- 1Australian Institute of Health Innovation (AIHI), Macquarie University, Sydney, NSW, Australia
- 2IIMPACT in Health, Allied Health and Human Performance, University of South Australia, Adelaide, SA, Australia
- 3Centre for Human Factors and Sociotechnical Systems, University of the Sunshine Coast, Sunshine Coast, QLD, Australia
- 4Nursing Research Institute, Australian Catholic University, Sydney, NSW, Australia
Context: Patient Safety Incident (PSI) reviews are undertaken frequently across health services in response to serious adverse events. This study investigated experiences and perceptions of healthcare professionals involved in incident review processes across four jurisdictions in Australia, alongside insights from international patient safety experts. These findings will inform the co-design of improvements to PSI reviews.
Methods: Semi-structured interviews and focus groups were conducted, and participants completed an attitudinal and demographic survey. Inductive thematic analysis was conducted, and findings were deductively mapped against the Consolidated Framework for Implementation Research.
Findings: Australian (n = 99) and international (n = 11) participants took part in one of 25 focus groups (n = 78) or 32 interviews. Most participants (n = 99) completed the survey. Nearly all survey participants agreed/strongly agreed that PSI reviews are valuable for improving patient safety (95%), particularly when human factors and contextual influences on performance (76%) are considered. Two-thirds of participants agreed that investigations help prevent PSI recurrence (68%), avoid unfair blame (67%), and support continuous improvement (61%). However, fewer participants felt recommendations are consistently accepted by organisations (58%) or are appropriately targeted within the healthcare system (57%). Key strengths and challenges of the PSI review process were identified across three themes: Selection of PSI Reviews; Reviews, Recommendations and Implementation; and Health Organisations and Wider System Influences. Key PSI review challenges included: limited capacity and engagement, high staff workloads, turnover, and burnout, as well as variable skills, and limited human factors and systems thinking experience across review teams. Despite strong efforts to reduce a punitive culture, resistance to reporting and blame persists across some hospitals. Participants highlighted a learned powerlessness when developing systems thinking-based recommendations, resulting in the development of weaker, less resource intensive recommendations. Limited sharing of learnings and feedback on review findings, and variable monitoring, evaluation and accountability of recommendation implementation were also common challenges.
Conclusions: These findings have identified a need for system re-engineering of PSI reviews to address identified challenges and will inform the development of Best Practice Principles and a codesign of patient safety tactics for trial in-situ.
Introduction
Healthcare systems are designed to care for patients, however inadvertent harm can often occur (1–4). Patient safety incidents (PSIs) that arise during the provision of healthcare, including unexpected death or serious harm, are a concern internationally and significantly contribute to patient morbidity and mortality (5). Internationally, 12% of patients receiving medical care experience harm (5), a third of which are deemed preventable (6), with patient harm contributing to over 2.6 million deaths annually in low to middle income countries (LMICs) alone (7, 8). The most common PSIs involve drug-related incidents (e.g., wrong drug or dose), surgical or procedural events (e.g., item retained during surgery, wrong-site surgery), patient care events (e.g., falls), and hospital acquired infections (6). Annually, PSIs are estimated to cost the US health system $17.1 billion (2008 figures) (9), and internationally PSIs have been estimated to cost 13% of healthcare budgets in developed countries (10). The estimated cost of PSIs in LMICs (including lost productivity), is estimated to be USD1.6 trillion annually (8). PSIs increase the burden for patients, staff and the health system through extended lengths of stay, preventable readmissions, increased demand for health service use, and overall poorer health outcomes (11, 12).
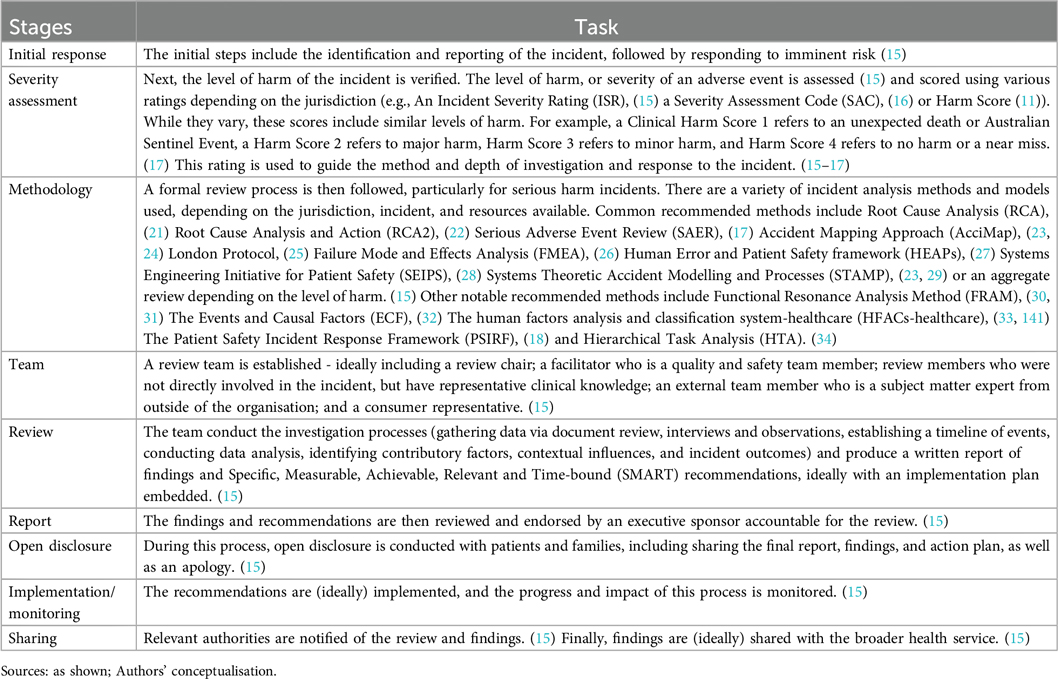
When a patient is harmed, healthcare organisations should report, manage and investigate the incident (13, 14), provide feedback to patients and families about review findings (11), and implement interventions designed to prevent future similar occurrences. The purpose of these incident reviews is to understand what happened and why, and to identify interventions to reduce the frequency of harm to other patients within the health system. In many countries this process is guided by incident best practice guidelines developed by health care organisations or national or state jurisdictions (15–19). By way of example, there are approximately 1,700 incident reviews of serious adverse events undertaken in Australian public health services each year (20). Reliable collated data from the US on these figures is not available. Conducting PSI reviews is resource and time intensive, involving multiple steps, and methodologies (15, 17, 18, 21–34) often with senior staff members (1, 15) (Box 1).
Major reports in the UK and US at the turn of century were published highlighting the problem of patient safety (35, 36). Despite concerted efforts by policy-makers including the World Health Organisation, national and state-wide bodies, healthcare executives, clinicians, and patients, the evidence is clear that current incident review processes do not effectively reduce the frequency of PSIs causing preventable harm to patients (1, 37–40). Despite decades of research and vast resources invested in the review and response process, limited improvements have been observed in the rates of PSIs, in Australian hospitals (4, 11, 12), in the US (4, 6), and internationally (4, 41–45).
Healthcare systems are notoriously multifaceted and intricate: most frequently described as complex adaptive systems (46), and PSIs are grounded in these complexities, within a multitude of healthcare system conditions, events and failures (11). There are many known inter-dependent determinants that impact the effectiveness of a response to PSIs across multiple levels of the healthcare system, including the clinical microsystem, complicated funding arrangements, organisational features, and the density of the policy and regulation milieu. This complexity underlies the importance of examining this topic in such detail. These include a historical culture of blame and fear of punitive consequences (47, 48), poor reporting systems and processes (47, 48), labyrinth-like governance structures, workforce demands, capacity and capability, including the composition and skills of review teams, and the many types of investigation methods utilised (47, 49). Despite decades of PSI Reviews in healthcare settings internationally, persisting themes include a lack of feedback on review findings, a failure to identify contributory factors in the broader healthcare system, poor quality recommendations, and poor-to-no evidence-based implementation strategies (47, 48), with a lack of systematic follow-up and limited perceived improvements following the review and reporting process (48). Limited incorporation of implementation science theory and methodology as well as quality improvement methods may contribute to this poor implementation process (50–52). A strong safety culture, staff engagement, national safety policies, and regulatory bodies, as well as support and staff upskilling, shared learning and patient engagement, are all considered important facilitators of better PSI reviews and safer care (53).
PSI Review recommendations are often unspecific and lacking measurability (54), limiting their effectiveness (45); weak recommendations frequently focus on staff and individual factors, the sharp-end of healthcare—rather than addressing system-wide improvements (15, 55). Implementation of such recommendations (38, 54, 56) also has limited effectiveness on rates of adverse events (38, 56). Further evidence is needed to understand the determinants of effective development and implementation of recommendations resulting from PSI reviews, to see reductions in patient harm (1, 37–40).
Recent development in patient safety emphasises a significant shift from reactive, individual-blame-focused investigations towards more proactive, system-oriented approaches that prioritise learning and improvement (15, 17, 57). Frameworks such as the United Kingdom's Patient Safety Incident Response Framework (PSIRF) (18) and the new version of the London Protocol (58, 59) exemplify this transition, promoting a proportionate, risk-based response to incidents and embedding principles of openness, system learning (60), and patient and family engagement in the investigation process. Complementing this, emerging international models increasingly draw on restorative justice principles, which seek to address not only what happened, but also who was affected, how they were affected, and what is needed for healing and collective accountability (61, 62). A recent cross-country analysis of restorative initiatives in five countries further illustrates the potential of these approaches to reorient investigations toward dialogue, dignity and trust (61). These shifts align well with global priorities articulated in the World Health Organisation's Global Patient Safety Action Plan 2021-2030 (8), which calls for strengthening system-level responses and engaging affected parties as active partners in safety (63, 64). These redevelopments underpin the growing recognition that meaningful and compassionate investigation processes are essential not only for identifying systemic risks but also for addressing the broader emotional, relational and ethical dimensions of harm, including compounded harm (65, 66). In particular, we note that compounded harm is not limited to patients and families (67, 68): health professionals (including investigators and clinicians) (69) and consumer representatives (70) can also experience moral distress and emotional exhaustion. These harms highlight the need for systems that attend not only to technical processes but also to the emotional dimensions of safety reviews.
Although the PSI response challenges outlined above are well known, what is less well understood are the factors that are contributing to these issues. This study aims to understand what is and is not working, when, and why in relation to incident response. This will be achieved by examining the perceptions, experiences, and current practices in incident response, management, investigation, analysis and implementation of improvements, across a cohort of Australian health service staff and international patient safety experts. This study examines the entire lifecycle of incident response, as due to their complexity and interdependency, they may all impact a health care organisation's learning and action to prevent similar incidents occurring again.
The findings from this study will inform the development of Best Practice Principles, a co-design process to re-engineer patient safety tactics to reduce patient risk, and in situ feasibility testing of identified practice improvements. This codesign and testing process will strive to support healthcare organisations to improve and measure their response analysis and learning from incidents, thereby reducing the risk of preventable harm to patients.
Methods
Context
This study is funded by a National Health and Medical Research Council (NHMRC) Partnership Grant project aiming to investigate ways to improve the health systems' responses when patients are harmed across four Australian state and territory public health systems: New South Wales (NSW), Victoria (VIC), the Australian Capital Territory (ACT), and Queensland (QLD). Approximately 77% (20.0 million) of the Australian population reside, and 78% (5.3 million) of hospital admissions occur in these states (71).
Our broader project included participants with lived experience of harm, such as consumer advocates or consumer representatives (CRs), but their data are not included in this paper. Their perceptions and experiences on PSI review teams were already published (70). Two additional papers are currently in draft: one focuses on best practice principles for working with CRs, and another explores consumer needs and expectations at various stages of PSI reviews.
Study type
This mixed methods research (MMR) study used a concurrent QUAL+QUAN design (72) to collect quantitative data from surveys and qualitative data from focus groups and interviews, with each dataset equally prioritised and findings compared and merged. This is aimed at increasing the validity of the data by exploring the survey data in more depth throughout the interviews and focus groups (73). The study is underpinned by a pragmatic worldview with the belief that utilising both data types will provide a more robust understanding of the key concepts (74). The reporting of this study was guided by the Good Reporting of A Mixed Methods Study (GRAMMS) checklist (75) and the Consolidated Criteria for REporting Qualitative (COREQ) guidance (76) (See Supplementary Files S1 and S2).
Recruitment
Health service staff involved in PSI reviews were recruited through stratified convenience sampling (77) conducted by health services across four Australian states and territories (NSW, VIC, QLD, ACT), as well as key organisations involved in PSI responses who are partners on this grant, and chief investigators (CIs). This sampling method was used to ensure representation of staff in Australian public health systems who: undertake incident management and PSI reviews; co-commission and are “customers” of reviews e.g., clinical directors, who co-commission, undertake, and quality assure investigations e.g., safety and quality directors and staff; or are from statewide organisations involved in policy or innovation around PSI reviews. Key contacts sent recruitment invitations to potential participants, who then contacted researchers to express interest in participating in an interview or focus group, and to complete a survey. There was no direct recruitment by the researchers.
In addition, international patient safety experts (based on their recognised contributions to patient safety research, policy development, systems design or healthcare quality improvement at a national or international level) were recruited by the network of CIs and partner organisations affiliated with this grant. This involved sending out invitation emails to a stratified convenience sample based on involvement in PSI review processes, including senior staff (such as human factors specialists, policy advisors, academics, and healthcare leaders) from regulatory bodies, government and policy making organisations, such as England's Health Services Safety Investigations Body. There were some existing professional relationships between CIs and participants (due to the nature of working in the same research area/industry), however, participation was voluntary. Interested individuals responded by contacting the research team to complete informed consent documentation and schedule an interview.
Data collection
Quantitative data
Once participants completed informed written consent, they completed an electronic demographic and attitudinal survey about PSI responses and management (via Redcap, web-based software methodology tool for designing clinical, translational and quality improvement databases: https://project-redcap.org/). Development of survey questions was informed by literature across implementation science (78, 79) and safety science (45, 80–89) domains, as well as team expertise. This survey collected participant demographic details and attitudes towards the patient safety response and review process on a 5-point Likert scale.
Qualitative data
After the survey was completed, focus groups and individual interviews were conducted via Microsoft Teams or Zoom software or over the phone following a predefined topic schedule (See Supplementary File S3), recorded and transcribed verbatim. Interviews and focus groups were conducted by researchers (PH (professor; male), MB (PhD, Research fellow; female) and YY (PhD, Research fellow; female)) who are experienced interviewers and health service qualitative researchers. Two of the interviewers (MB and YY) had no prior relationship with the interviewees prior to data collection, however, the lead investigator PH had prior professional relationships with several interviewees, but did not coerce participation. Participants were not reimbursed for their time.
Data analysis
The survey data was analysed descriptively. PSI investigations are referred to from here as reviews. Interview and focus group transcripts were imported into NVIVO v.14 software (90) and thematic analysis techniques (91) were used to guide the iterative inductive analysis of the data. This process was conducted by two researchers (MB and YY), with 25% of transcripts independently double coded to ensure consistency, creditability and rigour (92). The process began with both researchers reading transcripts in full to familiarise themselves with the data, followed by open, line-by-line coding to generate initial inductive codes. These codes were then categorised into broad themes on organisational culture (for example, leadership and patient safety team), the investigation process (for example, who was involved and what methodologies were used), and development and implementation of recommendations. An initial thematic framework was developed collaboratively, grounded in participants' language and recurring concepts across interviews and focus groups (91). The coding framework was refined iteratively through weekly team discussions, where coding decisions, emergent patterns, and thematic boundaries were debated and agreed upon. Discrepancies in coding or theme development were resolved through group consensus to ensure reliability and analytic coherence (92). Following this inductive coding process, the refined set of themes were deductively categorised into the Consolidated Framework for Implementation Research (CFIR) (78, 93). This mapping process involved aligning codes and themes with CFIR's five major domains- intervention characteristics, outer setting, inner setting, characteristics of individuals, and the process of implementation, to better understand the factors influencing how PSI review recommendations are enacted (94). The CFIR framework served as a theoretical lens to interpret and structure the qualitative data, allowing for the identification of both barriers and facilitators to implementation at multiple levels of the healthcare system (94). To deepen insights and strengthen validity through methodological triangulation, the qualitative data were then compared and integrated with quantitative survey findings. This involved identifying areas where interviews and focus group data converged with, complemented, or diverged from survey responses (73). This mixed-methods integration provided a more comprehensive understanding of participants' experiences with PSI reviews and highlighted key contextual and systemic factors influencing the development and implementation of recommendations.
Ethics approval
The study was granted ethics approval by the Northern Sydney Local Health District (NSLHD) Human Research Ethics Committee (an Institutional Review Board: approval number: 2023/ETH02341) in Sydney, Australia.
Results
Quantitative survey
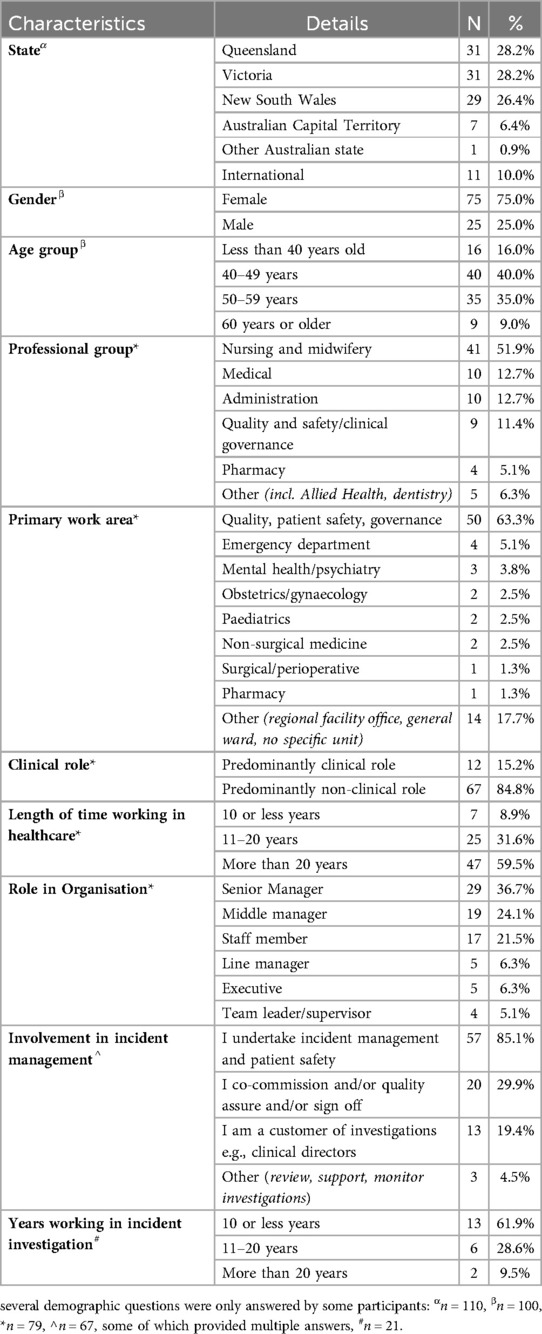
In total, 110 participants were recruited to participate in an interview or focus group, and survey. Participants in Australia (n = 99) were based in QLD (n = 31), VIC (n = 31) NSW (n = 29), the ACT (n = 7), and one other Australian state (unspecified, n = 1), or from international organisations (n = 11). Most participants completed the demographic (n = 100, 91%) and attitudinal components of the survey (n = 99, 90%). Not every question in the survey was answered by participants (see Table 1 for more detail). Participants were from a variety of clinical backgrounds and seniority. Of those who completed the survey, participants were typically from nursing or midwifery backgrounds (n = 41, 52%), working primarily in quality and safety/governance roles (n = 50, 63%), with more than 20 years' experience working in healthcare (n = 47, 60%). The majority of participants were female (n = 75, 75%), aged 40–59 years (n = 75, 75%) and working in a predominantly non-clinical role (n = 67, 85%) (Table 1).
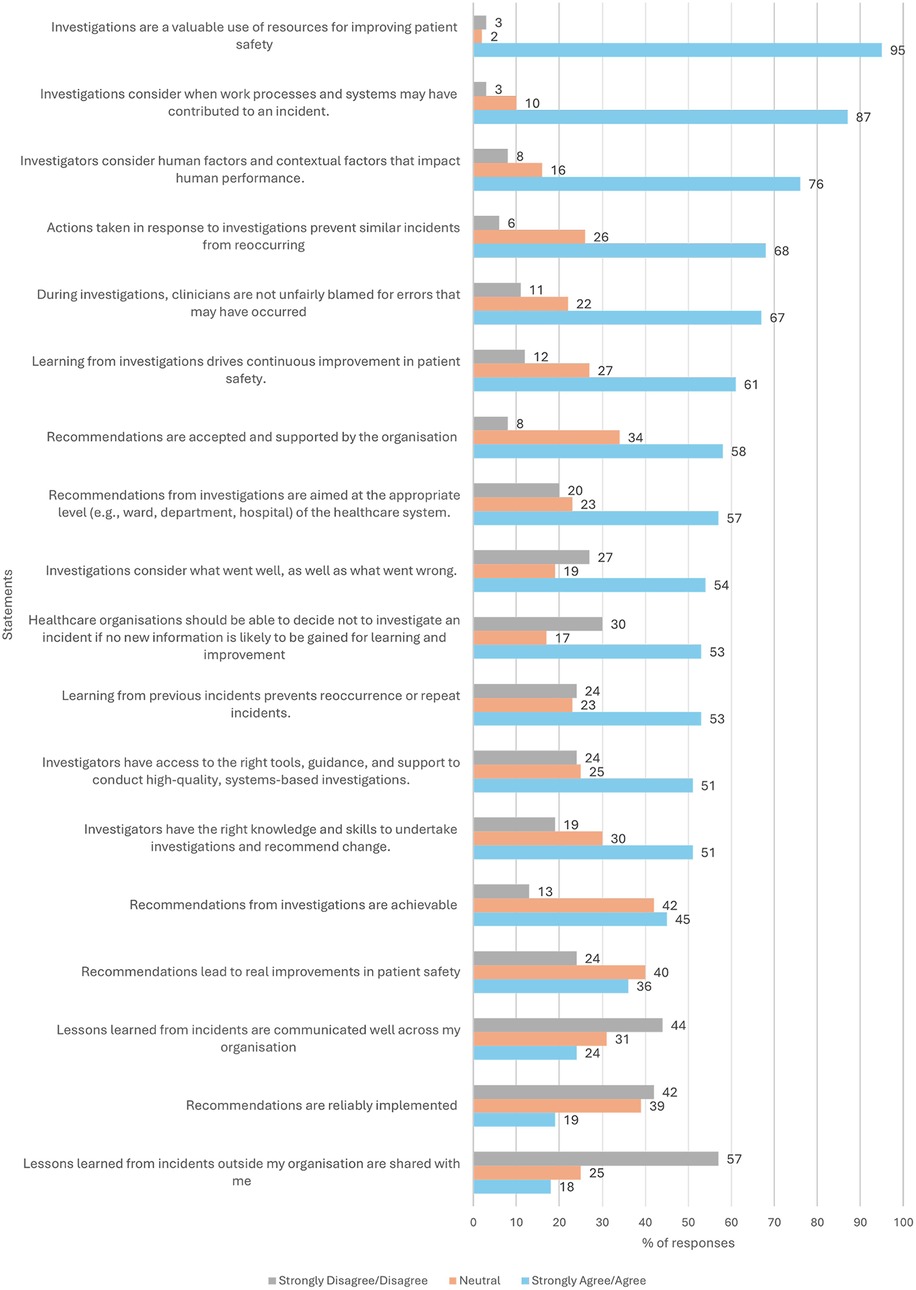
Participants were surveyed about their attitudes towards PSI reviews. The majority of participants agreed or strongly agreed that Investigations are a valuable use of resources for improving patient safety (n = 94/99, 95%), that consider when work processes and systems may have contributed to an incident (n = 87/100, 87%) and consider human factors and contextual factors that impact human performance (n = 76/100, 76%). Approximately two thirds or less of participants strongly agreed or agreed that Actions taken in response to investigations prevent similar incidents from reoccurring (n = 67/99, 68%), that Clinicians are not unfairly blamed for errors that may have occurred (n = 66/99, 67%) and that Learning from investigations drives continuous improvement in patient safety (n = 61/100, 61%). Just over half of the participants strongly agreed or agreed that that Recommendations are accepted and supported by the organisation (n = 58/100, 58%) and are aimed at the appropriate level (e.g., ward, department, hospital) of the healthcare system (n = 56/99, 57%).
Only half of the participants strongly agreed or agreed that: Investigations consider what went well, as well as what went wrong (n = 54/100, 54%); that Healthcare organisations should be able to decide not to investigate an incident if no new information is likely to be gained for learning and improvement (n = 52/98, 53%); that Learning from previous incidents prevents reoccurrence or repeat incidents (n = 53/100, 53%); and that Investigators have access to the right tools, guidance, and support to conduct high-quality, systems-based investigations (n = 51/100, 51%), and have the right knowledge and skills to undertake investigations and recommend change (n = 50/99, 51%). Less than half of participants strongly agreed or agreed and that recommendations from investigations are achievable (n = 45/100, 45%, while 42% neither agreed nor disagreed).
Approximately half of the participants disagreed or strongly disagreed that Lessons learned from incidents outside their organisation are shared with them (n = 57/100, 57%), that Lessons learned from incidents were well communicated across their organisations or shared from outside their organisation (n = 44/99, 44%, while 31% neither agreed, nor disagreed), and that Recommendations are reliably implemented (n = 41/98, 42%, while 39% neither agreed, nor disagreed). Most participants neither agreed, nor disagreed that Recommendations lead to real improvements in patient safety (n = 40/100, 40%, while 36% agreed/strongly agreed) (Figure 1).
Qualitative data
Individual interviews (n = 32 participants) or focus group (n = 78 participants across 25 focus groups) were conducted with participants across Australia (n = 99) (Victoria (n = 31), Queensland (n = 31), New South Wales (n = 29), the Australian Capital Territory (n = 7), and one other Australian state (n = 1)), and internationally (n = 11) (across the United Kingdom (n = 6), New Zealand (n = 3), Japan (n = 1), and Canada (n = 1)). Each interview and focus group ran for approximately 60 min, equalling a total of 57 h of data collection. Results from Australia and the international cohort are presented together. The thematic analysis of the interview and focus group transcripts identified key strengths and challenges of the PSI response process across three key themes: Selection of PSI Reviews; Reviews, Recommendations and Implementation; and Health Organisations and Wider System Influences (Figure 2). Exemplar quotes supporting the themes and subthemes are included. To maintain anonymity, quotes are labelled using participant codes and demographic data have not been presented alongside quotes.
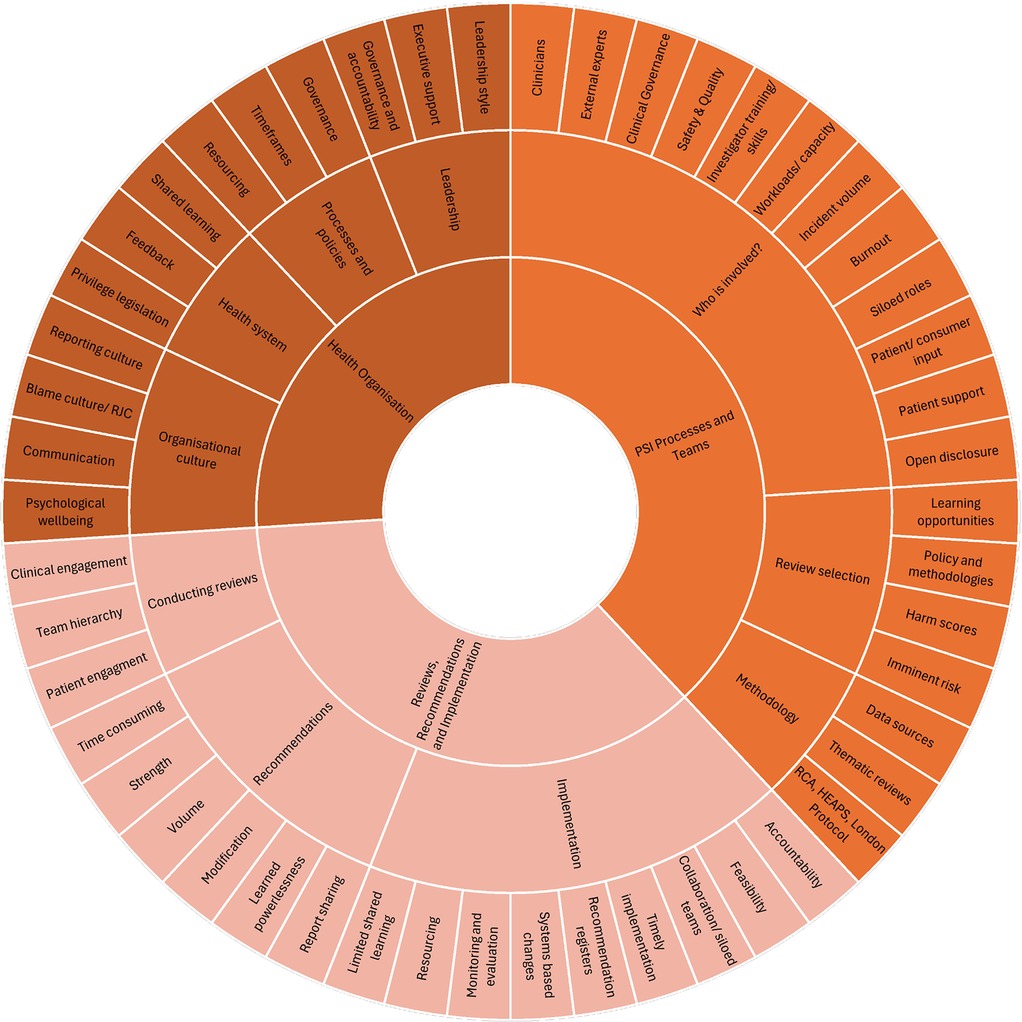
Figure 2. Themes and subthemes from the thematic analysis of the interview and focus group transcripts of the PSI response process.
Selection of patient safety reviews
How PSI reviews are selected
Participants indicated that all reported PSIs are assessed in one form or another, depending on the severity and outcome of the incident, to learn from and prevent recurrence. However, the depth in which they are reviewed is variable. Imminent risk is reviewed, and strategies put in place to prevent the incident from reoccurring in the short term. Participants discussed how the PSI review process is typically guided by triage using the incident harm score, as to whether the incident requires in-depth investigation or a more rapid review. The treating clinician or nurse reports the incident, within incident management software, and the severity score is assessed and verified. Participants noted that there was often misunderstanding of the criteria for different harm scores by the reporting clinician, resulting in more incidents being categorised as having a more severe harm score than necessary. Participants also noted potential for conflict of interest when line managers verify harm scores. They explained that incidents, initially rated as severe or serious (e.g., with a SAC, ISR or Harm Score 1 or 2), are typically triaged by an executive director, reviewed and finalised by an executive committee, and that harm scores are commonly revised to a lower harm level. Participants described how committee meetings may discuss a range of incident types with different severity levels. In addition to validating the harm score, they decide which methodology will be utilised to investigate the incident and assign review team members to conduct the review. It was highlighted that this executive review can be delayed, however, if executive staff are time poor.
Participants detailed how lower severity incidents may be reviewed by a Morbidity and Mortality review team (M & M) meeting, or a local line manager, discussed at Grand Rounds, or reviewed via a desk top review by the quality and safety team or a local ward/department clinical manager. These incidents are typically reviewed through a rapid review methodology or not at all in any meaningful way. If there is significant opportunity to learn from the incident, then an executive team may commission the patient safety team to lead a more in-depth review. Consideration may also be given to potential for harm, particularly in near miss events.
Participants explained how across different jurisdictions, policies dictate whether incidents with high harm scores are mandated to be reviewed using specific in-depth review methodologies [such as a Serious Adverse Event Review (SAER) for harm score 1 incidents in NSW] (17). They noted that this process may not specifically consider whether a comprehensive review would provide opportunities to learn from the incident. When not bound by such legislation or policy, the opportunity for learning from the incident is often considered to select the most appropriate review methodology.
Participants reported that serious incidents including those resulting in death or permanent harm make up a small proportion of incidents that occur annually but consume the vast majority of resources to conduct in-depth reviews (often in response to legislation) that tend to be reactive, case specific and focused on behaviour. They identified that this limits the opportunities and resources to review and learn from lower harm incidents, and near misses through proactive and preventative improvement work that aligns with a systems-thinking approach. For certain incident types, such as falls, or when a system wide issue is identified (similar events occurring across a hospital), participants explained that a rapid or thematic review may be conducted. Compared to an in-depth review, many felt that this rapid review option has the benefit of releasing resources for other in-depth investigations of serious harm events, or lower harm events and near misses, as well as the implementation of review recommendations.
“Someone in their 90s who’s had a fall in the hospital…not saying we don't review those, but can we do that through a one pager checklist, which is kind of what we did in COVID. We very much want to free up for those [reviews] that really have a lot of opportunity for learning” Participant 19, NSW
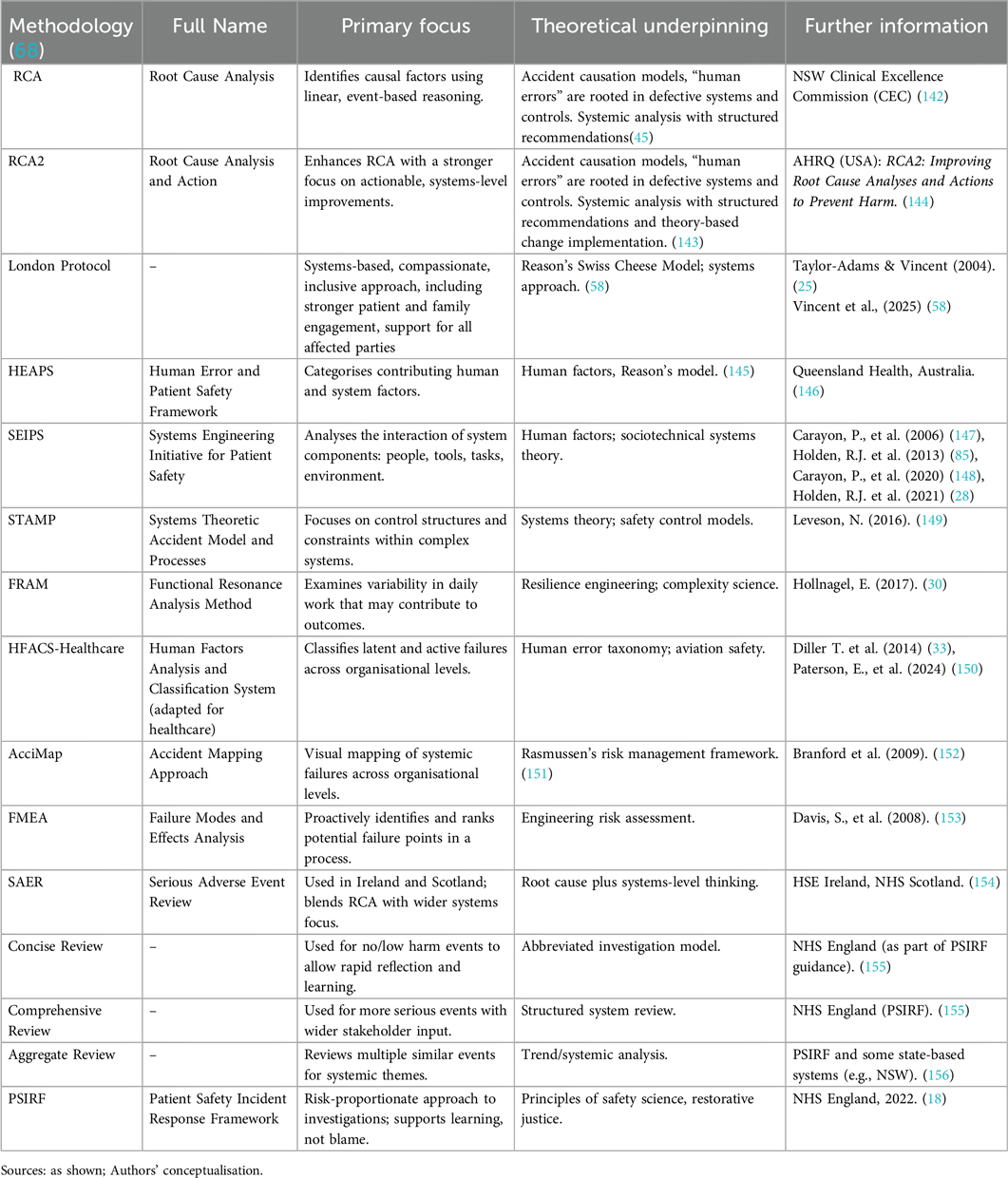
PSI review methodology
Participants discussed how they utilise various investigation methods during PSI reviews. Commonly described methodologies included Root Cause Analysis (RCA), the London Protocol, Human Error and Patient Safety framework (HEAPS), Root Cause Analysis and Action (RCA2), Concise and comprehensive reviews, and the Accident Mapping Approach (AcciMap), as well as methods such as audit and feedback, cause and effect analysis (Fish bone diagrams or Ishikawa analysis), Five Whys analysis, and more rapid processes of review by Morbidity and Mortality teams using a template. In our study, RCA and RCA2 remain the dominant method in many Australian states and territories. The international participants also reported using Functional Resonance Analysis Method (FRAM), Systems Theoretic Accident Modelling and Processes (STAMP), Hierarchical Task Analysis (HTA), Systems Engineering Initiative for Patient Safety (SEIPS), The Patient Safety Incident Response Framework (PSIRF), as well as the Yorkshire contributory factors framework and the Learning Review Methodology (See Box 2).
There was no consistent methodology reported to work well across different incidents. RCAs were perceived by participants to have limited effectiveness, learning opportunities and capacity to share findings, and incidents reviewed by RCA (typically high severity) were often protected by legal privilege legislation. Thematic reviews of high frequency and similar events that occur across a hospital were perceived to achieve change in practice and patient outcomes and seen as helpful tools to analyse commonly reoccurring incidents from a systems perspective.
“So, you know because SAC 1 is a myopic view of an incident that’s occurred to typically one person or a family…If they are aggregated then it tends to help change systems” Participant 30, QLD
A small number of participants described conducting thematic reviews themselves, with some noting that if a patient's family wanted individual findings and action, then an individual comprehensive review was typically conducted. Participants however felt that individual reviews often did not effectively capture contextual data around the incident. They noted that reviews in Australia tend not to undertake secondary observations of standard clinical practice and tend to rely on interviews and medical records as their key data sources, whereas in the UK, observations have become a well-regarded source of data to inform incident reviews.
“The observational work offers a lot more to us because I think that’s our segue between being a very traditional, ‘What happened to this person and why?’, to a broader understanding of ‘How do things normally work and how would you factor that into this thing happening?’’ Because that thing wasn't unique. That could have happened any day. It just seemed to happen this once and it could happen again. Why? So, the observation work, makes a difference in whatever we do. It’s really important” Participant 31, International expert (Healthcare leader, United Kingdom)
Who is involved in patient safety incident reviews?
Participants described how PSI review teams may be commissioned by a senior executive such as the Chief Executive Officer, or an executive triage team. Establishing an investigation team was seen as a fundamental step in the PSI review process as it requires careful planning for balance of clinical specialty subject matter expertise, experience and independence, and is time consuming. Getting buy-in from busy, senior clinicians, nurses and heads of units was identified as challenging with operational demands given precedence. Participants described how the ideal PSI team would include independent experts external to the organisation, but that recruitment is reportedly variable and challenging for those roles. Participants felt that independent panel members can bring expertise around systems thinking and human factors, dedicated focus, and encourage accountability and professionalism.
“[External experts] bring some expertise around systems thinking, around human factors. It also brings in a level of accountability. Everybody kind of behaves in the room well and follows the process a little bit better if there’s somebody external that they think is watching them” Participant 22, VIC
Participants also highlighted that proxy representation of the individual staff involved in the event (staff in similar roles with similar levels of experience) may also be included in the review team. While engaging with and interviewing individual staff directly involved in the incident provides valuable insight into what occurred, concern was noted that their perspective may bias a review, by reducing objectivity, and thus their inclusion on the review panel should be avoided. Participants felt that the chair of the PSI review panel should have human factors knowledge and systems-thinking experience, as well as clinical expertise relevant to the incident, without having been directly involved, as they play an important role to facilitate input from panel members in a non-hierarchical manner. Support by administration staff was also perceived to be beneficial for reviews teams, to reduce the logistical and organisational burden involved with conducting an incident review.
To be a skilled investigator, participants felt that individuals need clinical knowledge, expertise in systems thinking and human factors as well as a strong understanding of investigation methodologies and general principles. Review team members, however, were often perceived to lack experience and knowledge of those paradigms. Training and experience of review team members was reportedly variable across jurisdictions, partly influenced by high staff turnover, and limited training resources and courses available. Participants noted that inexperienced team members need additional training and support to conduct reviews and produce high quality reports with Specific, Measurable, Achievable, Relevant and Time-bound (SMART) recommendations. They described the same challenges for inexperienced quality and safety staff who require on the job training, adding to the workload of quality and safety teams. Staff working in higher volume metropolitan hospitals were perceived to have greater incident review experience, compared to lower volume rural and remote sites. More broadly, participants stated that review team members need capacity to conduct reviews, but that this is impacted by high workloads and limited time. Participants also noted staff burnout and frustration that despite effort and emotional investment during the review process, changes to care often do not eventuate.
Safety and Quality and Clinical Governance staff were perceived to provide expert guidance, facilitate reviews for serious harm incidents, and provide support and resources for lower harm incidents. They are also perceived to support the review team once the report is drafted, enabling refinement of recommendations, and providing insight regarding similar concurrent improvements projects to avoid duplication of work and share findings. While safety and quality staff are typically skilled clinically, participants expressed concern that they are not always remunerated in parallel to more high-paying clinical roles, and this in combination with the workload and emotional impact of the job, may contribute to high staff turnover. Participants noted that this high staff turnover in turn translates to constant training of new staff. Safety and Quality and Clinical Governance roles were perceived to have become siloed in some jurisdictions, limiting opportunity to learn from and collaborate with each other. Participants noted that a strong community of practice is needed, but not always available, to support and facilitate collaboration across (siloed) quality and safety teams.
Depending on the jurisdiction, participants reported that some review panels include consumer representatives (CRs), particularly in Victoria where it has been encouraged in policy. Participants generally considered CRs to be a valuable addition to the team, bringing a different perspective to the review. However, participants noted that CR involvement requires careful facilitation, executive support and training both for the CR, and the review panel. Participants described how effective engagement with CRs requires facilitation by the review panel Chair to ensure the wellbeing and psychological safety of the CR and the panel staff. Consumer input was considered useful by participants, even if the consumer is not directly on the review panel, with consumer review of reports and findings to be helpful.
Engagement with, and seeking input and feedback from, patients and family members about the PSI and review process was reportedly variable, but valued, adding depth to the review if facilitated sensitively and supported through staff training. Participants described how this may be conducted by a dedicated family contact (DFC, in New South Wales for serious incidents), a liaison staff member dedicated to support families, or a social worker, who aim to engage with patients and families, support them throughout the review process, and act as a point of contact. Participants noted that DFCs should also provide additional information around the review progress, findings and actions, as well as linking families to additional support services. However, this is variable across jurisdictions and was identified as an area for improvement.
Clinician disclosure to patients and families is conducted by the treating clinician, typically shortly after the incident. Participants noted how important this step is, but how variable the quality of the disclosure can be, influenced by the level of staff experience, training and confidence, as well as the organisational culture around clinician disclosure being conducted after an incident. Participants described how open disclosure, a process which includes an apology, is then conducted by independent staff members, such as quality and safety or executive clinical directors, typically before the review process begins. This process is embedded in the mandated Victorian Statutory Duty of Candour process, which participants noted has improved engagement with consumers. It was noted that patients and families may then be provided with a second open disclosure process about the review and findings, once complete.
Reviews, recommendations and implementation
Conducting reviews
The key purpose of a PSI review is to identify what went wrong, to learn from the incident and to prevent reoccurrences by identifying and implementing recommendations. Consulting with staff who were involved in the incident, as well as those likely to be affected by the recommendations including medical directors with oversight of staff and teams, was deemed useful, but variable in practice. Clinical engagement during the PSI review process was identified as a key challenge, when medical staff are reluctant to participate in the review process. Participants posited that this may be related to the Visiting Medical Officer (VMO) model, particularly in rural and regional areas, where clinicians are appointed to teams for short periods of time and therefore are not well integrated into the local system.
Consulting with the teams directly involved in the incident, and those who will be impacted by the recommendations was considered important, to capture their perspectives, and to support them after the incident, particularly when staff distress is identified. Participants felt that engagement with staff directly involved in the incident [acknowledging the second victim experience (95, 96)], needs to be managed carefully however, as the process of review can add to their trauma. Consulting with safety and quality or consumer engagement staff who are not directly involved in the review, was also identified as a useful quality check process to ensure rigour in the review process and findings.
Team hierarchy was perceived to influence the recognition of some review team members, influencing their input into report findings. Another challenge noted by participants was the introduction of new incident management or Electronic Medical Record (EMR) systems. According to participants, if staff do not know how to navigate new systems well, information may not be captured adequately, impacting the quality of analysis in the review.
In terms of engagement with patients and families while conducting the review and developing recommendations, participants reported variation in the formal processes used to hear the patient perspective, and what they want the review to achieve, as well as how this is considered and documented within the review report. This was identified as an area for improvement by most participants. Participants raised concerns about patient and family vulnerability and how this perception can lead to their exclusion from participation in reviews, though this remains a subject of ongoing discussion.
Developing recommendations
Participants posited that effective recommendations reflect a thoughtful and in-depth analysis of the contributing factors, address system and process change and clearly link to appropriate implementation strategies. Developing meaningful, concise, clear, and effective recommendations that are measurable, achievable and implementable, was identified as a challenging, time consuming, resource intensive process, requiring skill and engagement with large clinical teams. Participants felt that following SMART (Specific, Measurable, Achievable, Realistic and Timely) principles can support the development of quality recommendations. Consulting with past reviews of incidents (both locally, intra-state and nationally) was also considered to be helpful in learning about effective recommendations. However, this can be challenging as it relies on individual networking, with no current infrastructure available, or secure permission system, to search for such information easily.
Participants described how clinician workloads and lack of time to conduct the review and formulate recommendations can limit the quality of outputs. Participants also noted it was challenging to get busy clinicians to engage in review training to further develop skills. Development of recommendations by team members without relevant clinical experience or without consultation with relevant clinical staff was perceived to impact the applicability of recommendations. This was noted as a particular issue in rural settings, when external but non-rural clinicians may develop recommendations without contextual understanding of the setting, limiting the applicability of their recommendations.
Participants noted a tendency to develop weak and ineffective recommendations and attributed this to the fact that recommendations are an expected review component, and team members feel compelled to make recommendations. They felt that the resulting large volume of weak, standard, “go to” recommendations (such as to change a policy or educate a staff member or specified group) have resource implications by detracting resources from the implementation of higher quality recommendations. Participants described how clinicians may lack implementation science training/expertise limiting their use of evidence-based recommendations and behaviour change techniques. Participants noted that there are efforts in some jurisdictions to minimise the number of recommendations and ensure final recommendations are concise and strong.
Participants explained how incident analysis reports and recommendations are typically reviewed at various executive levels, modified as appropriate, finalised, endorsed by a general manager or clinical director, and signed off by a senior executive. Support and engagement with quality and safety teams, executives and leadership prior to formal sign off meetings was seen to support quality recommendation development. This process was also seen to help refine and strengthen recommendations, to ensure they are effective and sustainable, provide expert but independent advice and alert teams to similar recommendations or improvement work implemented elsewhere within the organisation, and to minimise the timeframe for signoff by executive.
On the other hand, participants noted that recommendations may be amended and weakened at the executive endorsement and sign off stage. This ‘sense of learned powerlessness’ was a common challenge discussed [a term that originates from the psychological phenomenon of learned helplessness (97)], when an issue and solution is identified, but no corresponding recommendation is made in the final report because system and resource-intensive recommendations are often seen as unfeasible, unrealistic, or unlikely to be approved by executives. Participants felt that they had limited authority to recommend meaningful changes. Participants reported that PSI review reports and findings are often influenced and modified by executives who are conscious of political or media pressure, as well as concern about reputational damage, or that certain recommendations could be interpreted as criticising health service organisations. They felt that such reactive responses to political and social influences can influence review processes, result in weaker recommendations and undermine the aim of the process. For example:
“You then go back with the draft report to the executive and more often than not, the initial response is defensiveness. ‘No, you can't say that. No, did you really find that? And I don't think you've shown that, have you’, regardless of the methodology that was used and the evidence that’s presented. I think that it’s human nature, right? People don't want to hear that there’s wrong in their house. And especially if the answer is that there’s going to need to be an investment in resources into trying to fix it. It’s very difficult to create change. And I think that boards and executive don't necessarily recognise that that change has to come from the top. It’s always a sort of a look down focus. ‘OK, how do we make these people at the at the pointy end work harder and work better?’” Participant 9, VIC
There was large variation noted as to whether review reports (or their drafts) are provided to patients and families, or findings simply summarised, with participants reporting that some organisations only provide reports to families following a Freedom of Information request, while others share both the draft and final reports. Participants noted that reports about higher severity incidents were often shared with families, however, reports or summaries of findings for lower severity incidents are typically not shared. Participants felt that sharing the draft report with families provides an opportunity to gather their perspective and input on the findings and recommendations, and the inclusion of a plain language summary can be beneficial. Several participants noted that often reports are not well received by families, as they inadequately capture the family's experience and trauma. Consideration of the benefit or impact of an incident review for patients and families, as well as staff wellbeing, was also considered important.
Implementing recommendations
Participants described how report findings and recommendations are uploaded into an incident management system and a timeframe is set for implementation based on the KPIs and policy of each jurisdiction. The implementation process may then be tracked and monitored through that system by safety and quality teams who are typically not tasked with responsibility for implementation, however participant responses suggest this is variable. Participants explained that in some jurisdictions, quality coordinators coordinate with clinical business units to facilitate the implementation of recommendations, document and monitor the process, and provide evidence back to the units. They noted that recommendation implementation may be monitored by executive committees and safety and quality teams, reporting on the progress and completion as appropriate. Participants reported this process to be variable in Australia and internationally with poor monitoring negatively impacting on effective implementation, sustainment and achievement of change. They posited that this may be as the development of recommendations and their implementation may be tasked to different siloed teams, limiting follow through and accountability. Participants were enthusiastic about the benefits of recommendation registers to support the tracking and monitoring of the implementation of recommendations, particularly when accountability was tasked to a position, rather than an individual, to account for staff turnover. Assigning recommendations and their implementation to appropriate senior staff who are responsible for the achievement of change, and who can delegate the process, was considered an important facilitator to this process. However, this was also noted as challenging when recommendations relate to multiple areas in the health service as opposed to a single ward.
When implementation of a recommendation is monitored, participants highlighted that evaluation to ensure fidelity (implementation as intended) and assessment of the quality of outcomes is variable. Quality monitoring and evaluation were considered important to establish evidence regarding strategies that successfully impact care and patient outcomes to garner support for sustainability and scale up of the change, or to apply improvement strategies to other areas. Dashboards tracking recommendation implementation, regular meetings, and biannual reports were perceived as ensuring accountability and support implementation:
“My level of confidence is growing. SAC 1 and SAC 2 recommendations are monitored in a live dashboard that is able to be searched by each of our directorates… We monitor it through the Executive Safety and Quality Committee, and they're also internally monitored by the Directorate Safety and Quality meeting…Whilst I have reporting that says someone has signed off that the recommendations have been implemented, we're not great at having a checking process to check that that’s true. And we had an internal audit process in the last 12 months that showed us that we were not, and that we need to actually implement that process of an audit process more effectively. We're working on what that might look like at the moment. But I don't believe, given that many of the old recommendations were nonsense, I don't believe most of them had been properly implemented at all” Participant 36, QLD
According to participants, the implementation of recommendations associated with serious incidents tends to be tracked; however, this is often not the case for lower harm incidents. Participants noted the high frequency of particular incidents reoccurring, resulting in similar review recommendations being developed but not effecting change, and how this indicates a need to enhance the quality of recommendations and their implementation. Implementation was perceived to have fewer resources and time allocated, in comparison to the review process. Participants noted that this results in recommendations and their implementation not achieving intended changes to care practices and patient outcomes. Similarly, participants reported that it can be challenging when funding dedicated to implementing a specific recommendation ends.
Participants explained that nurses in leadership roles (for example, Clinical Nurse Consultants and Nurse Unit Managers) or clinicians, are often tasked to implement recommendations in their teams, or areas, despite not always being familiar with the context, incident or contributory factors underpinning the recommendation. Hierarchies and power dynamics across teams were perceived to make it challenging to establish clinician buy-in with the implementation of recommendations, with both issues challenging engagement and the potential to influence change across a hospital. Greater collaboration and interdivisional agreement on implementation action plans was perceived to improve buy-in and holistic understanding of the drivers of change. Participants reported that high staff turnover also leads to loss of institutional knowledge and understanding of the review underpinning the recommendations, impacting the implementation of recommendations. While recommendations and implementation plans may be documented within the original reporting software, long-term monitoring of the implementation of the recommendation, and outcomes achieved was reported to be variable, particularly after the implementation process has been signed off.
Frustration was reported that recommendations and their implementation strategies get modified through various bureaucratic processes. Final implementation plans were often perceived to differ to what was intended by the review team, limiting the accountability for effective implementation. Staff turnover at the management or executive level was seen to contribute to this, leading to limited accountability when implementation is person specific, rather than role specific. Participants felt that management and executive role-accountability supported implementation and facilitated change. Participants also highlighted a tension between being reactive to an incident while also providing enough time for a quality review and implementation process. Timely but effective implementation of recommendations was considered fundamental, to ensure those involved feel confident they can enact change.
Weak recommendations that are not specific or measurable, were seen to be challenging to follow up and implement, making implementation an ineffective tick box exercise that rarely achieves the intended change to care practice or patient outcomes. However, participants reported that even strong recommendations may be poorly implemented with limited support and expertise to guide the process. Despite the weak nature and limited evidence for education alone as a behaviour change strategy, participants described how education-based recommendations are often recommended. This is in favour of more challenging systems thinking-based recommendations. Participants felt that system-wide changes are particularly difficult to implement, as they involve cooperation and coordination of multiple interdivisional and inter-organisational stakeholders, particularly in jurisdictions with devolved health services. They were also perceived to be more resource intensive, and therefore not always perceived as feasible. Participants noted limited shared learning about recommendations and implementation strategies that have been effective elsewhere. Participants noted that access to this information would be useful to support the development of more robust implementation plans. Providing patients and families with updates on the progress of implementation, sometimes as a part of the open disclosure process, was also variable, as staff felt some families were not ready to engage in the process, whereas others were keen to be updated.
Health organisation
Organisational processes and policies
Participants reported that there were generally clear, mandated review, governance and accountability processes to follow for incidents. They held that regular quality and safety meetings provide support to collaborate, and monitor, conduct preliminary assessments, assess the review criteria thresholds to determine the required methodologies for incident reviews, and support open disclosure and implementation of recommendations processes.
A commonly reported challenge for participants was the strict timeframes and associated Key Performance Indicators for the PSI review process to be initiated and completed within. Participants noted in QLD, for example, reviews of PSIs with a Severity Assessment Code 1 (SAC1) [equivalent to Harm score 1 in NSW, or Incident Severity Rating (ISR) in Vic] must be completed within 90 days. These timeframes were described as being unfeasible for overworked staff, particularly for complex incidents involving multiple clinical specialties requiring enormous coordination and engaging with an often part-time workforce. Resourcing challenges were discussed regarding a lack of staff and time, challenging and delaying the completion of reviews and findings. On the other hand, deadlines were also perceived to keep participants accountable. Adding to these challenges, the reporting management systems commonly used were not considered to be user friendly.
“Sometimes they're really rushed at the end of a process because the 60 days is so tight. So, there’s a risk there. And, and there’s been conversations definitely at the DCG level [Director of Clinical Governance—a role at a health service] around wouldn't it be wonderful if we had 60 days to do the findings report and then another month to do the Recs [recommendations] so we could really put some nice thought and planning into the recommendations. Often, they are weak if we look at sort of the hierarchy of recommendations and then they're often not implemented or the process for follow up or sustainability is weak” Participant 11, NSW
The value of undertaking individual reviews for certain incident types (such as falls) was queried, with participants expressing frustration at the resource intensive comprehensive review process that often results in limited learning. Participants explained that policies to assess the need for a comprehensive review lacked flexibility, leading to duplication of work through individual reviews of similar events, without learning from previous reviews, suggesting in some circumstances cluster/thematic reviews may provide greater value.
Broader health system
Similar to local organisations, participants reported limited sharing of learnings across health services, with siloed services and clinicians unaware of incident reviews and implementation strategies conducted elsewhere, and limited opportunities to learn from exemplar reports from inter and intra-state. Participants noted that certain jurisdictions are also bound by Qualified Privilege or Statutory Immunity legislation, which limits the capacity to share findings. Some participants reported limited comparative feedback from statewide or national departments of health about the quality of the review report and findings, limiting staff opportunities for learning,
“We don't actually get feedback from [statewide bodies] to say ‘We really liked what you did here’… I think that’s one of the failures in the systems of why it doesn't get better because we're just not getting that feedback or shared learning” Participant 14, (state suppressed)
Leadership
Participants indicated that leadership style influences the incident review process and culture around reporting. Transparent and collaborative leaders, with dual governance or safety based leadership and clinical roles support the culture of reporting PSIs, as well as systems thinking, while minimising blame and focusing on opportunities to learn from incidents and near misses. Executive support was considered important, providing broad oversight of the incident review process and guidance through legislative requirements, supporting communication with families, and endorsing review reports. However, participants also felt that executives were cautious of political influences, and wary of identifying contributory factors to an incident in a review that could be interpreted as criticisms of health departments. Similarly, participants identified that executives may amend final recommendations that have an operational impact and require resourcing for improvements, resulting in weaker recommendations.
“There’s often a fair amount of management input to reshape the recommendations. [They] tend to get a bit … modified by the time that it actually gets to the [Statewide body] … anything that involves resourcing. So, the overarching challenge with all of this is that the people who are conducting the reviews are constrained by the fact that many of the recommendations that they would like to make have operational impact and resourcing impact” Participant 2, VIC
A robust governance and accountability system was seen as a key strength to support the development, implementation and evaluation of evidence-based recommendations that are likely to be effective and sustainable. International experts identified this as an area to focus improvement efforts on, to enhance reporting, analysis and accountability, and reduce the siloed nature of services.
“It’s quite siloed. There’s so many statutory bodies set up at different levels of a system, but all statutory bodies and the responsibility and accountability and escalation and management of risk is very much more muddied” Participant 3, International expert (Policy advisor, New Zealand)
Organisational culture
An open, transparent and restorative just culture with a systems thinking focus was touted as a fundamental element to patient safety, to encourage reporting with timely feedback. A positive reporting culture was perceived to be improving across Australia and internationally, albeit slowly, encouraging staff to be open about incidents, but needs continuing investment to develop further. Participants noted that improvements to this culture can be hindered by staff turnover. Resistance to incident reporting remains a challenge, with participants noting under reporting or insufficient escalation of incidents, partly a result of staff not understanding the escalation and governance processes.
Participants highlighted the importance of listening to consumer voices was as component of a just and learning-oriented reporting culture. From their perspective, meaningful involvement of consumers and their families in the review processes should be carefully supported and embedded, not as a procedural task, but as an ethical commitment. Several participants acknowledged that complexities involved, including the vulnerability of those affected. Similarly, ensuring that clinician disclosure is conducted consistently, and that clinicians are well trained and consistently supported to conduct disclosure. was identified as another important improvement that needs to be embedded within the review process. Some participants noted that while strengthening a strong culture of reporting is important, if not managed carefully, it may also increase the workload of quality, safety and improvement teams.
“We’ve really got good clinician engagement in open and transparent reporting. So, we feel like we are almost having a bit of an over reporting process at the moment. People are putting in absolutely everything and we're having to really review and peel back” Participant 5, VIC
Participants discussed how many health services still face the challenge of overcoming a blame culture, embedded from the executive level down, and strive to ensure that the restorative justice message is consistent at all levels of the organisation. Poor and inconsistent communication, a lack of transparency and prevailing blame language were perceived to counteract efforts to bring about organisational cultural change, and efforts are required to address misconceptions staff hold about punitive consequences of reporting incidents. This is particularly challenging when staff are overworked.
“One in four or five people on the panel will be someone who we need as a subject matter expert, but will be coming with that perspective of, ‘This is just because Susie made that mistake’” Participant 4, VIC
Participants felt that some individuals and organisations harbor concerns about reputational damage resulting from PSI reviews. A lack of psychological wellbeing support for staff conducting the reviews or involved in the incident was also noted. In some cases, the trauma of the incident, and the review process, was reported to result in staff leaving their positions, losing valuable human and organisational knowledge in the process.
“There’s a reluctance and a fear of reputational damage in healthcare, and people don't want to be seen to be getting things wrong. And then that’s going to stifle the learning. And I think that’s just a cultural thing, which is a very big challenge to overcome” Participant 3, International expert (Policy advisor, New Zealand)
This lingering blame culture was seen to result in limited opportunities for shared learning from incidents, and near misses. Participants noted that learning can be further limited by the siloed nature of health services and teams leading to duplication of improvement work, with poor dissemination of findings from reports or thematic summaries of incidents, and limited sharing across teams, organisations, and health systems. Participants also felt that sharing can also be hindered by confusion around Qualified Privilege or Statutory Immunity legislation (98) and the limitations that it places on data sharing. Participants noted that findings from reviews are often not shared with the staff who reported the incident, which may discourage staff from reporting future incidents if they feel nothing was actioned by their report. Similarly, quality and safety teams may share findings from reviews, or thematic analyses with executive or senior staff, however participants noted that this information may not reach the clinicians on the ground who may be impacted by the implemented recommendations, nor the reporting clinician or clinicians who were directly involved in the original incident.
Comparison of qualitative and quantitative data
Survey data and interview and focus group data were compared and triangulated to provide a more in depth understanding of the key concepts. These findings were generally concordant or complementary (describing different facets of themes) (73). There were a few discordant findings: In the survey, most participants agreed that Investigations consider when work processes and systems may have contributed to an incident and the Investigators consider human factors and contextual factors that impact human performance. These were two points that participants highlighted as needing further development in the interviews, suggesting that systems thinking and human factors, and broader system change were not always adequately considered or reflected in PSI review recommendations. Similarly, the interviews identified that many reviewers felt despondent that implementation of recommendations resulting from PSI reviews was often ineffective, whereas two thirds of survey responses agreed that Actions taken in response to investigations prevent similar incidents from reoccurring. Two thirds of survey responses felt that individuals were not unfairly blamed during the review process; this may still be an area needing further development, with interview findings highlighting an ongoing culture of blame in some organisations. These discordant findings may reflect both how participants view the purpose of PSI reviews identified in survey responses, as well as the practical challenges to achieving those purposes identified in the interviews and focus groups. It is also worth noting that findings from the Australian cohort, across the four states and territories were largely aligned with each other and with responses from the international cohort.
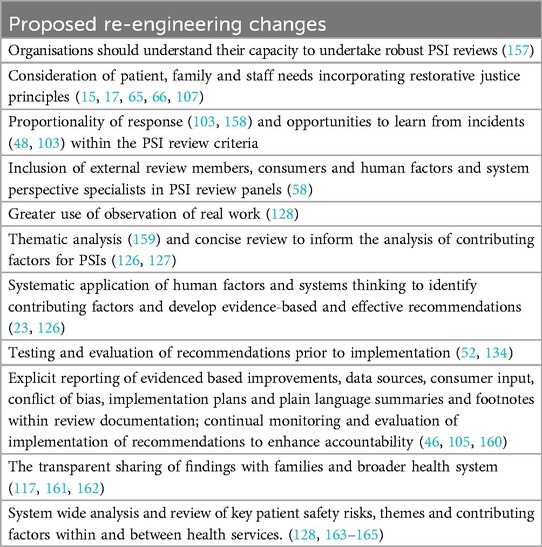
The key themes and subthemes have been mapped against the CFIR framework (93) to systematically analyse the key strengths and challenges to PSI reviews and implementation of recommendations. This process categorises and highlights key elements that are likely to influence the effectiveness of incident reviews across five domains: Characteristics of patient safety review process and implementation of recommendations (Innovation domain), External environment and context (Outer setting domain), Internal context (Inner setting domain), Characteristics and attitudes of practice staff and clinicians (Individual domain), Patient safety review implementation (Implementation process domain) (Table 2). These key determinants will inform the proceeding study to codesign a system-wide improvement to support the PSI review process.
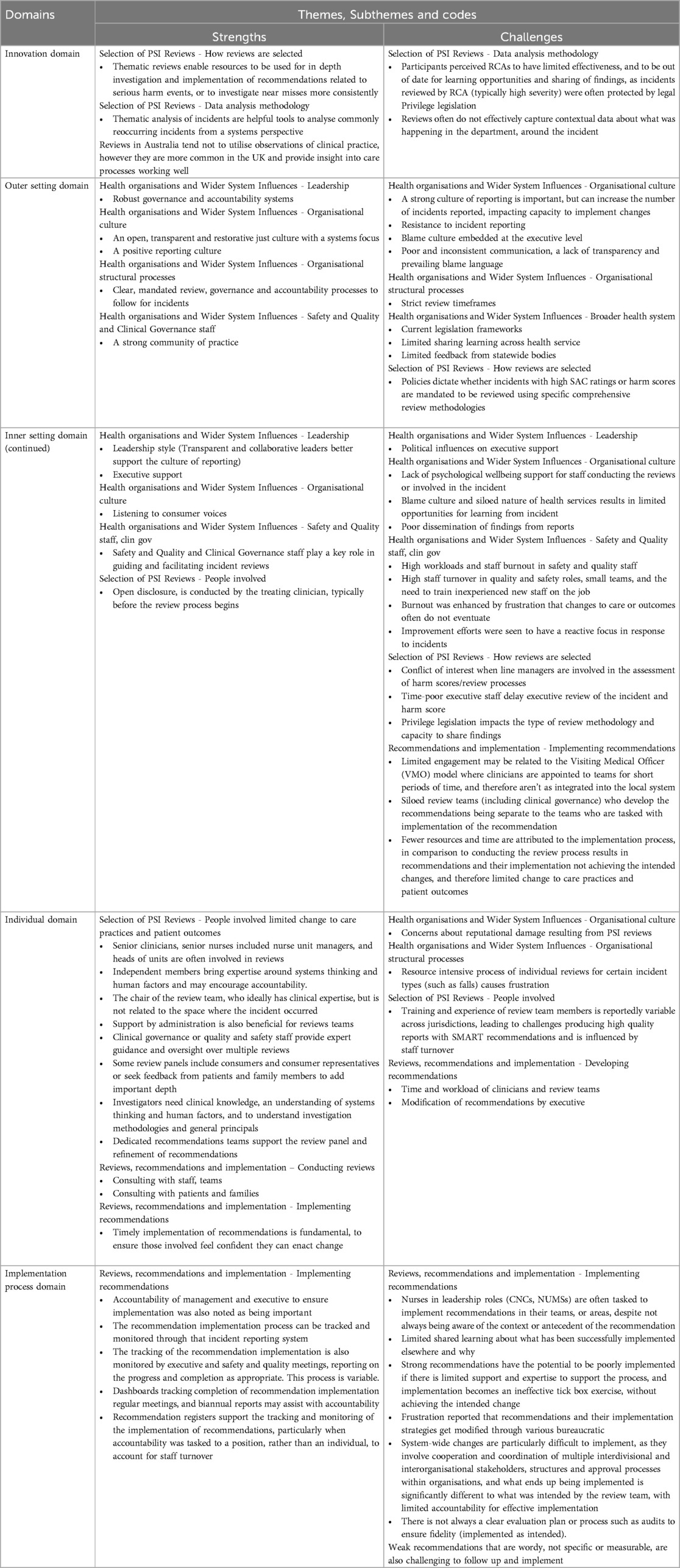
Table 2. Application of CFIR components to highlight facilitators and barriers to implementation of patient safety investigations [based on model by Keith 2017 (93)].
Discussion
This study identified key challenges in the incident review process. Despite strong efforts to reduce a blame culture, resistance to reporting and blame persists in some organisations, while reducing over time in others. We observed: a lack of systematic consumer involvement in the PSI review process; limited independence within the PSI review process; shortcomings in shared learning across organisations and health services, including limited feedback on review findings, which impacts opportunities to improve; variability in the strength of recommendations resulting from PSI reviews, with few recommendations underpinned by systems thinking; poor development of implementation monitoring and evaluation strategies; limited governance and accountability for the achievement of change resulting from PSI reviews and the implementation of recommendations; and a need to re-balance the resources spent on in-depth PSI reviews vs. conducting more concise or thematic reviews and QI improvement efforts.
Modifying the underlying blame culture
A blame-free approach to incident reporting, analysis, and learning has long been acknowledged as the most appropriate for effective prevention (99). The present analysis indicates that a persistent blame culture in some settings continues to be present. These findings suggest that further work is required to fully remove the blame culture from PSI, but that various barriers remain. The patient safety culture in a healthcare organisation underpins the reporting of incidents, the attribution of blame and embedded restorative just culture (100). It supports the identification of areas for improvement, evaluation of patient safety interventions, and benchmarking, through processes to effectively learn and improve from incidents (100). Hospitals with higher patient safety culture measures are associated with fewer adverse events (101). Similarly, a restorative just culture can enhance incident reporting, transparency, opportunities for learning, and psychological safety for staff involved in an incident (62, 102) [the second victim experience (95, 96)] by shifting the focus towards Safety-II which seeks to understand the everyday processes that work well (103). It is associated with increased performance resilience (104, 105), enhanced quality of review recommendations and lower rates of mortality (102, 106).
Systematic consumer involvement in the PSI review process
This study identified wide variability in the involvement and engagement of patients and families, to understand their needs from PSI investigations, the questions they want asked, and hearing their perspectives on what happened. This cohort can provide valuable insight into the PSI, prioritise issues, and provide guidance on what they want a PSI review to achieve, in the hope to gain closure or regain trust in the healthcare organisation (65, 66, 70). Systematic engagement with this cohort is needed as we strive to improve the PSI response process and reduce patient risk of harm.
The findings also point to variability in the engagement of CRs within the PSI review process (70). Meaningful engagement of this group within the review process, particularly when it is more than a one-time engagement event (107), can provide alternative and broader perspectives (80). In general, the participants in this study recognised the value that patients, families, carers and CRs could add to PSI reviews, and were supportive of and working towards improving this process. There is an opportunity to make CR engagement more explicit and consistent by embedding it in organisational policy, providing structural training and resources (70). To maximise effectiveness, the provision of resources, tools, and training for staff and consumers is needed to facilitate meaningful engagement and input from patients, families and CRs (63).
External contributors to the PSI review process
This study identified variability in the inclusion of external contributors to PSI review panels. Involving individuals from outside the organisation, whether a single external team member, an entirely external PSI review team, or an external investigation body, can help broaden perspectives, support accountability, impartiality and professionalism (108–110), and is common practice in other industries such as aviation (108, 109). However, it is important to critically reflect on the concept of “independence”. Safety science and human factors literature emphasise that all reviewers contribute different frameworks and assumptions, and no analysis is truly neutral (62). Rather than positioning external experts as impartial arbiters, our findings suggest the value of collaborative learning, where diverse forms of expertise, including lived experience and systems thinking, are brought together in ways that support mutual understanding and more holistic system-level insight.
Organisational barriers to engaging external contributors, however, exist. Some healthcare organisations may be reluctant to involve outsiders in review processes due to concerns about reputational risk, legal exposure, or loss of control over the narrative (111, 112). Acknowledging and addressing these tensions is crucial to fostering more open and participatory systems of learning, and lessons can be drawn from high-risk industries, such as aviation (113–115), where multidisciplinary collaboration supports both accountability and learning (110, 116). Health systems could benefit from adopting similarly transparent and restorative approaches. Integrating such approaches into PSI reviews in health can help shift the focus beyond local issues to broader structural and regulatory factors, while fostering rational, restorative and participatory forms of inquiry.
The need to enhance collaborative learning
Collaborative learning is a critical component of effective incident response and harm prevention. This study revealed significant concerns about the limited and inconsistent dissemination of learning from PSI reviews. Rather than viewing learning as a unidirectional transfer of information, a collaborative learning approach recognises that meaningful change arises from shared reflections and dialogue across all levels of the system. This includes those directly or indirectly impacted by the incident or subsequent changes, such as local teams impacted by the implemented change or the original incident, as well as the wider organisation, and intra- and inter-state organisations (62). Poor dissemination of review findings, recommendations and implementation outcomes can result in replicated effort, missed opportunities for system-wide improvement and disengagement among staff (117). When learning is not visible, relational or participatory, it undermines the creditability of PSI review processes and trust in their capacity to drive improvement.
Collaborative learning can impact the visibility of action, and in turn the culture of reporting and general morale around the effectiveness of PSI review processes achieving change (108, 117). Sharing of review findings could also be used as a resource for future review teams to support the development of high quality recommendations and their implementation (117), but this is not currently done effectively. Further research involving the development, testing, and implementation of effective PSI review sharing processes is therefore recommended.
Embedded systems to disseminate and share findings [such as the National Patient Safety Alerts (118) in the UK, and the Safety Alert Broadcast system in NSW (57)], may support teams to enhance review outputs (117) as would the development of a repository of completed and ongoing incident reviews, contributing factors, recommendations and evidence-based implementation strategies (54). Feedback on the quality of the review and outputs from internal and external expert organisations also impacts the opportunities for review members to learn from incidents, may impact willingness to report PSIs (117, 119), and is an identified area for improvement. There is a clear need for a sector wide incident reporting and learning system that uses consistent review methods and processes, to allow analysis at the hospital, health service, state, and national level and to support benchmarking at each level (120).
This study also found that the sharing of review findings with patients and families remains limited, which can undermine trust and perceptions of transparency in the healthcare organisation (65, 66, 121). Collaborative learning emphasises that patients and families are not merely recipients of information, but essential partners in the learning process following harm. Meaningful engagement requires more than disclosing outcomes. It involves creating space for dialogue and recognising the knowledge of those affected (including investigators, clinicians and CRs) to support mutual understanding of what happened and why (66). These principles align with the idea of a learning health system, in which learning is continuous, transparent and grounded in partnerships with healthcare providers, patients and families (122). The Australian Open Disclosure framework (59) supports this principle and strongly recommends that PSI review reports should be shared with patients and families, in an accessible format and language, as well as written and face-to-face communication that includes acknowledgement of patient and family concerns, acknowledgement of and apology for the harm caused, identification of the contributing factors, and a clear explanation of the actions taken to prevent recurrence and monitor implemented changes (59). Strengthening this collaborative approach can contribute to healing, foster shared accountability and support system-wide learning.
The challenges in developing effective and feasible recommendations
Recommendations are intended to improve processes and thus outcomes for healthcare consumers and staff (54). Poor quality or weak recommendations, however, remain a persistent issue (102), often with variable clarity of language used, impacting how recommendations are interpreted and how feasible and acceptable they are (54). Large numbers of weak recommendations being made increases the pressure across the healthcare system through the prioritisation and implementation of those improvements, leading to either poor or no-implementation or change (54). Failure to implement changes to prevent future harm can impact staff confidence in the PSI review and management process (108), as well as consumer confidence in the healthcare organisation or system (54).
Developing strong recommendations requires consideration of implementation science, systems thinking and humans factors (60), to ensure that system leverage points are targeted and that improvements use an evidence-based systems-thinking approach to reduce the likelihood of patient harm, and support staff and patients (123). Identification of contributing factors and recommendation development can be guided by established systems-based frameworks such as PreventiMaps (The Prevention Map) (124, 125). This approach considers systems-based contributing factors to support the development and implementation of effective recommendations (126). A critical feature of the PreventiMap approach is that it supports the development of a network of integrated recommendations that span all levels of the system in question, ensuring that the behaviour change desired at the sharp-end is facilitated through systemic change (126). Within this process, data sources used to guide the analysis of PSIs should incorporate observation of practice to ensure work-as-normal, and work-as-done is captured and considered within the analysis (127). This process also requires a skilled review panel to effectively consider and incorporate human factors and systems based thinking into the PSI review process (58).
Recommendation strength is typically assessed against the hierarchy of effectiveness (128), with policies, guidelines and education considered the least effective strategies, standardisation and checklists moderately effective, and system-based change considered the most effective tools to achieve change (129). For these to be effective, however, they need to be coupled with evidence-based implementation strategies (130). On their own, changes to policy or guidelines are considered weak recommendations, partly as unwarranted clinical variation in care is a persistent issue, and guideline adherence is a complex challenge, impacted by a multitude of factors (131–133). To increase the likelihood of effective implementation, recommendations should be high impact, and low effort, avoiding reliance on people's action by standardising or simplifying processes, introducing forcing functions or software changes, or architectural redesign (16). Frameworks such as PreventiMaps can support the development of recommendations that link changes across multiple levels, for example incorporating changes to policy along with education, and procedural changes, underpinned by evaluation and reporting to support adherence to the changes.
The importance of effective implementation design and evaluation
Variable monitoring and evaluation of recommendation implementation was also highlighted in this analysis. The survey findings in particular identified that the vast majority of participants disagreed that recommendations were reliably implemented or lead to real improvements in patient safety. One recent review identified less than 7% of recommendations (from 4,579) as being system-focused, effective or strong (55). This relates to the methodologies used to investigate incidents (55), such as RCA, which have limited capacity to identify systemic contributory factors and produce strong recommendations (40, 45, 128), also supported by findings from this study.
Internationally, the implementation of weak recommendations (38, 54, 56) has limited impact on rates of PSIs and the risk of harm (38, 56). Improving the implementation of strong system-based recommendations, along with enhanced monitoring and evaluation of recommendation implementation is fundamental to achieve changes in care processes and patient outcomes. This fundamental finding is underpinned by complex barriers to effective implementation, requiring a multifaceted approach to improve implementation practices (38, 56). Enhanced incorporation of implementation science and quality improvement principles, including using small scale iterative tests like Plan-do-study-act cycles (134), may support planning for effective implementation and evaluation strategies, taking into account known barriers and facilitators within supportive implementation frameworks, thus increasing the likelihood of effective change being achieved (50–52).
Governance and accountability for the implementation of recommendations
This study also identified limited systematic governance and accountability processes to ensure the implementation of recommendations is both accountable to a specific role and monitored in the short and long term. While monitoring in turn informs iterative changes to the implementation process to achieve effective change to patient risk and outcomes, this feedback loop is often weak or absent. These gaps reflect broader concerns in both national and international contexts. Limited governance structures are an international concern, limiting the processing of reported incidents, the review process, the implementation of recommendations and evaluation of impact of the PSI reviews (108). Although frameworks such as the Australian National Model Clinical Governance Framework explicitly hold health service executives and boards accountable not only for service delivery and financial performance but also for clinical governance (135, 136), this accountability is often not meaningfully enacted in practice. The tendency to prioritise operational and budgetary concerns can lead to a disconnect between the formal responsibilities of leadership and the day-to-day realities of implementing and learning from PSI reviews (137).
Resourcing and proportionality of PSI reviews
This study identified concern around the majority of patient safety resources being dedicated to in-depth reviews of serious harm PSIs, to the detriment of reviewing lower harm incidents or near misses or conducting preventative QI activities. In safety science it is widely acknowledged that minor incidents provide the learning opportunities to prevent major incidents (138, 139). The response to PSIs should therefore be proportionate and consider the opportunity to learn from PSIs and prevent future risk (80). This study highlights the potential to reassess the criteria for conducting extensive in-depth reviews, and consideration of conducting fewer but more effective in-depth reviews, particularly of reoccurring incidents, that achieve improvements to practice and patient risk (80). More concise or thematic reviews and quality improvement should be undertaken as an alternative option to in-depth reviews, within a system of finite resources. This aligns with recent policy shifts such as the NHS PSIRF (18) and the updated London Protocol (58), which both advocate for a more flexible, proportionate and systems-oriented approach to incident response and learning. Patient safety reviews, particularly in-depth reviews, are often seen as the key strategy to minimise harm but are in fact one of many tactics that can be employed by a health system. Other tactics include identifying, monitoring and managing clinical risk and ensuring a culture of learning and improvement (140).
Policy implications
Despite decades of research and efforts to improve the response to PSIs, findings from this study indicate limited impact and improvement. This is highlighted by the attitudinal survey findings that identified only half of the participant cohort agreed that recommendations were accepted, appropriately targeted, consider what went well as well as what went wrong, and are achievable, that learning from PSIs prevents recurrence, and that investigators have access to the rights tools, support, skills and knowledge to conduct quality reviews and achieve change.
Findings from this study, in conjunction with other arms of this project (20, 70, 71) will inform the development of Best Practice Principles for learning and improving from PSIs, and a codesign process to develop and test system-wide improvements to PSI review processes and implementation. The Best Practice Principles and co-design process will be deliberately wide in scope as the incident review process is complex and has many influences across the health system and beyond. The Best Practice Principles will draw upon relevant frameworks and systems thinking from safety science, policy frameworks, implementation science, organisational culture and learning health systems to ensure the approach is both evidence-informed and context-sensitive. Isolated changes in one part of the process, for example, changing the composition and expertise of the investigation team, is unlikely to have an impact on the overall effectiveness of the incident review process to reduce patient harm. A system-wide end-to-end re-thinking and re-engineering of the process is likely to be required.
Re-engineering patient safety practices to incorporate these Principles will require system and behaviour change supported by and reflected in policy change to implement a blame-free systems thinking-based approach to PSIs with an emphasis on systemic change and improvement. Proposed improvements are outlined in Table 3. The feasibility and acceptability of such changes will be trialled in the next codesign and feasibility phases of the project.
Strengths and limitations
This study includes a large analysis of Australian and international patient safety experts and healthcare professionals’ perspectives regarding PSI reviews. Rigour was enhanced through the use of triangulation of perspectives from participants across a variety of backgrounds, and settings, as well as survey findings, and the utilisation of multiple coders during the data analysis. A key strength was the inclusion of perspectives from health services that account for 78% of Australia's public hospital admissions, but the perspectives of HCPs from other public health and private services were not represented in the data, limiting to some degree, how generalisable the findings are across Australia. This study primarily reflects the perspectives of participants working in quality and safety roles, senior clinicians and safety professionals, many of whom are embedded within the healthcare hierarchies and institutional models of expertise. As such, the findings may not fully capture the experiences or frontline clinical staff or those who have been the subject of investigations and consumers, whose insights are critical to understanding the broader impact and effectiveness of PSI review processes. Future research should seek to include these voices to support more inclusive system learning. The research utilised a concurrent MMR approach. Had the research been conducted using a sequential MMR design, the survey findings may have informed the interview questions allowing for more nuanced investigation of participant perceptions and experiences.
Conclusion
PSI reviews are failing to support effective prevention of patient safety incidents. This study has provided insights into current practices and perceptions of the PSI review process. Key findings will inform codesigned improvements to better support review teams to learn from incidents and prevent future patient harm: PSI review panels should systematically incorporate input from external experts as well as CRs; continuous efforts to reinforce a just restorative and blame-free culture is fundamental to support incident reporting, and development and implementation of effective systems-focused recommendations; effective recommendation development requires consideration of systems thinking and humans factors; monitoring and evaluation of recommendation implementation is a fundamental mechanism to enhance accountability and achieve change; and finally, broad and transparent sharing of review findings will support the development of higher quality review and recommendations These strategies should not be implemented in isolation. The complexity of healthcare systems demands a coordinated, whole-of-system re-engineering of investigation processes, shifting from compliance-based reviews towards strategic, relational, restorative and sustainable approaches that support continuous improvement.
Data availability statement
The datasets presented in this article are not readily available because the data supporting the conclusions made in this paper may be available on request from the corresponding author subject to ethics and confidentiality requirements. Requests to access the datasets should be directed to Peter HibbertcGV0ZXIuaGliYmVydEBtcS5lZHUuYXU=.
Ethics statement
The studies involving humans were approved by Northern Sydney Human Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MB: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. YY: Data curation, Formal analysis, Investigation, Writing – review & editing. CM: Data curation, Investigation, Project administration, Writing – review & editing. LB: Investigation, Writing – review & editing. PS: Conceptualization, Funding acquisition, Writing – review & editing. SM: Conceptualization, Funding acquisition, Writing – review & editing. JB: Conceptualization, Funding acquisition, Writing – review & editing. PH: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This includes funding from the following partners: NSW Clinical Excellence Commission, Clinical Excellence QLD, Safer Care Victoria and ACT Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2025.1645575/full#supplementary-material
References
1. World Health Organization. Patient Safety Incident Reporting and Learning Systems: Technical Report and Guidance. Geneva. Switzerland: WHO (2020).
2. Hibbert PD, Molloy CJ, Hooper TD, Wiles LK, Runciman WB, Lachman P, et al. The application of the global trigger tool: a systematic review. Int J Qual Health Care. (2016) 28(6):640–9. doi: 10.1093/intqhc/mzw115
3. Runciman W, Hibbert P, Thomson R, Van Der Schaaf T, Sherman H, Lewalle P. Towards an international classification for patient safety: key concepts and terms. Int J Qual Health Care. (2009) 21(1):18–26. doi: 10.1093/intqhc/mzn057
4. Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. (2010) 363(22):2124–34. doi: 10.1056/NEJMsa1004404
5. Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. Br Med J. (2019) 366:l4185. doi: 10.1136/bmj.l4185
6. Bates DW, Levine DM, Salmasian H, Syrowatka A, Shahian DM, Lipsitz S, et al. The safety of inpatient health care. N Engl J Med. (2023) 388(2):142–53. doi: 10.1056/NEJMsa2206117
7. National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, Board on Global Health, Committee on Improving the Quality of Health Care Globally. Crossing the Global Quality Chasm: Improving Health Care Worldwide. Washington, DC: National Academies Press (US) (2018).
8. World Health Organization. Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care. Geneva: World Health Organization (2021).
9. Bos J VD, Rustagi K, Gray T, Halford M, Ziemkiewicz E, Shreve J. The $17.1 billion problem: the annual cost of measurable medical errors. Health Aff (Millwood). (2011) 30(4):596–603. doi: 10.1377/hlthaff.2011.0084
10. Slawomirski L, Klazinga N. The Economics of Patient Safety: From Analysis to Action. Paris, France: Organisation for Economic Cooperation and Development (OECD) (2022).
11. Australian Commission on Safety Quality in Health Care. The State of Patient Safety and Quality in Australian Hospitals 2019. Canberra (AUST): ACSQHC (2019).
12. Australian Institute of Health and Welfare. Australia’s Health 2018. Australia’s Health Series no 16. Canberra: ACT: AIHW (2018).
13. Howell A-M, Burns EM, Hull L, Mayer E, Sevdalis N, Darzi A. International recommendations for national patient safety incident reporting systems: an expert delphi consensus-building process. BMJ Qual Saf. (2017) 26(2):150–63. doi: 10.1136/bmjqs-2015-004456
14. Holmes A, Bugeja L, Ranson D, Griffths D, Ibrahim JE. The potential for inadvertent adverse consequences of open disclosure in Australia: when good intentions cause further harm. Med Sci Law. (2019) 59(4):265–74. doi: 10.1177/0025802419872049
15. Safer Care Victoria. Adverse patient safety event guideline. Safer Care Victoria. Melbourne, Australia: Victorian Government (2023).
16. Clinical Excellence Queensland. Best Practice Guide to Clinical Incident Management. Brisbane, Australia: The State of Queensland (2023).
17. Clinical Excellence Commission. Incident Management: Policy Directive, PD2020_047. Sydney, Australia: Clinical Excellence Commission, NSW Government (2020).
18. National Health Service England. Patient Safety Incident Response Framework Supporting Guidance: Guide to Responding Proportionately to Patient Safety Incidents. London, England: NHS England (2022).
19. Institute for Healthcare Improvement, National Steering Committee for Patient Safety. Safer Together: A National Action Plan to Advance Patient Safety. Boston, Massachusetts: Institute for Healthcare Improvement (2020).
20. Bowditch L, Molloy C, King B, Abedi M, Jackson S, Bierbaum M, et al. Do patient safety incident investigations align with systems thinking? An analysis of contributing factors and recommendations. BMJ Qual Saf. (2025). doi: 10.1136/bmjqs-2025-019063
21. Canham A, Jun GT, Waterson P, Khalid S. Integrating systemic accident analysis into patient safety incident investigation practices. Appl Ergon. (2018) 72:1–9. doi: 10.1016/j.apergo.2018.04.012
22. Wiegmann DA, Wood LJ, Solomon DB, Shappell SA. Implementing a human factors approach to RCA2: tools, processes and strategies. J Healthc Risk Manag. (2021) 41(1):31–46. doi: 10.1002/jhrm.21454
23. Salmon PM, Cornelissen M, Trotter MJ. Systems-based accident analysis methods: a comparison of accimap, HFACS, and STAMP. Saf Sci. (2012) 50(4):1158–70. doi: 10.1016/j.ssci.2011.11.009
24. Wheway JL, Jun GT. Adopting systems models for multiple incident analysis: utility and usability. Int J Qual Health Care. (2021) 33(4):mzab135. doi: 10.1093/intqhc/mzab135
25. Taylor-Adams S, Vincent C. Systems analysis of clinical incidents: the London protocol. Clin Risk. (2004) 10(6):211–20. doi: 10.1258/1356262042368255
26. Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys. (2008) 71(1):S187–S90. doi: 10.1016/j.ijrobp.2007.07.2385
27. Higham H, Vincent C. Human error and patient safety. In: Donaldson L, Ricciardi W, Sheridan S, Tartaglia R, editors. Textbook of Patient Safety and Clinical Risk Management. Switzerland: Springer (2020). p. 29–44.
28. Holden RJ, Carayon P. SEIPS 101 And seven simple SEIPS tools. BMJ Qual Saf. (2021) 30(11):901–10. doi: 10.1136/bmjqs-2020-012538
29. Zhang Y, Dong C, Guo W, Dai J, Zhao Z. Systems theoretic accident model and process (STAMP): a literature review. Saf Sci. (2022) 152:105596. doi: 10.1016/j.ssci.2021.105596
30. Hollnagel E. FRAM: The Functional Resonance Analysis Method: Modelling complex Socio-technical systems. London: CRC Press (2017).
31. Patriarca R, Di Gravio G, Woltjer R, Costantino F, Praetorius G, Ferreira P, et al. Framing the FRAM: a literature review on the functional resonance analysis method. Saf Sci. (2020) 129:104827. doi: 10.1016/j.ssci.2020.104827
32. Kingston J, Jager J, Koornneef F, Frei R, Schallier P. ECFA+ Events and Conditional Factors Analysis Manual. Delft: Noordwijk Risk Initiative Foundation (2004).
33. Diller T, Helmrich G, Dunning S, Cox S, Buchanan A, Shappell S. The human factors analysis classification system (HFACS) applied to health care. Am J Med Qual. (2014) 29(3):181–90. doi: 10.1177/1062860613491623
34. Salmon P, Jenkins D, Stanton N, Walker G. Hierarchical task analysis vs. Cognitive work analysis: comparison of theory, methodology and contribution to system design. Theor Issues Ergon Sci. (2010) 11(6):504–31. doi: 10.1080/14639220903165169
35. Donaldson MS, Corrigan JM, Kohn LT. To err is Human: Building a Safer Health System. Washington, D.C.: Institute of Medicine, Committee on Quality of Health Care in America (2000).
36. Donaldson L. An organisation with a memory. Clin Med. (2002) 2(5):452–7. doi: 10.7861/clinmedicine.2-5-452
37. Stavropoulou C, Doherty C, Tosey P. How effective are incident-reporting systems for improving patient safety? A systematic literature review. Milbank Q. (2015) 93(4):826–66. doi: 10.1111/1468-0009.12166
38. Martin-Delgado J, Martínez-García A, Aranaz-Andres JM, Valencia-Martín JL, Mira JJ. How much of root cause analysis translates to improve patient safety. A systematic review. Med Princ Pract. (2020) 29(6):524–31. doi: 10.1159/000508677
39. Macrae C. The problem with incident reporting. BMJ Qual Saf. (2016) 25(2):71–5. doi: 10.1136/bmjqs-2015-004732
40. Peerally MF, Carr S, Waring J, Dixon-Woods M. The problem with root cause analysis. BMJ Qual Saf. (2017) 26(5):417–22. doi: 10.1136/bmjqs-2016-005511
41. Nauman J, Soteriades ES, Hashim MJ, Govender R, Al Darmaki RS, Al Falasi RJ, et al. Global incidence and mortality trends due to adverse effects of medical treatment, 1990–2017: a systematic analysis from the global burden of diseases, injuries and risk factors study. Cureus. (2020) 12(3):e7265. doi: 10.7759/cureus.7265
42. De Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. BMJ Qual Saf. (2008) 17(3):216–23. doi: 10.1136/qshc.2007.023622
43. Sousa-Pinto B, Marques B, Lopes F, Freitas A. Frequency and impact of adverse events in inpatients: a nationwide analysis of episodes between 2000 and 2015. J Med Syst. (2018) 42:1–9. doi: 10.1007/s10916-018-0898-5
44. Connolly W, Rafter N, Conroy RM, Stuart C, Hickey A, Williams DJ. The Irish national adverse event study-2 (INAES-2): longitudinal trends in adverse event rates in the Irish healthcare system. BMJ Qual Saf. (2021) 30(7):547–58. doi: 10.1136/bmjqs-2020-011122
45. Kellogg KM, Hettinger Z, Shah M, Wears RL, Sellers CR, Squires M, et al. Our current approach to root cause analysis: is it contributing to our failure to improve patient safety? BMJ Qual Saf. (2017) 26(5):381–7. doi: 10.1136/bmjqs-2016-005991
46. Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. (2018) 16(1):63. doi: 10.1186/s12916-018-1057-z
47. Archer S, Hull L, Soukup T, Mayer E, Athanasiou T, Sevdalis N, et al. Development of a theoretical framework of factors affecting patient safety incident reporting: a theoretical review of the literature. BMJ Open. (2017) 7(12):e017155. doi: 10.1136/bmjopen-2017-017155
48. Sujan M. An organisation without a memory: a qualitative study of hospital staff perceptions on reporting and organisational learning for patient safety. Reliability Engineering & System Safety. (2015) 144:45–52. doi: 10.1016/j.ress.2015.07.011
49. Anderson JE, Kodate N. Learning from patient safety incidents in incident review meetings: organisational factors and indicators of analytic process effectiveness. Saf Sci. (2015) 80:105–14. doi: 10.1016/j.ssci.2015.07.012
50. Rapport F, Smith J, Hutchinson K, Clay-Williams R, Churruca K, Bierbaum M, et al. Too much theory and not enough practice? The challenge of implementation science application in healthcare practice. J Eval Clin Pract. (2022) 28(6):991–1002. doi: 10.1111/jep.13600
51. Bierbaum M, Hillier S, Ellis LA, Clay-Williams R, Goodrich A, Padbury R, et al. Continuous quality improvement across a South Australian health service and the role it plays in a learning health system: a qualitative study. BMC Health Serv Res. (2025) 25(1):457. doi: 10.1186/s12913-025-12557-4
52. Bierbaum M, Best S, Williams S, Fehlberg Z, Hillier S, Ellis LA, et al. The integration of quality improvement and implementation science methods and frameworks in healthcare: a systematic review. BMC Health Serv Res. (2025) 25(1):558. doi: 10.1186/s12913-025-12730-9
53. Hibbert PD, Stewart S, Wiles LK, Braithwaite J, Runciman WB, Thomas MJ. Improving patient safety governance and systems through learning from successes and failures: qualitative surveys and interviews with international experts. Int J Qual Health Care. (2023) 35(4):0. doi: 10.1093/intqhc/mzad088
54. Health Services Safety Investigations Body. Recommendations but no action: improving the effectiveness of quality and safety recommendations in healthcare. Dorset, UK. (2024).
55. Lea W, Lawton R, Vincent C, O’Hara J. Exploring the “black box” of recommendation generation in local health care incident investigations: a scoping review. J Patient Saf. (2023) 19(8):553–63. doi: 10.1097/PTS.0000000000001164
56. Connolly W, Li B, Conroy R, Hickey A, Williams DJ, Rafter N. National and institutional trends in adverse events over time: a systematic review and meta-analysis of longitudinal retrospective patient record review studies. J Patient Saf. (2021) 17(2):141–8. doi: 10.1097/PTS.0000000000000804
57. Clinical Excellence Commission. System-level Patient Safety Risks: Response co-ordination and Communication. Sydney, Australia: NSW Health (2024).
58. Vincent C, Irving D, Bellandi T, Higham H, Michel P, Staines A, et al. Systems analysis of clinical incidents: development of a new edition of the London protocol. BMJ Qual Saf. (2025) 34:413–20. doi: 10.1136/bmjqs-2024-017987
59. Australian Commission on Safety and Quality in Health Care. Australian Open Disclosure Framework. Sydney: ACSQHC (2013).
60. Salmon PM, King B, Hulme A, Chari S, McCormack L, Tresillian M, et al. Toward the translation of systems thinking methods in patient safety practice: assessing the validity of net-harms and accimap. Saf Sci. (2023) 159:106003. doi: 10.1016/j.ssci.2022.106003
61. Wailling J, Cameron G, Stolarek I, Turner S, Bleakley B, O’Connor N, et al. Restorative initiatives: emerging insights from design, implementation and collaboration in five countries. Frontiers in Health Services. (2025) 5:1472738. doi: 10.3389/frhs.2025.1472738
62. Wailling J, Kooijman A, Hughes J, O'Hara JK. Humanizing harm: using a restorative approach to heal and learn from adverse events. Health Expect. (2022) 25(4):1192–9. doi: 10.1111/hex.13478
63. O’Hara JK, Ramsey L, Partridge R, Redford C, McHugh S, Louch G, et al. The learn together programme (part A): co-designing an approach to support patient and family involvement and engagement in patient safety incident investigations. Front Health Serv. (2025) 5:1529035. doi: 10.3389/frhs.2025.1529035
64. Salmon PM, Hulme A, Walker GH, Waterson P, Berber E, Stanton NA. The big picture on accident causation: a review, synthesis and meta-analysis of AcciMap studies. Saf Sci. (2020) 126:104650. doi: 10.1016/j.ssci.2020.104650
65. Ramsey L, Sheard L, Waring J, McHugh S, Simms-Ellis R, Louch G, et al. Humanizing processes after harm part 1: patient safety incident investigations, litigation and the experiences of those affected. Frontiers in Health Services. (2025) 4:1473256. doi: 10.3389/frhs.2024.1473256
66. Ramsey L, Hughes J, Hazeldine D, Seddon S, Gould M, Wailling J, et al. Humanising processes after harm part 2: compounded harm experienced by patients and their families after safety incidents. Frontiers in Health Services. (2024) 4:1473296. doi: 10.3389/frhs.2024.1473296
67. Iedema R, Sorensen R, Manias E, Tuckett A, Piper D, Mallock N, et al. Patients’ and family members’ experiences of open disclosure following adverse events. Int J Qual Health Care. (2008) 20(6):421–32. doi: 10.1093/intqhc/mzn043
68. O’Hara J, Ramsey L, McHugh S, Langley J, Waring J, Simms-Ellis R, et al. Co-designing and testing the learn together guidance to support patient and family involvement in patient safety investigations: a mixed-methods study. Health and Social Care Delivery Research. (2025) 13(18):1–125. doi: 10.3310/KJHT3375
69. Lawless L. (2024). Available online at: https://www.medicalindependent.ie/comment/medico-legal/compounded-harm-why-we-should-take-it-seriously/ (Accessed May 08, 2025).
70. Hibbert P, Yu Y, Molloy C, Ames M, Brown D, Berrill J, et al. Perceptions and experiences of consumer representatives on patient safety investigation teams: a qualitative analysis. Health Expect. (2025) 28:e70281. doi: 10.1111/hex.70281
71. Hibbert PD, Raggett L, Molloy CJ, Westbrook J, Magrabi F, Mumford V, et al. Improving health system responses when patients are harmed: a protocol for a multistage mixed-methods study. BMJ Open. (2024) 14(7):e085854. doi: 10.1136/bmjopen-2024-085854
72. Teddlie C, Tashakkori A. A general typology of research designs featuring mixed methods. Res Sch. (2006) 13(1):12–28.
73. Curry L, Nunez-Smith M. Mixed Methods in Health Sciences Research: A Practical Primer. Thousand Oaks, CA: Sage publications (2014).
74. Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage publications (2017).
75. O'Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy. (2008) 13(2):92–8. doi: 10.1258/jhsrp.2007.007074
76. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19(6):349–57. doi: 10.1093/intqhc/mzm042
77. Etikan I, Musa SA, Alkassim RS. Comparison of convenience sampling and purposive sampling. American Journal of Theoretical and Applied Statistics. (2016) 5(1):1–4. doi: 10.11648/j.ajtas.20160501.11
78. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4(1):50. doi: 10.1186/1748-5908-4-50
79. Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. (2022) 17(1):75. doi: 10.1186/s13012-022-01245-0
80. Vincent C, Carthey J, Macrae C, Amalberti R. Safety analysis over time: seven major changes to adverse event investigation. Implement Sci. (2017) 12(1):151. doi: 10.1186/s13012-017-0695-4
81. Turner K, Stapelberg NJ, Sveticic J, Dekker SW. Inconvenient truths in suicide prevention: why a restorative just culture should be implemented alongside a zero suicide framework. Aust N Z J Psychiatry. (2020) 54(6):571–81. doi: 10.1177/0004867420918659
82. Kaur M, De Boer RJ, Oates A, Rafferty J, Dekker S. Restorative just culture: a study of the practical and economic effects of implementing restorative justice in an NHS trust. International Cross-industry Safety Conference (2019). p. 01007
83. Li J, Boulanger B, Norton J, Yates A, Swartz CH, Smith A, et al. “SWARMing” to improve patient care: a novel approach to root cause analysis. Jt Comm J Qual Patient Saf. (2015) 41(11):494–501. doi: 10.1016/S1553-7250(15)41065-7
84. Motuel L, Dodds S, Jones S, Reid J, Dix A. Swarm: a quick and efficient response to patient safety incidents. Nurs Times. (2017) 12(9):36–8.
85. Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. (2013) 56(11):1669–86. doi: 10.1080/00140139.2013.838643
86. University Hospitals Bristol and Weston NHS Foundation Trust. Standard Operating Procedure: Patient Safety Incident Investigation (PSII) Rapid Incident Review Meetings (RIRM). Bristol, UK: University Hospitals Bristol and Weston NHS Foundation Trust (2021).
87. Hibbert P, Thomas MJW, Deakin A, Runciman W, Braithwaite J. Final Report: Sentinel Event Research Project. A Report Submitted to the Victorian Department of Health and Human Services. Melbourne, VIC, Australia: Australian Patient Safety Foundation (2016).
88. Hibbert P, Schultz T. A Review of SA Health and Wellbeing’s Safety Learning System. Adelaide, SA: SA Health and Wellbeing (2020).
89. The Behavioural Insights Team. Behavioural Insights into Patient Motivation to Make a Claim for Clinical Negligence. London, UK: NHS Resolution (2018).
90. QSR International Pty Ltd. NVivo (version 14). Victoria: Qualitative Solutions and Research Pty Ltd (2023).
91. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3(2):77–101. doi: 10.1191/1478088706qp063oa
92. Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? Br Med J. (2001) 322(7294):1115–7. doi: 10.1136/bmj.322.7294.1115
93. Keith RE, Crosson JC, O’Malley AS, Cromp D, Taylor EF. Using the consolidated framework for implementation research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. (2017) 12:1–12. doi: 10.1186/s13012-017-0550-7
94. Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the consolidated framework for implementation research. Implement Sci. (2015) 11:1–13. doi: 10.1186/s13012-016-0437-z
95. Vanhaecht K, Seys D, Russotto S, Strametz R, Mira J, Sigurgeirsdóttir S, et al. An evidence and consensus-based definition of second victim: a strategic topic in healthcare quality, patient safety, person-centeredness and human resource management. Int J Environ Res Public Health. (2022) 19(24):16869. doi: 10.3390/ijerph192416869
96. Kable A, Kelly B, Adams J. Effects of adverse events in health care on acute care nurses in an Australian context: a qualitative study. Nurs Health Sci. (2018) 20(2):238–46. doi: 10.1111/nhs.12409
97. Moreland JJ, Ewoldsen DR, Albert NM, Kosicki GM, Clayton MF. Predicting nurses’ turnover: the aversive effects of decreased identity, poor interpersonal communication, and learned helplessness. J Health Commun. (2015) 20(10):1155–65. doi: 10.1080/10810730.2015.1018589
98. Ahern S, Hopper I, Loh E. Qualified privilege legislation to support clinician quality assurance: balancing professional and public interests. Med J Aust. (2019) 210(8):343–6.e1. doi: 10.5694/mja2.50124
99. Read GJ, Shorrock S, Walker GH, Salmon PM. State of science: evolving perspectives on ‘human error’. Ergonomics. (2021) 64(9):1091–114. doi: 10.1080/00140139.2021.1953615
100. Churruca K, Ellis LA, Pomare C, Hogden A, Bierbaum M, Long JC, et al. Dimensions of safety culture: a systematic review of quantitative, qualitative and mixed methods for assessing safety culture in hospitals. BMJ Open. (2021) 11(7):e043982. doi: 10.1136/bmjopen-2020-043982
101. Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. (2010) 6(4):226–32. doi: 10.1097/PTS.0b013e3181fd1a00
102. Turner K, Sveticic J, Grice D, Welch M, King C, Panther J, et al. Restorative just culture significantly improves stakeholder inclusion, second victim experiences and quality of recommendations in incident responses. J Hosp Adm. (2022) 11:8–17. doi: 10.5430/jha.v11n2p8
103. Sujan MA, Huang H, Braithwaite J. Learning from incidents in health care: critique from a safety-II perspective. Saf Sci. (2017) 99:115–21. doi: 10.1016/j.ssci.2016.08.005
104. Hollnagel E. Safety-II in Practice: Developing the Resilience Potentials. London: Routledge (2017).
105. Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. Int J Qual Health Care. (2015) 27(5):418–20. doi: 10.1093/intqhc/mzv063
106. Toffolutti V, Stuckler D. A culture of openness is associated with lower mortality rates among 137 English national health service acute trusts. Health Aff. (2019) 38(5):844–50. doi: 10.1377/hlthaff.2018.05303
107. Kok J, Leistikow I, Bal R. Patient and family engagement in incident investigations: exploring hospital manager and incident investigators’ experiences and challenges. J Health Serv Res Policy. (2018) 23(4):252–61. doi: 10.1177/1355819618788586
108. Mitchell I, Schuster A, Smith K, Pronovost P, Wu A. Patient safety incident reporting: a qualitative study of thoughts and perceptions of experts 15 years after ‘to err is human’. BMJ Qual Saf. (2016) 25(2):92–9. doi: 10.1136/bmjqs-2015-004405
109. Macrae C, Vincent C. Learning from failure: the need for independent safety investigation in healthcare. J R Soc Med. (2014) 107(11):439–43. doi: 10.1177/0141076814555939
110. de Kam D, Grit K, Bal R. Shared learning from incidents: a qualitative study into the perceived value of an external chair on incident investigation committees. Saf Sci. (2019) 120:57–66. doi: 10.1016/j.ssci.2019.06.031
111. Øyri SF, Wiig S, Tjomsland O. Influence of external assessment on quality and safety in surgery: a qualitative study of surgeons’ perspectives. BMJ Open Quality. (2024) 13(2):e002672. doi: 10.1136/bmjoq-2023-002672
112. Ocloo J, Garfield S, Franklin BD, Dawson S. Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health Research Policy and Systems. (2021) 19(1):8. doi: 10.1186/s12961-020-00644-3
113. Kim E, Rhee M. Learning from alliance membership: an empirical study of learning from the failure of their alliance members, liability and environmentally sustainable airline. Sustainability. (2021) 13(21):11794. doi: 10.3390/su132111794
114. Bennett S. Aviation Safety and Security: The Importance of Teamwork, Leadership, Creative Thinking and Active Learning. Faringdon: Libri Publishing Limited (2015).
115. Guo Y, Schwaninger A, Gall H. An architecture for an adaptive and collaborative learning management system in aviation security. 2008 IEEE 17th Workshop on Enabling Technologies: Infrastructure for Collaborative Enterprises (2008). IEEE.
116. Baxter D, Colledge T, Turner N. A study of accountability in two organizational learning frameworks: why accountability for learning is critical. European Management Review. (2017) 14(3):319–32. doi: 10.1111/emre.12112
117. Benn J, Koutantji M, Wallace L, Spurgeon P, Rejman M, Healey A, et al. Feedback from incident reporting: information and action to improve patient safety. BMJ Qual Saf. (2009) 18(1):11–21. doi: 10.1136/qshc.2007.024166
118. National Health Service. Safety Alerts Management and Implementation Policy V4.0. Cornwall, UK: NHS Trust (2024).
119. Uibu E, Põlluste K, Lember M, Kangasniemi M. Reporting and responding to patient safety incidents based on data from hospitals’ reporting systems: a systematic review. J Hosp Adm. (2020) 9(2):22–32. doi: 10.5430/jha.v9n2p22
120. McLean S, Coventon L, Finch CF, Dallat C, Carden T, Salmon PM. Evaluation of a systems ergonomics-based incident reporting system. Appl Ergon. (2022) 100:103651. doi: 10.1016/j.apergo.2021.103651
121. Wiig S, Hibbert PD, Braithwaite J. The patient died: what about involvement in the investigation process? Int J Qual Health Care. (2020) 32(5):342–6. doi: 10.1093/intqhc/mzaa034
122. Braithwaite J, Dammery G, Spanos S, Smith CL, Ellis LA, Churruca K, et al. Learning health systems 2.0: future-proofing healthcare against pandemics and climate change. A White Paper. Australian Institute of Health Innovation, Macquarie University Sydney. (2023).
123. World Health Organization. Human Factors: Technical Series on Safer Primary Care. Geneva: World Health Organization (2016).
124. Goode N, Read GJ, Van Mulken MR, Clacy A, Salmon PM. Designing system reforms: using a systems approach to translate incident analyses into prevention strategies. Front Psychol. (2016) 7:1974. doi: 10.3389/fpsyg.2016.01974
125. Salmon PM, Stanton NA, Walker GH, Hulme A, Goode N, Thompson J, et al. Handbook of Systems Thinking Methods. Florida: CRC Press (2022).
126. Salmon PM, Coventon L, Read GJ. A systems analysis of work-related violence in hospitals: stakeholders, contributory factors, and leverage points. Saf Sci. (2022) 156:105899. doi: 10.1016/j.ssci.2022.105899
127. Clay-Williams R, Hounsgaard J, Hollnagel E. Where the rubber meets the road: using FRAM to align work-as-imagined with work-as-done when implementing clinical guidelines. Implement Sci. (2015) 10:1–8. doi: 10.1186/s13012-015-0317-y
128. Hibbert PD, Thomas MJ, Deakin A, Runciman WB, Braithwaite J, Lomax S, et al. Are root cause analyses recommendations effective and sustainable? An observational study. Int J Qual Health Care. (2018) 30(2):124–31. doi: 10.1093/intqhc/mzx181
129. Health Quality and Safety Commission New Zealand. Recognising human factors and strategies for preventing errors New Zealand. (2015).
130. Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. Int J Qual Health Care. (2014) 26(3):321–9. doi: 10.1093/intqhc/mzu047
131. Bierbaum M, Rapport F, Arnolda G, Tran Y, Nic Giolla Easpaig B, Ludlow K, et al. Rates of adherence to cancer treatment guidelines in Australia and the factors associated with adherence: a systematic review. Asia Pac J Clin Oncol. (2023) 19(6):618–44. doi: 10.1111/ajco.13948
132. Bierbaum M, Rapport F, Arnolda G, Nic Giolla Easpaig B, Lamprell K, Hutchinson K, et al. Clinicians’ attitudes and perceived barriers and facilitators to cancer treatment clinical practice guideline adherence: a systematic review of qualitative and quantitative literature. Implement Sci. (2020) 15:1–24. doi: 10.1186/s13012-020-00991-3
133. Bierbaum M, Rapport F, Arnolda G, Delaney GP, Liauw W, Olver I, et al. Clinical practice guideline adherence in oncology: a qualitative study of insights from clinicians in Australia. PLoS One. (2022) 17(12):e0279116. doi: 10.1371/journal.pone.0279116
134. Leis JA, Shojania KG. A primer on PDSA: executing plan–do–study–act cycles in practice, not just in name. BMJ Qual Saf. (2017) 26(7):572–7. doi: 10.1136/bmjqs-2016-006245
135. Australian Commission on Safety and Quality in Health Care. National Model Clinical Governance Framework. (2021).
137. Murray M, Cope V. Leadership: patient safety depends on it!. Collegian. (2021) 28(6):604–9. doi: 10.1016/j.colegn.2021.07.004
139. McLean S, Finch CF, Goode N, Clacy A, Coventon LJ, Salmon PM. Applying a systems thinking lens to injury causation in the outdoors: evidence collected during 3 years of the understanding and preventing led outdoor accidents data system. Inj Prev. (2021) 27(1):48–54. doi: 10.1136/injuryprev-2019-043424
140. National Health Service U. Patient Safety Incident Response Framework, PRN01274. In: National Health Service U, editor. London, UK2024.
141. Cohen TN, Francis SE, Wiegmann DA, Shappell SA, Gewertz BL. Using HFACS-healthcare to identify systemic vulnerabilities during surgery. Am J Med Qual. (2018) 33(6):614–22. doi: 10.1177/1062860618764316
142. Clinical Excellence Commission. Serious adverse event review: root cause analysis toolkit. (2020).
143. Wolf L, Gorman K, Clark J, Gleason J, Henrickson Parker S. Implementing root cause analysis and action: integrating human factors to create strong interventions and reduce risk of patient harm. J Patient Saf. (2022) 18(8):e1160–e6. doi: 10.1097/PTS.0000000000001042
144. National Patient Safety Foundation. RCA2: Improving Root Cause Analyses and Actions to Prevent Harm. (2015).
147. Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. BMJ Qual Saf. (2006) 15(suppl 1):i50–i8. doi: 10.1136/qshc.2005.015842
148. Carayon P, Wooldridge A, Hoonakker P, Hundt AS, Kelly MM. SEIPS 3.0: human-centered design of the patient journey for patient safety. Appl Ergon. (2020) 84:103033. doi: 10.1016/j.apergo.2019.103033
149. Leveson NG. Engineering a Safer World: Systems Thinking Applied to Safety. Cambridge, MA: The MIT Press (2016).
150. Paterson E, Chari S, McCormack L, Sanderson P. Application of a human factors systems approach to healthcare control centres for managing patient flow: a scoping review. J Med Syst. (2024) 48(1):62. doi: 10.1007/s10916-024-02071-1
151. Salmon P, Read G. Reimagining Rasmussen’s risk management framework: a contemporary view on risk. Contemporary Ergonomics and Human Factors 2025: Proceedings of the Chartered Institute of Ergonomics and Human Factors Annual Conference; 2025: Chartered Institute of Ergonomics and Human Factors.
152. Branford K, Hopkins A, Naikar N. Guidelines for AcciMap Analysis. Learning from High Reliability Organisations. Sydney, NSW: CCH Australia Ltd (2009).
153. Davis S, Riley W, Gurses AP, Miller K, Hansen H. Failure modes and effects analysis based on in situ simulations: a methodology to improve understanding of risks and failures. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools). Rockville, MD: Agency for Healthcare Research and Quality (US) (2008).
154. NHS Borders. SAER information for patients and relatives. (2025). Available online at: https://rightdecisions.scot.nhs.uk/patient-information-leaflets/governance/saer-information-for-patients-and-relatives/ (Accessed May 08, 2025).
155. National Health Service England. Serious Incident Framework: Supporting learning to prevent recurrence. (2013).
157. Jones-Lee M, Aven T. ALARP—what does it really mean? Reliability Engineering & System Safety. (2011) 96(8):877–82. doi: 10.1016/j.ress.2011.02.006
158. McQueen JM, Gibson KR, Manson M, Francis M. Adverse event reviews in healthcare: what matters to patients and their family? A qualitative study exploring the perspective of patients and family. BMJ Open. (2022) 12(5):e060158. doi: 10.1136/bmjopen-2021-060158
159. Machen S. Thematic reviews of patient safety incidents as a tool for systems thinking: a quality improvement report. BMJ Open Qual. (2023) 12(2):e002020. doi: 10.1136/bmjoq-2022-002020
160. Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. (2015) 3:1–12. doi: 10.1186/s40359-015-0089-9
161. Rowland P, Lan MF, Wan C, Pozzobon L. Why is learning from patient safety incidents (still) so hard? A sociocultural perspective on learning from incidents in healthcare organizations. J Health Organ Manag. (2025). doi: 10.1108/JHOM-08-2024-0334
162. Runciman W, Williamson J, Deakin A, Benveniste K, Bannon K, Hibbert P. An integrated framework for safety, quality and risk management: an information and incident management system based on a universal patient safety classification. BMJ Qual Saf. (2006) 15(suppl 1):i82–90. doi: 10.1136/qshc.2005.017467
163. Bowie P. Exploring the science and philosophy of investigation: Presentation. United Kingdom: Health Services Safety Investigation Body; Date unknown.
164. McNab D, McKay J, Shorrock S, Luty S, Bowie P. Development and application of ’systems thinking’principles for quality improvement. BMJ Open Quality. (2020) 9(1):e000714. doi: 10.1136/bmjoq-2019-000714
Keywords: patient safety, hospital incident reporting, risk management, hospitals, medical errors, incident review, human factors, adverse events
Citation: Bierbaum M, Yu Y, Molloy CJ, Bowditch L, Salmon PM, Middleton S, Braithwaite J and Hibbert P (2025) Decades of failure to prevent harm to patients—where are we going wrong? A mixed methods study of the perspectives of health services staff across Australia and internationally. Front. Health Serv. 5:1645575. doi: 10.3389/frhs.2025.1645575
Received: 12 June 2025; Accepted: 13 August 2025;
Published: 2 September 2025.
Edited by:
Charles Vincent, University of Oxford, United KingdomReviewed by:
Jo Wailling, The National Collaborative for Restorative Initiatives in Health, New ZealandSipho Mkhize, University of KwaZulu-Natal, South Africa
Copyright: © 2025 Bierbaum, Yu, Molloy, Bowditch, Salmon, Middleton, Braithwaite and Hibbert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter Hibbert, cGV0ZXIuaGliYmVydEBtcS5lZHUuYXU=
 Mia Bierbaum
Mia Bierbaum Yinghua Yu1
Yinghua Yu1 Paul M. Salmon
Paul M. Salmon Sandy Middleton
Sandy Middleton Jeffrey Braithwaite
Jeffrey Braithwaite Peter Hibbert
Peter Hibbert