- 1Department of Sports Injury and Arthroscopy, Tianjin Hospital, Tianjin University, Tianjin, China
- 2Medical School of Tianjin University, Tianjin University, Tianjin, China
Arthroscopic management of scapular glenoid fractures caused by electrical injury represents an innovative approach for complex shoulder trauma involving both osseous and soft tissue damage. This technique uniquely combines the double-pulley system with a 3.0-mm double-suture anchor bridge fixation, allowing for smaller incisions and reduced surgical trauma. We report, for the first time, an arthroscopic case of comminuted anteroinferior glenoid fracture resulting from electrocution. A 53-year-old man presented with left shoulder dysfunction 8 days after electrical injury. CT and MRI revealed a comminuted glenoid fracture, a non-displaced greater tuberosity fracture, and a partial supraspinatus tear. Arthroscopic anchor fixation achieved anatomic reduction of the glenoid fragment without intraoperative complications, while the greater tuberosity fracture and rotator cuff injury were managed conservatively. At 15-month follow-up, the patient was pain-free (VAS score 0) with full shoulder function (Constant score 95, ASES score 94), and CT confirmed satisfactory glenohumeral congruency. This case demonstrates the technical feasibility of arthroscopic treatment for high-energy electrical shoulder trauma, with advantages of minimizing soft tissue disruption and reducing the risk of postoperative stiffness, though further studies are needed to validate long-term outcomes.
Introduction
In developed countries, electrical injuries account for approximately 3%–5% of all burn cases, whereas in developing countries the incidence is as high as 21%–27% (1–3). Fractures caused by electrocution are rare and usually result from either tetanic muscle contractions or falls secondary to the injury. Although previous reports have described vertebral compression fractures and posterior shoulder dislocations following electroconvulsive therapy or accidental electric shock (4–6), anterior glenoid fractures secondary to electrocution remain exceedingly uncommon.
Tarquinio et al. (7) first reported a case of bilateral scapular fractures after low-voltage electrical injury, attributing to forceful contractions of the shoulder muscles. Subsequent studies by Beswick et al. (8) and Dumas et al. (9) further emphasized the role of intense tetanic contraction in scapular fractures occurring without direct trauma. However, most of these reports focused on isolated scapular body fractures. Accordingly, the commonly recognized injury pattern after electrocution involves posterior muscle contraction leading to posterior shoulder dislocation, posterior glenoid rim fractures, or scapular body fractures (10).
It is noteworthy that the most frequent upper limb injury after electrical trauma is posterior fracture-dislocation of the proximal humerus (6, 11, 12). In contrast, the present patient sustained a rare combination of a comminuted anteroinferior glenoid fracture with a concomitant nondisplaced greater tuberosity fracture. This injury pattern poses diagnostic challenges, for which computed tomography (CT) and magnetic resonance imaging (MRI) are critical in detecting comminuted glenoid fractures and associated soft tissue injuries.
This research reports a case of comminuted anteroinferior glenoid fracture following electrical injury, which to our knowledge represents the first successful arthroscopic management of an electrocution-related glenoid fracture. The concomitant nondisplaced greater tuberosity fracture and partial rotator cuff tear were treated conservatively. This case highlights the complexity of shoulder injuries induced by electrical trauma and introduces a novel minimally invasive surgical option for their management.
Presentation of case
A 53-year-old man sustained an electrical injury while bending over to touch a generator, with an estimated contact time of 3–5 s. He reported sharp, burning pain in the left upper arm and shoulder, followed by numbness, restricted mobility, local swelling, and tenderness several hours later. He was unable to actively elevate the left arm. No chest pain, palpitations, or trauma from falling were reported. Eight days of post-injury, he presented to our clinic. Physical examination revealed no obvious shoulder deformity but marked tenderness over the coracoid process, greater tuberosity, and bicipital groove. Active/passive ranges of motion were as follows: forward flexion 45°/90°, extension 10°/20°, adduction 10°/20°, abduction 40°/70°, and internal rotation to the lateral thigh. Radial and ulnar pulses were intact, with preserved sensation and muscle strength in all extremities. Electrocardiography, chest radiography, and routine blood tests were within normal limits.
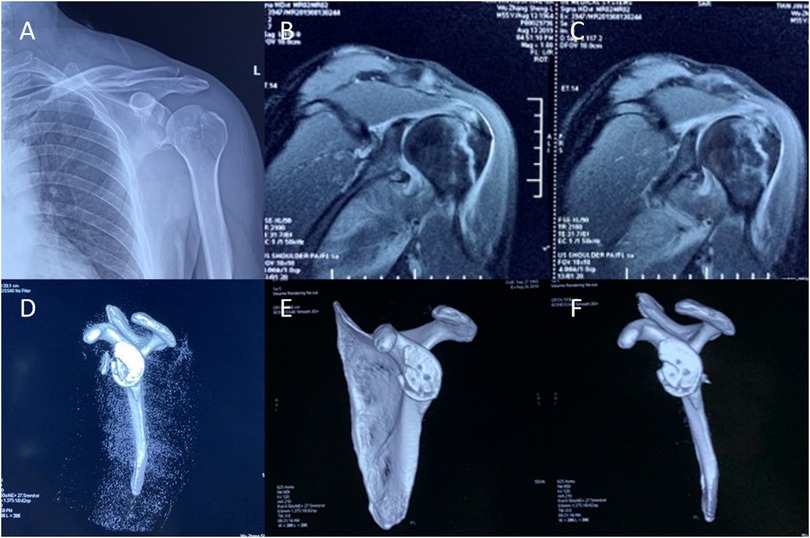
Radiographic and MRI evaluation identified a nondisplaced fracture of the left greater tuberosity (Figure 1A) and a fracture involving the anteroinferior glenoid rim with associated labral involvement (Figures 1B,C). MRI additionally revealed a partial tear of the supraspinatus tendon. CT confirmed the greater tuberosity fracture and demonstrated a comminuted anteroinferior glenoid fracture (Figure 1D). Preoperatively, the patient's pain score was 9 on the Visual Analog Scale (VAS scale), with a Constant-Murley Score (Constant score) of 33 and an American Shoulder and Elbow Surgeons Standardized Shoulder Assessment (ASES score) of 13.
Surgery procedure
The patient was positioned in the lateral decubitus position with longitudinal traction applied, and preoperative manipulation restored normal range of motion to the left shoulder. Following standard aseptic preparation and draping, anatomical landmarks including the acromion, coracoid process, and acromioclavicular joint were marked. Standard posterior, anterosuperior, and anteroinferior portals were established. Arthroscopic examination identified a displaced anteroinferior glenoid rim fracture, with a free bone fragment displaced anterior to the glenoid cavity. Notably, the labral structure remained intact without tearing (Figure 2A).
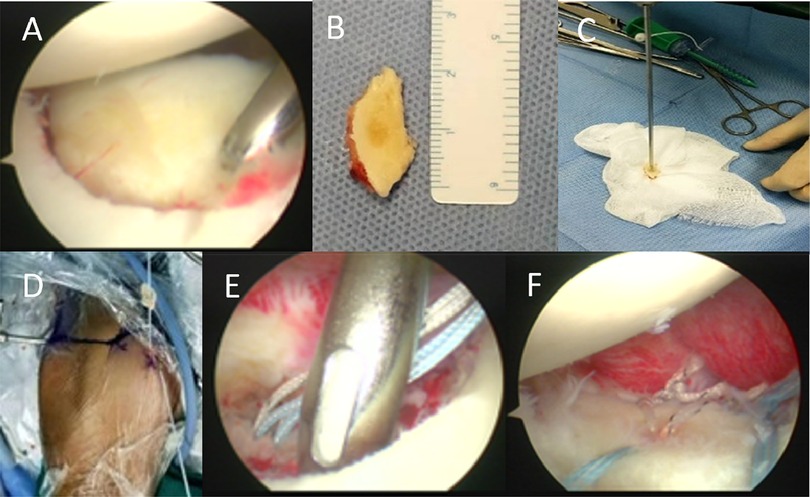
Figure 2. Several major key points in the patient's surgery. (A) Compare the size of the bone defect. (B) Measure the dimensions of the bone fragment. (C) Drill a hole in the center of the bone fragment. (D) Reduce the bone fragment into the joint. (E,F) Surgical fixation of the bone fragment.
After debridement of the fracture site, the free fragment was visualized, preserving its intact labral attachment. Reduction attempts revealed inadequate stability for direct intra-articular fixation. Consequently, the fragment was extracted and measured as 2 cm (length) × 1.5 cm (width) × 0.5 cm (thickness) (Figure 2B). A central drill hole was created in the fragment for subsequent fixation (Figure 2C). Two 3.0-mm double-threaded anchors (Arthrex, Munich, Germany) were implanted at the anteroinferior and central aspects of the glenoid bone bed. Sutures from the central anchor were passed through the pre-drilled hole to reduce the fragment into the joint (Figure 2D). The anteroinferior portion of the fragment was secured using a double pulley technique, while two blue sutures in a suture bridge configuration provided additional stabilization from the anterosuperior and posteroinferior directions (Figures 2E,F). Intraoperative stability testing confirmed rigid fixation.
Postoperative rehabilitation protocol and follow-up results
Postoperatively, the arm was immobilized with a shoulder sling for 6 weeks to protect the glenohumeral fixation site and facilitate fracture healing. During weeks 1–2, gentle pendulum (Codman) exercises were initiated, avoiding any active shoulder muscle contraction. From weeks 3–6, gradual passive and active-assisted range-of-motion exercises were introduced in forward flexion (scapular plane) and external rotation (with the arm at the side), limited to a comfortable range. Combined abduction–external rotation movements that could stress the anterior repair were strictly avoided. At week 6, the sling was discontinued, and isometric strengthening of the rotator cuff and deltoid muscles was initiated. Between 3 and 6 months, progressive resistance training with elastic bands was performed, targeting internal rotation, external rotation, abduction, and forward flexion. From 6 months onward, advanced strengthening focused on power and endurance.
CT at 6 months demonstrated satisfactory alignment and healing of the glenohumeral fracture (Figures 1E,F). At 15-month follow-up, the patient reported complete resolution of shoulder pain, with restored range of motion. Clinical scores were markedly improved: VAS 0, Constant score 95, and ASES score 94. Imaging confirmed postoperative healing changes in the left glenoid fossa fracture—with good bone repair and a relatively regular shape.
Discussion
Cases of shoulder fractures caused by electrical injury are rare, with only a few reports available in the literature (Table 1). In the present case, the patient underwent arthroscopic fixation of the glenoid fragment using suture anchors, while the nondisplaced greater tuberosity fracture and partial rotator cuff tear were treated conservatively. At 15 months postoperatively, the shoulder remained stable with full range of motion, excellent functional scores, and imaging confirming well-aligned fracture healing with satisfactory morphology.
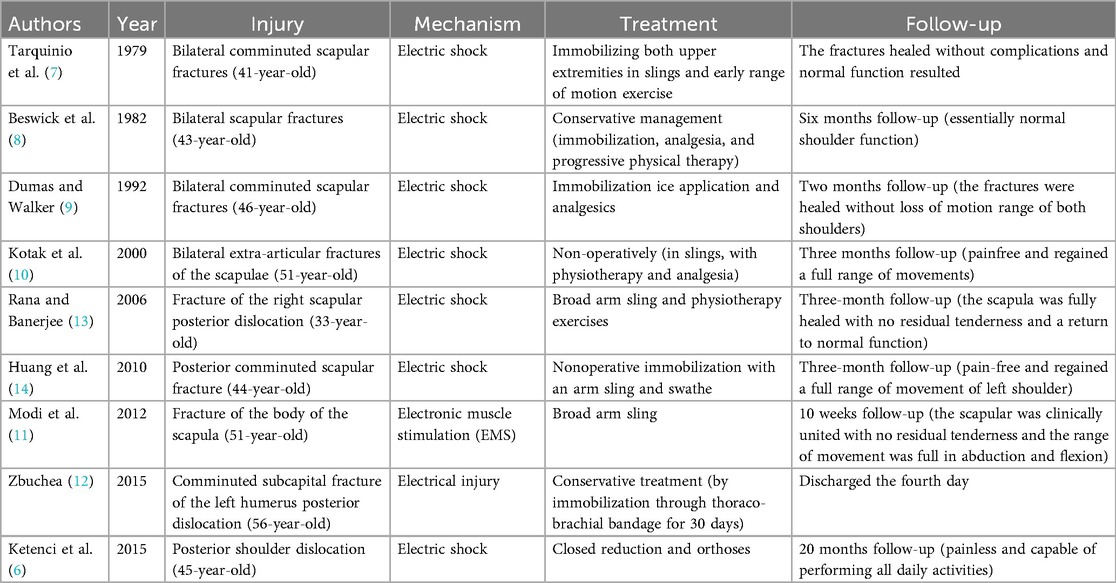
Table 1. List of publications describing shoulder fractures resulting from electric shock (electrical injury related).
The mechanism of fracture after electrocution is generally attributed to involuntary tetanic muscle contraction or secondary trauma from falls. Notably, the most commonly reported shoulder injuries following electrical trauma are posterior dislocations and posterior fractures. This pattern has been explained by the powerful contraction of muscles such as the infraspinatus, teres minor, and deltoid, which force the humeral head upward and posteriorly against the acromion, resulting in posterior glenoid rim injuries (11, 13, 15). Some authors have suggested that electrocution predominantly leads to posterior dislocation, whereas anterior dislocations are usually trauma related (16). In our case, however, the patient sustained a comminuted anteroinferior glenoid fracture without posterior dislocation or posterior involvement, despite the absence of additional trauma. This discrepancy may be explained by the arm position or the activation pattern of specific muscle groups at the time of injury. Specifically, the patient's arm was in forward flexion, adduction, and internal rotation when touching the generator. In this position, contact between the humeral head and glenoid is reduced and shifted toward the anteroinferior rim. The electric shock may therefore have reproduced a mechanism similar to anterior dislocation, leading to the observed glenoid fracture. The associated greater tuberosity fracture could also be linked to this anterior-dislocation–like mechanism, as such fractures occur in approximately 10% of shoulder dislocations (17). Nonetheless, we believe that the tuberosity fracture more likely resulted from avulsion due to sudden contraction of the infraspinatus, teres minor, and deltoid. Because the fracture was nondisplaced, no acute rotator cuff tear was observed; the partial cuff lesion detected on MRI was likely chronic. The greater tubercle fracture shows no displacement and is inherently stable. Furthermore, the rotator cuff injury is a partial tear, and the rotator cuff tendons can maintain the greater tubercle fragment in a favorable position. Therefore, under conservative immobilization of the shoulder joint, greater tubercle fractures have a high likelihood of healing (18). Since the rotator cuff injury is a partial tear rather than a “full-thickness tear,” conservative treatment is typically employed (19).
Importantly, scapular fractures caused solely by electrocution in the absence of direct trauma are exceptionally rare. Heggland et al. (20) described bilateral anterior glenoid rim fractures with anterior dislocations of both humeral heads, though that case resulted from sports trauma rather than electrical injury. Our case is consistent with earlier reports by Tarquinio et al. (7) and Kotak et al. (10), demonstrating that electrocution alone can induce shoulder fractures without concomitant falls. Interestingly, unlike the humeral head displacement commonly described by Ketenci et al. (6) in electrical injuries, our patient showed no posterior dislocation, again suggesting the role of limb positioning and muscle activation pattern during the incident.
This case also illustrates the diagnostic challenges of such injuries. Initial radiographs revealed only a nondisplaced fracture, whereas CT and MRI were required to detect the comminuted glenoid fracture and partial supraspinatus tear. This finding aligns with Beswick et al. (8), who emphasized that scapular fractures may be overlooked without high clinical suspicion and detailed imaging, underscoring the importance of advanced radiological assessment in electrical injuries.
When fractures are limited to the scapular body, conservative treatment—immobilization followed by early mobilization—is generally recommended. Surgical intervention is indicated for displaced intra-articular fractures of the glenoid, glenoid fractures associated with dislocation, coracoid fractures with acromioclavicular disruption, or fractures with neurovascular compromise (9). Most previously reported electrocution-related scapular fractures involved the body and were treated nonoperatively (Table 1). In contrast, our patient presented with a displaced comminuted glenoid fracture, which required surgery. Unlike the open reduction and screw fixation used by Heggland et al. (20), we performed arthroscopic fixation. Arthroscopy allowed direct visualization of intra-articular fragments, precise reduction, and stable fixation using suture anchors. The combination of the double-pulley and suture-bridge techniques provided multidirectional stability and minimized the risk of fragment displacement, a critical concern for long-term outcomes. Although plate-screw constructs may offer superior biomechanical strength (21), arthroscopy offers the advantage of minimal soft tissue trauma. More importantly, our patient achieved excellent clinical and radiological outcomes at 15 months, with satisfactory bone healing and restoration of glenoid morphology. These results reflect both the effectiveness of the surgical technique and the patient's adherence to rehabilitation.
Despite the favorable outcome in this case, it represents only a single report of arthroscopic management for an electrocution-induced glenoid fracture. Further studies with larger cohorts and diverse etiologies of glenoid fractures are needed to validate the efficacy and long-term benefits of this minimally invasive approach.
Conclusion
This case likely involved an anterior shoulder dislocation caused by an electric shock injury, subsequently leading to an avulsion fracture of the anterior inferior glenoid and greater tubercle. Conservative management was applied for the greater tubercle fracture and the chronic partial rotator cuff tear, while the glenohumeral bone fragment was repositioned using arthroscopic suture anchor fixation. This approach offers a minimally invasive surgical strategy for bone and joint trauma associated with electrical injuries. The arthroscopic double pulley technique combined with suture bridge technique achieved anatomical reduction and multidirectional stabilization of the intra-articular fracture fragments. This case demonstrates that applying arthroscopic precision repair techniques to shoulder fractures caused by electrical injury can overcome the limitations of traditional conservative treatment, particularly for comminuted fractures involving articular surfaces, while avoiding large surgical incisions and extensive wound sites. Thus, arthroscopically assisted suture anchor fixation represents a novel minimally invasive treatment option for shoulder fractures resulting from electrical injuries. Further studies are needed to validate the applicability of this surgical strategy in complex intra-articular fractures caused by electrical trauma.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of Tianjin University Tianjin Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZZ: Writing – original draft, Writing – review & editing. BM: Investigation, Writing – review & editing. WL: Investigation, Writing – review & editing. QW: Investigation, Methodology, Writing – review & editing. JC: Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Research Project of Tianjin Municipal Education Commission (Grant numbers 2022YGYB01) and Tianjin Science and Technology-Tianjin Natural Science Foundation (Grant numbers 24JCYBJC01350).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1662146/full#supplementary-material
References
1. Tredget EE, Shankowsky HA, Tilley WA. Electrical injuries in Canadian burn care. Identification of unsolved problems. Ann N Y Acad Sci. (1999) 888(1):75–87. doi: 10.1111/j.1749-6632.1999.tb07943.x
2. Cheng PT, Lee CE, Yang JY. Electrical injury–clinical report of 67 cases. Changgeng Yi Xue Za Zhi. (1994) 17(3):220–5.7954000
3. Maghsoudi H, Adyani Y, Ahmadian N. Electrical and lightning injuries. J Burn Care Res. (2007) 28(2):255–61. doi: 10.1097/BCR.0B013E318031A11C
4. Luccarelli J, Henry ME, McCoy TH. Quantification of fracture rate during electroconvulsive therapy (ECT) using state-mandated reporting data. Brain Stimul. (2020) 13(3):523–4. doi: 10.1016/j.brs.2019.12.007
5. Andrade C. Skeletal and dental fractures associated with electroconvulsive therapy. J Clin Psychiatry. (2023) 84(1):23f14797. doi: 10.4088/JCP.23f14797
6. Ketenci IE, Duymus TM, Ulusoy A, Yanik HS, Mutlu S, Durakbasa MO. Bilateral posterior shoulder dislocation after electrical shock: a case report. Ann Med Surg. (2015) 4(4):417–21. doi: 10.1016/j.amsu.2015.10.010
7. Tarquinio T, Weinstein ME, Virgilio RW. Bilateral scapular fractures from accidental electric shock. J Trauma. (1979) 19(2):132–3. doi: 10.1097/00005373-197902000-00014
8. Beswick DR, Morse SD, Barnes AU. Bilateral scapular fractures from low-voltage electrical injury. Ann Emerg Med. (1982) 11(12):676–7. doi: 10.1016/S0196-0644(82)80264-3
9. Dumas JL, Walker N. Bilateral scapular fractures secondary to electrical shock. Arch Orthop Trauma Surg. (1992) 111(5):287–8. doi: 10.1007/BF00571527
10. Kotak BP, Haddo O, Iqbal M, Chissell H. Bilateral scapular fractures after electrocution. J R Soc Med. (2000) 93(3):143–4. doi: 10.1177/014107680009300310
11. Modi BN, Machin JT, Tudor F, Peckham T. Scapular fracture following electronic muscle stimulation. J Surg Case Rep. (2012) 2012(1):4. doi: 10.1093/jscr/2012.1.4
12. Zbuchea A. Humeral neck fracture after electrocution - case report and literature review. Chirurgia. (2015) 110(5):490–2.26531798
13. Rana M, Banerjee R. Scapular fracture after electric shock. Ann R Coll Surg Engl. (2006) 88(2):3–4. doi: 10.1308/147870806X95203
14. Huang W-C, Chiu Y-H, How C-K, Chen J-D, Lam C. Posterior comminuted scapular fracture induced by a low-voltage electric shock. Am J Emerg Med. (2010) 28(9):1060.e3–4. doi: 10.1016/j.ajem.2010.01.026
15. Stone N, Karamitopoulos M, Edelstein D, Hashem J, Tucci J. Bilateral distal radius fractures in a 12-year-old boy after household electrical shock: case report and literature summary. Case Rep Med. (2014) 2014:1–5. doi: 10.1155/2014/235756
16. Meena S, Saini P, Singh V, Kumar R, Trikha V. Bilateral anterior shoulder dislocation. J Nat Sci Biol Med. (2013) 4(2):499–501. doi: 10.4103/0976-9668.117003
17. Gleeson AP. Anterior glenohumeral dislocations: what to do and how to do it. J Accid Emerg Med. (1998) 15(1):7–12. doi: 10.1136/emj.15.1.7
18. Wang F, Niu X, Xia H, Liang W, Hu Z, Lan J. Novel calcaneal plate versus traditional philos plate for treating split fractures of humeral greater tuberosity. Front Surg. (2024) 10:1272887. doi: 10.3389/fsurg.2023.1272887
19. Sciarretta FV, Moya D, List K. Current trends in rehabilitation of rotator cuff injuries. SICOT J. (2023) 9:14. doi: 10.1051/sicotj/2023011
20. Heggland EJH, Parker RD. Simultaneous bilateral glenoid fractures associated with glenohumeral subluxation/dislocation in a weightlifter. Orthopedics. (1997) 20(12):1180–4. doi: 10.3928/0147-7447-19971201-14
Keywords: electrical shock injury, glenoid fracture, arthroscopic technique, fracture fixation, case report
Citation: Zhang Z, Meng B, Li W, Wang Q and Cao J (2025) Arthroscopic management of comminuted fracture of the scapular glenoid secondary to electrical shock injury: a case report and literature review. Front. Surg. 12:1662146. doi: 10.3389/fsurg.2025.1662146
Received: 8 July 2025; Accepted: 22 September 2025;
Published: 3 October 2025.
Edited by:
Farid Amirouche, University of Illinois Chicago, United StatesReviewed by:
Philipp Zehnder, Technical University of Munich, GermanyShota Hoshika, Funabashi Orthopaedic Hospital, Japan
Copyright: © 2025 Zhang, Meng, Li, Wang and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiangang Cao, bWVkaWNhbF96ejExMDJAdGp1LmVkdS5jbg==
†These authors have contributed equally to this work
‡ORCID:
Jiangang Cao
orcid.org/0009-0008-2528-5686
 Zi Zhang1,2,†
Zi Zhang1,2,† Jiangang Cao
Jiangang Cao