- 1Department of Social Work, Umeå University, Umeå, Sweden
- 2School of Public Health and Community Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
The objectives are to, for neighborhoods with different levels of social capital, (1) map out the levels of social interactions, emotional support, and instrumental support before the COVID-19 crisis, (2) analyze how social interactions, emotional support, and instrumental support had changed during the pandemic and, (3) analyze changes in self-rated health during the pandemic. This study is based on a telephone survey with a subsample of 168 respondents in Umeå municipality who participated in a large base-line social capital survey in 2006. We asked whether neighbors talk to, care for, and help each other, before and during the Covid crisis. Individuals rated their health as poor or good. We compared people's self-rated health and their perceptions about their neighborhoods between those who lived in high or low/medium social capital neighborhoods. Before the pandemic, participants in high social capital neighborhoods reported more active neighborhood interaction and support. During the crisis, social interaction and support increased in all neighborhoods, but more in high social capital neighborhoods. Overall, people seemed to help and care for each other more during than before the crisis. More individuals in the high social capital neighborhoods reported improvement in their health during the pandemic, than those in the low/medium social capital neighborhoods. Our findings indicate that neighborhoods social capital can be strengthened during a crisis, in particular in areas with existing high levels of social capital. The findings need to be interpreted carefully due to its small sample size but observed patterns warrant further investigation.
Introduction
Together with other UN members, Sweden has ratified the 2030 Agenda for Sustainable Development, containing 17 goals for ensuring economic, environmental, and social sustainability. Social sustainability allows many different interpretations but involves preserving and developing social values, such as strengthening social cohesion, preventing segregation, and promoting integration (Boström, 2012; United Nations, 2016; Ström et al., 2017). Thus, social sustainability clearly relates to the concept of social capital. Social capital, conceptualized as a characteristic of a local area, emanates from the work of the political scientist Putnam (2000). According to Putnam, a community with high social capital is characterized by the existence of dense and strong social networks, high involvement in these networks, and strong norms of reciprocity and generalized trust between people. Therefore, social capital can be useful as a conceptual tool in local policies for social sustainability. Putnam (1993, 2000) differentiates between three essential forms of social capital: networks of civic engagement, norms of reciprocity, and social trust. These forms influence each other in that networks foster norms of reciprocity which in turn create social trust. Reciprocity is created by the obligations that are almost always involved in social networks (Putnam, 2000), indicating that when people interact in social networks, norms of reciprocal help and support become the glue that holds the network together. In addition, social capital is divided into structural and cognitive forms. Structural social capital refers to the actual participation in networks and the social interaction between people, while cognitive social capital refers to perceptions about social network involvement such as trust and reciprocity norms (Krishna and Shrader, 2000; Harpham et al., 2002).
Studies suggest that living in an area with high social capital is good for health, at least for some population groups (Kim et al., 2008; Eriksson et al., 2011, 2019; Gilbert et al., 2013; Ehsan et al., 2019; Rodgers et al., 2019). Previous research also shows how the nature and level of social capital affect the ways communities manage different forms of crisis. Societies and neighborhoods with high levels of social capital tend to be more resilient, recover more easily, and facilitate adaptation processes (e.g., Nakagawa and Shaw, 2004; Helliwell et al., 2014; Aldrich and Meyer, 2015). However, little is known about how social capital is created and how it might be influenced by a pandemic, with restrictions such as staying at home and avoiding close contact with other people. A recent literature review indicates that access to social networks decreases during times of crisis, and especially so for older and marginalized groups (Gauthier et al., 2021). Therefore, investigating how social support and social relationships between neighbors might change during the COVID-19 pandemic is needed.
In our ongoing research project (Santosa et al., 2020), we use social capital, conceptualized as a collective, place-specific feature in our theoretical framework to explore how social capital can be used as a conceptual tool in housing policy for social sustainability in the north of Sweden. For the sub-study described in this paper, we use collective social capital to understand how a societal crisis like the COVID-19 pandemic affects neighbor relations in Umeå municipality. We investigate possible changes in three different dimensions of social capital, one structural form and two cognitive forms: social interactions (social networks, structural social capital), emotional support (reciprocity norms, cognitive social capital), and instrumental support (reciprocity norms, cognitive social capital). Due to the nature of the pandemic, where physical contact is restricted while the need for practical support might be high, we can expect different patterns of change for different forms of social capital.
The objective of this brief research report is (1) to map out the levels of social interactions, emotional support, and instrumental support in neighborhoods with different levels of social capital before the COVID-19 crisis, (2) to analyze how social interactions, emotional support, and instrumental support had changed during the COVID-19 crisis in neighborhoods with different levels of social capital, and (3) to analyze changes in self-rated health during the COVID-19 crisis across neighborhoods with different social capital levels.
Method
This paper presents results from a telephone survey with a subsample of 168 respondents. The survey is part of a larger research project on neighborhood social capital conducted in Umeå municipality, in northern Sweden (Santosa et al., 2020). In the beginning of 2020, just over 18,000 adult individuals living in Umeå municipality received a social capital survey by mail. The majority consisted of a new cross-sectional sample but the sample included 2,419 individuals who participated in a previous baseline survey on social capital in 2006/2007. These respondents left their personal ID-number voluntarily and consented to be contacted by the researchers for a follow-up study. Those who still lived in Umeå municipality by the end of 2019 were invited to participate in the survey. The original questionnaire was developed based on a review of existing international instruments and adapted to a northern Swedish context (see Eriksson et al., 2011). The same protocol and instruments were used as in the baseline 2006/2007, and was approved by the Swedish Ethical Authority (Dnr 2019-04395).
By the end of February 2020 (i.e., before the pandemic started), we had reached a response rate of 33% in the cross-sectional survey and 65% in the follow-up survey. The survey was concluded at the end of June 2020 and the final response rate was 36.4% in the cross-sectional survey and 70.1% in the follow-up survey. To further increase the response in the follow-up survey, we contacted the remaining non-responders in the cohort by phone. For the telephone survey, we constructed a shortened version of the survey instrument and included new questions related to COVID-19. We hypothesize that the COVID-19 crisis had potentially influenced interactions and support between neighbors in the neighborhood. Therefore, we added some questions related to perceptions about social interaction with neighbors and health aspects during the pandemic. The Swedish Ethical Authority provided the ethical permission to conduct the telephone survey (Dnr 2020-02757). A total of 168 individuals agreed to participate in the telephone survey that was conducted during June–November 2020. This resulted in a final response rate of 77.1% among the cohort.
We measured neighborhood social capital based on people's perceptions about their neighborhoods; whether neighbors talk to each other, help each other, are expected to be involved in issues concerning the neighborhood, and care for each other. Responses from the survey participants were used to derive the social capital score for each of the individuals using the principal component analysis methods (Vyas and Kumaranayake, 2006). Subsequently, we averaged the individual-level scores for all individuals who lived in the same neighborhoods to derive the neighborhood-level social capital score. We then ranked the neighborhoods based on their social capital scores from the lowest to the highest and grouped them into quintiles (five equal groups labeled as very low, low, medium, high, and very high) (Eriksson et al., 2011). In this sub-study, we dichotomized the neighborhood social capital level into two groups of high social capital neighborhoods (high and very high) and low/medium social capital neighborhoods (very low, low, and medium).
Three of the social capital variables, i.e., whether neighbors talk to each other, care for each other, and help each other less, the same, or more, were chosen to measure changes in social capital during the COVID-19 crisis. They represent different dimensions of social capital and represent social interactions (structural social capital), emotional support (reciprocity norms, cognitive social capital), and instrumental support (reciprocity norms, cognitive social capital), consecutively. These are the three dimensions that could be expected to be affected differently due to the nature of the pandemic, with staying-at-home restrictions and recommendations to avoid physical contact with other people. Perceptions about changes were dichotomized in the analysis into categories of increase (more) or no increase (the same or less).
Health was measured as self-rated health on a 5-point Likert scale, from very good to very poor. We dichotomized the variable into good health (very good/good) and bad health (very bad/bad/moderate).
We presented the results in descriptive tables, comparing individuals in the high vs. low/medium social capital neighborhoods. We assessed the level of social capital dimensions and health before the COVID-19 pandemic, and their changes during the pandemic.
Results
A total of 168 individuals, with a mean age of 41 years old and 54% of which were men, participated in the telephone interview. 35.7% lived in high social capital neighborhoods and 64.3% lived in low/medium social capital neighborhoods.
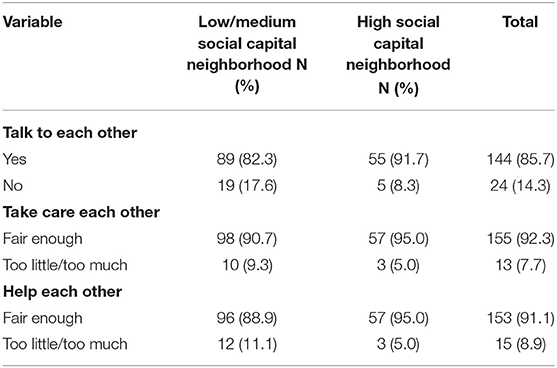
Levels of Social Interactions, Emotional Support, and Instrumental Support in Neighborhoods With Different Levels of Social Capital Before COVID-19
Table 1 illustrates that, before the pandemic, participants in high social capital neighborhoods reported higher levels of social interactions and emotional and instrumental support compared to those in the low/medium social capital neighborhoods. People in high social capital neighborhoods talked to each other more and were more satisfied with how much people in their neighborhood cared for each other and how much they were willing to help each other, as could be expected. None of the differences were statistically significant though due to the small sample size.
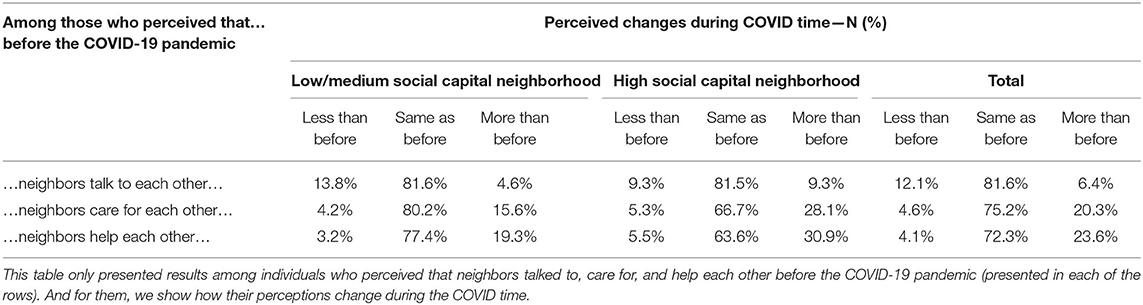
Changes in the Levels of Social Interactions, Emotional Support, and Instrumental Support in Neighborhoods With Different Levels of Social Capital During the Pandemic
Table 2 shows that, during the COVID-19 crisis, a higher proportion of our participants perceived that the levels of social capital increased during the pandemic, or at least remained the same as before, while a smaller proportion perceived that the levels of social capital decreased during the pandemic. This is true when asked to assess if neighbors cared for and helped each other during the pandemic, but not when asked if neighbors talked to each other (12.1% perceived that neighbors talked less as compared to only 6.4% who perceived that neighbors talked more during the pandemic). Among individuals who already perceived that neighbors talked, cared for, and helped each other before the pandemic, more of individuals who lived in the high social capital neighborhoods perceived that neighbors talked more, care for more, and helped each other more during the COVID-19 crisis (9.3, 28.1, 30.9%, respectively) compared to those living in the low/medium social capital neighborhoods (4.6, 15.6, 19.3%, respectively).
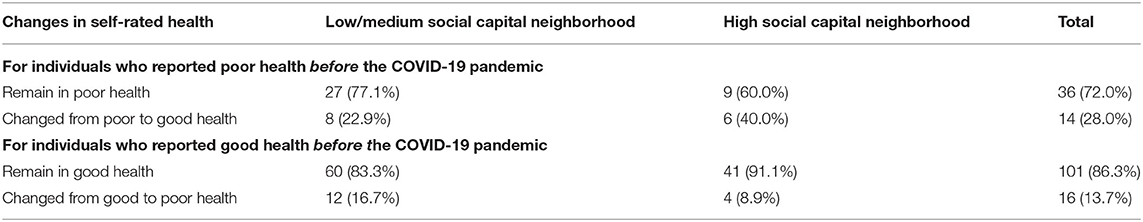
Changes in Self-Reported Health in Neighborhoods With Different Levels of Social Capital During the Pandemic
Table 3 illustrates how self-reported health has changed during the COVID-19 pandemic for people living in the low/medium vs. high social capital neighborhoods. Overall, 68.9% of respondents stayed healthy. Of those reported poor health before the pandemic, 72% did not improve their health and the remaining 28% reported better health during the pandemic. A higher proportion of those living high social capital neighborhoods reported better health during the pandemic compared to those living in low/medium social capital neighborhoods (40 vs. 22.9%, respectively).
Of those reported good health before the pandemic, 13.7% reported worse health during the pandemic. The majority of people in both low/medium and high social capital neighborhoods who reported good health before the pandemic rated their health as equally good during COVID-19 pandemic (91.1 and 83.3%, respectively). These figures must be cautiously interpreted, due to the low number of participants.
Discussion
This brief research report presents results from an ongoing project that investigates the role of social capital for health and wellbeing in local neighborhoods, and how local social capital might change over time due to housing and social interventions. Our research setting in Northern Sweden is characterized by long-term political and social stability. However, the sudden global COVID-19 pandemic has led to a societal crisis with several challenges such as fear, social insecurity, and social isolation. The staying-at-home restriction measures during the COVID-19 crisis might make the immediate neighborhood become even more important. Since our data collection took place during the first wave of the pandemic, we had the possibility to study how a pandemic crisis might possibly influence neighborhood social interactions and support.
Unsurprisingly, the study shows that before the pandemic, those living in neighborhoods with high social capital reported higher levels in all three dimensions of social capital investigated in this report compared to the ones living in low/medium social capital neighborhoods. Moreover, the results show that during a time when government restrictions encouraged social isolation and limiting social networks, many respondents reported that social capital has grown stronger in both the high and the low/medium social capital neighborhoods. Several respondents perceived that neighbors cared more for each other and were more willing to help each other than before the crisis, the latter being the one that has increased the most. These patterns were consistent for both high and low/medium social capital neighborhoods. However, this increase was greater for the neighborhoods that already had high social capital before the crisis. These results indicate that neighborhood relations might become even more important in times of societal crisis and social restriction measures, when the access to and usage of public social support services might decrease. A recent survey among older people in the UK found that usage of social support service decreased significantly post COVID-19, resulting in an increased level of anxiety (Giebel et al., 2020). Our survey results show that more respondents who lived in the low/medium social capital neighborhoods reported poor health during the pandemic compared to those in high social capital neighborhoods. This indicates that living in a neighborhood with high social capital seems to be protective when it comes to maintaining wellbeing during times of crisis. Several studies from various countries have found protective effects from social support and social networks during the COVID-19 pandemic (e.g., Killgore et al., 2020; Özmete and Pak, 2020; Qi et al., 2020; Yu et al., 2020; Skalski et al., 2021). The findings in our study need to be interpreted carefully considering the threat of a selection bias. The respondents who experienced very poor health could have been less likely to participate in a telephone survey or even to answer the call, resulting in a potentially healthier and unrepresentative sample of people participating in our study.
Findings from this study indicate that neighborhoods with high social capital seem to be more resilient to crises like the COVID-19 pandemic. This corresponds with findings from previous research, suggesting that a high level of social capital promotes health (Kim et al., 2008; Gilbert et al., 2013; Ehsan et al., 2019; Rodgers et al., 2019). Previous research also found that social capital can contribute to resilience in times of crises. Aldrich and Meyer (2015) demonstrate several examples (mainly of natural disasters) where strong social capital within and across social groups has proven important both during crises, through mobilization and sharing of resources and knowledge, and for rebuilding and recovering in post-disaster communities. Helliwell et al. (2014) point to the importance of social capital, particularly social trust, for the experience of well-being in the context of rapid institutional transition in Europe. Moreover, several previous studies have pointed to social capital as a factor associated with adherence to government recommendations during the COVID-19 pandemic, and thus potentially affecting the spread of the virus and health outcomes directly related to influenza (e.g., Bai et al., 2020; Fraser et al., 2020; Makridis and Wu, 2021; Wu, 2021). The results from our current study could indicate that high levels of social capital may also mitigate other health risks caused by the crisis, such as mental health and general well-being.
Another interesting finding is that respondents in both the high and the low/medium social capital neighborhoods reported strengthened social capital in two of the three social capital dimensions during the crisis compared to before (care and help between neighbors), suggesting that crises like the pandemic might foster increased support among neighbors. Perhaps such increased levels of social capital can be seen as an effect of government recommendations to limit social networks and restrict movement, thus making interaction with the local community increasingly important. A study from Egypt (El-Zoghby et al., 2020) found that social support from family members increased more than support from friends during the COVID-19 pandemic, indicating the importance of proximity in social networks. Thus, for people living alone, the proximity of relationships among neighbors might be crucial for accessing social support during a pandemic crisis.
The findings in this study need to be interpreted carefully due to its small sample size. Nevertheless, the different patterns of social interaction and support observed in neighborhoods with different levels of social capital warrant further investigation to understand how a societal and public health crisis like the COVID-19 pandemic affects different neighborhoods. We believe that our findings from this small-scale survey can contribute to increasing our understanding about how social capital might operate during a time of societal crisis, and that it can inspire and inform further research on the topic.
Data Availability Statement
The datasets presented in this article are not readily available because of restrictions in the ethical approval for this project. Questions related to the data in this study should be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Swedish Ethics Review Authority (Dnr: 2019-04395; Dnr: 2020-00160; Dnr 2020-02757). The participants provided their informed consent to participate in this study.
Author Contributions
LZ, AS, ME, and NN conceptualized the study. LZ and MK collected the data. AS and NN analyzed the data. All authors contributed to the drafting of the manuscript, critically reviewed, and provided feedback on the final revised version of the manuscript.
Funding
This project was funded by Formas, the Swedish Research Council for Sustainable Development (Dnr. 2018-00262 and Dnr. 2018-00276).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aldrich, D. P., and Meyer, M. (2015). Social capital and community resilience. Am. Behav. Sci. 59:2. doi: 10.1177/0002764214550299
Bai, J. J., Jin, W., and Wan, C. (2020). The impact of social capital on individual responses to COVID-19 pandemic: evidence from social distancing. SSRN Electron. J. doi: 10.2139/ssrn.3609001. [Epub ahead of print].
Boström, M. (2012). A missing pillar? challenges in theorizing and practicing social sustainability: introduction to the special issue. Sustain. Sci. Pract. Policy 8.1. doi: 10.1080/15487733.2012.11908080
Ehsan, A., Klaas, H. S., Bastianen, A., and Spini, D. (2019). Social capital and health: a systematic review of systematic reviews. SSM Popul. Health 8:100425. doi: 10.1016/j.ssmph.2019.100425
El-Zoghby, S. M., Soltan, E. M., and Salama, H. M. (2020). Impact of the COVID-19 pandemic on mental health and socialsupport among adult egyptians. J. Community Health 45, 689–695. doi: 10.1007/s10900-020-00853-5
Eriksson, M., Lindgren, U., Ivarsson, A., and Ng, N. (2019). The effect of neighbourhood social capital on child injuries: a gender-stratified analysis. Health Place 60:102205. doi: 10.1016/j.healthplace.2019.102205
Eriksson, M., Ng, N., Weinehall, L., and Emmelin, M. (2011). The importance of gender and conceptualization for understanding the association between collective social capital and health: a multilevel analysis from northern Sweden. Soc. Sci. Med. 73, 264–273. doi: 10.1016/j.socscimed.2011.05.013
Fraser, T., Aldrich, D. P., and Tan, C. (2020). Bowling alone or masking together? the role of social capital in excess death rates from COVID19. SSRN Electron. J. doi: 10.2139/ssrn.3744251. [Epub ahead of print].
Gauthier, G. R., Smith, J. A., Garcia, C., Garcia, M. A., and Thomas, P. A. (2021). Exacerbating inequalities: social networks, racial/ethnic disparities, and the COVID-19 pandemic in the United States. J. Gerontol. Ser. B 76:3. doi: 10.1093/geronb/gbaa117
Giebel, C., Lord, K., Cooper, C., Shenton, J., Cannon, J., Pulford, D., et al. (2020). A UK survey of COVID-19 related social support closures and their effects on older people, people with dementia, and carers. Int. J. Geriatr. Psychiatry 36:3. doi: 10.1002/gps.5434
Gilbert, K. L., Quinn, S. C., Goodman, R. M., Butler, J., and Wallace, J. (2013). A meta-analysis of social capital and health: a case for needed research. J. Health Psychol. 18, 1385–1399. doi: 10.1177/1359105311435983
Harpham, T., Grant, E., and Thomas, E. (2002). Measuring social capital within health surveys: key issues. Health Policy Plan. 17, 106–111. doi: 10.1093/heapol/17.1.106
Helliwell, J. F., Huang, H., and Wang, S. (2014). Social capital and well-being in times of crisis. J. Happiness Stud. 15, 145–162. doi: 10.1007/s10902-013-9441-z
Killgore, W., Taylor, E., Cloonan, S., and Dailey, N. (2020). Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 291:113216. doi: 10.1016/j.psychres.2020.113216
Kim, D., Subramanian, S. V., and Kawachi, I. (2008). “Social capital and physical health: a systematic review of the literature,” in Social Capital and Health, eds I. Kawachi, S.V. Subramanian, and D. Kim. (New York, NY: Springer), 139–190.
Krishna, A., and Shrader, E. (2000). Cross-Cultural Measures of Social Capital: A Tool and Results From India and Panama. Social Capital Initiative, Working paper No. 21. Washington, DC: The World Bank. Available online at: http://siteresources.worldbank.org/INTRANETSOCIALDEVELOPMENT/882042-1111750197177/20502292/SCI-WPS-21-paper.pdf (accessed February 15, 2021).
Makridis, C. A., and Wu, C. (2021). How Social capital helps communities weather the COVID-19 pandemic. PLoS ONE 16:e0245135. doi: 10.1371/journal.pone.0245135
Nakagawa, Y., and Shaw, R. (2004). Social capital: a missing link to disaster recovery. Int. J. Mass Emerg. Disasters 22, 5–34.
Özmete, E., and Pak, M. (2020). The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Soc. Work Public Health 35:7. doi: 10.1080/19371918.2020.1808144
Putnam, R. D. (1993). Making Democracy Work: Civic Traditions in Modern Italy. Princeton, NJ: Princeton University Press.
Putnam, R. D. (2000). Bowling Alone: The Collapse and Revival of American Community. New York, NY: Simon and Schuster.
Qi, M., Zhou, S.-J., Guoc, Z.-C., Zhang, L.-G., Min, H.-J., Li, X.-M., et al. (2020). The effect of social support on mental health in chinese adolescents during the outbreak of COVID-19. J. Adolesc. Health 67:4. doi: 10.1016/j.jadohealth.2020.07.001
Rodgers, J., Valuev, A. V., Hswen, Y., and Subramanian, S. V. (2019). Social capital and physical health: an updated review of the literature for 2007–2018. Soc. Sci. Med. 236:112360. doi: 10.1016/j.socscimed.2019.112360
Santosa, A., Ng, N., Zetterberg, L., and Eriksson, M. (2020). Study protocol: social capital as a resource for the planning and design of socially sustainable and health promoting neighborhoods–a mixed method study. Front. Public Health 8:581078. doi: 10.3389/fpubh.2020.581078
Skalski, S., Urama, P., Dobrakowski, P., and Kwiatkowskaa, A. (2021). The link between ego-resiliency, social support, SARS-CoV-2 anxiety, and trauma effects. Polish adaptation of the Coronavirus Anxiety Scale. Pers. Individ. Diff. 171:110540. doi: 10.1016/j.paid.2020.110540
Ström, L., Molnar, S., and Isemo, S. (2017). Social hållbarhet ur ett samhällsplaneringsperspektiv—en kunskapsöversikt [Social Capital From a Planning Perspective—An Overview]. Gothenburg: Mistra Urban Future.
United Nations (2016). The Sustainable Development Agenda. New York, NY: Department of Economic and Social Affairs.
Vyas, S., and Kumaranayake, L. (2006). Constructing socioeconomic status indices: how to use principal component analysis. Health Policy Plan. 6, 459–468. doi: 10.1093/heapol/czl029
Wu, C. (2021). Social capital and COVID-19: a multidimensional and multilevel approach. Chin. Sociol. Rev. 53:1. doi: 10.1080/21620555.2020.1814139
Keywords: COVID, neighborhood, social capital, social interaction, emotional support, instrumental support, Sweden, social sustainability
Citation: Zetterberg L, Santosa A, Ng N, Karlsson M and Eriksson M (2021) Impact of COVID-19 on Neighborhood Social Support and Social Interactions in Umeå Municipality, Sweden. Front. Sustain. Cities 3:685737. doi: 10.3389/frsc.2021.685737
Received: 25 March 2021; Accepted: 05 May 2021;
Published: 09 June 2021.
Edited by:
Linchuan Yang, Southwest Jiaotong University, ChinaReviewed by:
Jixiang Liu, The University of Hong Kong, ChinaYibin Ao, Chengdu University of Technology, China
Copyright © 2021 Zetterberg, Santosa, Ng, Karlsson and Eriksson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liv Zetterberg, bGl2LnpldHRlcmJlcmdAdW11LnNl
 Liv Zetterberg
Liv Zetterberg Ailiana Santosa
Ailiana Santosa Nawi Ng
Nawi Ng Matilda Karlsson
Matilda Karlsson Malin Eriksson
Malin Eriksson