- 1Department of Medical and Surgical Sciences, Spasticity and Movement Disorders “ReSTaRt”, Unit Physical Medicine and Rehabilitation Section, University of Foggia, Foggia, Italy
- 2Department of Medical and Surgical Specialties and Dentistry, University of Campania “Luigi Vanvitelli”, Naples, Italy
- 3Department of Scientific Research, Campus Ludes, Off-Campus Semmelweis University, Lugano, Switzerland
- 4Neurorehabilitation Unit, Istituti Clinici Scientifici Maugeri, IRCCS, Institute of Bari, Bari, Italy
Glioma is a group of tumors that originate from glial cells within the central nervous system and comprise 27% of all tumors and 80% of malignant tumors. With remarkable progress in surgical practices, chemotherapy, and radiation therapy, patients with glioma are experiencing greater survival times, which means they need more rehabilitative care. In fact, people with this condition may experience a variety of symptoms that can affect their functions and drastically reduce their quality of life. In fact, patients suffering from glioma has a distinctive symptom complex highlighting the requirement for customized care. Growing evidence shows that rehabilitation therapy can improve the functional prognosis and quality of life of glioma patients. However, there is limited evidence of the success of rehabilitation protocols designed specifically for individuals with glioma. It is essential to determine the most comprehensive rehabilitation programs as well as the sufficient resources, dosage, and duration. The goal of this mini-review was to classify and map rehabilitation interventions used to treat multiple disabling sequalae in individuals affected by glioma. We aim to provide a comprehensive overview of the rehabilitation protocols used for this population, so that clinicians have a guide to support treatment and an inspiration for further research. This document is intended to be a reference point for professionals involved in the management of adult patients with gliomas. Further exploration is needed to form improved care models for recognizing and addressing functional restrictions in this population.
1. Introduction
Gliomas are tumors that originate from glial cells in the central nervous system. They can be divided into two main groups: diffuse gliomas, which infiltrate their surroundings, and those with a more circumscribed growth pattern (1). The World Health Organization updated the Classification of Tumors of the Central Nervous System in 2021 (2). This update separated paediatric-type and adult-type diffuse gliomas, as they differ in clinical and biological aspects (3). Recent advances in surgical techniques, chemotherapy, and radiation therapy have increased the survival of glioma patients, but they also need more rehabilitation support and services (4).
Patients diagnosed with glioma have specific functional impairments and restrictions in physical activity, making them a distinct patient population. They experience many symptoms that affect their neurological functions and quality of life. A recent review (5) reveals that the ten most prevalent symptoms in glioma patients are: seizures (37%), cognitive deficits (36%), drowsiness (35%), dysphagia (30%), headache (27%), confusion (27%), aphasia (24%), motor deficits (21%), fatigue (20%) and dyspnea (20%). Moreover, approximately 60% of glioma patients are insufficiently active or sedentary and do not meet the Physical Activity Guideline provided by the World Health Organization (6). Glioma patients are a distinct group within the cancer population because of their unique burden of symptoms. The International Classification of Functioning, Disability and Health (ICF) framework can help to explain how this disease impacts different areas of life, such as impairments (headaches, seizures, etc.), activity (decreased mobility), and participation (work, family, etc.), affecting the quality of life (7).
The purpose of rehabilitation is to effectively improve the motor, consciousness and psychology of glioma patients (8). The guidelines stated that patients “with any type of brain tumor should be referred for rehabilitation consultation upon diagnosis and at every stage of following up, including with metastatic disease” (9). However, crucial information on best practices, settings, type, intensity, duration, and cost-effectiveness of therapy is lacking.
To accurately assess the issues and plan effective interventions, a range of factors needed to be considered and only a multidisciplinary approach could ensure that each person can receive support tailored to their individual physical, sensory, cognitive, psychological and social needs. Preliminary research suggests that rehabilitation can reduce disability in glioma patients, by improving both functional abilities and cognitive functioning compared to standard care. A recent meta-analysis (10) indicates that patients with glioma receiving rehabilitation have better outcomes on neurological function and quality of life.
To date, there is limited evidence of the success of rehabilitation programs designed specifically for individuals with glioma. The impact of multidisciplinary treatment was examined by a Cochrane Review completed in 2013, although no RCTs could be included due to the difficulties in locating high-quality research. The twelve lower-quality observational studies included led the authors to draw the following conclusions: interdisciplinary rehabilitation is not detrimental and may even improve disability and quality of life (11). A few years later, the same authors provided only low evidence that multidisciplinary rehabilitation may reduce short- and long-term motor disabilities in people after primary brain tumor treatment. Indeed, there is still a gap in this research area and the need for new research is evident (11).
This mini-review is not intended to be a comprehensive review of the available literature on glioma tumor rehabilitation as it serves as a guide for clinicians to support treatment and facilitate further research. We aim to offer a comprehensive overview of the rehabilitation protocols used for this population.
2. Rehabilitation intervention
2.1. Literature research
References for this review were obtained by searching the online databases PUBMED, CINAHL, Web of Science, Cochrane, and Scopus until November 2022. Search terms included: brain, glioma, rehabilitation, intervention with the Boolean operator “AND” to narrow results and connect terms. We considered articles published after the year 2000 and papers printed in or translated into English. Only observational studies and randomized control trials were included. Some of the references were not found through online databases, but rather through reference lists of other articles.
The raw search of the databases yielded a total of 164 articles, then an initial filtering within the same databases by document type (Article; Clinical Trial;) and a subsequent filtering of duplicate articles, left 31 unique articles. These 31 articles were subjected to a review of titles and abstracts, leaving 29 articles as candidates for assessment for eligibility. Only 13 articles met the inclusion criteria with 16 articles being excluded. To ensure the homogeneity of the study population, we excluded 6 papers that reported on various brain tumor types, such as meningiomas, metastases, and other tumors, besides glioma (Prisma Flow Chart in Supplementary Material).
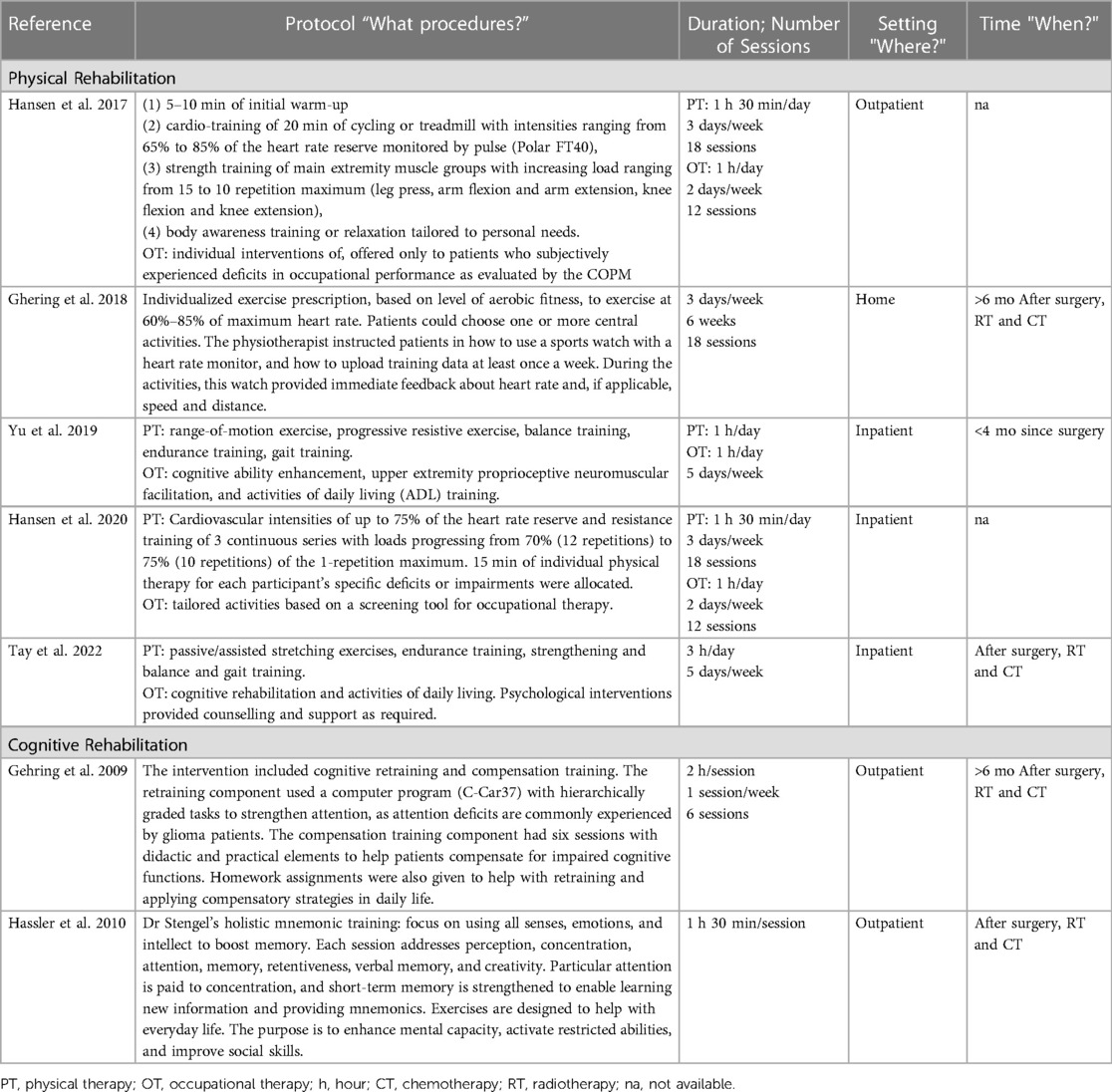
Studies included in the present review are those reporting a full description of the rehabilitation protocol applied. For this research, we used the TIDieR (Template for Intervention Description and Replication) checklist to capture intervention descriptions. This checklist included categories such as “brief name”, “why”, “what (materials)”, “what (procedures)”, “who provided”, “how”, “where”, “when and how much”. The TIDieR checklist is designed to ensure that authors provide enough detail for others to replicate their interventions.
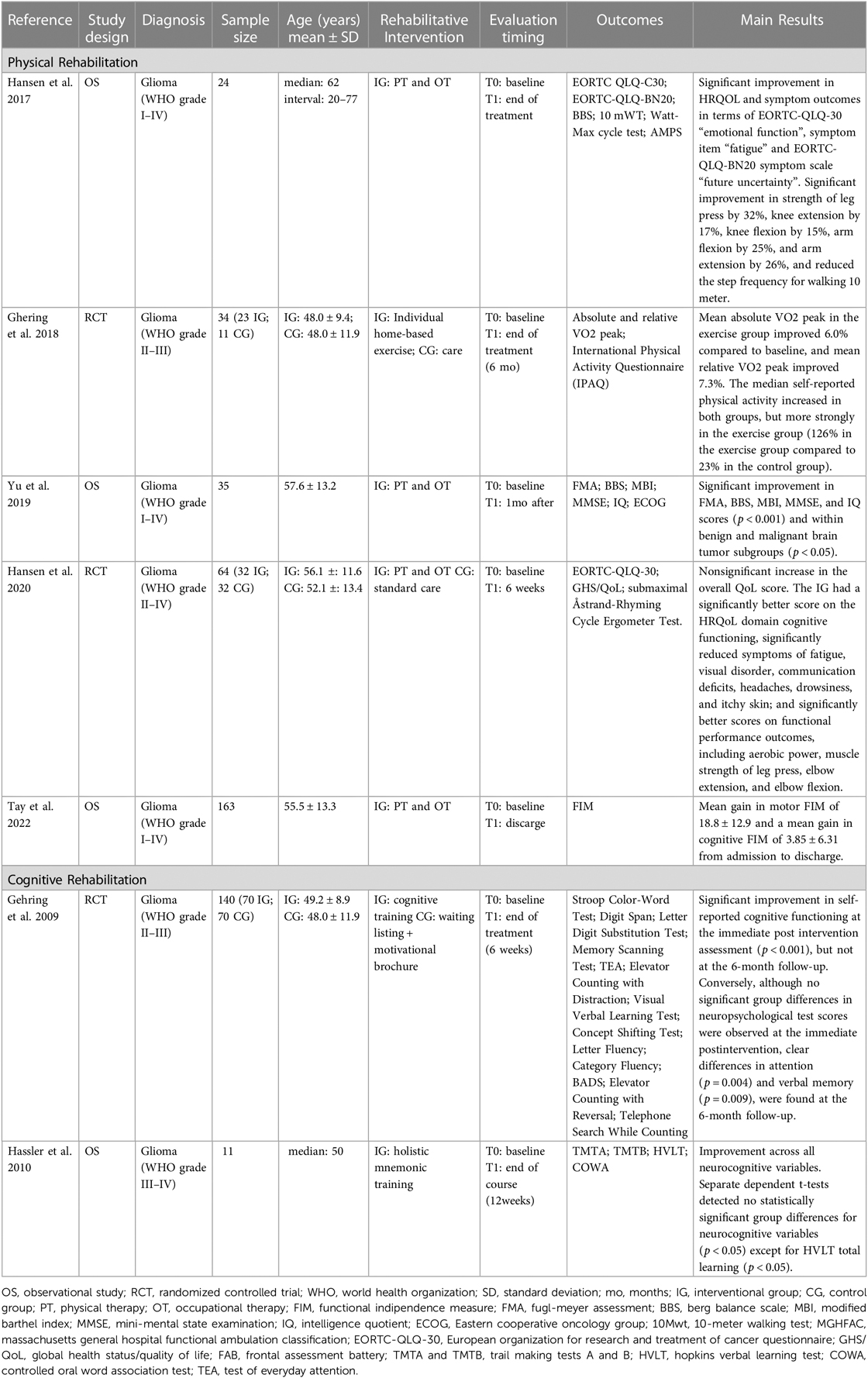
Data extracted are summarized in Tables 1, 2. Studies are divided in two groups: physical and cognitive therapy.
2.2. Physical therapy
Motor deficits associated with brain tumors can vary greatly and include focal deficits such as hemiparesis/plegia with spasticity, gait impairment, ataxia, and incoordination. These impairments depend on the location and extent of the tumor or its treatment, and may affect different muscles or limbs (12). Patients may also experience muscle weakness, fatigue, and reduced physical activity due to chronic steroid use and inflammation caused by the tumor. Furthermore, patients may have trouble performing complex movements, lose motor skills, and become clumsy. These motor impairments can impair mobility and daily functioning, and can result in pain, anxiety and/or depression, loss of independence, and lower quality of life. Therefore, patients need appropriate treatment to improve their motor function, prevent complications of immobility such as pressure ulcers, muscle atrophy, and contractures, and enhance their well-being and quality of life (13). Rehabilitation aims to address the causes of motor dysfunction and the effects it has on physical function, well-being, and quality of life (14).
Five studies were included: two RCTs and three observational studies that examined inpatient, outpatient, and home-based rehabilitation for benign and malignant brain tumors. Different grades of brain tumors were included in all studies. The timing of the rehabilitation varied from study to study—from early after surgery to weeks after the completion of proper management. Rehabilitation protocols usually include physical therapy, occupational therapy, psychological support, and cognitive therapies.
Yu et al. (15) in a retrospective study on the effectiveness of intensive rehabilitation for people recovering from a brain tumor surgery, found that intensive rehabilitation during hospitalization (2 h/die, 5 days/week) after brain tumor surgery resulted in a significant improvement in the outcomes of motor, cognition, and ADL function regardless of the type of tumor. The program included range-of-motion exercise, progressive resistive exercise, balance training, endurance training and gait training.
Tay et al. (16) provided evidence for the effects of an inpatient protocol including passive/assisted stretching exercises, endurance training, strengthening, balance and gait training. They found an improvement in the FIM score, describing a mean gain in motor FIM of 18.8 (SD = 12.9) and a mean gain in cognitive FIM of 3.85 (SD = 6.31) from admission to discharge.
Hansen et al. (17) conducted an interdisciplinary outpatient rehabilitation intervention to assess safety and feasibility. The intervention was a 90-minute protocol, three times a week, with up to four patients in a group exercising together, including warm-up exercise, cardio-training, strength training, and body awareness training or relaxation tailored to personal needs. The results were impressive as patients experienced improved HRQOL and symptom outcomes in terms of EORTC-QLQ-30 “emotional function”, symptom item “fatigue”, and EORTC-QLQ-BN20 symptom scale “future uncertainty”. Furthermore, participants increased their muscle strength and reduced the step frequency for walking 10 meters. Moreover, participants were satisfied with the results. Some years later, the same authors (18) another study to see how effective a 6-week therapy program would be. This program included both physical and occupational therapy with a strong focus on exercise. The exercise included cardiovascular training, resistance training and personalized interventions to help with each participant's specific needs. The results of this trial indicated that the participants who received the intervention did not experience an overall improvement in quality of life, compared to those who received usual care during active anticancer treatment. However, they did display greater aerobic power and muscle strength compared to the control group. Six weeks might be not enough time to observe an impact on overall quality of life, as well as the choice of overall quality of life as the primary outcome measure.
Gehring et al. (19) recently conducted a successful pilot RCT exploring the feasibility of a home-based aerobic exercise intervention for people with grade II and III gliomas. The intervention included three aerobic training sessions per week for six months, and a physiotherapist provided individualized exercise prescriptions based on each patient's aerobic fitness. With the help of a sports watch with a heart rate monitor, patients monitored their heart rate and other metrics during their activities, while the physiotherapist regularly monitored the training data. This program featured several features to ensure adherence, such as allowing patients to exercise at home and providing regular guidance from technology and a physiotherapist. The results showed that the intervention was effective in improving physical fitness, with no adverse events reported. Moreover, cognitive test performance showed trends towards better cognitive performance in the exercise group, with differences in favor of the exercise group observed on measures of attentional inhibition, attention span, auditory selective attention, and working memory (20).
2.3. Cognitive therapy
Cognitive dysfunctions are common and debilitating consequences of brain tumors that affect patients' quality of life and daily functioning. The causes of these impairments are complex and depend on tumor characteristics, such as type, location, size, and edema, as well as on the involvement of neural pathways. The most frequently affected cognitive domains are attention (30%) and working memory (20%), followed by visual memory (14%), verbal memory (13%), information processing speed (11%), and executive functioning (8%) (21). The prevalence of cognitive impairment in low-grade glioma varies widely, ranging from 31%–75% before treatment, with higher rates for tumors in the dominant hemisphere (22). Cognitive recovery usually occurs within 3–6 months, but 19%–83% of patients remain impaired (23). Low-grade patients commonly demonstrate cognitive impairments in attention and concentration, processing speed, learning and memory, and executive functions (24). High-grade tumors can cause brain tissue to atrophy, leading to slower or stopped plasticity processes and more disabling deficits in cognitive domains (25). Cognitive rehabilitation interventions can help patients with brain tumors cope with their cognitive impairments and improve their quality of life. Previous studies have shown promising outcomes and high satisfaction levels among patients and their families who received these interventions (26).
This mini-review included two studies with a focus on cognitive rehabilitation, one randomized control trials and one observational study.
Gehring et al. (27) explored the impact of a cognitive rehabilitation program (CRP) on objective and subjective measures of cognitive ability in patients with gliomas in remission. The program consisted of six weekly 2-hour sessions and incorporated both cognitive retraining and compensation training, with a focus on attention in the retraining component and attention, memory, and executive functions in the compensation component. Results showed that self-reported cognitive functioning improved after the intervention and there were distinct differences in attention and verbal memory observed at the 6-month follow-up. The intervention also had a significant effect on long-term mental fatigue scores. However, there was no significant difference between the two groups for self-reported mental health-related quality of life or community integration. Both groups showed improved objective cognitive performance in the short term, but the CRP group demonstrated continued improvement at 6-month follow-up, while the control group did not.
Hassler et al. (28) in a pilot study found that over a 3-month period, patients with glioblastoma improved their attention and memory skills after participating in weekly group training sessions. This training discipline uses exercises to train perception, concentration, attention, memory, retentiveness, verbal memory, and creativity Its goal is to improve cognitive function, maintain functional potential for intellectual and memory abilities, and reactivate any limited capacities. The training environment is stress-free and in a small group setting to also foster social skills development. Special emphasis is placed on training concentration skills and empowering short-term memory, and mnemotechnics are used to help attendees learn new information. Neuropsychological tests revealed improvements in all cognitive functions on a group basis, but individual patients showed both improvement and deterioration in cognitive performance.
3. Discussion
The studies reviewed explore protocols of various rehabilitation interventions for glioma patients. Rehabilitation protocols typically include physical therapy, occupational therapy, psychological support, and cognitive therapies, and the timing of the rehabilitation can vary from early after surgery to weeks after the completion of proper management. The interventions included inpatient, outpatient, and home-based rehabilitation, with varying exercises and therapy components.The studies showed that rehabilitation can lead to improvements in motor function, cognition, activities of daily living, and quality of life, with some studies also demonstrating improvements in physical fitness and cognitive performance. However, it is important to note that the timing, intensity, and duration of rehabilitation may influence its effectiveness. Some studies showed mixed results, highlighting the need for further research in this area. Overall, rehabilitation interventions can play an important role in improving the outcomes and well-being of patients with brain tumors. It is important for healthcare providers to consider rehabilitation as part of the comprehensive care for these patients and to tailor the interventions to individual needs and circumstances. Infact, the interventions with the most successful outcomes were those that included personalized exercise prescriptions, individualized training, and adherence strategies such as monitoring training data and regular guidance from a physiotherapist.
As for the cognitive rehabilitation protocol, the two studies included in this mini-review provide valuable insights into the effectiveness of cognitive rehabilitation interventions for patients with gliomas. Gehring et al. highlights the potential benefits of early cognitive rehabilitation interventions for patients with gliomas in remission; while Hassler et al.'s pilot study also showed promising results, indicating that group training sessions targeting attention and memory skills can lead to improvements in cognitive function, particularly in perception, concentration, and retentiveness. Overall, these studies suggest that cognitive rehabilitation interventions can significantly contribute to improvement in the quality of life of patients with gliomas and should be further explored in larger and more rigorous studies.
It is noteworthy that some studies were excluded because they included other patients besides gliomas. However, they are still relevant for glioma rehabilitation and may offer useful insights. So, we summarized their findings in the discussion section and provided detailed information about their protocols in the Supplementary Material.
Regarding the physical rehabilitation a study by Yoon et al. (29) investigated the potential of combining VR-based rehabilitation with conventional Occupational Therapy (OT) to improve upper extremity function in patients with brain tumors, including glioma. They found that the intervention group showed more improvement in proximal UE function, while the control group experienced better fine motor function and overall coordination. Bartolo et al. (30) also found significant improvements in motor outcomes with a physical therapy intervention after surgical treatment, which included patients with glioma. Beginning soon after surgical treatment, the physical therapy intervention consisted of one hour per day, six days a week, and a protocol of five phases, each lasting 10 to 15 min. These phases passive and active stretch and strengthening exercises, balance, and walking training.
Concerning cognitive rehabilitation, we discovered five studies that incorporated glioma patients as well as those with other brain tumor types. For instance, Zucchella et al. (31) demonstrated the efficacy of cognitive training in post-surgical patients, which suggests that early intervention may be beneficial for improving cognitive function in brain tumor patients. A 16-session program combining direct training and metacognitive training was conducted by psychologists to enhance cognitive abilities. Patients completed computer exercises targeting various cognitive functions and were provided guidance on tasks and metacognitive strategies. Significant improvement in visual attention and verbal memory was observed, suggesting a successful retraining approach to improving cognitive performance. Other cognitive domains may also benefit from improvements in attention. Yang et al. (32) showed that combining virtual reality with computer-assisted cognitive rehabilitation can have positive effects on cognitive improvement in brain tumor patients. Maschio et al. (33) found that cognitive rehabilitation training can improve short-term verbal memory, episodic memory, fluency, and long-term visuospatial memory in patients with brain tumor-related epilepsy and cognitive issues. The cognitive rehabilitation training consisted of 10 weekly individual 1-hour sessions, each led by a trained psychologist, and focused on memory, attention, visuo-spatial functions, language, and reasoning. Richard et al. (34) demonstrated that Goal Management Training, a behavioral intervention combining mindfulness and strategy training, could improve executive functions and functional goal attainment in brain tumours patients. Finally, Van der Linden et al. (35) showed that a tablet-based cognitive rehabilitation program can be effective in improving cognitive performance, cognitive complaints, fatigue, and psychological distress in primary brain tumour patients following neurosurgery.
4. Conclusion
This review shows that rehabilitation interventions, such as physical and cognitive therapies, can enhance quality of life and function in glioma patients. Rehabilitation is a safe, feasible, and well-tolerated option that should be considered for glioma patients. However, more studies are required to clarify the rehabilitation effects on glioma patients, such as finding the best rehabilitation models, assessing motor and cognitive outcomes, choosing the appropriate physical activity strategies, evaluating the long-term training effects, and measuring the influence of motor and cognitive rehabilitation on patient daily life and caregivers. New approaches such as neuromodulation have been proposed as a new strategy to increase the safety of brain tumor resection, promote cortical reorganization and accelerate functional recovery after surgery (36, 37). Investigating the functional connectivity of gliomas to healthy brain regions could help to accurately assess tumor aggressiveness and inform therapeutic and rehabilitation strategies (38, 39). A multidisciplinary approach and powerful collaboration among healthcare professionals, with extensive experience in the area, are essential (40). Future clinical trials are needed to optimize multimodal interventions to mitigate the glioma consequences and provide optimal care to patients.
Author contributions
SS, SF: concept and design. SS: drafting and reviewing the manuscript. SF: literature analysis and manuscript revision. NC, RP, PF and AS: technical support and study supervision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1137516/full#supplementary-material.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 world health organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. (2016) 131(6):803–20. doi: 10.1007/s00401-016-1545-1
2. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. (2021) 2;23(8):1231–51. doi: 10.1093/neuonc/noab106
3. Berger TR, Wen PY, Lang-Orsini M, Chukwueke UN. World health organization 2021 classification of central nervous system tumors and implications for therapy for adult-type gliomas: a review. JAMA Oncol. (2022) 8(10):1493–501. doi: 10.1001/jamaoncol.2022.2844
4. Liu H, Qin X, Zhao L, Zhao G, Wang Y. Epidemiology and survival of patients with brainstem gliomas: a population-based study using the SEER database. Front Oncol. (2021) 11(June):1–7. doi: 10.3389/fonc.2021.692097
5. IJzerman-Korevaar M, Snijders TJ, de Graeff A, Teunissen SCCM, de Vos FYF. Prevalence of symptoms in glioma patients throughout the disease trajectory: a systematic review. J Neurooncol. (2018) 140(3):485–96. doi: 10.1007/s11060-018-03015-9
6. Paw , Mai Chin A, Amika Singh, Saskia te Velde, Maïté Verloigne, Willem van Mechelen, Johannes Brug. Physical activity and sedentary behaviour In youth. In: Routledge Handbook of Youth Sport ed. Ken Green and Andy Smith (Abingdon: Routledge, 07 gen 2016).
7. Gilchrist LS, Galantino ML, Wampler M, Marchese VG, Morris GS, Ness KK. A framework for assessment in oncology rehabilitation. Phys Ther. (2009) 89(3):286–306. doi: 10.2522/ptj.20070309
8. Barcikowski J. Rehabilitation of adult patients with primary brain tumors. Curr Phys Med Rehabil Reports. (2022) 10(2):106–13. doi: 10.1007/s40141-022-00345-8
9. NICE guidelines [NG99]. Brain tumours (primary) and brain metastases in over 16s | Guidance | NICE. NICE Natl Inst Heal Care Excell. 2021;(July 2018):1.3. Available at: https://www.nice.org.uk/guidance/ng99/chapter/recommendations#follow-up-for-glioma
10. Zhao K, Yu C, Gan Z, Huang M, Wu T, Zhao N. Rehabilitation therapy for patients with glioma: a PRISMA-compliant systematic review and meta-analysis. Medicine. (2020) 99(45):e23087. doi: 10.1097/MD.0000000000023087
11. Khan F, Amatya B, Ng L, Drummond K, Galea M. Multidisciplinary rehabilitation after primary brain tumour treatment. Cochrane Database Syst Rev. (2015) 2017(8):CD009509. doi: 10.1002/14651858.CD009509.pub3
12. Amidei C, Kushner DS. Clinical implications of motor deficits related to brain tumors. Neurooncol Pract. (2015) 2(4):179–84. doi: 10.1093/nop/npv017
13. Vargo M, Henriksson R, Salander P. Rehabilitation of patients with glioma. Handb Clin Neurol. (2016) 134:287–304. doi: 10.1016/B978-0-12-802997-8.00017-7
14. Kushner DS, Amidei C. Rehabilitation of motor dysfunction in primary brain tumor patients. Neurooncol Pract. (2015) 2(4):185–91. doi: 10.1093/nop/npv019
15. Yu J, Jung Y, Park J, Kim JM, Suh M, Cho KG, et al. Intensive rehabilitation therapy following brain tumor surgery: a pilot study of effectiveness and long-term satisfaction. Ann Rehabil Med. (2019) 43(2):129–41. doi: 10.5535/arm.2019.43.2.129
16. Tay MRJ, Seah JD, Chua KSG. Long-Term outcomes of patients with primary brain tumors after acute rehabilitation: a retrospective analyses of factors. Life. (2022) 12(8):1–11. doi: 10.3390/life12081208
17. Hansen A, Søgaard K, Minet LR, Jarden JO. A 12-week interdisciplinary rehabilitation trial in patients with gliomas–a feasibility study. Disabil Rehabil. (2018) 40(12):1379–85. doi: 10.1080/09638288.2017.1295472
18. Hansen A, Pedersen CB, Jarden JO, Beier D, Minet LR, Søgaard K. Effectiveness of physical therapy- and occupational therapy-based rehabilitation in people who have glioma and are undergoing active anticancer treatment: single-blind, randomized controlled trial. Phys Ther. (2020) 100(3):564–74. doi: 10.1093/ptj/pzz180
19. Gehring K, Kloek CJJ, Aaronson NK, Janssen KW, Jones LW, Sitskoorn MM, et al. Feasibility of a home-based exercise intervention with remote guidance for patients with stable grade II and III gliomas: a pilot randomized controlled trial. Clin Rehabil. (2018) 32(3):352–66. doi: 10.1177/0269215517728326
20. Gehring K, Stuiver MM, Visser E, Kloek C, Van Den Bent M, Hanse M, et al. A pilot randomized controlled trial of exercise to improve cognitive performance in patients with stable glioma: a proof of concept. Neuro Oncol. (2020) 22(1):103–15. doi: 10.1093/neuonc/noz178
21. Habets EJJ, Hendriks EJ, Taphoorn MJB, Douw L, Zwinderman AH, Vandertop WP, et al. Association between tumor location and neurocognitive functioning using tumor localization maps. J Neurooncol. (2019) 144(3):573–82. doi: 10.1007/s11060-019-03259-z
22. van Kessel E, Baumfalk AE, van Zandvoort MJE, Robe PA, Snijders TJ. Tumor-related neurocognitive dysfunction in patients with diffuse glioma: a systematic review of neurocognitive functioning prior to anti-tumor treatment. J Neurooncol. (2017) 134(1):9–18. doi: 10.1007/s11060-017-2503-z
23. Weyer-Jamora C, Brie MS, Luks TL, Smith EM, Hervey-Jumper SL, Taylor JW. Postacute cognitive rehabilitation for adult brain tumor patients. Neurosurgery. (2021) 89(6):945–53. doi: 10.1093/neuros/nyaa552
24. Weyer-Jamora C, Brie MS, Luks TL, Smith EM, Braunstein SE, Villanueva-Meyer JE, et al. Cognitive impact of lower-grade gliomas and strategies for rehabilitation. Neurooncol Pract. (2021) 8(2):117–28. doi: 10.1093/nop/npaa072
25. Acevedo-Vergara K, Perez-Florez M, Ramirez A, Torres-Bayona S, Dau A, Salva S, et al. Cognitive deficits in adult patients with high-grade glioma: a systematic review. Clin Neurol Neurosurg. (2022) 219(64):107296. doi: 10.1016/j.clineuro.2022.107296
26. Bergo E, Lombardi G, Pambuku A, Della Puppa A, Bellu L, D’avella D, Zagonel V. Cognitive rehabilitation in patients with gliomas and other brain tumors: state of the art. Biomed Res Int. (2016) 2016:3041824. doi: 10.1155/2016/3041824
27. Gehring K, Sitskoorn MM, Gundy CM, Sikkes SAM, Klein M, Postma TJ, et al. Cognitive rehabilitation in patients with gliomas: a randomized, controlled trial. J Clin Oncol. (2009) 27(22):3712–22. doi: 10.1200/JCO.2008.20.5765
28. Hassler MR, Elandt K, Preusser M, Lehrner J, Binder P, Dieckmann K, et al. Neurocognitive training in patients with high-grade glioma: a pilot study. J Neurooncol. (2010) 97(1):109–15. doi: 10.1007/s11060-009-0006-2
29. Yoon J, Chun MH, Lee SJ, Kim BR. Effect of virtual reality-based rehabilitation on upper-extremity function in patients with brain tumor. Am J Phys Med Rehabil. (2015) 94(6):449–59. doi: 10.1097/PHM.0000000000000192
30. Bartolo M, Zucchella C, Pace A, Lanzetta G, Vecchione C, Bartolo M, et al. Early rehabilitation after surgery improves functional outcome in inpatients with brain tumours. J Neurooncol. (2012) 107(3):537–44. doi: 10.1007/s11060-011-0772-5
31. Zucchella C, Capone A, Codella V, De Nunzio AM, Vecchione C, Sandrini G, et al. Cognitive rehabilitation for early post-surgery inpatients affected by primary brain tumor: a randomized, controlled trial. J Neurooncol. (2013) 114(1):93–100. doi: 10.1007/s11060-013-1153-z
32. Yang S, Chun MH, Son YR. Effect of virtual reality on cognitive dysfunction in patients with brain tumor. Ann Rehabil Med. (2014) 38(6):726–33. doi: 10.5535/arm.2014.38.6.726
33. Maschio M, Dinapoli L, Fabi A, Giannarelli D, Cantelmi T. Cognitive rehabilitation training in patients with brain tumor-related epilepsy and cognitive deficits: a pilot study. J Neurooncol. (2015) 125(2):419–26. doi: 10.1007/s11060-015-1933-8
34. Richard NM, Bernstein LJ, Mason WP, Laperriere N, Maurice C, Millar BA, et al. Cognitive rehabilitation for executive dysfunction in brain tumor patients: a pilot randomized controlled trial. J Neurooncol. (2019) 142(3):565–75. doi: 10.1007/s11060-019-03130-1
35. van der Linden SD, Rutten GJM, Dirven L, Taphoorn MJB, Satoer DD, Dirven CMF, et al. Ehealth cognitive rehabilitation for brain tumor patients: results of a randomized controlled trial. J Neurooncol. (2021) 154(3):315–26. doi: 10.1007/s11060-021-03828-1
36. Poologaindran A, Profyris C, Young IM, Dadario NB, Ahsan SA, Chendeb K, et al. Interventional neurorehabilitation for promoting functional recovery post-craniotomy: a proof-of-concept. Sci Rep. (2022) 12(1):1–11. doi: 10.1038/s41598-022-06766-8
37. Ille S, Kelm A, Schroeder A, Albers LE, Negwer C, Butenschoen VM, et al. Navigated repetitive transcranial magnetic stimulation improves the outcome of postsurgical paresis in glioma patients—a randomized, double-blinded trial. Brain Stimul. (2021) 14(4):780–7. doi: 10.1016/j.brs.2021.04.026
38. Sprugnoli G, Rossi S, Rotenberg A, Pascual-Leone A, El-Fakhri G, Golby AJ, et al. Personalised, image-guided, noninvasive brain stimulation in gliomas: rationale, challenges and opportunities. EBioMedicine. (2021) 70:103514. doi: 10.1016/j.ebiom.2021.103514
39. Sprugnoli G, Rigolo L, Faria M, Juvekar P, Tie Y, Rossi S, et al. Tumor BOLD connectivity profile correlates with glioma patients' survival. Neurooncol Adv. (2022) 4(September):1–12. doi: 10.1093/noajnl/vdac153
Keywords: glioma, brain tumor, rehabilitative care, physical therapy, cognitive theraphy, rehabilitation interventions
Citation: Spina S, Facciorusso S, Cinone N, Pellegrino R, Fiore P and Santamato A (2023) Rehabilitation interventions for glioma patients: a mini-review. Front. Surg. 10:1137516. doi: 10.3389/fsurg.2023.1137516
Received: 4 January 2023; Accepted: 6 April 2023;
Published: 16 June 2023.
Edited by:
Francesco Carbone, Städtisches Klinikum Karlsruhe, GermanyReviewed by:
Giada Cangemi, University of Messina, ItalyFederica Morelli, University of Bari Aldo Moro, Italy
Tracy L. Luks, University of California, United States
Khawaja Muthammir Hassan, Mayo Hospital, Pakistan
© 2023 Spina, Facciorusso, Cinone, Pellegrino, Fiore and Santamato. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Salvatore Facciorusso cy5mYWNjaW9ydXNzbzg5QGdtYWlsLmNvbQ==
 Stefania Spina
Stefania Spina Salvatore Facciorusso
Salvatore Facciorusso Nicoletta Cinone1
Nicoletta Cinone1 Andrea Santamato
Andrea Santamato