- 1Institute for Maternal and Child Health, Istituto di Ricovero e Cura a Carattere Scientifico “Burlo Garofolo”, Trieste, Italy
- 2Department of Medical and Surgical Sciences, Institute of Obstetrics and Gynecology, University of Foggia, Foggia, Italy
- 3University Clinical Department of Medical, Surgical and Health Sciences, University of Trieste, Trieste, Italy
Introduction: A high level of surgical ability is required to perform endoscopic knot tying. Barbed sutures help in avoiding this procedure, thus reducing intraoperative time and lowering blood loss and hospitalization time when compared to traditional sutures. Some cases of bowel occlusion following the use of barbed sutures have been described in literature. All of them are characterized by the entanglement of an intestinal loop in wire barbs with bowel occlusion symptoms.
Case Presentation: We report two more cases which occurred in our Institute in 2020 and review those which have been reported in the literature by searching on Pubmed, Scopus, and Embase. We used the search terms: “Barbed,” ”Suture,” “Bowel,” and ”Obstruction.” We examined in the literature the surgical procedures, the type of complications, the time to onset of the complications, and the type of barbed suture.
Discussion: Twenty-two cases in total were reported in the literature from 2011 to 2020, and bowel complications were largely subsequent to interventions such as hernia surgical repair and myomectomy. In order to take advantage of barbed sutures while minimizing the risk of adverse events, such as intestinal occlusion, some precautions may be considered, such as the shortening of thread tails and use of antiadhesive barriers. Moreover, performing a few stitches backwards when ending the suture might be a useful suggestion. Further studies in this field may be useful in order to assess whether it might be better avoiding barbed suture application on serosal tissues to prevent bowel damage.
Introduction
It is well-established that laparoscopic suturing with knot tying requires a substantial level of surgical skills, causing a significant increase in terms of operative time. Moreover, diverse animal studies showed that the knot tension obtained when performed by endoscopic means is lower than that obtained with traditional sutures (1). This fact may lead to an augmented risk of postoperative bleeding, hematomas, and cuff dehiscence (2, 3). After two cases of complications occurred in our hospital, we decided to investigate the pros and the cons of this relatively new type of knotless surgical thread.
Barbed sutures are nowadays widely used both in general surgery and gynecological procedures, and have been in use since the early sixties. Currently, different types of barbed suture are available on the market: Quill™ knotless tissue closure device (Angiotech™, Vancouver, BC, Canada), V-loc™ by Covidien™ (Covidien™, Mansfield, MA, USA), and Stratafix™ by Ethicon™ (Ethicon™, Cincinnati, OH, USA). All of them present barbs oriented in the opposite direction of the needle, which do not allow the suture to slide back (4).
The objective of this study is to provide an objective overview of the complications which may occur following the use of barbed sutures, considering all the benefits and disadvantages of this kind of wire. In the conclusion, some suggestions which may help avoiding adverse events are described.
Case Description
Case 1
In January 2020 a 32-year-old woman was admitted to the emergency room with nausea, vomiting, constipation, and abdominal pain. The woman underwent laparoscopic myomectomy 7 weeks before and had a history of multiple admissions to the emergency room for the same symptoms. Every time she had medical treatment, no pathologic clinical findings were diagnosed after clinical evaluation, ultrasonography, blood test, and X-rays. Meglumine diatrizoate (Gastrografin™) was administered to pursue bowel disobstruction, with no resolution of the symptomatology.
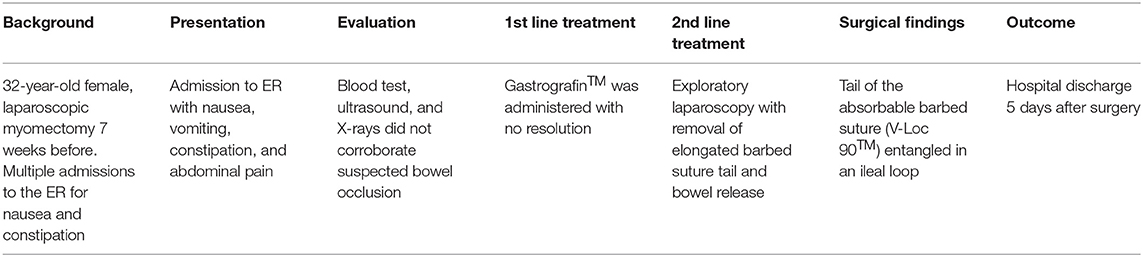
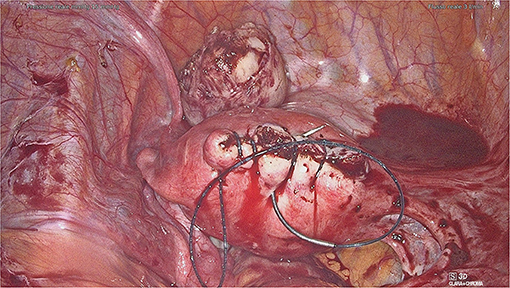
Considering the symptoms and the previous history of the woman, the decision was made to perform an urgent diagnostic laparoscopy. The scenario was the following: a tail of the absorbable barbed suture (V-Loc 90™ filament by Covidien™) which had been used to suture the uterine wound after the hysterotomy was entangled in an ileal loop, hence causing a subocclusion of the patient's small intestine. In addition to that, another V-Loc™ tail was entangled in the mesum close to the ileocecal valve (Figure 1). The filaments were promptly removed, and no resection of the small intestine was needed as the normal vascularization of the ansae was rapidly restored. The woman was discharged from the hospital 5 days after the surgery in good general condition. At the 6-month follow-up evaluation, no complications were reported (Table 1).
Case 2
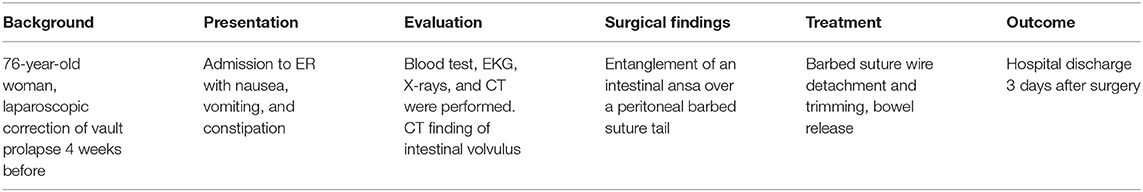
At the end of the month of January 2020, a 76-year-old woman underwent surgery for vault prolapse. The surgeons' intention was to perform laparoscopic colposacropexy, but due to the intraoperative finding of a bone callus over the sacrum which had not been diagnosed before, colposacropexy could not be accomplished. Since the peritoneum covering the sacral bone had already been dissected, its closure was performed by the use of V-Loc 90 absorbable barbed suture. A laparoscopic lateral suspension was then achieved in order to treat the patient's prolapse. After 4 weeks the woman was admitted to the ER for bowel occlusion symptoms. Blood tests, electrocardiogram, X-rays, and CT were performed. A radiologic finding of intestinal volvulus emerged. Due to the poor clinical condition, a mini-laparotomy was then performed, and an entanglement of an intestinal ansa over the barbed suture tail was observed. Barbed suture wire detachment and trimming was carried out. The procedure was completed with volvulus untwisting and adhesiolysis. No bowel resection was needed. The woman was then discharged 3 days after the procedure. At the 6-month follow-up evaluation, no complications were reported (Table 2).
Discussion
A review of the literature was performed by searching on Pubmed, Scopus, and Embase. We used the search terms: “Barbed,” ”Suture,” “Bowel,” and ”Obstruction.” We examined in the literature the surgical procedures, the type of complications, the time to onset of the complications, and the type of barbed suture. English only articles were included. The two patients involved in our manuscript signed their informed consent for the use of their data. The present study was designed according to the Helsinki declaration ethical principles. This retrospective observational descriptive study was approved by our Institutional Review Board (IRB-Burlo RC 08/2020).
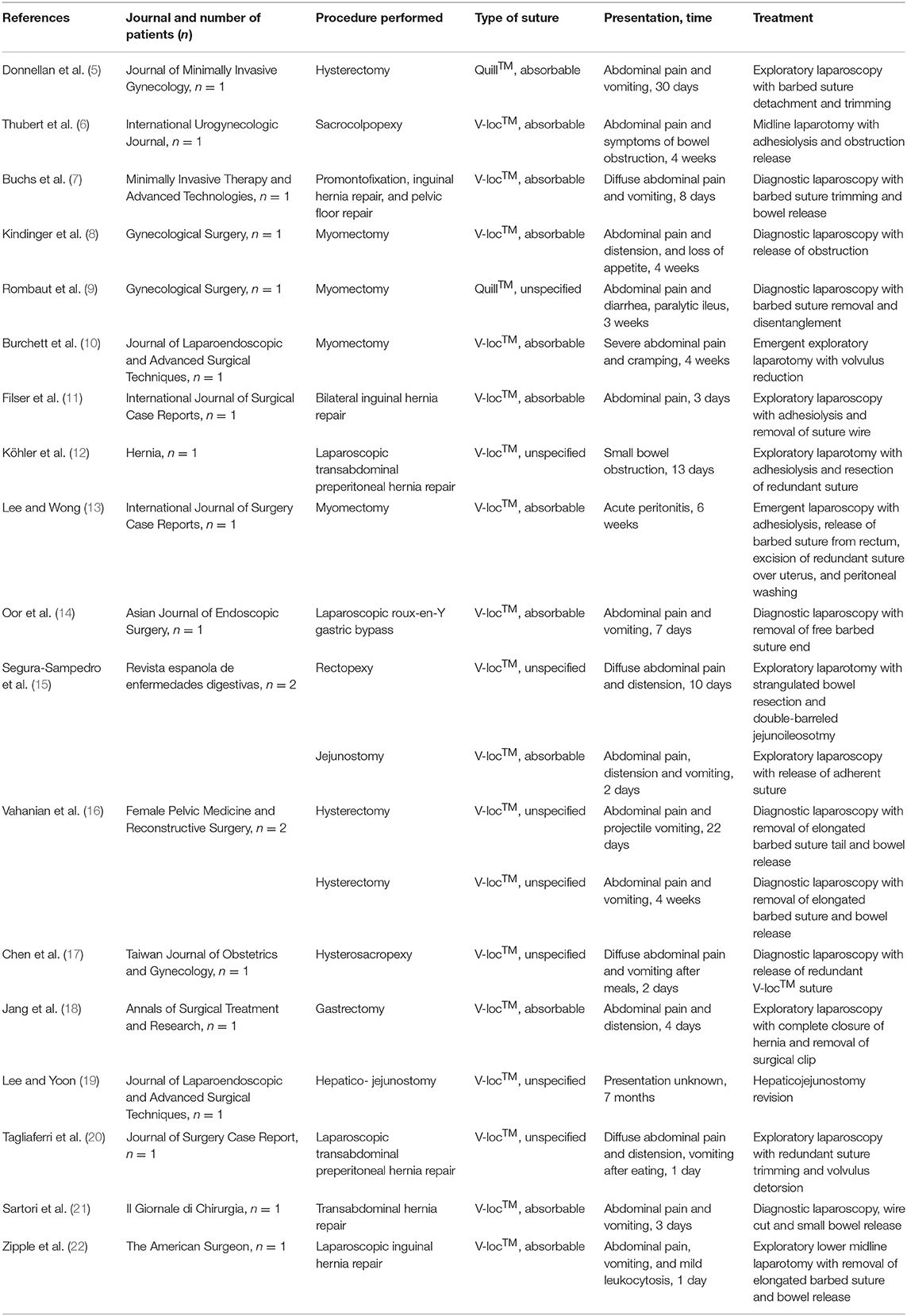
Twenty cases of bowel occlusion have been described in the literature, from 2011 to 2020 (Table 3). The majority of them occurred following hernia surgical repair (30%, n = 6), alone or combined with other surgical techniques. After that, myomectomy (20%, n = 4) represents the second most frequent surgery causing this complication. Other less common causes are hysterectomy or sacrocolpopexy (15% each). Mean presentation time was 25 days (ranging from 1 to 210 days). Symptoms most commonly reported were abdominal pain, nausea, and vomiting. Less reported conditions were diarrhea and peritonitis. In 75% of cases (n = 15), resolution was achieved by laparoscopic ansae disentanglement; the remaining 15% (n = 5) underwent laparotomic surgery.
Due to the development of mini-invasive surgery in the last decade (23), barbed sutures' usage during surgical procedures is becoming more and more common, thus allowing young surgeons to avoid knot tying which represents one of the most difficult surgical steps. A range of studies have been conducted to assess whether the barbed suture is better than the traditional one in abdominal and pelvic surgery (24). In minimally invasive laparoscopic surgeries, the ability to quickly and properly tie surgical knots has presented a new challenge. In cases in which knot tying is difficult, the use of knotless barbed sutures can securely reapproximate tissues with less time, cost, and aggravation (25). Zhang et al. (26) in 2016 highlighted that barbed wires have the ability to reduce operative time both in laparoscopic myomectomy and mini-laparotomic myomectomy. In a 2020 meta-analysis (27), Wiggins et al. found that the use of barbed sutures for gastrointestinal anastomosis appears to be associated with shorter overall operative times, and no difference in rates of complications (including anastomotic leak, bleeding, or stricture) emerged when compared with standard suture materials. The suturing time decrease is attributable to multiple reasons, such as there being no need to tie knots nor to keep tension in the suture, due to the wire self-anchoring intrinsic feature (suture resists to migration) (28). Moreover, barbed sutures reduce total operative time and total amount of intraoperative blood loss when compared with traditional sutures (29). As proven by multiple studies, these observations are valid not only for gynecological procedures, but for other surgical areas too. Another characteristic of barbed sutures is the ability to maintain an equal distribution of tensile strength along the suture (28), which may be responsible for the avoidance of intramural hematomas formation. These, together with lowering the blood loss, may explain the reduction of post-operative patient's hemoglobin drop that has been observed (30). Surgery technical complexity is reduced too, as it is widely believed that laparoscopic sutures are one of the most difficult and time-consuming tasks during endoscopic surgery (29, 30). Finally, perioperative complications such as nosocomial infections or organic stressed events are diminished, as well as hospital stay; shorter hospitalization positively affects patients' physical and emotional quality of life, and may reduce hospital assistance costs too (31, 32).
Despite all the previously mentioned benefits, barbed suture-related complications must be carefully considered. The risk of bowel obstruction or intestinal volvulus is a significant downside to barbed suturing. A potential explanation of the occurrence of this kind of adverse event is the entanglement of barbed wires tails between intestinal ansae or mesa. Cutting barbed filament tails short enough may contribute to lessening this risk (33–35). Suture peritonization may not represent a valid solution since it does not avoid adhesion formation, as demonstrated by Api et al. in rats (36). The cases we reported in this study are the 21st and 22nd described in the literature by the time this article was written. These are the only two cases out of more than 400 surgeries accomplished in our Institute in which barbed sutures have been used (overall complication risk: 0.5%). Focusing just on gynecological procedures, our cases are part of fewer than 15 cases of bowel obstruction ever described following the usage of barbed sutures. This must be related to the fact that barbed sutures are increasingly executed in the gynecological field due to their ease of use and their efficacy in preventing hematoma formation and blood loss. As shown in Table 3, most of the cases of intestinal occlusion following the use of barbed sutures occurred after laparoscopic myomectomy (Table 3). This fact may be due to the close contact of intestinal loops with the barbed wires on the uterine wound. Other less common cases occurred after hysterectomy, and were related to entanglement of barbed sutures on the vaginal vault with the ansae. Furthermore, intestinal occlusion may happen following sacrocolpopexy, with adhesion formation between the ansae or mesum, and those wire barbs which protrude from the peritoneal suture. The cases we described belong to these categories.
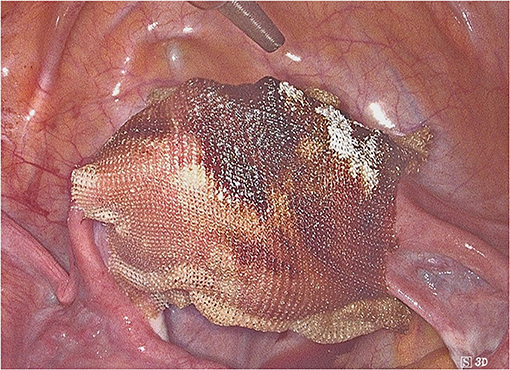
After a careful analysis of our cases and those reported in the literature, we propose to perform a second non-barbed suture above the barbed one in order to minimize complication risk. The closure of the uterine breach after myomectomy might be the procedure of choice when applying this precaution, as it often requires the execution of several suturing layers. This procedure may ensure a better tissue hemostasis and may reduce suture thread exposure too (Supplementary Video 1). Unfortunately, our suggestion partly decreases barbed suture advantages in terms of operating time. Moreover, on some occasions it might not be possible to perform a double layer suture, especially on serosa or peritoneum. Hence, if this expedient cannot be accomplished, adhesion barriers may be placed to avoid direct bowel contact with the barbed suture (Figure 2). Another trick that might help the surgeon to avoid excessive tail exposure is performing a few stitches backwards when ending the suture. Tissue shrinkage may lead to an overexposure of the barbed suture, and this must be kept in mind, especially when the suture is performed on myometrium after myomectomy. Tightening the suture by one or more backwards passages might avoid these problems too (Figure 3, Supplementary Video 2).
The weakness of our study is that is based largely on case reports, which do not provide solid solutions to barbed suture disadvantages. It is clear that more studies need to be done in order to understand how barbed sutures can be safely used, enjoying their benefits while minimizing the risk of complications.
Barbed sutures are an efficient device to minimize operative time, blood loss, and hospitalization time, which is of course related to the patient's recovery time. It is also an important aid for young surgeons with less experience in endoscopic surgery and laparoscopic knot tying (29). However, complications must be avoided. We summarized some precautions a good surgeon should consider when using barbed sutures: (1) performing one or two backwards stitches when ending the suture, in order to minimize the risk of suture slippage; (2) trying to use barbed sutures for intra-organ knots only (i.e., for deeper myometrial layers); (3) preferring absorbable non-barbed wires for serosal layers; (4) shortening thread free tails, especially when the suture is performed on myometrium after myomectomy (due to tissue shrinkage); and (5) applying long-lasting adhesion barrier devices when external barbed suture is inevitable. Development of long-lasting adhesion barriers may be a valid prospect for improving barbed suturing. More studies need to be done to understand how the use of this device can be optimized in surgical procedures.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of IRCCS BURLO GAROFOLO (RC 08/2020) approved this retrospective observational descriptive study. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the relevant individual(s), and/or minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article. All patients signed an informed consent form before treatment. Permission for the publication was taken in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Author Contributions
GS, FR, DD, and GR: conceptualization. GS, FC, DD, and FR: methodology. FC: software. FS and LN: validation. GS, FC, and FS: formal analysis. GS, FR, and FS: investigation. FC, GS, DD, and LN: data curation. GS and FC: writing original draft preparation. GR, FR, LN, and FS: writing, review, and editing. GR and LN: supervision. GR, LN, and GS: project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This retrospective observational descriptive study was approved by our Institutional Review Board (IRB-Burlo RC 08/2020). The research was supported by a grant from the Institute for Maternal and Child Health IRCCS Burlo Garofolo (RC 08/2020).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.626505/full#supplementary-material
Abbreviations
ER, emergency room; EKG, electrocardiogram; CT, computed tomography.
References
1. López CC, Ríos JFDL, González Y, Vásquez-Trespalacios EM, Serna D, Arango A, et al. Barbed suture versus conventional suture for vaginal cuff closure in total laparoscopic hysterectomy: randomized controlled clinical trial. J Minim Invasive Gynecol. (2019) 26:1104–9. doi: 10.1016/j.jmig.2018.08.030
2. Jeung IC, Baek JM, Park EK, Lee HN, Kim CJ, Park TC, et al. A prospective comparison of vaginal stump suturing techniques during total laparoscopic hysterectomy. Arch Gynecol Obstet. (2010) 282:631–8. doi: 10.1007/s00404-009-1300-0
3. Uccella S, Malzoni M, Cromi A, Seracchioli R, Ciravolo G, Fanfani F, et al. Laparoscopic vs transvaginal cuff closure after total laparoscopic hysterectomy: a randomized trial by the Italian Society of Gynecologic Endoscopy. Am J Obstet Gynecol. (2018) 218:500.e1–13. doi: 10.1016/j.ajog.2018.01.029
4. Lin Y, Lai S, Huang J, Du L. The efficacy and safety of knotless barbed sutures in the surgical field: a systematic review and meta-analysis of randomized controlled trials. Sci Rep. (2016) 6:23425. doi: 10.1038/srep23425
5. Donnellan NM, Mansuria SM. Small bowel obstruction resulting from laparoscopic vaginal cuff closure with a barbed suture. J Minim Invasive Gynecol. (2011) 18:528–30. doi: 10.1016/j.jmig.2011.03.011
6. Thubert T, Pourcher G, Deffieux X. Small bowel volvulus following peritoneal closure using absorbable knotless device during laparoscopic sacral colpopexy. Int Urogynecol J. (2011) 22:761–3. doi: 10.1007/s00192-010-1348-1
7. Buchs NC, Ostermann S, Hauser J, Roche B, Iselin CE, MoreL P. Intestinal obstruction following use of laparoscopic barbed suture: a new complication with new material? Minim Invasive Ther Allied Technol. (2012) 21:369–71. doi: 10.3109/13645706.2011.638643
8. Kindinger LM, Setchell TE, Miskry TS. Bowel obstruction due to entanglement with unidirectional barbed suture following laparoscopic myomectomy. Gynecol Surg. (2012) 9:357–8. doi: 10.1007/s10397-012-0733-9
9. Rombaut S, Baulies S, Cusidó M, Barri-Soldevila P, Rodriguez I, Úbeda A. Quill barbed suture-related complication. Gynecol Surg. (2012) 9:359–61. doi: 10.1007/s10397-012-0749-1
10. Burchett MA, Mattar SG, McKenna DT. Iatrogenic intestinal and mesenteric injuries with small bowel volvulus following use of barbed suture during laparoscopic myomectomy. J Laparoendosc Adv Surg Tech. (2013) 23:632–4. doi: 10.1089/lap.2013.0065
11. Filser J, Reibetanz J, Krajinovic K, Germer C-T, Dietz UA, Seyfried F. Small bowel volvulus after transabdominal preperitoneal hernia repair due to improper use of V-LocTM barbed absorbable wire – do we always “read the instructions first”? Int J Surg Case Rep. (2015) 8:193–5. doi: 10.1016/j.ijscr.2015.02.020
12. Köhler G, Mayer F, Lechner M, Bittner R. Small bowel obstruction after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report and review of the literature. Hernia. (2015) 19:389–94. doi: 10.1007/s10029-014-1301-1
13. Lee ETC, Wong FWS. Small bowel obstruction from barbed suture following laparoscopic myomectomy—a case report. Int J Surg Case Rep. (2015) 16:146–9. doi: 10.1016/j.ijscr.2015.09.039
14. Oor J, de Castro S, van Wagensveld B. V-locTM capable of grasping surrounding tissue causes obstruction at the jejunojejunostomy after Roux-en-Y laparoscopic gastric bypass. Asian J Endosc Surg. (2015) 8:209–11. doi: 10.1111/ases.12169
15. Segura-Sampedro JJ, Ashrafian H, Navarro-Sánchez A, Jenkins JT, Morales-Conde S, Martínez-Isla A. Small bowel obstruction due to laparoscopic barbed sutures: an unknown complication? Rev Española Enfermedades Dig. (2015) 107:677–80. doi: 10.17235/reed.2015.3863/2015
16. Vahanian SA, Finamore PS, Lazarou G. Delayed small bowel obstruction after robotic-assisted sacrocolpopexy. Female Pelvic Med Reconstr Surg. (2015) 21:e11–3. doi: 10.1097/SPV.0000000000000101
17. Chen H, Hong M-K, Ding D-C. Acute small bowel obstruction caused by barbed suture on the second day after laparoscopic hysterosacropexy: a case report and literature review. Taiwan J Obstet Gynecol. (2017) 56:247–9. doi: 10.1016/j.tjog.2016.03.008
18. Jang SH, Jung YK, Choi SJ, Ha TK. Postoperative mechanical small bowel obstruction induced by V-Loc barbed absorbable suture after laparoscopic distal gastrectomy. Ann Surg Treat Res. (2017) 92:380. doi: 10.4174/astr.2017.92.5.380
19. Lee JS, Yoon YC. Laparoscopic treatment of choledochal cyst using barbed sutures. J Laparoendosc Adv Surg Tech. (2017) 27:58–62. doi: 10.1089/lap.2016.0022
20. Tagliaferri EM, Wong Tavara SL, Abad de Jesus JL, Bergmann H, Hammans S, Seidlmayer CM. Small bowel obstruction SBO after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report. J Surg Case Rep. (2018) 2018:rjy165. doi: 10.1093/jscr/rjy165
21. Sartori A, De Luca M, Clemente N, De Luca A, Scaffidi G, Piatto G, et al. Small bowel occlusion after trans-abdominal preperitoneal hernia approach caused by barbed suture: case report and review of literature. G Chir. (2019) 40:322–4.
22. Zipple MK, Bankhead-Kendall B, Roy MD, Yaldo B. Small bowel obstruction secondary to barbed suture after minimally invasive inguinal hernia repair. Am Surg. (2020). doi: 10.1177/000313482008600108
23. Romano F, Rizzo M, Stabile G, Di Lorenzo G, Liguori G, Trombetta C, et al. Laparoscopic and laparotomic guided ureteral stenting during gynecological surgery without use of imaging: safety and feasibility in a single institutional case series. Eur J Obstet Gynecol Reprod Biol. (2020) 251:125–8. doi: 10.1016/j.ejogrb.2020.05.032
24. Lin Y, Long Y, Lai S, Zhang Y, Guo Q, Huang J, et al. The Effectiveness and safety of barbed sutures in the bariatric surgery: a systematic review and meta-analysis. Obes Surg. (2019) 29:1756–64. doi: 10.1007/s11695-019-03744-4
25. Greenberg JA, Goldman HR. Barbed suture: a review of the technology and clinical uses in obstetrics and gynecology. Rev Obstet Gynecol. (2013) 6:107–15.
26. Zhang Y, Ma D, Li X, Zhang Q. Role of barbed sutures in repairing uterine wall defects in laparoscopic myomectomy: a systemic review and meta-analysis. J Minim Invasive Gynecol. (2016) 23:684–91. doi: 10.1016/j.jmig.2016.03.008
27. Wiggins T, Majid MS, Markar SR, Loy J, Agrawal S, Koak Y. Benefits of barbed suture utilisation in gastrointestinal anastomosis: a systematic review and meta-analysis. Ann R Coll Surg Engl. (2020) 102:153–9. doi: 10.1308/rcsann.2019.0106
28. Alessandri F, Remorgida V, Venturini PL, Ferrero S. Unidirectional barbed suture versus continuous suture with intracorporeal knots in laparoscopic myomectomy: a randomized study. J Minim Invasive Gynecol. (2010) 17:725–9. doi: 10.1016/j.jmig.2010.06.007
29. Song T, Kim TJ, Kim WY, Lee SH. Comparison of barbed suture versus traditional suture in laparoendoscopic single-site myomectomy. Eur J Obstet Gynecol Reprod Biol. (2015) 185:99–102. doi: 10.1016/j.ejogrb.2014.11.022
30. Angioli R, Plotti F, Montera R, Damiani P, Terranova C, Oronzi I, et al. A new type of absorbable barbed suture for use in laparoscopic myomectomy. Int J Gynecol Obstet. (2012) 117:220–3. doi: 10.1016/j.ijgo.2011.12.023
31. Soto E, Flyckt R, Falcone T. Minimally invasive myomectomy using unidirectional knotless barbed suture. J Minim Invasive Gynecol. (2014) 21:27. doi: 10.1016/j.jmig.2013.09.007
32. Gardella B, Dominoni M, Iacobone AD, De Silvestri A, Tinelli C, Bogliolo S, et al. What is the role of barbed suture in laparoscopic myomectomy? A meta-analysis and pregnancy outcome evaluation. Gynecol Obstet Invest. (2018) 83:521–32. doi: 10.1159/000488241
33. Stabile G, Zinicola G, Romano F, Buonomo F, Mangino FP, Ricci G. Management of non-tubal ectopic pregnancies: a single center experience. Diagnostics. (2020) 10:652. doi: 10.3390/diagnostics10090652
34. Tulandi T, Einarsson JI. The use of barbed suture for laparoscopic hysterectomy and myomectomy: a systematic review and meta-analysis. J Minim Invasive Gynecol. (2014) 21:210–6. doi: 10.1016/j.jmig.2013.09.014
35. Giampaolino P, De Rosa N, Tommaselli GA, Santangelo F, Nappi C, Sansone A, et al. Comparison of bidirectional barbed suture Stratafix and conventional suture with intracorporeal knots in laparoscopic myomectomy by office transvaginal hydrolaparoscopic follow-up: a preliminary report. Eur J Obstet Gynecol Reprod Biol. (2015) 195:146–50. doi: 10.1016/j.ejogrb.2015.10.011
Keywords: barbed suture, bowel occlusion, laparoscopy, hernia surgical repair, myomectomy
Citation: Stabile G, Romano F, De Santo D, Sorrentino F, Nappi L, Cracco F and Ricci G (2021) Case Report: Bowel Occlusion Following the Use of Barbed Sutures in Abdominal Surgery. A Single-Center Experience and Literature Review. Front. Surg. 8:626505. doi: 10.3389/fsurg.2021.626505
Received: 06 November 2020; Accepted: 11 March 2021;
Published: 20 April 2021.
Edited by:
Shingo Tsujinaka, Jichi Medical University Saitama Medical Center, JapanReviewed by:
Yifei Lin, Sichuan University, ChinaStefano Restaino, Ospedale Santa Maria della Misericordia di Udine, Italy
Copyright © 2021 Stabile, Romano, De Santo, Sorrentino, Nappi, Cracco and Ricci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guglielmo Stabile, Z3VnbGllbG1vc3RAZ21haWwuY29t
 Guglielmo Stabile
Guglielmo Stabile Federico Romano
Federico Romano Davide De Santo1
Davide De Santo1 Felice Sorrentino
Felice Sorrentino Giuseppe Ricci
Giuseppe Ricci