- 1Department of Anesthesiology, American University of Beirut, Beirut, Lebanon
- 2School of Medicine, Wayne State University, Detroit, MI, United States
- 3Outcomes Research Consortium®, Houston, TX, United States
Familial support in perioperative care is increasingly being recognized as essential for better surgical outcomes, treatment protocols, and overall recovery. Recent work suggests that standardized family involvement leads to measurable improvements, including reduced postoperative delirium (POD) and complications, lower anxiety, shorter hospital stay, and increased patient and family satisfaction. Examples include the Tailored, Family-Involved Hospital Elder Life Program (t-HELP), which reduced POD incidence from 19.4%–2.6% while preserving functional and cognitive changes in elderly; as well as the Family Involvement Program (FIP), which integrates caregiver training, ward-round participation, and post-discharge support to reduce pneumonia, delirium, and readmissions incidences. Despite these benefits, family engagement remains inconsistently integrated into perioperative settings due to the lack of policies, limited staff training, cultural differences, and workflow concerns. This study reviews recent high-quality evidence, identifies common obstacles, and proposes a structured operational framework for family support comprising: 1. structured perioperative updates at defined milestones; 2. need-based caregiver training; 3. active family inclusion in care planning; 4. integration of digital home monitoring systems; and 5. cultural tailoring of policies and educational materials. If adopted by healthcare systems, this framework can help build perioperative protocols with dedicated resources, supportive policies and leadership endorsement. Future research should explore multicenter implementation, cost-effectiveness, and long-term outcomes of culturally-adapted, digitally-enabled family engagement models.
Introduction
During perioperative care, family involvement is not merely supportive; it is clinically impactful. Evidence from multiple trials shows its ability to improve patient safety, adherence, and recovery. The Tailored, Family-Involved Hospital Elder Life Program (t-HELP) reduced POD in older adults from 19.4%–2.6%, preserved functional independence, and shortened hospital stay by over four days (1). The Family Involvement Program (FIP) offers structured caregiver training, participation in ward rounds, and active involvement in postoperative care, with preliminary data showing reduced pneumonia, delirium, and readmissions (2, 3). In pediatric anesthesia, meta-analyses demonstrate that parental presence at induction of anesthesia (PPIA) reduces both child and parental anxiety without prolonging induction times (4).
These benefits have been observed in pediatric inpatient settings when parents are trained and actively encouraged to engage in their child's care. In a randomized controlled trial (RCT), Çamur and Sarikaya Karabudak (2021) found that structured parental involvement training, covering both routine and moderately invasive care activities, significantly increased parent satisfaction across domains of communication, emotional needs, and overall experience. Importantly, both parent and child anxiety scores decreased more in the intervention group than in controls (p < .05), underscoring that the active engagement of caregivers, when supported by targeted education and observation, can enhance emotional well-being for both patient and family (5). These findings, while from pediatric care, reinforce the value of structured, competency-based family involvement in reducing perioperative anxiety and improving satisfaction, two principles easily transferable to adult surgical contexts.
These principles are transferable to adult surgery: structured, purposeful family presence can improve emotional stability and procedural cooperation. In a multicenter RCT, Aslakson et al. (2019) evaluated pre- and post-operative palliative care interventions for patients undergoing curative-intent upper gastrointestinal cancer surgery. While the primary endpoint of health-related quality of life at 3 months did not differ significantly from surgeon-alone management, early improvements in distress scores were observed. This suggests that structured family-inclusive support—starting before surgery and continuing throughout recovery—is operationally possible and may provide early psychological benefits, even if longer-term outcomes require further study (6).
In another RCT, families receiving structured perioperative updates at key milestones reported significantly lower anxiety, ranking their anxiety as 2.48/5 where 5 represents extreme anxiety on the provided survey and higher satisfaction with communication than those receiving only a final update (7). Moreover, programs such as SAFER Care that use bilingual discharge tools and structured handovers, reduced postoperative ED visits by improving the understanding of care plans (8). Digital home monitoring further extends the benefits of family involvement. After thoracic surgery, digital symptom reporting reduced unplanned healthcare use and enabled earlier interventions, with families trained to assist in monitoring (Nagappa et al., 2025) (9). These tools not only improve recovery but also ensure inclusion through cultural and linguistic adaptation.
Unfortunately, barriers persist as system-level obstacles include unclear protocols, limited staff resources, and the absence of adequate policy (10). Understanding patient and family needs is essential for designing effective perioperative engagement strategies. In a cross-sectional survey at King Abdullah Medical City, Alsabban et al. (2020) found that both patients and family members prioritized clear communication about surgical progress, emotional support, and updates during recovery. Families expressed a strong desire to participate in care decisions and valued structured opportunities to receive timely information from the surgical team. These findings emphasize that effective perioperative family engagement must be responsive to needs and expectations, which may vary by cultural and institutional context. Cultural expectations vary, influencing the acceptability and form of family involvement (11). Family-level challenges include caregiver readiness and emotional burden, though structured programs like FIP have shown minimal burden when designed appropriately (3). Provider-level barriers include workflow concerns and discomfort with family presence in high-acuity situations (Figure 1).
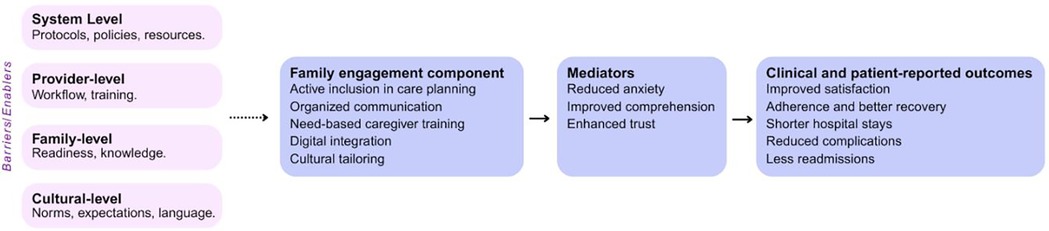
Figure 1. Multi-system variables that influence clinical and patient-reported outcomes. Visual representation of how system, provider, family, and cultural level variables can impact and improve clinical and patient reported outcomes through actively engaging family members in a patient's care.
Some perioperative contexts remain markedly underexplored in terms of family support. For example, a recent scoping review on partner presence during emergency caesarean sections found that, despite widespread parental preference for involvement, the available evidence is sparse, geographically limited, and often of low quality, which represents a priority area for future research (12). Additionally, the use of random domain intercept technology has demonstrated to be a possible efficient and widespread way to survey patients and families regarding their healthcare experiences (13). The ability to gather and analyze these opinions will allow for healthcare centers to improve the perioperative experience for all involved.
Future directions
To transition from theory to practice, healthcare systems should adopt a standardized perioperative familial support framework comprising:
1. Active inclusion in care planning: participation in ward rounds and shared decision-making.
2. Structured communication: timed updates at surgical milestones, adapted to family preferences and cultural norms.
3. Need-based caregiver training: skills in mobilization, wound care, symptom recognition, and medication adherence (2, 14).
4. Digital integration: at home monitoring platforms for symptom tracking and telehealth follow-up.
5. Cultural tailoring: policies and materials adapted to linguistic, cultural, and religious contexts.
These strategies require policy integration, staff training, leadership endorsement, and evaluation using standardized patient- and family-centered care metrics. Future research should focus on multicenter RCTs, cost-effectiveness studies, and long-term functional outcomes to solidify the case for universal adoption.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
NA: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. HB: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. KG: Validation, Writing – original draft, Writing – review & editing. WS: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang Y-Y, Yue J-R, Xie D-M, Carter P, Li Q-L, Gartaganis SL, et al. Effect of the tailored, family-involved hospital elder life program on postoperative delirium and function in older adults: a randomized clinical trial. Arch Intern Med. (2020) 180(1):17–25. doi: 10.1001/jamainternmed.2019.4446
2. Musters SCW, Kreca S, van Dieren S, van der Wal-Huisman H, Romijn JA, Chaboyer W, et al. Activating relatives to get involved in care after surgery: protocol for a prospective cohort study. JMIR Res Protoc. (2023) 12:e38028. doi: 10.2196/38028
3. Musters SCW, Kreca SM, van Dieren S, van der Wal-Huisman H, Romijn JA, Chaboyer W, et al. Family caregiver outcomes after participating in a hospital-based family involvement program after major gastrointestinal surgery: a subgroup analysis of a patient preferred cohort study. Int J Surg. (2024) 110(8):4746–53. doi: 10.1097/JS9.0000000000001473
4. Shih MC, Elvis PR, Nguyen SA, Brennan E, Clemmens CS. Parental presence at induction of anesthesia to reduce anxiety: a systematic research and meta-analysis. J Perianesth Nurs. (2023) 38(1):12–20. doi: 10.1016/j.jopan.2022.03.008
5. Çamur Z, Karabudak SS. The effect of parental participation in the care of hospitalized children on parent satisfaction and parent and child anxiety: randomized controlled trial. Int J Nurs Pract. (2021) 27(5):e12910. doi: 10.1111/ijn.12910
6. Aslakson RA, Chandrashekaran SV, Rickerson E, Fahy BN, Johnston FM, Miller JA, et al. A multicenter, randomized controlled trial of perioperative palliative care surrounding cancer surgery for patients and their family members (PERIOP-PC). J Palliat Med. (2019) 22(S1):44–57. doi: 10.1089/jpm.2019.0130
7. Howe LS, Wigmore D, Nelms N, Schottel P, Bartlett C, Halsey D, et al. Perioperative family updates reduce anxiety and improve satisfaction: a randomized controlled trial. J Patient Cent Res Rev. (2021) 8(2):107–12. doi: 10.17294/2330-0698.1805
8. Agency for Healthcare Research and Quality. Engaging Family Caregivers with Structured Communication for Safe Care Transitions (Making Healthcare Safer IV: An Evidence Review of Patient Safety Practices). Rockville, MD: U.S. Department of Health and Human Services (2023). Available online at: https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/engaging-caregivers-protocol.pdf
9. Nagappa M, Subramani Y, Yang H, Wood N, Querney J, Fochesato L-A, et al. Enhancing quadruple health outcomes after thoracic surgery: feasibility pilot randomized controlled trial using digital home monitoring. JMIR Perioper Med. (2025) 8:e58998. doi: 10.2196/58998
10. Hamilton G, Corlett J, Dowling M. Adult-trained perioperative nurses’ practice of family-centered care. Br J Nurs. (2014) 23(9):477–82. doi: 10.12968/bjon.2014.23.9.477
11. Alsabban W, Alhadithi A, Faisal SA, Abdullah Mutlaq AK, Altheeb S, Ahmed SB. Assessing needs of patients and families during the perioperative period at king abdullah medical city. Perioper Med. (2020) 9:1–8. doi: 10.1186/s13741-020-00141-9
12. Nedergaard HK, Balaganeshan T, Weitling EE, Petersen HS, Brøchner AC. Presence of the partner in the operating room during emergency caesarean section: a scoping review. Eur J Anaesthesiol. (2022) 39(12):939–52. doi: 10.1097/EJA.0000000000001761
13. Saasouh W, Ghanem K, Al-Saidi N, LeQuia L, McKelvey G, Jaffar M. Patient-centered perspectives on perioperative care. Front Anesth. (2024) 3:1267127. doi: 10.3389/fanes.2024.1267127
14. Zhu S, Yang C, Bai Y, Kang L, Li T, Yang X, et al. Effects of a perioperative support program on reducing psychological distress for family caregivers of patients with early-stage lung cancer: a pilot randomised controlled trial. BMC Nurs. (2025) 24(1):Article 220. doi: 10.1186/s12912-025-02857-9
Keywords: perioperative care, familial support, patient safety, communication, patient satisfaction, patient centered approach, family-centered care
Citation: Assaf N, Bazzi H, Ghanem K and Saasouh W (2025) Optimizing surgical outcomes through increased familial support in the perioperative period. Front. Anesthesiol. 4:1650491. doi: 10.3389/fanes.2025.1650491
Received: 20 June 2025; Accepted: 26 August 2025;
Published: 15 September 2025.
Edited by:
Alparslan Turan, Cleveland Clinic, United StatesReviewed by:
Weiwei Zhang, Tsinghua University, ChinaCopyright: © 2025 Assaf, Bazzi, Ghanem and Saasouh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wael Saasouh, d2FlbC5zYWFzb3VoQHdheW5lLmVkdQ==
 Nour Assaf1
Nour Assaf1 Kristina Ghanem
Kristina Ghanem Wael Saasouh
Wael Saasouh