- Laboratory of Veterinary Internal Medicine, School of Veterinary Medicine, Faculty of Veterinary Science, Nippon Veterinary and Life Science University, Tokyo, Japan
In recent years, hypertrophic cardiomyopathy (HCM) in cats has become much more common in clinical practice due to improvements in diagnostic techniques and equipment performance. One phenotype is obstructive HCM with left ventricular (LV) outflow tract obstruction (DLVOTO). It has been reported that the presence or absence of DLVOTO does not affect long-term prognosis in cats with HCM. In this study, we evaluated and compared myocardial function in HCM-affected cats with and without DLVOTO using the two-dimensional speckle-tracking echocardiography. LV longitudinal strain of the endocardial, epicardial, and whole layer and LV circumferential strain of the epicardium were significantly decreased in all HCM-affected cats compared to healthy cats. However, these values were not significantly different between those with and without DLVOTO. In contrast, the endocardial and whole layers of LV circumferential strain were only significantly decreased in HCM-affected cats with DLVOTO compared to healthy cats. This could be attributed to the fact that the LV pressure load associated with DLVOTO affected the endocardial myocardium more in the LV endocardial layer, and that lower values of LV endocardial strain lowered the values of LV strain in the whole layer. In conclusion, our results suggest that LV myocardial function may have been more compromised in the HCM-affected cats with DLVOTO.
1. Introduction
Hypertrophic cardiomyopathy (HCM) in the cat is a cardiac disease that is frequently encountered in the clinical practice. HCM is characterized by myocardial hypertrophy and its phenotype is diverse. The prognosis of cats with HCM also varies from asymptomatic cases to cats with congestive heart failure even at a young age (1–5). One phenotype, systolic anterior motion of the mitral valve leaflet, is an event in which the tip of the mitral valve septal apex is pulled toward the aortic outflow tract during systole. This event involved in mitral regurgitation, as well as dynamic left-ventricular (LV) outflow-tract obstruction (DLVOTO), which results in pressure overload in the left ventricle (6). DLVOTO causes an increased left ventricular pressure, which leads to increased wall stress and myocardial ischemia (7). The presence of DLVOTO in humans aggravates the pathogenesis of HCM and is a poor prognostic factor (8); however, it has been reported that the presence or absence of DLVOTO in feline HCM does not affect the long-term prognosis (4).
Recently, two-dimensional speckle-track echocardiography (2D-STE) has been widely performed to evaluate HCM in cats and humans (9–14). 2D-STE studies in cats with HCM have shown that assessment of segmental radial and circumferential deformities in systole (12) and torsion (14), as well as diastolic deformities (12, 13), can be helpful in distinguishing cats with HCM from healthy cats.
Therefore, we hypothesized that myocardial function in HCM-affected cats with DLVOTO (HOCM) would be decreased compared to HCM-affected cats without DLVOTO (HNCM). This study aimed to analyze myocardial function using 2D-STE and compared the results between the HNCM and HOCM.
2. Materials and methods
A prospective cross-sectional design was used in this study. This study was conducted in accordance with our institution’s guidelines (Guidelines for the Care and Use of Animals at Nippon Veterinary and Life Science University) and was approved by the university’s ethics committee (approval number: R2-4). With prior informed consent and agreement, all cat owners participated in the study.
2.1. Animals
Sixty-seven client-owned cats (healthy cats: n = 16; HCM-affected cats: n = 51) were included in this study. All cats underwent a physical examination, blood pressure measurement, electrocardiogram, chest radiograph and echocardiography. The cats classified as healthy cats had no abnormal findings on these examinations. Some HCM-affected cats were already on medication. No history of medication, cardiac disease, or clinical signs were noted in the other cats. The diagnosis of HCM was made by confirming LV hypertrophy on echocardiography and excluding diseases that might cause LV hypertrophy. LV hypertrophy was defined as LV wall thickness ≥ 6 mm at end-diastole as evaluated by echocardiography. LV wall thickening was confirmed using LV short-axis images averaged over three consecutive heartbeats (15). The following previously reported criteria were used to diagnose HOCM: Peak LV outflow-tract velocity (LVOT Vmax) > 2.5 m/s and systolic anterior motion of mitral valve leaflet on B-mode (14, 16). Other cardiomyopathies were ruled out by checking for normal to near-normal LV systolic function using allometric scaling, referring to previous reports (17, 18). Cats with suspected dehydration, hypertension (Systolic blood pressure greater than 160 mmHg), or other cardiovascular or systemic disease were excluded.
2.2. Echocardiography
Conventional echocardiography was performed by experienced researchers using Vivid E95 echocardiography scanner and 12 MHz transducer (GE Healthcare, Tokyo, Japan). During the examination, the lead II electrocardiogram was concurrently acquired and monitored on the screen. Holding during echocardiography was performed with an assisting human hand, and all cats were not sedated. Data were obtained for at least 5 heartbeats. Analysis of the echocardiographic data was performed on a separate day from the acquisition of the images by one researcher using an offline workstation (EchoPAC PC, version 204, GE Healthcare, Tokyo, Japan). The left atrial-to-aortic diameter ratio was measured in the right parasternal short-axis view at the level of basal heart. The end-diastolic interventricular septal thickness (IVSd), LV end-diastolic posterior wall thickness (LVPWd), LV end-diastolic internal diameter (LVIDd), LV end-systolic internal diameter, and fractional shortening were measured in the right parasternal short-axis view at the level of the chordae tendineae. Relative LV wall thickness (RWT) was calculated using the following formula:
Trans-mitral inflow in the left apical four-chamber view was measured by pulsed-wave Doppler, and the peak velocities of the early diastolic wave (E-wave) and late diastolic wave (A-wave) were determined. The E-wave to A-wave velocity ratio (E/A) was also calculated. In the case of fusion of E- and A-waves, values for cases containing these waves were excluded.
2.3. Two-dimensional speckle-tracking echocardiography
An overview of the 2D-STE analysis for cats has been previously described (9, 14, 15, 19, 20). 2D-STE analysis is performed using high-quality images obtained from conventional echocardiography. For evaluation of LV myocardial deformation, images of the left ventricle at the level of the papillary muscle were acquired in the right parasternal short-axis view and the left apical four-chamber view. Left apical four-chamber view images modified for right heart measurements were also obtained to analyze right myocardial deformations (21). Longitudinal and circumferential systolic strain peaks (SL and SC, respectively) were obtained in the endocardium, the entire layer, and the epicardium of the LV (LV-SL and LV-SC, respectively) (21). SC was measured at the papillary muscle level of the LV (14, 22). The endocardial-to-epicardial strain ratio (Endo/Epi), which is believed to reflect compensatory mechanisms of cardiac function in patients with HCM, was also calculated (23, 24). Previous studies have shown observer variability in 2D-STE analysis in our laboratory (14, 19–21).
2.4. Statistical analysis
Variables in each table are expressed as mean ± standard deviation values. Commercially available software (R 2.8.1; https://www.r-project.org/) was used for statistical analyses. One-way analysis of variance followed by Tukey’s multiple comparison test for normally distributed data or Kruskal–Wallis test followed by Steel–Dwass test for non-normally distributed data was used to compare continuous variables between groups. The significance level was set at p < 0.05.
3. Results
3.1. Demographic data
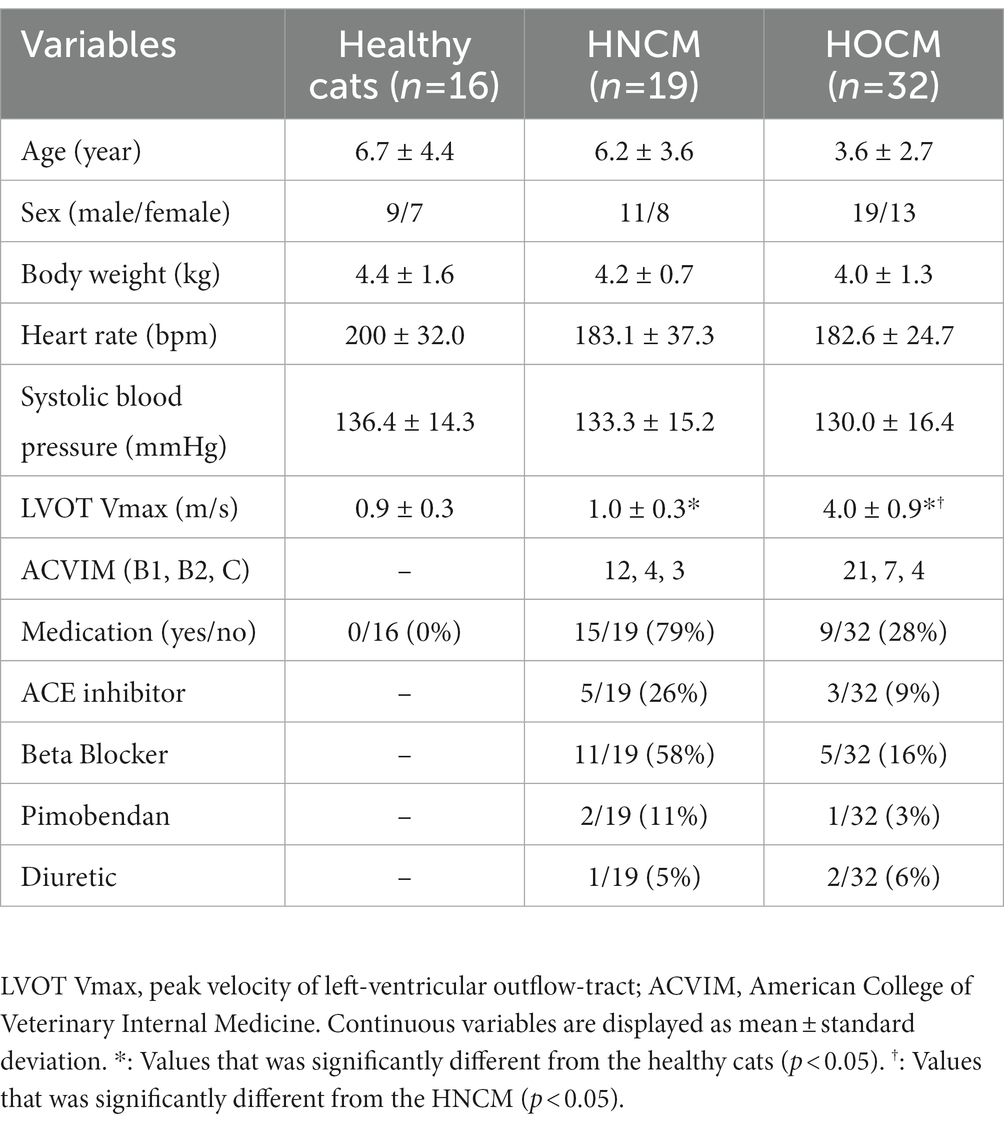
Data regarding demographic characteristics and physical examination results are summarized in Table 1. Nineteen of the 51 cats with HCM belonged to the HNCM, while the remaining 32 belonged to the HOCM. There were no significant differences in age, weight, heart rate, or blood pressure between the two groups. There were significant differences in LVOT Vmax between healthy cats and the HNCM, healthy cats and the HOCM, and the HNCM and HOCM.
3.2. Echocardiography
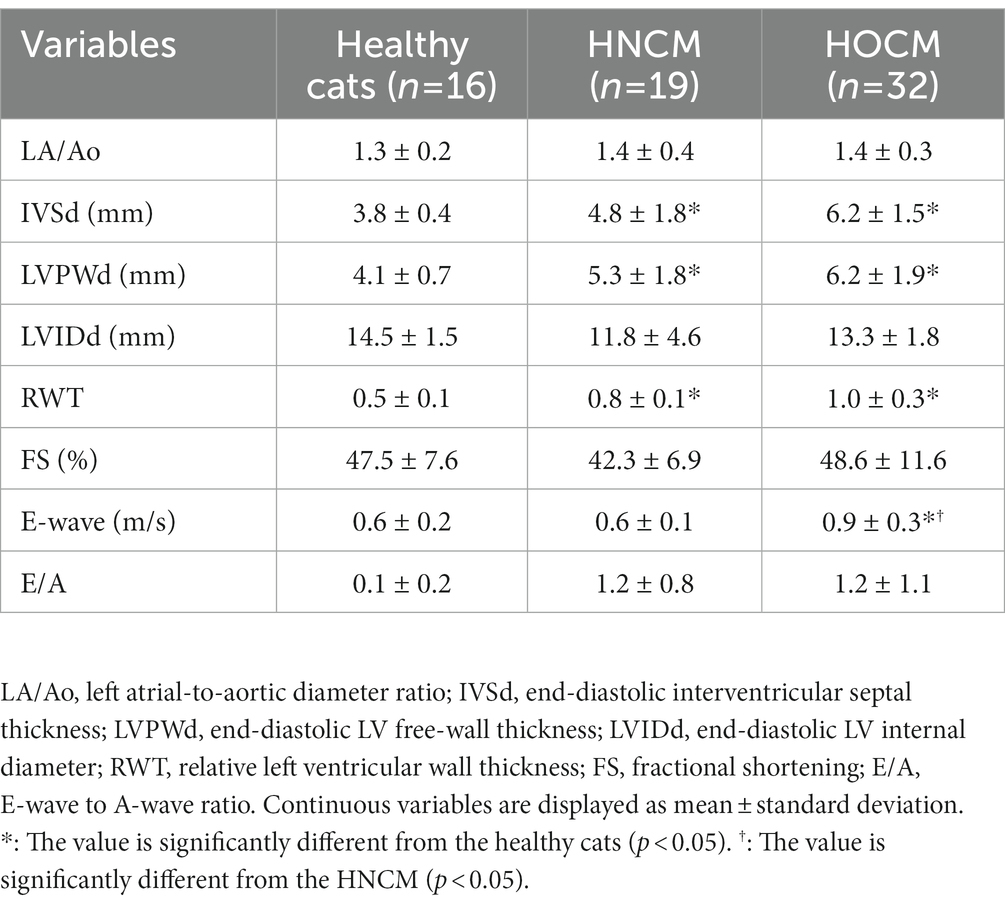
The echocardiographic variable data are summarized in Table 2. IVSd, LVPWd, and RWT were significantly higher in the HNCM and HOCM than in healthy cats (all p < 0.01). E-wave velocity of the HOCM was increased compared to healthy cats and HNCM (p < 0.05). E-wave and E/A analyses were partially excluded because of waveform fusion in some cases.
3.3. Two-dimensional speckle-tracking echocardiography
The 2D-STE results are summarized in Table 3. Representative results of the 2DSTE method in the endocardium are shown in Figure 1. In addition, box-and-whisker diagrams of the LV-SL and LV-SC are also shown in Figures 2, 3, respectively. The LV-SL of whole layer was significantly decreased in the HNCM and HOCM compared to healthy cats (p < 0.05). There was no significant difference in LV-SL in any layer between the HNCM and HOCM. LV-SC in the epicardium was significantly decreased in the HNCM and HOCM compared to healthy cats (both p < 0.01). LV-SC in the HOCM of the endocardium and whole layers were decreased compared to healthy cats (p = 0.01, p < 0.01 respectively). There was no significant difference in LV-SC in any layer between the HNCM and HOCM. The LV-SL Endo/Epi was increased in the HNCM and HOCM compared to healthy cats (p < 0.01, p = 0.02 respectively). In comparison, there was no significant difference in LV-SC Endo/Epi between the HNCM and HOCM.
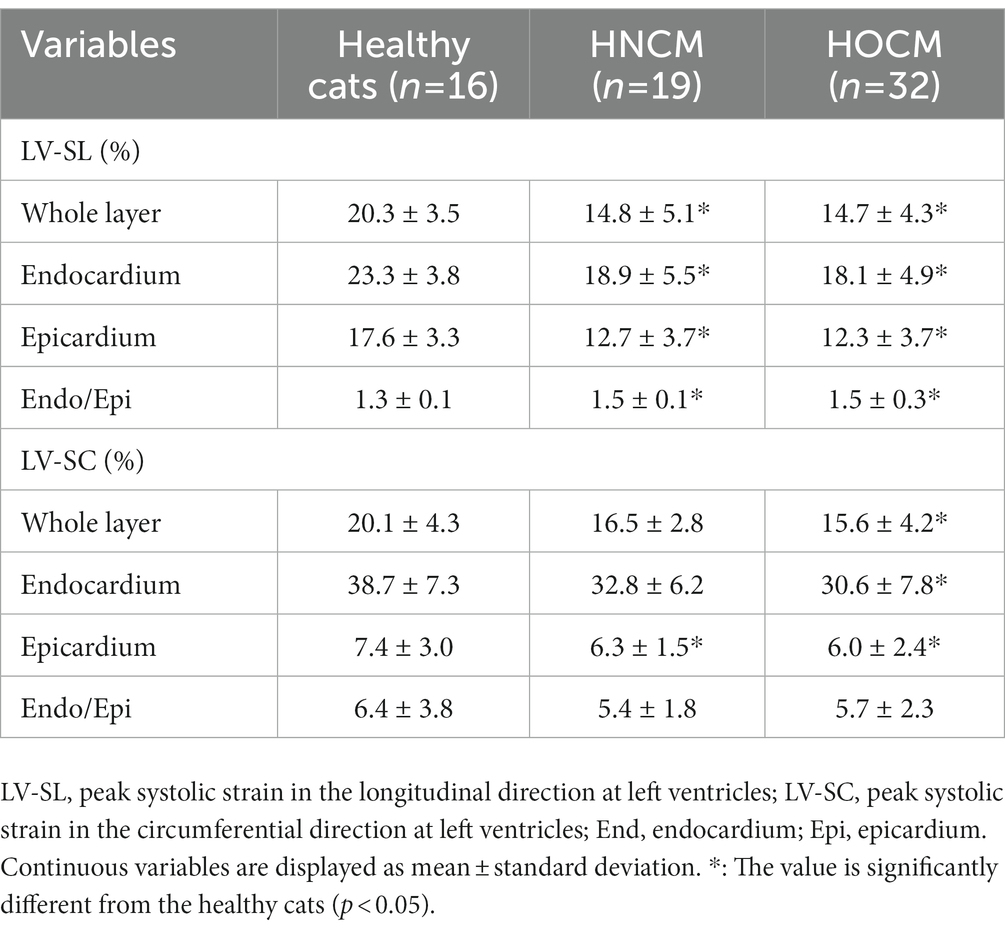
Table 3. Strain assessed by two-dimensional speckle tracking echocardiography in healthy cats and cats with cardiomyopathy.
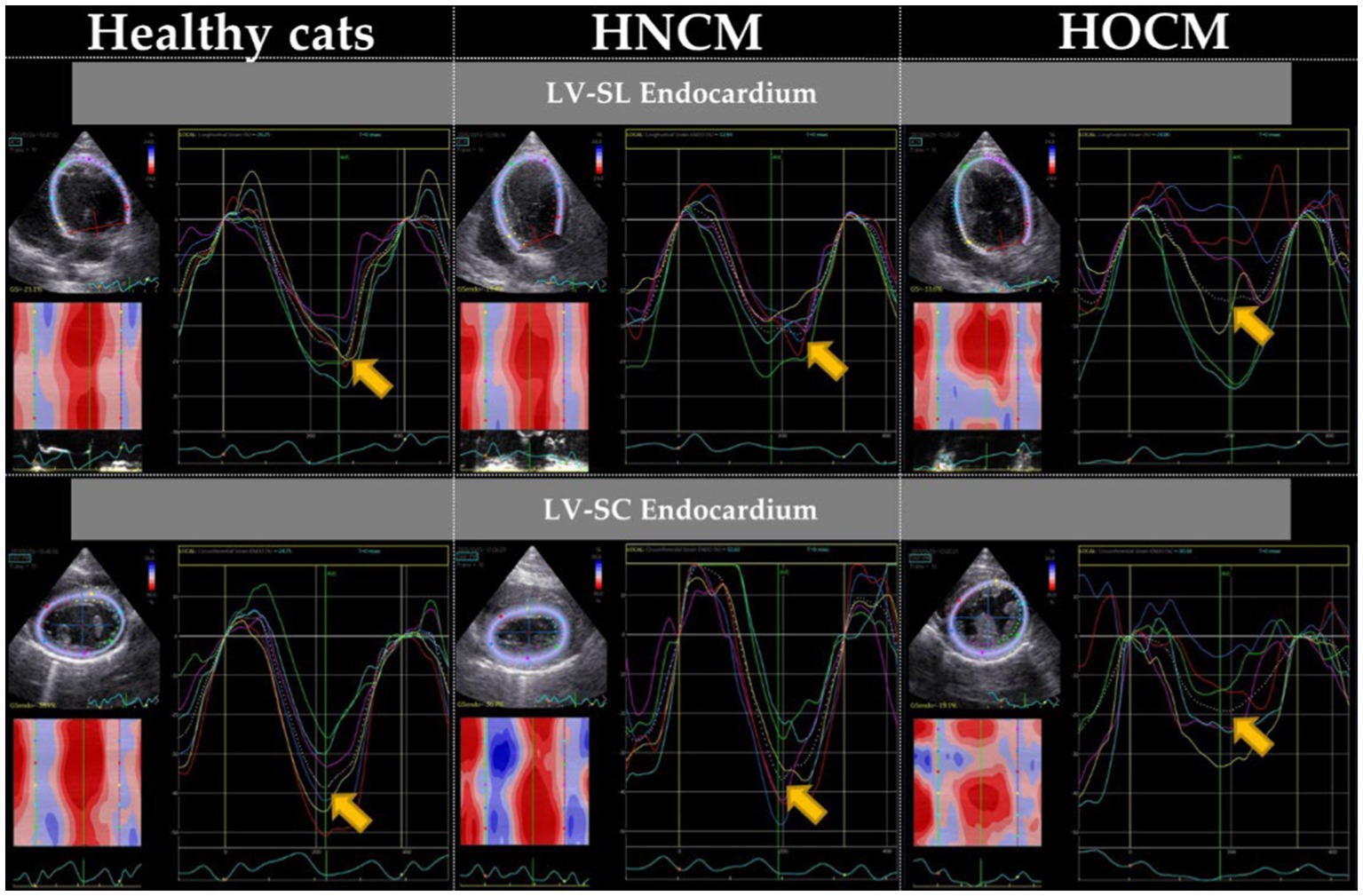
Figure 1. Myocardial motion analysis results of endocardium by 2D-STE method (representative data). LV-SL, peak systolic strain in the longitudinal direction at left ventricles; LV-SC, peak systolic strain in the circumferential direction at left ventricles. Arrows indicate the peak of the endocardium.
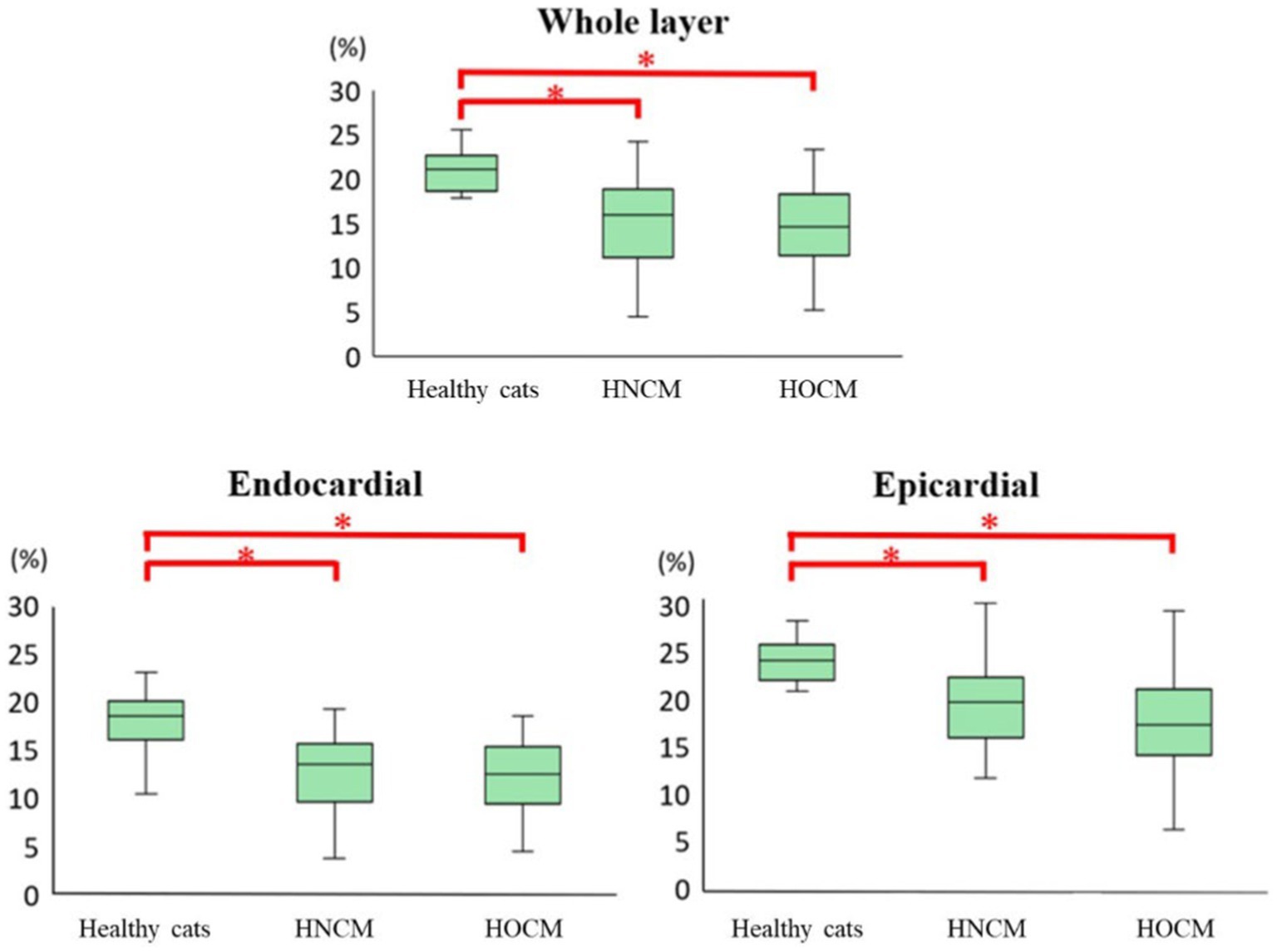
Figure 2. Results of longitudinal strain by 2D-STE method (box-and-whisker diagram). *The value is significantly different from the healthy cats (p < 0.05).
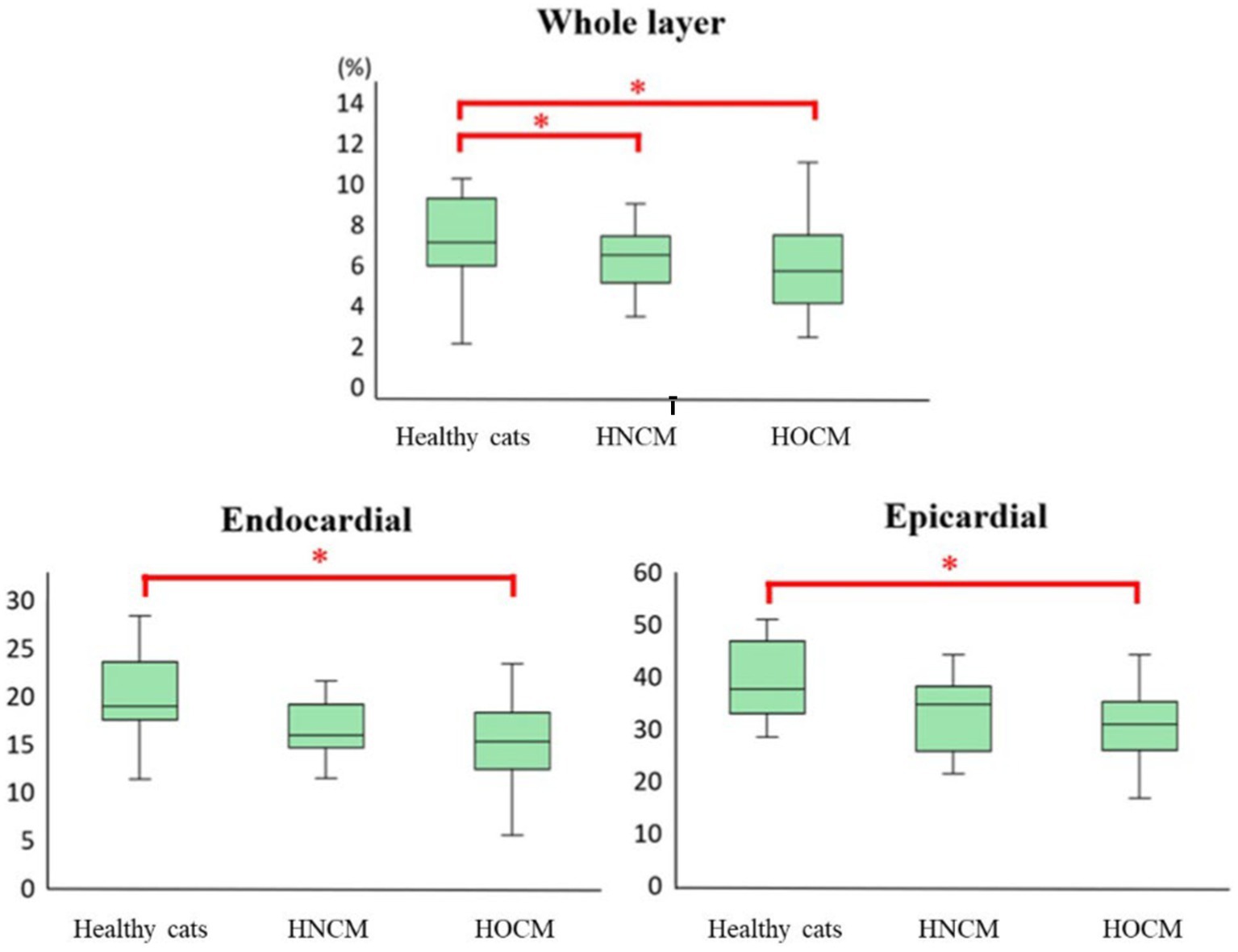
Figure 3. Results of circumferential strain by 2D-STE method (box-and-whisker diagram). *The value is significantly different from the healthy cats (p < 0.05).
4. Discussion
In this study, the HNCM and HOCM had decreased LV-SL in whole layers and LV-SC in the epicardium, which is consistent with the results of previous studies (20). Previous 2D-STE studies in cats with HCM have reported lower longitudinal strain in asymptomatic HCM cats than in healthy cats (13, 19). This has been shown to be caused by myocardial dysfunction and histopathologic changes (10, 11, 25, 26). Along with histopathological changes such as modifications in myocardial fiber orientation, myocardial compensatory mechanisms are believed to be linked with these dysfunctions (14, 19, 27). Even in human HCM, there are cases in which LV-SL in whole layers is decreased, even if the left ventricular ejection fraction appears normal. These cases have been reported to have a poor prognosis (28) and should not be judged as having normal LV systolic function based on conventional echocardiography only. However, in this study, there was no significant difference in LV-SL between the HNCM and HOCM in whole layer, so it was unlikely that the HOCM would have a worse prognosis based on LV-SL results. Previous studies on cats reported no differences in survival between the HNCM and HOCM (4). In contrast, in humans, HOCM is reported to be associated with a shorter survival time and worse prognosis owing to DLVOTO than HNCM (7). The detailed cause of why DLVOTO has a poorer prognosis in HCM is unknown. However, the mechanism has been discussed in previous papers as follows (7); The increased left ventricular pressure due to DLVOTO is expected to result in increased wall stress. Myocardium also devotes more effort to contraction, which can lead to myocardial ischemia. These abnormalities may contribute to eventual cardiomyocyte death and scarring (29–31). These changes are thought to result in stiffening of the myocardium, leading to diastolic dysfunction (32–34) as well as increased susceptibility to electrical instability and sudden death. DLVOTO of HCM-affected cats may reduce endocardial myocardial function through a mechanism similar to that reported in humans (7). In addition, the decreased LV-SC in the endocardial may have inevitably decreased LV-SC in the whole layer. The aforementioned human study also reported that older patients with HOCM (age ≥ 40 years) were more likely to experience deterioration than younger patients with HOCM by a similar mechanism (7). It is unclear whether it is appropriate to extrapolate this mechanism directly to cats, and the fact that the duration of obstruction is different in cats than in humans may be related to the finding that survival is not affected in the former. Nevertheless, based on this mechanism and the results of this study, we believe that careful evaluation of the long-term prognosis of cats with HOCM is warranted in the future.
In this study, LV-SL Endo/Epi was significantly increased in the HOCM and HNCM compared to the healthy cats, but there was no significant difference in LV-SC Endo/Epi. However, LV-SC Endo/Epi was decreased in the HOCM and HNCM compared to the healthy cats, although the difference was not significant. LV-SC Endo/Epi in asymptomatic cats-affected HCM was increased compared to healthy cats in a previous study, although there was no significant difference in LV-SL Endo/Epi (20). Increased LV-SC Endo/Epi is considered to be circumferential endocardial compensation for depressed epicardial contraction (20, 23, 24). Therefore, the HCM-affected cats included in this study were relatively severe and the compensatory mechanisms may have become dysfunctional. Although this study included cats with HCM of various American College of Veterinary Internal Medicine stages and thus the results should be interpreted with caution, a lower LV-SC Endo/Epi may be associated with worse prognosis in cats-affected HCM.
There were several limitations to the study. The sample size was small, which may have affected the results owing to case bias. In addition, some affected cats were prescribed oral medications, which may have affected the results. Furthermore, diagnosis was based on echocardiography, and not pathological findings. The study also included cats with HCM of varying severities, which may have affected the results. Specifically, it is possible that pathological severity was milder in the HNCM, resulting in a significant difference only in the HOCM compared to the healthy cats. However, no significant differences were found between the HNCM and HOCM with respect to left ventricular wall thickness or American College of Veterinary Internal Medicine stage. Therefore, it is considered that there is no extreme difference in severity of disease.
5. Conclusion
Our results also indicate that 2D-STE is useful for detecting HCM, as shown in previous studies, and that cats with HOCM may have worse myocardial function than those with HNCM. However, predicting prognosis requires caution, and further studies are warranted to clarify these aspects.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The animal study was reviewed and approved by Nippon Veterinary and Life Science University. Written informed consent was obtained from the owners for the participation of their animals in this study.
Author contributions
RS and TS conceptualized and designed the study, acquired and interpreted the data, and drafted and critically revised the manuscript. YY, HF, and SS acquired, analyzed, and summarized the data and approved the article. TT and HM acquired and interpreted the data, supervised the study, and approved the article. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the Japan Society for the Promotion of Science KAKENHI (grant number 22K05995).
Acknowledgments
This study was conducted at the Laboratory of Veterinary Internal Medicine, School of Veterinary Science, Nippon Veterinary and Life Science University, Tokyo, Japan. We would also like to thank Editage (www.editage.com) for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
2D-STE, Two-dimensional speckle-tracking echocardiography; A-wave, Peak velocity of the late diastolic wave; DLVOTO, Dynamic left-ventricular outflow-tract obstruction; E-wave, Peak velocity of the early diastolic wave; E/A, E-wave to A-wave velocity ratio; FS, Fractional shortening; HCM, Hypertrophic cardiomyopathy; HNCM, Non-obstructive HCM; HOCM, Obstructive HCM; IVSd, End-diastolic interventricular septal thickness; LA/Ao, Left atrium to aortic diameter ratio; LV, Left-ventricular; LVIDd, End-diastolic LV internal diameter; LVOT Vmax, Peak velocity of left-ventricular outflow-tract; LVPWd, End-diastolic LV free-wall thickness; RWT, Relative left-ventricular wall thickness; SC, Circumferential strain; SL, Longitudinal strain.
References
1. Rush, JE, Freeman, LM, and Fenollosa, NKBD. Population and survival characteristics of cats with hypertrophic cardiomyopathy: 260 cases (1990–1999). J Am Vet Med Assoc. (2002) 220:202–7. doi: 10.2460/javma.2002.220.202
2. Payne, JR, Brodbelt, DC, and Luis, FV. Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study). J Vet Cardiol. (2015) 17:S244–57. doi: 10.1016/j.jvc.2015.03.008
3. Paige, CF, Abbott, JA, and Elvinger, FPR. Prevalence of cardiomyopathy in apparently healthy cats. J Am Vet Med Assoc. (2009) 234:1398–403. doi: 10.2460/javma.234.11.1398
4. Fox, PR, Keene, BW, Lamb, K, Schober, KA, Chetboul, V, Luis Fuentes, V, et al. International collaborative study to assess cardiovascular risk and evaluate long-term health in cats with preclinical hypertrophic cardiomyopathy and apparently healthy cats: the REVEAL study. J Vet Intern Med. (2018) 32:930–43. doi: 10.1111/jvim.15122
5. Fox, PR . Hypertrophic cardiomyopathy. Clinical and pathologic correlates. J Vet Cardiol. (2003) 5:39–45. doi: 10.1016/S1760-2734(06)70051-0
6. Fox, PR, Liu, SK, and Maron, BJ. Echocardiographic assessment of spontaneously occurring feline hypertrophic cardiomyopathy. An animal model of human disease. Circulation. (1995) 92:2645–51. doi: 10.1161/01.CIR.92.9.2645
7. Maron, MS, Olivotto, I, Betocchi, S, Casey, SA, Lesser, JR, Losi, MA, et al. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N Engl J Med. (2003) 348:295–303. doi: 10.1056/NEJMoa021332
8. Williams, LK, Chan, RH, Carasso, S, Durand, M, Misurka, J, Crean, AM, et al. Effect of left ventricular outflow tract obstruction on left atrial mechanics in hypertrophic cardiomyopathy. Biomed Res Int. (2015) 2015:1–10. doi: 10.1155/2015/481245
9. Suzuki, R, Mochizuki, Y, Yoshimatsu, H, Niina, A, Teshima, T, Matsumoto, H, et al. Early detection of myocardial dysfunction using two-dimensional speckle tracking echocardiography in a young cat with hypertrophic cardiomyopathy. J Feline Med Surg Open Reports. (2018) 4:205511691875621. doi: 10.1177/2055116918756219
10. Liu, Y, Deng, Y, Li, X, et al. Assessment of left ventricular longitudinal regional myocardial systolic function by strain imaging echocardiography in patients with hypertrophic cardiomyopathy. J Huazhong Univ Sci Technol Med Sc. (2005) 25:703–5. doi: 10.1007/BF02896176
11. Serri, K, Reant, P, Lafitte, M, Berhouet, M, Le Bouffos, V, Roudaut, R, et al. Global and regional myocardial function quantification by two-dimensional strain: application in hypertrophic cardiomyopathy. J Am Coll Cardiol. (2006) 47:1175–81. doi: 10.1016/j.jacc.2005.10.061
12. Takano, H, Isogai, T, Aoki, A, Wakao, Y, and Fujii, Y. Feasibility of radial and circumferential strain analysis using 2D speckle tracking echocardiography in cats. J Vet Med Sci. (2015) 77:193–201. doi: 10.1292/jvms.13-0241
13. Sugimoto, K, Fujii, Y, Sunahara, H, and Aoki, T. Assessment of left ventricular longitudinal function in cats with subclinical hypertrophic cardiomyopathy using tissue Doppler imaging and speckle tracking echocardiography. J Vet Med Sci. (2015) 77:1101–8. doi: 10.1292/jvms.14-0354
14. Suzuki, R, Mochizuki, Y, Yoshimatsu, H, Ohkusa, T, Teshima, T, Matsumoto, H, et al. Myocardial torsional deformations in cats with hypertrophic cardiomyopathy using two-dimensional speckle-tracking echocardiography. J Vet Cardiol. (2016) 18:350–7. doi: 10.1016/j.jvc.2016.06.004
15. Suzuki, R, Mochizuki, Y, Yuchi, Y, Yasumura, Y, Saito, T, Teshima, T, et al. Assessment of myocardial function in obstructive hypertrophic cardiomyopathy cats with and without response to medical treatment by carvedilol. BMC Vet Res. (2019) 15:1–8. doi: 10.1186/s12917-019-2141-0
16. Jackson, BL, Adin, DB, and Lehmkuhl, LB. Effect of atenolol on heart rate, arrhythmias, blood pressure, and dynamic left ventricular outflow tract obstruction in cats with subclinical hypertrophic cardiomyopathy. J Vet Cardiol Off J Eur Soc Vet Cardiol. (2015) 17:S296–305. doi: 10.1016/j.jvc.2015.03.002
17. Luis Fuentes, V, Abbott, J, Chetboul, V, Côté, E, Fox, PR, Häggström, J, et al. ACVIM consensus statement guidelines for the classification, diagnosis, and management of cardiomyopathies in cats. J Vet Intern Med. (2020) 34:1062–77. doi: 10.1111/jvim.15745
18. Visser, LC, Sloan, CQ, and Stern, JA. Echocardiographic assessment of right ventricular size and function in cats with hypertrophic cardiomyopathy. J Vet Intern Med. (2017) 31:668–77. doi: 10.1111/jvim.14688
19. Suzuki, R, Mochizuki, Y, Yoshimatsu, H, Teshima, T, Matsumoto, H, and Koyama, H. Determination of multidirectional myocardial deformations in cats with hypertrophic cardiomyopathy by using two-dimensional speckle-tracking echocardiography. J Feline Med Surg. (2017) 19:1283–9. doi: 10.1177/1098612X17691896
20. Suzuki, R, Mochizuki, Y, Yoshimatsu, H, Niina, A, Teshima, T, Matsumoto, H, et al. Layer-specific myocardial function in asymptomatic cats with obstructive hypertrophic cardiomyopathy assessed using 2-dimensional speckle-tracking echocardiography. J Vet Intern Med. (2019) 33:37–45. doi: 10.1111/jvim.15339
21. Suzuki, R, Yuchi, Y, Kanno, H, Teshima, T, Matsumoto, H, and Koyama, H. Left and right myocardial functionality assessed by two-dimensional speckle-tracking echocardiography in cats with restrictive cardiomyopathy. Animals. (2021) 11:1578. doi: 10.3390/ani11061578
22. Hutagalung, A . Noninvasive clinical assessment of systolic torsional motions by two-dimensional speckle-tracking echocardiography in dogs with myxomatous mitral valve disease. Angew Chemie Int Ed. (1967) 6:951–2. doi: 10.1111/jvim.12024
23. Ozawa, K, Funabashi, N, Takaoka, H, Kamata, T, Kanaeda, A, Saito, M, et al. Characteristic myocardial strain identified in hypertrophic cardiomyopathy subjects with preserved left ventricular ejection fraction using a novel multi-layer transthoracic echocardiography technique. Int J Cardiol. (2015) 184:237–43. doi: 10.1016/j.ijcard.2015.01.070
24. Okada, K, Yamada, S, Iwano, H, Nishino, H, Nakabachi, M, Yokoyama, S, et al. Myocardial shortening in 3 orthogonal directions and its transmural variation in patients with nonobstructive hypertrophic cardiomyopathy. Circ J. (2015) 79:2471–9. doi: 10.1253/circj.CJ-15-0646
25. Popović, ZB, Kwon, DH, Mishra, M, Buakhamsri, A, Greenberg, NL, Thamilarasan, M, et al. Association between regional ventricular function and myocardial fibrosis in hypertrophic cardiomyopathy assessed by speckle tracking echocardiography and delayed hyperenhancement magnetic resonance imaging. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. (2008) 21:1299–305. doi: 10.1016/j.echo.2008.09.011
26. Urbano-Moral, JA, Rowin, EJ, Maron, MS, Crean, A, and Pandian, NG. Investigation of global and regional myocardial mechanics with 3-dimensional speckle tracking echocardiography and relations to hypertrophy and fibrosis in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging. (2014) 7:11–9. doi: 10.1161/CIRCIMAGING.113.000842
27. Carasso, S, Yang, H, Woo, A, Vannan, MA, Jamorski, M, Wigle, ED, et al. Systolic myocardial mechanics in hypertrophic cardiomyopathy: novel concepts and implications for clinical status. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. (2008) 21:675–83. doi: 10.1016/j.echo.2007.10.021
28. Liu, H, Pozios, I, Haileselassie, B, Nowbar, A, Sorensen, LL, Phillip, S, et al. Role of global longitudinal strain in predicting outcomes in hypertrophic cardiomyopathy. Am J Cardiol. (2017) 120:670–5. doi: 10.1016/j.amjcard.2017.05.039
29. Maron, BJ, Wolfson, JK, Epstein, SE, and Roberts, WC. Intramural (“small vessel”) coronary artery disease in hypertrophic cardiomyopathy. J Am Coll Cardiol. (1986) 8:545–57. doi: 10.1016/S0735-1097(86)80181-4
30. Cannon, RO, Rosing, DR, Maron, BJ, Leon, MB, Bonow, RO, Watson, RM, et al. Myocardial ischemia in patients with hypertrophic cardiomyopathy: contribution of inadequate vasodilator reserve and elevated left ventricular filling pressures. Circulation. (1985) 71:234–43. doi: 10.1161/01.CIR.71.2.234
31. Factor, SM, Butany, J, Sole, MJ, Wigle, ED, Williams, WC, and Rojkind, M. Pathologic fibrosis and matrix connective tissue in the subaortic myocardium of patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. (1991) 17:1343–51. doi: 10.1016/S0735-1097(10)80145-7
32. Wigle, ED, Sasson, Z, Henderson, MA, Ruddy, TD, Fulop, J, Rakowski, H, et al. Hypertrophic cardiomyopathy. The importance of the site and the extent of hypertrophy. A review. Prog Cardiovasc Dis. (1985) 28:1–83. doi: 10.1016/0033-0620(85)90024-6
33. Wigle, ED, Rakowski, H, Kimball, BP, and Williams, WG. Hypertrophic cardiomyopathy. Clin Spectr Treatment Circ. (1995) 92:1680–92. doi: 10.1161/01.CIR.92.7.1680
Keywords: cat, cardiomyopathy, speckle tracking echocardiography, myocardial function, strain
Citation: Saito T, Suzuki R, Yuchi Y, Fukuoka H, Satomi S, Teshima T and Matsumoto H (2023) Comparative study of myocardial function in cases of feline hypertrophic cardiomyopathy with and without dynamic left-ventricular outflow-tract obstruction. Front. Vet. Sci. 10:1191211. doi: 10.3389/fvets.2023.1191211
Edited by:
Ryou Tanaka, Tokyo University of Agriculture and Technology, JapanReviewed by:
Hussein M. El-Husseiny, Tokyo University of Agriculture and Technology, JapanAna Patrícia Fontes-Sousa, University of Porto, Portugal
Copyright © 2023 Saito, Suzuki, Yuchi, Fukuoka, Satomi, Teshima and Matsumoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ryohei Suzuki, cnlvaGVpc3V6dWtpMDEzMEBnbWFpbC5jb20=
 Takahiro Saito
Takahiro Saito Ryohei Suzuki*
Ryohei Suzuki* Yunosuke Yuchi
Yunosuke Yuchi Takahiro Teshima
Takahiro Teshima