- 1Air Force Institute of Technology, Civilian Institutions Programs, Wright Patterson Air Force Base, Dayton, OH, United States
- 2Department of Anesthesiology, Michigan Medicine, Ann Arbor, MI, United States
Interscalene blockade is a widely accepted regional analgesic technique that has been demonstrated to limit postoperative pain and opioid consumption in total shoulder arthroplasty. Phrenic nerve paresis is an unintended consequence of this block and is well-tolerated in the majority of patients. The development of liposomal bupivacaine (LB) offers the potential for extended-duration analgesia over standard bupivacaine. US Food and Drug Administration approval for the use of a specific preparation of LB for interscalene block was obtained in 2018, and research is ongoing on the analgesic duration, benefits, and side effect profile of this relatively new local anesthetic. We report on a case of a total shoulder replacement with a single-shot interscalene block with LB and subsequent intensive care unit admission for 25 days for persistent hypoxemia requiring bilevel positive airway pressure and heated high-flow oxygen. Following extensive evaluation by a multidisciplinary pulmonology and anesthesiology critical care team, it was determined that his hypoxemia was due to phrenic nerve palsy in the setting of interscalene nerve block in a patient with reduced pulmonary capacity at baseline, although no overt signs of severe or decompensated disease were identified preoperatively. Patient comorbidities, mechanisms to prolong blockade, and alternatives to an interscalene block should be carefully considered to avoid significant pulmonary complications.
Introduction
The use of interscalene nerve blockade for shoulder surgery has long been considered the standard of care in the immediate postoperative period to improve pain and reduce opioid consumption (1, 2). Notably, the side effect profile of ipsilateral phrenic nerve palsy is well-described but also well-tolerated and limited in the majority of patients (3). However, as rates of obesity and pulmonary disease increase and methods to prolong the duration of anesthesia evolve, the risks and benefits of an interscalene nerve block and consideration of alternatives must be carefully considered.
Demographics and course
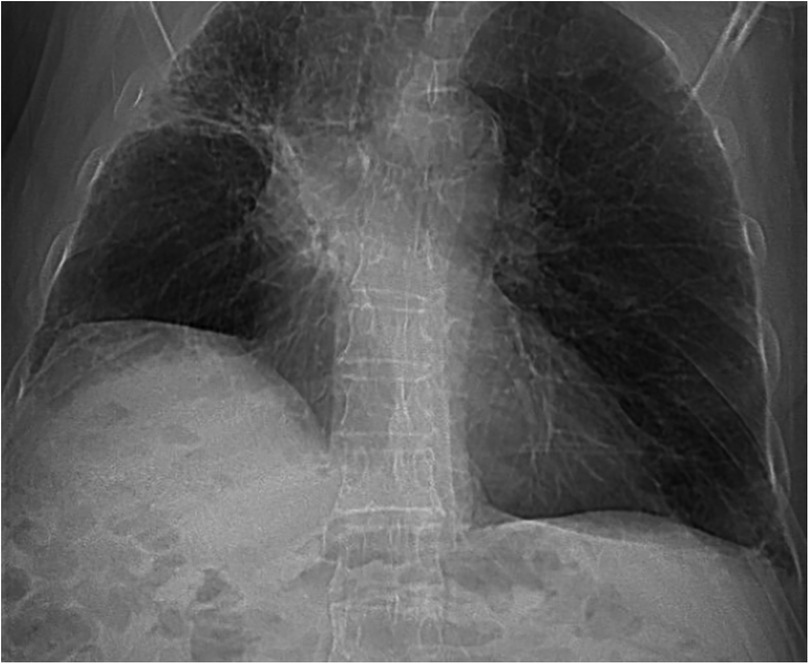
Our case was a 75-year-old male American Society of Anesthesiologists (ASA) 3 patient presenting for an elective right total shoulder arthroplasty for glenohumeral arthritis that limited his activities of daily living. The patient's past medical history included right upper lobe adenocarcinoma with brain metastases diagnosed in 2017, which had been treated with radiation and immunotherapy without the need for surgery. This was now in remission, although he regularly consulted his pulmonologist, who arranged periodic computed tomography (CT) scans and bronchoscopies, which only revealed granulomas from Mycobacterium chimaera/intracellulare that did not require antibiotic treatment. He was a former smoker with a six-pack year smoking history, who had quit 40 years prior and had well-controlled gastroesophageal reflux disease. Pre-operative medications included an as-needed albuterol inhaler, fluticasone, and omeprazole. Of note, the patient had an elevated right hemidiaphragm, thought to be secondary to his radiation or underlying lung disease (Figure 1), and had a remote history of supplemental oxygen use while undergoing active treatment for his lung cancer. The patient did not require long-acting bronchodilators, systemic steroids, or supplemental oxygen, having been on room air for 4 years after lung cancer treatment. The patient had undergone pulmonary function testing 1 month before his procedure with normal spirometry [predicted forced expiratory volume in 1 s (FEV1) of 95% and predicted forced vital capacity (FVC) of 95%] and oxygen saturation of 96% on room air. His past surgical history included a left rotator cuff repair in 2018 and a vasectomy. His pre-operative weight and body mass index (BMI) were 84.6 kg and 27.15 kg/m2, respectively. No additional concerning findings such as hypoxemia, fever, weight loss, or recent chronic obstructive pulmonary disease (COPD) exacerbations were noted on his pre-operative anesthesiology assessment. The patient's anesthesiologist placed a pre-operative right-sided interscalene block (ISB), using 7.5 ml of bupivacaine (0.5%) and 7.5 ml of liposomal bupivacaine (LB) (1.3%). The patient then underwent general endotracheal anesthesia utilizing propofol, rocuronium, dexamethasone, and ketamine, and 1 L of crystalloid and sugammadex for neuromuscular blockade reversal prior to emergence. He did not require rapid sequence induction, and there was no noted concern of aspiration. No opioids were used intraoperatively or postoperatively. There was no concern postoperatively for incomplete muscle relaxation reversal, and the estimated blood loss was 150 ml per the operative report. The patient had an uneventful post-anesthesia care unit (PACU) stay and was discharged home on postoperative day (POD) 0 without any noted respiratory concerns.
On the evening of POD 1, the patient developed shortness of breath at home and self-medicated with an oxygen concentrator, which he had kept from his previous cancer treatment. Symptoms persisted, and on POD 3, the patient presented to an outside hospital Emergency Department where he was noted to have a pulse oximetry reading of 74% recorded despite administration of 4 L of oxygen via nasal cannula (NC). He was immediately placed on continuous positive airway pressure (CPAP) therapy, with an improvement in his oxygen saturation. A chest x-ray revealed no evidence of pneumothorax, and a contrast CT scan of his chest revealed no new effusion, pneumonia, or pulmonary embolus. Admission hemoglobin was found to be 15 g/dl, with no other abnormal laboratory findings. The only imaging finding noted was a persistently elevated hemidiaphragm, consistent with his previous plain films. The patient was admitted to the intensive care unit (ICU) and treated with steroids and doxycycline/ceftriaxone for possible COPD exacerbation with no improvement. He was transitioned to a heated high-flow NC but was unable to be weaned. On POD 8, the patient was transferred to our tertiary care center for further evaluation.
The patient's hospital course included additional CT scans of the chest with contrast (PODs 5 and 9), a transthoracic echo (PODs 9 and 19), and a nuclear medicine perfusion study for possible shunt evaluation (POD 12). These studies were significant only for stable post-radiation changes and scarring when compared to previous imaging. Throughout his hospital stay, the patient was afebrile with normal blood pressure, and his multiple chest x-rays and CTs were not suspicious for an infectious etiology. Respiratory viral panels were also attained multiple times throughout admission with negative results. On POD 9, the patient reported the first sensation of pain in his operative shoulder, which had been well-controlled with only acetaminophen without any need for the non-steroidal anti-inflammatory drugs (NSAIDs) and opioids prescribed at discharge. On POD 21, the patient was found to have an absent diaphragmatic sniff on the right side; however, no pre-operative sniff test was available for comparison. After infectious, malignant, and hematologic causes were ruled out, magnetic resonance imaging (MRI) of the brachial plexus (Figure 2) was performed to investigate a possible phrenic nerve injury or compression from a traumatic block. This study was also unremarkable. Electromyography (EMG) was ordered; however, it was not performed in the hospital. Eventually, on POD 35, the patient was able to be reliably weaned from the heated high-flow NC in the ICU and was discharged home on 4 L NC and eventually weaned to room air 3 months later after outpatient pulmonary rehabilitation.
Discussion
Appropriate patient selection for peripheral nerve blockade is vital. Interscalene nerve blockade for shoulder arthroscopy, rotator cuff repair, and shoulder replacement is often well-tolerated on an outpatient basis. Interscalene block options can include a single-shot deposition of local anesthetic, the use of perineural catheters to deliver local anesthetic postoperatively, or the use of LB. However, due to the near 100% incidence of diaphragmatic paresis, caution is warranted in patients with underlying lung disease. Various strategies have been attempted to reduce or mitigate pulmonary dysfunction in shoulder surgery (3). While our patient had a pre-existing elevated hemidiaphragm but normal pulmonary function testing, it was felt that an ipsilateral interscalene block would be safe. Typically, the sensation of dyspnea is widely observed but is not clinically significant (no evidence of hypoxemia) and often resolves while analgesia persists. For those patients with persistent hypoxemia associated with interscalene block, case reports have typically found resolution within days to weeks after administration of supplemental oxygen while waiting for local anesthetic metabolism (4).
However, there have been instances where dyspnea has persisted. Case reports exist of prolonged diaphragmatic paresis with an elevated hemidiaphragm and new-onset dyspnea on exertion for over a year in an otherwise healthy patient (5). Interestingly, these case reports describe traditional local anesthetics and did not involve LB.
The decision of which local anesthetic to use can vary regionally, among institutions, and due to supply chain constraints. Long-acting amides such as bupivacaine and ropivacaine are frequently used and studied. A meta-analysis of studies comparing LB to plain bupivacaine found that its use was not superior for clinically significant postoperative pain control (6). A randomized, double-blind control study comparing LB to bupivacaine with perineural dexamethasone revealed no significant difference in postoperative opioid use or pain scores (7).
When evaluating nerve palsy, consideration of the surgical technique and possible etiologies other than anesthetic is required. In reverse total shoulder techniques, Dwyer et al. reported that most brachial plexus injuries are more distal in the ulnar, musculocutaneous, and axillary nerve distributions. This is often attributed to the traction required for the procedure, but phrenic nerve injury has not been well-described (8). In our patient, we had a lower suspicion of a mechanical etiology from surgical manipulation.
While LB is US Food and Drug Administration (FDA)-approved for interscalene brachial plexus blockade, specifics about the duration of analgesia and rates of adverse drug reactions continue to be elucidated in the literature. Berg et al. described statistically significant reductions in diaphragmatic excursion and pulmonary function testing with liposomal bupivacaine when compared to plain bupivacaine for interscalene blocks (9). Malige et al. noted a minor and major complication rate of 10.5% and 6.0%, respectively, in 352 patients receiving LB for shoulder surgery, with age, ASA score, and Charlson comorbidity score as significant predictors of major complications, while a history of pulmonary disease was not (10). Of particular concern is that 12.5% of these patients reported a degree of dyspnea when LB, alone or mixed with bupivacaine, was used for single-shot interscalene blockade. Alternatively, other long-lasting regional techniques carry risk: Fredrickson et al. noted a 27% rate of dyspnea, and in a prospective study of 1,505 patients receiving continuous nerve catheter analgesia for shoulder surgery, the duration and interquartile range of dyspnea were 2 and 1–8 days, respectively (11). Our patient had several concerning findings in his past medical history, but we believe that the lack of symptoms or signs of respiratory insufficiency at the time of surgery warranted consideration of an interscalene block, although, in this case, it led to severe and unintended complications. While the sniff test performed postoperatively supports the diagnosis of phrenic nerve palsy, regardless of etiology, the presence of pre-existing lung disease on the same side can confound this possibility and open up other possibilities, such as diaphragmatic trauma, which could have been exacerbated by interscalene blockade.
Regardless of local anesthetic choice, alternative block strategies to mitigate phrenic nerve palsy have been shown to be non-inferior in terms of analgesia. Auyong et al. conducted a randomized controlled trial comparing the anterior suprascapular nerve block (SSNB) to the interscalene block and found it to be non-inferior with respect to pain scores while simultaneously preserving diaphragmatic function—the same study found the supraclavicular block to be inferior (3). A meta-analysis by Sun et al. investigating ISB vs. SSNB in 1,255 patients in 17 randomized controlled studies showed that patients who received an ISB had lower pain with movement at 1 h postoperatively but similar scores at 4–6 h, lower scores at 8–12 h, and similar pain again at 1 and 2 days (12). Moreover, 24-hour morphine consumption and PACU length of stay were similar between the patients who received an ISB and those who received an SSNB, while the SSNB group had lower rates of complications such as Horner’s syndrome, dyspnea, hoarseness, and numbness (12). Our patient would likely have benefited from an alternative technique, such as the suprascapular nerve block; thus, it is worth consideration in such patients. Currently, however, LB is not FDA-approved for anterior suprascapular blockade.
Conclusion
Patients undergoing shoulder procedures benefit from regional anesthesia techniques; however, careful consideration of a patient's pulmonary reserve and comorbidities should drive block selection and local anesthetic choice. Catheter-based techniques and LB are intended to prolong the well-established analgesic efficacy of the interscalene block, and our patient had markedly prolonged analgesia of 9 days. The literature notes that pulmonary complications are frequent with both approaches, warranting careful patient selection. In patients with significant pulmonary disease, such as in this case report, caution is warranted, but this does not outright contraindicate interscalene block, however, anterior suprascapular block presents a non-inferior opioid-sparing alternative with much better preservation of vital capacity (3). Cases such as this reinforce that while interscalene block is commonly used in an outpatient setting and offers significant benefit to the patient, anesthesiologists must be vigilant during patient assessment and risk/benefit discussions when considering regional anesthesia for shoulder surgery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the studies involving humans because this is a Case Report of an adverse event to a standard of care treatment (liposomal bupivacaine peripheral nerve block). The care of the patient described met the standard of care with no experimental intervention. The report discusses alternatives and side effects of our medications and regional anesthesia. The patient provided informed consent to discuss his case, which can be provided if required. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MB: Conceptualization, Writing – original draft, Writing – review & editing, Funding acquisition. DA: Conceptualization, Supervision, Visualization, Writing – review & editing, Funding acquisition. RM: Conceptualization, Supervision, Validation, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The article processing charge was funded by the Michigan Medicine Department of Anesthesiology.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI Statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in this article are those of the authors and do not reflect the official policy or position of the University of Michigan, the United States Air Force, Department of Defense, or the U.S. Government.
References
1. Elmer DA, Coleman JR, Renwick CM, Amato PE, Werner BC, Brockmeier SF, et al. Comparing bupivacaine alone to liposomal bupivacaine plus bupivacaine in interscalene blocks for total shoulder arthroplasty: a randomized, non-inferiority trial. Reg Anesth Pain Med. (2023) 48(1):1–6. doi: 10.1136/rapm-2022-103997
2. Mojica JJ, Ocker A, Barrata J, Schwenk ES. Anesthesia for the patient undergoing shoulder surgery. Clin Sports Med. (2022) 41(2):219–31. doi: 10.1016/j.csm.2021.11.004
3. Auyong DB, Hanson NA, Joseph RS, Schmidt BE, Slee AE, Yuan SC. Comparison of anterior suprascapular, supraclavicular, and interscalene nerve block approaches for Major outpatient arthroscopic shoulder surgery: a randomized, double-blind, noninferiority trial. Anesthesiology. (2018) 129(1):47–57. doi: 10.1097/ALN.0000000000002208
4. Randhawa S, Creed KA, Hassanin E, Barton J. Interscalene nerve block-induced hemidiaphragmatic paralysis. CHEST. (2023) 164(4):A6262. doi: 10.1016/j.chest.2023.07.4028
5. Nickless JT, Waterman BR, Romeo AA. Persistent diaphragmatic paralysis associated with interscalene nerve block after total shoulder arthroplasty: a case report. JSES Open Access. (2018) 2(3):165–8. doi: 10.1016/j.jses.2018.05.003
6. Hussain N, Brull R, Sheehy B, Essandoh MK, Stahl DL, Weaver TE, et al. Perineural liposomal bupivacaine is not superior to nonliposomal bupivacaine for peripheral nerve block analgesia. Anesthesiology. (2021) 134(2):147–64. doi: 10.1097/ALN.0000000000003651
7. Kim DH, Liu J, Beathe JC, Lin Y, Wetmore DS, Kim SJ, et al. Interscalene brachial Plexus block with liposomal bupivacaine versus standard bupivacaine with perineural dexamethasone: a noninferiority trial. Anesthesiology. (2022) 136(3):434–47. doi: 10.1097/ALN.0000000000004111 Erratum in: Anesthesiology. 2023 138(2):233. doi: 10.1097/ALN.0000000000004255.35041742
8. Dwyer T, Henry PD, Cholvisudhi P, Chan VW, Theodoropoulos JS, Brull R. Neurological complications related to elective orthopedic surgery: part 1: common shoulder and elbow procedures. Reg Anesth Pain Med. (2015) 40(5):431–42. doi: 10.1097/AAP.0000000000000178
9. Berg AA, Flaherty JM, Habeck JM, Harrison AK, Braman JP, Kaizer AM, et al. Evaluation of diaphragmatic function after interscalene block with liposomal bupivacaine: a randomized controlled trial. Anesthesiology. (2022) 136(4):531–41. doi: 10.1097/ALN.0000000000004118
10. Malige A, Yeazell S, Ng-Pellegrino A, Carolan G. Risk factors for complications and return to the emergency department after interscalene block using liposomal bupivacaine for shoulder surgery. J Shoulder Elbow Surg. (2020) 29(11):2332–8. doi: 10.1016/j.jse.2020.03.012
11. Fredrickson MJ, Leightley P, Wong A, Chaddock M, Abeysekera A, Frampton C. An analysis of 1505 consecutive patients receiving continuous interscalene analgesia at home: a multicentre prospective safety study. Anaesthesia. (2016) 71(4):373–9. doi: 10.1111/anae.13385
Keywords: interscalene analgesia, phrenic nerve palsy, unanticipated admission, postoperative complication, bupivacaine
Citation: Byrne MC, Anderson DH and Meral RM (2025) Case Report: Complications of an interscalene block with liposomal local anesthetic resulting in ICU admission for over 25 days—critical sequelae of outpatient surgical procedures. Front. Anesthesiol. 4:1554730. doi: 10.3389/fanes.2025.1554730
Received: 2 January 2025; Accepted: 26 March 2025;
Published: 25 April 2025.
Edited by:
Hong Liu, UC Davis Health, United StatesReviewed by:
Christian Bohringer, UC Davis Medical Center, United StatesMichael Fettiplace, Massachusetts General Hospital and Harvard Medical School, United States
Copyright: © 2025 Byrne, Anderson and Meral. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew C. Byrne, bWF0dGhldy5ieXJuZS40QHVzLmFmLm1pbA==
 Matthew C. Byrne
Matthew C. Byrne Douglas H. Anderson
Douglas H. Anderson Ryan M. Meral2
Ryan M. Meral2