- 1Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 2Department of Health Policy and Management, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 3Department of Implementation Science, Wake Forest University School of Medicine, Winston-Salem, NC, United States
- 4Wake Forest Baptist Comprehensive Cancer Center, Winston-Salem, NC, United States
- 5Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
Background: Lessening the Impact of Financial Toxicity (LIFT) is an intervention designed to address financial toxicity (FT) and improve cancer care access and outcomes through financial navigation (FN). FN identifies patients at risk for FT, assesses eligibility for financial support, and develops strategies to cope with those costs. LIFT successfully reduced FT and improved care access in a preliminary study among patients with high levels of FT in a single large academic cancer center. Adapting LIFT requires distinguishing between core functions (components that are key to its implementation and effectiveness) and forms (specific activities that carry out core functions). Our objective was to complete the first stage of adaptation, identifying LIFT core functions.
Methods: We reviewed LIFT's protocol and internal standard-operating procedures. We then conducted 45–90 min in-depth interviews, using Kirk's method of identifying core functions, with key LIFT staff (N = 8), including the principal investigators. Interviews focused on participant roles and intervention implementation. Recorded interviews were transcribed verbatim. Using ATLAS.ti and a codebook based on the Model for Adaptation Design and Impact, we coded interview transcripts. Through thematic analysis, we then identified themes related to LIFT's intervention and implementation core functions. Two report back sessions with interview participants were incorporated to further refine themes.
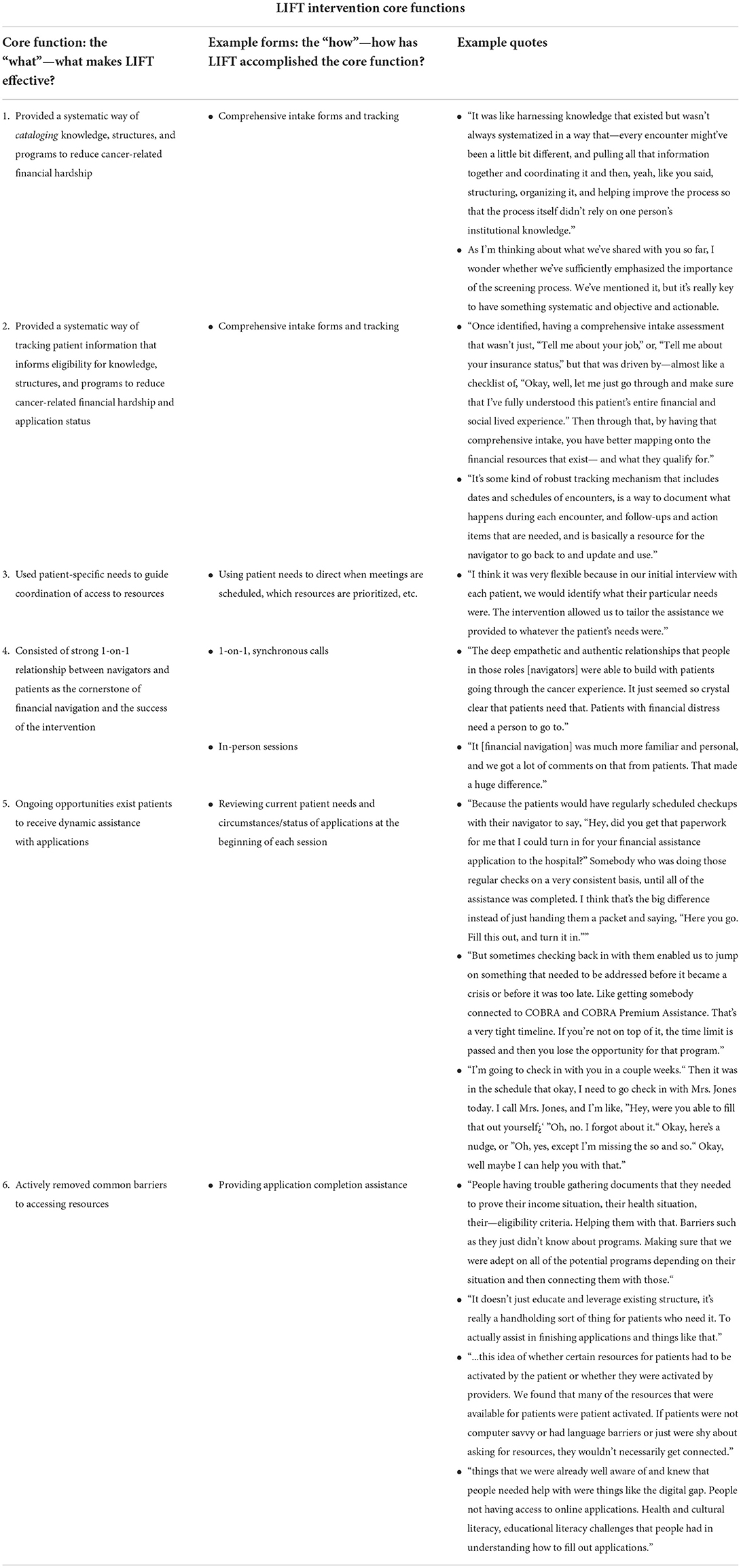
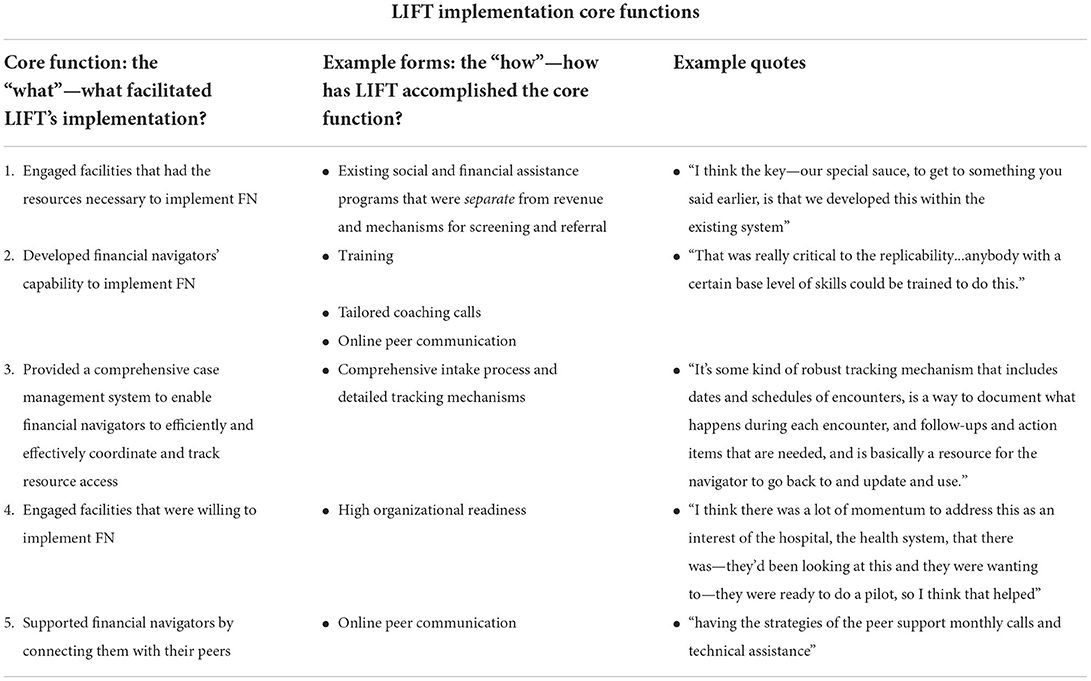
Results: Six intervention core functions (i.e., what makes LIFT effective) and five implementation core functions (i.e., what facilitated LIFT's implementation) were identified to be sufficient to reduce FT. Intervention core functions included systematically cataloging knowledge and tracking patient-specific information related to eligibility criteria for FT relief. Repeat contacts between the financial navigator and participant created an ongoing relationship, removing common barriers to accessing resources. Implementation core functions included having engaged sites with the resources and willingness necessary to implement FN. Developing navigators' capabilities to implement LIFT—through training, an established case management system, and connections to peer navigators—were also identified as implementation core functions.
Conclusion: This study adds to the growing evidence on FN by characterizing intervention and implementation core functions, a critical step toward promoting LIFT's implementation and effectiveness.
Introduction
Cancer care in the United States is associated with substantial—and in many cases, ongoing—financial burdens that patients with cancer and their families struggle to manage. Individuals historically underserved by medical institutions (e.g., patients living in rural areas, non-English speaking patients, patients of color) experience disproportionate financial burden and poor access to cancer care (1–3). Mounting evidence has documented the extraordinary burden of out-of-pocket medical and non-medical expenses on patients, leading to an increased risk of downstream adverse consequences, such as worse health-related quality of life, care avoidance and discontinuation, bankruptcy, and mortality (4–8). Collectively, these risks have been termed financial toxicity (FT). In addition to leading to harmful consequences for patients, FT has also been shown to negatively impact caregivers and other members of the household (9, 10). Furthermore, FT may negatively impact healthcare system finances through cost-related missed appointments and uncompensated care (11, 12).
Increasing awareness of this problem has motivated the development of interventions to prevent or mitigate FT (13, 14). Although validated measures exist to identify FT (15, 16), and most NCI-designated cancer centers and National Comprehensive Cancer Network member institutions report providing some forms of financial support for their patients (17, 18), cancer centers' approaches to systematic FT identification and mitigation are highly variable and, as a result, variably effective. For cancer care providers to more effectively reach and assist patients with disproportionate financial burden, it is essential that structured interventions are developed and disseminated with those communities in mind.
One such structured intervention to address FT is financial navigation (FN). FN identifies patients at risk for or experiencing FT, educates patients about programs and services that may help address FT, directly assists patients in applying for, and receiving benefits from, existing programs and services, and tracks and manages patient needs in an ongoing manner (4, 19). Administered by a trained financial navigator, FN is designed to build capacity to address financial needs of patients with cancer and improve quality of care, while reducing duplication of effort and integrating workflows across cancer supportive care service providers. FN training typically includes education about health insurance and government structures, policies and resources and tools and techniques to assess and address financial concerns of patients (e.g., through the Association of Community Cancer Centers Financial Advocacy Bootcamp). The ACCC Financial Advocacy Bootcamp is a national, online resource provides basic information on federal financial aid programs and eligibility requirements, patient communication recommendations, and problem-solving strategies (20). FN training also typically includes orientation to the needs and care trajectories of patients with cancer (through evidence reviews, testimonials, and other mechanisms); case management skills-building and tracking; review of local, state, and national resources for financial support services and eligibility; review of relevant case management protocols (e.g., frequency and duration of case sessions, protection of privacy and confidentiality, referral processes); and access to senior FN specialists who train and mentor other financial navigators and can share personal experiences with FN.
FN interventions have been shown to decrease patient financial distress, provide material financial support, and improve revenue recovery for uncompensated care at hospitals (4, 19). To extend the benefits of FN to new care contexts and populations, such as patients living in rural areas, we must first identify the intervention core functions of FN—i.e., the features that drive its effectiveness and thus cannot be compromised. Simultaneously, we must understand the features of FN that are required for its integration into routine clinical practice (i.e., its implementation core functions) since poor implementation will compromise effectiveness. Understanding the intervention and implementation core functions of an evidence-based FN intervention will equip cancer programs with the knowledge required to adapt FN to new contexts and populations without compromising its effectiveness. To that end, our objective in this manuscript was to identify FN core functions to facilitate adaptation for implementation in diverse populations and contexts.
Materials and methods
Study design
We used Kirk et al.'s methods of identifying core functions for an evidence-based FN intervention—Lessening the Impact of Financial Toxicity (LIFT).
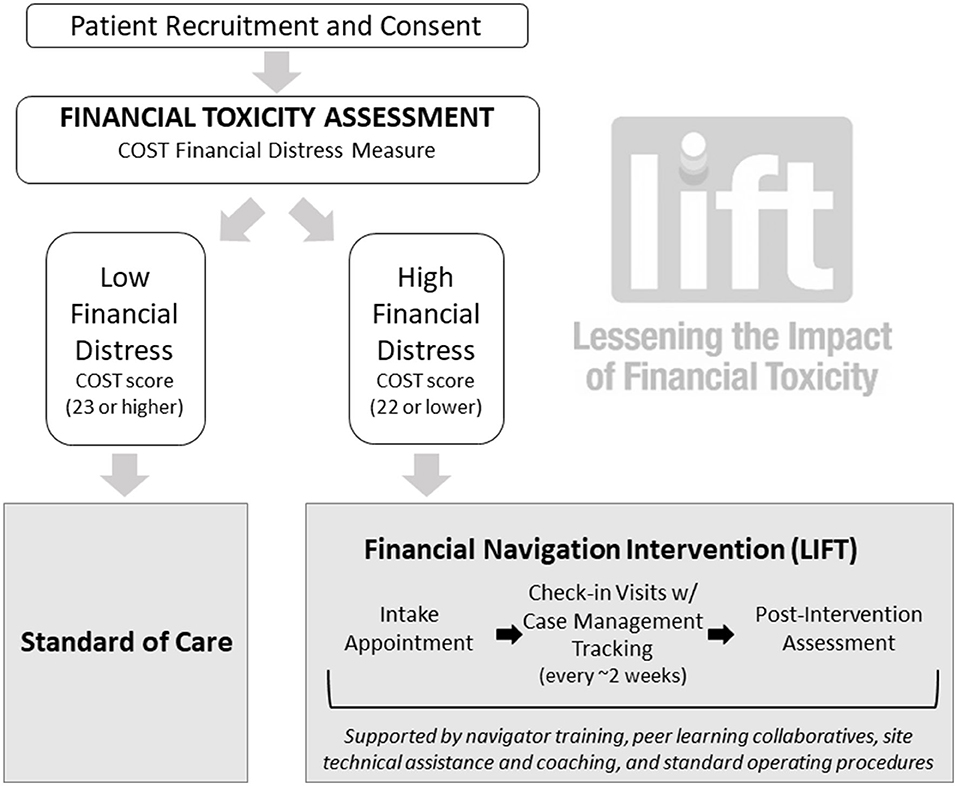
Lessening the Impact of Financial Toxicity (LIFT) program
The LIFT program was tested at the UNC Lineberger Comprehensive Cancer Center in 2019. The initial intervention study was supported by an internal grant from the UNC Innovation Center and was approved by the UNC IRB (UNC IRB # 18-2765). The FN intervention consisted of (1) systematic identification of cancer patients at high risk for FT using the Comprehensive Score for Financial Toxicity (COST) measure (COST ≤ 22 considered high risk for FT) (15, 16); (2) connection of patients experiencing FT, or at high risk for FT, with dedicated and trained oncology financial navigators, who employed a comprehensive assessment tool to determine financial needs and one-on-one appointments to direct patients to specific financial support resources and assist with applications; and (3) routine electronic tracking and monitoring of patients' financial and health outcomes. The intervention included regular, biweekly phone or in-person check-ins for up to 6 months, or until patients reported meeting one or more of their financial goals. Outcomes of this program have been reported elsewhere. Briefly, the FN intervention was associated with a statistically significant, nearly 7-point improvement in patient-reported financial distress (measured by the COST instrument, range: 0–44), and patients viewed LIFT as acceptable, timely and highly responsive to their needs (21).
Data collection and study procedures
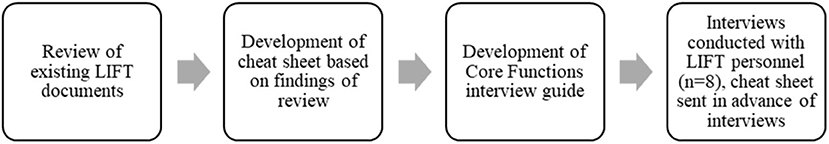
SAB and CRW led the process of identifying LIFT core functions using Kirk et al.'s theory-based method using a multi-step system (Figure 1). First, SAB and CRW reviewed the existing documents describing LIFT, including the LIFT protocol, internal standard operating procedures, and patient-facing materials. Second, SAB and CRW developed a “cheat sheet” (Appendix 1) that provided an overview of perceived core functions of the LIFT program based on the review of existing documents. This cheat sheet was sent to participants to review in advance of the interview and used during the interview to guide discussion. Third, SAB and CRW developed a semi-structured interview guide (Appendix 2) designed to enhance understanding of LIFT forms, and how those forms were thought to drive LIFT's implementation and effectiveness. The interview guide was designed based on Kirk et al.'s methods of identifying core functions, with additional questions added to fill in gaps and answer questions from the initial data collection from existing documents. Questions fell into categories of participant information, questions about accuracy and gaps of the “cheat sheet,” causal pathways, core functions of the intervention, and ways in which the intervention would need to be adapted for additional populations. Interviews were conducted by SAB and CRW with eight UNC Lineberger faculty, staff, administrators, and research team members who were involved in LIFT's development and pilot testing. Both SAB and CRW are trained in qualitative methods, have significant experience conducting qualitative research, and conducting semi-structured interviews. Participants were asked about their roles and LIFT's central implementation and programmatic activities. Additional questions focused on the aspects of the LIFT study that were specific to the site infrastructure and patient demographics for the purposes of future adaptation. Each interview was conducted in person or on Webex in 2021 and lasted 45–90 min. An interviewer's report summarizing key points, notable quotes, and overall findings was drafted at the conclusion of each interview. Digital recordings of each interview were independently transcribed verbatim.
Analysis
Using ATLAS.ti version 22 (22), SAB and CRW then coded the existing LIFT documents and interview transcripts using the Model for Adaptation Design and Impact (23). Thematic analysis was used to understand how LIFT was integrated into clinical practice (implementation core functions) and decreased FT (intervention core functions). Themes were initially built by identifying patterns related to LIFT core functions and organizing those themes into related groups. In a thorough member-checking exercise, SAB and CRW met with interview participants to refine the themes. They first discussed an initial draft of themes with SBW and DR, LIFT developers, to refine the themes based on their experience with LIFT. CW and SAB then presented the refined themes in two subsequent meetings with other interview participants. Once interview participants had no additional feedback on the themes, CW and SAB classified themes as either implementation or intervention core functions. Intervention core functions were defined as intervention components that were necessary and sufficient in combination to achieve the intended effectiveness outcome of reduced FT. Implementation core functions were components that were necessary and sufficient in combination to achieve the intended implementation outcomes of acceptability and feasibility. We then developed a spreadsheet with this information for interview participants' final review of core functions' accuracy and comprehensiveness.
Finally, to explain the change underlying LIFT's implementation and effectiveness—i.e., the mechanism(s) thought to drive LIFT's integration into practice and reduction of FT—SAB identified relevant organization theories. Based on concepts related to power, autonomy, and control, organization theories explain how and why interventions such as LIFT are adopted, implemented, and sustained in new contexts.
Results
Interview participants included the principal investigators who initially designed LIFT (SBW and DR), the LIFT project director (MM), the LIFT program manager (MG), two research assistants (NP and CB), and the two financial navigators engaged in the original pilot study (CR and JR).
Intervention structure
Figure 2 details the structure of the LIFT intervention. Patients referred for FN were identified through multiple channels (self-referral, provider referral, electronic health record system-facilitated referral) and typically had at least 2 visits with the financial navigator with some patients receiving more intensive, needs-dependent support. Repeated visits with the financial navigator were often important for navigators to review patients' eligibility and applications for financial support services, clarify paperwork needs, correct errors, and assist with application submission. Appointments involved one-on-one consultation with the financial navigator, who assessed patients' individual and household financial situation and financial assistance goals. Financial navigators also collected information about employment status, billing information, insurance status and other indicators used to triage patients to the appropriate financial resource(s). At the end of this initial appointment and comprehensive intake assessment, patients were provided a checklist of resources they were potentially eligible for and a list of the personal paperwork (e.g., tax forms, W-2, pay stubs) needed to apply. During the follow-up appointment(s), the financial navigator reviewed the initial intake forms, verified that the patient had the necessary paperwork and worked with the patient to complete resource applications. Patients were educated about and referred to financial resources, including but not limited to, hospital-based assistance programs, local nonprofits, foundation-provided financial support, medication assistance programs, Medicaid, Medicare, private health insurance plans, Social Security Disability Insurance and Supplemental Security Income, and legal assistance. Patients were re-contacted by the financial navigator 2–3 weeks after each FN clinic visit to assess progress toward their financial assistance goals. The intervention lasted between 2 weeks and 6 months, with an average intervention time of 4 months, depending on needs. The original FN intervention was delivered in-person by social work-trained navigators at varying ranks and levels, from senior oncology social worker to social work student trainees.
We identified six intervention core functions that were collectively necessary and sufficient to reduce FT, and five implementation core functions that drove LIFT's integration into clinical practice (see Tables 1, 2, respectively).
Intervention core functions
The change underlying LIFT's effectiveness, represented by LIFT's intervention core functions, can be explained using Transaction Cost Economics theory (24). Transaction Cost Economics proposes that there are costs associated with planning, implementing, and enforcing transactions with other organizations. In the context of FN, transactions include soliciting, coordinating, and administering financial resources and support from the cancer programs and external organizations (e.g., foundations) to address FT. The costs of FN transactions are particularly high due to their specificity, uncertainty, and frequency. Negotiating transactions to garner financial support requires substantial skill. Information regarding what funding was available, when it would be available, and to whom it was available was difficult to ascertain and depended upon irregular information-gathering transactions. Transaction Cost Economics proposes that transaction costs can be minimized with governance structures; LIFT represents a compilation of governance structures that minimized the costs associated with FN. LIFT involved financial navigators with specialized training that allowed them to develop strong one-on-one relationships with patients and use patient-specific needs to guide coordination of access to resources. As an example, one interview participant said, “It just seemed so crystal clear that patients [with financial distress] need[ed]…the deep empathetic and authentic relationships that people in those roles [navigators] were able to build.” Another participant said, “[I]n our initial interview with each patient, we would identify what their particular needs were. The intervention allowed us to tailor the assistance we provided to whatever the patient's needs were.” As a result, LIFT financial navigators reported feeling confident in their roles; the quality, trust and rapport of the navigator-patient relationship; and their ability to remove barriers to reducing FT.
LIFT addressed FN transaction irregularity and uncertainty by offering dynamic assistance to patients. One interview participant said, “…[P]atients would have regularly scheduled checkups with their navigator to say, “Hey, did you get that paperwork for me that I could turn in for your financial assistance application to the hospital?” Somebody who was doing those regular checks on a very consistent basis until all of the assistance was completed. I think that's the big difference instead of just handing them a packet and saying, “Here you go. Fill this out, and turn it in.”” This dynamic patient assistance was supported by systematic methods of cataloging FN resources and tracking patient information, allowing financial navigators to efficiently remove common barriers to accessing resources. An interview participant said, “Once identified, having a comprehensive intake assessment that wasn't just, “Tell me about your job,” or, “Tell me about your insurance status,” but that was driven by—almost like a checklist of, “Okay, well, let me just go through and make sure that I've fully understood this patient's entire financial and social lived experience.” Then through that, by having that comprehensive intake, you have better mapping onto the financial resources that exist— and what they qualify for.” Another participant said, “It was like harnessing knowledge that existed but wasn't always systematized in a way that—every encounter might've been a little bit different, and pulling all that information together and coordinating it and then, yeah, like you said, structuring, organizing it, and helping improve the process so that the process itself didn't rely on one person's institutional knowledge.” Without systematic methods of cataloging FN resources and tracking patient information, financial navigators were previously reliant on personal knowledge, paper-based notes, and less standardized approaches to meeting patients' needs.
Implementation core functions
LIFT's implementation core functions can be explained using Organizational Readiness Theory (25). Organizational readiness is defined as organizational members' shared resolve and perceived capability to implement a change such as LIFT. Consistent with Organizational Readiness Theory, we found that LIFT's implementation required engaging facilities that were willing to do the work of implementation and had the resources required to implement LIFT. One interview participant said, “I think there was a lot of momentum to address this as an interest of the hospital, the health system, that there was—they'd been looking at this and they were wanting to…so I think that helped.” Another said, “I think the key—our special sauce…is that we developed this within the existing system.” Implementing LIFT also required developing financial navigators' capability and providing the systems necessary to support implementation. One participant said, “That was really critical to the replicability...anybody with a certain base level of skills could be trained to do this.”
Discussion
We identified core functions associated with the LIFT FN intervention and its implementation and mapped them onto existing theories of change. Our findings suggest that FN reduces FT by minimizing the transaction costs associated with delivering financial support to patients experiencing FT. Intervention core functions minimizing transaction costs included systematically cataloging knowledge and tracking patient-specific information related to eligibility criteria for FT relief. Furthermore, repeat contacts between the financial navigator and participant created an ongoing relationship, removing common barriers to accessing resources. We also found that the successful implementation of LIFT was predicated on organizational readiness. Implementation core functions included having engaged sites with the resources and willingness necessary to implement FN. Developing navigators' capabilities to implement LIFT—through training, an established case management system, and connections to peer navigators—were also identified as implementation core functions. These findings serve to clarify features of the LIFT intervention that must be retained when adapting LIFT to new settings and populations. They also serve to supplement studies evaluating financial navigation interventions more broadly by providing a framework of core functions to be built upon, revised, and adapted over time (26).
The success of LIFT and other FN interventions is predicated on retention of core functions, while being attentive to the local, contextually-specific needs that may warrant adaptation to improve fit, for example, in patients living in rural areas and seeking care at community cancer centers. Cancer care in rural settings is unique (27); resource constraints and limited geographic access to care providers may directly affect how FN is delivered (28) (for example, in terms of the financing and differences in workflows and duties of rural navigators, as well as the delivery of FN via phone or in person). Our findings suggest that LIFT can reduce FT in even the most challenging practice contexts as long as its core functions are retained. Our findings, taken with previous adaptation studies for which organization theories were also relevant explanations of intervention and implementation core functions, suggest that organization theories are particularly relevant for explaining how and why interventions such as LIFT are adopted, implemented, and sustained in new contexts (29).
Financial hardship associated with cancer is prevalent, yet interventions to alleviate its burden are few and far between. FN holds considerable promise, but like most patient navigation models that respond to patient-centered needs and contextual realities, the details of these interventions can be perceived as amorphous. Our findings provide generalizable guidelines for those seeking to implement FN. Although FN generally, and LIFT specifically, may take on specific forms in a particular context or population, the success of such programs is buoyed by its core intervention and implementation functions. LIFT's core functions thus enable diverse cancer care settings to implement programs that are expected to succeed for various populations.
Our study has limitations. Our approach to identifying core functions was not experimental; that is, we do not have data regarding the causal relationship between the core functions that we identified and key implementation and intervention outcomes. However, our approach is theory-based and thus posits specific mechanisms underlying the relationship between core functions and key implementation and intervention outcomes. These relationships should be studied in future work. We also relied on the perspectives of LIFT designers and implementers. To the extent that existing study documents and interview data reflect a biased view of LIFT, the core functions that we identified may be inaccurate. However, we included a diverse group of LIFT designers and implementers, ranging from study principal investigators to financial navigators to research assistants, and relied on extensive intervention documents to promote as accurate a representation of the intervention and its implementation as possible. This study also reflects an intervention developed and delivered initially in a single, large, academic medical center and may not be representative of other FN interventions that are concurrently being developed and tested.
Despite these limitations, the strength of this study lies in its theory-based approach to identifying an initial set of core functions underlying FN interventions, using LIFT as a case example. The core functions that we identified in this study should be regarded as living documents to be continuously revised based on the implementation of LIFT in new contexts and populations.
In conclusion, to our knowledge, this is the first study to report core functions of a FN intervention. Our findings contribute to a growing body of literature that reports intervention and implementation core functions (30–32). Identifying core functions is critical for extending the benefits of effective interventions into new contexts and populations. Indeed, we expect findings from this study to improve the practice of FN for patients with cancer because it will demonstrate the benefits of a scalable, pragmatic, individualized intervention that focuses on patients at high risk of FT. It also can be delivered remotely outside the clinical encounter, equipping oncology practices, health systems and payers with a process to optimize cancer care delivery through addressing FT.
Data availability statement
Data from this study will be available upon reasonable request to the corresponding author.
Author contributions
SW, SB, and DR conceived of and designed the study, oversaw all data collection, analyses and interpretation, wrote/edited and approved the final manuscript. CW, MM, MG, NP, CB, CR, and JR contributed data to the manuscript, revised and approved the final manuscript. CS and RB aided in interpretation of the data, revised and approved the final manuscript. All authors agree that they are accountable for all aspects of the work.
Funding
This research was supported by the National Cancer Institute (NCI) at the National Institutes of Health (NIH) via three grants: 1-R01-CA240092-02 (SW and DR), 3-P30-CA016086-44-S4, PI: Earp, Project Leads: SW and DR), and P30CA012197-45S5 (Wake Forest's Supplement, PI: Boris Pasche, Project Leads: RB and SB). Additional funding for this project was provided by the National Comprehensive Cancer Network and Pfizer Independent Grants for Learning and Change (PI: SW and DR) and the University of North Carolina Innovation Center. In addition, SW, SB, and CW receive support for this work, in part, through the Cancer Prevention and Control Research Network, funded by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS) (U48 DP006400). CB is supported by a Cancer Care Quality Predoctoral Traineeship, UNC-CH, Grant No. T32-CA-116339. SW receives grant funding paid to her institution from Pfizer Foundation.
Acknowledgments
The authors would like to acknowledge the critical contributions of patients with cancer to this study. The authors also thank Ms. Erin Laurie for administrative support. We also acknowledge the contributions of the Cancer Prevention and Control Research Network's Organization Theory for Implementation Science workgroup in making Transaction Cost Economics available for application in this implementation research. This publication was supported in part by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS, or the U.S. Government.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2022.958831/full#supplementary-material
References
1. Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomark Prev. (2020) 29:308–17. doi: 10.1158/1055-9965.EPI-19-0460
2. Odahowski CL, Zahnd WE, Zgodic A, Edward JS, Hill LN, Davis MM, et al. Financial hardship among rural cancer survivors: an analysis of the medical expenditure panel survey. Prevent Med. (2019) 2019:105881. doi: 10.1016/j.ypmed.2019.105881
3. Zahnd WE, Davis MM, Rotter JS, Vanderpool RC, Perry CK, Shannon J, et al. Rural-urban differences in financial burden among cancer survivors: an analysis of a nationally representative survey. Support Care Cancer. (2019) 27:4779–86. doi: 10.1007/s00520-019-04742-z
4. Ramsey SD, Bansal A, Fedorenko CR, Blough DK, Overstreet KA, Shankaran V, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. (2016) 34:980–6. doi: 10.1200/JCO.2015.64.6620
5. Ramsey SD, Blough DK, Kirchhoff AC, Fedorenko CR, Snell KS, Kreizenbeck KL, et al. Washington cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. (2013) 32:1143–52. doi: 10.1377/hlthaff.2012.1263
6. Zheng Z, Han X, Zhao J, Banegas MP, Tucker-Seeley R, Rai A, et al. Financial hardship, healthcare utilization, and health among US cancer survivors. Am J Prev Med. (2020) 59:68–78. doi: 10.1016/j.amepre.2020.02.016
7. Nipp RD, Zullig LL, Samsa G, Peppercorn JM, Schrag D, Taylor DH, et al. Identifying cancer patients who alter care or lifestyle due to treatment-related financial distress. Psychooncology. (2016) 25:719–25. doi: 10.1002/pon.3911
8. Park J, Look KA. Relationship between objective financial burden and the health-related quality of life and mental health of patients with cancer. J Oncol Pract. (2018) 14:e113–e21. doi: 10.1200/JOP.2017.027136
9. Kazzi B, Chino F, Kazzi B, Jain B, Tian S, Paguio JA, et al. Shared burden: the association between cancer diagnosis, financial toxicity, and healthcare cost-related coping mechanisms by family members of non-elderly patients in the USA. Support Care Cancer. (2022) 2022:1–13. doi: 10.1007/s00520-022-07234-9
10. Rotter JS, Spencer JC, Wheeler SB. Can cancer care costs impact quality of life outcomes for the entire household? Psychooncology. (2019) 28:924–7. doi: 10.1002/pon.5006
11. Yezefski T, Steelquist J, Watabayashi K, Sherman D, Shankaran V. Impact of trained oncology financial navigators on patient out-of-pocket spending. Am J Manag Care. (2018) 24:S74–s9.
12. Maldonado JA, Fu S, Chen YS, Acquati C, Yabroff KR, Banegas MP, et al. Sensitivity of psychosocial distress screening to identify cancer patients at risk for financial hardship during care delivery. JCO Oncol Pract. (2021) 17:e1856–e65. doi: 10.1200/OP.20.01009
13. Zafar SY. Financial toxicity of cancer care: it's time to intervene. J Natl Cancer Inst. (2016) 108:370. doi: 10.1093/jnci/djv370
14. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D. Population-based assessment of cancer survivors' financial burden and quality of life: a prospective cohort study. J Oncol Pract. (2015) 11:145–50. doi: 10.1200/JOP.2014.001542
15. de Souza JA, Yap BJ, Hlubocky FJ, Wroblewski K, Ratain MJ, Cella D, et al. The development of a financial toxicity patient-reported outcome in cancer: the COST measure. Cancer. (2014) 120:3245–53. doi: 10.1002/cncr.28814
16. de Souza JA, Yap BJ, Wroblewski K, Blinder V, Araújo FS, Hlubocky FJ, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer. (2017) 123:476–84. doi: 10.1002/cncr.30369
17. de Moor JS, Mollica M, Sampson A, Adjei B, Weaver SJ, Geiger AM, et al. Delivery of financial navigation services within national cancer institute-designated cancer centers. JNCI Cancer Spect. (2021) 5:33. doi: 10.1093/jncics/pkab033
18. Khera N, Sugalski J, Krause D, Butterfield R, Zhang N, Stewart FM, et al. Current practices for screening and management of financial distress at NCCN member institutions. J Natl Compr Canc Netw. (2020) 18:825–31. doi: 10.6004/jnccn.2020.7538
19. Shankaran V, Leahy T, Steelquist J, Watabayashi K, Linden H, Ramsey S, et al. Pilot feasibility study of an oncology financial navigation program. J Oncol Pract. (2018) 14:e122–e9. doi: 10.1200/JOP.2017.024927
20. Mangir C, Schneider L, Santiago A, Boehmer L, Draper F, Plotkin E, Lucas L. Assessing effectiveness of a self-guided training program for oncology financial advocates. J Clin Oncol. (2021) 39(28_suppl):271. doi: 10.1200/JCO.2020.39.28_suppl.271
21. Wheeler SB, Rodriguez-O'Donnell J, Rogers C, Fulcher J, Deal A, et al. Reducing cancer-related financial toxicity through financial navigation: results from a pilot intervention. Cancer Epidemiol Biomark Prev. (2020) 29:694. doi: 10.1158/1055-9965.EPI-20-0067
22. GmbH AtSSD. ATLAS.tiWindows. 22nd ed. Berlin: ATLAS.ti Scientific Software Development GmbH (2022).
23. Kirk MA, Moore JE, Wiltsey Stirman S, Birken SA. Towards a comprehensive model for understanding adaptations' impact: the model for adaptation design and impact (MADI). Implement Sci IS. (2020) 15:56. doi: 10.1186/s13012-020-01021-y
24. Stiles RA, Mick SS, Wise CG. The logic of transaction cost economics in health care organization theory. Health Care Manag Rev. (2001) 26:85–92. doi: 10.1097/00004010-200104000-00010
25. Weiner BJ. A theory of organizational readiness for change. Implement Sci IS. (2009) 4:67. doi: 10.1186/1748-5908-4-67
26. Doherty MJ, Thom B, Gany F. Evidence of the feasibility and preliminary efficacy of oncology financial navigation: a scoping review. Cancer Epidemiol Biomark Prev. (2021) 30:1778–84. doi: 10.1158/1055-9965.EPI-20-1853
27. Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P. Challenges of rural cancer care in the United States. Oncology. (2015) 29:633–40.
28. Biddell CB, Spees LP, Petermann V, Rosenstein DL, Manning M, Gellin M, et al. Financial assistance processes and mechanisms in rural and nonrural oncology care settings. JCO Oncol Pract. (2022) 2022:Op2100894. doi: 10.1200/OP.21.00894
29. Birken SA, Ko LK, Wangen M, Wagi CR, Bender M, Nilsen P, et al. Increasing access to organization theories for implementation science. Front Health Serv. (2022) 2:891507. doi: 10.3389/frhs.2022.891507
30. Anderson DM, Birken SA, Bartram JK, Freeman MC. Adaptation of water, sanitation, and hygiene interventions: a model and scoping review of key concepts and tools. Front Health Serv. (2022) 2:896234. doi: 10.3389/frhs.2022.896234
31. Kirk MA, Hanson LC, Weinberger M, Haines ER, Rokoske FS, Powell BJ, et al. Pilot test of an adapted intervention to improve timeliness of referrals to hospice and palliative care for eligible home health patients. J Palliat Med. (2019) 22:1266–70. doi: 10.1089/jpm.2018.0504
Keywords: financial toxicity, cancer, financial navigation, adaptation, implementation
Citation: Wheeler SB, Birken SA, Wagi CR, Manning ML, Gellin M, Padilla N, Rogers C, Rodriguez J, Biddell CB, Strom C, Bell RA and Rosenstein DL (2022) Core functions of a financial navigation intervention: An in-depth assessment of the Lessening the Impact of Financial Toxicity (LIFT) intervention to inform adaptation and scale-up in diverse oncology care settings. Front. Health Serv. 2:958831. doi: 10.3389/frhs.2022.958831
Received: 01 June 2022; Accepted: 21 September 2022;
Published: 09 November 2022.
Edited by:
Reza Yousefi Nooraie, University of Rochester, United StatesReviewed by:
Alice Avancini, University of Verona, ItalyMargaret Liang, University of Alabama at Birmingham, United States
Copyright © 2022 Wheeler, Birken, Wagi, Manning, Gellin, Padilla, Rogers, Rodriguez, Biddell, Strom, Bell and Rosenstein. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephanie B. Wheeler, U3RlcGhhbmllX1doZWVsZXJAdW5jLmVkdQ==
†These authors have contributed equally to this work and share first authorship
 Stephanie B. Wheeler
Stephanie B. Wheeler Sarah A. Birken
Sarah A. Birken Cheyenne R. Wagi
Cheyenne R. Wagi Michelle L. Manning1
Michelle L. Manning1 Caitlin B. Biddell
Caitlin B. Biddell Ronny Antonio Bell
Ronny Antonio Bell