toxics. (2021) 9:228. doi: 10.3390/toxics9090228
14. Fucic A, Duca RC, Galea KS, Maric T, Garcia K, Bloom MS, et al. Reproductive health risks associated with occupational and environmental exposure to pesticides. Int J Env Res Pub He. (2021) 18. doi: 10.3390/ijerph18126576
15. Amaral AF. Pesticides and asthma: challenges for epidemiology. Front Public Health. (2014) 2:6. doi: 10.3389/fpubh.2014.00006
16. Panis C, Kawassaki AC, Crestani AP, Pascotto CR, Bortoloti DS, Vicentini GE, et al. Evidence on human exposure to pesticides and the occurrence of health hazards in the Brazilian population: a systematic review. Front Public Health. (2021) 9:787438. doi: 10.3389/fpubh.2021.787438
17. Kamel F, Hoppin JA. Association of pesticide exposure with neurologic dysfunction and disease. Environ Health Persp. (2004) 112:950–8. doi: 10.1289/ehp.7135
18. Farnham A, Fuhrimann S, Staudacher P, Quiros-Lepiz M, Hyland C, Winkler MS, et al. Long-term neurological and psychological distress symptoms among smallholder farmers in costa rica with a history of acute pesticide poisoning. Int J Env Res Pub He. (2021) 18. doi: 10.3390/ijerph18179021
19. Ramirez-Santana M, Zuniga-Venegas L, Corral S, Roeleveld N, Groenewoud H, Van der Velden K, et al. Reduced neurobehavioral functioning in agricultural workers and rural inhabitants exposed to pesticides in northern Chile and its association with blood biomarkers inhibition. Environ Health. (2020) 19:84. doi: 10.1186/s12940-020-00634-6
20. Cham EYK, Tse JCL, Chong YK, Chen ML, Wong OF, Fung HT, et al. case of pyrethroid poisoning with clinical presentation mimicking organophosphate poisoning. Hong Kong J Emerg Me. (2016) 23:47–51. doi: 10.1177/102490791602300207
21. Panwar M, Usha G, Kumath M. Status epilepticus: An association with pyrethroid poisoning. Indian J Crit Care Med. (2013) 17:119–20. doi: 10.4103/0972-5229.114825
22. Bradberry SM, Cage SA, Proudfoot AT, Vale JA. Poisoning due to pyrethroids. Toxicol Rev. (2005) 24:93–106. doi: 10.2165/00139709-200524020-00003
23. Fiedler N, Rohitrattana J, Siriwong W, Suttiwan P, Strickland PO, Ryan PB, et al. Neurobehavioral effects of exposure to organophosphates and pyrethroid pesticides among Thai children. Neurotoxicology. (2015) 48:90–9. doi: 10.1016/j.neuro.2015.02.003
24. Sapbamrer R, Thammachai A. A systematic review of factors influencing farmers' adoption of organic farming. Sustain-Basel. (2021) 13. doi: 10.3390/su13073842
25. Cabrera NL, Leckie JO. Pesticide risk communication, risk perception, and self-protective behaviors among farmworkers in California's Salinas Valley. Hisp J Behav Sci. (2009) 31:258–72. doi: 10.1177/0739986309331877
26. Barraza D, Jansen K, Wesseling C, de Joode BV. Pesticide risk perceptions among bystanders of aerial spraying on bananas in Costa Rica. Environ Res. 2020 189. doi: 10.1016/j.envres.2020.109877
27. Remoundou K, Brennan M, Sacchettini G, Panzone L, Butler-Ellis MC, Capri E, et al. Perceptions of pesticides exposure risks by operators, workers, residents and bystanders in Greece, Italy and the UK. Sci Total Environ. (2015) 505:1082–92. doi: 10.1016/j.scitotenv.2014.10.099
28. Subiza-Perez M, Santa Marina L, Irizar A, Gallastegi M, Anabitarte A, Urbieta N, et al. Who feels a greater environmental risk? Women, younger adults and pro-environmentally friendly people express higher concerns about a set of environmental exposures. Environ Res. (2020) 181:108918. doi: 10.1016/j.envres.2019.108918
29. Sodjinou E, Glin L.C., Nicolay G., Tovignan S., Hinvi J. Socioeconomic determinants of organic cotton adoption in Benin, West Africa. Agric Food Econ. (2015) 3:1–22. doi: 10.1186/s40100-015-0030-9
30. Wang WY, Jin JJ, He R, Gong HZ. Gender differences in pesticide use knowledge, risk awareness and practices in Chinese farmers. Sci Total Environ. (2017) 590:22–8. doi: 10.1016/j.scitotenv.2017.03.053
31. Christie ME, Van Houweling E, Zseleczky L. Mapping gendered pest management knowledge, practices, and pesticide exposure pathways in Ghana and Mali. Agr Hum Values. (2015) 32:761–75. doi: 10.1007/s10460-015-9590-2
32. Nouhoheflin T. Assessing the economic impacts of tomato Integrated Pest Management in Mali and Senegal. Blacksburg, VA: Virginia Polytechnic Institute and State University. (2010).
33. Gesesew HA, Woldemichael K, Massa D, Mwanri L. Farmers knowledge, attitudes, practices and health problems associated with pesticide use in rural irrigation villages, Southwest Ethiopia. Plos ONE. (2016) 11. doi: 10.1371/journal.pone.0162527
34. Santaweesuk S, Boonyakawee P, Siriwong W. Knowledge, attitude and practice of pesticide use and serum cholinesterase levels among rice farmers in Nakhon Nayok Province, Thailand. J Health Res. (2020) 34:379–87. doi: 10.1108/JHR-09-2019-0204
35. Damalas CA, Telidis GK, Thanos SD. Assessing farmers' practices on disposal of pesticide waste after use. Sci Total Environ. (2008) 390:341–5. doi: 10.1016/j.scitotenv.2007.10.028
36. Gaber S, Abdel-Latif SH. Effect of education and health locus of control on safe use of pesticides: a cross sectional random study. J Occ Med Toxicol. 2012 7. doi: 10.1186/1745-6673-7-3
37. Recena MCP, Caldas ED, Pires DX, Pontes ERJC. Pesticides exposure in Culturama, Brazil–Knowledge, attitudes, and practices. Environ Res. (2006) 102:230–6. doi: 10.1016/j.envres.2006.01.007
38. Rostami F, Afshari M, Rostami-Moez M, Assari MJ, Soltanian AR. Knowledge, Attitude, and Practice of Pesticides Use Among Agricultural Workers. Indian J Occup Envir. (2019) 23:42–7. doi: 10.4103/ijoem.IJOEM_153_18
39. Yassin MM, Abu Mourad TA, Safi JM. Knowledge, attitude, practice, and toxicity symptoms associated with pesticide use among farm workers in the Gaza Strip. Occup Environ Med. (2002) 59:387–93. doi: 10.1136/oem.59.6.387
40. Arbiol J, Orencio PM, Romena N, Nomura H, Takahashi Y, Yabe M. Knowledge, attitude and practices towards leptospirosis among lakeshore communities of Calamba and Los Banos, Laguna, Philippines. Agriculture-Basel. (2016) 6. doi: 10.3390/agriculture6020018
41. Salameh PR, Baldi I, Brochard P, Saleh BA. Pesticides in Lebanon: a knowledge, attitude, and practice study. Environ Res. (2004) 94:1–6. doi: 10.1016/S0013-9351(03)00092-6
42. Damalas CA, Georgiou EB, Theodorou MG. Pesticide use and safety practices among Greek tobacco farmers: a survey. Int J Environ Heal R. (2006) 16:339–48. doi: 10.1080/09603120600869190
43. Hashemi SM, Hosseini SM, Hashemi MK. Farmers' perceptions of safe use of pesticides: determinants and training needs. Int Arch Occ Env Hea. (2012) 85:57–66. doi: 10.1007/s00420-011-0641-8
44. Mengistie BT, Mol APJ, Oosterveer P. Pesticide use practices among smallholder vegetable farmers in Ethiopian Central Rift Valley. Environ Dev Sustain. (2017) 19:301–24. doi: 10.1007/s10668-015-9728-9
45. Palis FG, Flor RJ, Warburton H, Hossain M. Our farmers at risk: behaviour and belief system in pesticide safety. J Public Health. (2006) 28:43–8. doi: 10.1093/pubmed/fdi066
46. Sapbamrer R, Thammachai A. Factors affecting use of personal protective equipment and pesticide safety practices: a systematic review. Environ Res. (2020) 185. doi: 10.1016/j.envres.2020.109444
47. Iyyadurai R, Peter JV, Immanuel S, Begum A, Zachariah A, Jasmine S, et al. Organophosphate-pyrethroid combination pesticides may be associated with increased toxicity in human poisoning compared to either pesticide alone. Clin Toxicol. (2014) 52:538–41. doi: 10.3109/15563650.2014.909933
48. Basrai Z, Koh C, Celedon M, Warren J. Clinical effects from household insecticide: pyrethroid or organophosphate toxicity? BMJ Case Rep. (2019) 12. doi: 10.1136/bcr-2019-230966
49. McKelvey W, Jacobson JB, Kass D, Barr DB, Davis M, Calafat AM, et al. Population-based biomonitoring of exposure to organophosphate and pyrethroid pesticides in New York City. Environ Health Persp. (2013) 121:1349–56. doi: 10.1289/ehp.1206015
50. Bateman DN. Management of pyrethroid exposure. J Toxicol Clin Toxicol. (2000) 38:107–9. doi: 10.1081/CLT-100100924
51. Proudfoot AT. Poisoning due to Pyrethrins. Toxicol Rev. (2005) 2:107–13. doi: 10.2165/00139709-200524020-00004
52. Chakraborty S, Mukherjee S, Roychoudhury S, Siddique S, Lahiri T, Ray MR. Chronic Exposures to Cholinesterase-inhibiting Pesticides Adversely Affect Respiratory Health of Agricultural Workers in India. J Occup Health. (2009) 51:488–97. doi: 10.1539/joh.L9070
53. Sekiyama M, Tanaka M, Gunawan B, Abdoellah O, Watanabe C. Pesticide usage and its association with health symptoms among farmers in rural villages in West Java, Indonesia. Environ Sci. (2007) 14:23–33.
54. Giyanwani PR, Zubair U, Salam O, Zubair Z. Respiratory failure following organophosphate poisoning: a literature review. Cureus. (2017) 9:e1651. doi: 10.7759/cureus.1651
55. Vorselaars ADM, van den Berg PM, Drent M. Severe pulmonary toxicity associated with inhalation of pyrethroid-based domestic insecticides (Bop/Sapolio): a case series and literature review. Curr Opin Pulm Med. (2021) 27:271–7. doi: 10.1097/MCP.0000000000000779
56. Jokanovic M. Neurotoxic effects of organophosphorus pesticides and possible association with neurodegenerative diseases in man: A review. Toxicology. (2018) 410:125–31. doi: 10.1016/j.tox.2018.09.009
57. Woltjer RL. Chapter 50—Neuropathologic Effects of Chemical Warfare Agents. Handjournal of Toxicology of Chemical Warfare Agents (Second Edition) ed: Academic Press. (2015). doi: 10.1016/B978-0-12-800159-2.00050-6
58. Wilks MF. Pyrethroid-induced paresthesia—a central or local toxic effect? J Toxicol Clin Toxicol. (2000) 38:103–5. doi: 10.1081/CLT-100100923
59. Yang PY, Lin JL, Hall AH, Tsao TC, Chern MS. Acute ingestion poisoning with insecticide formulations containing the pyrethroid permethrin, xylene, and surfactant: a review of 48 cases. J Toxicol Clin Toxicol. (2002) 40:107–13. doi: 10.1081/CLT-120004397
60. Stallones L, Beseler C. Pesticide illness, farm practices, and neurological symptoms among farm residents in Colorado. Environ Res. (2002) 90:89–97. doi: 10.1006/enrs.2002.4398
61. Wesseling C, van Wendel de. Joode B, Keifer M, London L, Mergler D, Stallones L. Symptoms of psychological distress and suicidal ideation among banana workers with a history of poisoning by organophosphate or n-methyl carbamate pesticides. Occup Environ Med. (2010) 67:778–84. doi: 10.1136/oem.2009.047266
62. Albers JW, Garabrant DH, Schweitzer S, Garrison RP, Richardson RJ, Berent S. Absence of sensory neuropathy among workers with occupational exposure to chlorpyrifos. Muscle Nerve. (2004) 29:677–86. doi: 10.1002/mus.20007
Keywords: practice, health symptoms, organophosphates, pyrethroids, pesticides, farmers, knowledge, awareness
Citation: Thammachai A, Sapbamrer R, Rohitrattana J, Tongprasert S, Hongsibsong S and Wangsan K (2022) Differences in Knowledge, Awareness, Practice, and Health Symptoms in Farmers Who Applied Organophosphates and Pyrethroids on Farms. Front. Public Health 10:802810. doi: 10.3389/fpubh.2022.802810
Received: 17 November 2021; Accepted: 10 January 2022;
Published: 02 February 2022.
Edited by:
Mohiuddin Md. Taimur Khan, Washington State University Tri-Cities, United StatesReviewed by:
Shikha Singh, Allahabad University, IndiaLiliana Cori, Italian National Research Council, Italy
María Teresa Muñoz Quezada, Catholic University of the Maule, Chile
Copyright © 2022 Thammachai, Sapbamrer, Rohitrattana, Tongprasert, Hongsibsong and Wangsan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ratana Sapbamrer, lekratana56@yahoo.com; ratana.sapbamrer@cmu.ac.th
 Ajchamon Thammachai
Ajchamon Thammachai Ratana Sapbamrer
Ratana Sapbamrer Juthasiri Rohitrattana
Juthasiri Rohitrattana Siam Tongprasert
Siam Tongprasert Surat Hongsibsong
Surat Hongsibsong Kampanat Wangsan
Kampanat Wangsan