Abstract
Background:
Klebsiella pneumoniae is a common Gram-negative bacterium frequently associated with wound infections. A major public health concern is the emergence of carbapenem-resistant strains, particularly those carrying the blaKPC gene. This study aimed to detect the blaKPC gene and to determine the antibiotic resistance patterns of K. pneumoniae isolates obtained from wound specimens in a tertiary care hospital in North India.
Methods:
A total of 1,080 wound swab specimens were collected between October 2023 and September 2024. The isolates were identified as K. pneumoniae using the VITEK-2 identification system and standard biochemical tests. Antimicrobial susceptibility was determined with the Kirby–Bauer disk diffusion method and broth microdilution, interpreted according to the Clinical and Laboratory Standards Institute (CLSI) guidelines. Carbapenemase production was assessed using the modified Hodge test. Real-time quantitative PCR (qPCR), with 16S rRNA as the internal control, was employed to detect the blaKPC gene in isolates resistant to meropenem.
Results:
Out of 560 K. pneumoniae isolates, 110 (19.6%) were resistant to meropenem. These resistant isolates also displayed high rates of multidrug resistance, with over 90% resistant to amikacin, ceftazidime, ampicillin, and cefazolin. The qPCR assay revealed that all 110 meropenem-resistant isolates carried the blaKPC gene, with PCR cycle threshold (Ct) values ranging from 12 to 32. No amplification was observed in the meropenem-sensitive negative controls. The diagnostic performance of the qPCR assay demonstrated an area under the curve (AUC) of 0.99, confirming its high accuracy as a diagnostic tool. Furthermore, 83.6% of the isolates harboring the blaKPC gene.
Conclusion:
In conclusion, K. pneumoniae isolates exhibit a concerning rate of carbapenem resistance mediated by the blaKPC gene. Antimicrobial stewardship and molecular surveillance are crucial for the prevention of the spread of carbapenem-resistant K. pneumoniae in clinical settings.
Introduction
Gram-negative bacteria pose a major threat to healthcare systems across the world. Klebsiella pneumoniae is a rod-shaped, capsulated, facultative, anaerobic Gram-negative bacterium belonging to the family Enterobacteriaceae. It can be seen in soil and water and in various hosts, including people and animals (AlTamimi et al., 2017). There is substantial mortality associated with community- or hospital-acquired infections with this bacterium, particularly in immunocompromised individuals (Gandor et al., 2022). The Centers for Disease Control and Prevention (CDC) categorized carbapenem-resistant K. pneumoniae (CRKP) as an urgent threat to human health in 2019, citing its resistance to such antibiotics as carbapenem (Huang et al., 2023). Carbapenem-resistant Enterobacterales (CRE) are microorganisms that destroy carbapenems or produce carbapenem (Papanikolopoulou et al., 2024).
The increasing antibiotic resistance of Enterobacterales limits the services that can be used to treat infection. Carbapenems are commonly used as a treatment measure against infections caused by organisms that are resistant to a variety of drugs (Dong et al., 2022; Darby et al., 2024). However, it is unfortunate that the bacteria have also developed defenses against this line of drugs. These are the organisms that comprise the Enterobacterales family and are resistant to carbapenem (i.e., CRE). CRE is characterized by the presence of a carbapenemase or the resistance to at least one carbapenem (van Duin and Paterson, 2020). Carbapenemase-producing Enterobacterales (CRE) are of particular concern owing to having a beta-lactamase called carbapenemase that can hydrolyze the antibiotics of the carbapenem group or resistance to a carbapenem to which the organism is not known to be naturally resistant (Tamma et al., 2024). Due to its wide range, carbapenems are typically employed only in the periodical treatment of multidrug-resistant (MDR) bacteria (Tamma et al., 2023).
The most common class A carbapenemases are K. pneumoniae carbapenemase (KPC), imipenem (IMI)-hydrolyzing beta-lactamase, class A non-metallo-carbapenemases (NMC-A), Guyana extended-spectrum (GES) beta-lactamase, and Serratia marscescens enzyme (SME) (Mutuku et al., 2022a, b). Class A carbapenemases possess a serine amino acid in the active sites and are able to cleave penicillins, cephalosporins, carbapenems, and aztreonam (AZT). The most common gene of the carbapenemase-producing CRE is KPC and is the most prevalent in the United States. However, they are common to people in the Middle East, Africa, Asia, South America, Spain, France, Belgium, and Romania (Albiger et al., 2015). According to the Center for Disease Dynamics, Economics, and Policy (CDDEP), up to 60% Indian K. pneumoniae isolates are resistant to carbapenems and 80% are resistant to cephalosporins. Parveen et al. (2010) noted that the rate of individuals resistant to carbapenem rose to 44% in 2010 in comparison to the figure in 2008, i.e., 9%.
KPC is currently an Ambler class A beta-lactamase and is the most common carbapenem-resistant enzyme occurring globally. It is also very dominant in North America and Europe. The primary origin of carbapenem resistance is the class B New Delhi metallo-lactamase (NDM) that is produced by the Ambler (Johnson and Woodford, 2013).
Clinical dissemination of the blaKPC gene-bearing bacteria can add to the problem of antibiotic resistance globally due to the promotion of the increase of meropenem (MEM)- and IMI-resistant strains of bacteria (Richter et al., 2012). It appears that KPC is topical due to the mistreatment and the misuse of antibiotics named as carbapenem, which is one of the risks currently posing a threat with regard to the spread of the carbapenemase enzyme. Due to an outbreak in the number of strains with the blaKPC gene, the KPC and OXA-48 strains can further intensify (Bina et al., 2015). The antibiotic resistance attributable to KPC is transmissible, and it spreads extremely quickly, particularly where the transferred genes are expressing carbapenemase. This causes serious pandemics and results in the number of treatments being very scarce. The most common group is the carbapenemase gene that is sharable among humans. There has been a connection between morbidity and mortality and severe KPC-KP infections treated with insufficient empirical therapy (Adhikari et al., 2018; Giacobbe et al., 2023).
There is a clinically significant global concern over carbapenem resistance in K. pneumoniae, in particular MEM resistance. This study was designed to assess the current distribution of the blaKPC gene among clinical isolates obtained from wound samples using real-time quantitative reverse transcription PCR (qRT-PCR). This approach accurately identified the carbapenemase genes in pre-validated clinical CRE isolates, demonstrating its excellent specificity and sensitivity. A simple, sensitive technique was developed for the rapid detection of clinical carbapenemases.
Materials and methods
Study design and sample collection
This prospective study was conducted in Dasmesh Hospital in Faridkot, India, between October 2023 and September 2024. A total of 1,080 non-duplicate wound swab specimens were collected from patients presenting with wound infections. The specimens were processed in the Microbiology Laboratory using conventional and molecular methods. The ethical principles of the World Medical Association and the Declaration of Helsinki were used in the conduct of the study to ascertain safe handling of the bacterial strains used and for the protection of the general public health. This study was approved by the Institutional Review Board of the Dasmesh Institute of Research College.
Isolation and identification of K. pneumoniae
Identification of the K. pneumoniae isolates was done first using conventional microbiology methods according to Koshi (2001). The colony morphology, the Gram reaction, and a set of biochemical tests confirmed the large, mucoid, lactose-fermenting colony production on MacConkey agar. The final identification of the species within the bacteria was done in the automated identification system VITEK 2 (bioMerieux, Marcy-l’Étoile, France).
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing (AST) was carried out utilizing both the Kirby–Bauer disk diffusion and the broth microdilution (BMD) methods. Disc diffusion was performed on Mueller–Hinton agar, and the findings were interpreted using the Clinical and Laboratory Standards Institute (CLSI) recommendations document M100, Performance Standards for Antimicrobial Susceptibility Testing, 35th edition (CLSI, 2025). The following antimicrobials were tested: ampicillin (AMP, 10 μg), AMP–sulbactam (10/10 μg), ceftazidime (CAZ, 30 μg), cefuroxime (30 μg), cefotaxime (CTX, 10 μg), cefepime (5 μg), AZT (30 μg), ertapenem (10 μg), and IMI (10 μg). The fluoroquinolones included levofloxacin (LEV, 5 μg) and ciprofloxacin (CIP, 5 μg). Gentamicin (10 μg) is an aminoglycoside. All other/cotrimoxazole (1.25/23.75 μg) disks were obtained from HiMedia (Thane, India).
Broth microdilution
The minimum inhibitory concentrations (MICs) of carbapenem were determined using a method based on BMD. The MIC panels were produced internally in accordance with the principles set forth by the CLSI (CLSI, 2024). The MICs of CTX, CAZ, AZT, MEM, CIP, amikacin (AN), AMP, LEV, trimethoprim (TMP), nitrofurantoin (NIT), tigecycline (TIG), and tetracycline (TET) were determined. The MICs of MEM were interpreted based on the CLSI breakpoints as susceptible (≤ 4 µg/ml), intermediate (8 µg/ml), or resistant (≥ 16 µg/ml).
Phenotypic detection of KPC production
The modified Hodge test (MHT) was used to determine whether carbapenemase production is present in the carbapenem-resistant isolates in accordance with the CLSI guidelines. The occurrence of a cloverleaf-like depression around the MEM disk was believed to denote carbapenemase activity (Zohu et al., 2018). The disks containing MEM were the negative controls. The positive control of the MHT was K. pneumoniae ATCC BAA-1705, while the negative control was K. pneumoniae ATCC BAA-1706. Spots of higher growth distortion around the MEM disks implied the formation of carbapenemase. Isolates that were determined to be KPC (blaKPC) producers using MIC determination and the MHT were selected for testing using real-time qPCR that targeted the blaKPC gene. Isolates that tested negative with these phenotypic methods were excluded from the molecular analysis.
Quality control
Quality control was assured in the AST and the phenotypic confirmation of carbapenemase production using the MHT with standard reference strains. For the MHT, K. pneumoniae ATCC BAA-1705 was used as the positive control strain and K. pneumoniae ATCC BAA-1706 as the negative control strain, while MEM disks were used as the test antibiotic.
Genomic DNA extraction
Extraction of plasmid DNA was according to the manufacturer, performed using the QIAprep Spin Miniprep Kit (QIAGEN, Hilden, Germany). Briefly, 2 ml of an overnight bacterial culture was centrifuged at 10,000 × g for 5 min and a cell pellet obtained. The supernatant was disposed of and the pellet suspended in 250 µl of buffer P1 in the presence of RNase A to remove the contamination of RNA. This was followed by lysing the content with 250 µl of buffer P2 and subsequent incubation for 5 min. Centrifugation was performed, followed by 350 μl of buffer N3, which neutralizes the lysis. Following the loading of a clear supernatant on a QIAprep Spin Column, the column was then successively washed with 500 μl of buffer PB and 750 μl of buffer PE. Any excess buffer was removed by centrifugation. Of buffer EB (10 mM Tris–Cl, pH 8.5), 60 μl was used to elute the plasmid DNA. Its concentration and purity were assessed using a NanoDrop spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA), and the samples were stored at −20°C until required.
Primer and probe sequences
The TaqMan Gene Expression Master Mix (lot no. 4369016; Thermo Fisher Scientific, Waltham, MA, USA), which contains AmpliTaq Gold DNA Polymerase Ultra Pure, was used for real-time PCR with primers and probes targeting the blaKPC gene: forward primer 5′-GGC CGC CGT GCA ATA C-3′, reverse primer 5′-GCC GCC CAA CTC CTT CA-3′, and FAM probe 5′-TG ATA ACG CCG CCG CCA ATT TGT-3′. 16S rRNA served as the internal control using the forward primer 5′-TGG AGC AGC ATG TGG TTT AAT TCG A-3′, the reverse primer 5′-TGC GGG ACT TAA CCC AAC AAC AAC A-3′, and the CY5 probe 5′-CA CGA GCT GAC GAC GAC ARC CAT GCA-3′.
Detection of the blaKPC gene by real-time PCR
All reagents were prepared and treated on ice to preserve the activity of the enzymes and to prevent degradation. The primer and probe mixture was prepared by combining 20 µM of each primer and 10 µM of each probe. The master mix was made on ice with 10 µl of the Probe PCR Master Mix, 5 µl of the primer–probe mix, and 3 µl of sterile water prepared on ice for every 20 µl reaction. Once the master mix was thoroughly mixed, 18 µl of this mixture was added into a 96-well PCR plate. A 2-µl DNA template was added to each of the reaction wells.
Thermal cycle conditions
Real-time PCR was carried out according to the CDC protocol, with an initial denaturation step at 95°C for 3 min, denaturation at 95°C for 3 s, and annealing/extension at 60°C for 30 s (40 cycles). Amplification was regarded positive only if the cycle threshold (Ct) value was between 10 and 32. The amplification of the 16S rRNA gene detected between cycles 31 and 40 and the no-template control (NTC) had to exhibit no amplification of the target genes (Ct > 40).
Sensitivity and specificity
The analytical sensitivity of the assay was also determined with real-time PCR at 10-fold serial dilutions of the K. pneumoniae cultures harboring the KPC, starting at an initial concentration of 8.0 × 107 CFU/ml. The sensitivity of the assay was high in terms of analysis as reduction in the bacterial loadings allowed the target gene to be detected. The phenotypic reference tool was MHT, also described as MHT. The MHT was applied to compare the sensitivity and the specificity of the real-time PCR assay. The real-time PCR test, as a method for the detection of blaKPC in inculcated isolates, proved to be fast and extremely specific, with a turnaround time of 2–3 h.
Results
Distribution and identification of K. pneumoniae from wound infections
Of the total 1,080, only 560 (51.8%) K. pneumoniae samples were examined. Of these, 19.6% (n = 110) of the isolates were found to be KPC producers. The initial identification also involved Gram staining, routine biochemical testing, and colony examination. The determination of the first antimicrobial susceptibility of all the isolates of K. pneumoniae was performed with the Kirby–Bauer disk diffusion procedure using IMI and MEM. reduced sensitivity to carbapenems (with minimum zone diameter less than that of the CLSI 2023 interpretation of breakpoints) to carbapenems were additionally assessed using BMD. Resistant isolates were then characterized phenotypically with regard to carbapenemase activity. The MHT was used to validate the carbapenemase production phenotypically (Figure 1, MHT). These isolates were then chosen for the blaKPC gene-focused molecular investigation.
Figure 1

Modified Hodge test showing the phenotypic characterization of the carbapenemase-producing Klebsiella pneumoniae clinical isolates.
Antimicrobial susceptibility pattern of K. pneumoniae
In this study, a total of 560 K. pneumoniae clinical isolates were used to examine their susceptibility to antimicrobial agents. Their resistance, on an individual antimicrobial agent basis, is shown in Table 1. The AMP resistance rates were found to be the highest (9905%). This was followed by AZT (85.0%), CAZ (85.0%), cefuroxime (80.0%), LEV (77.0%), and ceftriaxone (74.0%). The resistance levels of CIP (63.0%) and TMP–sulfamethoxazole (60.0%) were also high. There were higher susceptibility rates with the carbapenems IMI (44.0%) and MEM (44.0%), as well as gentamicin (54.0%) and AN (60.0%).
Table 1
| S. no. | Clinical Isolates | MEM | CAZ | CTX | AZT | CIP | AN | AMP | TMP | TIG | TET | NIT | LEV |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | KPC001 | 32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 32 |
| 2 | KPC002 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 2 | 0.5 | 4 | 2 |
| 3 | KPC003 | 4 | 0.25 | 4 | 0.25 | 0.06 | 1 | 8 | 0.25 | 2 | 0.5 | 4 | 2 |
| 4 | KPC004 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 4 | 1 | 16 | 16 |
| 5 | KPC005 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 16 |
| 6 | KPC006 | >16 | 16 | 16 | 4 | >16 | >16 | >32 | >16 | 2 | 2 | 8 | 4 |
| 7 | KPC007 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 2 | 0.125 | 16 | 4 |
| 8 | KPC008 | 8 | >16 | 16 | >16 | >16 | >16 | >32 | >16 | 1 | 0.25 | 16 | 2 |
| 9 | KPC009 | 16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 2 | 0.5 | 4 | 0.25 |
| 10 | KPC010 | 4 | 16 | 16 | 0.5 | >16 | >16 | >32 | >16 | 0.5 | 0.125 | 4 | 2 |
| 11 | KPC011 | 8 | 0.125 | 0.03 | >16 | 0.03 | 0.5 | 16 | 0.06 | 0.5 | 0.125 | 8 | 8 |
| 12 | KPC012 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 1 | 0.5 | 8 | 16 |
| 13 | KPC013 | 8 | >16 | 16 | 16 | >16 | >16 | >32 | 16 | 1 | 8 | 16 | 32 |
| 14 | KPC014 | 4 | >16 | 4 | >16 | >16 | >16 | >32 | >16 | 2 | 8 | 16 | 32 |
| 15 | KPC015 | 4 | >16 | >16 | 16 | >16 | >16 | >32 | >16 | 0.3 | 4 | 16 | 0.5 |
| 16 | KPC016 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | >8 | >16 | >16 | 16 |
| 17 | KPC017 | >16 | 16 | 16 | 8 | >16 | >16 | >32 | >16 | 1 | 0.25 | 4 | 0.13 |
| 18 | KPC018 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 0.5 | 2 | 8 | 2 |
| 19 | KPC019 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 0.5 | 0.125 | 2 | 2 |
| 20 | KPC020 | 8 | 0.06 | 0.03 | 4 | 0.125 | 0.25 | 8 | 0.03 | 1 | 2 | 4 | >16 |
| 21 | KPC021 | 8 | >16 | >16 | 4 | >16 | >16 | >32 | 0.03 | 1 | 8 | >16 | >16 |
| 22 | KPC022 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 0.5 | 0.5 | 2 | 0.05 |
| 23 | KPC023 | 4 | 0.06 | 8 | 4 | 1 | 4 | 16 | 1 | 4 | >16 | >16 | 8 |
| 24 | KPC024 | 8 | 8 | 8 | 4 | >16 | 2 | 16 | >16 | 0.3 | 1 | 4 | 8 |
| 25 | KPC025 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 2 | 2 | 8 | 16 |
| 26 | KPC026 | 4 | 16 | 16 | 8 | >16 | >16 | >32 | >16 | 2 | 8 | 16 | 8 |
| 27 | KPC027 | >16 | >16 | >16 | >16 | >16 | >16 | >32 | >16 | 8 | >16 | >16 | >32 |
| 28 | KPC028 | 16 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 0.5 | 2 | 4 | 0.5 |
| 29 | KPC029 | 32 | >32 | >32 | >32 | >32 | >32 | >32 | 1 | 2 | 4 | 16 | 16 |
| 30 | KPC030 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 4 | 16 | >16 | >16 |
| 31 | KPC031 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 1 | 4 | 16 | >16 |
| 32 | KPC032 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 1 | 1 | 4 | >16 | >16 |
| 33 | KPC033 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 2 | 1 | 4 | 2 |
| 34 | KPC034 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 8 | >16 | >16 | 8 |
| 35 | KPC035 | 16 | 16 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 8 |
| 36 | KPC036 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | >32 |
| 37 | KPC037 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 32 |
| 38 | KPC038 | 16 | 16 | 16 | 16 | >32 | 8 | >32 | >32 | 1 | 0.5 | 4 | 2 |
| 39 | KPC039 | 32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 2 | 2 | 8 | 8 |
| 40 | KPC040 | 4 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 8 |
| 41 | KPC041 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 8 |
| 42 | KPC042 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 8 |
| 43 | KPC043 | 4 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | >8 | >16 | >16 | 8 |
| 44 | KPC044 | >16 | 32 | 32 | 32 | 32 | 32 | >32 | 32 | >8 | >16 | 16 | 16 |
| 45 | KPC045 | >16 | >16 | >32 | >32 | 32 | >32 | >32 | >16 | 2 | >16 | >16 | 32 |
| 46 | KPC046 | >16 | >16 | >32 | >32 | 32 | >32 | >32 | >16 | >4 | >16 | >16 | >32 |
| 47 | KPC047 | >16 | >16 | >32 | >32 | 32 | >16 | >32 | 16 | 2 | >16 | 8 | 16 |
| 48 | KPC048 | 4 | 0.125 | 32 | 0.25 | 0.5 | >16 | 8 | 4 | 2 | 32 | 32 | 16 |
| 49 | KPC049 | >16 | >16 | 32 | >32 | >32 | >16 | >32 | >16 | >4 | 8 | 16 | 16 |
| 50 | KPC050 | >16 | >16 | >32 | 32 | >32 | >16 | >32 | >16 | 4 | 1 | >16 | 16 |
| 51 | KPC051 | 8 | <0.03 | 0.06 | >16 | 0.06 | >16 | 8 | 2 | 4 | 1 | >16 | 8 |
| 52 | KPC052 | >16 | >16 | >32 | >16 | >32 | >32 | >32 | >16 | 1 | >16 | >16 | 8 |
| 53 | KPC053 | >16 | >16 | >32 | >16 | >32 | >32 | >32 | >16 | >4 | >16 | >16 | 16 |
| 54 | KPC054 | >16 | 0.25 | 0.5 | 0.5 | 0.125 | >16 | 4 | 4 | 4 | >16 | >16 | 32 |
| 55 | KPC055 | >16 | >32 | 32 | >16 | >16 | >16 | >64 | >32 | >8 | >32 | >32 | 32 |
| 56 | KPC056 | 4 | >32 | >32 | >16 | >16 | >16 | >64 | >32 | 0.5 | >32 | 16 | 32 |
| 57 | KPC057 | 32 | >32 | >32 | 16 | >16 | >16 | >64 | >16 | >4 | 16 | >32 | 32 |
| 58 | KPC058 | >32 | >32 | >32 | >16 | >16 | >16 | 64 | >16 | >8 | >32 | >32 | >32 |
| 59 | KPC059 | >32 | >32 | >32 | 16 | 0.03 | 0.06 | 8 | >16 | >8 | 16 | >32 | <4 |
| 60 | KPC060 | 16 | >32 | >32 | >16 | >16 | >32 | >64 | >16 | >8 | >32 | 16 | <4 |
| 61 | KPC061 | >32 | >32 | >32 | 8 | 16 | >32 | 64 | >16 | 2 | >32 | >32 | <4 |
| 62 | KPC062 | >32 | >32 | >32 | >16 | >16 | >16 | >64 | >16 | 2 | 16 | >32 | <4 |
| 63 | KPC063 | >32 | >32 | >32 | >16 | >16 | >16 | >64 | >16 | >4 | >32 | >32 | 32 |
| 64 | KPC064 | >32 | >32 | 32 | 4 | 16 | >16 | >64 | >16 | >4 | >32 | >32 | >32 |
| 65 | KPC065 | <2 | 16 | 32 | 4 | 16 | >32 | 8 | 4 | 4 | <2 | >32 | <2 |
| 66 | KPC066 | >32 | >32 | 32 | >16 | >16 | >32 | >64 | >16 | 4 | 4 | <2 | 32 |
| 67 | KPC067 | <2 | >32 | 16 | 4 | >16 | >16 | >64 | >16 | 2 | <2 | >32 | 16 |
| 68 | KPC068 | >32 | >32 | 32 | 4 | 16 | >16 | >64 | >16 | >8 | 8 | >32 | 32 |
| 69 | KPC069 | >32 | >32 | 32 | >16 | >16 | >16 | >64 | >32 | >4 | >32 | >32 | 32 |
| 70 | KPC070 | <2 | <2 | 2 | 8 | 16 | >16 | >64 | >32 | 4 | <2 | >32 | >32 |
| 71 | KPC071 | >64 | >64 | >32 | >16 | 16 | >16 | >64 | >16 | >8 | >64 | >64 | >64 |
| 72 | KPC072 | >32 | >32 | >32 | >32 | >16 | >32 | >64 | >16 | >4 | >32 | >32 | >32 |
| 73 | KPC073 | 16 | >32 | >32 | >32 | >16 | >32 | >64 | >16 | 2 | >32 | >32 | >32 |
| 74 | KPC074 | >32 | >32 | >32 | >32 | >16 | >16 | >64 | >16 | 2 | >32 | >32 | >32 |
| 75 | KPC075 | 8 | >32 | >32 | >32 | >16 | >16 | >64 | >16 | >4 | >32 | >32 | >32 |
| 76 | KPC076 | >32 | 16 | 32 | >32 | >32 | >32 | >64 | >16 | 2 | 4 | >32 | 32 |
| 77 | KPC077 | >32 | 4 | 2 | >32 | >32 | >32 | 32 | >32 | >8 | >16 | >32 | 32 |
| 78 | KPC078 | 4 | >32 | 16 | >32 | >32 | >16 | 32 | >32 | >8 | >32 | >32 | 32 |
| 79 | KPC079 | 8 | >32 | 32 | >32 | >32 | >32 | 32 | >32 | >8 | >32 | >32 | 32 |
| 80 | KPC080 | 8 | >32 | >32 | >32 | >32 | >32 | >64 | >32 | >8 | 32 | >32 | 16 |
| 81 | KPC081 | >64 | >64 | >32 | >32 | >32 | >32 | 64 | >32 | >8 | >64 | >64 | >64 |
| 82 | KPC082 | 8 | <2 | 2 | 16 | >32 | >32 | 16 | >32 | 2 | <2 | >32 | <2 |
| 83 | KPC083 | 4 | >32 | 32 | >32 | >32 | >32 | 32 | >32 | >8 | >32 | 32 | 16 |
| 84 | KPC084 | >32 | >32 | >32 | >32 | >32 | >32 | >64 | >16 | >8 | >32 | >32 | >32 |
| 85 | KPC085 | 16 | >32 | >32 | >32 | >32 | >16 | >64 | >16 | >4 | 32 | 32 | 16 |
| 86 | KPC086 | 8 | >32 | >32 | >32 | >32 | >16 | >64 | >32 | 2 | >32 | >32 | >32 |
| 87 | KPC087 | 16 | 16 | >32 | >32 | >32 | >32 | >64 | >32 | >8 | 16 | >32 | 16 |
| 88 | KPC088 | 8 | >32 | >32 | 32 | >32 | >32 | >64 | >32 | 2 | >32 | >32 | 16 |
| 89 | KPC089 | >32 | >32 | >32 | 32 | >32 | >16 | >64 | >32 | 2 | 2 | >32 | >32 |
| 90 | KPC090 | 16 | >32 | >32 | 32 | >32 | >32 | >64 | >32 | 1 | 2 | >32 | 4 |
| 91 | KPC091 | 32 | >32 | >32 | 16 | >32 | >32 | >64 | >16 | 4 | >32 | >32 | >32 |
| 92 | KPC092 | >32 | >32 | >32 | 32 | 32 | >16 | >64 | >16 | >4 | >32 | >32 | 32 |
| 93 | KPC093 | 32 | >32 | >32 | 32 | 16 | >16 | 32 | >32 | 8 | 2 | >32 | 0.5 |
| 94 | KPC094 | 8 | >32 | >32 | 32 | 32 | >32 | 32 | >32 | >4 | >32 | >32 | >32 |
| 95 | KPC095 | 8 | 0.5 | 0.25 | 32 | 0.125 | >32 | 16 | >32 | 2 | 0.25 | 4 | 0.5 |
| 96 | KPC096 | 32 | 32 | 32 | >32 | 32 | >16 | 32 | >16 | >4 | >16 | >32 | >32 |
| 97 | KPC097 | >16 | >8 | 32 | >32 | 16 | >16 | >64 | >16 | 4 | >8 | >16 | 2 |
| 98 | KPC098 | >16 | >8 | 16 | 32 | 16 | >16 | >64 | >32 | 4 | >8 | >16 | 4 |
| 99 | KPC099 | >16 | >8 | >32 | >32 | 32 | >16 | >64 | >32 | 4 | >8 | >16 | 4 |
| 100 | KPC100 | >16 | >8 | >32 | >32 | >32 | >16 | >64 | >32 | 4 | >8 | >16 | 4 |
| 101 | KPC101 | >16 | >8 | >32 | >32 | >32 | 32 | >64 | >16 | 2 | >8 | >16 | 4 |
| 102 | KPC102 | >16 | >8 | 16 | 32 | >32 | >32 | >64 | >16 | 2 | >8 | >16 | 4 |
| 103 | KPC103 | >16 | >8 | >32 | 32 | >32 | >32 | >64 | >32 | 2 | >8 | >16 | 2 |
| 104 | KPC104 | >16 | >8 | 16 | 32 | >32 | >32 | >64 | >32 | 2 | >8 | >16 | 4 |
| 105 | KPC105 | >16 | >8 | 32 | 16 | >32 | >32 | >64 | >32 | 4 | >8 | >16 | 4 |
| 106 | KPC106 | >16 | >8 | 32 | 16 | >32 | >32 | >64 | >16 | 4 | >8 | >16 | 2 |
| 107 | KPC107 | >32 | >32 | >32 | >32 | >32 | >32 | 64 | >16 | 4 | 0.25 | 16 | >32 |
| 108 | KPC108 | >16 | >32 | >32 | >32 | 0.125 | 0.5 | 8 | 2 | 4 | 0.5 | >32 | 16 |
| 109 | KPC109 | 8 | >32 | >32 | 32 | 16 | 32 | 32 | >16 | >32 | 0.063 | >32 | 16 |
| 110 | KPC110 | >32 | >32 | 16 | >32 | 32 | 32 | 32 | >16 | >32 | 0.5 | >32 | >32 |
MIC values of 110 ioslates.
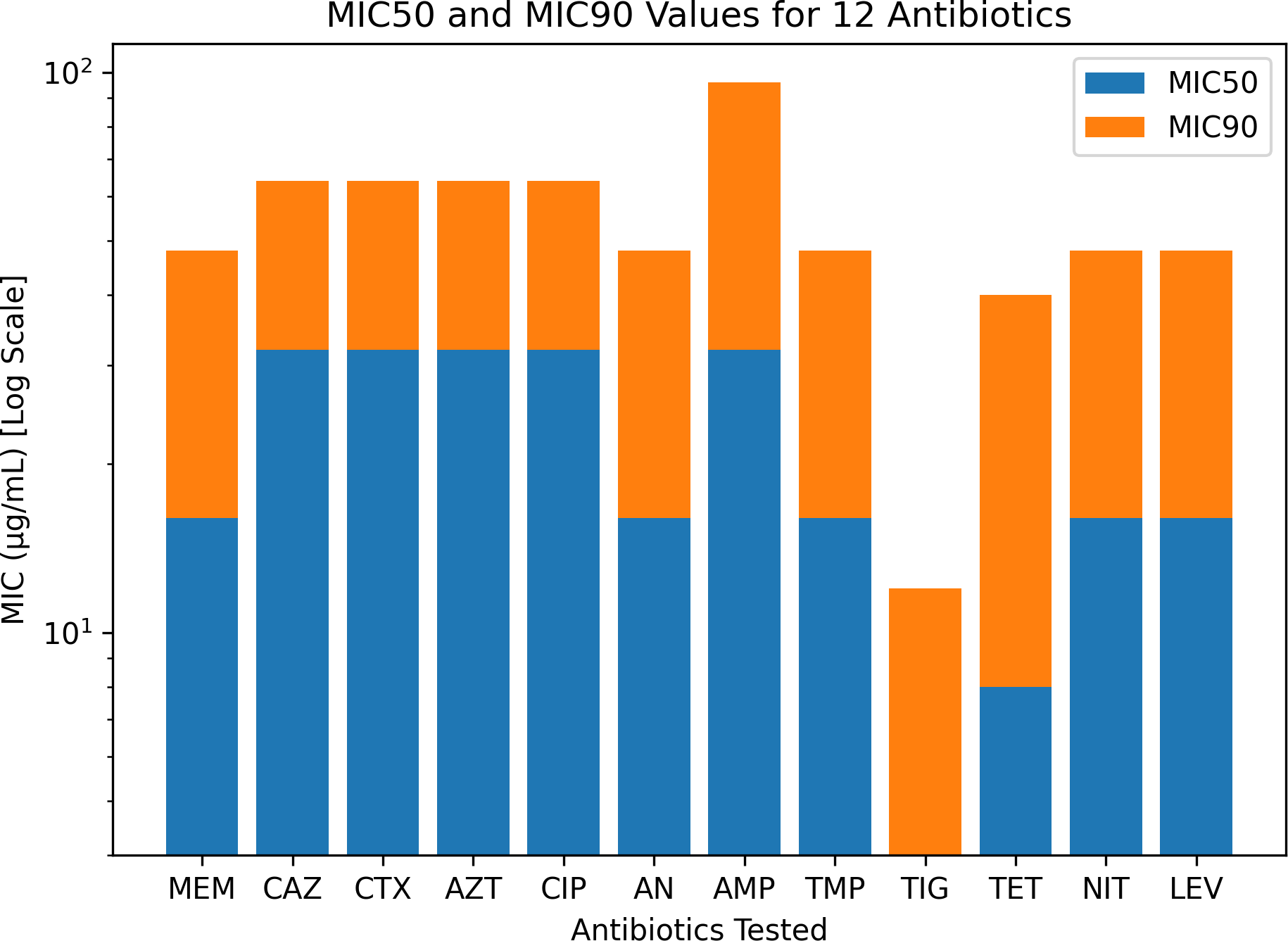
Among the 110 clinical isolates of K. pneumoniae, high resistance was observed against AMP (100%), AN (94.5%), CAZ (92.7%), CIP (91.8%), TMP (91.8%), CTX (91.0%), and AZT (89.1%). Significant resistance was also noted for LEV (91.0%), NIT (89.1%), TET (84.5%), and TIG (76.3%). The resistance rates were comparatively lower for some other antibiotics (Figure 2). The MIC interpretation against the 110 clinical K. pneumoniae isolates is shown in Figure 3. In addition, Figure 4 shows the distribution of the MICs of MEM alone, out of which 12 (10.9%) isolates had low MICs (≤4 μg/ml), 6 (5.4%) isolates had intermediate resistance (MIC = 8–16 μg/ml), and 92 (83.6) isolates displayed high resistance (MICs > 16 μg/ml). Histogram plots were used to represent the distribution of the MICs (in micrograms per milliliter) for the 110 K. pneumoniae clinical isolates tested against 12 antibiotics (Figure 5). The MICs from the BMD are presented in a Supplementary Table.
Figure 2
Antibiotic resistance patterns of the Klebsiella pneumoniae clinical isolates (n = 110). The percentage of resistant isolates is shown for each antibiotic tested, illustrating the resistance landscape across multiple antimicrobial classes.
Figure 3

Minimum inhibitory concentration (MIC) interpretation for the 110 Klebsiella pneumoniae clinical isolates against 12 antibiotics: meropenem (MEM), ceftazidime (CAZ), cefotaxime (CTX), aztreonam (AZT), ciprofloxacin (CIP), amikacin (AN), ampicillin (AMP), trimethoprim (TMP), tigecycline (TIG), tetracycline (TET), nitrofurantoin (NIT), and levofloxacin (LEV).
Figure 4

Minimum inhibitory concentration (MIC) interpretation of the Klebsiella pneumoniae isolates specifically against meropenem (MEM), demonstrating the distribution of the susceptible, intermediate, and resistant categories.
Figure 5
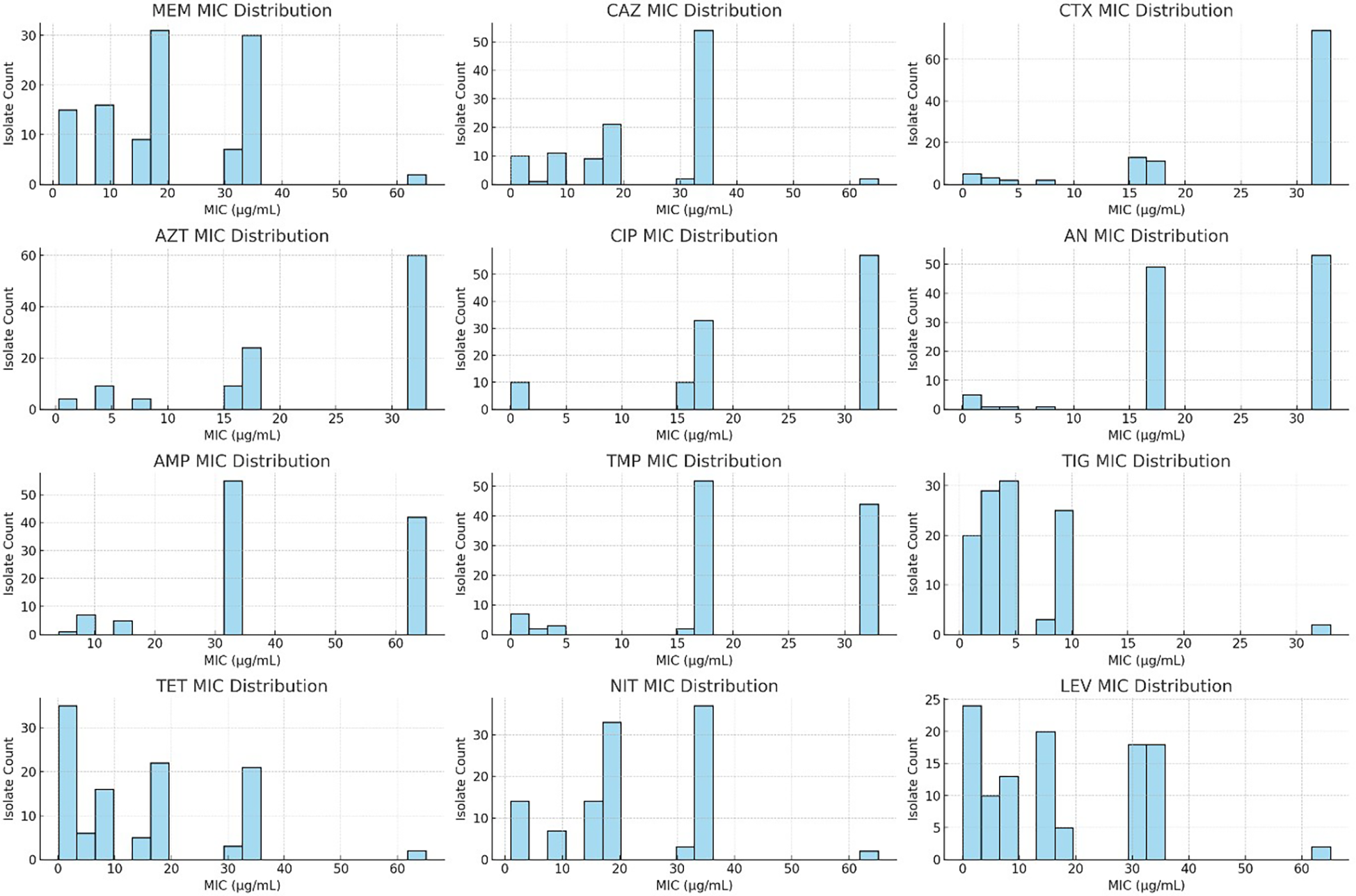
Minimum inhibitory concentration (MIC) distribution of the Klebsiella pneumoniae clinical isolates against 12 commonly used antibiotics. The histogram plots display the MIC values (in micrograms per milliliter) for the 110 isolates tested against meropenem (MEM), ceftazidime (CAZ), cefotaxime (CTX), aztreonam (AZT), ciprofloxacin (CIP), amikacin (AN), ampicillin (AMP), trimethoprim (TMP), tigecycline (TIG), tetracycline (TET), nitrofurantoin (NIT), and levofloxacin (LEV). Values reported as “>X” were transformed (e.g., “>32” as 33) to allow histogram visualization. Elevated MICs, particularly for β-lactams and fluoroquinolones, indicate multidrug resistance trends.
Meropenem susceptibility and KPC production in K. pneumoniae
Of the 560 clinical isolates of K. pneumoniae evaluated, 110 (19.6%) isolates were resistant to MEM. Real-time PCR confirmed the presence of the blaKPC gene. On the other hand, 450 (80.4%) isolates were susceptible to the antibiotic, and none of them possessed the blaKPC gene.
Real-time PCR detection of the blaKPC gene
All 110 K. pneumoniae isolates were successfully amplified utilizing primers and probes that targeted the blaKPC gene using real-time qPCR on the CFX 96 System (Bio-Rad, Hercules, CA, USA). Positive amplification of the blaKPC gene was observed, with Ct values ranging from 12 to 32 confirming the molecular presence of the resistance gene (Figure 6). No amplification was observed in the NTCs, confirming the absence of contamination. Amplification of 16S rRNA consistently occurred in all template wells. A FAM-labeled probe was used to detect the blaKPC gene, while a CY5-labeled probe was used to detect the 16S rRNA gene, which served as an internal control. A distinct melt peak was observed at approximately 77°C, confirming the specificity of the amplified product. The uniform melting profiles across samples further validated the consistency and specificity of amplification. No nonspecific products or primer–dimers were detected. The melt curves were generated using the CFX96 Touch™ Real-Time PCR Detection System (Bio-Rad, Hercules, CA, USA) (Figure 7). The Ct values for the 110 isolates are shown in a Supplementary File.
Figure 6
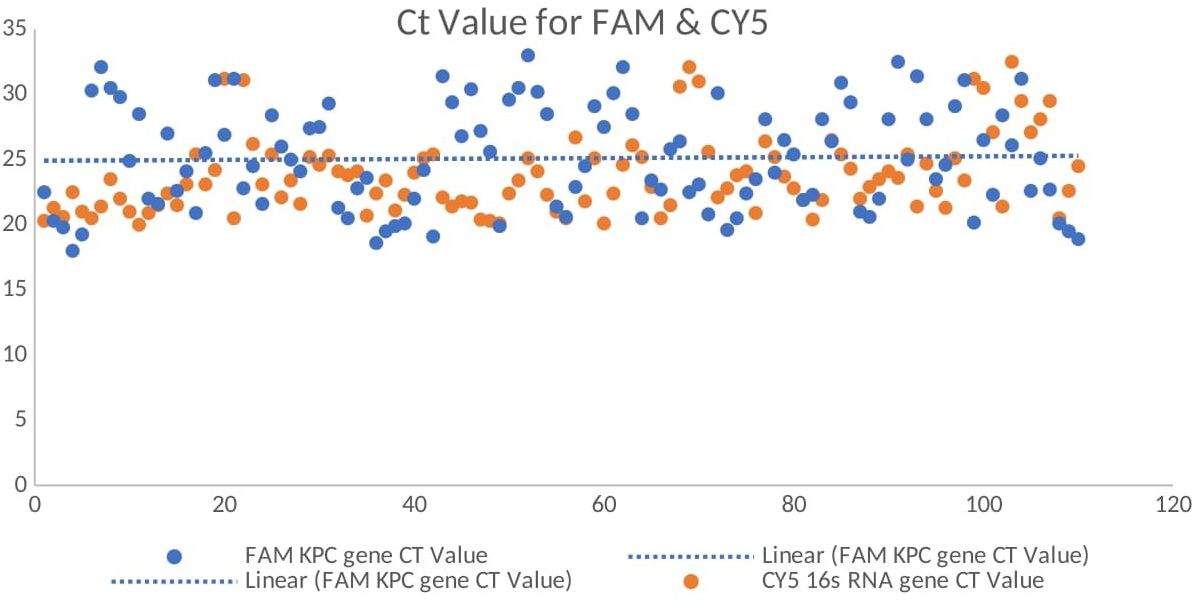
Real-time quantitative reverse transcription PCR (qRT-PCR) amplification curves showing the Ct values for the blaKPC gene (FAM channel) and the 16S rRNA gene (CY5 channel, internal control) among the Klebsiella pneumoniae isolates.
Figure 7
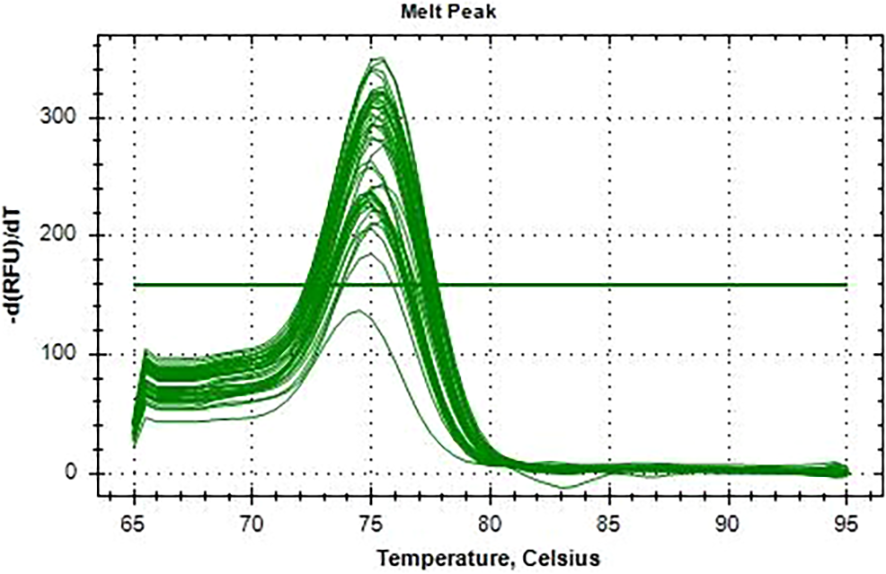
Melting curve analysis of the blaKPC amplicons from the 110 Klebsiella pneumoniae isolates. A single melt peak at ~77°C confirms the specificity of the amplified product.
The receiver operating characteristic (ROC) curve exhibited exceptional diagnostic performance, with an area under the curve (AUC) of 0.99 and nearly perfect sensitivity and specificity. It was possible to distinguish between isolates that were blaKPC-positive and blaKPC-negative using real-time PCR assay. Figure 8 displays the sensitivity analysis results.
Figure 8

Receiver operating characteristic (ROC) curve demonstrating the excellent diagnostic performance of the quantitative PCR (qPCR) assay, with an area under the curve (AUC) of 0.99, indicating near-perfect ability to distinguish between blaKPC-positive and blaKPC-negative isolates.
Discussion
A serious health concern that affects disease control in both industrialized and developing nations due to the high rates of antibiotic abuse and improper infection control is the increase in CRKP infections. In this study, the proportion of K. pneumoniae isolates that expressed blaKPC was 19.6%. KPC is the most widespread carbapenemase reported in India. Veeraraghavan et al. (2017) found an increase in K. pneumoniae carbapenem resistance from 9% to 14% in India during 2008 and 2010. Albiger et al. (2015), as well as the CDDEP, reported more than 60% resistance in Indian isolates and highlighted the widespread presence of blaKPC and blaNDM as two of the most common carbapenemase genes. It is important that hospitals in India monitor the prevalent carbapenemases in every region in order to demonstrate shifts in the trend from NDM enzymes to OXA-48. Greece has the highest rate of carbapenem resistance in the world, at 68%. This is followed by India and the Eastern Mediterranean, with resistance rates of 54% each (WHO 2014). The carbapenemase mechanisms of carbapenem resistance and KPC have particular limited options in the management of infections due to the reduced treatment options with antimicrobials (Lan et al., 2021).
The results in this study showed a high rate of resistance to the major antimicrobials: AMP (100%), CAZ (92.7%), CIP (91.8%), and AZT (89.1%). These results correlate with other studies that found high multidrug resistance in KPC-producing Enterobacterales (Mutuku et al., 2022; Tamma et al., 2023; Bashir et al., 2023). Notably, our findings showed significantly reduced resistance rates to aminoglycosides (gentamicin, 54%; AN, 60%) and carbapenems (IMI, 44%; MEM, 44%) compared with those of other regional studies (Albiger et al., 2015), implying potential institutional discrepancies with regard to the antimicrobial prescribing habits and the infection control procedures.
We demonstrated the potential utility of a real-time PCR assay that specifically detects the blaKP gene, which resolved these challenges and showed an unmatched accuracy, with a Ct value range of 12–32 and an AUC of 0.99. This supports the results of Wang et al. (2012), who showed that diagnostic tests based on molecular techniques yield better results than traditional phenotypic tests, especially with regard to the early identification and control of KPC-producing strains in hospital environments.
The precision of the molecular recognition of the blaKPC pathogen using qPCR is swift, with a turnaround time of 2–3 h, which is critical for the adoption of a suitable treatment. We are in agreement with the recent studies by Mangold et al. (2011) and Hindiyeh et al. (2008) on the importance of molecular technologies in early-stage diagnoses in the context of preventing the progression of infectious diseases. Furthermore, the fact that the 16S rRNA gene was amplified in each reaction indicates that there is no PCR inhibition and that the bacterial DNA is still intact. The rapid detection of blaKPC genes is of utmost importance as these MDR organisms have the potential to spread rapidly in hospital settings and cause nosocomial infections with high death rates (Samra et al., 2007). The diagnosis of carbapenem-resistant organisms has been problem as some of the isolates have a low expression of resistance, which may not be screened via conventional automated and non-automated procedures. blaKPC resistance genes have been rapidly detected using molecular techniques on samples taken directly from patients. We have adapted a fast, sensitive, and specific qPCR assay for the detection of blaKPC genes in wound samples. The assay can be completed in less than 3 h, which will assist in speeding up the process, thereby decreasing the possibility of the transmission of the organism within hospitals. This is in contrast to the time-consuming, less sensitive, and non-standardized methods of culturing bacteria, which may take over 24 h to identify carbapenem-resistant bacteria (Landman et al., 2005; Solanki et al., 2013). qPCR avoids the possibility of post-PCR contamination and all post-PCR requirements of the method, including gel electrophoresis (Hindiyeh et al., 2005). blaKPC genes have been reported in the United States, and further reports have affirmed their presence in Europe, Latin America, China, and India. The capacity of KPC-producing populations to spread through plasmids and other mobile genetic components is of real concern for the horizontal transmission of the gene within Enterobacterales (Chen et al., 2014). These findings concur with those of Albiger et al. (2015), which confirmed the unparalleled predominance of KPC in Asia and the pervasive dispersion of KPC-producing strains that lead the carbapenemase system in the majority of locations.
This study was focused on the blaKPC gene rather than on the investigation of other key genes such as blaNDM, blaOXA, and blaVIM, which are also common in India. Multiplex PCR, as well as other multi-gene detection procedures, might therefore provide a more detailed resistance profile. Secondly, this is a single-site study; hence, the results might not represent other areas. Thirdly, no clinical data were gathered that would have demonstrated significant findings pertaining to patient outcomes, length of stay, or treatment response, which would have provided valuable insights into the clinical implications of KPC-producing isolates. Despite such limitations, the critical significance of real-time PCR in daily diagnostic laboratories, especially in high-burden countries, can hardly be ignored. The identification of KPC-positive isolates can prevent the unnecessary use of carbapenem-based empirical therapy by allowing a targeted, prioritized use of empirical therapy and preventing nosocomial outbreaks.
The novelty of this study lies in its demonstration of the utility of a rapid, sensitive, and specific qPCR assay for the detection of the blaKPC gene in clinical wound isolates of K. pneumoniae. With a turnaround time of less than 3 h and a diagnostic accuracy reflected by an AUC of 0.99, this approach offers a superior alternative to conventional culture-based or phenotypic methods that are often time-consuming and less reliable.
Conclusion
This study found a significant prevalence of MDR and KPC-producing K. pneumoniae in wound infections, with only a few therapeutic choices due to widespread resistance. These findings highlight the importance of the routine implementation of molecular diagnostics such as real-time PCR for the timely identification of high-risk clones. Future research should concentrate on whole-genome sequencing of resistant isolates to identify new resistance determinants, assess clonal propagation, and inform infection control measures.
Statements
Data availability statement
The raw data has been deposited here: Zenodo Research data repository Version v110.5281/zenodo.17060580.
Ethics statement
The study was approved by the Damesh Institute of Research Committee on Bio-Ethics Approval No. DIRDC/304/41; Date: 6 April 2023). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
BA: Formal analysis, Writing – original draft, Resources, Investigation, Conceptualization, Methodology, Validation. SF: Software, Writing – review & editing, Investigation, Project administration, Methodology, Formal analysis, Supervision. FS: Visualization, Investigation, Validation, Project administration, Supervision, Resources, Formal analysis, Writing – review & editing. BT: Writing – review & editing, Methodology, Writing – original draft, Investigation.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Acknowledgments
Bader S. Alotaibi gratefully acknowledges the Deanship of Scientific Research at Shaqra University for supporting this work.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frabi.2025.1700157/full#supplementary-material
References
1
Adhikari R. P. Shrestha S. Richhinbung Rai J. Amatya R. (2018). Antimicrobial resistance patterns in clinical isolates of Enterobacteriaceae from a tertiary care hospital, Kathmandu, Nepal. Nepalese Med. J.1, 45–50. doi: 10.3126/nmj.v1i2.21578
2
Albiger B. Glasner C. Struelens M. J. Grundmann H. Monnet D. L. European Survey of Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) Working Group (2015). Carbapenemase-producing Enterobacteriaceae in Europe: assessment by national experts from 38 countries, May 2015. Eurosurveillance20, 30062. doi: 10.2807/1560-7917.ES.2015.20.45.30062
3
AlTamimi M. AlSalamah A. AlKhulaifi M. AlAjlan H. (2017). Comparison of phenotypic and PCR methods for detection of carbapenemase production by Enterobacteriaceae. Saudi J. Biol. Sci.24, 155–161. doi: 10.1016/j.sjbs.2016.02.009
4
Bashir N. Dablool A. S. Khan M. I. Almalki M. G. Ahmed A. Mir M. A. et al . (2023). Antibiotics resistance as a major public health concern: A pharmaco-epidemiological study to evaluate prevalence and antibiotics susceptibility-resistance pattern of bacterial isolates from multiple teaching hospitals. J. Infection Public Health16, 61–68. doi: 10.1016/j.jiph.2023.09.009
5
Bina M. Pournajaf A. Mirkalantari S. Talebi M. Irajian G. (2015). Detection of the Klebsiella pneumoniae carbapenemase (KPC) in K. pneumoniae isolated from clinical samples by phenotypic and genotypic methods. Iranian J. Pathol.10, 190–197.
6
Chen L. Mathema B. Chavda K. D. DeLeo F. R. Bonomo R. A. Kreiswirth B. N. (2014). Carbapenemase-producing Klebsiella pneumoniae: molecular and genetic decoding. Trends Microbiol.22, 686–696. doi: 10.1016/j.tim.2014.09.003
7
Clinical and Laboratory Standards Institute (CLSI) (2024). “ Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically,” in CLSI standard M07, 12th edn ( Clinical and Laboratory Standards Institute, Wayne, PA).
8
Clinical and Laboratory Standards Institute (CLSI) (2025). “ Performance standards for antimicrobial disc susceptibility testing,” in CLSI supplement M100, 35th edn ( Clinical and Laboratory Standards Institute, Wayne, PA).
9
Darby E. M. Trampari E. Siasat P. Gaya M. S. Alav I. Webber Blair M. A. J. M. A. et al . (2024). Author Correction: Molecular mechanisms of antibiotic resistance revisited. Nat. Rev. Microbiol.22, 255. doi: 10.1038/s41579-024-00825-1
10
Dong N. Li R. Lai Y. (2022). Klebsiella pneumoniae: antimicrobial resistance, virulence and therapeutic strategies. Front. Cell. Infection Microbiol.12. doi: 10.3389/fcimb.2022.00012
11
Gandor N. H. M. Amr G. E.-S. Eldin Algammal S. M. S. Ahmed A. A. (2022). Characterization of carbapenem-resistant Klebsiella pneumoniae isolated from intensive care units of Zagazig University hospitals. Antibiotics11, 1108. doi: 10.3390/antibiotics11081108
12
Giacobbe D. R. Di Pilato V. Karaiskos I. Giani T. Marchese A. Rossolini G. M. et al . (2023). Treatment and diagnosis of severe KPC-producing Klebsiella pneumoniae infections: a perspective on what has changed over the last decades. Ann. Med.55, 101–113. doi: 10.1080/07853890.2023.2184169
13
Hindiyeh M. Levy V. Azar R. Varsano N. Regev L. Shalev Y. et al . (2005). Evaluation of a multiplex real-time reverse transcriptase PCR assay for detection and differentiation of influenza viruses A and B during the 2001–2002 influenza season in Israel. J. Clin. Microbiol.43, 589–595. doi: 10.1128/JCM.43.2.589-595.2005
14
Hindiyeh M. Smollen G. Grossman Z. Ram D. Davidson Y. Mileguir F. et al . (2008). Rapid detection of blaKPC carbapenemase genes by real-time PCR. J. Clin. Microbiol.46, 2879–2883. doi: 10.1128/JCM.00566-08
15
Huang W. Qiao F. Deng Y. Zhu S. Li J. Zong Z. et al . (2023). Analysis of risk factors associated with healthcare-associated carbapenem-resistant Klebsiella pneumoniae infection in a large general hospital: a case-case-control study. Eur. J. Clin. Microbiol. Infect. Dis.42, 529–541. doi: 10.1007/s10096-023-04612-7
16
Johnson A. P. Woodford N. (2013). Global spread of antibiotic resistance: the example of New Delhi metallo-β-lactamase (NDM)-mediated carbapenem resistance. J. Med. Microbiol.62, 499–513. doi: 10.1099/jmm.0.052555-0
17
Koshi M. (2001). Myer’s and Koshi’s Manual of Diagnostic Procedures in Medical Microbiology and Immunology/Serology (Vellore, India: Christian Medical College and Hospital).
18
Lan P. Jiang Y. Zhou J. Yu Y. (2021). A global perspective on the convergence of hypervirulence and carbapenem resistance in Klebsiella pneumoniae. J. Global Antimicrobial. Resistance25, 26–34. doi: 10.1016/j.jgar.2021.03.011
19
Landman D. Salvani J. K. Bratu S. Quale J. (2005). Evaluation of techniques for detection of carbapenem-resistant Klebsiella pneumoniae in stool surveillance cultures. J. Clin. Microbiol.43, 5639–5641. doi: 10.1128/JCM.43.11.5639-5641.2005
20
Mangold K. A. Santiano K. Broekman R. Krafft C. A. Voss B. Wang V. et al . (2011). Real-time detection of blaKPC in clinical samples and surveillance specimens. J. Clin. Microbiol.49, 3338–3339. doi: 10.1128/JCM.00516-11
21
Mutuku C. Gazdag Z. Melegh S. (2022a). Occurrence of antibiotics and bacterial resistance genes in wastewater: resistance mechanisms and antimicrobial resistance control approaches. World J. Microbiol. Biotechnol.38, 123. doi: 10.1007/s11274-022-03292-7
22
Mutuku C. Melegh S. Kovacs K. Urban P. Virág E. Heninger R. et al . (2022b). Characterization of β-lactamases and multidrug resistance mechanisms in enterobacterales from hospital effluents and wastewater treatment plant. Antibiotics (Basel)11, 776. doi: 10.3390/antibiotics11060776
23
Papanikolopoulou A. Vini L. Stoupis A. Kalimeri D. Pangalis A. Chronopoulou G. et al . (2024). Carbapenem-resistant Klebsiella pneumoniae bacteremia: counterbalance between the endemic load and the infection control program in a hospital. Acta Microbiologica Hellenica69, 81–92. doi: 10.12681/amh.31254
24
Parveen R. M. Harish B. N. Parija S. C. (2010). Emerging carbapenem resistance among nosocomial isolates of Klebsiella pneumoniae in South India. Int. J. Pharma Bio Sci.1, 1–11.
25
Richter S. N. Frasson I. Franchin E. Bergo C. Lavezzo E. Barzon L. et al . (2012). KPC mediated resistance in Klebsiella pneumoniae in two hospitals in Padua, Italy, June 2009- December 2011: massive spreading of a KPC-3-encoding plasmid and involvement of non- intensive care units. Gut Pathogens4, 7. doi: 10.1186/1757-4749-4-7
26
Samra Z. Ofir O. Lishtzinsky Y. Madar-Shapiro L. Bishara J. (2007). Outbreak of carbapenem-resistant Klebsiella pneumoniae producing KPC-3 in a tertiary medical centre in Israel. Int. J. Antimicrobial. Agents30, 525–529. doi: 10.1016/j.ijantimicag.2007.07.012
27
Solanki R. Vanjari L. Ede N. Gungi A. Soory A. Vemu L. (2013). Evaluation of LAMP assay using phenotypic tests and conventional PCR for detection of blaNDM-1 and blaKPC genes among carbapenem-resistant clinical Gram-negative isolates. J. Med. Microbiol.62, 1540–1544. doi: 10.1099/jmm.0.056644-0
28
Tamma P. D. Aitken S. L. Bonomo R. A. Mathers A. J. van Duin D. Clancy C. J. (2023). Infectious Diseases Society of America 2023 guidance on the treatment of antimicrobial-resistant Gram-negative infections. Clin. Infect. Dis.76, ciad428. doi: 10.1093/cid/ciad428
29
Tamma P. D. Heil E. L. Justo J. A. Mathers A. J. Satlin M. J. Bonomo R. A. (2024). Infectious Diseases Society of America 2024 guidance on the treatment of antimicrobial-resistant Gram-negative infections. Clin. Infect. Dis.78, ciae403. doi: 10.1093/cid/ciae403
30
Van Duin D. Paterson D. L. (2020). Multidrug resistant bacteria in the community: an update. Infect. Dis. Clinics North America34, 709–722. doi: 10.1016/j.idc.2020.07.002
31
Veeraraghavan B. Shankar C. Karunasree S. Kumari S. Ravi R. Ralph R. (2017). Carbapenem-resistant Klebsiella pneumoniae isolated from bloodstream infection: Indian experience. Pathog. Global Health111, 240–246. doi: 10.1080/20477724.2017.1340247
32
Wang L. Gu H. Lu X. (2012). Rapid low-cost detection of Klebsiella pneumoniae carbapenemase genes by internally controlled real-time PCR. J. Microbiological Methods91, 361–363. doi: 10.1016/j.mimet.2012.08.010
33
World Health Organization . (2014). Antimicrobial resistance: Global report on surveillance 2014. World Health Organization. https://iris.who.int/handle/10665/112642
34
Zhou M. Wang D. Kudinha T. Yang Q. Yu S. Xu Y.-C. (2018). Comparative evaluation of four phenotypic methods for detection of class A and B carbapenemase- producing Enterobacteriaceae in China. J. Clin. Microbiol.56, e00395–18. doi: 10.1128/JCM.00395-18
Summary
Keywords
Klebsiella pneumoniae , antimicrobial resistance, blaKPC gene, real-time PCR, meropenem resistance
Citation
Alotaibi BS, Syed F, Almufarriji FM and Tantry BA (2026) Antimicrobial resistance and real-time PCR detection of blaKPC in Klebsiella pneumoniae isolated from wound infections in a tertiary care hospital. Front. Antibiot. 4:1700157. doi: 10.3389/frabi.2025.1700157
Received
06 September 2025
Revised
03 November 2025
Accepted
09 December 2025
Published
27 January 2026
Volume
4 - 2025
Edited by
Yusuf Oloruntoyin Ayipo, Kwara State University, Nigeria
Reviewed by
Arunagirinathan Narasingam, Meenakshi Academy of Higher Education and Research, India
Wadhah Hassan Edrees, Hajjah University, Yemen
Updates
Copyright
© 2026 Alotaibi, Syed, Almufarriji and Tantry.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bilal Ahmad Tantry, bilaltantry@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.