- 1Emeritus Professor of Medical Statistics, University of Milano-Bicocca, Milan, Italy
- 2National Centre for Healthcare Research and Pharmacoepidemiology, University of Milano-Bicocca, Milan, Italy
- 3Welfare Councilor Office, Lombardy Region, Milan, Italy
- 4Unit of Biostatistics, Epidemiology and Public Health, Department of Statistics and Quantitative Methods, University of Milano-Bicocca, Milan, Italy
- 5Unit of Mental Health, Addictions, and Prison Health, Territorial Care Department, Emilia-Romagna Region, Bologna, Emilia-Romagna, Italy
- 6Department of Mental Health and Addiction Services, AUSL Reggio Emilia, Reggio Emilia, Italy
- 7National PhD Programme in One Health Approaches to Infectious Diseases and Life Science Research, Department of Public Health, Experimental and Forensic Medicine, University of Pavia, Pavia, Italy
- 8Territorial Network Organizational Unit; Structure of Mental Health, Addiction Services, Disabilities and Penitentiary Health; Regional Directorate for Health and Welfare, Lombardy Region, Milan, Lombardy, Italy
- 9Department of Mental Health and Addiction Services, ASST Lecco, Lecco, Italy
Introduction: The care provided to patients with severe mental disorders remains a major challenge for the organization of healthcare systems. Data on recent treatment patterns within mental health services are essential to estimate the unmet needs for care and to guide service planning and resource allocation.
Aim: To identify individual patient and organizational-level predictors of the provision of minimally adequate care for patients with severe mental illness.
Methods: A population-based study was designed, retrieving data from Healthcare Utilization databases of Lombardy region (Italy). 72,115 patients from Departments of Mental Health (DMHs) in care for schizophrenic, bipolar or major depressive disorder, were identified. Minimally Adequate Treatment (MAT) was calculated as either minimum psychiatric visits (≥4) with pharmacological treatment (≥2 months) or psychotherapy sessions (≥8, for major depressive disorder only). Patients meeting these criteria were considered as having received MAT; others were classified as having received less than adequate treatment. Multilevel analyses were performed to estimate the association between patients' individual (e.g., age, sex, education, marital status) and DMHs' aggregate (i.e., organizational features, activity volume, staff employed in facilities providing MHC) characteristics and provision of MAT.
Results: Overall, 45% of patients received MAT. Patients with increased probability of receiving MAT included married individuals (8%, 95% CI: 4%–12%), those with schizophrenia (11%, 95% CI: 9%–13%) or bipolar disorder (23%, 20%–25%), younger patients (22%, 20%–25%), and those with previous continuity of care (48%, 46%–51%). Differences in DMHs' structural features (e.g., number of day-treatment facilities, presence of multidisciplinary teams) contributed to heterogeneous MAT coverage. Moreover, the composition of psychiatric teams (in terms of hours worked by each category of healthcare professionals) and the number of affiliated facilities were associated with MAT delivery.
Conclusions: This study ascertained that the quality of care offered to psychiatric patients is still low and not adequate. Administrative data can usefully contribute to identify both individual and organizational-level predictors of MAT provision, offering a valuable benchmark for managing organizational features of DMHs and for optimally allocating the working hours in multidisciplinary professional teams, with the goal of maximizing the provision of adequate mental healthcare.
Introduction
The World Health Organization includes the provision of mental healthcare in community-based settings as a key objective of Mental Health Care (MHC) systems (1). As a country, Italy offers a unique opportunity to explore community-oriented MHC. Indeed, since the approval of the psychiatric reform law in 1978 (2), a process of deinstitutionalization had led to a profound shift from hospital-based to community-oriented MHC (3). However, community-based MHC requires a continuous effort from healthcare professionals, patients and their families. While adherence to therapies is often suboptimal among people with mental disorders (4–6), inadequate outpatient follow-up further challenges the effectiveness of community-based care. Previous research has identified multiple barriers, including lack of service integration and poor continuity of care, which are associated with worse clinical outcomes, including relapses and re-hospitalizations (7). Indeed, emergency room (ER) visits may indicate suboptimal outpatient management and serve as a marker of inadequate continuity of care, predicting subsequent psychiatric hospitalizations (8, 9). Experience suggests that community-oriented MHC facilities often do not provide adequate care for patients with severe mental illness, resulting in worse prognosis, shorter life expectancy and poor quality of life (10–13). For example, it has been reported that in Italy less than a half of patients affected by severe mental disorders, including schizophrenic, affective and depressive disorders, received adequate care (5, 14–16), and this translates into higher rates of hospitalization and relapses (17). These challenges highlight the importance of developing robust tools to evaluate mental health care.
To assess the quality of MHC, it is essential to define a set of indicators that allow to compare different mental health systems and levels of care within the same system (e.g., primary care vs. specialized services). Among such indicators, the concept of the Minimally Adequate Treatment (MAT) has become relevant (16, 18, 19), and is particularly suitable for the purposes of such comparisons. MAT is typically defined as receiving a sufficient number of psychotherapy sessions or an adequate duration of pharmacological treatment, and it refers to the minimum level of care required to achieve meaningful clinical outcomes (18). A growing body of international evidence suggests that access to MAT is associated with improved clinical outcomes, including reductions in symptom severity, broader impacts on health service utilization and mortality (20). Therefore, ensuring MAT provision to patients with mental disorders is key in evaluating the appropriateness, equity, efficiency, and sustainability of MHC provided by mental health systems.
This paper, moving in the field of retrospective real-world investigation, aims to identify predictors at both the individual patient and organizational levels that influence the provision of the so-called minimally adequate treatment (16, 21–23) for patients with severe mental illness receiving care from the Departments of Mental Health (DMHs) accredited by the Health Service of Lombardy Region. We used multilevel analyses to assess the effect of individual and organizational (POU-level) predictors simultaneously (24). In such analyses, organizational predictors included volume of activity, structural features and staff employed in the facilities providing MHC. From this point of view, the current paper represents an exploratory investigation aimed at supporting policymakers in allocating mental health resources and managing services to optimize the delivery of mental healthcare.
Methods
Setting
In Lombardy, an italian region with nearly 10 million inhabitants (around 16% of the whole national population) (25) MHC is currently provided through Departments of Mental Health (DMHs), each of them being structured into Psychiatric Operative Units (POUs). In accordance with the principles established by the Italian psychiatric reform of 1978 (Law 180/1978) (26), which reshaped MHC in Italy, each POU (defined to cover areas with roughly similar populations while accounting for differences in territorial morphology and urbanization) represents a widespread and integrated network of community mental health facilities, including community mental health centres (CMHCs), general hospital psychiatric wards (GHPWs), day-treatment and community residential facilities (27, 28). Each of the 52 POUs currently active in Lombardy at the study time was staffed by a multidisciplinary team that included psychiatrists, psychologists, nurses, social workers, and auxiliary personnel.
Data source
In Italy, all citizens have equal access to healthcare provided by the National Health Service (NHS). An automated system of healthcare utilization (HCU) databases is used to manage health services in each region. These databases were originally established to record all payments made to healthcare providers for reimbursement purposes, and therefore gathers, on an ongoing basis, administrative and disease-related data for all patients assisted by the Regional Health Services (6). Therefore, HCU data contain a wide range of information on all individuals resident in Lombardy and beneficiaries of the NHS, such as diagnosis at discharge from public or private hospitals, outpatient drug prescriptions, specialist visits and diagnostic exams provided fully, or in part, free-of-charge by the NHS. In addition, a specific national information system dedicated to mental health care is implemented through regional DMH facilities accredited by the NHS. This system gathers detailed information on healthcare services and social interventions provided to patients with mental disorders and their families (5, 29). This information system, called “Mental Health Information System” (MHIS) includes socio-demographic information, diagnostic and therapeutic codes for patients receiving specialist MHC by regional DMH facilities (5). Data on interventions and activities delivered by DMHs in outpatient, home-care, or day-treatment facilities are also recorded within the MHIS.
These various types of data in the HCU databases can be interconnected since a unique individual identification code is used by all databases for each NHS beneficiary, enabling the study of the complete care pathway for each patient. To preserve privacy, each identification code is automatically anonymized, the inverse process being only allowed to the Regional Authority upon request of judicial Authorities. Diagnostic and therapeutic codes, as well as outpatients specialist visits ones, used in the current study for drawing records and fields from Healthcare Utilization databases are reported in the Supplementary Table S1; whereas, the full list of interventions provided by community Mental Health services, as recorded in the MHIS, is reported in Supplementary Table S2. Further details on HCU databases in the field of MHC have been reported elsewhere (12, 14, 29, 30).
In addition to individual-level data obtained through record-linkage procedures across HCU databases, aggregate data on the POUs currently operating in Lombardy were provided by the Regional Directorate for Welfare, with support from their technical IT staff.
Study population
The target population consisted in all the NHS beneficiaries residents in Lombardy who on 1st January 2015 were aged 18 years or older (about 8.27 million inhabitants in 2015, http://demo.istat.it, last access 22nd May 2025). Of these, individuals who received at least one contact with DMH services (i.e., an hospital admission in a GHPW or a healthcare service at any facility affiliated with DMHs) during the year 2015 were identified, with the date of the first contact with DMH being referred to as the index date. Among those patients, those who received a diagnosis of schizophrenic, bipolar or major depressive disorder were identified and included into the study population. Diagnoses of severe mental disorders were considered as mutually exclusive. For patients with more than one diagnosis, the classification to the most updated one (i.e., the diagnosis recorded in the MHIS at the latest date) was performed by technical staff.
Based on mental healthcare received during the four-year wash-out period prior to the index date (2011–2014), patient histories were examined and patients were classified into three mutually exclusive groups reflecting continuity of care: (i) new patients, who had no previous contact with mental health facilities; (ii) former patients, who had at least one contact with mental health facilities between 2011 and 2013, but none in 2014; and (iii) continuous patients, who received continuous care (one contact per month) throughout the entire period from 2011–2014. Only patients with a minimum of four years of available historical data prior to the index date were included, to avoid selection bias and ensure reliable classification.
Patients included in the study cohort were observed for one year, accumulating person time of follow-up from the index date to the earliest of the following events: death, emigration from the Region or administrative censorship (set at 365 days after the index date; for patients with an index date on 31 December 2015, follow-up could have ended on 31 December 2016).
Individual and aggregate predictors
Baseline characteristics measured for each patient in the study population (hereafter referred to as “individual-level” data) included sex, age, years of education, employment status and marital status. In addition, physical comorbidities that could act as potential confounders in receiving mental healthcare (e.g., diabetes, hypertension, etc) were assessed both individually and through the Multisource Comorbidity Score (MCS). The MCS is a recently developed comorbidity index that captures patients' clinical status based on inpatient diagnostic information and outpatient drug prescriptions, which has been validated for outcome prediction in several Italian regions (31, 32).
Several characteristics reflecting the organizational features of facilities providing MHC (hereafter referred to as “aggregate” predictors) were assessed for each POU active during the study period, with a brief description of the most relevant structural features of DMHs provided in Supplementary Table S3. Among these predictors, one of the main organizational features of interest was the proportion of hours worked by each professional category related to the total number of hours worked by all professional categories within the POU. For each POU, this proportion was computed as the ratio between the hours worked by each professional category and the total number of hours worked by all healthcare professionals within the same unit. This variable was conceived as an indicator of workforce composition, reflecting the relative weight of each professional category within the multidisciplinary team, as information on the total workforce volume was not available for the analysis. Healthcare professionals were grouped into five categories: (i) medical staff (psychiatrists), (ii) nurses, (iii) psychologists, (iv) social staff (including social workers, educators, and rehabilitation therapists), and (v) auxiliary and administrative staff. Additional aggregate-level predictors of interest included: (i) the number of facilities affiliated with each POU and (ii) the total number of patients under care within the POU.
Minimally adequate treatment
The so-called Minimally Adequate Treatment (MAT), an indicator developed according to the main recommendations of the American Psychiatric Association (16, 18, 19), was calculated over the one-year observation period for each patient belonging to the study population, and was defined as the outcome of interest.
MAT consists of either a combination of minimum psychiatric and pharmacological treatment, or a minimum number of psychotherapy sessions. For each diagnostic groups considered, a patient was considered as having received MAT if he/she had at least four or more psychiatric visits and was covered for a minimum of two months by appropriate pharmacological therapy (i.e., antidepressants for patients diagnosed with major depressive disorder, antipsychotics for those with schizophrenic disorder, and either antipsychotics, mood stabilizers or both for those with bipolar disorder) (18). Additionally, patients diagnosed with major depressive disorder who attended at least eight psychotherapy sessions were also considered as having received a MAT, even in the absence of psychiatric visits or drug prescriptions (19). Patients not meeting any of these criteria were classified as not having received MAT.
Drug coverage was calculated according with the Defined Daily Dose (DDD) metric. The number of days covered by a given pharmacological class during the 365-day observation period (i.e., the total number of days covered by dispensed drugs belonging to that class) was considered for assessing adherence to drug therapy (33). Hospitalization days and periods spent in residential facilities were considered as days covered by therapy, thereby taking into account the so-called “immeasurable time bias” (34).
Data analyses
Differences in individual-level characteristics according to MAT provision were investigated. Given the large sample size and the potential for type I error, the standardized mean difference (SMD) was used to identify meaningful differences between patients who did and did not receive MAT. Indeed, SMD is an alternative to the p-value and not influenced by sample size (35). Based on previous literature, a threshold of 10% or higher was considered indicative of a relevant difference (35, 36). A multivariable log-binomial model was fitted to estimate the relative risk (RR), and corresponding 95% confidence interval (CI), of MAT provision (outcome) associated with individual-level characters (exposures).
Since one of the main aim was to identify organizational features of POUs associated with MAT provision, and given the clear hierarchical structure of the data, with patients (individual-level) nested within the POUs (aggregate-level), a multilevel log-binomial regression model was fitted. The association between aggregate-level predictors and MAT was assessed by adjusting for individual-level predictors, with POUs included as a random intercept to account for clustering. Between-POUs heterogeneity in the proportion of patients receiving MAT, adjusted for individual-level predictors, was first assessed. As aggregate-level predictors were expressed as continuous variables (see Methods, Individual and Aggregate Predictors section for details), and a non-linear association with outcome was expected, restricted cubic splines with four knots (37, 38) were employed, with the reference value set at the first knot.
All the analyses were performed with the SAS software version 9.4 (SAS Institute, Cary, NC, USA) and the Excel Software (from the Microsoft Office Personal Productivity Software Suite, Version 2019 16.0.6742.2048).
Results
Patients
Overall, 72,115 patients were identified, of whom 32,773 (45.4%) received MAT during the one-year observation period. The mean age was 51.6 years (SD = 14.5), and the majority were women (55.6%), employed (54.5%), with no evidence of physical comorbidities (52.9%), and never married (42.7%). Most patients (79.7%) were classified as continuous patients (i.e., those who received ongoing mental healthcare between 2011 and 2014). Regarding primary psychiatric diagnosis, nearly half had a diagnosis of major depressive disorder (47.1%), while 39.4% had a schizophrenic spectrum disorder, and 13.5% had bipolar disorder.
Individual predictors of minimally adequate treatment
According to the bivariate analysis, younger patients, those who were never married, those with previous continuity of care, and those diagnosed with schizophrenic or bipolar disorder showed, on average, a higher likelihood of receiving MAT compared to their respective comparators (Table 1). No other individual characteristics generated meaningful between-patients differences in our setting. Consistently, according with multivariable log-binomial estimates (Table 2), significantly higher MAT provision was observed among patients with bipolar disorder (+23% than patients with major depressive disorders), patients younger than 29 years (+22% than patients aged 60 years or older), and those with previous continuity of care (+22% compared to newly taken-in-care patients). Other characteristics showed weaker associations with MAT provision compared to the main predictors. For example, male patients had a lower probability of receiving MAT compared to females (relative risk 0.98, 0.96–0.99), patients with disabilities had a slightly higher probability (RR 1.03, 1.00–1.05), while other characteristics showed minimal (RRs close to 1) or non-significant differences.
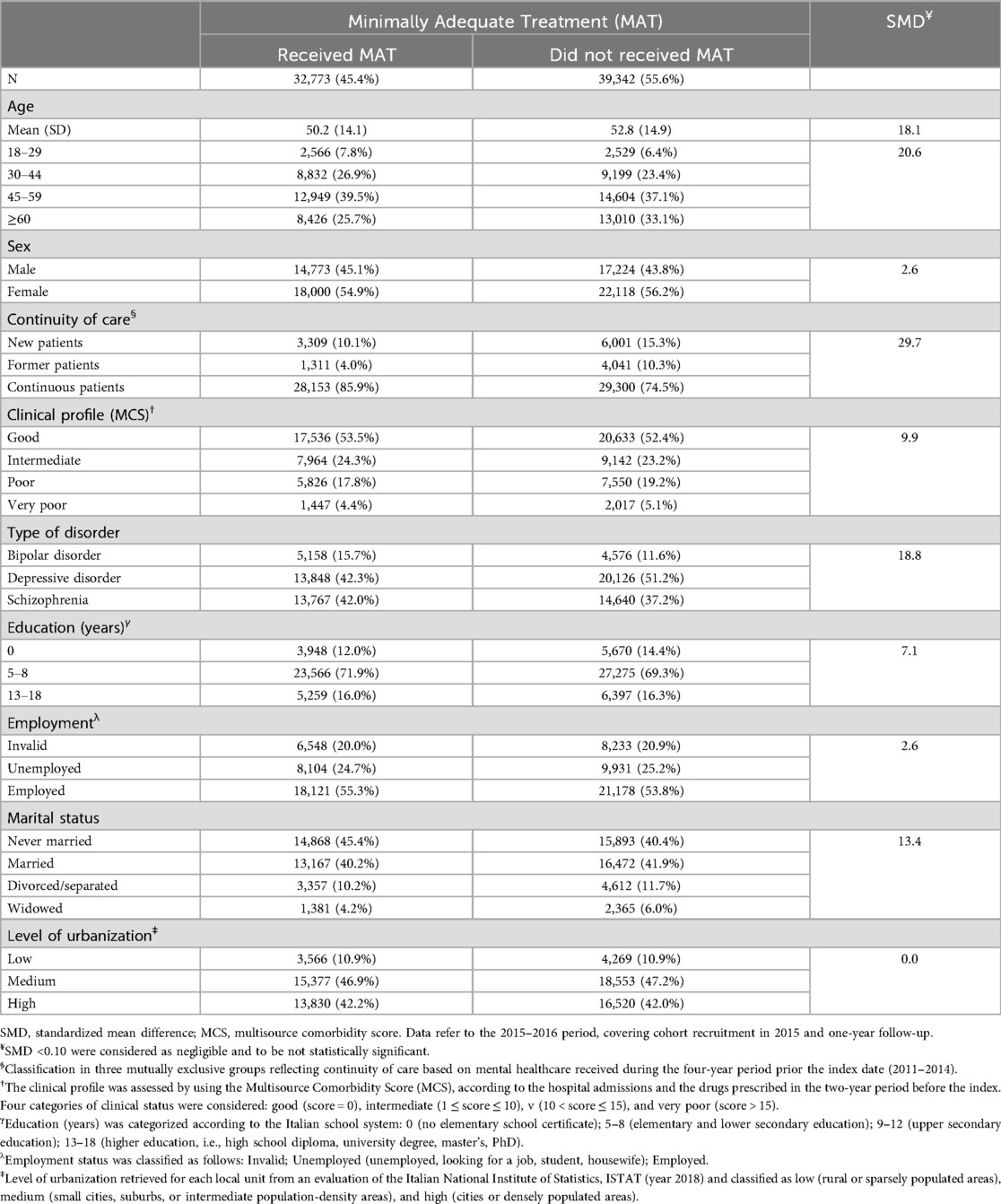
Table 1. Baseline characteristics of patients with severe mental disorder treated by DMHs of lombardy region, according to Minimally Adequate Treatment (MAT) status. Lombardy, Italy, 2015–2016.
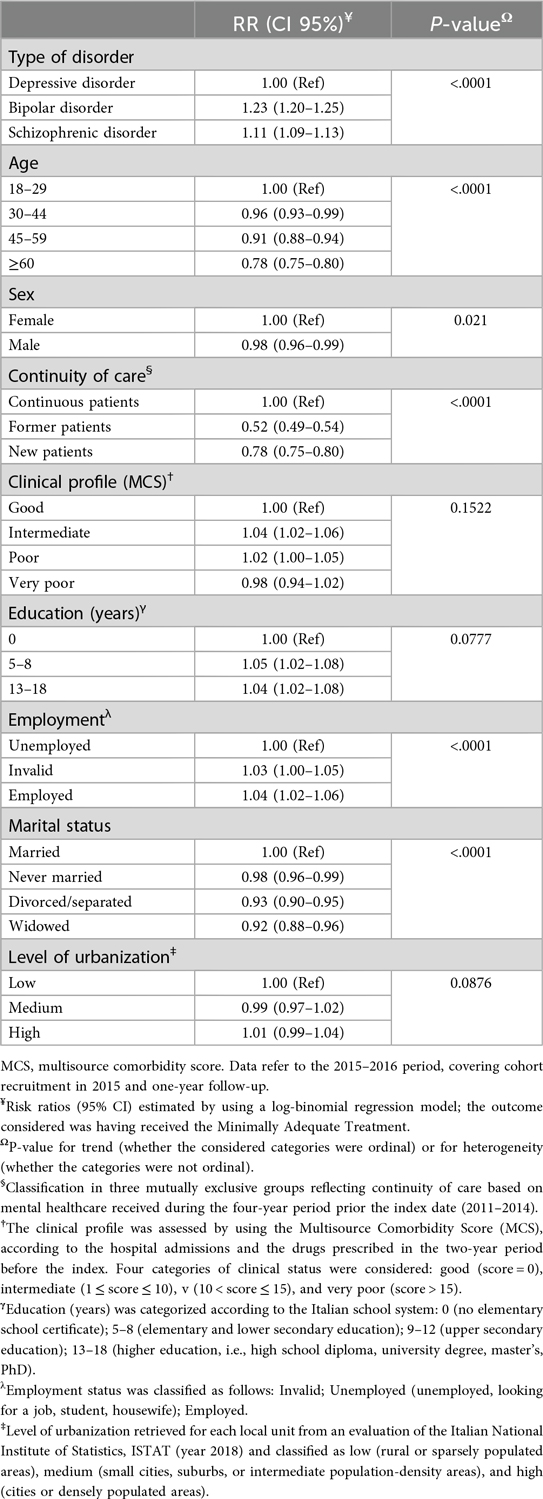
Table 2. Risk ratio (RR), and corresponding 95% confidence interval (95% CI), for the association between selected characteristics and Minimally Adequate Treatment (MAT) provision. Lombardy, Italy, 2015–2016.
Aggregate predictors of minimally adequate treatment
Descriptive statistics for key POU-level characteristics are provided in Supplementary Table S4. Between POUs differences were observed in structural features and activities. Medical staff, nurses, psychologists and social workers contributed, on average, 17%, 44%, 5%, and 16% respectively of the total employed hours, with ranges from 8%–28%, 3%–67%, 0%–11%, and 3%–60%, respectively. Additionally, the number of patients taken in case by the POUs ranged from 493–5,923, with a mean of 2,103, while the number of affiliated facilities per POU ranged from 1–25, averaging 10.
Estimates of the adjusted probability (and 95% CI) of receiving MAT according to the POI where patients were taken into care are shown in Supplementary Figure S1. Each horizontal bar represents a specific unit, highlighting a great variability among POUs, with values ranging from a 60% reduction (95% CI, 48%–68%) to a 20% increase (9%–30%) compared with the regional average. Notably, among the 52 considered POUs, 17 (32.7%) showed probability of providing MAT significantly different with respect to the regional average, with ten of them exhibiting a significantly lower probability of delivering MAT to their patients.
As shown in Figures 1, 2, a portion of the observed between-POU heterogeneity can be explained by the considered aggregate predictors which reflect POUs organizational and structural differences. Figure 1 illustrates the patterns of MAT provision according to the proportion of hours employed by each category of healthcare professionals. When the percentage of hours worked by each category was low, the relative proportion of patients receiving MAT remained below one (indicating, on average, the provision of inadequate treatment). Then, as the proportion of hours worked by healthcare professionals increased, this probability of MAT provision progressively increased before stabilizing. Considering the distinct categories of healthcare professionals, the highest relative proportions of patients receiving MAT were reached when: 16% of the total hours were provided by psychiatrists (with an increase of +8.5%; 95% CI: +6.3% to +10.9%), 34% of the total hours were provided by nurses (+10.4%; +6.4% to +14.2%), 4% by psychologists (+9.8%; +7.7% to +12.6%), and 29% by social workers (+14.8%; +12.1% to +17.8%). Figure 2, left panel, shows that higher numbers of patients treated at a POU (i.e., greater POU's activity volumes) were associated with larger increases in MAT provision, with the highest value (+9.5%; +6.1% to +12.8%) being reached by structures caring at least 5,900 patients. Finally, Figure 2, right panel, shows the relationship between the number of affiliated facilities per POU and treatment adequacy. POUs composed by less than 5 affiliated facilities provided inadequate treatment (i.e., relative proportions of MAT provision under the unit), while the relative proportions of patients receiving MAT progressively increased up to POUs with 13 affiliated facilities (gain of +7.2%; 95% CI +5.0% to +9.4%).
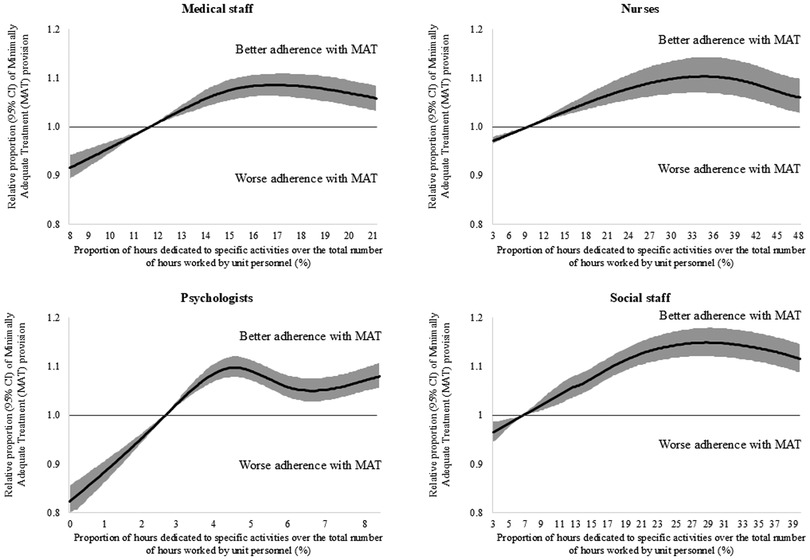
Figure 1. Restricted cubic splines to flexibly modelling the relationship between the proportion of hours worked by each professional category (on the total number of hours worked by all professional within the POU) and relative proportion of patients receiving minimally adequate treatment.
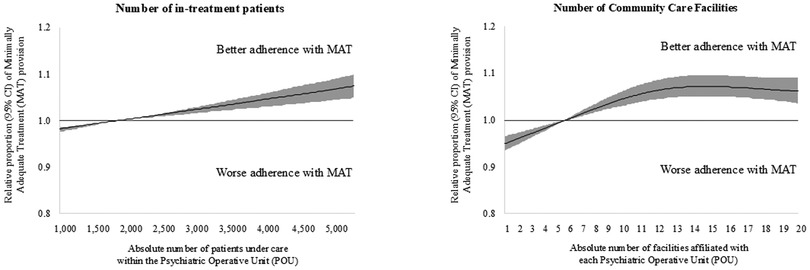
Figure 2. Restricted cubic splines to flexibly modelling the relationship between selected psychiatric operating units structural features (i.e., the number of patients in care, left panel, and of affiliated facilities, right panel) and relative proportion of patients receiving Minimally Adequate Treatment.
Discussion
The results of the present study offer evidence on the association between several individual-level characteristics of patients with severe mental disorders and the adequacy of mental healthcare provided. Consistently, we observed that new patients were more likely to meet the criteria for minimally adequate treatment (MAT), while patients with longer histories of care may often receive only medication monitoring. In particular, patients who were newly taken-in-care, those diagnosed with major depressive disorders, older patients, and those with a history of treatment interruption in the last few years had a lower probability of receiving minimally adequate treatment (MAT). As a novel and original message, our approach aimed to explore the role of organizational features of mental healthcare facilities. It showed that psychiatric units with low activity volumes and those with fewer territorial structures belonging to them, were less likely to provide minimally adequate treatment to patients they assist. Moreover, our findings may provide a preliminary reference for the distribution of working hours among multidisciplinary professionals to maximize the provision of adequate mental health care. Taken together, these results must be considered a valuable resource for policymakers for appropriately allocating resources to maximize benefits for patients.
Several additional findings of our study deserve to be mentioned. First, accordingly with previous investigations (16, 18, 28, 39), we confirmed that adequacy of community-oriented MHC is not largely achieved, with less than half of patients treated in public facilities in Lombardy receiving minimally adequate treatment. Second, individual-level factors influencing MHC adequacy were only partially consistent with literature: older age and major depressive disorders are well-known risk factors for receiving inadequate treatment and experiencing worse outcomes (16, 40). Conversely, unlike other studies (41–45) we did not find a significant association between social and educational characteristics and the adequacy of care provided. Finally, previous investigations found no clear impact of selected organizational features of Mental Health Departments of Lombardy (e.g., number of psychiatric beds and employed hours in community facilities) on the adequacy of care provided (16). However, it should be considered that in the current investigation was made a great effort to improve the accuracy of metrics measuring organizational features. For example, given that healthcare professionals may work across multiple facilities, we characterized each psychiatric unit based on the percentage of hours worked (an information not easy to retrieve), rather than simply the number of staff, offering a more precise metric.
Strengths and limitations
The study presented several strengths. HCU databases carry high-quality individual information on outpatient and inpatient services provided by the NHS (46). These data, linked to those collecting information for care provided by public DMHs (e.g., the MHIS), offer the opportunity to trace and evaluate the complete care pathway of patients with severe mental disorders. Thus, administrative databases are a useful tool to reflect routine clinical practice and to generate reliable real-world evidence on mental healthcare (14). Moreover, studies based on HCU data are not affected by selective participation or recall bias. Furthermore, since in Italy a free healthcare system is available to all citizens, using HCU data allow to perform studies on large, unselected cohorts. As a consequence of that, the present population-based study offers guarantees of representativeness and generalizability.
However, the use of administrative databases also presents several limitations. First, HCU data do not capture services provided in primary care settings, private facilities or those paid out-of-pocket (47–49). Moreover, using HCU databases the drug use is based on the assumption that the prescription (and its purchase) corresponds to the real consumption, and this may lead to a possible exposure misclassification. Despite this, HCU data were originally established to reimburse healthcare providers, and an incomplete or incorrect reporting leads to legal consequences, therefore assuring a high quality for the data source (50). Second, the lack of socio-economic and clinical data, such as the severity of the disease, physical complications and comorbidities, represents another important limitation. Indeed, the inability to account for socio-economic and physical characteristics (such as deprivation, BMI, blood pressure, etc.), and procedures not traced by the HCU data (e.g., private outpatients visits) represents an important boundary that doesn't allow to fully explore the complexity of mental disorders and their physical, mental and socio-economic implications. Furthermore, the absence of data on patients with drug addiction limited analyses for this vulnerable subgroup (51). Nevertheless, although patients with multiple mental disorder diagnoses could not be explicitly identified, the Multisource Comorbidity Score (MCS) was used to account for clinical complexity, integrating information from previous diagnoses and prescriptions over the two years prior to the index date. Additionally, the classification into continuity-of-care groups relied on a fixed four-year retrospective window, and only patients with at least four years of available historical data prior to the index date were included, to ensure reliable classification and minimizing selection bias.
Despite the robust study design and the use of advanced statistical methods, as an observational study, the possibility of residual confounding cannot be completely ruled out. Factors such as lifestyle behaviors (e.g., smoking, physical activity, alcohol consumption) or other contextual influences (e.g., work schedules, family responsibilities, or transportation barriers) may still affect treatment delivery). Fourth, while the concept of minimally adequate treatment has been developed in the setting of community surveys, its measurement using secondary administrative data poses challenges for several reasons: (i) individual care needs vary based on clinical, demographic, and social factors, many of which are not captured in HCU databases; (ii) the adequacy of care is assessed only through psychiatric/psychotherapist visits and pharmacological therapy, thus not considering the whole complexity of severe mental disorders and the need for continuous care they often require; (iii) psychosocial interventions are in this way excluded, even though their effectiveness have been largely demonstrated (19). Finally, our approach allowed for the assessment of the effect of the number of hours worked by each professional category only within the limits of the observed data. For example, a limited number of psychologists was employed in each POU of Lombardy, resulting in a low variability of hours compared to other professional categories; due to the absence of a comparator with a higher proportion of hours worked by psychologists, it is not possible to make inferences or logical extrapolations about the effect of a greater contribution beyond the observed range. In light of these considerations, further high-quality investigations are needed to confirm these findings.
Conclusions
Patients with severe mental illness are, and should remain, one of the primary focusses of the mental health community-based system. However, the low quality of care that many psychiatric patients still receive underscores the urgent need for action at both local and regional levels. To improve community care and ensure adequate support for those who need it most, a data-driven approach must be embraced. “Let us be driven by data for reducing uncertainty” should become the guiding principle for supporting policymakers to improve community mental health services.
Data availability statement
The datasets presented in this article are not readily available. Indeed, the data that support the findings of this study are available from the Region of Lombardy, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Lombardy Region. Requests to access the datasets should be directed toZ2lvdmFubmkuY29ycmFvQHVuaW1pYi5pdA==.
Ethics statement
All methods were carried out in accordance with the Declaration of Helsinki. The Ethical Committee of the University of Milano-Bicocca approved the study protocol (Protocol number 497, Year 2019) and established that the study (i) was exempt from patients informed consent (according to General Authorization for the Processing of Personal Data for Scientific Research Purposes Issued by the Italian Privacy Authority on August 10, 2018; https://www.garanteprivacy.it/web/guest/home/docweb/-/docweb-display/docweb/9124510); (ii) provides sufficient guarantees of individual records anonymity; and (iii) was designed according to quality standards of good practice of observational research based on secondary data. Informed consent was waived by the Ethical Committee of the University of Milano-Bicocca.
Author contributions
GC: Conceptualization, Supervision, Writing – review & editing, Writing – original draft, Methodology, Investigation, Visualization, Funding acquisition. MM: Data curation, Visualization, Conceptualization, Investigation, Methodology, Validation, Project administration, Supervision, Formal analysis, Resources, Writing – original draft, Writing – review & editing, Software. CC: Methodology, Conceptualization, Investigation, Writing – review & editing, Visualization, Software, Formal analysis, Writing – original draft, Data curation. PS: Writing – review & editing, Writing – original draft, Visualization, Investigation, Conceptualization, Supervision. AL: Writing – original draft, Writing – review & editing, Supervision, Resources, Investigation, Project administration, Conceptualization, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported and funded by grants from the Italian Ministry of the Education, University, and Research (“Fondo d'Ateneo per la Ricerca” portion, year 2018; grant number: 2018-ATE-0485) and from the Italian Ministry of Health (“Clinical pathways in patients with severe mental disorders in Italy”, QUADIM project, grant number: F52F16001420001). The funding sources had no role in the design of the study, the collection, analysis, and interpretation of the data or in the writing of the manuscript, or in the decision to approve publication of the finished manuscript.
Conflict of interest
GC received research support from the European Community (EC), the Italian Agency of Drug (AIFA), and the Italian Ministry for University and Research (MIUR). He took part to a variety of projects that were funded by pharmaceutical companies (i.e., Novartis, GSK, Roche, AMGEN and BMS). He also received honoraria as member of Advisory Board from Roche. No other potential conflicts of interest relevant to this article were disclosed.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2025.1655225/full#supplementary-material
Abbreviations
ATC, anatomical therapeutic chemical classification system; CI, confidence interval; CMHC, community mental health centers; DTF, day-treatment facilities; DMH, department of mental health; ER, emergency room; GHPW, general hospital psychiatric ward; HCU, healthcare utilization databases; ICD, international classification of diseases; RR, risk ratio; MAT, minimally adequate treatment; MHC, mental health care; MCS, multisource comorbidity score; MHIS, mental health information system; NHS, national health service; POU, psychiatric operative unit; SAS, statistical analysis system software.
References
1. WHO. Comprehensive Mental Health Action Plan 2013–2030. Geneva: World Health Organization (2021). p. 30. Available online at: https://apps.who.int/iris/handle/10665/345301 (Accessed August 11, 2022).
2. Ferrannini L, Ghio L, Gibertoni D, Lora A, Tibaldi G, Neri G, et al. Thirty-five years of community psychiatry in Italy. J Nerv Ment Dis. (2014) 202(6):432–9. doi: 10.1097/NMD.0000000000000141
3. Volpe U, Fiorillo A, Luciano M, Del Vecchio V, Palumbo C, Calò S, et al. Pathways to mental health care in Italy: results from a multicenter study. Int J Soc Psychiatry. (2014) 60(5):508–13. doi: 10.1177/0020764013501648
4. Corrao G, Monzio Compagnoni M, Conflitti C, Lora A. Is the long-term poor prognosis of acute myocardial infarction in patients with mental illness mediated through their poor adherence with recommended healthcare? Eur J Public Health. (2024) 34(3):584–91. doi: 10.1093/eurpub/ckae005
5. Monzio Compagnoni M, Caggiu G, Allevi L, Barbato A, Carle F, D’Avanzo B, et al. Assessment and monitoring of the quality of clinical pathways in patients with depressive disorders: results from a multiregional Italian investigation on mental health care quality (the QUADIM project). J Clin Med. (2023) 12(9):3297. doi: 10.3390/jcm12093297
6. Sanza M, Monzio Compagnoni M, Caggiu G, Allevi L, Barbato A, Campa J, et al. Assessing the quality of the care offer for people with personality disorders in Italy: the QUADIM project. A multicentre research based on the database of use of mental health services. Int J Ment Health Syst. (2023) 17(1):31. doi: 10.1186/s13033-023-00603-9
7. Sfetcu R, Musat S, Haaramo P, Ciutan M, Scintee G, Vladescu C, et al. Overview of post-discharge predictors for psychiatric re-hospitalisations: a systematic review of the literature. BMC Psychiatry. (2017) 17(1):227. doi: 10.1186/s12888-017-1386-z
8. Zhao Y, Hoenig JM, Protacio A, Lim S, Norman CC. Identification of risk factors for early psychiatric rehospitalization. Psychiatry Res. (2020) 285:112803. doi: 10.1016/j.psychres.2020.112803
9. Lebrat M, Megard R, Dananché C, Zimmer L, Plasse J, Franck N. Identification of factors associated with hospitalization in an outpatient population with mental health conditions: a case–control study. Front Psychiatry. (2024) 15:1341160. doi: 10.3389/fpsyt.2024.1341160
10. Bajraktarov S, Kalpak G, Jovanovic N. Community mental healthcare: new developments and innovative strategies. Curr Opin Psychiatry. (2020) 33(5):491–500. doi: 10.1097/YCO.0000000000000629
11. Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13(2):153–60. doi: 10.1002/wps.20128
12. Lora A, Monzio Compagnoni M, Allevi L, Barbato A, Carle F, D’avanzo B, et al. The quality of mental health care delivered to patients with schizophrenia and related disorders in the Italian mental health system. The QUADIM project: a multi-regional Italian investigation based on healthcare utilisation databases. Epidemiol Psychiatr Sci. (2022) 31:e15. doi: 10.1017/S2045796022000014
13. Starace F, Mungai F, Baccari F, Galeazzi GM. Excess mortality in people with mental illness: findings from a Northern Italy psychiatric case register. Soc Psychiatry Psychiatr Epidemiol. (2018) 53(3):249–57. doi: 10.1007/s00127-017-1468-8
14. Corrao G, Barbato A, D’Avanzo B, Di Fiandra T, Ferrara L, Gaddini A, et al. Does the mental health system provide effective coverage to people with schizophrenic disorder? A self-controlled case series study in Italy. Soc Psychiatry Psychiatr Epidemiol. (2022) 57(3):519–29. doi: 10.1007/s00127-021-02114-9
15. D’Avanzo B, Barbato A, Monzio Compagnoni M, Caggiu G, Allevi L, Carle F, et al. The quality of mental health care for people with bipolar disorders in the Italian mental health system: the QUADIM project. BMC Psychiatry. (2023) 23(1):424. doi: 10.1186/s12888-023-04921-7
16. Lora A, Conti V, Leoni O, Rivolta AL. Adequacy of treatment for patients with schizophrenia spectrum disorders and affective disorders in Lombardy, Italy. Psychiatr Serv Wash DC. (2011) 62(9):1079–84. doi: 10.1176/ps.62.9.pss6209_1079
17. Thornicroft G, Sunkel C, Alikhon Aliev A, Baker S, Brohan E, El Chammay R, et al. The lancet commission on ending stigma and discrimination in mental health. Lancet. (2022) 400(10361):1438–80. doi: 10.1016/S0140-6736(22)01470-2
18. Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. Am J Public Health. (2002) 92(1):92–8. doi: 10.2105/AJPH.92.1.92
19. Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Arch Gen Psychiatry. (2005) 62(6):629. doi: 10.1001/archpsyc.62.6.629
20. Vasiliadis HM, Lamoureux-Lamarche C, Grenier S, Roberge P. Minimally adequate treatment for depression and anxiety associated with mortality in primary care older adults. Can J Psychiatry. (2022) 67(9):669–78. doi: 10.1177/07067437221082883
21. Lu MW, Duckart JP, O’Malley JP, Dobscha SK. Correlates of utilization of PTSD specialty treatment among recently diagnosed veterans at the VA. Psychiatr Serv. (2011) 62(8):943–9. doi: 10.1176/ps.62.8.pss6208_0943
22. Seal KH, Maguen S, Cohen B, Gima KS, Metzler TJ, Ren L, et al. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses: VA mental health utilization in OEF and OIF veterans. J Trauma Stress. (2010) 23(1):5–16. doi: 10.1002/jts.20493
23. Spoont MR, Murdoch M, Hodges J, Nugent S. Treatment receipt by veterans after a PTSD diagnosis in PTSD, mental health, or general medical clinics. Psychiatr Serv. (2010) 61(1):58–63. doi: 10.1176/ps.2010.61.1.58
24. Suzuki E, Yamamoto E, Takao S, Kawachi I, Subramanian SV. Clarifying the use of aggregated exposures in multilevel models: self-included vs. self-excluded measures. PLoS One. (2012) 7(12):e51717. doi: 10.1371/journal.pone.0051717
25. Istat. Popolazione Residente (2023). Available online at: https://demo.istat.it/app/?l=it&a=2023&i=POS (Accessed May 23, 2023).
26. Barbui C, Papola D, Saraceno B. The Italian mental health-care reform: public health lessons. Bull World Health Organ. (2018) 96(11):731–731A. doi: 10.2471/BLT.18.216002
27. Lombardy Region. Services for the Protection of Mental Health. Information Sheet. Available online at: https://www.regione.lombardia.it/wps/portal/istituzionale/HP/DettaglioRedazionale/servizi-e-informazioni/cittadini/salute-e-prevenzione/Cure-specialistiche-e-consultori/tutela-salute-mentale/tutela-salute-mentale#:∼:text=In%20Lombardia%20sono%20operanti% (Accessed October 3, 2022).
28. Lora A. An overview of the mental health system in Italy. Ann Ist Super Sanita. (2009) 45(1):5–16.19567972
29. Monzio Compagnoni M. The quality of clinical pathways delivered to patients with severe mental disorders. A multi-regional Italian investigation based on healthcare utilization databases. The QUADIM project (Phd thesis). University of Milano-Bicocca, School of Medicine and Surgery, Milan (2020). [First Edition I]. Available online at: https://hdl.handle.net/10281/262317 (Accessed October 25, 2025).
30. Corrao G, Monzio Compagnoni M, Barbato A, D’Avanzo B, Di Fiandra T, Ferrara L, et al. From contact coverage to effective coverage of community care for patients with severe mental disorders: a real-world investigation from Italy. Front Psychiatry. (2022) 13:1014193. doi: 10.3389/fpsyt.2022.1014193
31. Corrao G, Rea F, Di Martino M, De Palma R, Scondotto S, Fusco D, et al. Developing and validating a novel multisource comorbidity score from administrative data: a large population-based cohort study from Italy. BMJ Open. (2017) 7(12):e019503. doi: 10.1136/bmjopen-2017-019503
32. Corrao G, Rea F, Carle F, Di Martino M, De Palma R, Francesconi P, et al. Measuring multimorbidity inequality across Italy through the multisource comorbidity score: a nationwide study. Eur J Public Health. (2020) 30(5):916–21. doi: 10.1093/eurpub/ckaa063
33. Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. (2006) 15(8):565–74. doi: 10.1002/pds.1230
34. Suissa S. Immeasurable time bias in observational studies of drug effects on mortality. Am J Epidemiol. (2008) 168(3):329–35. doi: 10.1093/aje/kwn135
35. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. (2009) 38(6):1228–34. doi: 10.1080/03610910902859574
36. Normand SLT, Landrum MB, Guadagnoli E, Ayanian JZ, Ryan TJ, Cleary PD, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly. J Clin Epidemiol. (2001) 54(4):387–98. doi: 10.1016/S0895-4356(00)00321-8
37. Greenland S. Dose-response and trend analysis in epidemiology: alternatives to categorical analysis. Epidemiology. (1995) 6(4):356–65. doi: 10.1097/00001648-199507000-00005
38. Herndon JE, Harrell FE. The restricted cubic spline as baseline hazard in the proportional hazards model with step function time-dependent covariables. Stat Med. (1995) 14(19):2119–29. doi: 10.1002/sim.4780141906
39. Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. (2017) 210(2):119–24. doi: 10.1192/bjp.bp.116.188078
40. Pratt SI, Mueser KT, Driscoll M, Wolfe R, Bartels SJ. Medication nonadherence in older people with serious mental illness: prevalence and correlates. Psychiatr Rehabil J. (2006) 29(4):299–310. doi: 10.2975/29.2006.299.310
41. Borges G, Aguilar-Gaxiola S, Andrade L, Benjet C, Cia A, Kessler RC, et al. Twelve-month mental health service use in six countries of the Americas: a regional report from the world mental health surveys. Epidemiol Psychiatr Sci. (2020) 29:e53. doi: 10.1017/S2045796019000477
42. Cairney J, Veldhuizen S, Vigod S, Streiner DL, Wade TJ, Kurdyak P. Exploring the social determinants of mental health service use using intersectionality theory and CART analysis. J Epidemiol Community Health. (2014) 68(2):145–50. doi: 10.1136/jech-2013-203120
43. Levine DS, McCarthy JF, Cornwell B, Brockmann L, Pfeiffer PN. Primary care–mental health integration in the VA health system: associations between provider staffing and quality of depression care. Psychiatr Serv. (2017) 68(5):476–81. doi: 10.1176/appi.ps.201600186
44. Vigo DV, Kazdin AE, Sampson NA, Hwang I, Alonso J, Andrade LH, et al. Determinants of effective treatment coverage for major depressive disorder in the WHO world mental health surveys. Int J Ment Health Syst. (2022) 16(1):29. doi: 10.1186/s13033-022-00539-6
45. Woods A, Solomonov N, Liles B, Guillod A, Kales HC, Sirey JA. Perceived social support and interpersonal functioning as predictors of treatment response among depressed older adults. Am J Geriatr Psychiatry. (2021) 29(8):843–52. doi: 10.1016/j.jagp.2020.12.021
46. Corrao G, Mancia G. Research strategies in treatment of hypertension: value of retrospective real-life data. Eur Heart J. (2022) 43(35):3312–22. doi: 10.1093/eurheartj/ehab899
47. Islek D, Kilic B, Akdede BB. Out-of-pocket health expenditures in patients with bipolar disorder, anxiety, schizophrenia and other psychotic disorders: findings from a study in a psychiatry outpatient clinic in Turkey. Soc Psychiatry Psychiatr Epidemiol. (2018) 53(2):151–60. doi: 10.1007/s00127-017-1465-y
48. Pauly NJ, Talbert JC, Brown J. Low-cost generic program use by medicare beneficiaries: implications for medication exposure misclassification in administrative claims data. J Manag Care Spec Pharm. (2016) 22(6):741–51. doi: 10.18553/jmcp.2016.22.6.741
49. Sevilla-Dedieu C, Kovess-Masfety V, Gilbert F, Vilagut G, Koenig HH, Bruffaerts R, et al. Mental health care and out-of-pocket expenditures in Europe: results from the ESEMeD project. J Ment Health Policy Econ. (2011) 14(2):95–105.21881165
50. Corrao G, Mancia G. Generating evidence from computerized healthcare utilization databases. Hypertension. (2015) 65(3):490–8. doi: 10.1161/HYPERTENSIONAHA.114.04858
Keywords: mental healthcare, healthcare services, healthcare utilization database, minimally adequate treatment, healthcare research, public health, severe mental illness, multilevel analysis
Citation: Corrao G, Monzio Compagnoni M, Conflitti C, Sacchi P and Lora A (2025) Association between organizational characteristics of community-oriented mental health facilities and treatment adequacy. A multilevel analysis from Lombardy, Italy. Front. Health Serv. 5:1655225. doi: 10.3389/frhs.2025.1655225
Received: 27 June 2025; Accepted: 28 October 2025;
Published: 21 November 2025.
Edited by:
Graham Reid, Western University, CanadaReviewed by:
Giuseppe Di Martino, G. d'Annunzio University of Chieti and Pescara, ItalyMatthieu Lebrat, Hospices Civils de Lyon, France
Copyright: © 2025 Corrao, Monzio Compagnoni, Conflitti, Sacchi and Lora. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matteo Monzio Compagnoni, bWF0dGVvLm1vbnppb2NvbXBhZ25vbmlAdW5pbWliLml0
†These authors have contributed equally to this work and share first authorship
‖ORCID:
Giovanni Corrao
orcid.org/0000-0002-1034-8444
Matteo Monzio Compagnoni
orcid.org/0000-0002-2105-4572
Claudia Conflitti
orcid.org/0009-0009-1502-4228
Antonio Lora
orcid.org/0000-0002-6806-5199
 Giovanni Corrao
Giovanni Corrao Matteo Monzio Compagnoni
Matteo Monzio Compagnoni Claudia Conflitti
Claudia Conflitti Paola Sacchi8
Paola Sacchi8