- 1Beijing Normal-Hong Kong Baptist University, Zhuhai, China
- 2Jinan University, Guangzhou, Guangdong, China
Objectives: Chronic pain, particularly when undiagnosed, is often misunderstood by clinicians due to its invisible and subjective nature. This study aimed to design and evaluate a narrative-driven Virtual Reality (VR) experience that immerses medical students in the fragmented reality of a patient living with undiagnosed chronic pain. The project seeks to bridge the empathy gap in clinical training for medical students and healthcare professionals while enhancing understanding of patient experiences.
Methods: We developed a 4-minute immersive VR experience. Seventy undergraduate medical and health professional students with prior clinical exposure to chronic pain patients participated in the study. Following the experience, participants completed two questionnaires: one assessed the usability and validity of the VR application, while the other evaluated the medical students’ empathy and learning outcomes through a comparative analysis of post-experience surveys.
Results: The SUS score was 70.13 ± 7.38, suggesting an above-average evaluation of the system’s usability and maturity. VR-experienced participants showed significantly better comprehension of chronic pain’s daily impacts and stronger emotional resonance with patient suffering. Additionally, the students in VR-experienced group rated the tool higher for its effectiveness in fostering empathy and improving knowledge retention.
Conclusion: Overall, the VR experience achieved the expected outcomes, with students identifying it as an immersive and impactful educational tool. It holds promise for enhancing empathy in clinical training, such as regarding undiagnosed chronic pain, potentially improving diagnosis and treatment approaches. While the results underscore VR’s potential to humanize chronic pain education, future studies should include longitudinal assessments, expanded narratives that reflect diverse patient experiences, and opportunities for users to engage with multiple scenarios, thereby better representing the full spectrum of challenges in many diseases.
1 Introduction
Chronic pain is a pervasive issue affecting millions worldwide, presenting a multifaceted challenge to healthcare systems due to its interplay of physiological, psychological, and social factors (Breivik et al., 2006). Particularly when the underlying cause is undiagnosed. Patients often face skepticism and invalidation from medical professionals and society, leading to significant psychological distress. Conventional pain management strategies, heavily reliant on pharmacotherapy, often yield inconsistent outcomes and carry risks of dependency or adverse effects (Furlan et al., 2006). This underscores the need for innovative, non-invasive interventions. Virtual reality (VR), an immersive technology that simulates three-dimensional (3D) environments, has emerged as a promising tool for modulating pain perception through neural distraction and sensory engagement (Patterson et al., 2010; Hoffman et al., 2000; Lan et al., 2023). Studies demonstrate that VR reduces acute and chronic pain by redirecting cognitive attention and altering pain-processing pathways, offering a scalable alternative to traditional methods (Hoffman et al., 2000; Parsons and Rizzo, 2008).
1.1 VR in chronic pain relief and empathy training
Virtual Reality (VR) has emerged as a transformative tool in healthcare, particularly in managing chronic pain and enhancing empathy among healthcare professionals. The immersive nature of VR allows patients to engage in virtual environments, effectively distracting them from pain and providing therapeutic benefits. Studies have demonstrated that VR significantly reduces acute and chronic pain by diverting attention from pain stimuli through immersive experiences, offering a non-pharmacological alternative for pain management (Moreau et al., 2024). For instance, immersive VR has shown efficacy in controlling pain during medical procedures such as wound care, chemotherapy, and physical therapy, highlighting its adaptability across clinical settings (Teh et al., 2024). Beyond procedural applications, VR also empowers patients to self-manage chronic pain by improving health literacy and equipping them with coping strategies, thereby fostering long-term resilience against discomfort (Lee and Patel, 2023).
In parallel, VR simulations are reshaping empathy training for healthcare providers by enabling them to experience patient perspectives firsthand. Research indicates that VR-based simulations, such as those replicating dual sensory impairments or age-related conditions, enhance empathy among healthcare workers, leading to more compassionate patient interactions (Dutton et al., 2021). Immersive VR has been integrated into medical education to simulate patient experiences, such as chronic illness or cognitive decline, which deepens students’ understanding of patient challenges and improves care quality (Ghaempanah et al., 2024). Virtual patient scenarios in VR further provide a controlled environment for medical trainees to practice empathetic communication, allowing educators to assess and refine their empathetic responses (Gilbert et al., 2024). Similarly, VR-based training programs for mental health staff have proven effective in building empathy by simulating scenarios that mirror service users’ lived experiences, thereby bridging gaps in understanding and fostering patient-centered care (Riches et al., 2022).
1.2 Virtual reality storytelling
Virtual Reality (VR) storytelling is an immersive form of narrative that leverages VR technology to engage users in interactive and enveloping narrative experiences. This dynamic form of storytelling offers users the ability to influence the narrative, making choices that directly impact the outcome. This level of interactivity significantly enhances user agency and complicates narrative design, offering users the opportunity to explore nonlinear storytelling. This dynamic form of storytelling not only increases user agency but also adds complexity to narrative design (Ostrin et al., 2018; Aylett and Louchart, 2003).
A crucial element in VR storytelling is the use of binaural sound, which dramatically enhances the experience of presence. Binaural audio simulates how humans perceive sound in three-dimensional space, adding a layer of realism that heightens the immersive experience (Dourou et al., 2023). This realistic auditory environment deepens the user’s emotional and cognitive connection with the narrative, creating a more convincing and emotionally resonant experience. By engaging multiple senses, both visual and auditory, VR becomes a more powerful tool for emotional engagement than traditional media, making it an ideal medium for applications in therapy and education where emotional depth is essential (Saroka, 2024; Murphy and Pitt, 2001).
Moreover, the cognitive effects of immersive VR storytelling go beyond emotional engagement, influencing memory retention, spatial awareness, and attentional focus. Research indicates that VR can enhance memory and learning outcomes by immersing users in interactive environments, which stimulate cognitive processes essential for learning complex information (Bujić et al., 2023; Conrad et al., 2024; Cummings et al., 2022). This capacity for deep cognitive engagement is why VR has found utility not only in entertainment but also in educational and training applications, where the retention and understanding of material are critical. By combining immersive audio, interactive narrative, and engaging environments, VR storytelling has proven to be a potent tool for both emotional and cognitive development (Conrad et al., 2024).
Current research on VR for chronic pain management has primarily focused on patients with diagnosed conditions, emphasizing pain distraction or clinician empathy training through simulated scenarios (Husain and Chalder, 2021). However, the challenges faced by individuals with undiagnosed chronic pain, such as diagnostic ambiguity, identity-related distress due to medical skepticism, and the lack of tailored interventions, have received limited attention. While immersive VR storytelling shows promise in enhancing emotional engagement and cognitive processing through interactive narratives and multisensory immersion, its potential to validate lived experiences or address the unique therapeutic needs of specific populations, such as those with mental health conditions or trauma, remains underexplored (Lumley et al., 2011). To address the research gaps mentioned above, this VR experience could offer a tool in mitigating distress linked to unexplained pain and bridging gaps in clinician-patient communication.
2 Materials and methods
2.1 VR setup
The virtual reality (VR) experience “It’s All in Your Head” was developed using the Unity game engine and implemented on the Samsung Odyssey immersive headset, chosen for its high-end specifications and ease of setup. The VR application was connected to a development PC meeting recommended hardware specifications (CPU: Intel Core i7-8809G @ 3.1 GHz and GRAPHICS: Radeon RX Vega M GC). The application features interactive representations of neurological pathways, incorporates real patient narratives, and integrates 3D captures of real-world settings. Additionally, existing media assets were adapted into interactive formats, and experimental integration of 3D-printed accessories was explored to expand the platform’s accessibility.
2.2 VR experience design
The design of our VR experience is grounded in an adaptation of Kolb’s Experiential Learning Cycle (1984) (Kolb, 1984). Kolb’s theory posits that transformative learning occurs through a cycle of concrete experience, reflective observation, abstract conceptualization, and active experimentation. Our framework implements this cycle by immersing users in a patient’s perspective (concrete experience), facilitating contemplation through narrative cues (reflective observation), enabling users to derive insights about the patient’s lived reality (abstract conceptualization), and implicitly encouraging empathetic behaviors post-experience (active experimentation). This patient-embodied VR approach is strongly supported by extensive research showing that embodying another’s perspective in VR enhances empathetic understanding. Research by Bertrand et al. and Kalyanaraman et al. establishes a direct link between patient-embodied VR experiences and improved empathy and attitudes among healthcare professionals, further validating the foundation of our methodology (Bertrand et al., 2018; Kalyanaraman et al., 2010).
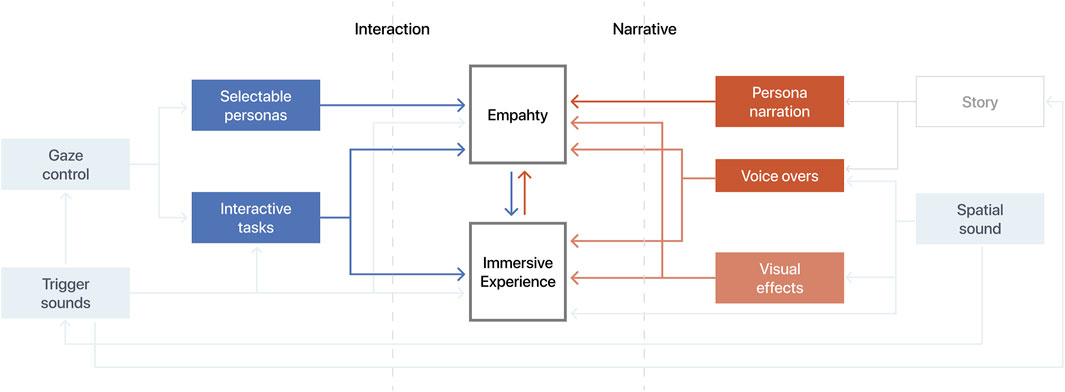
As illustrated in Figure 1, the framework comprises two synergistic components: interaction and narrative. The interaction component enables active exploration and agency within the virtual environment, while the narrative component provides context, emotional resonance, and scaffolding for reflection. Their combined effect within the immersive medium generates the targeted empathetic response. To apply this framework, the chronic pain simulation was developed iteratively through collaboration between clinicians, technical experts, and individuals with lived chronic pain experience. Interaction employs gaze control, requiring users to focus on objects like a clock, doll, or “ray of hope” for 2 seconds to activate scenes. Interactive elements are subtly indicated by a lighter, subtle glow, distinguishing them from the background. Object placement adheres to ergonomic principles, with most triggers positioned near eye level within a 180-degree frontal plane (±45° vertical variance) to minimize physical strain while supporting discovery through natural head movement. Spatialized audio cues further guide exploration within the 360° environment, collectively supporting the phase of Kolb’s cycle.
To intensify the empathic impact, the experience features an opening sequence beginning from the user’s own perspective. This is followed by a visual transition (e.g., blurred vision, tunnel effect) and narrative audio explicitly signaling the shift into the patient’s viewpoint. This design choice leverages the proven empathic effects of patient-embodied VR identified by Shin and Bertrand et al., moving users beyond passive observation into simulated lived experience to drive deeper cognitive and affective engagement essential for immersive learning (Bertrand et al., 2018; Shin, 2018). As our prototype has progressed, we refined this approach, ultimately settling on narration and effects to indicate the perspective switch.
2.3 VR experience
The 4-minute VR experience aimed to foster empathy for patients with undiagnosed chronic neuropathic pain. By combining immersive storytelling with sensory stimuli, it sought to enhance empathy, immersion, and perspective-taking by simulating the patient’s viewpoint. The objective was to help students adopt a patient’s perspective through sights and sounds designed to represent chronic neuropathic pain, thereby gaining insight into the subjective nature of such conditions. Designed as a complement to traditional teaching methods, the VR experience aimed to help students emotionally connect with abstract clinical concepts and understand the emotional challenges faced by patients.
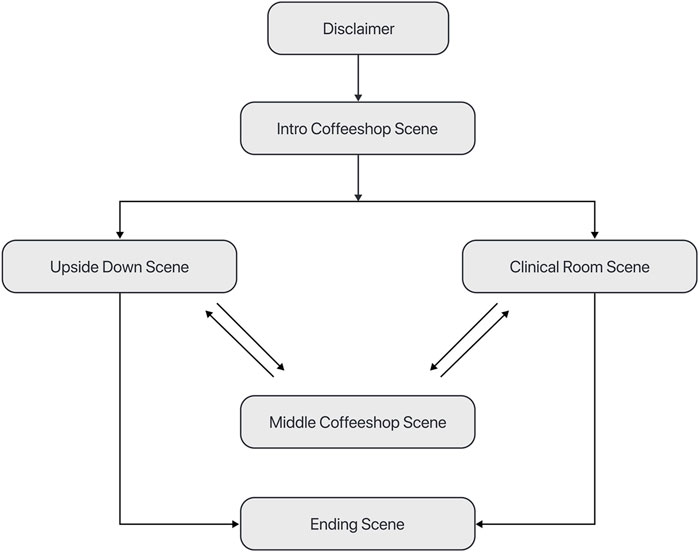
The VR experience comprises six VR scenes (Figure 2): Disclaimer, IntroCoffeeShop, UpsideDown, ClinicalRoom, MiddleCoffeeShop, and EndingScene. Each scene employs targeted sound and visual elements to simulate the emotional and physical toll of chronic pain. The simulation begins with the Disclaimer scene (Figure 3A), displaying the experience logo and a safety disclaimer. Participants then enter the IntroCoffeeShop scene (Figure 3B), a calming 360-degree coffee shop environment where discomfort is introduced through modulatable audio and video effects, such as increasing noise and visual obstructions. These effects escalate over time, but participants can briefly reduce their intensity by focusing on an “Area of Safety” (Figure 3C), represented as a ray of light. This feature provides temporary relief and transitions participants into the UpsideDown (Figures 3D,E) or ClinicalRoom scenes (Figure 3F).
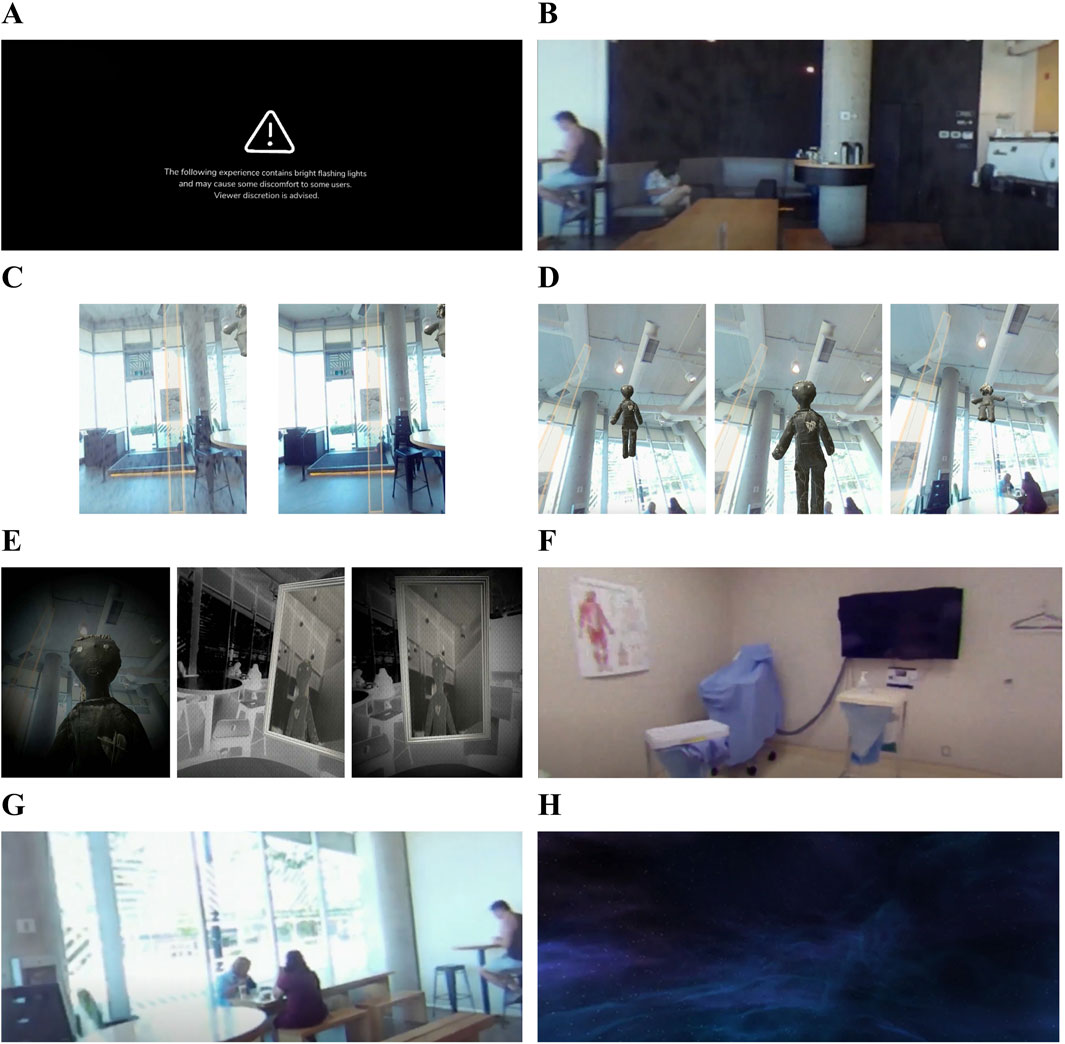
Figure 3. An overview of the VR experience, showcasing various VR scenes and their corresponding visuals. (A) Disclaimer scene. (B) IntroCoffeeShop scene. (C) “Area of Safety”. (D) UpsideDown scene 1. (E) UpsideDown scene 2. (F) ClinicalRoom scene. (G) MiddleCoffeeShop scene. (H) EndingScene.
The UpsideDown scene, a distorted black-and-white inversion of the coffee shop, symbolizes the user’s embodiment of pain. Participants encounter flashing lights, isochronic sounds, and mirrored imagery that reflect their pain through the presence of dolls. The ClinicalRoom scene, on the other hand, recreates the emotional dissonance of being told “everything is normal” despite feeling unwell. Visual distortions such as chromatic aberration, vignette, and warping effects are coupled with unsettling soundscapes, including a never-ending countdown and modulated audio of doctors’ voices. These elements amplify the sensation of discomfort, leaving users in a state of unease. After navigating these intense experiences, participants return to the MiddleCoffeeShop scene (Figure 3G), similar to the introduction but retaining subtle traces of discomfort to maintain continuity. Finally, the EndingScene (Figure 3H) provides a soothing environment, allowing participants to reflect on their journey and the realities of chronic pain. The complete video demonstration can be accessed via the direct link provided for “Supplementary Video”.
2.4 Participants
Seventy undergraduate students from the International School of Guangzhou Huali College, majoring in medical and health professions, were recruited for VR program through open calls (via social media, email, on-site invitations, and an on-campus student association) and were asked to complete a post-experience survey. Participants, aged 19 to 24 (average 22.71 ± 1.32 years), comprised 40% male and 60% female students, with academic years ranging from first to third year. Selection criteria included a healthcare education background and prior clinical experience with chronic pain patients, to align with the VR-based empathy training’s target learner population. Participation was voluntary, and all respondents received detailed information about the study’s procedures, along with assurances regarding the confidentiality of their responses.
2.5 Questionnaires
To evaluate the usability of the VR experience and its effectiveness in evoking empathy, two validated questionnaires were distributed via WJX. Two questionnaires were employed in the present survey to assess the participants’ experiences with and acceptance of the VR experience. The first questionnaire was based on the System Usability Scale (SUS) (Bangor et al., 2008), a well-established instrument for evaluating the usability of various products and services. It consists of 10 questions, each with a 5-point Likert scale ranging from “strongly disagree” to “strongly agree.” Participant scores were combined and then multiplied by 2.5 to convert the original scores (ranging from 0–40) to a new scale (ranging from 0–100). This scale was adopted from previous studies that have validated its use for evaluating technology usability, such as VR systems. This scale was adopted from previous studies that have validated its use for evaluating technology usability, such as VR systems. The SUS has an empirical foundation in usability research, and its widespread use ensures its reliability across different technological contexts.
The second questionnaire was designed to gather user feedback on the application of VR for evoking empathy and studying undiagnosed chronic pain, focusing on areas such as ease of use, immersion, learning effectiveness, and the perceived potential of VR-based education. It was evaluated using Kirkpatrick’s Evaluation Model (Kirkpatrick and Kirkpatrick, 2006), assessing educational outcomes across four levels: reaction (Q8,14,15,16), learning (Q1,2,3,12), behavior (Q5,6,7,13), and results (Q4,9,10,11). The questionnaire was piloted with 10 college students to ensure clarity, resulting in revisions made by senior faculty members at Huali International school to improve question specificity. The final version consisted of 16 items rated on a 5-point Likert scale. The survey measured various outcomes, including emotional engagement, understanding of chronic pain, behavioral changes in clinical practice, and the comparative effectiveness of VR versus traditional learning methods. It also assessed knowledge retention, reflection on clinical efficiency and patient experience, and overall learning enjoyment.
In addition to the quantitative analysis from the questionnaires, qualitative analysis was conducted on open-ended responses, allowing users to offer detailed descriptions of their experiences and providing deeper insights into their perceptions of VR-based learning for chronic pain. Participants were also encouraged to share suggestions for future development and identify any challenges or limitations they encountered. This feedback will play a crucial role in refining the VR application to better meet users’ needs moving forward.
2.6 Data analysis
SPSS 27.0 was used to conduct independent samples t-tests to investigate differences in VR empathy and educational effectiveness-related feedback between medical students with VR experience and those without VR experience or clinical exposure to chronic pain patients. For statistically significant differences (p < 0.05), Cohen’s d values were calculated using the formula |M1 − M2|/SDpooled to quantify the magnitude of differences, where the absolute mean difference was divided by the standard deviation.
3 Results
3.1 Evaluating the usability of VR experience implementation
The SUS questionnaires were completed by the participating medical and health professional students, with the final SUS score serving as a measure of the VR experience’s usability and maturity. A score exceeding 68 is typically regarded as above average, while a score above 80.3 places it within the top 10th percentile. In this study, the mean score was 70.13 ± 7.38, indicating a level of usability that is above average and suggesting that the score provides a reliable reflection of the VR users’ experiences. Table 1 presents the average scores for each item included in the SUS questionnaire.
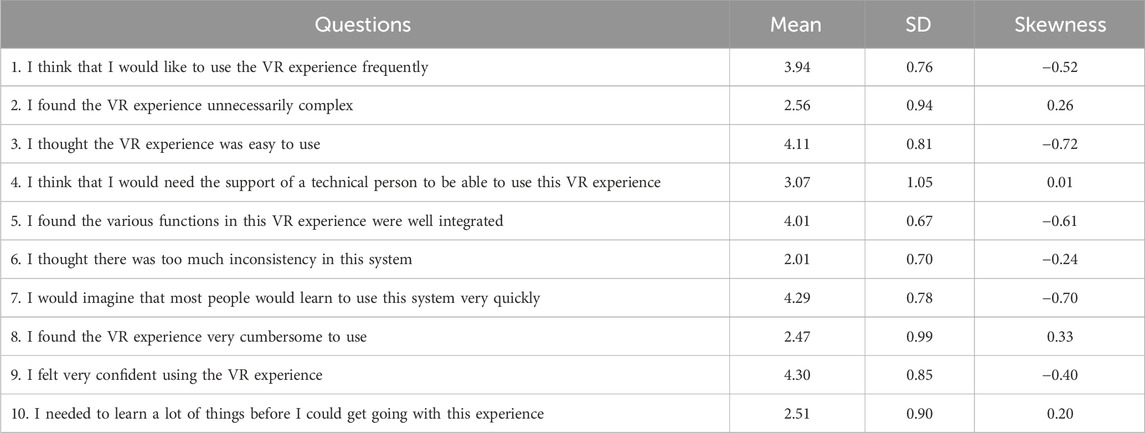
Table 1. The participants’ evaluation of the usability, comfort, and interaction experience of the VR experience.
3.2 The analysis of undiagnosed chronic pain education using VR
We compared the participants’ responses to the questionnaire based on their categorization as VR-experienced (n = 30) and VR-inexperienced groups (n = 40). The statistical analysis revealed significant differences between the two groups on several items, particularly those related to empathy and knowledge retention regarding chronic pain.
The statistical analysis (Table 2) revealed that, for Question 1 “This experience provided me with a genuine understanding of how undiagnosed chronic pain affects patients’ daily activities (e.g., work, social interactions),” the VR-experienced group reported significantly higher ratings (3.97 ± 0.61) compared to the VR-inexperienced group (3.48 ± 0.75), with a statistically significant difference (t = −3.009, p = 0.004, Cohen’s d = 0.706), suggesting that VR exposure enhanced participants’ understanding of chronic pain’s impact on daily life. Similarly, for Question 2 “During the experience, I felt an emotional connection to the narrator’s suffering from undiagnosed chronic pain (e.g., sadness, concern),” the VR-experienced group scored 4.30 ± 0.75 versus the VR-inexperienced group’s 3.70 ± 0.76 (t = −3.293, p = 0.002, Cohen’s d = 0.795), indicating that VR exposure fostered greater emotional empathy. For the statement (Question 8) “I would recommend this VR training to other health professional students as it can foster empathy” the VR-experienced group (2.35 ± 0.53) again reported significantly higher scores than the VR-inexperienced group (1.93 ± 0.74), with t = −2.739, p = 0.008, and Cohen’s d = 0.662, reflecting a stronger endorsement of VR as an empathy-enhancing educational tool. Additionally, in response to Question 12 “The ‘pain externalization’ design was more effective than verbal descriptions in helping me retain related knowledge,” the VR-experienced group scored 3.73 ± 0.94, while the VR-inexperienced group scored 3.20 ± 0.76 (t = −2.621, p = 0.011, Cohen’s d = 0.633), indicating that students perceived VR’s “externalized pain” visualization as more effective in supporting knowledge retention than text-based methods, based on self-reported perceptions. No significant differences were observed between VR-experienced and VR-inexperienced participants in their responses to the remaining questions.
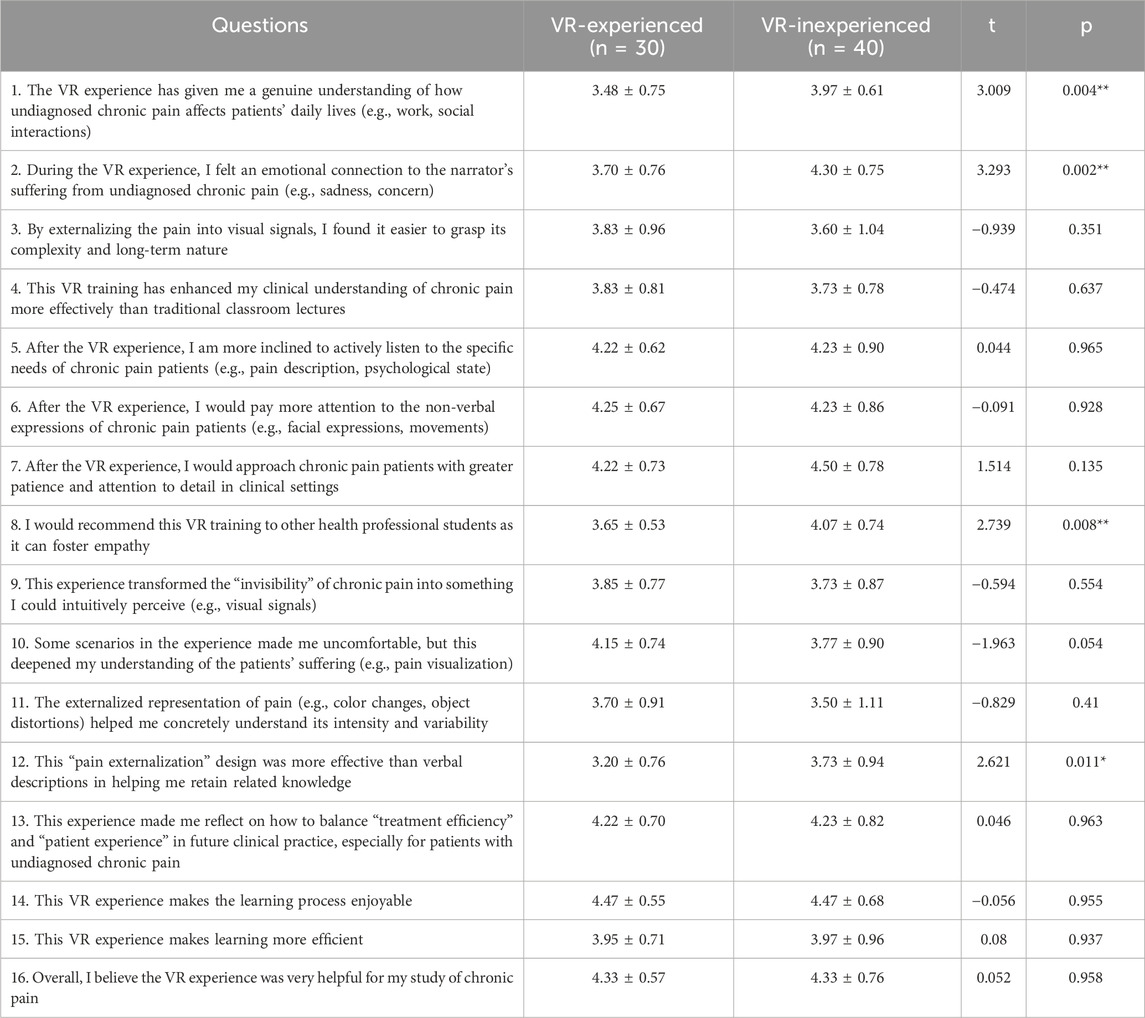
Table 2. The assessment of virtual reality experiences on empathy development and educational outcomes.
4 Discussion
Empathy is a cornerstone of effective healthcare, yet undiagnosed chronic pain, a condition often invisible and misunderstood, poses unique challenges for clinicians and caregivers striving to comprehend its subjective burden. While most VR applications related to pain aim to alleviate patient discomfort, such as during medical procedures or in chronic pain management (Hojat, 2016; Goudman et al., 2022), our study adopts a different perspective. Instead of targeting symptom relief, we utilize VR as an educational tool to foster empathy and enhance understanding among future healthcare professionals.
To evaluate the experience, we first assessed the system’s usability using the System Usability Scale (SUS), a validated measure for user-friendliness and interface quality. Participants reported generally positive usability perceptions, though feedback also highlighted areas for improvement such as initial intuitiveness and physical comfort during use. With regard to the learning experience, we applied Kirkpatrick’s Four-Level Evaluation Model, a well-established framework for analyzing training effectiveness. The results indicate the VR training was perceived more positively by the VR-experienced group (Level 1), with participants in the VR-experienced group expressing high engagement and a greater willingness to recommend the experience as an effective empathy-enhancing tool. At the Learning level (Level 2), these participants also reported a deeper understanding of how undiagnosed chronic pain impacts patients’ daily lives and developed stronger emotional resonance with the narrator’s suffering, reflecting both cognitive and affective learning gains. Behaviorally (Level 3), the VR-experienced group indicated that the training could influence their future clinical approach, particularly in terms of adopting more empathetic practices when treating patients with chronic pain. At the Results level (Level 4), to fully evaluate the impact of the training, it is essential to measure actual improvements in patient care, such as changes in clinical outcomes or the quality of patient interactions, that can be attributed to the empathy and knowledge gained. Without this data, the effectiveness of the training remains uncertain, relying only on the participants’ self-reported perceptions. While demonstrated learning outcomes (Level 2) and behavioral intentions (Level 3) suggest that this VR method may contribute to improved patient-centered care outcomes, such as enhanced patient satisfaction or better pain management, formal evaluation of tangible Level 4 results requires longitudinal measurement of actual clinical performance and patient health metrics, extending beyond the scope of this initial assessment.
Comparative analysis between VR-experienced and inexperienced groups underscored VR’s potential to deepen understanding of chronic pain’s daily impacts and foster emotional resonance with patient narratives. Participants exposed to VR training exhibited stronger endorsement of its value in cultivating empathy and reported enhanced retention of knowledge through visual “pain externalization” compared to conventional methods. These findings emphasize VR’s promise as an empathy-building and knowledge-retention tool while highlighting the need for iterative design improvements to address gaps in engagement and practical application. Future exploration into experiential elements and user-centered adaptations could refine VR’s role in medical education, ensuring alignment with diverse learning needs and educational objectives.
The qualitative analysis was conducted following the COREQ (Consolidated Criteria for Reporting Qualitative Research) guidelines (Tong et al., 2007), which helped ensure a systematic and transparent approach to reporting the open-ended responses from participants. The responses were categorized into two main groups: potential improvement suggestions and reactions to the VR experience.
Participants provided valuable feedback regarding the usability of the interactive elements in the VR experience, documented through COREQ’s standards for comprehensive reporting of participant perspectives. A common challenge identified was the difficulty users faced when navigating scenes without prompts, which could interrupt the narrative flow and limit their exposure to key audiovisual components. To address this issue, participants suggested several enhancements aimed at improving navigation. Notably, the idea of replacing hand tracking with gaze-based navigation was introduced to reduce cognitive load and facilitate a more immersive experience. Additional suggestions included repositioning interactive objects to align with the user’s natural eye-level range, refining the activation timing of interactive elements from 5 s to two, and introducing subtle luminance shifts as visual cues to indicate interactivity while preserving the immersion of the experience. Furthermore, participants highlighted the need for improvements in hardware comfort and interface intuitiveness during initial use, aligning with COREQ’s emphasis on reporting practical participant-driven recommendations to enhance accessibility.
The reactions to the VR experience, as described by participants and reported per COREQ’s criteria for capturing subjective responses. Many participants expressed feelings of discomfort, disturbance, anxiety, and even claustrophobia while using the VR application. These emotional responses reflect the effectiveness of the narrative pacing, symbolic storytelling, and environmental design, all of which contributed to fostering empathy and conveying the emotional realities of living with chronic pain. The intensity of these emotional reactions underscored the success of the VR experience in achieving its intended educational and emotional objectives, while also pointing to areas that could benefit from further refinement.
The initial idea behind the experience was to help students develop empathy for undiagnosed pain that is difficult to understand. Future iterations of the experience could include various pain experiences as “modules” that the user can select or go through. By providing a number of modules for the students to follow, they have the chance to experience a variety of different points of view, and learn to recognize that the experiences of people living with chronic pain can differ vastly. This also increases the replayability of the experience, so that medical students have the chance to develop empathy over a stretch of time, and maintain their interest in the experience and the various patient stories while doing so.
5 Conclusion and limitations
This study demonstrated the potential of VR storytelling to enhance empathy and understanding of undiagnosed chronic pain among healthcare trainees. Participants exposed to the VR experience reported improved comprehension of chronic pain’s daily impacts, stronger emotional resonance with patient narratives, and greater endorsement of VR as an empathy-building tool compared to those without VR exposure. The integration of sensory stimuli, nonlinear storytelling, and perspective-taking mechanisms facilitated a visceral understanding of patients’ subjective experiences, aligning with findings from prior VR healthcare applications. While usability assessments revealed generally positive perceptions of the system’s design, the results underscored VR’s unique capacity to externalize abstract pain concepts and improve knowledge retention, positioning it as a complementary tool in medical education. These findings advocate for the broader adoption of narrative-driven VR interventions to bridge the empathy gap in patient-provider interactions.
This study has strengths but also several limitations. First, the short-term assessment design precludes conclusions about the durability of empathy enhancements or behavioral changes in clinical practice. Second, the current narrative framework focuses on a singular perspective, which may not fully capture the diversity of undiagnosed chronic pain experiences. Future studies should incorporate longitudinal assessments, expanded narrative content reflecting varied patient journeys, and opportunities for users to engage with multiple scenarios to better represent the spectrum of chronic pain challenges.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee at International School (Guangzhou Huali College). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’; legal guardians/next of kin because As the study is educational in nature and involves a VR simulation without the collection of sensitive personal data or any interventions outside of typical educational activities, specific informed consent procedures were not deemed necessary.
Author contributions
WX: Writing – original draft, Writing – review and editing. XY: Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2025.1602957/full#supplementary-material
References
Aylett, R., and Louchart, S. (2003). Towards a narrative theory of virtual reality. Virtual Real. 7, 2–9. doi:10.1007/s10055-003-0114-9
Bangor, A., Kortum, P. T., and Miller, J. T. (2008). An empirical evaluation of the system usability scale. Int. J. Hum.-Comput. Interact. 24 (6), 574–594. doi:10.1080/10447310802205776
Bertrand, P., Guegan, J., Robieux, L., McCall, C. A., and Zenasni, F. (2018). Learning empathy through virtual reality: multiple strategies for training empathy-related abilities using body ownership illusions in embodied virtual reality. Front. Robotics AI 5, 26. doi:10.3389/frobt.2018.00026
Breivik, H., Collett, B., Ventafridda, V., Cohen, R., and Gallacher, D. (2006). Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur. J. Pain 10 (4), 287–333. doi:10.1016/j.ejpain.2005.06.009
Bujić, M., Salminen, M., and Hamari, J. (2023). Effects of immersive media on emotion and memory: an experiment comparing article, 360-video, and virtual reality. Int. J. Human-Computer Stud. 179, 103118. doi:10.1016/j.ijhcs.2023.103118
Conrad, M., Kablitz, D., and Schumann, S. (2024). Learning effectiveness of immersive virtual reality in education and training: a systematic review of findings. Comput. and Educ. X Real. 4, 100053. doi:10.1016/j.cexr.2024.100053
Cummings, J., Tsay-Vogel, M., Cahill, T., and Zhang, L. (2022). Effects of immersive storytelling on affective, cognitive, and associative empathy: the mediating role of presence. New Media and Soc. 24, 2003–2026. doi:10.1177/1461444820986816
Davis, C., et al. (2022). Virtual patients for empathy assessment in medical training: a pilot study, 31 17–18, 2500–2512. doi:10.1111/jocn.16091
Dourou, N., Bruschi, V., Generosi, A., Mengoni, M., and Cecchi, S. (2023). “The effect of immersive audio rendering on Listeners’ emotional state,” in 2023 Immersive and 3D Audio: from Architecture to Automotive (I3DA), Bologna, Italy, 05-07 September 2023, 1–7. doi:10.1109/I3DA57090.2023.10289263
Dutton, S., and Cimino, A. (2021). Impact of virtual reality on healthcare provider empathy for older adults with sensory impairment. Inno. Aging. 5, 759, doi:10.1093/geroni/igab046.2813
Furlan, A. D., Sandoval, J. A., Mailis-Gagnon, A., and Tunks, E. (2006). Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ 174 (11), 1589–1594. doi:10.1503/cmaj.051528
Ghaempanah, F., Moasses Ghafari, B., Hesami, D., Hossein Zadeh, R., Noroozpoor, R., Moodi Ghalibaf, A., et al. (2024). Metaverse and its impact on medical education and health care system: a narrative review. Health Sci. Rep. 7 (9), e70100. doi:10.1002/hsr2.70100
Gilbert, A., Carnell, S., Lok, B., and Miles, A. (2024). Using virtual patients to support empathy training in health care education: an exploratory study. Simul. Healthcare 19 (3), 151–157. doi:10.1097/SIH.0000000000000742
Goudman, L., Jansen, J., Billot, M., Vets, N., De Smedt, A., Roulaud, M., et al. (2022). Virtual reality applications in chronic pain management: systematic review and meta-analysis. JMIR Serious Games 10 (2), e34402. doi:10.2196/34402
Hoffman, H. G., Doctor, J. N., Patterson, D. R., Carrougher, G. J., and Furness, T. A. (2000). Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 85 (1–2), 305–309. doi:10.1016/S0304-3959(99)00275-4
Hojat, M. (2016). Empathy in health professions education and patient care. Springer International Publishing. doi:10.1007/978-3-319-27625-0
Husain, M., and Chalder, T. (2021). Medically unexplained symptoms: assessment and management. Clin. Med. 21 (1), 13–18. doi:10.7861/clinmed.2020-0947
Kalyanaraman, S. S., Penn, D. L., Ivory, J. D., and Judge, A. (2010). The virtual doppelganger: effects of a virtual reality simulator on perceptions of schizophrenia. J. Nerv. Ment. Dis. 198 (6), 437–443. doi:10.1097/NMD.0b013e3181e07d66
Kirkpatrick, D. L., and Kirkpatrick, J. D. (2006). Evaluating training programs: the four levels. 3rd ed. San Francisco, CA, USA: Berrett-Koehler.
Kolb, D. A. (1984). Experiential learning: experience as the source of learning and development. Prentice-Hall.
Lan, X., Tan, Z., Zhou, T., Huang, Z., Huang, Z., Wang, C., et al. (2023). Use of virtual reality in burn rehabilitation: a systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 104 (3), 502–513. doi:10.1016/j.apmr.2022.08.005
Lee, M., and Patel, R. (2023). VR-driven self-management strategies for chronic pain: a longitudinal study, 24 3, 502–515. doi:10.1093/pm/pnac145
Lumley, M. A., Cohen, J. L., Borszcz, G. S., Cano, A., Radcliffe, A. M., Porter, L. S., et al. (2011). Pain and emotion: a biopsychosocial review of recent research. J. Clin. Psychol. 67 (9), 942–968. doi:10.1002/jclp.20816
Moreau, S., Thérond, A., Cerda, I. H., Studer, K., Pan, A., Tharpe, J., et al. (2024). Virtual reality in acute and chronic pain medicine: an updated review. Curr. Pain Headache Rep. 28 (9), 893–928. doi:10.1007/s11916-024-01246-2
Murphy, D., and Pitt, I. (2001). “Spatial sound enhancing virtual story telling,” in Virtual Storytelling: Using Virtual Reality Technologies for Storytelling, International Conference, ICVS 2001, Avignon, France, September 27-28, 2001, 20–29. doi:10.1007/3-540-45420-9_3
Ostrin, G., Frey, J., and Cauchard, J. R. (2018). “Interactive narrative in virtual reality,” in Proceedings of the 17th International Conference on Mobile and Ubiquitous Multimedia (MUM '18), Cairo, Egypt, Nov 25–28, 2018, 463–467. doi:10.1145/3282894.3289740
Parsons, T. D., and Rizzo, A. A. (2008). Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J. Behav. Ther. Exp. Psychiatry 39 (3), 250–261. doi:10.1016/j.jbtep.2007.07.007
Patterson, D. R., Jensen, M. P., Wiechman, S. A., and Sharar, S. R. (2010). Virtual reality hypnosis for pain associated with recovery from physical trauma. Int. J. Clin. Exp. Hypn. 58 (3), 288–300. doi:10.1080/00207141003760595
Riches, S., Iannelli, H., Reynolds, L., Fisher, H. L., Cross, S., and Attoe, C. (2022). Virtual reality-based training for mental health staff: a novel approach to increase empathy, compassion, and subjective understanding of service user experience. Adv. Simul. 7 (1), 19. doi:10.1186/s41077-022-00217-0
Shin, D. (2018). Empathy and embodied experience in virtual environment: to what extent can virtual reality stimulate empathy and embodied experience? Comput. Hum. Behav. 78, 64–73. doi:10.1016/j.chb.2017.09.012
Teh, J., Pascoe, D., Hafeji, S., Parchure, R., Koczoski, A., Rimmer, M., et al. (2024). Efficacy of virtual reality for pain relief in medical procedures: a systematic review and meta-analysis. BMC Med. 22. doi:10.1186/s12916-024-03266-6
Keywords: virtual reality (VR), empathy training, medical education, undiagnosed chronic pain, narrative-driven learning
Citation: Xu W and Yang X (2025) Enhancing empathy of medical students in clinical training: a narrative-driven virtual reality experience for understanding undiagnosed chronic pain. Front. Virtual Real. 6:1602957. doi: 10.3389/frvir.2025.1602957
Received: 30 March 2025; Accepted: 24 July 2025;
Published: 18 September 2025.
Edited by:
Chao Ma, Southeast University, ChinaReviewed by:
Rute F. Meneses, Fernando Pessoa University, PortugalNeeraj Vedi, Parul Institute of Medical Sciences and Research, India
Krista Hoek, Leiden University Medical Center (LUMC), Netherlands
Copyright © 2025 Xu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuesong Yang, eWFuZ194dWVzb25nQDEyNi5jb20=
 Wenjie Xu
Wenjie Xu Xuesong Yang
Xuesong Yang