- 1Department of Orthopedics, The First Affiliated Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
- 2The School of Clinical Medicine, Fujian Medical University, Fuzhou, China
- 3Department of Orthopaedics, Faculty of Medicine, Chulalongkorn University, and King Chulalongkorn Memorial Hospital, Bangkok, Thailand
- 4Center of Excellence in Biomechanics and Innovative Spine Surgery, Chulalongkorn University, Bangkok, Thailand
- 5Division of Neurosurgery, Department of Surgery, Changhua Christian Hospital, Changhua, Taiwan
- 6Department of Leisure Industry Management, National Chin-Yi University of Technology, Taichung, Taiwan
- 7Department of Neurosurgery, The First Affiliated Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
Objective: Oblique lumbar interbody fusion (OLIF) and transforaminal lumbar interbody fusion (TLIF) are widely used in the treatment of lumbar degenerative diseases. A meta-analysis was performed to examine the clinical and radiological effects of these two techniques.
Methods: A search of relevant literature from several databases was conducted until November 2021. Perioperative outcomes, clinical and radiological results, and complications were analyzed.
Results: Fifteen qualified studies were included. OLIF showed a shorter operative time and length of hospital stay and less blood loss than TLIF. Early postoperative Visual Analogue Scale for back pain were significantly lower in OLIF than in TLIF (P = 0.004). Noteworthy, although the preoperative Oswestry Disability Index (ODI) of the OLIF group was higher than that of the TLIF group (P = 0.04), the postoperative ODI was significantly lower (P < 0.05). Radiologically, the results showed that the disc and foraminal heights of OLIF were significantly higher than those of TLIF postoperatively. Moreover, OLIF can restore more segmental lordosis than TLIF in the early postoperative period. Furthermore, OLIF showed better fusion rates than TLIF (P = 0.02), with no difference in cage subsidence (13.4% vs. 16.6%). No significant differences in overall and approach-related complications between the two groups.
Conclusion: The OLIF group showed an advantage in terms of operative time, hospitalization, intraoperative blood loss, early back pain relief, postoperative function recovery, disc and foraminal heights, early segmental lordosis, and fusion rate compared to TLIF. For both procedures, the incidence rates of overall and approach-related complications were comparable.
Introduction
Lumbar degenerative disease (LDD) is a common spinal condition that causes discomfort and difficulty walking as a result of aberrant motion or compression of neural structures (1). Patients with long-term low back and leg pain that has a detrimental effect on their quality of life and for whom conservative treatment has proven futile might consider surgery (2, 3). Posterolateral lumbar interbody fusion, represented by transforaminal lumbar interbody fusion (TLIF), has long been widely used for the treatment of various LDDs (4). However, TLIF, including minimally invasive TLIF (MI-TLIF), not only requires intraoperative stripping of the paravertebral muscles but also results in complications, such as fusion collapse, nerve damage, cerebrospinal fluid leakage, and postoperative paravertebral muscle atrophy due to denervation, which affect the patient's postoperative quality of life (5).
Recently, as surgical techniques have evolved toward precision and minimal invasiveness, many new interbody fusion procedures have emerged for the treatment of LDD, such as oblique lumbar interbody fusion (OLIF). OLIF, first proposed by Silvestre et al. (6) in 2012, involves reaching the lumbar interbody space through the corridor between the retroperitoneal abdominal vascular sheath and major psoas muscle, and multi-segment fusion can be accomplished through the same anatomic space, reducing soft tissue injury (7, 8). Compared with TLIF, OLIF is less invasive, preserves the posterior column bony stable structures of the spine, and reduces soft tissue injury, while restoring the coronal and sagittal balance of the spine more easily (9, 10). However, because of more neurovascular and complex structures within the anterior lateral lumbar spine surgery, postoperative lumbar sympathetic trunk injury, femoral nerve injury, and segmental artery injury can occur, and the surgical technique is also more demanding (11). TLIF is more familiar to the surgeon than OLIF. It uses a single posterior approach to the lumbar spine, which prevents damage to the anterior vascular nerves, allows direct decompression, and corrects lumbar scoliosis by implantation of intervertebral fusion and osteotomy, so it is still used by many surgeons. Overall, both surgical approaches have their advantages and shortcomings.
However, because of the differences in surgical approach and fusion technique between TLIF and OLIF, it is still unclear whether surgery has superior results. Several studies have also directly compared TLIF and OLIF, but their results lack consistency and convincing evidence. In this regard, we performed a meta-analysis to compare the clinical outcomes and radiological results of TLIF and OLIF and provide the surgeon with an evidence-based reference.
Materials and methods
Search strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) criteria were used to conduct a systematic literature review (12). We searched for randomized controlled trials (RCTs) and nonrandomized cohort studies that compared TLIF and OLIF for LDD. Relevant English-language papers were retrieved from PubMed, Web of Science, Embase, and the Cochrane Library from database inception to November 2021. The following keywords were used in the search: “oblique lumbar interbody fusion” OR “pre-psoas approach spinal fusion” OR “anterior to psoas approach spinal fusion” OR “OLIF” AND “transforaminal lumbar interbody fusion” OR “TLIF.” We also found pertinent papers from references to help with our search. The titles and abstracts of all search results were evaluated separately by two researchers (G.X.L. and C.M.C.). Then, the relevance of these studies, whose material appeared to be relevant, was evaluated. Discussions with a third party (B.S.H.) were used to settle any disagreements.
Inclusion and exclusion criteria
The included studies satisfied the following criteria: (1) all relevant clinical original studies, (2) articles comparing OLIF and TLIF for LDD, (3) studies reporting clinical or radiological assessment measures, (4) studies exhibiting a mean follow-up period of >6 months, and (5) studies published in the English language. The exclusion criteria were as follows: (1) single-arm studies without comparison groups, (2) studies without relevant data, and (3) case reports, technical notes, and review articles.
Quality evaluation
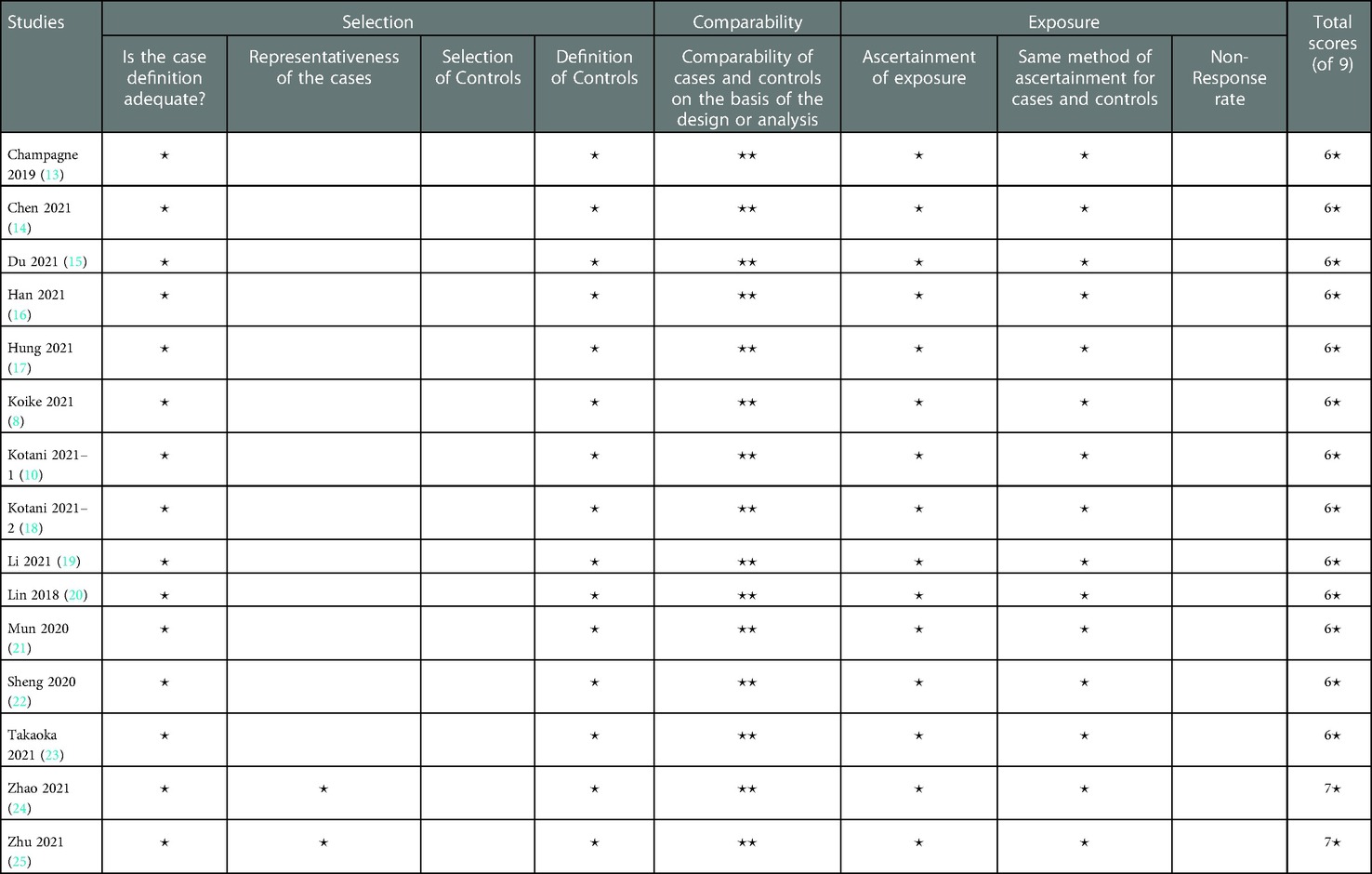
Two reviewers independently assessed the quality of each study included in this meta-analysis (G.X.L. and C.M.C.). To assess the quality of non-RCTs, the Newcastle–Ottawa Scale (NOS) was utilized. Each study was assessed in terms of selection, comparability, and exposure/outcome. Our review included studies that received more than five “stars” using these criteria.
Data extraction
Two reviewers (G.X.L. and C.M.C.) collected data independently using conventional data extraction procedures. The general characteristics derived from each study were as follows: authors, year, study design, country, number of cases, operative level, surgical intervention details, and age, sex, and a follow-up period of patients. The primary outcomes were clinical and radiological outcomes. Clinical outcomes included Visual Analogue Scale (VAS) scores for back and leg pain and Oswestry Disability Index (ODI) scores, both of which were measured preoperatively and postoperatively. Radiological outcomes included disc height (DH), disc angle, foraminal height (FH), segmental lordotic angle (SLA), lumbar lordosis (LL), cage subsidence, adjacent segment disease (ASD), and fusion state. The secondary outcomes were perioperative parameters (operative time, estimated blood loss, and length of hospital stay) and complications.
Statistical analysis
The data were analyzed using RevMan version 5.4 (Cochrane Collaboration, Oxford, UK Continuous data were presented as mean differences and 95% confidence intervals (CI). In comparative studies, dichotomous variables were assessed using odds ratios (ORs) or risk ratios. Weighted mean differences (WMD) or standard mean differences (SMD) were used to evaluate continuous variables. To examine heterogeneity, the x2 and I2 tests were performed, with P > 0.1 or I2 < 50% being homogeneous among studies, and a fixed-effects model was applied. In contrast, if I2 was >50%, a random-effects model was used. A P-value < 0.05 was used to determine statistical significance. Forest plots were built to graphically show the findings of numerous studies and pooled impact estimates.
Results
Study results and quality assessment
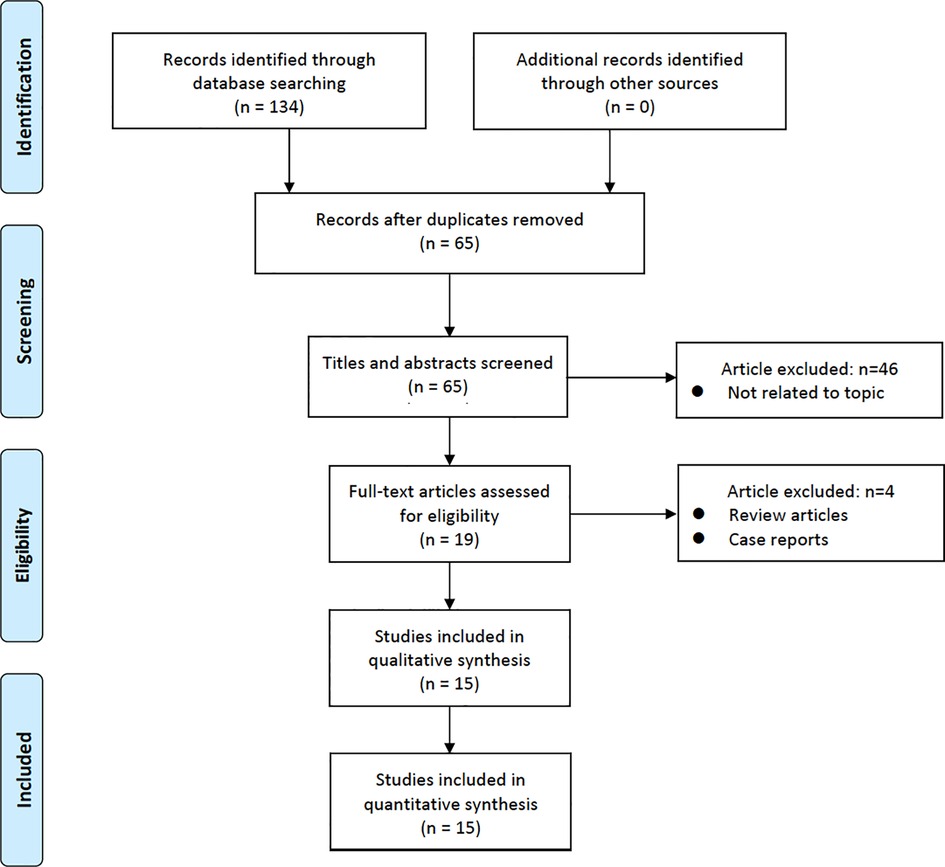
Overall, 134 studies were identified. After screening the titles and abstracts, 69 papers were discarded. The remaining 65 studies were extensively investigated, and 15 studies that met the inclusion criteria were included in the analysis. The PRISMA flowchart (Figure 1) depicts the entire search algorithm.
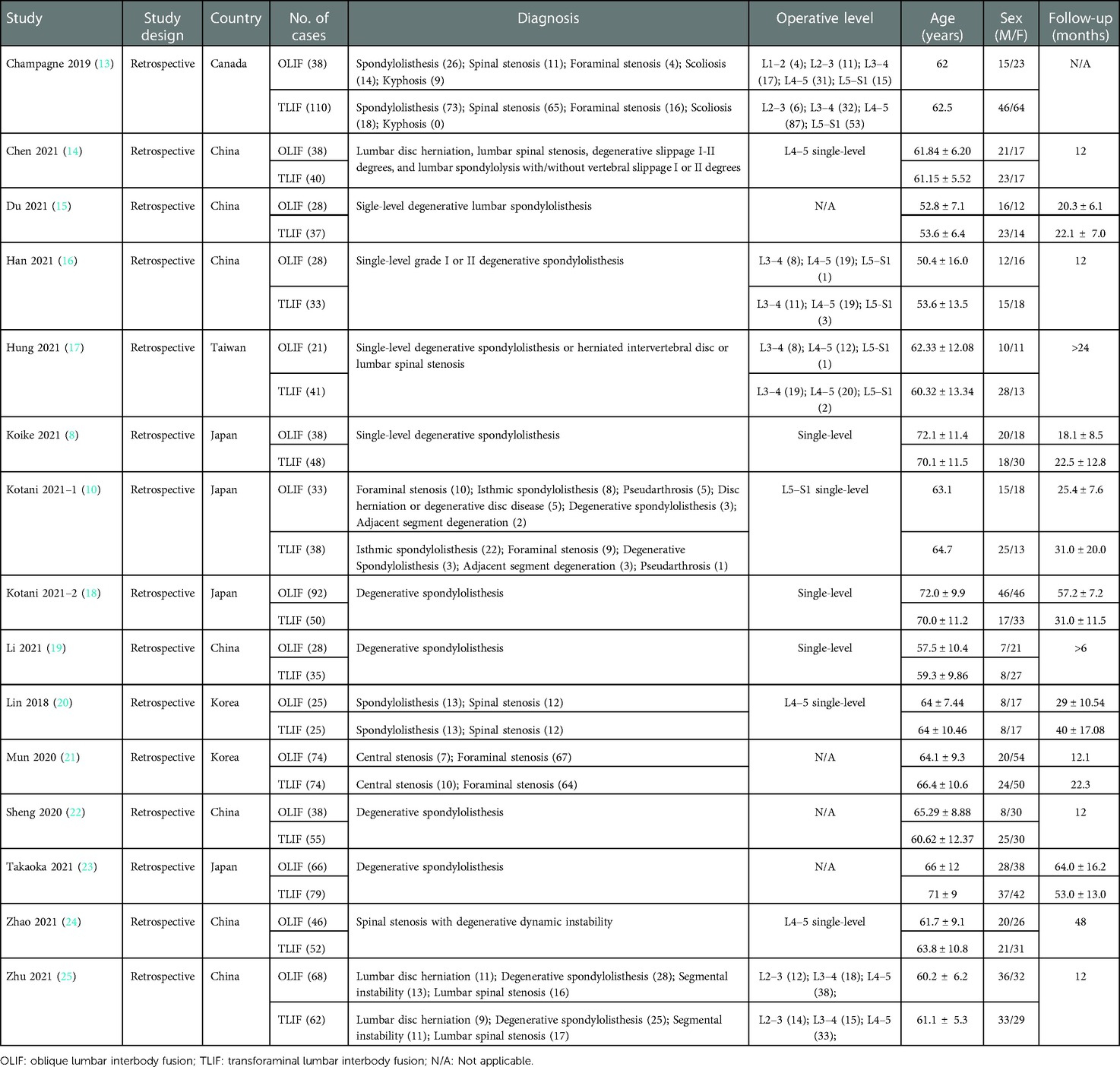
A total of 1,440 patients were enrolled in the 15 studies, with 661 and 779 patients recruited in the OLIF and TLIF groups, respectively. Seven studies were conducted in China, four in Japan, two in Korea, one in Taiwan, and one from Canada. The segment most frequently subject to surgery was the L4–L5. Table 1 summarizes the demographic data.
All 15 studies had retrospective comparative cohort design and were of moderate to high quality, according to our NOS rating (Table 2).
Clinical outcomes
Eleven included studies provided VAS scores for back pain.There was no significant difference between the OLIF and TLIF groups in VAS scores for back pain preoperatively (SMD, 0.00; 95% CI, −0.27, 0.28; I2 = 80%; P = 0.97; Figure 2A) and final follow-up postoperatively (SMD, −0.32; 95% CI, −0.84, 0.21; I2 = 91%; P = 0.24; Figure 2C). Noteworthy, early postoperative (3 months) VAS scores for back pain were significantly lower in the OLIF group than in the TLIF group (SMD, −0.65; 95% CI, −1.09, −0.21; I2 = 77%; P = 0.004; Figure 2B).
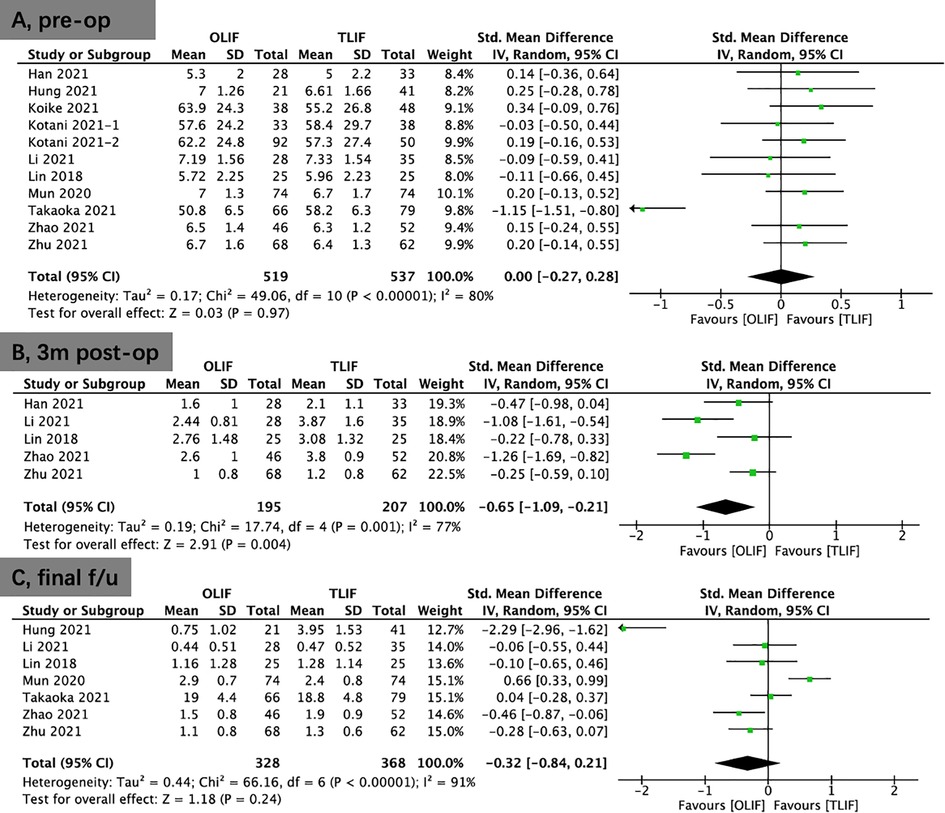
Figure 2. Forest plots for comparison of VAS for back at preoperative (A), early (3 months) postoperative (B), and final follow-up (C) between OLIF and TLIF. VAS, visual analog scale; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Moreover, 11 included studies provided VAS scores for leg pain. There was no significant difference in these scores between the OLIF and TLIF groups preoperatively (SMD, 0.02; 95% CI, −0.16, 0.21; I2 = 54%; P = 0.79; Figure 3A), early postoperatively (3 months) (SMD, 0.19; 95% CI, −0.02, 0.41; I2 = 0%; P = 0.08; Figure 3B), and at the final follow-up (SMD, 0.18; 95% CI, −0.53, 0.90; I2 = 95%; P = 0.61; Figure 3C).
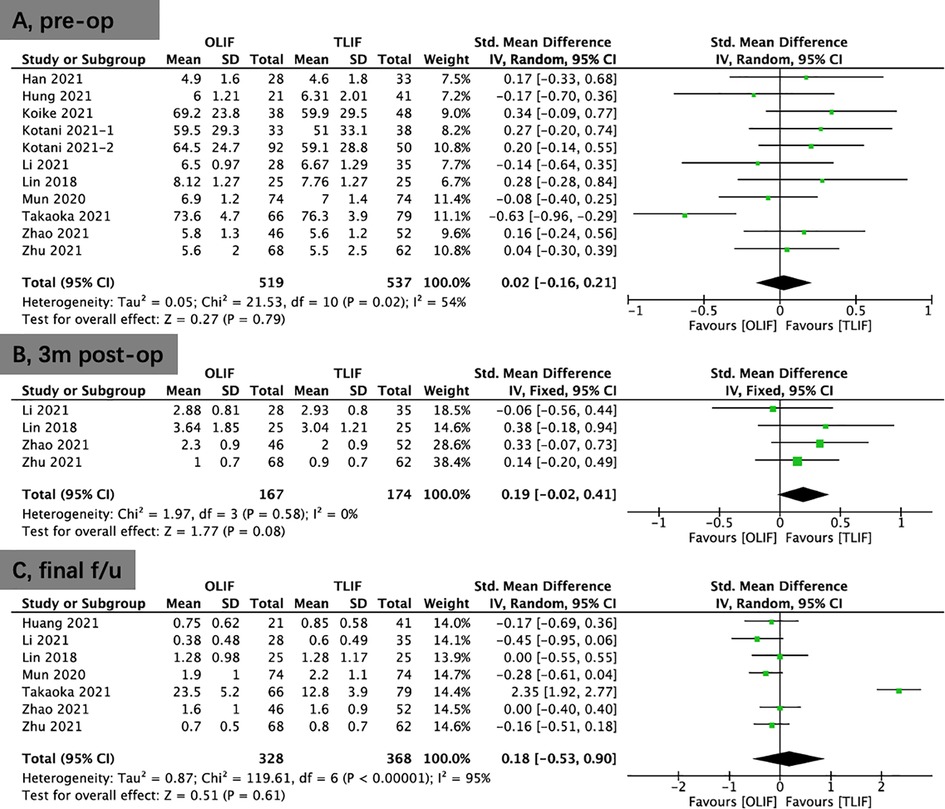
Figure 3. Forest plots for comparison of VAS for leg at preoperative (A), early (3 months) postoperative (B), and final follow-up (C) between OLIF and TLIF. VAS, visual analog scale; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Eight studies provided ODI scores. There were higher preoperative ODI scores in the OLIF group than in the TLIF group (WMD, 1.11; 95% CI, 0.03, 2.19; I2 = 20%; P = 0.04; Figure 4A). The results showed that significantly improvement in the OLIF group than in the TLIF group at 3 months postoperatively (WMD, −3.14; 95% CI, −6.19, −0.08; I2 = 90%; P = 0.04; Figure 4B) and the final follow-up (WMD: −2.35; 95% CI: −4.47, −0.22; I2 = 92%; P = 0.03; Figure 4C).
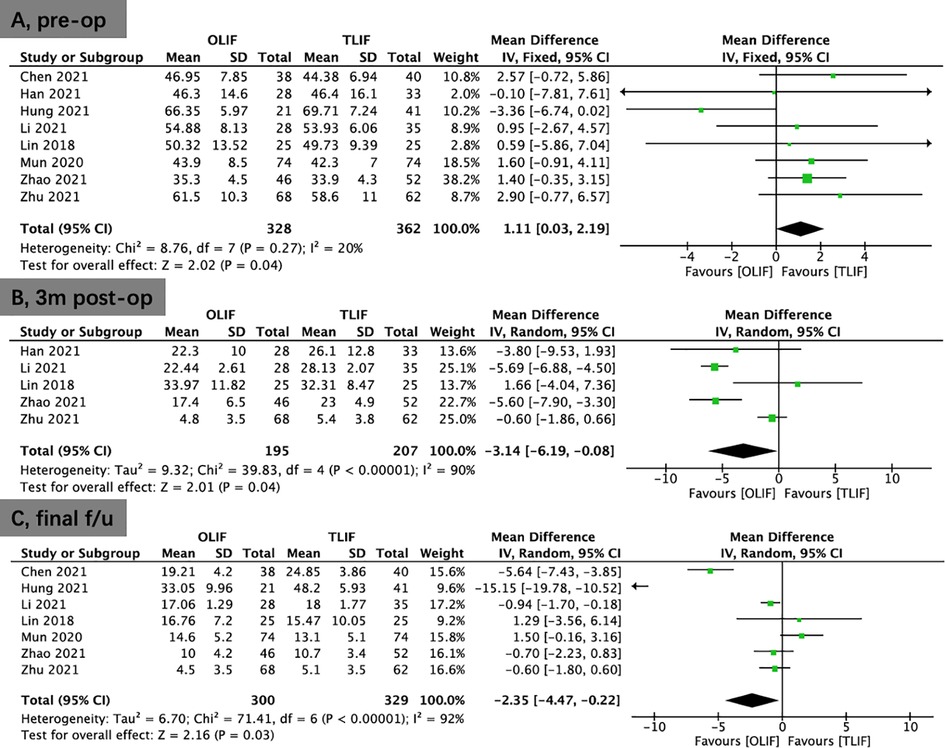
Figure 4. Forest plots for comparison of ODI at preoperative (A), early (3 months) postoperative (B), and final follow-up (C) between OLIF and TLIF. ODI, oswestry disability index; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Radiological parameters
Seven studies reported the DH. No significant difference was shown between the OLIF and TLIF groups preoperatively (WMD, −0.01; 95% CI, −0.38, 0.35; I2 = 44%; P = 0.94; Figure 5A). A pooled study revealed that OLIF resulted in greater DH restitution in the early postoperative period (<1 week; WMD, 1.50; 95% CI, 0.83, 2.17; I2 = 81%; P < 0.0001; Figure 5B) and the final follow-up compared to TLIF (WMD, 1.71; 95% CI, 0.94, 2.47; I2 = 88%; P < 0.0001; Figure 5C).
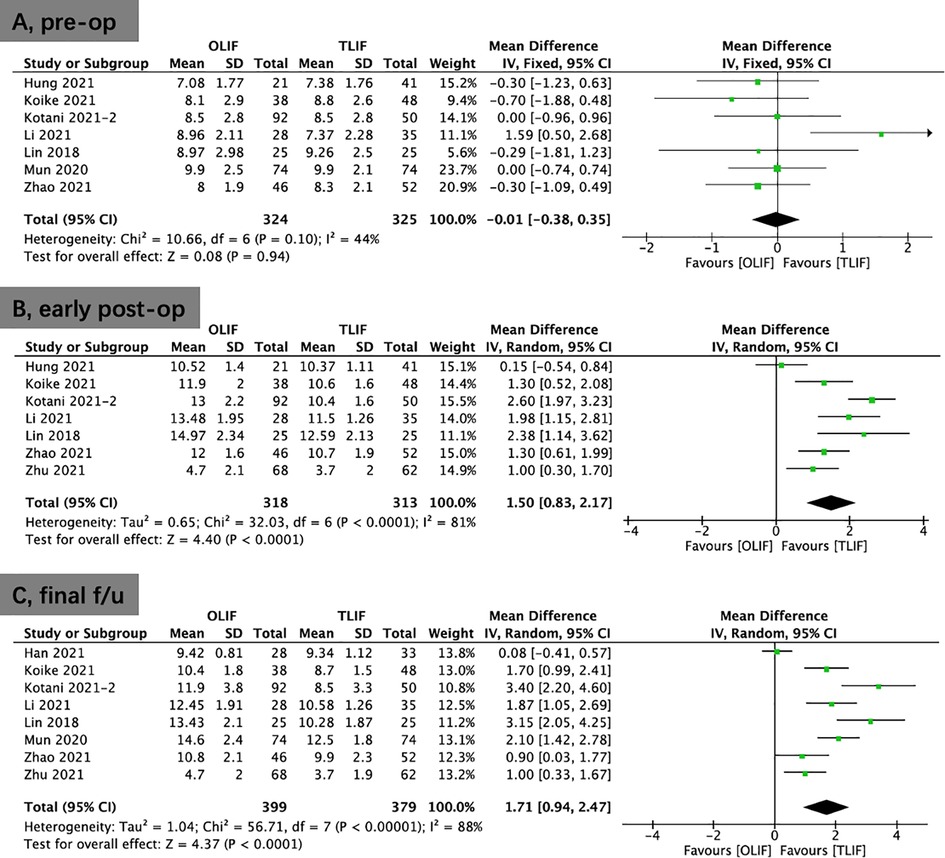
Figure 5. Forest plots for comparison of DH at preoperative (A), early (<1 week) postoperative (B), and final follow-up (C) between OLIF and TLIF. DH, disc height; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Two studies provided the disc angle. No significant difference was shown between the two groups at the preoperative (WMD, 0.03; 95% CI, −1.22, 1.27; I2 = 3%; P = 0.97; Supplementary Figure S1A) and postoperative (WMD, 5.50; 95% CI, −3.91, 14.91; I2 = 99%; P = 0.25; Supplementary Figure S1B) periods.
Four studies provided data on FH. No significant difference was shown between the OLIF and TLIF groups in FH preoperatively (WMD, −0.17; 95% CI, −0.72, 0.39; I2 = 6%; P = 0.56; Figure 6A). Compared to TLIF, the data demonstrated that OLIF might considerably increase FH postoperatively (WMD, 1.67; 95% CI, 0.64, 2.70; I2 = 70%; P = 0.002; Figure 6B).
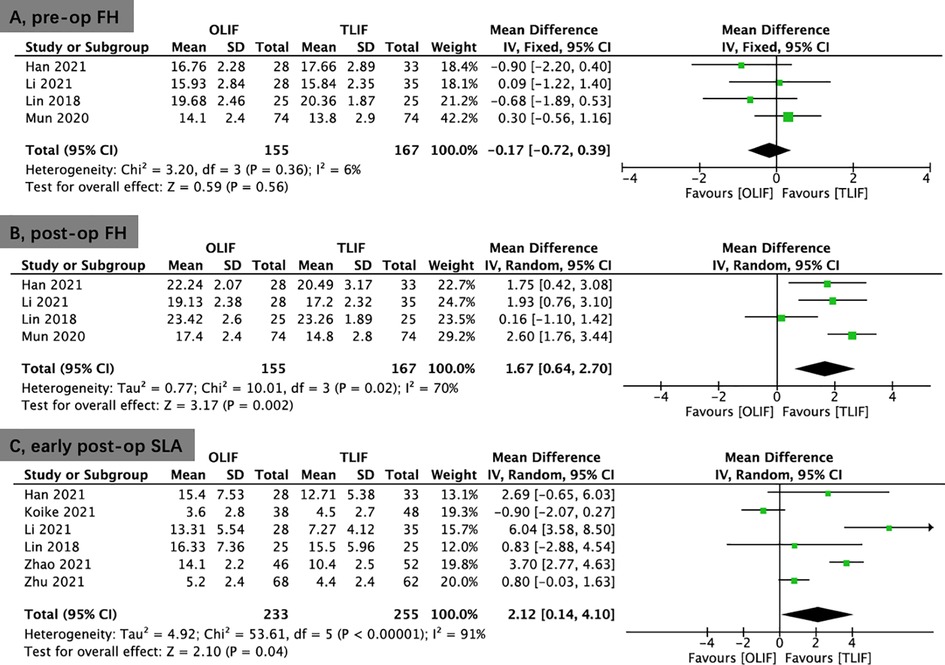
Figure 6. Forest plots for comparison of FH at preoperative (A), and postoperative (B) between OLIF and TLIF. (C), Forest plots for comparison of SLA at early postoperative (<1 week) between OLIF and TLIF. FH, foraminal height; SLA, segmental lordotic angle; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Six studies reported the SLA. No significant differences was shown in SLA preoperatively (WMD, −0.45; 95% CI, −1.85, 0.95; I2 = 66%; P = 0.53; Supplementary Figure S2A) and at the final follow-up (WMD, 1.93; 95% CI, −0.22, 4.08; I2 = 93%; P = 0.08; Supplementary Figure S2C) between the OLIF and TLIF groups. However, there was better early postoperative (<1 week) SLA in the OLIF group than in the TLIF group (WMD, 2.12; 95% CI, 0.14, 4.10; I2 = 91%; P = 0.04; Figure 6C).
Five studies provided data on LL. No significant differences was shown in LL preoperatively (WMD, −0.52; 95% CI, −2.77, 1.73; I2 = 0%; P = 0.65; Supplementary Figure S3A), early postoperatively (<1 week; WMD, 2.60; 95% CI, −0.88, 6.09; I2 = 79%; P = 0.14; Supplementary Figure S3B), and at the final follow-up (WMD, 2.07; 95% CI, −1.87, 6.01; I2 = 84%; P = 0.30; Supplementary Figure S3C) between the OLIF and TLIF groups.
The fusion rate was reported in 11 studies. The results showed better fusion rate in the OLIF group (86.2%) compared with that in the TLIF group (79.6%) at the final follow-up (OR, 1.66; 95% CI, 1.08, 2.56; I2 = 0%; P = 0.02; Figure 7A).
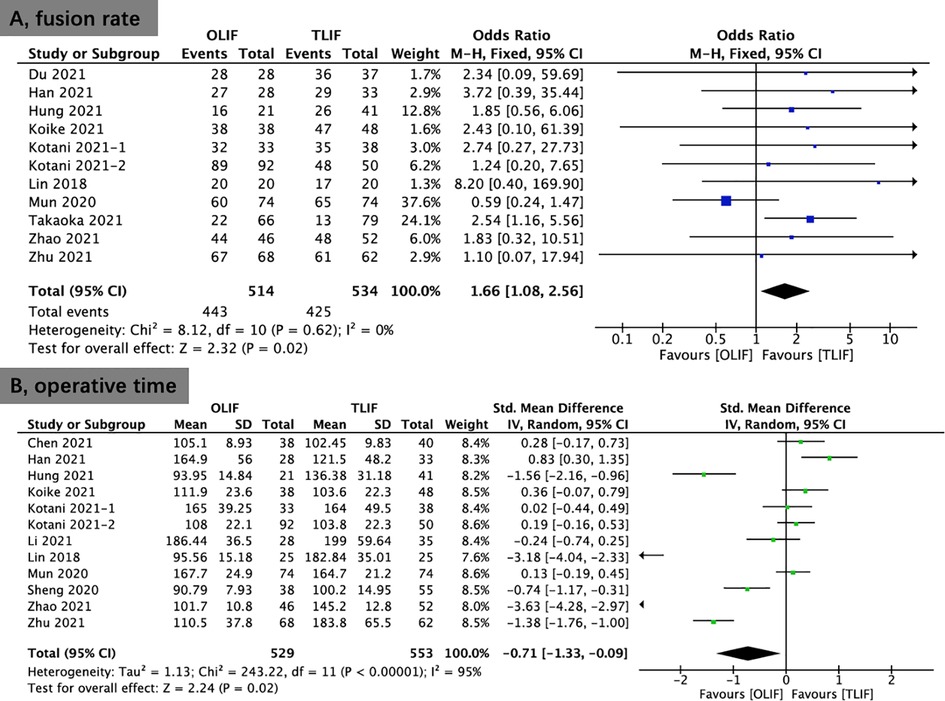
Figure 7. Forest plots comparing fusion rate (A) and operative time (B) between OLIF and TLIF. OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Perioperative outcomes
Twelve studies provided data on operative time. The operative time of the OLIF group was significantly shorter than that of the TLIF group (SMD, −0.71; 95% CI, −1.33, −0.09; I2 = 95%; P = 0.02; Figure 7B).
Eleven studies provided data on estimated intraoperative blood loss. The estimated intraoperative blood loss of the OLIF group was less than that of the TLIF group (WMD, −119.24; 95% CI, −189.05, −49.44; I2 = 99%; P = 0.0008; Figure 8A).
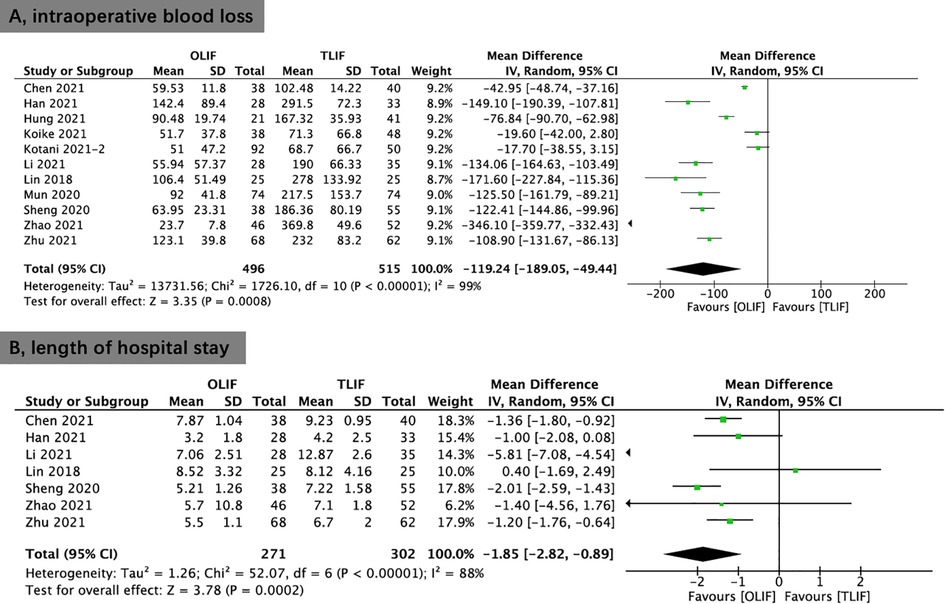
Figure 8. Forest plots comparing intraoperative blood loss (A) and length of hospital stay (B) between OLIF and TLIF. OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Seven studies provided data on the length of hospital stay. The length of hospital stay in the OLIF was substantially shorter than that of the TLIF group (WMD, −1.85; 95% CI, −2.82, −0.89; I2 = 88%; P = 0.0002; Figure 8B).
Incidence of complications
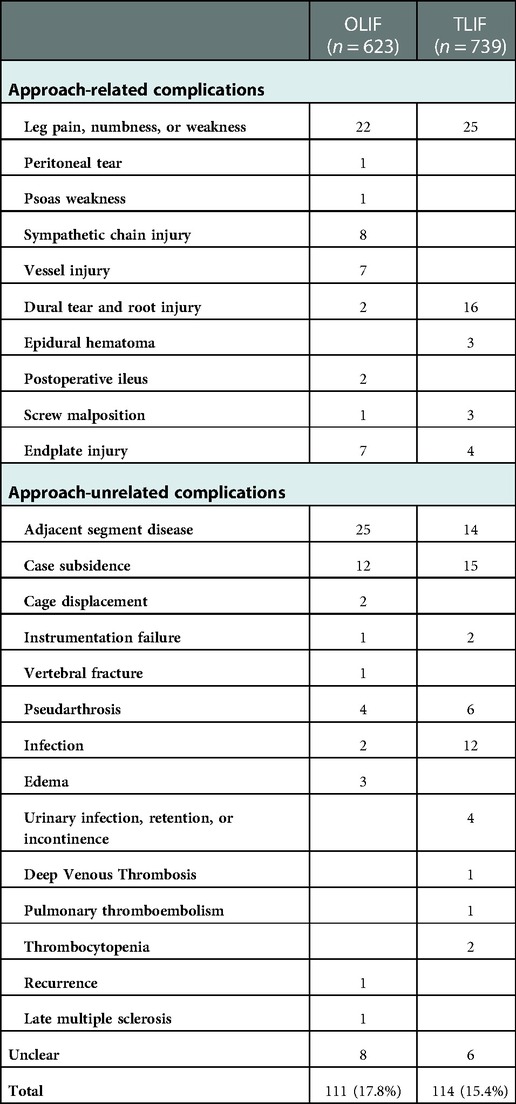
Fourteen studies reported data on complications. There were no statistically significant differences in the development of complications between OLIF and TLIF (OR, 1.26; 95% CI, 0.94, 1.70; I2 = 16%; P = 0.13; Figure 9A). Table 3 shows the details of the complications reported in the included studies. Similarly, no remarkable variations in the approach-related complications between OLIF and TLIF (OR, 1.35; 95% CI, 0.88, 2.06; I2 = 6%; P = 0.17; Figure 9B).
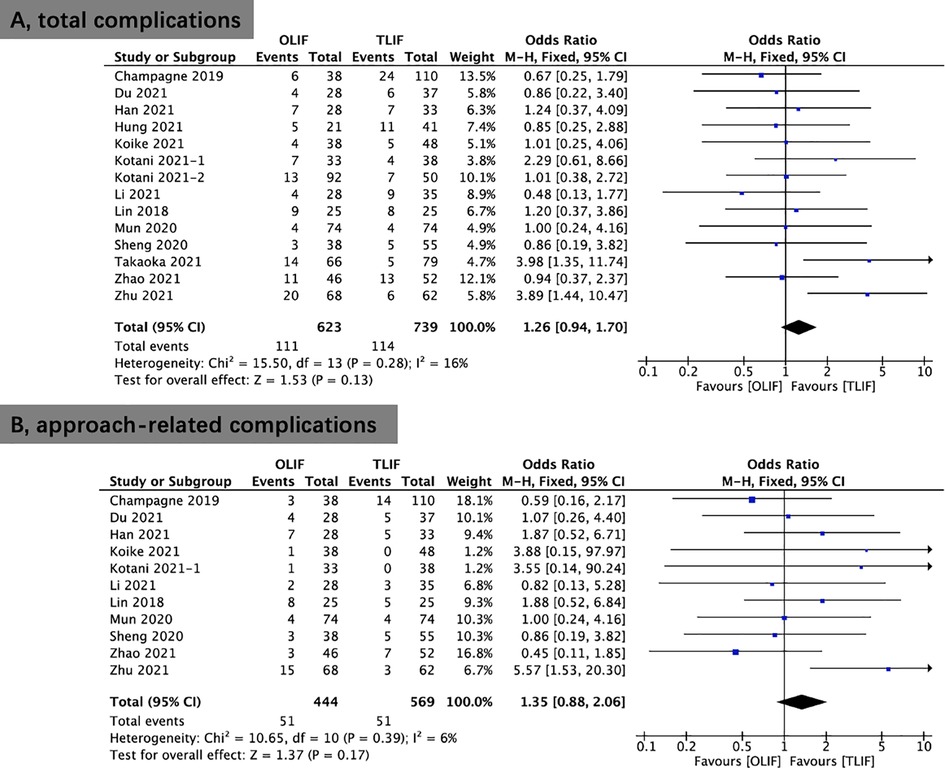
Figure 9. Forest plots comparing total complications (A) and approach-related complications (B) between OLIF and TLIF. OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Six studies provided data on cage subsidence. No significant differences was shown in cage subsidence (OR, 0.81; 95% CI, 0.49, 1.31; I2 = 19%; P = 0.39; Figure 10A) between the OLIF and TLIF groups. Five studies provided data on ASD. No significant differences was shown in ASD (OR, 1.69; 95% CI, 0.93, 3.09; I2 = 19%; P = 0.09; Figure 10B) between the OLIF and TLIF groups. Moreover, eight studies reported data on infection. The results revealed no significant differences in infection (OR, 0.47; 95% CI, 0.16, 1.35; I2 = 0%; P = 0.16; Figure 1C) between the OLIF and TLIF groups.
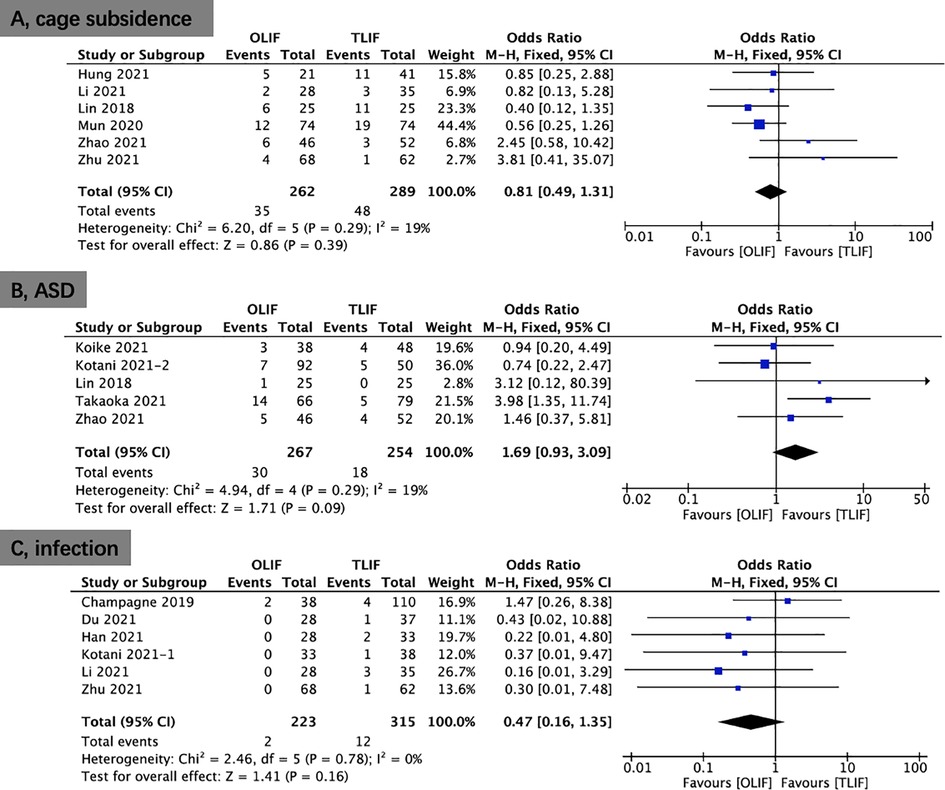
Figure 10. Forest plots comparing case subsidence (A), ASD (B), and infection rate (C) between OLIF and TLIF. ASD, adjacent segment disease; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
Sensitivity analysis
The sensitivity analysis was required to examine the stability of the results. The analysis results revealed that operative time, estimated intraoperative blood loss, length of hospital stay, DH (early postoperative and final follow-up), postoperative FH, LLA (preoperative and final follow-up), SLA (preoperative, early postoperative and final follow-up), VAS back pain (preoperative, early postoperative and final follow-up), VAS leg pain (preoperative and final follow-up), and ODI (3 months postoperative and final follow-up) showed significant heterogeneity.
In terms of operative time, length of hospital stay, DH (early postoperative and final follow-up), postoperative FH, final follow-up LLA, preoperative SLA, VAS back pain (early postoperative and final follow-up), preoperative VAS leg pain, and 3-month postoperative ODI, the included studies were excluded one by one, and the remaining articles were pooled. Sensitivity analyses demonstrated that the meta-analysis results did not change, indicating that the results were relatively stable.
In terms of operative time, preoperative VAS back pain, final follow-up VAS leg pain, final follow-up ODI, early postoperative LLA, and early postoperative and final follow-up SLA, sensitivity analysis revealed that after removing the most heterogeneous article, the meta-analysis results changed. Therefore, readers should be cautious about the results of these aspects.
Finally, in terms of postoperative disc angle, sensitivity analysis could not be performed because the number of included studies was only two.
Publication bias
Funnel plot (postoperative DH) was analyzed, and the result showed that the funnel plot was symmetrical (Supplementary Figure S4).
Discussion
Lumbar interbody fusion surgery has been conducted using various approaches as technology has advanced, including TLIF and OLIF. TLIF comprises direct decompression into the intervertebral space by laminectomy and facetectomy, which necessitates disruption of the paravertebral muscles and posterior spinal structures and retraction of nerve roots; nevertheless, major arteries, such as the aorta, are not impacted (14, 17, 18, 25). OLIF works differently way; it decompresses the disc space via the anatomical space between the psoas muscle and aorta. Many recent studies have demonstrated promising clinical outcomes with OLIF (19, 21, 24). However, high-quality comparison publications are required to assess the superiority of OLIF over TLIF methods. Therefore, we conducted this meta-analysis study to compare perioperative outcomes, clinical and radiological results, and complications.
Perioperative outcomes
Several studies have found that a longer operative time is associated with more surgical complications and that a shorter operative time is beneficial for postoperative outcomes (15, 17). Patients benefit from less perioperative blood loss because it lowers the risk of pathogen exposure, transfusion issues, perioperative anemia, morbidity, and death. In this meta-analysis, TLIF has a longer operative time and length of hospital stay and is associated with greater blood loss than OLIF. These outcomes were consistent with previous studies. The following are some possible explanations: in the TLIF, the paravertebral muscles on one side are stripped, along with a portion of the facet joint and lamina, neither of which is performed in OLIF (20). Moreover, in OLIF, the surgeon can perform disc space preparation under direct vision, but in TLIF, discectomy and endplate preparation are performed under blind conditions (13). The less postoperative drainage and shorter length of hospitalization stay in the OLIF group may potentially be attributed to the greater surgical damage of TLIF. Furthermore, we expect that the advantages of OLIF in terms of operative time and intraoperative blood loss will be further amplified as the number of fused segments increases. OLIF for LDD is outperformed by TLIF in terms of operative time, intraoperative bleeding, and length of hospital stay.
Clinical outcomes
Both the clinicians and patients were primarily concerned with postoperative pain alleviation and function recovery. In the current study, OLIF is preferred over TLIF in terms of early postoperative back pain relief. However, there was no statistically considerable difference in terms of postoperative leg pain relief. Noteworthy, although the preoperative ODI score of OLIF was higher than that of TLIF, the ODI of OLIF was significantly lower than that of TLIF postoperatively, which indicated that the postoperative function recovery of OLIF was better than that of TLIF. To the best of our knowledge, back muscles are important in linking various major muscles of the human body, and OLIF permits back muscles to stay intact postoperatively (17). By protecting the paraspinal muscles from injury and utilizing less soft tissue traction, OLIF benefits in improved postoperative recovery and pain for patients. Moreover, standard OLIF does not require additional posterior decompression and there is less intraoperative stimulation of the nerve roots.
Radiological parameters
TLIF is a direct decompression procedure to reduce nerve compression by expanding the spinal canal space and restoring the DH and FH. In pursuit of the same goals, OLIF introduces a larger lordotic cage to boost DH and FH, reduce disc bulging, and stretch the hypertrophied ligamentum flavum; therefore, indirectly decompressing the neuronal component (20). Our pooled analysis showed that OLIF provided better improvement in DH and FH than TLIF. The large lordotic OLIF cage is arguably the point. This might be attributed to the formation of a quite wide space in OLIF for adequate anterior release and insertion of a large lordotic cage. However, given the restricted surgical space and obstruction of the nerve roots and dural sac in TLIF, only a small cage with essentially little inclination angle may be implanted through the intervertebral foramen (22). Furthermore, the cage employed in OLIF has its own anterior convex characteristics (up to 12°) but they are mostly lacking in TLIF; as a result, LL in TLIF is only attained by compressing the posterior column.
LL and SLA are a critical radiological metric for determining the effectiveness of lumbar interbody fusion surgery. It was verified that LL and SLA were related to postoperative lumbar back discomfort and that correcting and maintaining LL and SLA were critical for reducing back pain and providing improved function (19). With lordotic OLIF cage, OLIF can restore more SLA than TLIF. Another potential explanation is that the large lordotic cage of OLIF is relatively placed anterior to the vertebral body and therefore performs better in terms of recovery from SLA in the early postoperative period. However, there was no remarkable difference in LL between the OLIF and TLIF groups in the early and final postoperative follow-ups. We consider that this difference may not be fully reflected in single-segment fusions (most of which were single segment in this study) and that the benefit of OLIF in producing pronation may become statistically significant as the number of fused segments increases.
This meta-analysis found better fusion rates in OLIF (86.2%) than TLIF (79.6%). OLIF allows better preparation of endplate and protection from intraoperative endplate injury, which may be one of the reasons for better fusion rates than TLIF. Another possibility is that the cages in the OLIF group occupied more intervertebral space than the cages in the TLIF group (16). This implies that a large cage footprint may offer a greater biologically efficient environment for the fusion process while also decreasing the likelihood of cage subsidence (23). Another concern is the generally low fusion rates in our study, probably due to the short follow-up period.
Previous studies have shown that the anterior region of the endplate is the strongest region and that implanting a cage in the anterior region of the vertebral body may contribute to cage subsidence (20). As a result, patients who underwent OLIF should have a lower risk of postoperative cage subsidence. However, our results revealed no variation in the incidence of cage subsidence between the OLIF (13.4%) and TLIF (16.6%) groups.
Complications
In terms of complications, TLIF (15.4%) had a slightly lower overall complication incidence than OLIF (17.8%); nevertheless, the difference was statistically insignificant. The most common approach-related complications in TLIF are dural tears and postoperative lower extremity discomfort caused by narrow intervertebral foraminal corridors and intraoperative distraction of the nerve roots. The most common approach-related complications following OLIF are vessel injury, transient thigh pain, and numbness, due to the anatomical features that the lumbar plexus, sympathetic trunk, and vascular tissues are all positioned on the lateral aspect of the anterior lumbar spine and are prone to stimulation or injury.
Moreover, the incidence of surgical site infection after OLIF was slightly lower compared to TLIF (0.9% vs. 3.8%), whereas the incidence of ASD appeared to be slightly higher (11.2% vs. 7.1%). However, no statistically relevant difference was found between the two groups.
Study limitations
There were some limitations in the current investigation. The first is its poor level of evidence, which was due to the fact that the all included studies had a retrospective design. Second, data on outcomes and heterogeneity of study cohorts were incomplete. Third, a subgroup analysis of the minimally invasive TLIF and open TLIF was not conducted. Finally, long-term results are lacking. Because of the aforementioned factors, high-quality research is still necessary to confirm the relative benefits of TLIF and OLIF.
Conclusions
According to our meta-analysis, OLIF results in a shorter operative time and length of hospital stay and less intraoperative blood loss compared to TLIF. Clinically, OLIF demonstrated quicker postoperative back pain alleviation and better benefit in postoperative function recovery compared to TLIF. Radiologically, OLIF demonstrated better restoration of DH and FH, improvement of early segmental lordosis, and higher fusion rate compared with TLIF. For both procedures, the incidence rates of overall and approach-related complications were comparable.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
GXL: performed drafted the work; WBX: helped the revisived manuscript; VK: performed the investigation and data curation; CMC: interpreted of data; ZD: performed software; MTZ: conceptualized or designed of the work. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the Natural Science Foundation of Fujian Province, grant number 2021J05282; funded by the “Xiamen Health System Discipline Leaders and their Backup Candidates, Senior Management Talent Training Candidates Training Program”.
Acknowledgments
The author Guang-Xun Lin would like to give thanks for the “Xiamen Health High-Level Talent Training Program”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1004870/full#supplementary-material.
References
1. Kim HS, Wu PH, Jang IT. Lumbar degenerative disease part 1: anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: a prospective case series and review of literature. Int J Mol Sci. (2020) 21(4):1483. doi: 10.3390/ijms21041483
2. Teng I, Han J, Phan K, Mobbs R. A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci. (2017) 44:11–7. doi: 10.1016/j.jocn.2017.06.013
3. Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment. Neurosurg Clin N Am. (2019) 30(3):299–304. doi: 10.1016/j.nec.2019.02.003
4. Heemskerk JL, Oluwadara Akinduro O, Clifton W, Quinones-Hinojosa A, Abode-Iyamah KO. Long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases: a meta-analysis. Spine J. (2021) 21(12):2049–65. doi: 10.1016/j.spinee.2021.07.006
5. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. (2015) 1(1):2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05
6. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. (2012) 6(2):89–97. doi: 10.4184/asj.2012.6.2.89
7. Chang MC, Kim GU, Choo YJ, Lee GW. Transforaminal lumbar interbody fusion (TLIF) versus oblique lumbar interbody fusion (OLIF) in interbody fusion technique for degenerative spondylolisthesis: a systematic review and meta-analysis. Life. (2021) 11(7):693. doi: 10.3390/life11070696
8. Koike Y, Kotani Y, Terao H, Iwasaki N. Comparison of outcomes of oblique lateral interbody fusion with percutaneous posterior fixation in lateral position and minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis. Asian Spine J. (2021) 15(1):97–106. doi: 10.31616/asj.2019.0342
9. Zhang QY, Tan J, Huang K, Xie HQ. Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: a meta-analysis. BMC Musculoskelet Disord. (2021) 22(1):802. doi: 10.1186/s12891-021-04687-7
10. Kotani Y, Ikeura A, Tokunaga H, Saito T. Single-level controlled comparison of OLIF51 and percutaneous screw in lateral position versus MIS-TLIF for lumbosacral degenerative disorders: clinical and radiologic study. J Orthop Sci. (2021) 26(5):756–64. doi: 10.1016/j.jos.2020.08.005
11. Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med. (2018) 6(6):104. doi: 10.21037/atm.2018.03.24
12. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. (2009) 339:b2535. doi: 10.1136/bmj.b2535
13. Champagne PO, Walsh C, Diabira J, Plante ME, Wang Z, Boubez G, et al. Sagittal balance correction following lumbar interbody fusion: a comparison of the three approaches. Asian Spine J. (2019) 13(3):450–8. doi: 10.31616/asj.2018.0128
14. Chen W, Yang H, Jiang X, Fan S. The effect of oblique lumbar interbody fusion compared with transforaminal lumbar interbody fusion combined with enhanced recovery after surgery program on patients with lumbar degenerative disease at short-term follow-up. Biomed Res Int. (2021) 2021:5806066. doi: 10.1155/2021/5806066
15. Du X, She Y, Ou Y, Zhu Y, Luo W, Jiang D. Oblique lateral interbody fusion versus transforaminal lumbar interbody fusion in degenerative lumbar spondylolisthesis: a single-center retrospective comparative study. Biomed Res Int. (2021) 2021:6693446. doi: 10.1155/2021/6693446
16. Han XG, Tang GQ, Han X, Xing YG, Zhang Q, He D, et al. Comparison of outcomes between robot-assisted minimally invasive transforaminal lumbar interbody fusion and oblique lumbar interbody fusion in single-level lumbar spondylolisthesis. Orthop Surg. (2021) 13(7):2093–101. doi: 10.1111/os.13151
17. Hung SF, Liao JC, Tsai TT, Li YD, Chiu PY, Hsieh MK, et al. Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci Rep. (2021) 11(1):12783. doi: 10.1038/s41598-021-92330-9
18. Kotani Y, Koike Y, Ikeura A, Tokunaga H, Saito T. Clinical and radiologic comparison of anterior-posterior single-position lateral surgery versus MIS-TLIF for degenerative lumbar spondylolisthesis. J Orthop Sci. (2021) 26(6):992–8. doi: 10.1016/j.jos.2020.10.013
19. Li R, Shao X, Li X, Liu Y, Jiang W. Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine. (2021) 100(3):e23783. doi: 10.1097/MD.0000000000023783
20. Lin GX, Akbary K, Kotheeranurak V, Quillo-Olvera J, Jo HJ, Yang XW, et al. Clinical and radiologic outcomes of direct versus indirect decompression with lumbar interbody fusion: a matched-pair comparison analysis. World Neurosurg. (2018) 119:e898–909. doi: 10.1016/j.wneu.2018.08.003
21. Mun HY, Ko MJ, Kim YB, Park SW. Usefulness of oblique lateral interbody fusion at L5-S1 level compared to transforaminal lumbar interbody fusion. J Korean Neurosurg Soc. (2020) 63(6):723–9. doi: 10.3340/jkns.2018.0215
22. Sheng SR, Geng YB, Zhou KL, Wu AM, Wang XY, Ni WF. Minimally invasive surgery for degenerative spondylolisthesis: transforaminal or oblique lumbar interbody fusion. J Comp Eff Res. (2020) 9(1):45–51. doi: 10.2217/cer-2019-0055
23. Takaoka H, Inage K, Eguchi Y, Shiga Y, Furuya T, Maki S, et al. Comparison between intervertebral oblique lumbar interbody fusion and transforaminal lumbar interbody fusion: a multicenter study. Sci Rep. (2021) 11(1):16673. doi: 10.1038/s41598-021-95774-1
24. Zhao L, Xie T, Wang X, Yang Z, Pu X, Lu Y, et al. Comparing the medium-term outcomes of lumbar interbody fusion via transforaminal and oblique approach in treating lumbar degenerative disc diseases. Spine J. (2021) 22(6):993–1001. doi: 10.1016/j.spinee.2021.12.006
25. Zhu HF, Fang XQ, Zhao FD, Zhang JF, Zhao X, Hu ZJ, et al. Comparison of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for treatment of lumbar degeneration disease: a prospective cohort study. Spine. (2021) 47(6):E233–E242. doi: 10.1097/BRS.0000000000004303
Keywords: oblique lumbar interbody fusion, transforaminal lumbar interbody fusion, OLIF, TLIF, meta-analysis, lumbar degenerative diseases
Citation: Lin G, Xu W, Kotheeranurak V, Chen C, Deng Z and Zhu M (2023) Comparison of oblique and transforaminal approaches to lumbar interbody fusion for lumbar degenerative disease: An updated meta-analysis. Front. Surg. 9:1004870. doi: 10.3389/fsurg.2022.1004870
Received: 27 July 2022; Accepted: 22 December 2022;
Published: 16 January 2023.
Edited by:
Wenyuan Ding, Third Hospital of Hebei Medical University, ChinaReviewed by:
Hui-Min Li, Zhejiang University, ChinaGabriel Tender, Louisiana State University, United States
© 2023 Lin, Xu, Kotheeranurak, Chen, Deng and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming-Tao Zhu em10ZHl5eUAxNjMuY29t Zhi-Hong Deng ZHpnaDEyMzQ1NkBzaW5hLmNvbQ== Chien-Min Chen OTYwMTVAY2NoLm9yZy50dw==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Guang-Xun Lin
Guang-Xun Lin Wen-Bin Xu1
Wen-Bin Xu1 Vit Kotheeranurak
Vit Kotheeranurak Chien-Min Chen
Chien-Min Chen