- 1Department of Internal Medicine and Radboud Center for Infectious Diseases, Radboud University Medical Center, Nijmegen, Netherlands
- 2The Global Tuberculosis Program, Texas Children’s Hospital, Department of Pediatrics, Baylor College of Medicine, Houston, TX, United States
- 3Division of Infectious Disease and Global Health, University of St Andrews, St Andrews, United Kingdom
- 4FIND, Geneva, Switzerland
- 5Division of Infectious Diseases and Tropical Medicine, LMU University Hospital, Munich, Germany
- 6German Center for Infection Research (DZIF), Partner Site Munich, Munich, Germany
- 7Otsuka Novel Products GmbH, Munich, Germany
- 8German Center for Infection Research (DZIF), Partner Site Hamburg-Lübeck-Borstel-Riems, Borstel, Germany
- 9Division of Clinical Infectious Diseases, Research Center Borstel, Borstel, Germany
- 10Respiratory Medicine & International Health, University of Lübeck, Lübeck, Germany
- 11Janssen Global Public Health R&D, Janssen Pharmaceutica NV, Beerse, Belgium
- 12Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, United Kingdom
Tuberculosis drug trials are primarily designed to identify antibiotic regimens with the strongest potency to kill Mycobacterium tuberculosis. However, microbiologic cure is not synonymous with improved health and recovery. Beyond antimicrobial efficacy, parameters such as morbidity and mortality related to lung function, cardiovascular health, and cancer should be prioritized. This narrative review emphasizes the critical need to emphasize clinical outcomes as much, if not more, than microbiological endpoints. We examine the underlying pathophysiological mechanisms and determinants of non-microbiological outcomes in tuberculosis, providing a synthesis of current knowledge. While there is growing evidence for some biomarkers to risk stratify TB patients for risk of all-cause mortality, relapse, or lung damage, no evidence was found on TB-associated cancer or cardiovascular disease. In addition to monitoring microbiologic outcomes, clinical trials and treatment cohorts need to capture patient-centered health dimensions more broadly. Finally, we highlight key research gaps and opportunities to evaluate non-microbiological biomarkers, aiming to improve patient monitoring and enable stratified approaches to tuberculosis management.
Introduction
Tuberculosis (TB) morbidity and mortality arise not only from Mycobacterium tuberculosis infection but also from immune dysregulation. Current TB drug development primarily focuses on microbiological endpoints, such as bacillary clearance, to define treatment success (Gillespie et al., 2024). However, these measures fail to capture long-term clinical outcomes, including relapse free cure and post-treatment morbidity and mortality. While antibiotics kill the bacilli, they do not repair immune dysregulation or heal lung dysfunction (Malherbe et al., 2016; Azam et al., 2022; Wallis et al., 2022), which can lead to sterile inflammation, paradoxical reactions, and increased rates of non-communicable diseases and recurrent infections (Critchley et al., 2024; Romanowski et al., 2019; Lee-Rodriguez et al., 2020; Menzies et al., 2021; Vega et al., 2021).
Extrapulmonary TB, such as TB meningitis, TB pericarditis, and spondylodiscitis, highlights the disconnect between microbiological cure and restored health. For instance, TB meningitis is often complicated by severe inflammation, causing stroke, seizures, hydrocephalus, or cranial nerve palsy, with mortality rates of 20–50% during treatment (Soria et al., 2021), and long-term neurological sequelae among survivors (Christensen et al., 2011). However, this review focuses on pulmonary TB, the most prevalent form of the disease with available data.
As part of the UNITE4TB consortium, we recently developed a target product profile (TPP) outlining the ideal characteristics of biomarker tools that would assist with treatment monitoring by quantifying viable M. tuberculosis and replacing culture based endpoints (Gillespie et al., 2024). Building on this work, we advocate for the inclusion of non-microbiological endpoints in TB drug trials. This narrative review first outlines the epidemiology of clinical and patient-centered outcomes during and after TB treatment. We then explore the underlying mechanisms of these outcomes, assess putative exploratory biomarkers that reflect these broader health dimensions, and propose a framework for integrating non-microbiological endpoints and biomarkers into TB drug trials to inform comprehensive guideline development.
Patient-centered outcomes in tuberculosis
The World Health Organization (WHO) estimated that 10.8 million people developed tuberculosis in 2023 (Global Tuberculosis Pragramme W, 2024). The WHO reports an 88% drug-susceptible TB treatment success rate, but this metric is based on completing a full course of antibiotics or achieving bacteriological clearance, defined as smear or culture negativity (Linh et al., 2021). In clinical trials, “cure” is similarly restricted to microbiological endpoints, often assessed at the conclusion of antibiotic therapy and after one or two years, without accounting for patients’ overall health or functional recovery. A more patient-centered approach would prioritize measures of morbidity and mortality outcomes, providing a more holistic appraisal of treatment efficacy.
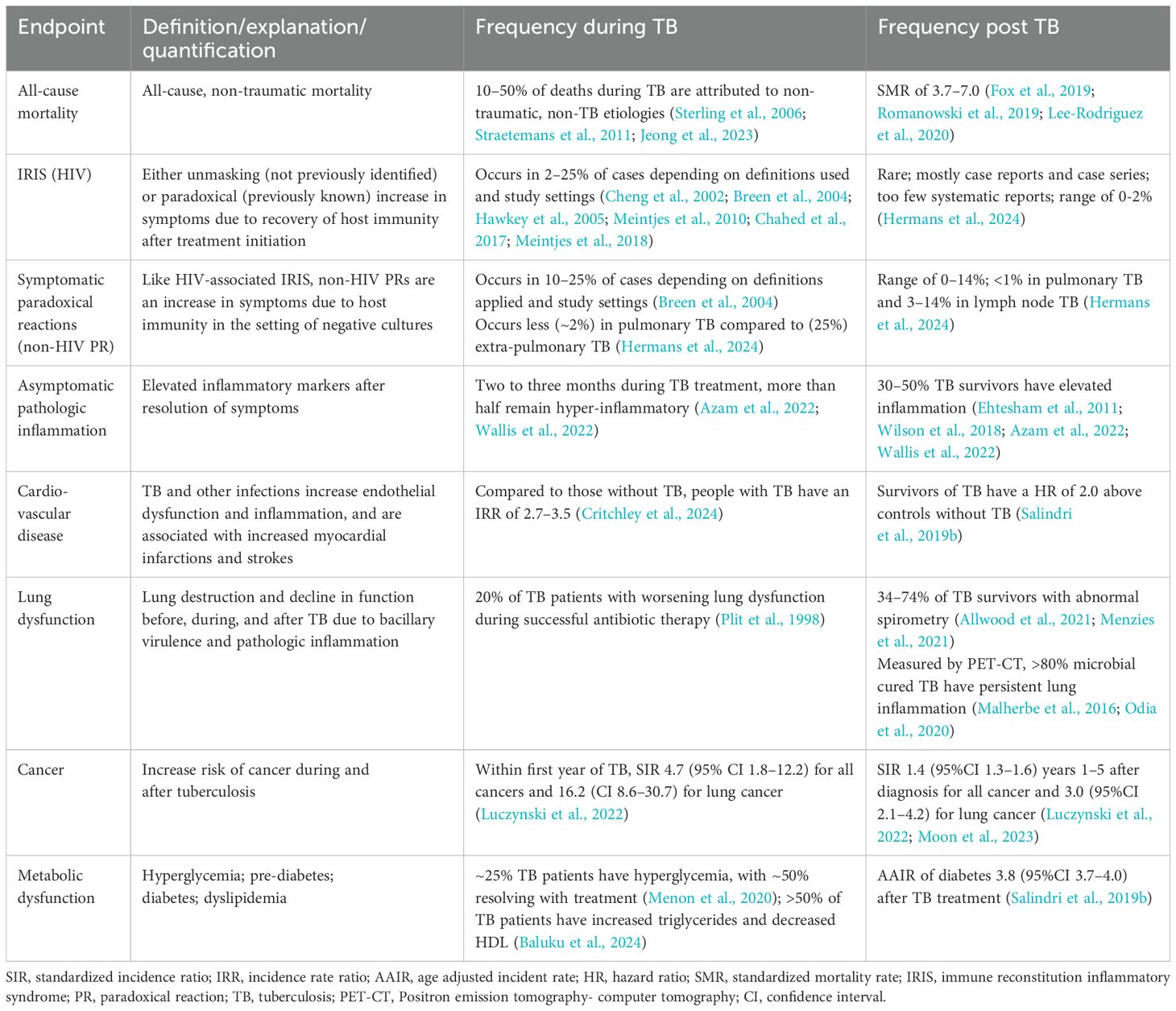
Microbiological cure does not always equate to restored health. For example, HIV co-infected individuals undergoing anti-retroviral therapy (ART) often experience immune reconstitution inflammatory syndrome (IRIS), a paradoxical reaction driven by sterile inflammation that causes significant morbidity and mortality. However, sterile inflammation and clinical worsening are not exclusive to HIV-associated TB. Estimates suggest that 10–25% of non-HIV-infected patients may also develop paradoxical worsening (Table 1), which is usually non-severe, but can be severe including complications, such as hemophagocytic lymphohistocytosis (HLH), a rare but life-threatening inflammatory syndrome (Cheng et al., 2002; Breen et al., 2004; Hawkey et al., 2005; Meintjes et al., 2010; Chahed et al., 2017; Meintjes et al., 2018; Kurver et al., 2024).
Persistent inflammation is common despite microbiological cure and studies report elevated systemic and lung-specific inflammation in 50–80% of TB patients following treatment (Malherbe et al., 2016; Odia et al., 2020; Azam et al., 2022). Additionally, significant mortality during TB treatment is often attributed to non-TB-related causes, such as acute myocardial infarctions and strokes, which are markedly increased both during and after therapy (Critchley et al., 2024; Huaman et al., 2015; Salindri et al., 2019b). Non-violent deaths not attributed to tuberculosis account for a substantial proportion of deaths among TB patients in many studies (Sterling et al., 2006; Gillespie et al., 2014; Jeong et al., 2023).
Table 1 summarizes some key patient-centered, non-microbiological outcomes observed during and after TB therapy. These outcomes emphasize the need for broader endpoints in TB research that reflect not just pathogen clearance but also comprehensive health restoration.
Post-tuberculosis morbidity and mortality
Despite successful antibiotic therapy, the burden of TB-attributable morbidity extends well beyond treatment completion. Studies estimate that approximately 47% of TB-related disability is experienced in the post-TB period (Menzies et al., 2021). A recent meta-analysis of long-term health describes a 3.7 higher risk of death (95% confidence interval (CI) 3.0–4.6) among TB survivors, compared to matched controls, independent of HIV co-infection (Romanowski et al., 2019). Increased mortality risk is predominantly due to increased cardiovascular, cancer, and respiratory disease among post-TB survivors (Figure 1) (Romanowski et al., 2019; Lee-Rodriguez et al., 2020). Similarly, a cohort study in Vietnam reported a standardized mortality ratio (SMR) of 4.0 (95% CI 3.7–4.2) for TB patients compared to the general population (Fox et al., 2019). In the United States, a retrospective cohort study of microbiologically confirmed TB cases revealed an adjusted loss of 7.0 years of life (95% CI 5.5 to 8.4) among TB survivors (Lee-Rodriguez et al., 2020).
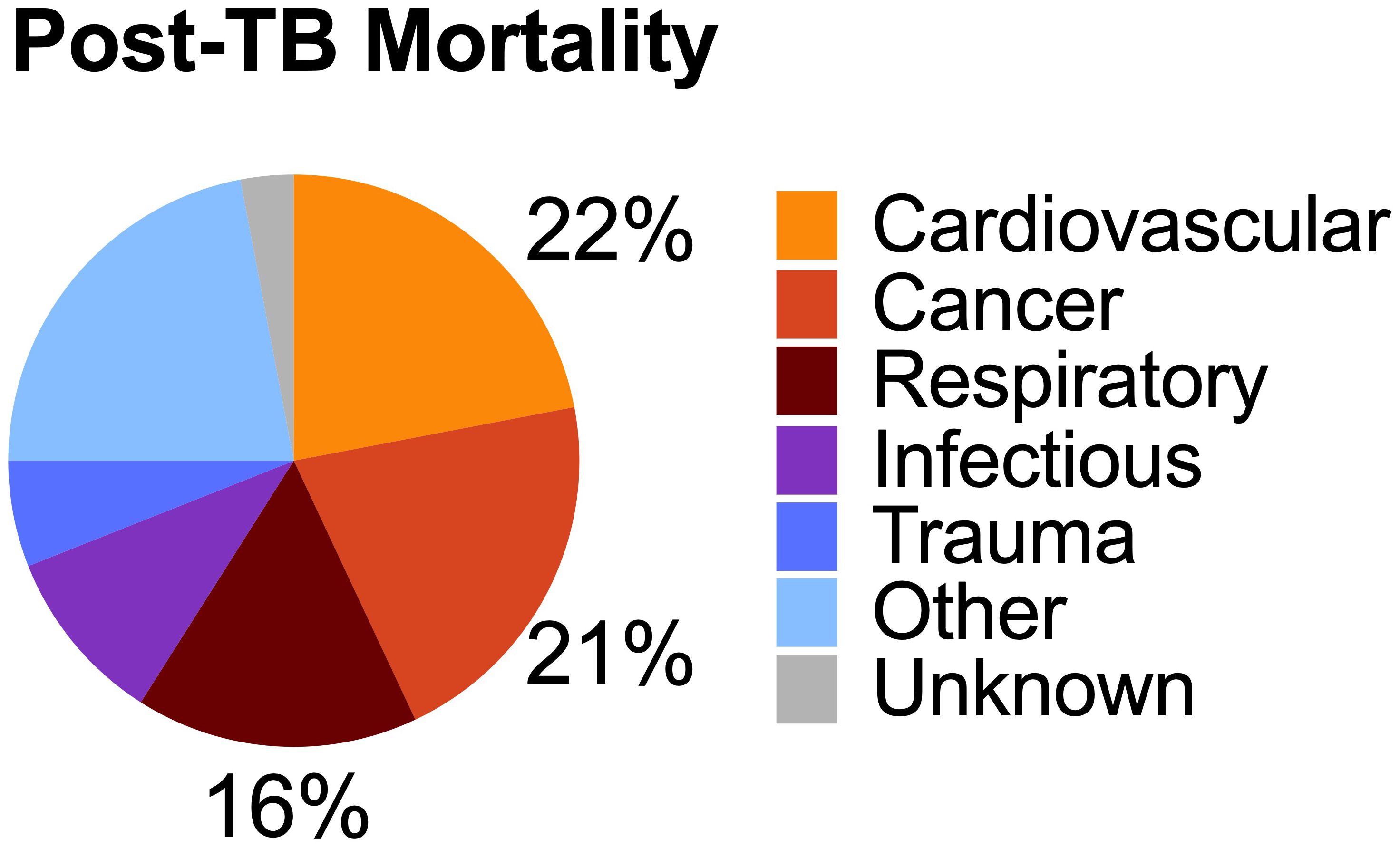
Figure 1. Burden of Post-tuberculosis mortality. Tuberculosis survivors have an increased risk of mortality compared to matched controls. The most common cause of death were cardiovascular, cancer, and respiratory. Source: Based on data from Romanowski et al. (2019).
Cardiovascular disease is the leading cause of death among TB survivors. A systematic review reported that 20% (95% CI 15–26) of post-TB deaths were due to cardiovascular disease (Romanowski et al., 2019). Additional studies confirm an increased risk of acute coronary syndromes and other cardiovascular events (Chung et al., 2014; Huaman et al., 2015). Malignancy attributable deaths comprise up to 19% of all post-TB deaths (Romanowski et al., 2019), with an incidence risk ratio of 1.9 at 2–4 years after TB treatment compared to controls (Wu et al., 2011). For example, an analysis using the Korean National health and Nutrition Survey found that TB survivors had elevated atherosclerotic cardiovascular disease (ASCVD) risk, one of the most common risk calculators for assessing non-TB cardiovascular disease (Yang et al., 2024).
Despite antimicrobial cure, many TB survivors have persistent respiratory symptoms and decreased quality of life (Mpagama et al., 2021). These respiratory complications are another major source of morbidity among TB survivors. Systematic reviews demonstrate that 10–15% of TB survivors have severe lung impairment, while any form of lung function loss affects 34–74% of TB survivors (Ivanova et al., 2023). Variable presentations include obstructive (18.4–86%), restrictive (16.1–29.7%), or mixed patterns (Ravimohan et al., 2018; Allwood et al., 2020; Khosa et al., 2020; Meghji et al., 2020). Secondary respiratory infections, such as cavitary fungal infections, non-tuberculosis mycobacteria, and recurrent TB are common. In many survivors, chronic inflammation, vascular damage, and lung fibrosis often culminate in post-TB pulmonary hypertension (van Heerden et al., 2024).
The psychological impact of TB persists long after treatment. Stigma, social isolation, income loss, and physical disabilities contribute to a vicious cycle resulting in ongoing mental health challenges. Underlying poverty and catastrophic costs, defined as the loss of at least 20% of annual family income, affect roughly half of TB patients and exacerbate economic and psychological burdens (Bagcchi, 2023). Evidence on post-TB health-related quality of life is mixed, with some studies showing normal scores and others indicating declines in psychological and physical well-being (Muniyandi et al., 2007; Laxmeshwar et al., 2019). The heterogeneity and drivers of normalized or persistent isolation and economic challenges should be evaluated, especially as how this relates to morbidity and mortality.
Modeling studies incorporating post-TB lung disease highlight significant variations in years of life lost, years lived with disability, and disability-adjusted life years (Menzies et al., 2021). Given the complexity and heterogeneity of these various outcomes, a single biomarker seems unlikely to predict the full spectrum of post-TB health challenges.
Biologic mechanisms
The diverse non-microbiological health outcomes associated with TB are driven by a complex interplay of external factors and biological mechanisms, with immune dysregulation playing a central role. This dysregulation can manifest as anergy (decreased immune responsiveness) and or pathological inflammation. Anergy includes hyporesponsive myeloid cells (immune tolerance) or lymphoid cells (immune exhaustion) (DiNardo et al., 2021). Paradoxically, many TB patients experiencing immune hypo-responsiveness simultaneously with pathologic inflammation (DiNardo et al., 2022). However, the response to TB therapy is highly variable with some TB survivors normalizing inflammatory and immune responsiveness while others experience persistent immune dysregulation.
Although inflammation decreases during TB treatment, a significant proportion of patients exhibit persistent systemic inflammation even after completing successful antibiotic therapy. For instance, studies assessing inflammation via C-reactive protein (CRP) indicate that 30–50% of patients have elevated CRP levels at the end of treatment (Ehtesham et al., 2011; Wilson et al., 2018; Azam et al., 2022; Wallis et al., 2022). Among healthy individuals, elevated CRP and other inflammatory cytokines Interleukin-1 (IL1) and IL6 are associated with increased risks of cardiovascular disease, cancer, and infections (Emerging Risk Factors et al., 2010; Guo et al., 2013; Everett et al., 2020; Khan et al., 2024). Notably, the resolution of hyperinflammation often lags behind the clearance of bacillary load. In one study, only 14% of participants achieved normalized CRP levels at six months of treatment, despite 88% having undetectable bacillary loads (Azam et al., 2022).
In addition to systemic inflammation, TB survivors frequently exhibit persistent lung-specific inflammation. Positron emission tomography-computed tomography (PET-CT) imaging has shown elevated metabolic activity in over 80% of patients following successful TB treatment, highlight the localized inflammatory burden (Malherbe et al., 2016; Odia et al., 2020). Inflammation, a broad and multifaceted phenomenon, is mediated by diverse, redundant, and overlapping molecular pathways. It remains unclear whether different inflammatory drivers necessitate distinct monitoring and management strategies.
Multiple factors contribute to persistent inflammation and immune dysregulation during and after TB (Figure 2). Residual dead bacilli or M. tuberculosis antigens that are not fully cleared from tissues can act as chronic immunogens. Persistent inflammation may also arise from malnutrition, micronutrient deficiencies, bronchiectasis with recurrent infections, residual cavities prone to secondary infections, endothelial cell disruption, clonal hematopoiesis, post-TB epigenetic modifications, co-infections, or antibiotic-induced redox imbalances, particularly with isoniazid (Canetti, 1955; Zentner et al., 2020; Allwood et al., 2021; DiNardo et al., 2021; VanValkenburg et al., 2022).
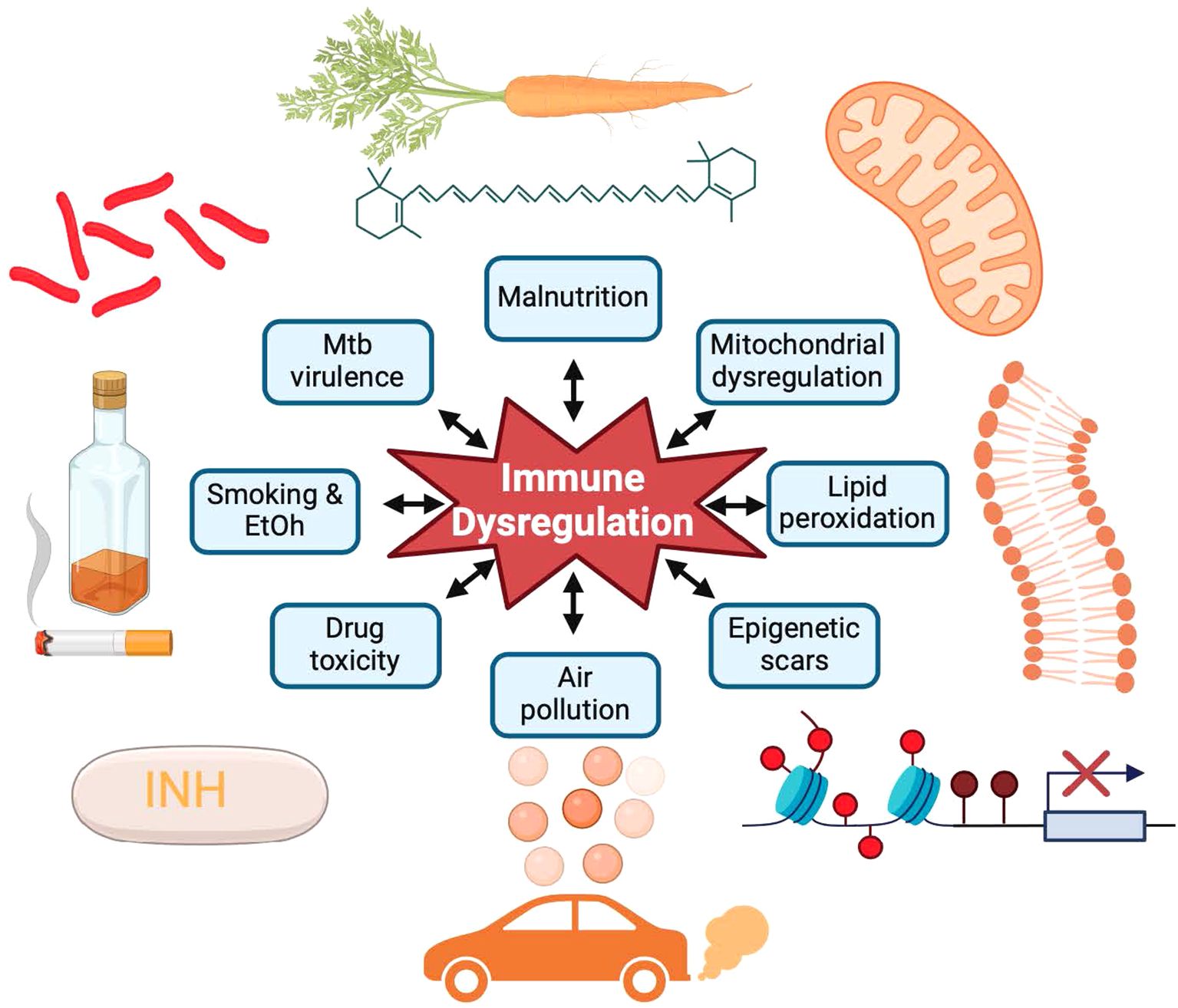
Figure 2. Contributing factors and biologic mechanisms driving tuberculosis morbidity and mortality. Mycobacterial virulence factors, persistent smoking, alcohol (EtOH) use, drug toxicity, malnutrition, and air pollution result in mitochondrial dysfunction, lipid peroxidation, and epigenetic scars resulting in immune dysregulation and inflammation despite successful antibiotic treatment. Source: Created with BioRender.com.
Beyond biological contributors, TB survivors often endure ongoing social and psychological stressors, such as stigma, economic hardships, and social isolation, which can exacerbate systemic inflammation and immune dysregulation. Addressing these multifactorial drivers is critical for improving long-term health outcomes for TB survivors (Green et al., 2023).
Immune dysregulation can also manifest as immune hypo-responsiveness. Depending on the study and definition, approximately 7–35% of successfully treated TB survivors exhibit persistently low immune responsiveness (Delgado et al., 2002; Alexander et al., 2023). This heterogeneity reflects underlying immune dysfunction, with many survivors showing reduced M. tuberculosis-specific antigen-induced up-regulation of IL-12, IL-2, IFNγ, diminished antigen-driven proliferative capacity, and heightened expression of immune checkpoint inhibitors and regulatory cytokines such as IL-10 (Boussiotis et al., 2000; Sahiratmadja et al., 2007). Monocytes and myeloid cells also show persistent hypo-responsiveness, with long-term decreased production of IL1β, IL6, and IL12 (Sahiratmadja et al., 2007; DiNardo et al., 2022). Effective host immunity requires a delicate balance that includes generating sufficient pro-inflammatory signals to eradicate the intracellular pathogen without triggering an immune responses that induces collateral tissue damage and increase the risk of cardiovascular disease or lung dysfunction. Some patients suffer from excessive inflammation as well as immune hypo-responsiveness, with TB-associated hemophagocytic lymphohistiocytosis (HLH) as a rare example (Kurver et al., 2024).
Animal and human studies have identified several mechanisms that mitigate immune-induced pathology, including immune checkpoint inhibitors (e.g. PD-1, TIM-3, CTLA-4), inhibitory cytokines (e.g. IL-10, TGF-β), inhibitory metabolites (e.g. itaconate, succinate), and epigenetic immune regulation (Boussiotis et al., 2000; Barber et al., 2011; Nair et al., 2018; DiNardo et al., 2020; Abhimanyu et al., 2024). These pathways likely prevent IRIS and paradoxical reactions during treatment. Future biomarkers must distinguish beneficial immune suppression from detrimental immune inhibition to guide clinical management.
In addition to immune dysregulation, many TB survivors endure tissue destruction that perpetuates inflammation and predisposes them to recurrent infections. Pulmonary cavities often harbor secondary bacterial, fungal and non-tuberculosis mycobacterial infections, compounding inflammation and morbidity (Auld et al., 2024). Residual cicatrization and fibrosis frequently result in restrictive lung impairment, reduced lung volume, and pulmonary hypertension (van Heerden et al., 2024). Other lung complications include tracheobronchial stenosis, bronchiectasis, small airway thickening, parenchymal fibrosis, and pleural thickening. Studies have yet to determine whether the diverse manifestations of lung pathology require a similarly diverse suite of biomarkers for predicting pulmonary outcomes. Current means to monitor TB associated lung damage, not universally available in resource constrained settings, include chest X-rays, spirometry, CT scans, oscillometry, and gas exchange measurements.
Several factors may contribute to immune-dysregulation and tissue pathology in TB. Malnutrition and diabetes increase TB risk and mortality, and are associated with immune dysfunction and tissue pathology. Both human and mycobacterial genetics influence inflammation resolution, and treatment-associated morbidity and mortality. For instance, polymorphisms to human leukocyte antigens or the human matrix mateloproteinase-1 (MMP-1) gene have been associated with increased risk of TB disease risk, development of IRIS, or TB-induced fibrosis (Wang et al., 2010; Tervi et al., 2023; Messah et al., 2024). Similarly, genetic variants regulating inflammasomes correlate with decreased IL-18 and IL-6 levels, and improved forced vital capacity (FVC) (Ravimohan et al., 2020). On the microbial side, evidence from animal models and human studies suggests that M. tuberculosis genetics affect disease progression, cavitation, dissemination, and host immune-metabolic responses (Via et al., 2013; Howard et al., 2018). Likely, the interplay between host and mycobacterial genetics shapes inflammation persistence, immune responsiveness, and post-TB sequelae (McHenry et al., 2019).
Unfortunately, tradeoffs exist between achieving microbiologic cure and optimizing overall health. For example, a clinical trial demonstrated that receiving metformin alongside standard antibiotic therapy had slower microbiologic culture conversion rates but showed improved radiographic lung healing (Padmapriydarsini et al., 2021). Moreover certain antibiotics contribute to inflammation. Isoniazid, a cornerstone of TB treatment for over 50 years, produces hydrazine and acetylhydrazine, toxic, reactive metabolites that induces lipid peroxidation and inflammation (Zentner et al., 2020). This mechanism may partly explain the increased cardiovascular risk observed during and after TB.
In summary, persistent immune dysregulation in TB survivors arises from a complex interplay of molecular, social, and anatomic factors, resulting in significant morbidity and mortality (Malefane and Maarman, 2024). Addressing these challenges requires linking these drivers to diverse clinical outcomes, an endeavor that large clinical trial platforms are well-positioned to undertake.
Putative biomarkers for patient-centered, non-microbiological outcomes
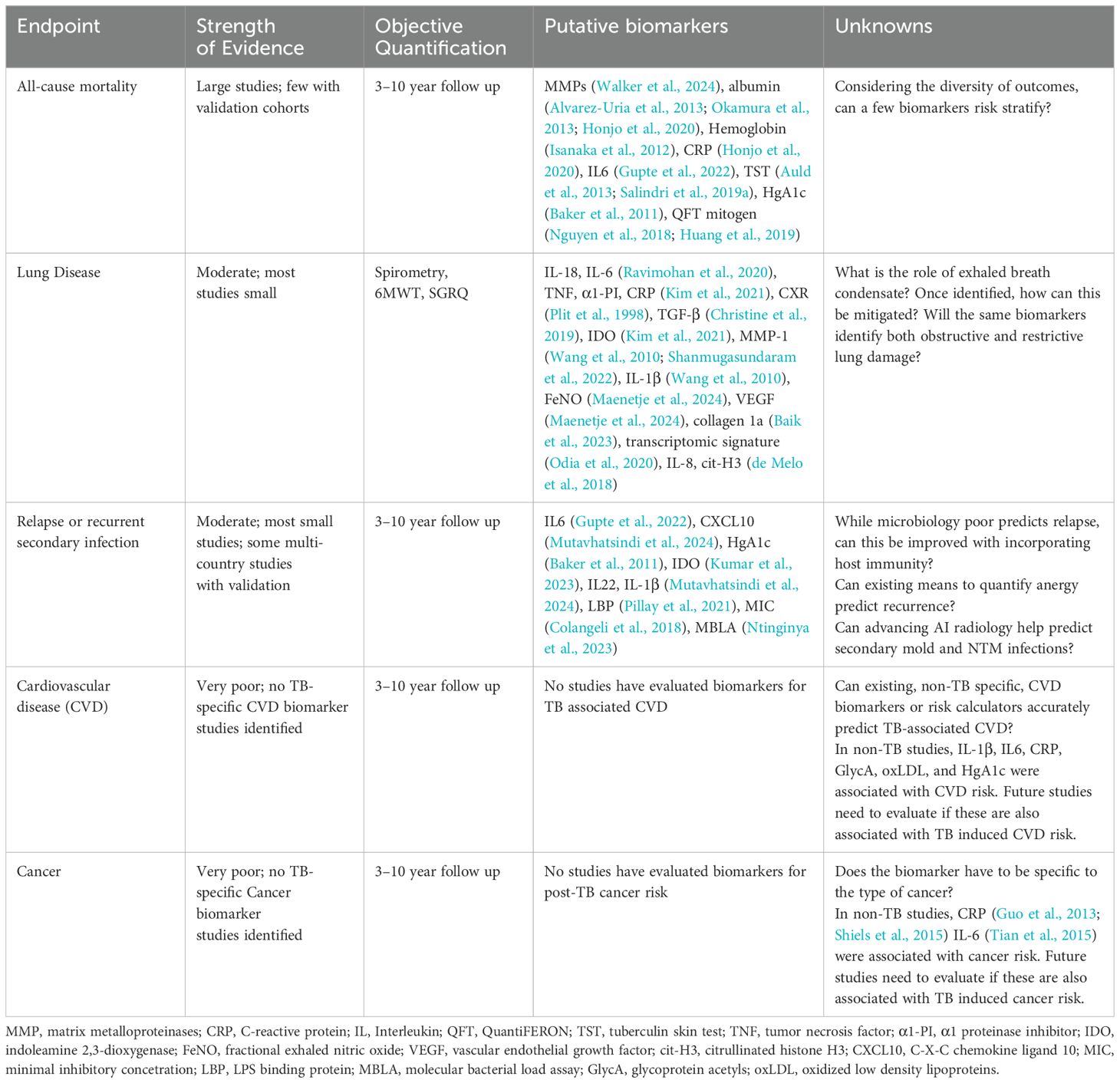
We identified few studies evaluating biomarkers for TB-associated lung damage, all-cause mortality, and relapse. However, no studies specifically addressed biomarkers for TB-associated cardiovascular disease or cancer (Table 2).
Most studies on all-cause mortality during TB treatment identified non-specific biomarkers. For example, two large studies, including 466 and 2,854 TB patients, demonstrated that anergy, defined by lower mitogen levels (Huang et al., 2019) or negative QuantiFERON IGRA results (Nguyen et al., 2018), was associated with higher mortality. Similarly, negative TB skin test reactions were linked to increased mortality in two additional large studies (Auld et al., 2013; Salindri et al., 2019a). Other non-specific markers, including anemia, low albumin, lymphopenia, and elevated IL-6 or CRP levels, were also correlated with increased mortality (Table 2) (Isanaka et al., 2012; Alvarez-Uria et al., 2013; Okamura et al., 2013; Honjo et al., 2020; Gupte et al., 2022). Interestingly, these studies suggest that both anergy (failure to mount an immune response) and excessive inflammation, increase the risk for death during and after TB.
Research on biomarkers for TB-associated lung disease remains limited, primarily involving smaller studies. For instance, end-of-therapy (EOT) CRP, and α1-protease inhibitor levels were inversely correlated with EOT forced expiratory velocity in the first second (FEV1) (Plit et al., 1998). Elevated TGF levels have been associated with fibrotic lung damage, while proinflammatory cytokines such as IL-6, IL-8, and tumor necrosis factor (TNF) predict necrosis and cavitation (Bekker et al., 1998; Tsao et al., 2000; Lasco et al., 2005; Christine et al., 2019). Persistent neutrophil activation and of inflammasome activation, such as through neutrophil extracellular traps (NETs), have been implicated in lung damage (Ravimohan et al., 2020), highlighting the need for resolving inflammation to facilitate lung healing.
Non-invasive biomarkers for TB-induced lung damage also show promise. For example, measurements of the fraction of exhaled nitric oxide (FeNO) or exhaled breath condensates (e.g. reduced glutathione, lipid peroxidation, and cytokines) identify TB-related lung pathology in smaller preliminary studies (Table 2) (Ravimohan et al., 2020; Guzman-Beltran et al., 2021; Mosquera-Restrepo et al., 2022; Maenetje et al., 2024).
TB relapse can be due to recurrence or reinfection. Recurrences, relapses from the same strain, likely results from both residual viable mycobacteria and a deficient immune response. TB reinfection, which occurs at higher risk among individuals with previous TB, likely occurs due to a combination of persistent environmental exposures and persistent immune suppression (Vega et al., 2024). Initial bacillary burden, measured by culture or PCR, is a poor predictor of relapse (Phillips et al., 2016), with a meta-analysis reporting culture having a sensitivity of only 40% for predicting relapse (Horne et al., 2010; DiNardo et al., 2020; Bobak et al., 2022; DiNardo et al., 2022). Quantifying bacterial killing rate may improve relapse prediction (Magombedze et al., 2021), and molecular methods like the Mycobacterial Load Assay (MBLA), which detects viable M. tuberculosis RNA, demonstrates initial promise to increase risk of relapse (Ntinginya et al., 2023).
Relapse prediction improves when bacillary burden is combined with additional clinical and immune parameters. For example, a study in South Africa, validated in cohorts in Uganda and Brazil, found that combining culture results, body mass index (BMI), and immune biomarkers (e.g. CXCL10, soluble IL6R, IL12p40, and TNFβ) achieved 75% sensitivity for detecting relapse. Another study involving 130 TB patients from Brazil, Uganda and South Africa reported that combining BMI, culture time to positivity, and biomarkers (e.g. IL1β, CXCL10, IL-22, and complement C3) demonstrated over 80% sensitivity for relapse prediction, a dramatic improvement over culture alone (Mutavhatsindi et al., 2024). Biomarkers of intestinal translocation (e.g. lipopolysaccharide (LPS), LPS-binding protein, soluble CD14) have also been linked to relapse risk (Kumar et al., 2022), with LPS-binding protein confirmed as a strong predictor in a South African cohort (adjusted OR: 8.7, CI 1.2-62.6) (Pillay et al., 2021).
Despite its role as a major cause of TB-associated mortality, no studies were identified evaluating biomarkers for TB-induced cardiovascular disease. Similar to other infections (e.g. HIV, sepsis, pneumonia) (Musher et al., 2019), TB-induced cardiovascular disease likely stems from proinflammatory cytokines (e.g. TNF, IL-6, Il1β) that impair endothelial function, resulting in plaque rupture, and vascular occlusion. Infections also induce dyslipidemia (e.g. elevated low density lipoprotein (LDL), triglycerides, and oxidized LDL) (Baluku et al., 2024), warranting investigation into whether these biomarkers can stratify TB patients at risk for cardiovascular events. Future studies should explore the applicability of traditional cardiovascular risk markers (e.g. hemoglobin A1c, BMI) and identify TB-specific pathophysiological mechanistic drivers of cardiovascular disease.
TB increases the risk of lung cancer (SIR 3.0), esophageal cancer (SIR 2.8), hematologic malignancies (SIR 2.1), and lymphoma (SIR 2.3) (Shiels et al., 2015; Luczynski et al., 2022; Moon et al., 2023). However, we identified no studies evaluating biomarkers for predicting post-TB cancer. Existing cancer biomarkers such as CA19, AFP, or CEA should be explored for TB survivors. Non-TB studies demonstrate that chronic inflammation (elevated IL-6 and CRP) is associated with increased cancer risk (Guo et al., 2013; Shiels et al., 2015; Zhao et al., 2021). Future studies should evaluate the role of IL-6 and CRP in risk stratification for TB associated cancer. TB-related mechanisms, such as epigenetic changes, clonal hematopoiesis, fibrosis, cicatrization, scar formation, immune senescence, and infection induced ROS-mediated gene mutations, likely contribute to cancer development (Hormaechea-Agulla et al., 2021). Identifying these mechanisms could guide biomarker discovery for cancer risk in TB survivors.
Certain non-specific biomarkers could potentially predict multiple poor patient-centered outcomes. For example, pre-treatment IL-6 elevations have been associated with in-treatment mortality, relapse risk, and TB-induced lung damage (Gupte et al., 2022; Khan et al., 2024). Similarly, CRP, a general marker of inflammation, has been linked to cardiovascular disease, cancer risk, lung damage, and recurrent infections in non-TB studies. Low QuantIFERON (QFT) mitogen values, a marker of anergy, correlates with slower culture conversion and higher mortality (Nguyen et al., 2018; Huang et al., 2019; Jacquier et al., 2022). Further research is essential to validate these biomarkers and develop comprehensive strategies for improving patient outcomes beyond microbiological cure.
Conclusions and recommendations
Despite achieving microbiological cure through successful antibiotic therapy, TB survivors continue to experience significant morbidity and mortality. This includes elevated risks of all-cause mortality, cardiovascular disease, lung dysfunction, cancer, recurrent infections, and diminished quality of life. These outcomes are often overlooked in TB clinical trials due to a historical over-emphasis on microbial endpoints. Unfortunately, there is not yet robust evidence to recommend specific biomarkers. To address these challenges, we propose that clinical trials include host biomarkers in addition to conventional bacterial markers and prioritize patient-centered clinical outcomes. This approach could facilitate the identification of antibiotic regimens with optimal patient-centered outcomes and identify host-directed therapies that effectively eradicate M. tuberculosis while minimizing inflammation and reducing long-term morbidity and mortality.
Comprehensive assessment of host and mycobacterial factors, including genetics, nutrition, cytokine levels, epigenetics, and metabolism, alongside extended post-treatment follow-up is critical. However, such efforts are often cost prohibitive for individual clinical trials. Lessons can be drawn from large-scale initiatives such as the UK Biobank and The Cancer Genome Atlas (TCGA), which successfully integrate extensive biomarker data with long-term clinical outcomes. The UK Biobank, supported by a public–private partnership, includes a median of 7 years of follow-up linked to robust epidemiological and genetic data. Similarly, the NIH-funded TCGA has compiled multiomic profiles of more than 40 tumor types from over 30,000 patients. Large clinical trial platforms like UNITE4TB could adopt similar models to establish biobanks addressing multifaceted drivers of TB-associated morbidity and mortality while facilitating access for researchers, via innovative funding mechanisms.
The broad spectrum of TB-related morbidity and mortality underscores the need for more comprehensive research. Current evidence on biomarkers predictive of post-TB outcomes in limited, with few studies examining post-TB lung disease and no studies addressing biomarkers of TB-associated cardiovascular disease or cancer. Given this diversity, a suite of biomarkers is likely necessary to stratify TB survivors based on their risk of adverse outcomes.
Drawing inspiration from the cardiovascular field, research should focus on identifying a core set of clinical and laboratory tests capable of formulating practical risk assessments. Widely used cardiovascular risk calculators such as ASCVD, PREVENT, and the Framingham Risk Score are examples of tools that rely on readily available clinical data. As evidence grows, these scores will need to assess risks specific to country, region, age (pediatric, adult, elderly), HIV, viral load, TB disease location (pulmonary versus extrapulmonary or both) and gender. Similarly, TB research could aim to develop analogous tools to predict and mitigate specific types of TB-associated morbidity and mortality.
In addition to advancing antibiotic regimens, large clinical trial platforms have a unique opportunity to close critical knowledge gaps by identifying biomarkers predictive of the large range of TB-associated morbidity and mortality. By doing so, the field can foster a more comprehensive, patient-centered approach to TB care, ultimately improving long-term outcomes for TB survivors.
Author contributions
AD: Writing – original draft, Writing – review & editing. WS: Writing – original draft, Writing – review & editing. SHG: Writing – original draft, Writing – review & editing. SBG: Writing – original draft, Writing – review & editing. NHe: Writing – original draft, Writing – review & editing. NHi: Writing – original draft, Writing – review & editing. ST: Writing – original draft, Writing – review & editing. DL: Writing – original draft, Writing – review & editing. UP: Writing – original draft, Writing – review & editing. CM: Writing – original draft, Writing – review & editing. CL: Writing – original draft, Writing – review & editing. AV: Writing – original draft, Writing – review & editing. RA: Writing – original draft, Writing – review & editing. AM: Writing – original draft, Writing – review & editing. MR: Writing – original draft, Writing – review & editing. RC: Writing – original draft, Writing – review & editing. MK: Writing – original draft, Writing – review & editing. LS: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
Author NHi was employed by the company Otsuka Novel Products GmbH.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frabi.2025.1570989/full#supplementary-material
References
Abhimanyu, Longlax S. C., Nishiguchi T., Ladki M., Sheikh D., Martinez A. L., et al. (2024). TCA metabolism regulates DNA hypermethylation in LPS and Mycobacterium tuberculosis-induced immune tolerance. Proc. Natl. Acad. Sci. United States America. 121, e2404841121. doi: 10.1073/pnas.2404841121
Alexander V., Sindhu K. N., Ralph R., Paul J. S., Manimegalai B., and Zachariah A. (2023). Anergy to purified protein derivative and chronic energy deficiency in sputum-positive pulmonary tuberculosis: Dynamic assessment at baseline and treatment completion. Int. J. Mycobacteriol. 12, 436–442. doi: 10.4103/ijmy.ijmy_176_23
Allwood B. W., Byrne A., Meghji J., Rachow A., van der Zalm M. M., and Schoch O. D. (2021). Post-tuberculosis lung disease: clinical review of an under-recognised global challenge. Respiration 100, 751–763. doi: 10.1159/000512531
Allwood B. W., Maasdorp E., Kim G. J., Cooper C. B., Goldin J., van Zyl-Smit R. N., et al. (2020). Transition from restrictive to obstructive lung function impairment during treatment and follow-up of active tuberculosis. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 1039–1047. doi: 10.2147/COPD.S219731
Alvarez-Uria G., Midde M., Pakam R., and Naik P. K. (2013). Diagnostic and prognostic value of serum albumin for tuberculosis in HIV infected patients eligible for antiretroviral therapy: datafrom an HIV cohort study in India. Bioimpacts 3, 123–128. doi: 10.5681/bi.2013.025
Auld S. C., Barczak A. K., Bishai W., Coussens A. K., Dewi I. M. W., Mitini-Nkhoma S. C., et al. (2024). Pathogenesis of post-tuberculosis lung disease: defining knowledge gaps and research priorities at the second international post-tuberculosis symposium. Am. J. respiratory Crit. Care med 210, 979–993. doi: 10.1164/rccm.202402-0374SO
Auld S. C., Click E. S., Heilig C. M., Miramontes R., Cain K. P., Bisson G. P., et al. (2013). Tuberculin skin test result and risk of death among persons with active TB. PloS One 8, e78779. doi: 10.1371/journal.pone.0078779
Azam K., Khosa C., Viegas S., Massango I., Bhatt N., Jani I., et al. (2022). Reduction of blood C-reactive protein concentration complements the resolution of sputum bacillary load in patients on anti-tuberculosis therapy. Front. Immunol. 13. doi: 10.3389/fimmu.2022.1005692
Bagcchi S. (2023). WHO’s global tuberculosis report 2022. Lancet Microbe 4, e20. doi: 10.1016/S2666-5247(22)00359-7
Baik Y., Maenetje P., Schramm D., Tiemessen C., Ncube I., Churchyard G., et al. (2023). Lung function and collagen 1a levels are associated with changes in 6 min walk test distance during treatment of TB among HIV-infected adults: a prospective cohort study. BMC Pulm. Med. 23, 53. doi: 10.1186/s12890-023-02325-7
Baker M. A., Harries A. D., Jeon C. Y., Hart J. E., Kapur A., Lonnroth K., et al. (2011). The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med. 9, 81. doi: 10.1186/1741-7015-9-81
Baluku J. B., Nalwanga R., Kazibwe A., Olum R., Nuwagira E., Mugenyi N., et al. (2024). Association between biomarkers of inflammation and dyslipidemia in drug resistant tuberculosis in Uganda. Lipids Health Dis. 23, 65. doi: 10.1186/s12944-024-02063-7
Barber D. L., Mayer-Barber K. D., Feng C. G., Sharpe A. H., and Sher A. (2011). CD4 T cells promote rather than control tuberculosis in the absence of PD-1-mediated inhibition. J. Immunol. 186, 1598–1607. doi: 10.4049/jimmunol.1003304
Bekker L. G., Maartens G., Steyn L., and Kaplan G. (1998). Selective increase in plasma tumor necrosis factor-alpha and concomitant clinical deterioration after initiating therapy in patients with severe tuberculosis. J. Infect. dis 178, 580–584. doi: 10.1086/517479
Bobak C. A., Abhimanyu, Natarajan H., Gandhi T., Grimm S. L., Nishiguchi T., et al. (2022). Increased DNA methylation, cellular senescence and premature epigenetic aging in Guinea pigs and humans with tuberculosis. Aging (Albany NY) 14, 2174–2193. doi: 10.18632/aging.203936
Boussiotis V. A., Tsai E. Y., Yunis E. J., Thim S., Delgado J. C., Dascher C. C., et al. (2000). IL-10-producing T cells suppress immune responses in anergic tuberculosis patients. J. Clin. investig 105, 1317–1325. doi: 10.1172/JCI9918
Breen R. A., Smith C. J., Bettinson H., Dart S., Bannister B., Johnson M. A., et al. (2004). Paradoxical reactions during tuberculosis treatment in patients with and without HIV co-infection. Thorax 59, 704–707. doi: 10.1136/thx.2003.019224
Canetti G. (1955). The Tubercle Bacillus in the Pulmonary Lesion of Man (New York: Springer Publishing Company).
Chahed H., Hachicha H., Berriche A., Abdelmalek R., Mediouni A., Kilani B., et al. (2017). Paradoxical reaction associated with cervical lymph node tuberculosis: predictive factors and therapeutic management. Int. J. Infect. Dis. 54, 4–7. doi: 10.1016/j.ijid.2016.10.025
Cheng V. C., Ho P. L., Lee R. A., Chan K. S., Chan K. K., Woo P. C., et al. (2002). Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur. J. Clin. Microbiol Infect. Dis. 21, 803–809. doi: 10.1007/s10096-002-0821-2
Christensen A. S., Andersen A. B., Thomsen V. O., Andersen P. H., and Johansen I. S. (2011). Tuberculous meningitis in Denmark: a review of 50 cases. BMC Infect. dis 11, 47. doi: 10.1186/1471-2334-11-47
Christine T., Tarigan A. P., and Ananda F. R. (2019). The correlation between levels of transforming growth factor-beta with pulmonary fibrosis in post pulmonary tuberculosis in Medan, North Sumatera - Indonesia. Open Access Maced J. Med. Sci. 7, 2075–2078. doi: 10.3889/oamjms.2019.544
Chung W. S., Lin C. L., Hung C. T., Chu Y. H., Sung F. C., Kao C. H., et al. (2014). Tuberculosis increases the subsequent risk of acute coronary syndrome: a nationwide population-based cohort study. Int. J. tubercul Lung Dis. 18, 79–83. doi: 10.5588/ijtld.13.0288
Colangeli R., Jedrey H., Kim S., Connell R., Ma S., Chippada Venkata U. D., et al. (2018). Bacterial factors that predict relapse after tuberculosis therapy. New Engl. J. med 379, 823–833. doi: 10.1056/NEJMoa1715849
Critchley J. A., Limb E. S., Khakharia A., Carey I. M., Auld S. C., DeWilde S., et al. (2024). Tuberculosis and increased incidence of cardiovascular disease: Cohort study using US and UK health records. Clin. Infect. Dis. doi: 10.1093/cid/ciae538
Delgado J. C., Tsai E. Y., Thim S., Baena A., Boussiotis V. A., Reynes J. M., et al. (2002). Antigen-specific and persistent tuberculin anergy in a cohort of pulmonary tuberculosis patients from rural Cambodia. Proc. Natl. Acad. Sci. United States America. 99, 7576–7581. doi: 10.1073/pnas.062056099
de Melo M. G. M., Mesquita E. D. D., Oliveira M. M., da Silva-Monteiro C., Silveira A. K. A., Malaquias T. S., et al. (2018). Imbalance of NET and alpha-1-antitrypsin in tuberculosis patients is related with hyper inflammation and severe lung tissue damage. Front. Immunol. 9. doi: 10.3389/fimmu.2018.03147
DiNardo A. R., Gandhi T., Heyckendorf J., Grimm S. L., Rajapakshe K., Nishiguchi T., et al. (2022). Gene expression signatures identify biologically and clinically distinct tuberculosis endotypes. Eur. respiratory J. 40. doi: 10.1183/13993003.02263-2021
DiNardo A. R., Nishiguchi T., Grimm S. L., Schlesinger L. S., Graviss E. A., Cirillo J. D., et al. (2021). Tuberculosis endotypes to guide stratified host-directed therapy. Med. (N Y) 2, 217–232. doi: 10.1016/j.medj.2020.11.003
DiNardo A. R., Rajapakshe K., Nishiguchi T., Grimm S. L., Mtetwa G., Dlamini Q., et al. (2020). DNA hypermethylation during tuberculosis dampens host immune responsiveness. J. Clin. investig 130, 3113–3123. doi: 10.1172/JCI134622
Ehtesham N. Z., Nasiruddin M., Alvi A., Kumar B. K., Ahmed N., Peri S., et al. (2011). Treatment end point determinants for pulmonary tuberculosis: human resistin as a surrogate biomarker. Tuberculosis 91, 293–299. doi: 10.1016/j.tube.2011.04.007
Emerging Risk Factors C., Kaptoge S., Di Angelantonio E., Lowe G., Pepys M. B., Thompson S. G., et al. (2010). C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet 375, 132–140. doi: 10.1016/S0140-6736(09)61717-7
Everett B. M., MacFadyen J. G., Thuren T., Libby P., Glynn R. J., and Ridker P. M. (2020). Inhibition of interleukin-1beta and reduction in atherothrombotic cardiovascular events in the CANTOS trial. J. Am. Coll. Cardiol. 76, 1660–1670. doi: 10.1016/j.jacc.2020.08.011
Fox G. J., Nguyen V. N., Dinh N. S., Nghiem L. P. H., Le T. N. A., Nguyen T. A., et al. (2019). Post-treatment mortality among patients with tuberculosis: A prospective cohort study of 10–964 patients in Vietnam. Clin. Infect. Dis. 68, 1359–1366. doi: 10.1093/cid/ciy665
Gillespie S. H., Crook A. M., McHugh T. D., Mendel C. M., Meredith S. K., Murray S. R., et al. (2014). Four-month moxifloxacin-based regimens for drug-sensitive tuberculosis. New Engl. J. med 371, 1577–1587. doi: 10.1056/NEJMoa1407426
Gillespie S. H., DiNardo A. R., Georghiou S. B., Sabiiti W., Kohli M., Panzner U., et al. (2024). Developing biomarker assays to accelerate tuberculosis drug development: defining target product profiles. Lancet Microbe. 5 (9). doi: 10.1016/S2666-5247(24)00085-5
Global Tuberculosis Pragramme W (2024). Global Tuberculosis report 20242024. Available online at: https://www.who.int/publications/i/item/9789240101531 (Accessed January 2, 2025).
Green D. L., Keenan K., Fredricks K. J., Huque S. I., Mushi M. F., Kansiime C., et al. (2023). The role of multidimensional poverty in antibiotic misuse: a mixed-methods study of self-medication and non-adherence in Kenya, Tanzania, and Uganda. Lancet Global Health 11, e59–e68. doi: 10.1016/S2214-109X(22)00423-5
Guo Y. Z., Pan L., Du C. J., Ren D. Q., and Xie X. M. (2013). Association between C-reactive protein and risk of cancer: a meta-analysis of prospective cohort studies. Asian Pac J. Cancer Prev. 14, 243–248. doi: 10.7314/apjcp.2013.14.1.243
Gupte A. N., Kumar P., Araujo-Pereira M., Kulkarni V., Paradkar M., Pradhan N., et al. (2022). Baseline IL-6 is a biomarker for unfavourable tuberculosis treatment outcomes: a multisite discovery and validation study. Eur. respiratory J. 59. doi: 10.1183/13993003.00905-2021
Guzman-Beltran S., Carreto-Binaghi L. E., Carranza C., Torres M., Gonzalez Y., Munoz-Torrico M., et al. (2021). Oxidative stress and inflammatory mediators in exhaled breath condensate of patients with pulmonary tuberculosis. A pilot study with a biomarker perspective. Antioxid. (Basel). 10. doi: 10.3390/antiox10101572
Hawkey C. R., Yap T., Pereira J., Moore D. A., Davidson R. N., Pasvol G., et al. (2005). Characterization and management of paradoxical upgrading reactions in HIV-uninfected patients with lymph node tuberculosis. Clin. Infect. Dis. 40, 1368–1371. doi: 10.1086/429317
Hermans S. M., Akkerman O. W., Meintjes G., and Grobusch M. P. (2024). Post-tuberculosis treatment paradoxical reactions. Infection 52, 2083–2095. doi: 10.1007/s15010-024-02310-0
Honjo K., Komiya K., Kan T., Uchida S., Goto A., Takikawa S., et al. (2020). The impact of performance status on tuberculosis-related death among elderly patients with lung tuberculosis: A competing risk regression analysis. J. Infect. Chemother. 26, 69–75. doi: 10.1016/j.jiac.2019.07.008
Hormaechea-Agulla D., Matatall K. A., Le D. T., Kain B., Long X., Kus P., et al. (2021). Chronic infection drives Dnmt3a-loss-of-function clonal hematopoiesis via IFNgamma signaling. Cell Stem Cell. 28, 1428–42 e6. doi: 10.1016/j.stem.2021.03.002
Horne D. J., Royce S. E., Gooze L., Narita M., Hopewell P. C., Nahid P., et al. (2010). Sputum monitoring during tuberculosis treatment for predicting outcome: systematic review and meta-analysis. Lancet Infect. dis 10, 387–394. doi: 10.1016/S1473-3099(10)70071-2
Howard N. C., Marin N. D., Ahmed M., Rosa B. A., Martin J., Bambouskova M., et al. (2018). Mycobacterium tuberculosis carrying a rifampicin drug resistance mutation reprograms macrophage metabolism through cell wall lipid changes. Nat. Microbiol. 3, 1099–1108. doi: 10.1038/s41564-018-0245-0
Huaman M. A., Henson D., Ticona E., Sterling T. R., and Garvy B. A. (2015). Tuberculosis and cardiovascular disease: linking the epidemics. Trop. Dis. Travel Med. Vaccines. 1. doi: 10.1186/s40794-015-0014-5
Huang C. T., Lee M. R., Ruan S. Y., Tsai Y. J., Wang J. Y., and Yu C. J. (2019). Prognostic value of the mitogen response in the interferon-gamma release assay in patients with culture-confirmed tuberculosis. Respir. Med. 158, 49–54. doi: 10.1016/j.rmed.2019.10.004
Isanaka S., Mugusi F., Urassa W., Willett W. C., Bosch R. J., Villamor E., et al. (2012). Iron deficiency and anemia predict mortality in patients with tuberculosis. J. Nutr. 142, 350–357. doi: 10.3945/jn.111.144287
Ivanova O., Hoffmann V. S., Lange C., Hoelscher M., and Rachow A. (2023). Post-tuberculosis lung impairment: systematic review and meta-analysis of spirometry data from 14–621 people. Eur. Respir. Rev. 32. doi: 10.1183/16000617.0221-2022
Jacquier M., Binquet C., Manoha C., Audia S., Simonet-Lamm A. L., Casenaz A., et al. (2022). Beyond quantiFERON-TB results, the added value of a weak mitogen response. Front. Med. (Lausanne). 9. doi: 10.3389/fmed.2022.876864
Jeong Y. J., Park J. S., Kim H. W., Min J., Ko Y., Oh J. Y., et al. (2023). Deaths from tuberculosis: differences between tuberculosis-related and non-tuberculosis-related deaths. Front. Public Health 11. doi: 10.3389/fpubh.2023.1207284
Khan M. S., Talha K. M., Maqsood M. H., Rymer J. A., Borlaug B. A., Docherty K. F., et al. (2024). Interleukin-6 and cardiovascular events in healthy adults: MESA. JACC Adv. 3, 101063. doi: 10.1016/j.jacadv.2024.101063
Khosa C., Bhatt N., Massango I., Azam K., Saathoff E., Bakuli A., et al. (2020). Development of chronic lung impairment in Mozambican TB patients and associated risks. BMC Pulm. Med. 20, 127. doi: 10.1186/s12890-020-1167-1
Kim D. J., Oh J. Y., Rhee C. K., Park S. J., Shim J. J., and Cho J. Y. (2021). Metabolic fingerprinting uncovers the distinction between the phenotypes of tuberculosis associated COPD and smoking-induced COPD. Front. Med. (Lausanne). 8. doi: 10.3389/fmed.2021.619077
Kumar N. P., Moideen K., Viswanathan V., Sivakumar S., Ahamed S. F., Ponnuraja C., et al. (2022). Heightened microbial translocation is a prognostic biomarker of recurrent tuberculosis. Clin. Infect. Dis. 75, 1820–1826. doi: 10.1093/cid/ciac236
Kumar N. P., Nancy A., Viswanathan V., Sivakumar S., Thiruvengadam K., Ahamed S. F., et al. (2023). Chitinase and indoleamine 2, 3-dioxygenase are prognostic biomarkers for unfavorable treatment outcomes in pulmonary tuberculosis. Front. Immunol. 14. doi: 10.3389/fimmu.2023.1093640
Kurver L., Seers T., van Dorp S., van Crevel R., Pollara G., and van Laarhoven A. (2024). Tuberculosis-associated hemophagocytic lymphohistiocytosis: diagnostic challenges and determinants of outcome. Open Forum Infect. Dis. 11, ofad697. doi: 10.1093/ofid/ofad697
Lasco T. M., Cassone L., Kamohara H., Yoshimura T., and McMurray D. N. (2005). Evaluating the role of tumor necrosis factor-alpha in experimental pulmonary tuberculosis in the Guinea pig. Tuberculosis 85, 245–258. doi: 10.1016/j.tube.2005.01.001
Laxmeshwar C., Stewart A. G., Dalal A., Kumar A. M. V., Kalaiselvi S., Das M., et al. (2019). Beyond ‘cure’ and ‘treatment success’: quality of life of patients with multidrug-resistant tuberculosis. Int. J. tubercul Lung Dis. 23, 73–81. doi: 10.5588/ijtld.18.0149
Lee-Rodriguez C., Wada P. Y., Hung Y. Y., and Skarbinski J. (2020). Association of mortality and years of potential life lost with active tuberculosis in the United States. JAMA Netw. Open 3, e2014481. doi: 10.1001/jamanetworkopen.2020.14481
Linh N. N., Viney K., Gegia M., Falzon D., Glaziou P., Floyd K., et al. (2021). World Health Organization treatment outcome definitions for tuberculosis: 2021 update. Eur. respiratory J. 58. doi: 10.1183/13993003.00804-2021
Luczynski P., Poulin P., Romanowski K., and Johnston J. C. (2022). Tuberculosis and risk of cancer: A systematic review and meta-analysis. PloS One 17, e0278661. doi: 10.1371/journal.pone.0278661
Maenetje P., Baik Y., Schramm D. B., Vangu M. D. W., Wallis R. S., Mlotshwa M., et al. (2024). Circulating biomarkers, fraction of exhaled nitric oxide, and lung function in patients with human immunodeficiency virus and tuberculosis. J. Infect. dis 229, 824–832. doi: 10.1093/infdis/jiad232
Magombedze G., Pasipanodya J. G., and Gumbo T. (2021). Bacterial load slopes represent biomarkers of tuberculosis therapy success, failure, and relapse. Commun. Biol. 4, 664. doi: 10.1038/s42003-021-02184-0
Malefane L. and Maarman G. (2024). Post-tuberculosis lung disease and inflammatory role players: can we characterise the myriad inflammatory pathways involved to gain a better understanding? Chem. Biol. Interact. 387, 110817. doi: 10.1016/j.cbi.2023.110817
Malherbe S. T., Shenai S., Ronacher K., Loxton A. G., Dolganov G., Kriel M., et al. (2016). Persisting positron emission tomography lesion activity and Mycobacterium tuberculosis mRNA after tuberculosis cure. Nat. med 22, 1094–1100. doi: 10.1038/nm.4177
McHenry M. L., Bartlett J., Igo R. P., Wampande E., Benchek P., Mayanja-Kizza H., et al. (2019). Interaction between host genes and M. tuberculosis lineage can affect tuberculosis severity: evidence for coevolution. bioRxiv, 769448. doi: 10.1101/769448
Meghji J., Lesosky M., Joekes E., Banda P., Rylance J., Gordon S., et al. (2020). Patient outcomes associated with post-tuberculosis lung damage in Malawi: a prospective cohort study. Thorax 75, 269–278. doi: 10.1136/thoraxjnl-2019-213808
Meintjes G., Stek C., Blumenthal L., Thienemann F., Schutz C., Buyze J., et al. (2018). Prednisone for the prevention of paradoxical tuberculosis-associated IRIS. New Engl. J. med 379, 1915–1925. doi: 10.1056/NEJMoa1800762
Meintjes G., Wilkinson R. J., Morroni C., Pepper D. J., Rebe K., Rangaka M. X., et al. (2010). Randomized placebo-controlled trial of prednisone for paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome. Aids 24, 2381–2390. doi: 10.1097/QAD.0b013e32833dfc68
Menon S., Rossi R., Dusabimana A., Zdraveska N., Bhattacharyya S., and Francis J. (2020). The epidemiology of tuberculosis-associated hyperglycemia in individuals newly screened for type 2 diabetes mellitus: systematic review and meta-analysis. BMC Infect. dis 20, 937. doi: 10.1186/s12879-020-05512-7
Menzies N. A., Quaife M., Allwood B. W., Byrne A. L., Coussens A. K., Harries A. D., et al. (2021). Lifetime burden of disease due to incident tuberculosis: a global reappraisal including post-tuberculosis sequelae. Lancet Global Health 9, e1679–e1e87. doi: 10.1016/S2214-109X(21)00367-3
Messah A. D. V., Darmiati S., Rumende C. M., Soemarwoto R. A., Prihartono J., and Asmarinah A. (2024). Correlation between Gene polymorphism levels of serum matrix metalloproteinases with cavitary features and pulmonary fibrosis of the Patient tuberculosis multi-drug resistance using high-resolution computerized tomography of the Thorax. Heliyon 10, e33671. doi: 10.1016/j.heliyon.2024.e33671
Moon S. M., Choi H., Kim S. H., Kang H. K., Park D. W., Jung J. H., et al. (2023). Increased lung cancer risk and associated risk factors in tuberculosis survivors: A Korean population-based study. Clin. Infect. Dis. 77, 1329–1339. doi: 10.1093/cid/ciad373
Mosquera-Restrepo S. F., Zuberogoitia S., Gouxette L., Layre E., Gilleron M., Stella A., et al. (2022). A Mycobacterium tuberculosis fingerprint in human breath allows tuberculosis detection. Nat. Commun. 13, 7751. doi: 10.1038/s41467-022-35453-5
Mpagama S. G., Msaji K. S., Kaswaga O., Zurba L. J., Mbelele P. M., Allwood B. W., et al. (2021). The burden and determinants of post-TB lung disease. Int. J. tubercul Lung Dis. 25, 846–853. doi: 10.5588/ijtld.21.0278
Muniyandi M., Rajeswari R., Balasubramanian R., Nirupa C., Gopi P. G., Jaggarajamma K., et al. (2007). Evaluation of post-treatment health-related quality of life (HRQoL) among tuberculosis patients. Int. J. tubercul Lung Dis. 11, 887–892.
Musher D. M., Abers M. S., and Corrales-Medina V. F. (2019). Acute infection and myocardial infarction. New Engl. J. med 380, 171–176. doi: 10.1056/NEJMra1808137
Mutavhatsindi H., Manyelo C. M., Snyders C. I., Van Rensburg I., Kidd M., Stanley K., et al. (2024). Baseline and end-of-treatment host serum biomarkers predict relapse in adults with pulmonary tuberculosis. J. infect. 89, 106173. doi: 10.1016/j.jinf.2024.106173
Nair S., Huynh J. P., Lampropoulou V., Loginicheva E., Esaulova E., Gounder A. P., et al. (2018). Irg1 expression in myeloid cells prevents immunopathology during M. tuberculosis infection. J. Exp. med 215, 1035–1045. doi: 10.1084/jem.20180118
Nguyen D. T., Teeter L. D., Graves J., and Graviss E. A. (2018). Characteristics associated with negative interferon-gamma release assay results in culture-confirmed tuberculosis patients, Texas, USA, 2013-2015. Emerg. Infect. Dis. 24, 534–540. doi: 10.3201/eid2403.171633
Ntinginya N. E., Bakuli A., Mapamba D., Sabiiti W., Kibiki G., Minja L. T., et al. (2023). Tuberculosis molecular bacterial load assay reveals early delayed bacterial killing in patients with relapse. Clin. Infect. Dis. 76, e990–e9e4. doi: 10.1093/cid/ciac445
Odia T., Malherbe S. T., Meier S., Maasdorp E., Kleynhans L., du Plessis N., et al. (2020). The peripheral blood transcriptome is correlated with PET measures of lung inflammation during successful tuberculosis treatment. Front. Immunol. 11. doi: 10.3389/fimmu.2020.596173
Okamura K., Nagata N., Wakamatsu K., Yonemoto K., Ikegame S., Kajiki A., et al. (2013). Hypoalbuminemia and lymphocytopenia are predictive risk factors for in-hospital mortality in patients with tuberculosis. Intern. Med. 52, 439–444. doi: 10.2169/internalmedicine.52.8158
Padmapriydarsini C., Mamulwar M., Mohan A., Shanmugam P., Gomathy N. S., Mane A., et al. (2021). Randomized trial of Metformin with Anti-tuberculosis drugs For Early Sputum Conversion in Adults with Pulmonary Tuberculosis. Clin. Infect. Dis. doi: 10.1093/cid/ciab964
Phillips P. P., Mendel C. M., Burger D. A., Crook A. M., Nunn A. J., Dawson R., et al. (2016). Erratum to: Limited role of culture conversion for decision-making in individual patient care and for advancing novel regimens to confirmatory clinical trials. BMC Med. 14, 36. doi: 10.1186/s12916-016-0585-7
Pillay K., Lewis L., Rambaran S., Yende-Zuma N., Archary D., Gengiah S., et al. (2021). Plasma biomarkers of risk of tuberculosis recurrence in HIV co-infected patients from South Africa. Front. Immunol. 12. doi: 10.3389/fimmu.2021.631094
Plit M. L., Anderson R., Van Rensburg C. E., Page-Shipp L., Blott J. A., Fresen J. L., et al. (1998). Influence of antimicrobial chemotherapy on spirometric parameters and pro-inflammatory indices in severe pulmonary tuberculosis. Eur. respiratory J. 12, 351–356. doi: 10.1183/09031936.98.12020351
Ravimohan S., Kornfeld H., Weissman D., and Bisson G. P. (2018). Tuberculosis and lung damage: from epidemiology to pathophysiology. Eur. Respir. Rev. 27. doi: 10.1183/16000617.0077-2017
Ravimohan S., Maenetje P., Auld S. C., Ncube I., Mlotshwa M., Chase W., et al. (2020). A common NLRC4 gene variant associates with inflammation and pulmonary function in human immunodeficiency virus and tuberculosis. Clin. Infect. Dis. 71, 924–932. doi: 10.1093/cid/ciz898
Romanowski K., Baumann B., Basham C. A., Ahmad Khan F., Fox G. J., and Johnston J. C. (2019). Long-term all-cause mortality in people treated for tuberculosis: a systematic review and meta-analysis. Lancet Infect. dis 19, 1129–1137. doi: 10.1016/S1473-3099(19)30309-3
Sahiratmadja E., Alisjahbana B., de Boer T., Adnan I., Maya A., Danusantoso H., et al. (2007). Dynamic changes in pro- and anti-inflammatory cytokine profiles and gamma interferon receptor signaling integrity correlate with tuberculosis disease activity and response to curative treatment. Infect. immun. 75, 820–829. doi: 10.1128/IAI.00602-06
Salindri A. D., Auld S. C., Schechter M. C., Gandhi N. R., and Magee M. J. (2019a). Negative tuberculin skin test result predicts all-cause mortality among tuberculosis patients with HIV and diabetes comorbidity. Ann. Epidemiol. 33, 72–8 e4. doi: 10.1016/j.annepidem.2019.02.005
Salindri A. D., Wang J. Y., Lin H. H., and Magee M. J. (2019b). Post-tuberculosis incidence of diabetes, myocardial infarction, and stroke: Retrospective cohort analysis of patients formerly treated for tuberculosis in Taiwan, 2002-2013. Int. J. Infect. Dis. 84, 127–130. doi: 10.1016/j.ijid.2019.05.015
Shanmugasundaram K., Talwar A., Madan K., and Bade G. (2022). Pulmonary functions and inflammatory biomarkers in post-pulmonary tuberculosis sequelae. Tuberc. Respir. Dis. (Seoul). 85, 175–184. doi: 10.4046/trd.2021.0127
Shiels M. S., Katki H. A., Hildesheim A., Pfeiffer R. M., Engels E. A., Williams M., et al. (2015). Circulating inflammation markers, risk of lung cancer, and utility for risk stratification. J. Natl. Cancer Inst. 107. doi: 10.1093/jnci/djv199
Soria J., Chiappe A., Gallardo J., Zunt J. R., and Lescano A. G. (2021). Tuberculous meningitis: impact of timing of treatment initiation on mortality. Open Forum Infect. Dis. 8, ofab345. doi: 10.1093/ofid/ofab345
Sterling T. R., Zhao Z., Khan A., Chaisson R. E., Schluger N., Mangura B., et al. (2006). Mortality in a large tuberculosis treatment trial: modifiable and non-modifiable risk factors. Int. J. tubercul Lung Dis. 10, 542–549.
Straetemans M., Glaziou P., Bierrenbach A. L., Sismanidis C., and van der Werf M. J. (2011). Assessing tuberculosis case fatality ratio: a meta-analysis. PloS One 6, e20755. doi: 10.1371/journal.pone.0020755
Tervi A., Junna N., Broberg M., Jones S. E., FinnGen, Strausz S., et al. (2023). Large registry-based analysis of genetic predisposition to tuberculosis identifies genetic risk factors at HLA. Hum. Mol. Genet. 32, 161–171. doi: 10.1093/hmg/ddac212
Tian G., Mi J., Wei X., Zhao D., Qiao L., Yang C., et al. (2015). Circulating interleukin-6 and cancer: A meta-analysis using Mendelian randomization. Sci. Rep. 5, 11394. doi: 10.1038/srep11394
Tsao T. C., Hong J., Li L. F., Hsieh M. J., Liao S. K., and Chang K. S. (2000). Imbalances between tumor necrosis factor-alpha and its soluble receptor forms, and interleukin-1beta and interleukin-1 receptor antagonist in BAL fluid of cavitary pulmonary tuberculosis. Chest 117, 103–109. doi: 10.1378/chest.117.1.103
van Heerden J. K., Louw E. H., Thienemann F., Engel M. E., and Allwood B. W. (2024). The prevalence of pulmonary hypertension in post-tuberculosis and active tuberculosis populations: a systematic review and meta-analysis. Eur. Respir. Rev. 33. doi: 10.1183/16000617.0154-2023
VanValkenburg A., Kaipilyawar V., Sarkar S., Lakshminarayanan S., Cintron C., Prakash Babu S., et al. (2022). Malnutrition leads to increased inflammation and expression of tuberculosis risk signatures in recently exposed household contacts of pulmonary tuberculosis. Front. Immunol. 13. doi: 10.3389/fimmu.2022.1011166
Vega V., Cabrera-Sanchez J., Rodriguez S., Verdonck K., Seas C., Otero L., et al. (2024). Risk factors for pulmonary tuberculosis recurrence, relapse and reinfection: a systematic review and meta-analysis. BMJ Open Respir. Res. 11. doi: 10.1136/bmjresp-2023-002281
Vega V., Rodriguez S., van der Stuyft P., Seas C., and Otero L. (2021). Recurrent TB: a systematic review and meta-analysis of the incidence rates and the proportions of relapses and reinfections. Thorax 76, 494–502. doi: 10.1136/thoraxjnl-2020-215449
Via L. E., Weiner D. M., Schimel D., Lin P. L., Dayao E., Tankersley S. L., et al. (2013). Differential virulence and disease progression following Mycobacterium tuberculosis complex infection of the common marmoset (Callithrix jacchus). Infect. immun. 81, 2909–2919. doi: 10.1128/IAI.00632-13
Walker N. F., Schutz C., Ward A., Barr D., Opondo C., Shey M., et al. (2024). Elevated plasma matrix metalloproteinases are associated with mycobacterium tuberculosis bloodstream infection and mortality in human immunodeficiency virus-associated tuberculosis. J. Infect. Dis. doi: 10.1093/infdis/jiae296
Wallis R. S., Ginindza S., Beattie T., Arjun N., Likoti M., Sebe M., et al. (2022). Lung and blood early biomarkers for host-directed tuberculosis therapies: Secondary outcome measures from a randomized controlled trial. PloS One 17, e0252097. doi: 10.1371/journal.pone.0252097
Wang C. H., Lin H. C., Lin S. M., Huang C. D., Liu C. Y., Huang K. H., et al. (2010). MMP-1(-1607G) polymorphism as a risk factor for fibrosis after pulmonary tuberculosis in Taiwan. Int. J. tubercul Lung Dis. 14, 627–634.
Wilson D., Moosa M. S., Cohen T., Cudahy P., Aldous C., and Maartens G. (2018). Evaluation of tuberculosis treatment response with serial C-reactive protein measurements. Open Forum Infect. Dis. 5, ofy253. doi: 10.1093/ofid/ofy253
Wu C. Y., Hu H. Y., Pu C. Y., Huang N., Shen H. C., Li C. P., et al. (2011). Pulmonary tuberculosis increases the risk of lung cancer: a population-based cohort study. Cancer 117, 618–624. doi: 10.1002/cncr.25616
Yang J., Kim S. H., Sim J. K., Gu S., Seok J. W., Bae D. H., et al. (2024). Tuberculosis survivors and the risk of cardiovascular disease: analysis using a nationwide survey in Korea. Front. Cardiovasc. Med. 11. doi: 10.3389/fcvm.2024.1364337
Zentner I., Back H. M., Kagan L., Subbian S., Nagajyothi J., Srivastava S., et al. (2020). Redox imbalance and oxidative DNA damage during isoniazid treatment of HIV-associated tuberculosis: A clinical and translational pharmacokinetic study. Front. Pharmacol. 11. doi: 10.3389/fphar.2020.01103
Keywords: tuberculosis, biomarker, cardiovascular, sequelae, cancer
Citation: DiNardo AR, Sabiiti W, Gillespie SH, Georghiou SB, Heinrich N, Hittel N, Taghlabi S, Carrero Longlax D, Kohli M, Panzner U, Musia C, Lange C, Vasiliu A, Arts RJW, Mandalakas AM, Ruhwald M, Stuyver LJ and van Crevel R (2025) Inclusion of patient-centered, non-microbiological endpoints and biomarkers in tuberculosis drug trials. Front. Antibiot. 4:1570989. doi: 10.3389/frabi.2025.1570989
Received: 04 February 2025; Accepted: 09 April 2025;
Published: 22 May 2025.
Edited by:
Carlo Pallotto, Hospital of Santa Maria della Misericordia in Perugia, ItalyReviewed by:
Anna Gidari, University of Perugia, ItalyJunaid Shaik, Durban University of Technology, South Africa
Copyright © 2025 DiNardo, Sabiiti, Gillespie, Georghiou, Heinrich, Hittel, Taghlabi, Carrero Longlax, Kohli, Panzner, Musia, Lange, Vasiliu, Arts, Mandalakas, Ruhwald, Stuyver and van Crevel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrew R. DiNardo, YW5kcmV3LmRpbmFyZG9AYmNtLmVkdQ==
 Andrew R. DiNardo
Andrew R. DiNardo Wilbert Sabiiti
Wilbert Sabiiti Stephen H. Gillespie
Stephen H. Gillespie Sophia B. Georghiou4
Sophia B. Georghiou4 Norbert Heinrich
Norbert Heinrich Danna Carrero Longlax
Danna Carrero Longlax Mikashmi Kohli
Mikashmi Kohli Christoph Lange
Christoph Lange Anca Vasiliu
Anca Vasiliu Rob J. W. Arts
Rob J. W. Arts Anna M. Mandalakas
Anna M. Mandalakas Lieven J. Stuyver
Lieven J. Stuyver Reinout van Crevel
Reinout van Crevel