- 1Centre for Rehabilitation and Ageing Research, University of Nottingham, Nottingham, United Kingdom
- 2Rehabilitation Medicine, University Hospitals of Derby and Burton NHS Foundation Trust, Derby, United Kingdom
Objective: To assess the feasibility of delivering a virtual reality relaxation intervention on an inpatient neurorehabilitation unit within the NHS.
Methods: An open-label feasibility study. Participants undergoing inpatient neurorehabilitation were recruited to use a virtual-reality distraction intervention under the guidance of a clinician with a minimum of one session per participant and no upper limit. The main outcome measures were around recruitment and retention, acceptability, pain, and anxiety.
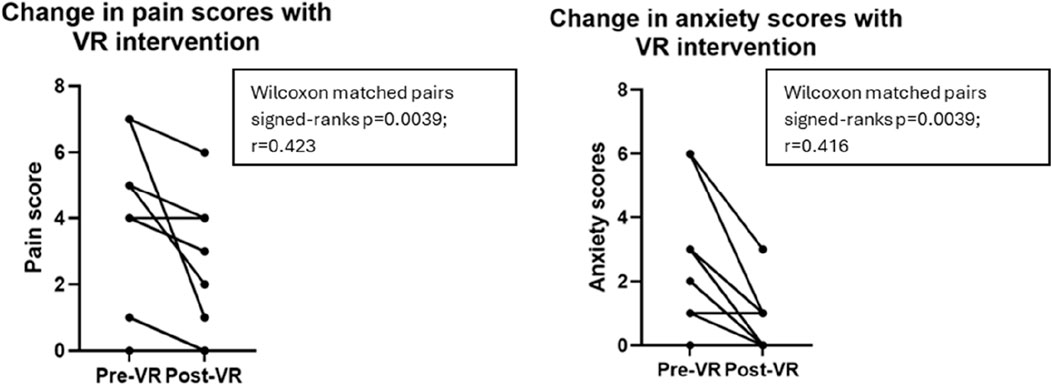
Results: Recruitment was lower than anticipated due to many potential participants not meeting inclusion criteria. Nine participants were recruited and used the intervention a total of 23 times. Pain and anxiety scores were statistically significantly reduced (p = 0.0039 for both). Participants enjoyed using the VR. No serious adverse events were noted.
Conclusion: Virtual reality relaxation is enjoyable and successfully reduced pain and anxiety scores in patients on our neurorehabilitation unit, but only few neurorehabilitation inpatients were eligible for this study.
Introduction
Inpatient neurorehabilitation can be challenging. Following acute illness or injury, patients often spend a long time in hospital before arriving at the rehabilitation unit, and they often face a lengthy stay as a rehabilitation inpatient. They are in an unfamiliar place, often dependent on others for many activities of daily living, they do not see their friends and family as often as they would like, and they are often restricted to a hospital ward for most hours of the day. They may face uncertainty around prognosis, discharge, and the future. Depression, anxiety, and low motivation are common and associated with poor rehabilitation outcomes (Lewis and Horn, 2017; Haagsma et al., 2015).
Virtual reality (VR) is increasingly used in healthcare. There has been considerable research into its use in cognitive and physical rehabilitation and into its effects on pain, mood, and wellbeing. VR “…allows the participant to experience a sense of presence in an immersive, computer-generated, three-dimensional environment that … facilitates emotional involvement” (Gerardi et al., 2010). Enjoyable VR interventions have been shown to help acute (Sikka et al., 2019) and chronic (Maddox et al., 2022) pain as well as anxiety (Sikka et al., 2019).
“Dr. VR” is a VR intervention which is a Class 1 Medical Device developed by Rescape. A feasibility study from an intensive care unit (ICU) in Wales showed that use of Dr. VR significantly improved mood and anxiety in patients, relatives, and staff members and significantly improved pain scores in patients. Dr. VR was concluded to be “safe, feasible and effective” for use in the ICU setting, with overwhelmingly positive qualitative feedback (Lynch and Jones, 2020). While this is promising, the specific challenges of neurorehabilitation necessitated a feasibility study in this setting.
Objectives
To assess the feasibility of delivering a definitive trial around the use of relaxation VR for inpatients undergoing neurorehabilitation in the NHS, we studied the following.
I. Feasibility of recruitment
II. Feasibility of retention
III. Practicality of delivering the intervention
IV. Acceptability of use
V. Feasibility of recording clinical outcome measures
a. Pain
b. Anxiety
Methods
Study design and participants
Ethical approval was given by East of England–Essex Research Ethics Committee (ref: 23/EE/0209) on 2 October 2023. The study was sponsored by the University of Nottingham.
This open-label feasibility study was conducted in an inpatient neurorehabilitation unit located in a community hospital in the East Midlands of the United Kingdom.
Participants were eligible for inclusion if they met the following criteria.
• Admission to King’s Lodge Neurorehabilitation Unit for a period of inpatient neurorehabilitation
• Aged 18 years or over
• Willing and able to give consent
• No history of epilepsy or seizures
• No wound or craniectomy in the area where the VR headset would apply pressure
• Oriented to time/place
Informed consent was taken from all participants.
Intervention
Dr. VR is a VR distraction-therapy product and comprises a PICO VR headset with optional noise-cancelling headphones, operated by a closed system which includes a Samsung tablet and internet router.
Participants were offered VR sessions depending on the availability of staff to deliver and supervise the sessions and participant choice.
Participants chose from a list of 28 VR experiences, classified as “escape” (visiting beautiful, distracting, or interesting locations including swimming underwater in the ocean, hiking through beaches and forests, and viewing wildlife or dinosaurs), “relax” (guided meditations in a range of environments), and “play” (interactive games). Most experiences lasted for 7–8 min.
A clinician supervised participants throughout the VR session, including helping with donning and doffing the headset and completing outcome measures if necessary.
Data collection
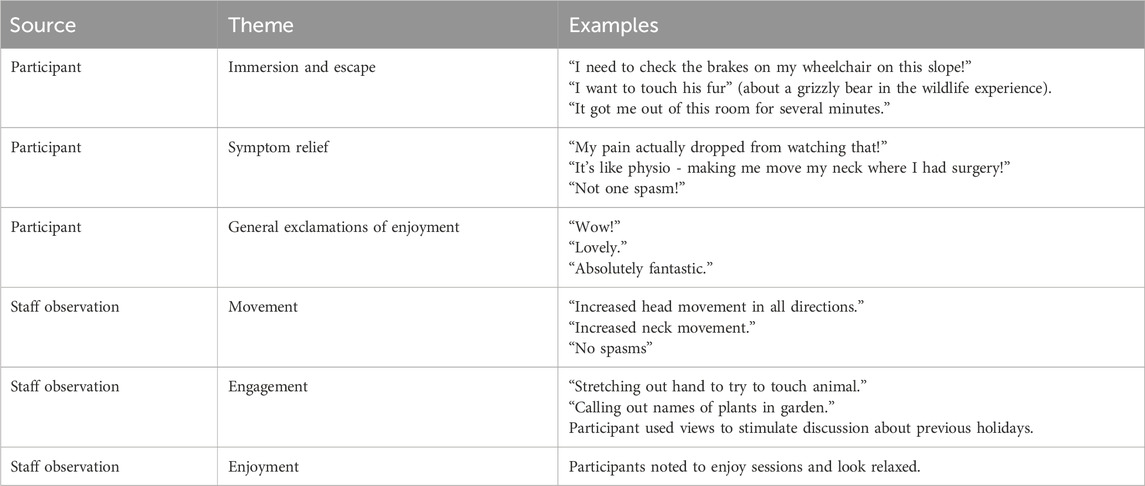
Participants scored their pain and anxiety severity using a face-based Likert scale before and after each VR intervention, scoring from 0 (no pain/anxiety) to 10 (extreme pain/anxiety). Supervising clinicians recorded comments made by participants during or immediately after the sessions and any relevant behaviours or movements from participants during the session. Acceptability for patients was based on willingness to use the VR headset; acceptability to staff was based on staff feedback.
Data analysis
Pain and anxiety scores were exported to an Excel spreadsheet and analysed using GraphPad Prism 10.
Comments made by participants and observations made by staff were handwritten at the time of or immediately following the session, transcribed into a Word document, and analyzed using simple thematic analysis.
Results
The CONSORT flow diagram is shown in the supplementary information.
Nine participants were recruited: three women and six men. Median age was 56 years, ranging from 34–83 years. Four participants were undergoing rehabilitation following a spinal cord injury, two had sustained a brain injury, and the remaining three had an acquired peripheral nerve injury.
In total, the nine participants used the device 23 times, with per-participant use ranging from one to six times.
Feasibility of recruitment
Forty potential participants were excluded. Among the common reasons for exclusion were the following:
• 10—not sufficiently oriented
• 7—declined to participate
• 7—medical outliers
• 6—history of seizures/epilepsy
• 5-significant hearing/visual impairment
• 3—craniectomy wound in area where device would sit
Feasibility of retention
1 participant used the device only once and then declined further use as they reported visual difficulties which had not previously been identified.
1 participant used the device twice then declined further use due to fatigue.
1 participant used the device on a total of 3 occasions but declined two sessions during the total due to fatigue.
2 more participants used the device only once but were keen to use it more; 3 participants used between 2-4 times and one participant used 6 times. All of these participants were keen to use the device more and did not decline any sessions.
The fatigue and visual disturbances were not directly related to the use of the VR.
Practicality of delivering the intervention
Of the 23 sessions delivered, 18 were delivered by a neurorehabilitation doctor, two by a physiotherapist, two by a speech and language therapist, and one by an occupational therapist. No differences were noted in outcomes depending on who delivered the session.
Several other members of staff were trained to deliver the intervention but, due to time and staffing pressures, could not.
No problems with delivering the intervention were reported in 9/23 sessions.
The most commonly reported problems were around optimizing volume (usually helped by use of noise-cancelling headphones) or headset positioning, particularly where participants had limited manual dexterity and so often relied on the investigator to place the headset on the participant’s head.
Acceptability to patients and staff
No problems were identified.
Feasibility of recording outcome measures
No problems were identified. Outcome measures were recorded pre- and post-intervention for all participants and all sessions.
Outcome measures
Statistically significant improvements were seen in both pain and anxiety scores comparing pre- and post-VR intervention (Figure 1). Comparing all pre- and post-scores, Wilcoxon matched-pair signed-rank test scores were p = 0.0039 for both analyses; effect size r = 0.423 for pain and r = 0.416 for anxiety. Excluding those participants whose starting and finishing scores were 0, median scores of pain were 4.0 pre- and 2.5 post-intervention, with anxiety 3.0 and 0.5, respectively.
Comments and observations
Feedback provided by participants and observations by staff members were nearly all positive (Table 1). One participant felt that the dinosaur park tour was “a bit childish,” and another commented that the dinosaurs “weren’t like you see on tv.” Staff reported that the VR sessions encouraged participants to move their head around to experience the 360° environment and that participants seemed relaxed and keen to discuss their experiences with staff and other patients.
Adverse events
One participant noted on two occasions that, immediately following the removal of the VR headset, they experienced increased sensitivity to ambient lighting, but this self-terminated within a few minutes. No other adverse events were noted.
Discussion
This small feasibility study using a distraction-based VR intervention for inpatients undergoing neurorehabilitation showed that, for patients experiencing pain and/or anxiety, their pain and anxiety scores were significantly lower following this use of VR. This correlated with qualitative feedback from participants who enjoyed the sessions, and most participants were keen to use the VR intervention on more than one occasion. This is in keeping with previous research in VR for pain and anxiety (Lynch and Jones, 2020; Mosadeghi et al., 2016; Tashjian et al., 2017).
Limitations
The study was limited by low participant numbers (primarily due to strict inclusion criteria) and limited staff availability to deliver VR sessions as frequently as might have been preferred. At times, participants did not wish to use the VR, most commonly due to pre-existing fatigue, which is very common for patients undergoing neurorehabilitation. Future research could explore gradual exposure to VR or re-introducing the concept at a later stage of recovery when fatigue is less disabling. Despite this, the positive feedback and improvements in pain and anxiety scores suggest that this type of VR intervention could be useful for selected patients and could be considered in addition to standard neurorehabilitation care.
Conclusion
Virtual-reality distraction therapy is feasible to deliver and can improve symptoms of pain and anxiety in selected patients undergoing inpatient neurorehabilitation. In a patient group with a high likelihood of fatigue and other neurological symptoms, close monitoring for any adverse effects is vital.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by East of England–Essex Research Ethics Committee (ref: 23/EE/0209). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LE: conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, and writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Many thanks to the study participants. I am grateful to the Rescape Team, particularly Gemma James-Smith, for the generous loan of the Dr VR system and all their support and advice. Thanks to Emily Bradley, Fattaneh Zonouzi, Rachel Singleton, and Lewis Craig for help with participant recruitment and intervention delivery.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author declares that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2025.1504894/full#supplementary-material
SUPPLEMENTARY FIGURE S1 | CONSORT diagram representing participant flow through the trial.
References
Gerardi, M., Cukor, J., Difede, J., Rizzo, A., and Rothbaum, B. O. (2010). Virtual reality exposure therapy for post-traumatic stress disorder and other anxiety disorders. Curr. Psychiatry Rep. 12 (4), 298–305. doi:10.1007/s11920-010-0128-4
Haagsma, J. A., Scholten, A. C., Andriessen, T. M., Vos, P. E., Van Beeck, E. F., and Polinder, S. (2015). Impact of depression and post-traumatic stress disorder on functional outcome and health-related quality of life of patients with mild traumatic brain injury. J. Neurotrauma 32 (11), 853–862. doi:10.1089/neu.2013.3283
Lewis, F. D., and Horn, G. J. (2017). Depression following traumatic brain injury: impact on post-hospital residential rehabilitation outcomes. NeuroRehabilitation 40 (3), 401–410. doi:10.3233/nre-161427
Lynch, C., and Jones, G. (2020). Feasibility and potential benefits of immersive virtual reality in the intensive care unit. ICU Manag. Pract. 20 (1), 92–98.
Maddox, T., Garcia, H., Ffrench, K., Maddox, R., Garcia, L., Krishnamurthy, P., et al. (2022). In-home virtual reality program for chronic low back pain: durability of a randomized, placebo-controlled clinical trial to 18 months post-treatment. Reg. Anesth. Pain Med. 49, 373–375. doi:10.1136/rapm-2022-104093
Mosadeghi, S., Reid, M. W., Martinez, B., Rosen, B. T., and Spiegel, B. M. (2016). Feasibility of an immersive virtual reality intervention for hospitalized patients: an observational cohort study. JMIR Ment. Health 3 (2), e28. doi:10.2196/mental.5801
Sikka, N., Shu, L., Ritchie, B., Amdur, R. L., and Pourmand, A. (2019). Virtual reality-assisted pain, anxiety, and anger management in the emergency department. Telemed. J. E Health. 25 (12), 1207–1215. doi:10.1089/tmj.2018.0273
Keywords: virtual reality, neurorehabilitation, relaxation, pain, anxiety
Citation: Edwards L (2025) A feasibility study of the use of virtual reality relaxation in an NHS inpatient neurorehabilitation unit. Front. Virtual Real. 6:1504894. doi: 10.3389/frvir.2025.1504894
Received: 04 October 2024; Accepted: 07 May 2025;
Published: 11 June 2025.
Edited by:
Ceri Lynch, Cwm Taf Morgannwg University Health Board, United KingdomReviewed by:
Omar Janeh, University of Technology, IraqAnfal Astek, King Abdulaziz University, Saudi Arabia
Copyright © 2025 Edwards. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura Edwards, bGF1cmEuZWR3YXJkc0Bub3R0aW5naGFtLmFjLnVr
 Laura Edwards
Laura Edwards