- Department of Surgery, Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
As a rare disease, intrahepatic sarcomatoid cholangiocarcinoma (s-CCC) represents less than 1% of malignancies of the hepatobiliary system and its main clinical symptoms include abdominal pain and fever. Results of pathological examinations, despite being the “gold standard”, can easily be confused with hepatocellular carcinoma (HCC). This report is about a 32-year-old male patient who was hospitalized due to occupancy of segment V of the liver for three days and had a history of chronic hepatitis B (CHB) over a 20-year span. Magnetic resonance imaging (MRI) showed a 43 mm × 52 mm-sized liver mass in the V segment, with patchy peripheral enhancement during the arterial phase and rapid wash-out during the portal and late phases. A laparoscopic hepatectomy of segment V, along with cholecystectomy, was performed. Histopathological and immunohistochemical examinations indicated a malignant neoplasm that was positive for vimentin and cytokeratin, with these features providing a positive diagnosis for intrahepatic sarcomatoid cholangiocarcinoma. After surgery, an adjuvant therapy of albumin-paclitaxel combined with gemcitabine regimen was given. No recurrence was found six months after the surgery, with follow-up still ongoing. This report aims to improve the awareness, diagnosis, and treatment of s-CCC.
Introduction
Primary liver cancer (PLC) is one of the malignant tumors with high morbidity and mortality (1). There was about 906,000 patients with primary liver cancer who were diagnosed each year, and nearly 830,000 patients died of PLC annually (2). According to histopathology, PLC is divided into three types as following: hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (ICC) and mixed hepatocellular cholangiocarcinoma (HCC-ICC), of which HCC is the predominant one. Intrahepatic cholangiocarcinoma, which accounts for 5% to 30% of PLC, is a rare hepatobiliary malignancy that arises from the epithelial cells of the intrahepatic bile ducts. However, intrahepatic sarcomatoid cholangiocarcinoma (s-CCC) is one of extremely rare type of ICC (3).
Intrahepatic sarcomatoid cholangiocarcinoma (s-CCC) is a condition that can affect different organs of the body including the urinary tract, uterus, thyroid, breast, skin, pancreas, lung, upper digestive tract and the gall bladder (4). However, being a rare disease that represents less than 1% of the malignancies affecting the hepatobiliary system (5), its pathogenesis remains to be clarified. Indeed, even though possible links between sarcomatoid hepatocellular carcinoma (HCC) and preoperative anticancer treatments such as radiofrequency ablation, transcatheter arterial chemoembolization or percutaneous ethanol injection have been reported (6), similar associations between s-CCC and anticancer treatments are yet to be demonstrated. Intrahepatic sarcomatoid cholangiocarcinoma is also most commonly characterized by fever and abdominal pain and since it is easily confused with hepatocellular carcinoma and other liver tumors, immunohistochemical staining is required for an accurate diagnosis. Although middle-aged and elderly individuals over 40 years old are considered to be the main high-risk group of s-CCC (7), in this study, the case of a 32-year-old patient, diagnosed with the condition, is described. A discussion of relevant literature is also undertaken in view of improving the awareness, diagnosis, and treatment of s-CCC.
Case report
The patient, a 32-year-old man was examined at a different hospital three days before and was found to have a hepatic V-segment occupancy. He complained of occasional upper abdominal pain at night, accompanied by nausea, but without fever, chills and other discomforts. With a history of chronic hepatitis B spanning over 20 years, the patient had also been under entecavir treatment. A physical examination showed no abnormal findings and no relevant family history was known.
The primary laboratory results showed normal levels for alanine aminotransferase (ALT), serum carcinoembryonic antigen (CEA), alpha-fetoprotein (AFP), serum total bilirubin and serum aspartate aminotransferase (AST). The tests also confirmed positive for hepatitis B surface antigen and hepatitis B core antibody in the serum.
A 43 mm × 52 mm-sized hypodense liver mass was observed in segment V based on contrasted computed tomography (CT) scans, with progressive peripheral enhancement during the arterial phase and a rapid wash-out during portal and late phases (Figure 1). A similarly sized mass was observed during contrasted liver magnetic resonance imaging (MRI), with a hypointense signal and a slightly hyperintense one noted on T1- and T2-weighted scans respectively. Additionally, obvious diffusion restriction was observed on diffusion weighted imaging (DWI) along with a hypointense signal in apparent diffusion coefficient (ADC) mapping, with patchy peripheral enhancement during the arterial phase and a rapid wash-out during the portal and late phases (Figure 2).
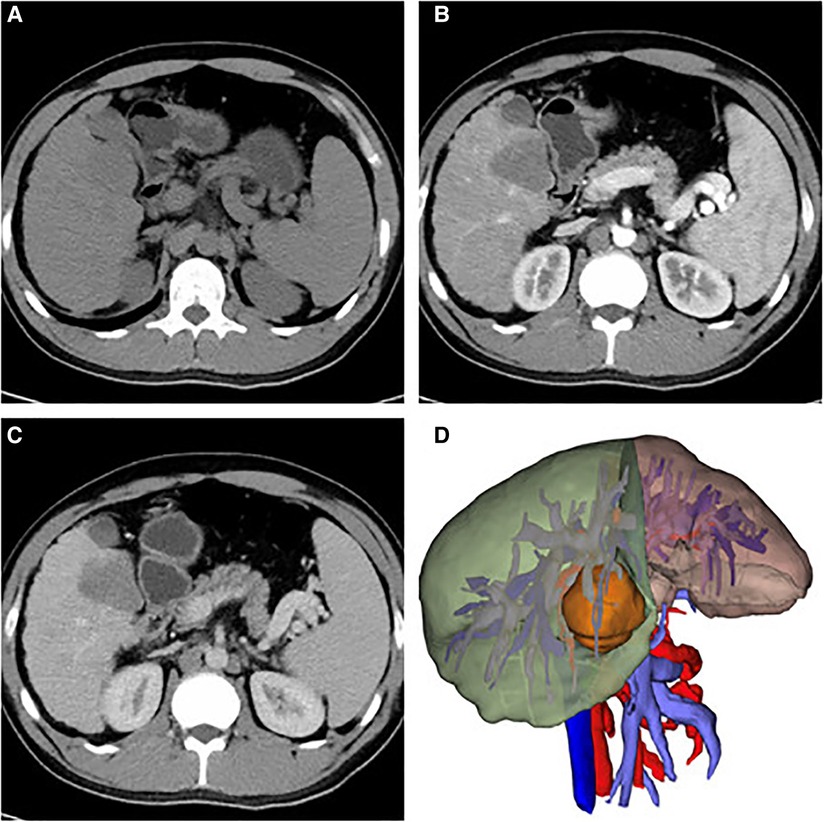
Figure 1. Ct images of axial sections: (A) A bulky hypodense mass in segment V of the liver indicates the lesion; arterial phase (B) shown enhancement of peripheral areas and slight progressive centripetal enhancement in portal phase (C); three-dimensional reconstruction of the liver mass in segment V (43 mm × 52 mm-sized) (D).
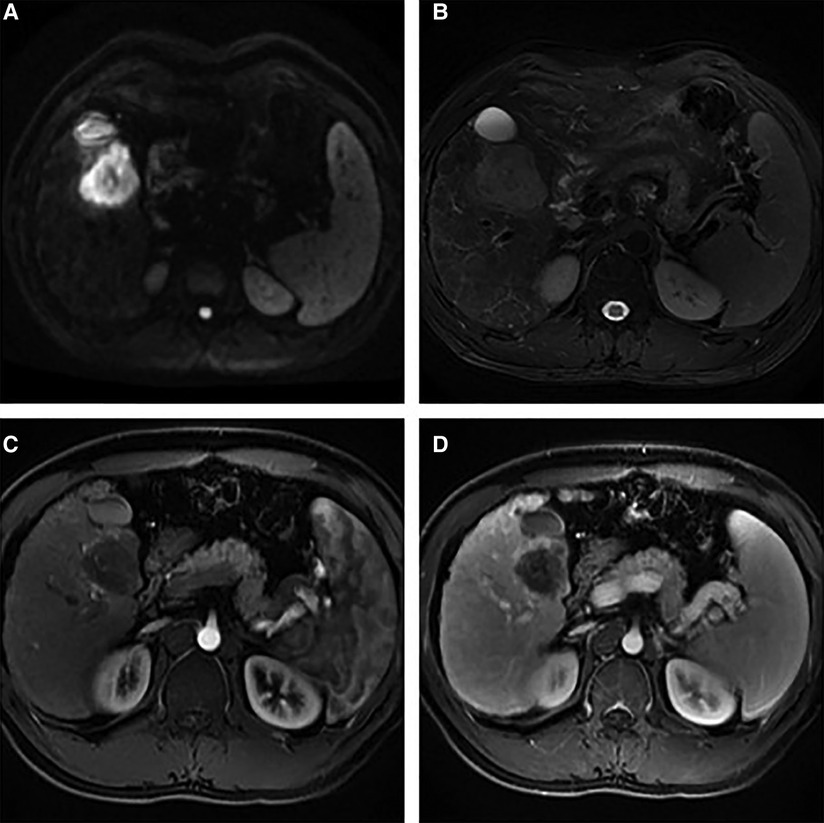
Figure 2. Contrasted MRI images of the liver: (A) an abnormal signal liver mass in segment V and obvious restricted diffusion on DWI; (B) a hypointense signal and a slightly hyperintense one on T1- and T2-weighted scans respectively; (C) patchy peripheral enhancement in the arterial phase, and (D) rapid washout in the portal and late phases.
A laparoscopic segmentectomy of segment V of the liver was carried out along with cholecystectomy and no postoperative bleeding, biliary fistula or other complications occurred. Following the surgery, the patient had an uneventful recovery and was therefore discharged after eight days.
Histological examinations showed a primary high-grade malignant tumor with patchy necrosis and abundant lymphocyte infiltration. The absence of cancer infiltration in nerves, in vessels or at the margin of hepatectomy was also noted (Figure 3). Furthermore, the neoplasm was found to be positive for vimentin, programmed cell death ligand 1 (PD-L1), cytokeratin (CK) 19, CK7, cluster of differentiation (CD) 34 (vessels) and CD31 (vessels) after immunohistochemical examination while staining for hepatocyte paraffin 1 (HepPar-1), AFP, CK20, Glypican-3 returned negative results. The Ki-67 score was approximately 50%. Altogether, the above results confirmed the diagnosis for intrahepatic sarcomatoid cholangiocarcinoma. An adjuvant therapy of albumin-paclitaxel combined with gemcitabine regimen was given for 8 cycles of treatment after surgery. No recurrence was found seventeen months after the operation, with follow-up still ongoing.
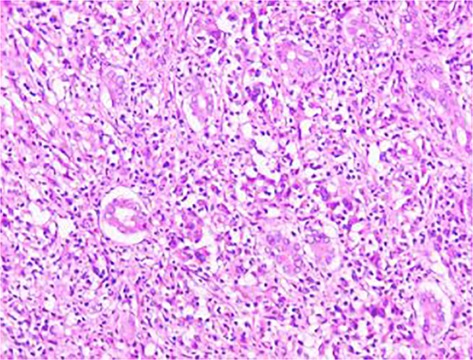
Figure 3. Histologic findings (hematoxylin and eosin staining, 40 × ): primary high-grade malignant tumor with patchy necrosis and abundant lymphocyte infiltration. Cancer infiltration was not observed in nerves, in vessels or at the margin of hepatectomy.
Discussion
Intrahepatic sarcomatoid cholangiocarcinoma represents a rare form of intrahepatic cholangiocarcinoma that mostly affects middle-aged and elderly individuals over 40 years old (8). This case report is about a 32-year-old man, the youngest patient with the condition.
Around 4.5% of autopsied and surgical cases of intrahepatic cholangiocarcinoma show sarcomatoid transformation (9), with similar transformations observed in sarcomatoid HCC which accounts for 3.9%–9.4% of HCC autopsy cases. As pointed out earlier, sarcomatoid HCC is reportedly linked with various preoperative anticancer treatments, including radiofrequency ablation, transcatheter arterial chemoembolization or percutaneous ethanol injection (10).
On the other hand, the pathogenesis of s-CCC has not yet been clarified, although a few possibilities have been put forward. Firstly, it was suggested to be the result of sarcomatoid transdifferentiation or the dedifferentiation of primary epithelial carcinoma cells, with these processes often referred to as metaplastic transformation or epithelial-mesenchymal transition (EMT). It is also possible that pluripotent stem cells could be undergoing biphasic differentiation to sarcoma or carcinoma in various directions, resulting in a combination of both cell types depending on the growth of each tumor type. Finally, carcinoma cells could give rise to cancer cells with multipotent differentiation potency that subsequently undergo sarcomatoid redifferentiation (5).
s-CCC can be asymptomatic, but it may also manifests itself by nonspecific symptoms or signs including weight loss, fatigue, nausea, fever and abdominal pain, with the latter two being more specific indicators of the condition. For the young patient under study, upper abdominal pain accompanied by nausea was reported but there was no fever or any other forms of discomfort.
Previously, common serological markers such as AFP, CA19–9, CEA as well as protein induced by vitamin K absence or antagonist-II (PIVKA-II), were negative or low for s-CCC (11–12). However, when analyzing the level of tumor markers in 11 cases of s-CCC, Kim D. K et al. found that they were not reliable to diagnose s-CCC (5). Similarly, the current report found the young patient's serum CEA and AFP content to be at normal levels. Moreover, even though hypoattenuation and peripheral region enhancement are common characteristics observed for s-CCC after contrast injection during CT scans, similar features may also be visible during CT scans of HCC, thus, making these features, on their own, unsuitable to distinguish s-CCC from HCC.
However, s-CCC also exhibits unique histopathological and molecular patterns, with one of these being the fact that its tumor cells usually have exact malignant epithelial cholangiocytic and sarcomatoid biphasic components (13). The cholangiocarcinomatous nature of tumors is normally diagnosed with the help of immunohistochemistry, with previous immunohistochemical results revealing that s-CCC tumors tend to be positive for both vimentin, the mesenchymal tumor marker as well as CK7 and CK8, the epithelial cholangiogenic tumor markers while tests for HepPar-1 tend to be yield negative results (14). For the current study, histological examinations showed a primary high-grade malignant tumor with patchy necrosis and abundant lymphocyte infiltration. Immunohistochemical examinations further showed positive staining for vimentin, CK19, CK7, CD34 (vessels), CD31 (vessels) and PD-L1 while results for AFP, Glypican-3, CK20, PD-L1 and HepPar-1 were negative. The latter, as a marker of hepatocytes, helps to distinguish cholangiocarcinoma and metastatic carcinoma in the liver from HCC and as such, it is of diagnostic value.
In addition to the above, the common characteristics of s-CCC were also reviewed by searching for relevant case reports or series from the available literature in PubMed (English only), with Table 1 showing the clinical aspects of 76 identified cases of s-CCC. Of the patients reported in the studies (age range: 32–87; mean age: 61 years old), 52 (68.4%) were males and 24 (31.6%) were females. The tumor size was, on average, 8.0 cm (range: 2.0–25.0 cm). The main complaint was also recorded for 52 patients, with the most common one being abdominal pain which occurred in 30 patients (57.7%). In contrast, only 15 patients (28.8%) complained of fever while 7 patients (13.5%) reported weight loss.
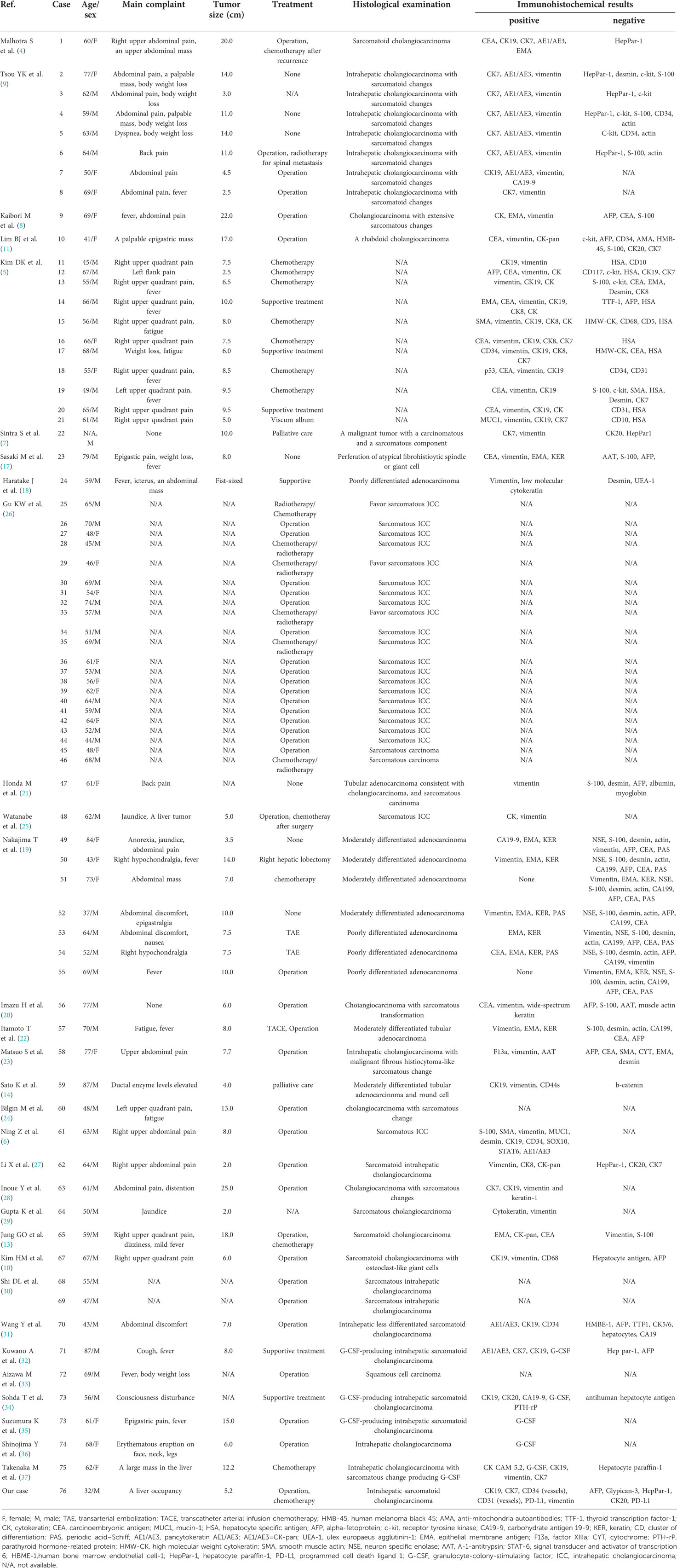
Table 1. Clinical findings and immunohistochemistry results of patients diagnosed with intrahepatic sarcomatoid cholangiocarcinoma.
As far as laboratory findings were concerned, results for the level of serum aspartate aminotransferase (AST) was available for 25 patients and they ranged from 16 to 205 (median: 34, normal: <40) U/L. Similarly, for 24 patients, the level of alanine aminotransferase (ALT) ranged from 10 to 356 (median: 33.5, normal: <40) U/L. In addition, the levels of alpha-fetoprotein (AFP), carbohydrate antigen 19-9 (CA19-9) and serum carcinoembryonic antigen (CEA) were found to be high in 8 (14.5%), 22 (40.7%) and 10 (28.6%) patients respectively while they were found to be normal for 47 (85.5%), 32 (59.3%) and 25 (71.4%) patients respectively (Supplementary Table S2).
The results of immunohistochemical analyses for 50 patients were also available and are presented in Table 1. Basically, 21 patients (42.0%) were positive for CK19 while for vimentin, 38 patients (76.0%) showed positive results. Furthermore, HepPar-1 and AFP were negative for 10 (20.0%) and 18 (36.0%) patients respectively, with these markers being significantly helpful in diagnosing s-CCC.
The treatment of tumors was recorded for 74 patients (Table 1). Of these, 35 (47.3%) underwent surgery, 15 (20.3%) were given radiotherapy or chemotherapy, 8 (10.8%) underwent supportive treatment or palliative care, 5 (6.8%) had surgery followed by chemotherapy/radiotherapy, 2 (2.7%) had transcatheter arterial embolization (TAE), 1 (1.3%) received viscum album treatment and 1 (1.3%) had transcatheter arterial infusion chemotherapy (TACE) as well as surgical treatment. 7 patients (9.5%) also remained untreated.
Follow-up information was available for 73 patients (Supplementary Table S1), of whom 44 (60.3%) experienced disease progression and died while 15 (20.5%) survived. In addition, 12 patients (16.4%) also experienced disease recurrence, and 2 (2.7%) were lost during follow-up.
Electron microscopy is also used to diagnose neoplasms of s-CCC and in this case, irrespective of their hepatocyte origin, the tumors are characterized by the presence of microvilli and basement membranes (4). Hence, based on results from electron microscopy, immunohistochemistry as well as histological examinations, sarcomatoid cholangiocarcinoma can be accurately diagnosed.
Guidelines to determine the progression of s-CCC and survival of patients are yet to be clearly defined or established. Furthermore, the extent to which radiation therapy or chemotherapy can be useful against s-CCC remains to be investigated. Nevertheless, it has been reported that viscum album, an extract from a hemiparasitic plant, could exhibit positive results against s-CCC. This extract can also be useful as part of palliative therapies for terminally-ill patients who turn resistant to conventional chemotherapy, who are suffering from hematologic diseases and even for those with lung cancer or accompanying malignant pleural effusion (15, 16). With an established treatment regimen yet to be developed, surgical resection remains the preferred approach, especially since it can even be complemented with adjuvant chemotherapy for improving the survival rate. In the current report, laparoscopic segmentectomy of segment V of the liver was undertaken alongside cholecystectomy and this was followed by adjuvant therapy with albumin-paclitaxel combined with gemcitabine. No recurrence was found seventeen months after surgery, with follow-up still ongoing.
Conclusion
Cholangiocarcinoma, with sarcomatoid features, is a rare but aggressive form of malignant tumor that can only be diagnosed through a combination of histopathological examination, electron microscopy and immunohistochemical studies. The early detection and complete removal of tumors offer the possibility for increased survival. However, in comparison with intrahepatic cholangiocarcinoma, more thorough postoperative follow-up is required for identifying recurrences or metastases.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/s for the publication of this case report.
Author contributions
LFX and YJ collected the data, performed the statistical analysis and drafted the manuscript. All authors read and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.963952/full#supplementary-material.
References
1. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet (London, England). (2018) 391(10127):1301–14. doi: 10.1016/S0140-6736(18)30010-2
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
3. Lee AJ, Chun YS. Intrahepatic cholangiocarcinoma: the AJCC/UICC 8th edition updates. Chin Clin Oncol. (2018) 7(5):52. doi: 10.21037/cco.2018.07.03
4. Malhotra S, Wood J, Mansy T, Singh R, Zaitoun A, Madhusudan S. Intrahepatic sarcomatoid cholangiocarcinoma. J Oncol. (2010) 2010:701476. doi: 10.1155/2010/701476
5. Kim DK, Kim BR, Jeong JS, Baek YH. Analysis of intrahepatic sarcomatoid cholangiocarcinoma: experience from 11 cases within 17 years. World J Gastroenterol. (2019) 25:608–21. doi: 10.3748/wjg.v25.i5.608
6. Zhang N, Li Y, Zhao M, Chang X, Tian F, Qu Q, et al. Sarcomatous intrahepatic cholangiocarcinoma: case report and literature review. Medicine (Baltimore). (2018) 97:e12549. doi: 10.1097/MD.0000000000012549
7. Sintra S, Costa R, Filipe C, Simão A. Intrahepatic sarcomatoid cholangiocarcinoma. BMJ Case Rep. (2018) 2018:bcr-2018. doi: 10.1136/bcr-2018-225017
8. Kaibori M, Kawaguchi Y, Yokoigawa N, Yanagida H, Takai S, Kwon AH, et al. Intrahepatic sarcomatoid cholangiocarcinoma. J Gastroenterol. (2003) 38:1097–101. doi: 10.1007/s00535-003-1203-y
9. Tsou YK, Wu RC, Hung CF, Lee CS. Intrahepatic sarcomatoid cholangiocarcinoma: clinical analysis of seven cases during a 15-year period. Chang Gung Med J. (2008) 31:599–605. doi: 10.202207/article.19241900
10. Kim HM, Kim H, Park YN. Sarcomatoid cholangiocarcinoma with osteoclast-like giant cells associated with hepatolithiasis: a case report. Clin Mol Hepatol. (2015) 21:309–13. doi: 10.3350/cmh.2015.21.3.309
11. Lim BJ, Kim KS, Lim JS, Kim MJ, Park C, Park YN. Rhabdoid cholangiocarcinoma: a variant of cholangiocarcinoma with aggressive behavior. Yonsei Med J. (2004) 45:543–6. doi: 10.3349/ymj.2004.45.3.543
12. Wang T, Kong J, Yang X, Shen S, Zhang M, Wang W. Clinical features of sarcomatoid change in patients with intrahepatic cholangiocarcinoma and prognosis after surgical liver resection: a propensity score matching analysis. J Surg Oncol. (2020) 121:524–37. doi: 10.1002/jso.25815
13. Watanabe G, Uchinami H, Yoshioka M, Nanjo H, Yamamoto Y. Prognosis analysis of sarcomatous intrahepatic cholangiocarcinoma from a review of the literature. Int J Clin Oncol. (2014) 19:490–6. doi: 10.1007/s10147-013-0586-x
14. Sato K, Murai H, Ueda Y, Katsuda S. Intrahepatic sarcomatoid cholangiocarcinoma of round cell variant: a case report and immunohistochemical studies. Virchows Arch. (2006) 449:585–90. doi: 10.1007/s00428-006-0291-5
15. Thronicke A, Oei SL, Merkle A, Matthes H, Schad F. Clinical safety of combined targeted and Viscum album L. Therapy in Oncological Patients. Medicines (Basel, Switzerland). (2018) 5:100–116. doi: 10.3390/medicines5030100
16. Schad F, Thronicke A, Steele ML, Merkle A, Matthes B, Grah C, et al. Overall survival of stage IV non-small cell lung cancer patients treated with Viscum album L. in addition to chemotherapy, a real-world observational multicenter analysis. PLoS One. (2018) 13:e0203058. doi: 10.1371/journal.pone.0203058
17. Sasaki M, Nakanuma Y, Nagai Y, Nonomura A. Intrahepatic cholangiocarcinoma with sarcomatous transformation: an autopsy case. J Clin Gastroenterol. (1991) 13:220–5. doi: 10.1097/00004836-199104000-00022
18. Haratake J, Yamada H, Horie A, Inokuma T. Giant cell tumor-like cholangiocarcinoma associated with systemic cholelithiasis. Cancer. (1992) 69:2444–8. doi: 10.1002/1097-0142(19920515)69:10<2444::aid-cncr2820691010>3.0.co;2-r
19. Nakajima T, Tajima Y, Sugano I, Nagao K, Kondo Y, Wada K. Intrahepatic cholangiocarcinoma with sarcomatous change. Clinicopathologic and immunohistochemical evaluation of seven cases. Cancer. (1993) 72:1872–7. doi: 10.1002/1097-0142(19930915)72:6<1872::aid-cncr2820720614>3.0.co;2-n
20. Imazu H, Ochiai M, Funabiki T. Intrahepatic sarcomatous cholangiocarcinoma. J Gastroenterol. (1995) 30:677–82. doi: 10.1007/bf02367798
21. Honda M, Enjoji M, Sakai H, Yamamoto I, Tsuneyoshi M, Nawata H. Case report: intrahepatic cholangiocarcinoma with rhabdoid transformation. J Gastroenterol Hepatol. (1996) 11:771–4. doi: 10.1111/j.1440-1746.1996.tb00330.x
22. Itamoto T, Asahara T, Katayama K, Momisako H, Dohi K, Shimamoto F. Double cancer - hepatocellular carcinoma and intrahepatic cholangiocarcinoma with a spindle-cell variant. J Hepatobiliary Pancreat Surg. (1999) 6:422–6. doi: 10.1007/s005340050144
23. Matsuo S, Shinozaki T, Yamaguchi S, Takami Y, Obata S, Tsuda N, et al. Intrahepatic cholangiocarcinoma with extensive sarcomatous change: report of a case. Surg Today. (1999) 29:560–3. doi: 10.1007/BF02482354
24. Bilgin M, Toprak H, Bilgin SS, Kondakci M, Balci C. CT And MRI findings of sarcomatoid cholangiocarcinoma. Cancer Imaging. (2012) 12:447–51. doi: 10.1102/1470-7330.2012.0036
25. Go W, Uchinami H, Yoshioka M, Nanjo H, Yamamoto Y. Prognosis analysis of sarcomatous intrahepatic cholangiocarcinoma from a review of the literature. Int J Clin Oncol. (2014) 19:490–6. doi: 10.1007/s10147-013-0586-x
26. Gu KW, Kim YK, Min JH, Ha SY, Jeong W K. Imaging features of hepatic sarcomatous carcinoma on computed tomography and gadoxetic acid-enhanced magnetic resonance imaging. Abdom Radiol. (2017) 42:1424–33. doi: 10.1007/s00261-016-1038-7
27. Li X, Li J, Liu K, Tan L, Ya L. Sarcomatoid intrahepatic cholangiocarcinoma in a patient with poor prognosis: a case report and literature review. J Int Med Res. (2020) 48:300060520969473. doi: 10.1177/0300060520969473
28. Inoue Y, Lefor AT, Yasuda Y. Intrahepatic cholangiocarcinoma with sarcomatous changes. Case Rep Gastroenterol. (2012) 6:1–4. doi: 10.1159/000335883
29. Gupta K, Powari M, Dey P. Sarcomatous cholangiocarcinoma. Diagn Cytopathol. (2003) 28:168–9. doi: 10.1002/dc.10259
30. Shi D, Ma L, Zhao D, Chang J, Shao C, Qi S, et al. Imaging and clinical features of primary hepatic sarcomatous carcinoma. Cancer Imaging. (2018) 18:36. doi: 10.1186/s40644-018-0171-7
31. Wang Y, Ming JL, Ren XY, Qiu L, Zhou LJ, Yang SD, et al. Sarcomatoid intrahepatic cholangiocarcinoma mimicking liver abscess: a case report. World J Clin Cases. (2020) 8:208–16. doi: 10.12998/wjcc.v8.i1.208
32. Kuwano A, Narutomi F, Nagasawa S, Tanaka K, Morita Y, Yada M, et al. A case of granulocyte colony-stimulating factor-producing intrahepatic sarcomatoid cholangiocarcinoma. Clin J Gastroenterol. (2021) 14:881–7. doi: 10.1007/s12328-021-01405-7
33. Aizawa M, Koshiyama H, Inoue D, Fukunaga Y, Katakami H, Miki M, et al. Postoperative aggravation of hypercalcemia-leukocytosis syndrome in a case of squamous cell type cholangiocarcinoma. Intern Med. (1997) 3:232. doi: 10.2169/internalmedicine.36.232
34. Sohda T, Shiga H, Nakane H, Watanabe H, Takeshita M, Sakisaka S. Cholangiocellular carcinoma that produced both granulocyte-colony-stimulating factor and parathyroid hormone-related protein. Int J Clin Oncol. (2006) 11:246–9. doi: 10.1007/s10147-006-0560-y
35. Suzumura K, Iimuro Y, Hirano T, Asano Y, Kuroda N, Okada T, et al. Granulocyte colony-stimulating factor-producing cholangiocellular carcinoma. Int Surg. (2015) 100:123–7. doi: 10.9738/INTSURG-D-13-00183.1
36. Shinojima Y, Toma Y, Terui T. Sweet syndrome associated with intrahepatic cholangiocarcinoma producing granulocyte colony-stimulating factor. Br J Dermatol. (2006) 155:1103–4. doi: 10.1111/j.1365-2133.2006.07521.x
Keywords: intrahepatic sarcomatoid cholangiocarcinoma, hepatobiliary malignancy, sarcomatoid change, immunohistochemical staining, case report
Citation: Xi L-F, Jin Y and Li J-T (2022) Intrahepatic sarcomatoid cholangiocarcinoma: A case report of the youngest patient on record and a review of the condition's characteristics. Front. Surg. 9:963952. doi: 10.3389/fsurg.2022.963952
Received: 8 June 2022; Accepted: 15 August 2022;
Published: 1 September 2022.
Edited by:
Sami Akbulut, İnönü University, TurkeyReviewed by:
Tevfiktolga Sahin, İnönü University, TurkeyArif Emre, Kahramanmaras Sütçü Imam University, Turkey
© 2022 Xi, Jin and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiang-Tao Li enJsanRAemp1LmVkdS5jbg==
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Long-Fu Xi
Long-Fu Xi Yun Jin
Yun Jin Jiang-Tao Li
Jiang-Tao Li